Abstract
Objective
Neurodevelopmental theories of psychosis highlight the potential benefits of early intervention, prevention, and/or preemption. How early intervention should take place has not been established, nor if interventions based on social learning principles can have preemptive effects. The objective was to test if a comprehensive psychosocial intervention can significantly alter psychotic symptom trajectories during adolescence – a period of heightened risk for a wide range of psychopathology.
Method
This study was a randomized controlled trial (RCT) of Multidimensional Treatment Foster Care (MTFC) for delinquent adolescent girls. Assessment of psychotic symptoms took place at baseline and then 6, 12, 18, and 24 months post-baseline using a standardized self-report instrument (Brief Symptom Inventory). A second source of information about psychotic symptoms was obtained at baseline or 12 months, and again at 24 months using a structured diagnostic interview (the Diagnostic Interview Schedule for Children [DISC]).
Results
Significant benefits for MTFC over treatment-as-usual for psychosis symptoms were observed over a 24-month period. Findings were replicated across both measures. Effects were independent of substance use and initial symptom severity, and persisted beyond the initial intervention period.
Conclusion
Ameliorating non-clinical psychotic symptoms trajectories beginning in early adolescence via a multifaceted psychosocial intervention is possible. Developmental research on non-clinical psychotic symptoms and their prognostic value should be complemented by more psychosocial intervention research aimed at modifying these symptom trajectories early in their natural history.
Keywords: psychotic symptoms, RCT, MTFC, juvenile justice, girls
Introduction
Childhood psychotic symptoms have been considered relatively benign and of little prognostic value. However, over the last 10–15 years, several studies have shown that ‘non-clinical’ psychotic symptoms reported in late childhood and/or early- to mid-adolescence predict psychotic disorders in adulthood, with odds ratios as high as 16.1–3 Early-emerging psychotic symptoms share many of the same features observed in adult psychotic disorders including early environmental and social risks (e.g., childhood maltreatment, psychosocial adversity, obstetric complications); cognitive, linguistic, and psychomotor deficits; similar brain morphology and patterns of psychiatric comorbidity; shared genetic influences; and familiality.4–10
This raises the question of whether it is possible to treat very early emerging psychotic symptoms and thus prevent some of the negative consequences that these symptoms appear to foretell. This question is particularly salient when applied to psychosis specifically because pharmaceutical treatments for clinical psychosis have limited benefit and fail to ameliorate symptoms in up to 50% of sufferers.11 This has motivated attempts to intervene earlier in the disease process, especially because the worst prognosis is associated with longer periods of untreated disease.12,13 For example, the ‘ultra-high-risk’ (UHR) concept is now well recognized in the psychosis field, describing non-diagnosed but unwell patients who are at incipient risk of developing overt psychosis.11,14 These patients have been shown to benefit from early, staged psychosocial interventions.15
Extending the rationale for UHR intervention, we posit that treating earlier, perhaps milder, expressions of psychosis may also reap benefits. A recent systematic review and meta-analysis showed positive effects, highlighting cognitive-behavioral therapy (CBT) augmented by family therapy as the most promising approach.16 However, the clinical trials included in this meta-analysis were restricted to patients seeking treatment, suggesting that non-trivial levels of disability were already present—a point in the disease process that is likely to have been preceded by a lengthy prodromal period of between three to six years.
One small case series demonstrated some benefits of individualized CBT among those with non-clinical psychotic symptoms;17 however, we are unaware of any randomized controlled trials (RCTs) of psychosocial interventions aimed at modifying the course of psychotic symptoms in adolescents who were not selected for psychosis symptoms. In the present study, we investigated the possibility that an existing RCT with multiple follow-up assessments post-intervention would reduce psychotic symptoms in a sample that was not selected for psychotic symptoms but who had elevated risk histories. The sample was comprised of delinquent girls with histories of significant abuse and neglect, two well-established risk factors for adult psychosis.18–21
Multidimensional Treatment Foster Care (MTFC)
Reduction of psychotic symptoms among delinquent youth might occur via methods that effectively treat their behavioral problems, given that these problems tend to co-occur and share some etiological and maintaining factors.8,10,22–24 MTFC is an efficacious family-based intervention for delinquency that is based on social learning theory.25 Youth in MTFC are placed in homes with foster parents trained to implement a behavioral reinforcement model. Youth attend public school and receive intensive support and intervention in settings that closely parallel normal life. Parents or other caregivers with whom youth live after treatment are also trained in effective parenting skills. Thus, MTFC aims to permanently change the contexts that support problem behaviors.
MTFC is an effective intervention for delinquency among girls.26,27 Specifically, girls receiving MTFC compared to those receiving community group care (GC) treatment-as-usual showed reduced delinquency (as indexed by rates of criminal referrals, days in locked settings, self-reported delinquency) at 24-month follow-up.26 Furthermore, other beneficial MTFC effects persist beyond the intervention period, including decreased associations with deviant peers,28 reduced rates of teenage pregnancy,29 and reduced depression.30
MTFC does not directly target psychotic symptoms. Still, such effects are plausible given some shared etiological features (e.g., abuse and neglect), and similar patterns of sequential comorbidity (i.e., diagnoses of juvenile conduct disorder/oppositional defiant disorder precede a range of adult psychiatric diagnoses, including schizophreniform disorder).31 This study sought to test whether MTFC has beneficial effects on adolescent psychotic symptoms. We hypothesized that girls randomly assigned to MTFC, compared to those assigned to a treatment-as-usual control condition, would show significantly greater declines in their trajectories of psychotic symptoms across adolescence.
Method
Participants
Girls (N = 166) participated in an RCT in one of two consecutively run cohorts (n = 81 and 85 for cohorts 1 and 2, respectively) conducted in the Northwestern United States between 1997 and 2006 to contrast MTFC and GC (i.e., services-as-usual). Participants had been court-mandated to community-based out-of-home care due to chronic delinquency. We attempted to enroll all referred girls ages 13–17 who had at least one criminal referral in the last 12 months, were placed in out-of-home care within 12 months after referral, and who were not pregnant at the time of recruitment. Girls provided assent, and their legal guardian provided consent to participate. The project coordinator randomly assigned girls to MTFC (n = 81) or GC (n = 85) using a coin toss. Examination of baseline characteristics (criminal referrals, alcohol, marijuana, and other illicit drug use, and demographic information including ethnicity, age, maltreatment history, single parent family, income parent criminality) indicated no significant differences between groups (all p > .10), suggesting the general success of the randomization process. After the baseline assessment, girls were placed in their randomized intervention setting. The mean length of stay in the randomized intervention setting was approximately 6 months and did not differ by condition. Clinical and assessment staff members were independent, and the latter were blind to intervention assignment at all timepoints. Assessment staff blinding could have been compromised during the post-baseline intervention period if girls were assessed in a treatment setting, although during this period some MTFC girls spent time in GC and some GC girls spent time in non-MTFC foster care. Intent to treat (ITT) analyses included the entire sample, regardless of time in assigned intervention setting.
Participating girls were 13–17 years old at baseline (M = 15.30, SD = 1.17); the sample self-identified as follows: 68.1% Caucasian, 1.8% African-American, 11.4% Hispanic, 0.6% Native American, and 0.6% Asian; 16.9% “multiracial” and 0.6% “other/unknown.” Prior 2-year follow-up studies of this sample29 had to rely on caregiver or caseworker reports of girls’ race/ethnicity in many cases. The present percentages were updated with self-reports collected in early adulthood and thus differ slightly from manuscripts that went to press prior to 2013. At baseline, 63% of the girls lived with single-parent families and 54% lived in families earning less than $10,000.
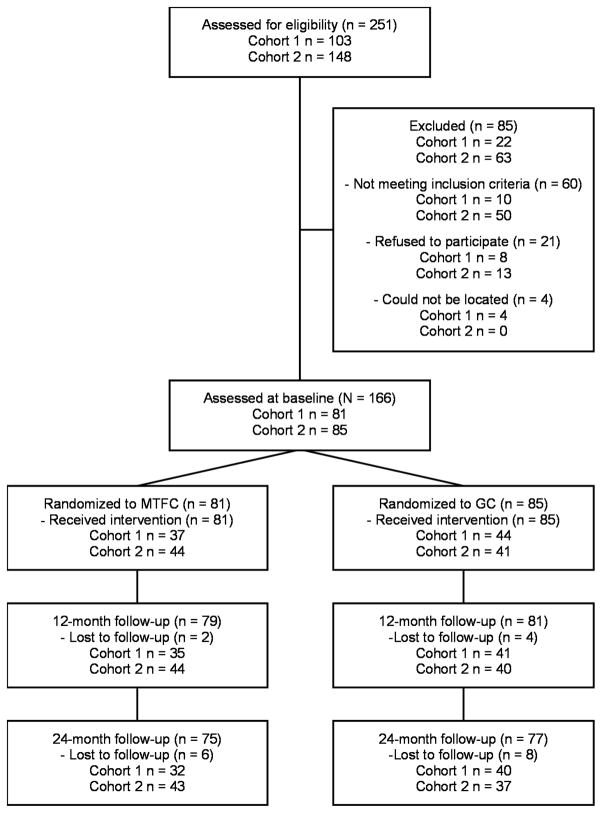
Girls were assessed regularly for 24–36 months post-baseline as part of the original RCTs. Analyses accommodated individual and cohort differences in assessment timing, as detailed below. Figure 1 depicts the CONSORT subject flow chart for the overall study; though sample sizes differed for some outcomes, our use of ITT and full information maximum likelihood in primary analyses makes use of data on the full sample. The original RCT and follow-up assessments were approved and regularly reviewed by the senior author’s institutional review board.
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) diagram of participant flow in the overall study through study recruitment, randomization to Multidimensional Treatment Foster Care (MTFC) or group care (GC), and follow-up for participants in cohorts 1 and 2.
MTFC condition
Girls in MTFC were placed in one of 22 homes with state-certified foster parents trained to implement a behavioral reinforcement program (e.g., point-and-level system). Experienced program supervisors with small caseloads supervised all clinical staff, coordinated all aspects of each youth’s placement, and maintained daily contact with foster parents to provide ongoing consultation, support, crisis intervention, and monitor treatment fidelity. Interventions were individualized but always included daily telephone contact with foster parents; weekly group supervision and support meetings for foster parents; an in-home, daily point-and-level program for girls; individual therapy for each girl; family therapy for the aftercare placement family focusing on parent management strategies; close monitoring of school attendance, performance, and homework completion; case management to coordinate the interventions in the foster family, peer, and school settings; and 24-hr on-call staff support for foster and biological parents. The individual therapy sessions focused on helping girls identify specific stressors, tracking the occurrence of symptoms, normalizing the presence of symptoms (given the trauma history), and role-playing coping responses. In cohort 2, MTFC also included components targeting substance use (e.g., motivational interviewing and incentives for clean urinalyses) and risky sexual behavior (e.g., information on behavior norms, and education and instruction about strategies for being sexually responsible). Otherwise, MTFC components were the same in cohorts 1 and 2.
Group care condition
Girls in GC were placed in intensive out-of-home care settings, with 24/7 care. These community-based group care programs represented community treatment as usual for girls being referred to out-of-home care by the juvenile justice system (n = 35 unique GC settings). Programs had 2–83 youths in residence (M = 13) and 1–85 staff members (Mdn = 9). Program philosophies were primarily behavioral (67%) or multi-perspective (33%); 80% of the programs reported delivering weekly therapeutic services. Sites either required on-grounds schooling (41%), sent only some girls to school off-grounds (38%), or sent all girls to off-grounds school (21%). Kerr et al.29 provides further details.
Measures
Psychotic symptoms
We included two measures of psychotic symptoms; one measure was collected at 5 time points over the first 24 months post-baseline (the Brief Symptom Inventory [BSI]: Psychotic Subscale)32 and was used in growth modeling analyses, and one measure was collected twice over the first 24 months of the study and was examined as an outcome controlling for earlier symptoms (the Diagnostic Interview Schedule for Children-IV [DISC-IV]: psychotic symptoms.).33
The BSI is the short form of the SCL-90R instrument, both of which have typically been used as objective methods of screening for psychological problems and measuring treatment progress. The psychosis subscale was computed as the mean of five items rated on a 5-point Likert-type scale from 1 (not at all) to 5 (very much). The five items assessed whether the participant felt in the last week that: (1) someone else was controlling her thoughts; (2) she was lonely even when with others; (3) she should be punished for her sins; (4) she never felt close to another person; and (5) something was wrong with her mind. Cronbach’s alphas were .70, .68, .76, .71, and .80, respectively, over five waves (0–3 mo; 6 mo; 12-mo; 18-mo; 24-mo.). In our analysis, we used the T-score form of this measure. Clinical prevalence rates (T-score ≥ 63) were 18%, 10%, 6%, 4%, and 5% for the five waves, respectively.
The DISC-IV is a diagnostic interview that was designed to be administered by clinically untrained interviewers and covers diagnostic criteria from the DSM-IV, the DSM-III-R, and the International Classification of Diseases, 10th Revision (ICD-10). Test-retest kappas range from .10 to .39; validity kappas range from .27 to .79. The DISC-IV was measured at baseline and 24 months for cohort I, and 12 and 24 months for cohort II. In our analysis, we used the count of the 22 psychotic symptoms at each DISC-IV assessment. Sample items include having visions, hearing things others didn’t hear, believing people were plotting against you, and believing that others were stealing your thoughts. Forty-three percent of the sample endorsed at least 1 symptom at the first assessment and 24% endorsed at least 1 symptom in the second assessment.
Predictor variables
Intervention group assignment was coded 0 (GC) or 1 (MTFC). We also included several covariates in the models, including baseline marijuana use (rated on a Likert-type scale from 1 [never] to 5 [1 or more times/day]), age at baseline (calculated based on birth date and baseline assessment date), and ethnicity (coded as 1 [Caucasian] and 0 [other]).
Analysis Plan
The main study hypotheses were evaluated with growth curve modeling with the BSI symptom data using Mplus.31 Mplus makes use of maximum likelihood analysis, which can provide unbiased estimates in the presence of missing data. Maximum likelihood is considered to be one of the most robust methods for handling missing data and is superior to list-wise deletion, which can introduce bias.35 In calculating the growth curve parameters for psychotic symptoms, we accounted for individual variations in assessment times (for example, the collection of the second or “6-month” wave ranged from 3 to 10 months after the baseline assessment, even though the target was 6 months). Mplus does not provide standard indices of fit or standardized coefficients for models where individuals have time-varying assessment points or count-based outcome variables, so none are reported.
We specified the time metric for estimating growth rates using each girl’s person-specific assessment timeline. We initially fitted an unconditional model to evaluate the shape of the curve, then added intervention condition as a predictor of the growth curve slope. This model also controlled for baseline marijuana use, baseline age, and ethnicity. Separate intercept and slope factors were included, which allowed us to assess the intervention effects on slope independent of baseline (intercept) symptoms. In a second set of models, we estimated psychotic symptom counts with the DISC-IV at 24 months while controlling for earlier psychotic symptom count, baseline marijuana use, baseline age, and ethnicity. Since the outcome was count-based, we used Poisson regression in the DISC-IV models.
Results
Descriptive Statistics
Table 1 provides correlations and descriptive information using approximate assessment waves. There was a degree of missing data, but Little’s Missing Completely At Random (MCAR) test36 was not significant (χ2[76] = 71.15, ns), which indicates that the missing data did not introduce bias into the analyses.
Table 1.
Means, Standard Deviations, and Intercorrelations of Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. MTFC condition | - | ||||||||||
| 2. Baseline marijuana use | −.08 | - | |||||||||
| 3. Baseline age | .01 | −.05 | - | ||||||||
| 4. Ethnicity | .07 | −.01 | −.08 | - | |||||||
| 5. BSI Psychotic symptoms (0–3 mo) | .19* | .07 | −.05 | .11 | - | ||||||
| 6. BSI Psychotic symptoms (6 mo) | .04 | −.01 | −.03 | −.01 | .53*** | - | |||||
| 7. BSI Psychotic symptoms (12 mo) | −.03 | −.08 | −.05 | .03 | .30*** | .46*** | - | ||||
| 8. BSI Psychotic symptoms (18 mo) | .05 | −.08 | −.10 | −.12 | .33*** | .34*** | .50*** | - | |||
| 9. BSI Psychotic symptoms (24 mo) | −.08 | −.03 | −.03 | −.05 | .21* | .38*** | .35*** | .56*** | - | ||
| 10. DISC Psychotic symptoms (0–12 mo) | −.15 | .12 | −.01 | −.19* | .04 | .25** | .25** | .31*** | .18* | - | |
| 11. DISC Psychotic symptoms (24 mo) | −.12 | .02 | −.06 | .08 | .10 | .20* | .28** | .27** | .24** | .37*** | - |
|
| |||||||||||
| M (Med) | .49 | 2.97 | 15.30 | .68 | 52.31 | 49.78 | 47.60 | 46.29 | 45.21 | .00 | .00 |
|
| |||||||||||
| SD (Range) | .50 | 1.36 | 1.17 | .47 | 10.41 | 10.14 | 10.19 | 9.34 | 9.81 | 3.00 | 2.00 |
|
| |||||||||||
| n | 166 | 163 | 166 | 166 | 160 | 158 | 140 | 139 | 132 | 158 | 133 |
Note. The Diagnostic Interview Schedule for Children (DISC) measure was count-based, so we report (a) Spearman’s correlation instead of Pearson’s correlation; (b) median instead of mean; and (c) range instead of standard deviation. BSI = Brief Symptom Inventory; MTFC = Multidimensional Treatment Foster Care.
p < .05.
p < .01.
p < .001.
Unconditional Growth Curve
The unconditional growth curve for psychotic symptoms included a positive intercept (51.84, SE = .76, p < .001) and a negative slope (−3.46, SE = .48, p < .001). The variance was significant for both intercept (60.99, SE = 12.61, p < .001) and slope (17.95, SE = 4.81, p < .001). The intercept and slope significantly and negatively covaried (coefficient = −19.54, SE = 6.86, p < .01). The standardized correlation coefficient was calculated to be −.59.
MTFC Effects on Trajectories of Psychotic Symptoms (BSI)
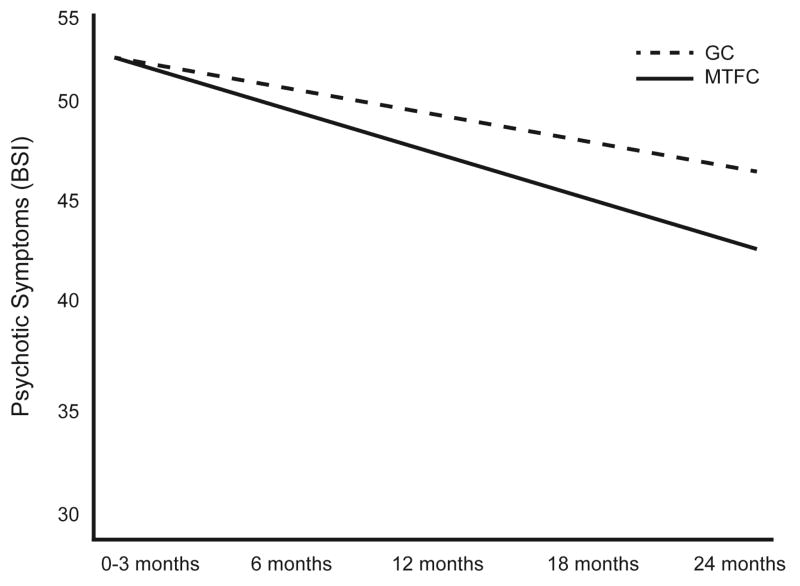
Results of the analysis are presented in Table 2. MTFC resulted in a significantly steeper decline in psychotic symptoms when compared to the GC condition. The raw coefficient for MTFC (−2.05) suggested that T-scores on the BSI were reduced by more than 2 points per year for the MTFC condition as compared to the GC condition. Age, ethnicity, and marijuana use were not significant predictors. The curves for the two groups are presented in Figure 2.
Table 2.
Unstandardized Model Coefficients for the Growth Curve and Poisson Regression Models
| Growth Curve (BSI) | Poisson Regression (DISC) | ||
|---|---|---|---|
|
| |||
| Coefficient (SE) | Coefficient (SE) | eCoefficient | |
| MTFC | −2.05* (.93) | −.65** (.22) | .52 |
| Baseline marijuana use | −.42 (.37) | −.42 (.37) | ns |
| Baseline age | .19 (.45) | .14 (.10) | ns |
| Ethnicity | −1.95 (1.08) | .30 (.23) | ns |
| Prior symptoms | - | .19*** (.03) | 1.21 |
Note. BSI = Brief Symptom Inventory; DISC = Diagnostic Interview Schedule for Children; MTFC = Multidimensional Treatment Foster Care; ns = not significant.
p < .05;
p < .01;
p < .001.
Figure 2.
Psychotic symptoms (Brief Symptom Inventory [BSI]) by group according to the growth curve analysis (see Table 2). Note: The graph assumes individuals with average (group mean) assessment intervals. GC = Group Care; MTFC = Multidimensional Treatment Foster Care.
MTFC Effects on Psychotic Symptoms (DISC-IV)
Results of the analysis are presented in Table 2. MTFC resulted in a significantly lower psychotic symptom count at 24 months when compared to the GC condition. The exponentiated regression coefficient suggested that MTFC girls reported roughly half the number of symptoms at 24 months as compared to GC girls, controlling for prior symptom counts (also a significant predictor). Age, ethnicity, and baseline marijuana use were not significant predictors.
Discussion
To our knowledge, this is the first report describing positive effects of an RCT on psychotic symptom trajectories among adolescents who were not selected for the presence of psychotic symptoms or via a psychosis high-risk approach. We observed significant benefits for MTFC over treatment-as-usual for psychosis symptoms that were independent of marijuana use and baseline severity and persisted beyond the intervention period. This follows publication of a small (n = 4) ‘proof of principle’ case series among children 9–14 years old demonstrating the efficacy of CBT for changing cognitive appraisals of psychotic-like experiences.17 Together, these findings raise hope that prevention and/or preemption of psychosis trajectories might be possible.37
MTFC was designed to address conduct problems and is effective in this regard.26,27 It comprises a comprehensive, multifaceted intervention program addressing a variety of environmental risks (e.g., the home environment) and teaches a range of coping skills, with plentiful opportunity for real-world application. The present findings are consistent with, but importantly extend, a growing literature showing that CBT is an effective intervention for those with first-episode psychotic disorder or deemed to be at ultra-high-risk,38, 39 as well as a recent review suggesting that CBT augmented by family therapy appeared to be the most promising approach for such at-risk patients.16 The findings are also consistent with a buffering effect of a positive family environment (indexed as higher levels of caregiver emotional involvement, positive remarks, and warmth), which predicted improvement in psychotic symptoms and social functioning among mainly adolescent patients.40 The present data suggest that to the extent that MTFC addresses key precipitants and/or maintaining factors for psychotic symptoms,41 improvement can also be expected among those not specifically seeking treatment for psychotic symptoms, but who may have a broad range of risk factors, including maltreatment.
The positive impact on psychotic symptom trajectories seen in the MTFC condition is likely due to both direct and indirect mechanisms.42 That is, beyond the direct effects on psychotic symptoms via, for example, reduced aversive expressed emotion in the home environment,43, 44 indirect effects may have operated via reduction in both delinquent and depressive symptoms.26,27,30 This is because both these disorders index reactivity to stress to some degree, and such reactivity can often lead to further stressors45 and/or unhelpful cognitive distortions.46 Thus, amelioration of these symptoms may have reduced the cumulative stress burden experienced by these young women, which in turn might explain their more marked decrease in psychotic symptoms over the 24-month period. This would also be consistent with the posited affective pathway to psychosis – one which underlines the potential importance of stressful family processes.46, 47 It also aligns with more recent data demonstrating a dynamic process of symptom reduction among adolescents reporting psychotic symptoms via cessation of trauma.23
Before considering the implications of these findings, we acknowledge the potential limitations of our study. Our sample was all-female, thus it is unknown whether the present findings also apply to males in similar circumstances. While it is known the men have early onset of psychotic disorder and slightly higher rates of schizophrenia during adulthood, our focus on adolescent girls may actually have been an advantage given recent data indicating higher base rates for psychotic symptoms reported by females at this age,48 as well as the over-representation of females in the highest risk trajectories for psychotic symptoms during adolescence.49 However, it is important to note that the majority of girls in this study showed subclinical levels of psychotic symptoms, even pre-treatment. A second limitation is that our psychotic symptom measures focused largely on positive symptoms, whereas negative symptoms and cognitive symptoms tend to be associated with worse long-term outcomes.50,51 Future studies should aim to measure all symptom types. However, these limitations should be viewed in the context of some notable strengths including the multiple, repeated measures of psychotic symptoms obtained via two methods (BSI, DISC-IV), the application of a high-quality MTFC intervention combined with a robust treatment-as-usual control group, and a comparatively high retention rate among this challenging adolescent group.
Mindful of these caveats, we believe our findings have implications for theory, research, clinical practice, and policy. With regard to theory and research, the neurodevelopmental theory of schizophrenia50,52,53 highlights the potential for, and value of, prevention efforts, and even the possibility of preemption.37 Until now, intervention work in this area has focused almost exclusively on preventing the transition into frank psychosis among those deemed at high or ultra-high risk.11 However, current interest in the predictive value of early psychotic experiences has begun to focus on the issue of specificity, with recent data indicating that psychotic symptoms may actually predict a wide range of psychopathology (i.e., not just psychosis), multiple co-occurring diagnoses, poorer social functioning in adulthood, and a massively increased risk for suicide attempts.6,23,54,55 For example, Fisher et al.55 reported from a prospective-longitudinal study that > 90% of those defined as having ‘strong’ psychotic symptoms at age 11 recorded at least one adult psychiatric diagnosis by age 38. Kelleher et al.23 found that adolescents with psychopathology who reported psychotic symptoms had nearly 70-fold increased odds of acute suicide attempt. As a result of these and other studies, interest in early psychotic experiences and their long-term sequelae has broadened to focus on the value of early psychotic symptoms as a harbinger of future poor psychiatric health more generally,55–57 as well as understanding homotypic (dis)continuities, as exemplified in the psychosis-proneness-persistence-impairment model of psychotic disorder.58 Our findings point to the value of complementing this important developmental research with greater investment in interventional prevention and preemption research.
With regard to clinical practice, treatments based on social learning principles have been found to work for psychosis,38 albeit with effect sizes varying with the rigor of the study. In contrast, the mainstay pharmacological treatments tend to have their greatest impact on positive symptoms, albeit with limited benefit for approximately half of these patients, and they are not effective in modifying negative psychotic symptoms such as apathy or anhedonia, nor do they improve cognitive symptoms (e.g., short-term memory problems, poor cognitive control), which together predict much of the later disability and poor social functioning seen in psychosis. Critically, psychosocial treatments can and do ameliorate these deficits.59
Implications for service-delivery policy are a hot topic of discussion and debate.60 Clearly, comprehensive psychosocial interventions delivered very early in the putative disease process could work to mitigate negative psychosis symptom trajectories and potentially avoid a lot of suffering for individuals and reduce considerable overall societal burden. Our results resonate with other calls for removal of multiple barriers to the routine application of psychosocial treatments for those suffering with psychosis,61 and the current data argue for going one step further to consider the potential benefits of comprehensive psychosocial approaches for very early-stage prevention and/or preemption.
Acknowledgments
This research received support from the Oregon Youth Authority and by the following grants: R01 DA015208, R01 DA024672, and P50 DA035763 (National Institute on Drug Abuse [NIDA]) and R01 MH054257 (National Institute of Mental Health [NIMH]).
Dr. Van Ryzin served as the statistical expert for this research.
The authors thank Courtenay Padgett, BA, of Oregon Social Learning Center, for project management; the team of interviewers and data management staff; and the study participants.
Footnotes
Disclosure: Dr. Chamberlain is a partner in TFC Consultants Inc., which disseminates multidimensional treatment foster care. Drs. Poulton, Ryzin, Harold, Cannon, Arseneault, and Leve and Mr. Fowler report no biomedical financial interests or potential conflicts of interest.
Clinical trial registration information—Juvenile Justice Girls Randomized Control Trial: Young Adult Follow-up; http://clinicaltrials.gov/; NCT01341626.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Richie Poulton, Dunedin Multidisciplinary Health and Development Research Unit, Dunedin School of Medicine, University of Otago, New Zealand.
Dr. Mark J. Van Ryzin, Oregon Social Learning Center, Eugene, OR.
Dr. Gordon T. Harold, School of Psychology, University of Sussex, UK, Tomsk State University, Tomsk, Russia, and the MRC Centre for Neuropsychiatric Genetics and Genomics, Cardiff University, Cardiff, Wales.
Dr. Patricia Chamberlain, Oregon Social Learning Center, Eugene, OR.
Mr. David Fowler, School of Psychology, University of Sussex, Brighton, UK.
Dr. Mary Cannon, Royal College of Surgeons in Dublin and Beaumont Hospital, Dublin.
Dr. Louise Arseneault, Institute of Psychiatry, King’s College London.
Dr. Leslie D. Leve, University of Oregon and the Oregon Social Learning Center.
References
- 1.Poulton R, Caspi A, Moffitt TE, Cannon M, Murray RM, Harrington HL. Children’s self-reported psychotic symptoms and adult schizophreniform disorder: A 15-year longitudinal study. Arch Gen Psychiatry. 2000;57:1053–1058. doi: 10.1001/archpsyc.57.11.1053. [DOI] [PubMed] [Google Scholar]
- 2.Welham J, Scott J, Williams G, et al. Emotional and behavioural antecedents of young adults who screen positive for non-affective psychosis: a 21-year birth cohort study. Psychol Med. 2009;39:625–634. doi: 10.1017/S0033291708003760. [DOI] [PubMed] [Google Scholar]
- 3.Kaymaz N, Drukker M, Lieb R, et al. Do subthreshold psychotic experiences predict clinical outcomes in unselected non-help-seeking population-based samples? A systematic review and meta-analysis, enriched with new results. Psychol Med. 2012;42:2239–2253. doi: 10.1017/S0033291711002911. [DOI] [PubMed] [Google Scholar]
- 4.Cannon M, Caspi A, Moffitt TE, et al. Evidence for early-childhood, pan-developmental impairment specific to schizophreniform disorder - Results from a longitudinal birth cohort. Arch Gen Psychiatry. 2002;59:449–456. doi: 10.1001/archpsyc.59.5.449. [DOI] [PubMed] [Google Scholar]
- 5.Kelleher I, Cannon M. Psychotic-like experiences in the general population: characterizing a high-risk group for psychosis. Psychol Med. 2011;41:1–6. doi: 10.1017/S0033291710001005. [DOI] [PubMed] [Google Scholar]
- 6.Kelleher I, Keeley H, Corcoran P, et al. Clinicopathological significance of psychotic experiences in non-psychotic young people: evidence from four population-based studies. Br J Psychiatry. 2012;201:26–32. doi: 10.1192/bjp.bp.111.101543. [DOI] [PubMed] [Google Scholar]
- 7.Laurens KR, West SA, Murray RM, Hodgins S. Psychotic-like experiences and other antecedents of schizophrenia in children aged 9–12 years: a comparison of ethnic and migrant groups in the United Kingdom. Psychol Med. 2008;38:1103–1111. doi: 10.1017/S0033291707001845. [DOI] [PubMed] [Google Scholar]
- 8.Polanczyk G, Moffitt TE, Arseneault L, et al. Etiological and clinical features of childhood psychotic symptoms results from a birth cohort. Arch Gen Psychiatry. 2010;67:328–338. doi: 10.1001/archgenpsychiatry.2010.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A. Childhood trauma and children’s emerging psychotic symptoms: A genetically sensitive longitudinal cohort study. Am J Psychiatry. 2011;168:65–72. doi: 10.1176/appi.ajp.2010.10040567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mackie CJ, Castellanos-Ryan N, Conrod PJ. Developmental trajectories of psychotic-like experiences across adolescence: impact of victimization and substance use. Psychol Med. 2011;41:47–58. doi: 10.1017/S0033291710000449. [DOI] [PubMed] [Google Scholar]
- 11.Yung AR, Nelson B. The ultra-high risk concept - A review. Can J Psychiatry. 2013;58:5–12. doi: 10.1177/070674371305800103. [DOI] [PubMed] [Google Scholar]
- 12.Harris MG, Henry LP, Harrigan SM, et al. The relationship between duration of untreated psychosis and outcome: An eight-year prospective study. Schizophr Res. 2005;79:85–93. doi: 10.1016/j.schres.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 13.Schimmelmann BG, Huber CG, Lambert M, Cotton S, McGorry PD, Conus P. Impact of duration of untreated psychosis on pre-treatment, baseline, and outcome characteristics in an epidemiological first-episode psychosis cohort. J Psychiatr Res. 2008;42:982–990. doi: 10.1016/j.jpsychires.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 14.McGorry PD, Killackey E, Yung A. Early intervention in psychosis: concepts, evidence and future directions. World Psychiatry. 2008;7:148–156. doi: 10.1002/j.2051-5545.2008.tb00182.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGorry P, van Os J. Redeeming diagnosis in psychiatry: timing versus specificity. Lancet. 2013;381:343–345. doi: 10.1016/S0140-6736(12)61268-9. [DOI] [PubMed] [Google Scholar]
- 16.Stafford MR, Jackson H, Mayo-Wilson E, Morrison AP, Kendall T. Early interventions to prevent psychosis: systematic review and meta-analysis. Br Med J. 2013;346:f185. doi: 10.1136/bmj.f185. doi:110.1136/bmj.f1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maddox L, Jolley S, Laurens KR, et al. Cognitive behavioural therapy for unusual experiences in children: a case series. Behav Cogn Psychother. 2013;41:344–358. doi: 10.1017/S1352465812000343. [DOI] [PubMed] [Google Scholar]
- 18.Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: A meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–671. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kelleher I, Harley M, Lynch F, Arseneault L, Fitzpatrick C, Cannon M. Associations between childhood trauma, bullying and psychotic symptoms among a school-based adolescent sample. Br J Psychiatry. 2008;193:378–382. doi: 10.1192/bjp.bp.108.049536. [DOI] [PubMed] [Google Scholar]
- 20.Lataster T, van Os J, Drukker M, et al. Childhood victimisation and developmental expression of non-clinical delusional ideation and hallucinatory experiences - Victimisation and non-clinical Psychotic experiences. Soc Psychiatry Psychiatr Epidemiol. 2006;41:423–428. doi: 10.1007/s00127-006-0060-4. [DOI] [PubMed] [Google Scholar]
- 21.Fisher HL, Jones PB, Fearon P, et al. The varying impact of type, timing and frequency of exposure to childhood adversity on its association with adult psychotic disorder. Psychol Med. 2010;40:1967–1978. doi: 10.1017/S0033291710000231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fisher HL, Schreier A, Zammit S, et al. Pathways between childhood victimization and psychosis-like symptoms in the ALSPAC birth cohort. Schizophr Bull. 2013;39:1045–1055. doi: 10.1093/schbul/sbs088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kelleher I, Corcoran P, Keeley H, et al. Psychotic symptoms and population risk for suicide attempt: A prospective cohort study. JAMA Psychiatry. 2013;70:940–948. doi: 10.1001/jamapsychiatry.2013.140. [DOI] [PubMed] [Google Scholar]
- 24.Breetvelt EJ, Boks MPM, Numans ME, et al. Schizophrenia risk factors constitute general risk factors for psychiatric symptoms in the population. Schizophr Res. 2010;120:184–190. doi: 10.1016/j.schres.2010.03.033. [DOI] [PubMed] [Google Scholar]
- 25.Chamberlain P. The Oregon Multidimensional Treatment Foster Care model: Features, outcomes, and progress in dissemination. Cognitive and Behavioral Practice. 2003;10:303–312. [Google Scholar]
- 26.Chamberlain P, Leve LD, DeGarmo DS. Multidimensional Treatment Foster Care for girls in the juvenile justice system: 2-year follow-up of a randomized clinical trial. J Consult Clin Psychol. 2007;75:187–193. doi: 10.1037/0022-006X.75.1.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leve LD, Chamberlain P, Reid JB. Intervention outcomes for girls referred from juvenile justice: Effects on delinquency. J Consult Clin Psychol. 2005;73:1181–1184. doi: 10.1037/0022-006X.73.6.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leve LD, Chamberlain P. Association with delinquent peers: Intervention effects for youth in the juvenile justice system. J Abnorm Child Psychol. 2005;33:339–347. doi: 10.1007/s10802-005-3571-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kerr DCR, Leve LD, Chamberlain P. Pregnancy rates among juvenile justice girls in two RCTs of Multidimensional Treatment Foster Care. J Consult Clin Psychol. 2009;77:588–593. doi: 10.1037/a0015289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harold GT, Kerr DCR, Van Ryzin M, DeGarmo DS, Rhoades KA, Leve LD. Depressive symptom trajectories among girls in the juvenile justice system: 24-month outcomes of an RCT of Multidimensional Treatment Foster Care. Prev Sci. 2013;14:437–446. doi: 10.1007/s11121-012-0317-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim-Cohen J, Caspi A, Moffitt T, Harrington H, Milne B, Poulton R. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. 2003;60:709–719. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- 32.Derogatis LR, Melisaratos N. The Brief Symptom Inventory - an introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- 33.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 34.Muthén LK, Muthén BO. Mplus user’s guide. 4. Los Angeles, CA: Muthén and Muthén; 2006. [Google Scholar]
- 35.Enders CK. Applied Missing Data Analysis. New York: Guilford Press; 2012. [Google Scholar]
- 36.Little RJA. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83:1198–1202. [Google Scholar]
- 37.Insel TR. From prevention to preemption: A paradigm shift in psychiatry. [Accessed March 1, 2014];Psychiatr Times. http://www.psychiatrictimes.com/articles/prevention-preemption-paradigm-shift-psychiatry. Published August 2008.
- 38.Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: Effect sizes, clinical models, and methodological rigor. Schizophr Bull. 2008;34:523–537. doi: 10.1093/schbul/sbm114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fowler D, Hodgekins J, Painter M, et al. Cognitive behaviour therapy for improving social recovery in psychosis: a report from the ISREP MRC Trial Platform study (Improving Social Recovery in Early Psychosis) Psychol Med. 2009;39:1627–1636. doi: 10.1017/S0033291709005467. [DOI] [PubMed] [Google Scholar]
- 40.O’Brien MP, Gordon JL, Bearden CE, Lopez SR, Kopelowicz A, Cannon TD. Positive family environment predicts improvement in symptoms and social functioning among adolescents at imminent risk for onset of psychosis. Schizophr Res. 2006;81:269–275. doi: 10.1016/j.schres.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 41.Lin A, Wigman JTW, Nelson B, et al. The relationship between coping and subclinical psychotic experiences in adolescents from the general population - a longitudinal study. Psychol Med. 2011;41:2535–2546. doi: 10.1017/S0033291711000560. [DOI] [PubMed] [Google Scholar]
- 42.Fowler D, Hodgekins J, Garety P, et al. Negative cognition, depressed mood, and paranoia: A longitudinal pathway analysis using structural equation modeling. Schizophr Bull. 2012;38:1063–1073. doi: 10.1093/schbul/sbr019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kuipers E. Family interventions in schizophrenia: evidence for efficacy and proposed mechanisms of change. J Fam Ther. 2006;28:73–80. [Google Scholar]
- 44.Onwumere J, Bebbington P, Kuipers E. Family interventions in early psychosis: specificity and effectiveness. Epidemiol Psychiatr Sci. 2011;20:113–119. doi: 10.1017/s2045796011000187. [DOI] [PubMed] [Google Scholar]
- 45.Poulton RG, Andrews G. Personality as a cause of adverse life events. Acta Psychiatr Scand. 1992;85:35–38. doi: 10.1111/j.1600-0447.1992.tb01439.x. [DOI] [PubMed] [Google Scholar]
- 46.Garety PA, Bebbington P, Fowler D, Freeman D, Kuipers E. Implications for neurobiological research of cognitive models of psychosis: a theoretical paper. Psychol Med. 2007;37:1377–1391. doi: 10.1017/S003329170700013X. [DOI] [PubMed] [Google Scholar]
- 47.Myin-Germeys I, van Os J. Stress-reactivity in psychosis: Evidence for an affective pathway to psychosis. Clin Psychol Rev. 2007;27:409–424. doi: 10.1016/j.cpr.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 48.Zammit S, Kounali D, Cannon M, et al. Psychotic experiences and psychotic disorders at age 18 in relation to psychotic experiences at age 12 in a longitudinal population-based cohort study. Am J Psychiatry. 2013;170:742–750. doi: 10.1176/appi.ajp.2013.12060768. [DOI] [PubMed] [Google Scholar]
- 49.Wigman JTW, van Winkel R, Raaijmakers QAW, et al. Evidence for a persistent, environment-dependent and deteriorating subtype of subclinical psychotic experiences: a 6-year longitudinal general population study. Psychol Med. 2011;41:2317–2329. doi: 10.1017/S0033291711000304. [DOI] [PubMed] [Google Scholar]
- 50.Insel TR. Rethinking schizophrenia. Nature. 2010;468:187–193. doi: 10.1038/nature09552. [DOI] [PubMed] [Google Scholar]
- 51.Bowie CR, McGurk SR, Mausbach B, Patterson TL, Harvey PD. Combined cognitive remediation and functional skills training for schizophrenia: Effects on cognition, functional competence, and real-world behavior. Am J Psychiatry. 2012;169:710–718. doi: 10.1176/appi.ajp.2012.11091337. [DOI] [PubMed] [Google Scholar]
- 52.Weinberger DR. Implications of normal brain-development for the pathogenesis of schizophrenia. Arch Gen Psychiatry. 1987;44:660–669. doi: 10.1001/archpsyc.1987.01800190080012. [DOI] [PubMed] [Google Scholar]
- 53.Murray RM, Jones P, Ocallaghan E. Fetal brain-development and later schizophrenia. Ciba Found Symp. 1991;156:155–170. doi: 10.1002/9780470514047.ch10. [DOI] [PubMed] [Google Scholar]
- 54.Werbeloff N, Drukker M, Dohrenwend BP, et al. Self-reported attenuated psychotic symptoms as forerunners of severe mental disorders later in life. Arch Gen Psychiatry. 2012;69:467–475. doi: 10.1001/archgenpsychiatry.2011.1580. [DOI] [PubMed] [Google Scholar]
- 55.Fisher HL, Caspi A, Poulton R, et al. Specificity of childhood psychotic symptoms for predicting schizophrenia by 38 years of age: a birth cohort study. Psychol Med. 2013;43:2077–2086. doi: 10.1017/S0033291712003091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Murray GK, Jones PB. Psychotic symptoms in young people without psychotic illness: Mechanisms and meaning. Br J Psychiatry. 2012;201:4–6. doi: 10.1192/bjp.bp.111.107789. [DOI] [PubMed] [Google Scholar]
- 57.van Os J, Murray RM. Can we identify and treat “schizophrenia light” to prevent true psychotic illness. Br Med J. 2013;346:f304. doi: 10.1136/bmj.f304. [DOI] [PubMed] [Google Scholar]
- 58.Linscott RJ, van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. 2013;43:1133–1149. doi: 10.1017/S0033291712001626. [DOI] [PubMed] [Google Scholar]
- 59.Schlosser DA, Miklowitz DJ, O’Brien MP, De Silva SD, Zinberg JL, Cannon TD. A randomized trial of family focused treatment for adolescents and young adults at risk for psychosis: study rationale, design and methods. Early Interv Psychiatry. 2012;6:283–291. doi: 10.1111/j.1751-7893.2011.00317.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.ANZ Journal of Psychiatry Special Issue: Psychosocial interventions in schizophrenia. Aust N Z J Psychiatry. 2013:47. [Google Scholar]
- 61.Harris A, Boyce P. Why do we not use psychosocial interventions in the treatment of schizophrenia. Aust N Z J Psychiatry. 2013;47:501–504. doi: 10.1177/0004867413489173. [DOI] [PubMed] [Google Scholar]