Abstract
Cardiovascular risk factors, such as abdominal obesity and obesity in general, are very prevalent among patients with bipolar disorder (BD). Although long-term use of psychotropic medications is an important determinant of these risk factors, other evidence suggests that early development may interact with the mood disorder diathesis to exponentially increase the risk of obesity. The goal of our study was to test whether season of birth is associated with adult body mass index (BMI) and abdominal obesity in individuals with bipolar disorder. We compared season of birth effects on BMI in 375 adult patients with bipolar disorder and 196 adult patients with unipolar major depression. We found a significant season of birth effect on BMI in patients with bipolar disorder, but not unipolar. In patients with bipolar disorder, season of birth was also associated with waist circumference, with a stronger effect in males. Season of birth affects adult BMI and waist circumference in patients with bipolar disorder, but not in patients with unipolar depression. Our results suggest that early environmental factors, yet to be identified, interact with specific neurobiological features of bipolar disorder to determine stable traits and disease risk factors in adult life.
Keywords: Abdominal obesity, Cardiovascular risk, Perinatal factors, Seasonal factors, Waist circumference
INTRODUCTION
Cardiovascular mortality is a leading cause of excess death in bipolar disorder, well above the mortality associated with suicide or accidents. Overall, it has been estimated that mortality for medical causes in bipolar disorder (BD) is between 1.5- and 2.5-fold when compared with the general population (Osby et al., 2001; Roshanaei-Moghaddam & Katon, 2009; Weiner et al., 2011). This high rate of mortality may be explained by the fact that individuals with BD have many risk factors such as obesity in general and, specifically, abdominal obesity (Fagiolini et al., 2002, 2005), a known proxy for diabetes and cardiovascular diseases. A well-known risk factor for obesity in patients with BD is the life-long use of psychotropic medication (McCloughen & Foster, 2011). However lifestyle and iatrogenic factors may not entirely explain the excess of overweight and obesity in this population. Indeed, the clinical observation that obesity is associated with cycloid mania date back to long before the psychopharmacologic drug era (Kretschmer & Sprott, 1925). In the past decade, studies have shown longitudinal association between overweight and mental illness (Hasler et al., 2004, 2005) and the presence of obesity in drug-naïve patients with bipolar disorder (Maina et al., 2008), suggesting that early developmental factors may interact with the mood disorder diathesis to exponentially increase the risk for obesity (Levitan et al., 2006).
Over the past few decades, a number of chronobiological studies have explored the effects of season of birth on several developmental traits and susceptibility to illnesses, including obesity (Wattie et al., 2008) and major psychiatric disorders (Boyd et al., 1986; Moore et al., 2001; Torrey & Miller, 1997). To date, there is solid evidence for an effect of season of birth on the risk of schizophrenia and bipolar disorder (Davies et al., 2003), with an excess of birth in winter/spring months for those individuals diagnosed with major affective disorder; moreover, some preliminary evidence of birth seasonality has been shown for patients with seasonal affective disorder and their unaffected siblings (Pjrek et al., 2007), consistent with the hypothesis that high degree of seasonality, once adaptive trait promoting better reproductive potential in our ancestors, is now associated with maladaptive behaviors—such as craving for calorie dense foods—predisposing to seasonal weight gain (Davis & Levitan, 2005).
Indeed, it has been suggested that season of birth may affect the phenotypic characteristics of these disorders, including patients’ body mass index (BMI) (Levitan et al., 2006; Pjrek et al., 2007). A small effect of season of birth on adult BMI has been described in the general population (Hillman & Conway, 1972; Tanaka et al., 2007; Wattie et al., 2008), but none of these studies has controlled for the presence of severe mood disorders in the sample.
The goal of our study was to explore the association between season of birth, adult BMI, and waist circumference in individuals with bipolar disorder. More specifically, we hypothesized that patients with a diathesis for bipolar disorder are especially vulnerable to cyclical environmental factors and would show a specific birth birth-seasonal pattern or a stronger effect of season of birth on the outcome variables. We therefore compared a group of patients with bipolar disorder with a sample of individuals with unipolar depression to test the pattern and strength of season of birth effects on BMI. We choose this comparison group because, although patient with unipolar depression share some of same cardiovascular risk factors as patients with bipolar disorder, a season of birth effect has not been unequivocally demonstrated.
METHODS
All the experimental procedures were approved by the University of Pittsburgh Institutional Review Committee and conform to international ethical standards (Portaluppi et al., 2010).
Sample
Participants in this study were 375 adult men and women with a bipolar disorder and 196 men and women with major depressive disorder taking part in two larger treatment studies. For detailed descriptions of all the study procedures, refer to Kupfer et al. (2009) and Frank et al. (2011). As part of the inclusion criteria for the parent study (ME02385, Bipolar Disorder Center for Pennsylvanians), participants were required to have a Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnosis for Bipolar I, Bipolar II, Bipolar Not Otherwise Specified (NOS) or Schizoaffective Bipolar subtype. Inclusion criteria for the Depression Phenotypes study (MH065376) were a diagnosis of Major Depressive disorder and a minimum Hamilton rating Scale for Depression (HAM-D) score of 15. Exclusion criteria for the bipolar study were IQ ≤ 70, current substance or alcohol dependence, organic mental disorder, and unstable and severe medical illness or other medical contradiction to treatment with mood stabilizers, antidepressants, or antipsychotic medications, including pregnancy or breastfeeding. Exclusion criteria for the parent study “Depression Phenotypes” were a primary diagnosis of schizophrenia, schizoaffective disorder, bipolar I or II disorder, current anorexia or bulimia, and antisocial personality disorder. Patients with current alcohol or substance abuse or dependence were excluded only if their drinking or substance use was unrelated to their depression. Individuals with severe, uncontrolled medical illness, those who had been unresponsive to an adequate trial of escitalopram or interpersonal psychotherapy (IPT) in the current episode, and women unwilling to practice an acceptable form of birth control were also excluded.
Assessments
All patients received their diagnosis via the structured clinical interview for DSM IV (SCID). In addition, comprehensive physical examinations were carried out at baseline, and measurements of height, weight, and waist circumference occurred at baseline and 12 and 24 mos for the bipolar study participants and measurement of weight occurred at each study visit for the unipolar study participants.
Statistical Analyses
We defined season of birth groups based on the calendar year: participants who were born between March 22 and June 21 were classified as spring-born, those born between June 22 and September 21 were summerborn, September 22 to December 21 fall-born, and December 22 to March 21 were winter-born. BMI was calculated as [weight (kg)/height2 (m2)].
For the bipolar group, we used BMI and waist circumference data from baseline and the 12- and 24-mo time points; for the unipolar depressed group we used BMI data from baseline and endpoint, approximately 8 mos later.
Since the distribution of the different classes of psychotropic medications was not significantly different by season of birth groups, we dropped the medications variable from further analyses.
Nineteen patients in the unipolar depression group had reported current alcohol use; since they did not differ in season of birth distribution, age, or BMI from the rest of the sample, we did not include it as a covariate.
As participants in the two studies were followed at different time points and for different durations, we first focused on baseline observations and combined the baseline data from the two studies together. Linear regression analyses were used to examine the effects of birth season and the season by study interaction on BMI.
To see whether the observed birth season effect persists over time, we next applied mixed models to baseline and follow-up data in the two groups separately. Mixed model for repeated measures were used to examine BMI or waist circumference with fixed terms of birth season, gender, gender by birth season (if significant), time (baseline and 12- and 24-mo follow-up in the bipolar group or baseline and 8-mo follow-up in the unipolar depressed group), and age. Subject was treated as a random term to take into account individual variability. We also set up contrasts to test whether spring-born subjects have larger BMI than those born in other seasons. For waist circumference, since we found a gender by birth season interaction, we set up contrasts to compare whether spring-born males have larger waist circumference than males born in other seasons and whether fall-born females are larger than females born in other seasons. The effect sizes were computed based on t tests.
RESULTS
Sample characteristics are summarized in Table 1. Compared with individuals with unipolar disorder, the patients with bipolar disorder are older (p = .03), tend to be larger at baseline (p = .06), and have a larger proportion of African Americans (p = .02). There are no significant differences in gender (p = .58), marital status (p = .71), and season of birth distribution (p = .41) between the bipolar and unipolar groups.
TABLE 1.
Sample characteristics and season of birth distribution
| Characteristics | Bipolar disorder group (n = 375) | Major depressive disorder group (n = 196) | t/χ2 | df | p |
|---|---|---|---|---|---|
| Age (SD) | 41.25 (11.79) | 38.96 (12.35) | 2.17 | 569 | .03 |
| BMI (SD) | 29.54 (7.88) | 28.34 (6.92) | 1.87 | 440 | .06 |
| M/F | 137/238 | 77/119 | .416 | 1 | .58 |
| AA/non-AA | 53/281 | 17/179 | 5.58 | 1 | .02 |
| Married/not | 116/218 | 65/131 | .13 | 1 | .71 |
| Season (Sp/Su/F/W) | 85/112/84/94 | 49/54/53/40 | 2.88 | 3 | .41 |
SD = Standard Deviation; AA = African American; df = degree of freedom.
We first focused on baseline observations and combined the data from the two studies together. In the overall sample, there was a significant season of birth effect on BMI (F(3, 555) = 2.68, p = .046). Consistent with the results in Table 1, participants in the bipolar study tend to be larger at baseline than those in the unipolar study (F(1, 433) = 3.67, p =.056, with an effect size of .18). Although there is no significant study by birth season interaction, subsequent contrasts indicate that spring-born patients with bipolar disorder are heavier than individuals with bipolar disorder born in other seasons (estimates (est) = 2.25, t = 2.33, p = .02), although there is no difference in BMI among unipolar patients born in spring or other seasons (est = .51, t = .51, p = .66).
Next, we examined the longitudinal data on BMI from both studies and on waist circumference from the bipolar study. Since the two studies had different follow-ups, mixed effect models were applied to longitudinal outcomes separately for the two studies. Mixed models on the repeated measures showed a significant season of birth effect on BMI at baseline and 12 and 24 mos for the bipolar group (F(3, 721) = 6.05, p = .0005), but not in the unipolar (F(3, 376) = 1.87, p = .134) (Figure 1).
FIGURE 1.
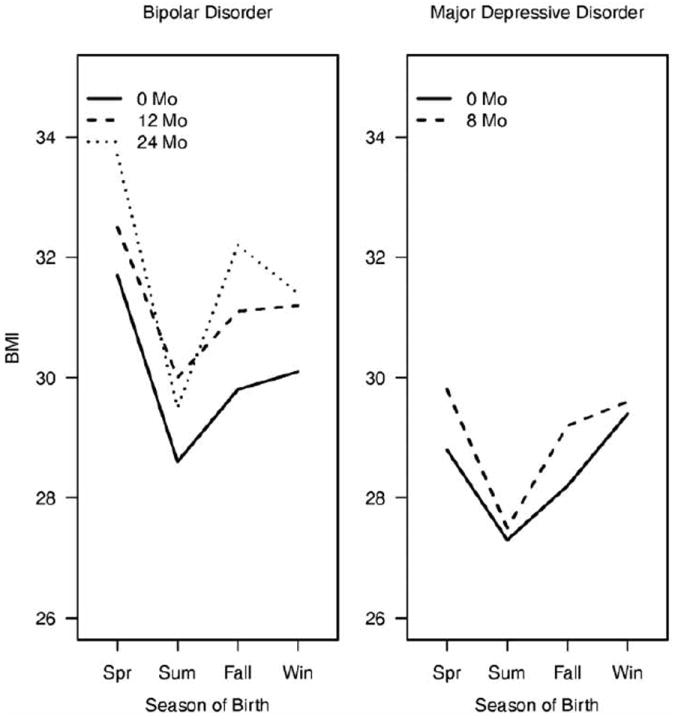
Mixed models for repeated measures show a significant season of birth effect on BMI in patients with bipolar disorder only; spring-born patients have larger BMI than patients born in other seasons.
Consistent with the baseline analysis, spring-born patients with bipolar disorder have larger BMI than those patients with bipolar disorder who were born in other seasons at all time points (i.e., baseline, 12 mos, and 24 mos (est = 2.24, t = 3.55, p = .0004, effect size = .26), and that individuals with unipolar depression born in spring did not differ in BMI from those born in other seasons at all time points (i.e., baseline and 8 mos) (est = .78, t = .94, p = .35, effect size = .10). There is also an age effect on BMI for patients with bipolar disorder with older patients having larger BMI (F(1, 721) = 16.86, p < .0001), but not for patients with unipolar disorder. The gender effect on BMI is not significant for both groups.
In the individuals with bipolar disorder, we also found a significant season of birth effect on waist circumference (F(3, 700) = 6.23, p = .0004) and a season of birth by gender interaction (F(3, 700) = 5.34, p = .001), with spring-born males having the largest waist circumference. Follow-up contrasts suggest that spring-born males have larger waist circumference than those male subjects born in other seasons (est = 3.71, t = 3.95, p < .0001, effect size = .30), whereas spring-born females do not differ from women born in other seasons (est = .92, t = 1.19, p = .23, effect size = .09). There is also an age effect, with older subjects being associated with larger waist circumference (F(1, 700) = 40.24, p < .0001).
DISCUSSION
This is the first study to show a season of birth effect on BMI and waist circumference in bipolar disorder. Season of birth effects on growth patterns have been documented in children and adolescents (Tanaka et al., 2007); however, the effects in adult individuals are small and often confounded or overruled by other intervening lifestyle factors (Frye & Heinrich, 2003; Wattie et al., 2008). The season of birth pattern that has been most commonly described is higher rates of obesity in individuals born in winter-spring (Levitan et al., 2006; Tanaka et al., 2007); however, different patterns in different age cohorts have also been described (Wattie et al., 2008) and some studies have also failed to detect a season of birth effect on BMI (Hackett et al., 2009). Moreover, none of the studies exploring effects of season of birth on adult BMI have controlled for the presence of psychiatric disorders that have been shown to be associated with birth seasonality. In this study, we show that patients with bipolar disorder born in spring have significantly higher BMI and waist circumference than other birth season groups. This effect was not present in patients with unipolar depression, who did not show significant differences in BMI among the four season of birth groups. These results suggest that individuals with a biological vulnerability for bipolar disorder are susceptible to cyclical environmental effects related to season. Several lines of evidence suggest a seasonal vulnerability in bipolar disorder, including the finding that season of birth confers a small, yet robust increased risk of developing bipolar disorder itself (Torrey & Miller, 1997), whereas weaker or no effects have been shown in major depression (Disanto et al., 2012; Fountoulakis et al., 2007) or other psychiatric disorders (Torrey and Miller, 1997). Our findings suggest a twofold question: what are the seasonal aspects that affect the characteristics of the disorder and what are the features of the disorder conferring vulnerability to seasonal factors? The environmental factors that most prominently follow the seasonal cycle are viral infections and daylight. A viral hypothesis has been suggested for both BD (Mortensen et al., 2011; Tedla et al., 2011) and obesity (Trovato et al., 2012; von Scholten et al., 2012). Although the evidence of an association between early viral infections and adult BD is still elusive, a more solid body of evidence is available to support the association between certain viral agents and obesity. In this framework, one could argue that in individuals who are born in late winter/early spring are more likely to be exposed to “adipogenic” viral agents and later become obese. However, the viruses implicated in the pathogenesis of obesity are not the same and do not follow the same seasonal pattern as those under study for BD. If a seasonal viral agent were responsible for the season of birth effects on BMI, we would expect that the same pattern to occur in patients with unipolar depression.
An alternative hypothesis is that perinatal light exposure, light intensity, and phase angle (Duffy & Wright, 2005) may be the environmental factors mediating the season of birth effects. Daylight is the main entraining component of the circadian system (Duffy & Wright, 2005), which comprises a central master clock (the suprachiasmatic nucleus [SCN]) and peripheral oscillators and which regulates a wide number of physiologic functions, including feeding behavior and metabolism (Huang et al., 2011). It is known that human SCN continues to develop few months after birth (Swaab et al., 1990), leading to the hypothesis that photoperiod around birth could have an impact on the adult functioning of the circadian system.
Patients with bipolar disorder often show disturbances in their sleep-wake cycle and other indicators of circadian disturbances, independent of their mood state (Murray & Harvey, 2010). Moreover, specific manipulations of the circadian system can trigger manic-like and depressive-like behaviors in animal models of mood disorder (Mukherjee et al., 2010), indicating that a weak circadian system may be at the core of bipolar disorder. Newborns with a bipolar disorder diathesis would be therefore especially vulnerable to the effects of the photoperiod at or around birth, affecting a number of adult traits, including metabolism. Indeed, preliminary evidence suggests that aspects of the circadian system, such as chronotype and sleep duration, may also contribute to obesity and cardiovascular disease (CVD) risk in patients with bipolar disorder (Soreca et al., 2009, 2012).
Finally, one intriguing finding in this data set was that season of birth showed a different effect on male and female waist circumference. To the best of our knowledge, this is the first report of a season of birth by gender interaction on waist circumference and further investigation will have to first clarify whether this is specific to bipolar disorder. The rate of fat accumulation around the waist is partly determined by sex hormones and our findings add to that, suggesting that early factors differentially affect males and females in determining adult cardiovascular risk factors.
This study has several limitations that need to be considered when interpreting the results. The first general consideration is that season of birth studies on outcomes in adult life link two events that are very far apart in time, without any realistic possibility of controlling for the myriad confounding factors during the life span. When studying BMI and waist circumference in particular, so many lifestyle and genetic factors that we did not control for could account for our results.
Our samples of patients with bipolar disorder and patients with unipolar depression were not matched, resulting in some baseline differences, such as age. Although we adjusted for age, we did not have the power to analyze each birth cohort separately. Certain environmental factors may change over time, resulting in different season of birth pattern for different birth cohorts.
We could not control for place of birth. Seasonal aspects, including daylight duration and intensity, vary considerably by latitude or in specific geographical pockets and could be possibly masking some of the birth season effects. We do not have a healthy control group for comparison, therefore, we cannot ascertain which group is deviating from the norm. In other words, although our explanation for our findings is that the biological diathesis for bipolar disorder increases the vulnerability to the perinatal photoperiod, one could also argue that the diathesis for unipolar depression may counteract the effects of perinatal light exposure. Studying the effects of season of birth on adult BMI in patients with and without family history for bipolar disorder and unipolar disorder may help clarify the direction of the association.
We do not have information about seasonality in patients’ symptomatology/recurrences. Season of birth has been shown to be associated with adult weight gain in women with seasonal affective disorder (Levitan et al., 2006) and seasonal aspect of the bipolar disorder could account for the association with adult BMI and waist circumference.
Season of birth effects on adult BMI and waist circumference could also reflect different severity of illness in spring-born patients compared with patients born in other seasons. Although we did not find any baseline difference in symptoms severity by season of birth group, different longitudinal course of the bipolar disorder may in part explain the association with BMI and waist circumference.
In the current study, we could not account for sleep characteristics. Sleep duration and timing are relevant to cardiovascular risk (Knutson, 2010; Soreca et al., 2012) and recent evidence suggests that season of birth can affect sleep characteristics in adult life (Tonetti et al., 2011)
Our study has also several strengths. Our samples of patients with bipolar disorder and unipolar depression were very well characterized clinically and all diagnoses had been made with a structured clinical interview administered by highly experienced clinicians. We had repeated measures of BMI (and waist circumference for the bipolar group only) and we showed that the effects are stable over time.
In summary, we found that season of birth affects adult BMI and waist circumference in patients with bipolar disorder, but not in patients with unipolar depression. Our results suggest that early environmental factors, yet to be identified, interact with specific neurobiological features of bipolar disorder to determine stable traits and disease risk factors in adult life. Further studies on the clinical characteristics of bipolar disorder affected by birth seasonality may help guide personalized treatment with particular focus on chronotherapy.
Acknowledgments
This study was funded in part by grants ME-02385 (principal investigator [PI]: David Kupfer) from the Commonwealth of Pennsylvania Department of Mental Health and grant MH065376 (PI: Ellen Frank) from the National Institute of Mental Health.
Footnotes
Declaration of Interest:
I.S., Y.C., and D.J.K. have no potential conflicts of interests to declare. E.F. is in the Servier International Advisory Board and owns Guilford Press and American Psychological Association Press Royalties. A.F. is/has been a consultant and/or a speaker and/or has received research grants and/or participated in studies supported by Angelini, Astra Zeneca, Boehringer-Ingelheim, Bristol-Myers Squibb, Lundbeck, Eli Lilly, Jannssen, Novartis, Pfizer, Sigma Tau, and Takeda.
The other authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper
References
- Boyd JH, Pulver AE, Stewart W. Season of birth: schizophrenia and bipolar disorder. Schizophr Bull. 1986;12:173–186. doi: 10.1093/schbul/12.2.173. [DOI] [PubMed] [Google Scholar]
- Davies G, Welham J, Chant D, Torrey EF, McGrath J. A systematic review and meta-analysis of Northern Hemisphere season of birth studies in schizophrenia. Schizophr Bull. 2003;29:587–593. doi: 10.1093/oxfordjournals.schbul.a007030. [DOI] [PubMed] [Google Scholar]
- Davis C, Levitan RD. Seasonality and seasonal affective disorder (SAD): an evolutionary viewpoint tied to energy conservation and reproductive cycles. J Affect Disord. 2005;87:3–10. doi: 10.1016/j.jad.2005.03.006. [DOI] [PubMed] [Google Scholar]
- Disanto G, Morahan JM, Lacey MV, Deluca GC, Giovannoni G, Ebers GC, Ramagopalan SV. Seasonal distribution of psychiatric births in England. PLoS ONE. 2012;7:e34866. doi: 10.1371/journal.pone.0034866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy JF, Wright KP., Jr Entrainment of the human circadian system by light. J Biol Rhythms. 2005;20:326–338. doi: 10.1177/0748730405277983. [DOI] [PubMed] [Google Scholar]
- Fagiolini A, Frank E, Houck PR, Mallinger AG, Swartz HA, Buysse DJ, et al. Prevalence of obesity and weight change during treatment in patients with bipolar I disorder. J Clin Psychiatry. 2002;63:528–533. doi: 10.4088/jcp.v63n0611. [DOI] [PubMed] [Google Scholar]
- Fagiolini A, Frank E, Scott JA, Turkin S, Kupfer DJ. Metabolic syndrome in bipolar disorder: findings from the Bipolar Disorder Center for Pennsylvanians. Bipolar Disord. 2005;7:424–430. doi: 10.1111/j.1399-5618.2005.00234.x. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Iacovides A, Karamouzis M, Kaprinis GS, Ierodiakonou C. Season of birth, clinical manifestations and Dexamethasone Suppression Test in unipolar major depression. Ann Gen Psychiatry. 2007;6:20. doi: 10.1186/1744-859X-6-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank E, Cassano GB, Rucci P, Thompson WK, Kraemer HC, Fagiolini A, et al. Predictors and moderators of time to remission of major depression with interpersonal psychotherapy and SSRI pharmacotherapy. Psychol Med. 2011;41:151–162. doi: 10.1017/S0033291710000553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye C, Heinrich J. Trends and predictors of overweight and obesity in East German children. Int J Obes Relat Metab Disord. 2003;27:963–969. doi: 10.1038/sj.ijo.0802321. [DOI] [PubMed] [Google Scholar]
- Hackett AF, Stott TA, Boddy LM, Stratton G. Is air temperature at birth associated with body mass index in 9–10 year-old children? Ecol Food Nutr. 2009;48:123–136. doi: 10.1080/03670240802690557. [DOI] [PubMed] [Google Scholar]
- Hasler G, Pine DS, Gamma A, Milos G, Ajdacic V, Eich D, et al. The associations between psychopathology and being overweight: a 20-year prospective study. Psychol Med. 2004;34:1047–1057. doi: 10.1017/s0033291703001697. [DOI] [PubMed] [Google Scholar]
- Hasler G, Pine DS, Kleinbaum DG, Gamma A, Luckenbaugh D, Ajdacic V, et al. Depressive symptoms during childhood and adult obesity: the Zurich Cohort Study. Mol Psychiatry. 2005;10:842–850. doi: 10.1038/sj.mp.4001671. [DOI] [PubMed] [Google Scholar]
- Hillman RW, Conway HC. Season of birth and relative body weight. Am J Clin Nutr. 1972;25:279–281. doi: 10.1093/ajcn/25.3.279. [DOI] [PubMed] [Google Scholar]
- Huang W, Ramsey KM, Marcheva B, Bass J. Circadian rhythms, sleep, and metabolism. J Clin Invest. 2011;121:2133–2141. doi: 10.1172/JCI46043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson KL. Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best Pract Res Clin Endocrinol Metab. 2010;24:731–743. doi: 10.1016/j.beem.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kretschmer E, Sprott WJH. Physique and character; an investigation of the nature of constitution and of the theory of temperament. London: K. Paul, Trench, Trubner & Co.; Harcourt, Brace & Company. Kretschmer & Sprott; 1925. [Google Scholar]
- Kupfer DJ, Axelson DA, Birmaher B, Brown C, Curet DE, Fagiolini A, et al. Bipolar disorder center for Pennsylvanians: implementing an effectiveness trial to improve treatment for at-risk patients. Psychiatr Serv. 2009;60:888–897. doi: 10.1176/appi.ps.60.7.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitan RD, Masellis M, Lam RW, Kaplan AS, Davis C, Tharmalingam S, et al. A birth-season/DRD4 gene interaction predicts weight gain and obesity in women with seasonal affective disorder: a seasonal thrifty phenotype hypothesis. Neuropsychopharmacology. 2006;31:2498–2503. doi: 10.1038/sj.npp.1301121. [DOI] [PubMed] [Google Scholar]
- Maina G, Salvi V, Vitalucci A, D’Ambrosio V, Bogetto F. Prevalence and correlates of overweight in drug-naive patients with bipolar disorder. J Affect Disord. 2008;110:149–155. doi: 10.1016/j.jad.2007.12.233. [DOI] [PubMed] [Google Scholar]
- McCloughen A, Foster K. Weight gain associated with taking psychotropic medication: an integrative review. Int J Ment Health Nurs. 2011;20:202–222. doi: 10.1111/j.1447-0349.2010.00721.x. [DOI] [PubMed] [Google Scholar]
- Moore PB, El-Badri SM, Cousins D, Shepherd DJ, Young AH, McAllister VL, et al. White matter lesions and season of birth of patients with bipolar affective disorder. Am J Psychiatry. 2001;158:1521–1524. doi: 10.1176/appi.ajp.158.9.1521. [DOI] [PubMed] [Google Scholar]
- Mortensen PB, Pedersen CB, McGrath JJ, Hougaard DM, Norgaard-Petersen B, Mors O, et al. Neonatal antibodies to infectious agents and risk of bipolar disorder: a population-based casecontrol study. Bipolar Disord. 2011;13:624–629. doi: 10.1111/j.1399-5618.2011.00962.x. [DOI] [PubMed] [Google Scholar]
- Mukherjee S, Coque L, Cao JL, Kumar J, Chakravarty S, Asaithamby A, et al. Knockdown of Clock in the ventral tegmental area through RNA interference results in a mixed state of mania and depression-like behavior. Biol Psychiatry. 2010;68:503–511. doi: 10.1016/j.biopsych.2010.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray G, Harvey A. Circadian rhythms and sleep in bipolar disorder. Bipolar Disord. 2010;12:459–472. doi: 10.1111/j.1399-5618.2010.00843.x. [DOI] [PubMed] [Google Scholar]
- Osby U, Brandt L, Correia N, Ekbom A, Sparen P. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry. 2001;58:844–850. doi: 10.1001/archpsyc.58.9.844. [DOI] [PubMed] [Google Scholar]
- Pjrek E, Winkler D, Praschak-Rieder N, Willeit M, Stastny J, Konstantinidis A, et al. Season of birth in siblings of patients with seasonal affective disorder. A test of the parental conception habits hypothesis. Eur Arch Psychiatry Clin Neurosci. 2007;257:378–382. doi: 10.1007/s00406-007-0720-8. [DOI] [PubMed] [Google Scholar]
- Portaluppi F, Smolensky MH, Touitou Y. Ethics and methods for biological rhythm research on animals and human beings. Chronobiol Int. 2010;27:1911–1929. doi: 10.3109/07420528.2010.516381. [DOI] [PubMed] [Google Scholar]
- Roshanaei-Moghaddam B, Katon W. Premature mortality from general medical illnesses among persons with bipolar disorder: a review. Psychiatr Serv. 2009;60:147–156. doi: 10.1176/ps.2009.60.2.147. [DOI] [PubMed] [Google Scholar]
- Soreca I, Fagiolini A, Frank E, Goodpaster BH, Kupfer DJ. Chronotype and body composition in bipolar disorder. Chronobiol Int. 2009;26:780–788. doi: 10.1080/07420520902929060. [DOI] [PubMed] [Google Scholar]
- Soreca I, Wallace ML, Frank E, Hasler BP, Levenson JC, Kupfer DJ. Sleep duration is associated with dyslipidemia in patients with bipolar disorder in clinical remission. J Affect Disord. 2012;141(2–3):484–487. doi: 10.1016/j.jad.2012.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swaab DF, Hofman MA, Honnebier MB. Development of vasopressin neurons in the human suprachiasmatic nucleus in relation to birth. Brain Res Dev Brain Res. 1990;52:289–293. doi: 10.1016/0165-3806(90)90247-v. [DOI] [PubMed] [Google Scholar]
- Tanaka H, Sei M, Binh TQ, Munakata H, Yuasa K, Nakahori Y. Correlation of month and season of birth with height, weight and degree of obesity of rural Japanese children. J Med Invest. 2007;54:133–139. doi: 10.2152/jmi.54.133. [DOI] [PubMed] [Google Scholar]
- Tedla Y, Shibre T, Ali O, Tadele G, Woldeamanuel Y, Asrat D, et al. Serum antibodies to Toxoplasma gondii and Herpesvidae family viruses in individuals with schizophrenia and bipolar disorder: a case-control study. Ethiop Med J. 2011;49:211–220. [PubMed] [Google Scholar]
- Tonetti L, Fabbri M, Martoni M, Natale V. Season of birth and sleep-timing preferences in adolescents. Chronobiol Int. 2011;28:536–540. doi: 10.3109/07420528.2011.590261. [DOI] [PubMed] [Google Scholar]
- Torrey EF, Miller J. Season of birth and schizophrenia: Southern Hemisphere data. Aust N Z J Psychiatry. 1997;31:308–309. [PubMed] [Google Scholar]
- Trovato GM, Martines GF, Pirri C, Trovato FM, Castro A, Garozzo A, et al. Obesity-independent association of human adenovirus Ad37 seropositivity with nonalcoholic fatty liver disease. J Clin Gastroenterol. 2012;46(6):e46–e54. doi: 10.1097/MCG.0b013e31824b225c. [DOI] [PubMed] [Google Scholar]
- von Scholten BJ, Andresen EN, Sorensen TI, Jess T. Aetiological factors behind adipose tissue inflammation: an unexplored research area. Public Health Nutr. 2012;16(1):27–35. doi: 10.1017/S1368980012000894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wattie N, Ardern CI, Baker J. Season of birth and prevalence of overweight and obesity in Canada. Early Hum Dev. 2008;84:539–547. doi: 10.1016/j.earlhumdev.2007.12.010. [DOI] [PubMed] [Google Scholar]
- Weiner M, Warren L, Fiedorowicz JG. Cardiovascular morbidity and mortality in bipolar disorder. Ann Clin Psychiatry. 2011;23:40–47. [PMC free article] [PubMed] [Google Scholar]


