Abstract
Objective
Intestinal perforation is associated with high morbidity and mortality in gynecologic oncology patients. We investigated potential factors associated with survival after perforation which may influence treatment recommendations.
Methods
A retrospective review of all gynecologic oncology patients experiencing intestinal perforation between 1993–2007 was performed. Demographics, cancer history, presenting symptoms, vital signs, laboratory values, and management of perforation were collected, and acute physiology and chronic health evaluation II (APACHE II) scores were calculated for each patient. Factors affecting survival from the time of perforation were analyzed using Kaplan Meier method and univariate and multivariate Cox proportional hazard models. Student’s t-test and chi-square analysis were also utilized to evaluate potential associations.
Results
Fifty-three patients met the inclusion criteria. No difference in survival was found based on disease site, history of radiation therapy, presenting symptoms, smoking history, or presence of bowel procedures performed during the most recent abdominal surgery prior to perforation. APACHE II score, disease status, body mass index and treatment method of perforation were found to be significant prognostic factors for survival. After multivariate Cox regression analysis, only APACHE II scores remained significantly associated with an increased risk of death. Median survival of patients with APACHE II scores <15 was 28.13 months compared to 2.90 months in patients with scores ≥ 15 (p<0.0001).
Conclusion
Many factors must be examined when determining the management of intestinal perforation in gynecologic oncology patients. Clinicians should consider the APACHE II score in their assessment to assist risk stratification and treatment planning of these patients.
Introduction
Peritonitis due to intestinal perforation is a clinically life-threatening condition associated with high morbidity and mortality. Bacterial contamination of the peritoneal cavity usually leads to abscess formation potentially followed by sepsis with reported mortality rates ranging from 11 to 81%.[1–3]. Patients often present with symptoms such as abdominal pain or distention, fever, and tachycardia. Factors associated with high morbidity and mortality include the use of corticosteroids, immunosuppression, and malnutrition; early recognition and treatment of sepsis is essential to improve patient outcome.[1, 2, 4] Surgical intervention is often required to control the septic focus, but individualized treatment comparing the risks and benefits of surgery to more conservative management must be considered.
Studies evaluating risk of death from bowel perforations in the gynecologic oncology patient population have been limited thus far. Most evaluations have focused primarily upon patients with cervical cancer who have received radiation therapy.[5, 6] Several case reports and case series have examined the potential association between intestinal perforation and taxane-based chemotherapy.[7–10] Additionally, the use of bevacizumab in the gynecologic oncology population has been found to increase the risk of perforation as well.[11] However, no other risk factors or prognostic identifiers for bowel perforation have been found in this patient population. Our study aimed to determine if other clinical and laboratory factors were associated with patient outcome in gynecologic oncology patients who experience this potentially lethal complication.
Methods
After obtaining approval from the Institutional Review Board, we reviewed the medical records of all patients at The University of Texas MD Anderson Cancer Center between 1/1/1993 to 12/31/2007 who were identified as having a gynecologic malignancy and intestinal perforation. The following ICD-9 codes were used to identify gynecologic oncology patients with intestinal perforation: 569.83, 180.0, 180.1, 180.8, 180.9, 182.1, 182.8, 183.0, 183.2, 183.4, 183.5, 183.8, 183.9, 184.0, 184.4, 184.8, and 184.9. Data abstracted from the medical records included demographic information, pertinent medical and surgical history, date of original cancer diagnosis, cancer treatment history, and date of and status at last contact. Additional data obtained included presenting symptoms, laboratory values, and disease status at the time of intestinal perforation, as well as method of perforation management.
All diagnoses of bowel perforation were made based upon a combination of clinical examination and radiologic evidence. Vital signs and presenting clinical symptoms, including abdominal pain, fever, nausea/vomiting, and abnormal bowel movements, were recorded on the date of perforation diagnosis. Laboratory data, including white blood cell (WBC) counts, absolute neutrophil counts (ANC), hematocrit levels, electrolytes, and arterial blood gases, were also collected within 24 hours of intestinal perforation. Acute physiology and chronic health evaluation II (APACHE II) scores were calculated according to the method of Knaus et al.[12] An albumin level measured within one week of perforation was considered a marker for patient nutritional status at the time of perforation. Body mass index (BMI) was calculated using the patient’s height and weight recorded closest to the time of intestinal perforation. Operative notes were examined, and potential causes for perforation were recorded. Patients were classified into four categories based on possible etiologies: 1) iatrogenic, 2) tumor-related, 3) colitis, appendicitis, or proctitis, or 4) unknown.
Statistical analyses were performed using SPSS 15.0 software (SPSS, Chicago, IL). Descriptive statistics were utilized to describe the study cohort. The chi-square test was used to analyze associations between categorical variables. Continuous variables were evaluated using the student’s t-test. Survival time was defined from the date of diagnosis of intestinal perforation to the date of last contact or date of death. The log-rank test was used to compare differences in Kaplan-Meier survival curves based upon potential prognostic factors. Univariate and multivariate analysis was performed using Cox proportional hazards regression. Factors with a p-value of ≤ 0.10 on univariate analysis were included in the multivariate analysis. P-values less than 0.05 were considered statistically significant, and all tests were two-sided.
Results
Over 28,000 gynecologic oncology patients were treated at our institution during the study time period, and 53 patients (0.19%) met the inclusion criteria for the study. The median patient age was 56 years (range 31–90 years) with a median BMI of 25.0 (range 16.2–44.6). Table 1 presents patient demographic characteristics. Patients who were diagnosed with rare gynecologic cancer diagnoses were classified as “other” and included one patient with pelvic spindle cell carcinoma and one patient with adenocarcinoma of the rectovaginal septum. Four patients were found to have synchronous primaries at the time of the initial staging surgery. Two patients had synchronous ovarian and endometrial cancer, one patient had concomitant cervical and endometrial cancer, and one patient was found to have synchronous endometrial and colon cancer.
Table 1.
Patient Characteristics (n=53)
| Age* (range) | 56 years (31–90) |
| BMI* (range) | 26.2 kg/m2 (16.2–44.6) |
| Cancer diagnosis (%) | |
| Cervical | 21 (39.6) |
| Uterine | 8 (15.1) |
| Ovarian/Primary peritoneal | 18 (34.0) |
| Other | 2 (3.8) |
| Synchronous cancer | 4 (7.6) |
| # prior chemo regimens* (range) | 0.87 (0–8) |
| History of radiation treatment | |
| Yes | 28 (52.8) |
| No | 25 (47.2) |
| Months from last abdominal surgery to bowel perforation* (range) | 37.64 (0–462) |
| Bowel injury during last abdominal surgery† | |
| Yes | 16 (30.2) |
| No | 24 (45.3) |
| Disease status at time of perforation | |
| No evidence of disease (NED) | 16 (30.2) |
| Newly diagnosed1 | 12 (22.6) |
| Progressive/Stable disease2 | 25 (47.2) |
| Receiving treatment at time of perforation | |
| Yes | 23 (43.3) |
| No | 30 (56.6) |
| White blood cell count (WBC)* | 12,800/μL |
| Absolute neutrophil count (ANC)* | 10,500/μL |
| Bicarbonate (HCO3−) * | 24.14 mEQ/L |
| Creatinine* | 1.1 mg/dL |
| Hematocrit* | 32.58% |
| Albumin | 2.58 g/dL |
Mean values
Diagnosis at time of perforation or patients receiving primary chemotherapeutic regimen
Evidence of worsening or stable disease on recent radiographic imaging or at time of surgery
Data missing for 13 patients
After diagnosis of intestinal perforation, 47 (88.7%) of patients were treated with surgical intervention with 6 (11.3%) patients managed conservatively. The etiology for the perforation was unknown for 29 (54.7%) of patients, but 8 (15.1%) patients were found to have tumor invading bowel serosa. Seven (13.2%) patients were suspected to have colitis, appendicitis, or proctitis as the inciting factor for perforation, and 9 (17.0%) had iatrogenic perforations or perforations diagnosed within 2 weeks after staging surgery, colonoscopy, or intraperitoneal catheter placement.
Twenty-three (43%) patients were receiving active chemotherapy at the time of intestinal perforation with 10 (19%) patients receiving taxane-based treatment (TC). One patient received bevacizumab and capecitabine two days prior to perforation, and a second patient had received combination carboplatin, paclitaxel, and bevacizumab approximately 4 weeks prior to perforation. Seventy-seven percent of cervical cancer and 63% of uterine cancer patients were not under active treatment compared to patients with ovarian/primary peritoneal and other cancers, 35% and 33%, respectively. Cervical and uterine cancer patients were combined into a single category due to small sample sizes. When patients were categorized either as ovarian/primary peritoneal/other cancers or cervical/uterine cancer, the association between disease site grouping and treatment status was statistically significant at p<0.01. No difference in age, BMI or race was found when comparing those receiving active treatment at the time of perforation to those not on active treatment.
Neither disease site nor history of prior abdominal or pelvic radiotherapy impacted survival from the time of perforation. Twenty-eight patients (52.8%) had a history of radiation therapy with perforations occurring as follows: 7 small bowel perforations with 1 documented perforation in the distal jejunum, 8 ileal perforations, 8 rectosigmoid perforations, 2 appendiceal perforations, and 3 perforations in unknown locations. Based on available records, it is difficult to determine the precise proportion of perforations which occurred in the irradiated fields. However, all 28 patients had a history of pelvic radiotherapy, and 25 of these perforations could have occurred within the standard pelvic fields.
When examined in a univariate fashion, there was no statistically significant difference in survival from the time of perforation with respect to smoking history, history of bowel surgery or injury during the most recent abdominal surgery prior to perforation, or patients’ presentation with abdominal pain, nausea/vomiting, fever, abnormal bowel movements, potential perforation etiology, or site of bowel perforation. However, patients who were without evidence of disease or who were newly diagnosed with a gynecologic malignancy were found to have a median survival time of 24.7 and 28.1 months, respectively, compared to patients with stable or progressive disease with a median survival time of 3.67 months from the time of perforation (p=0.006). Patients who underwent surgery for treatment of their bowel perforation had a longer median survival time compared to patients who were treated conservatively, including observation (13.7 months compared to 0.50 months, p=0.007). Survival from the time of perforation differed when compared by BMI groups (p-0.013). Patients with a normal BMI (18.5–25.0 kg/m2) had the longest survival time of 68.0 months, compared to underweight (BMI <18.5 kg/m2) and overweight patients (BMI 25.1–30.0 kg/m2), 14.10, and 13.7 months. Patients who were obese (BMI >30.0) had the shortest survival time of 2.47 months.
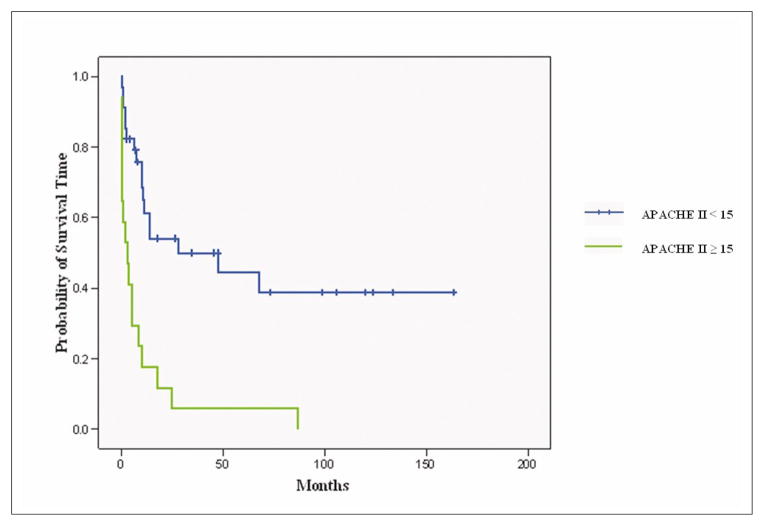
Prognostic factors examined by Cox regression in a univariate fashion are listed in Table 2. BMI, disease status, WBC, bicarbonate level, APACHE II, and treatment of perforation were all significantly associated with risk of death. When these variables, along with cancer treatment at the time of intestinal perforation, were included in a multivariate regression, only APACHE II scores remained significantly associated with an increased risk of death (HR=1.20, 95%CI 1.12, 1.29). Patients who had APACHE II scores < 15 had a median survival of 28.13 months compared to a survival of 2.90 months in those with scores ≥15 (p<0.0001) (Figure 1).
Table 2.
Univariate Cox Regression Analysis
| Variable | HR | 95% CI | p-value |
|---|---|---|---|
|
| |||
| BMI (kg/m2)† | 1.07 | 1.02, 1.12 | <0.01 |
|
| |||
| Age (yrs) | 1.00 | 0.97, 1.03 | 0.87 |
|
| |||
| XRT (no/yes) | 0.99 | 0.51, 1.93 | 0.98 |
|
| |||
| Prior bowel surgery/injury* (no/yes) | 0.55 | 0.24, 1.23 | 0.14 |
|
| |||
| Cancer treatment at time of perforation (no/yes)† | 1.82 | 0.92, 3.60 | 0.08 |
|
| |||
| Disease site | |||
| Cervical (reference) | 0.87 | ||
| Uterine | 0.74 | 0.24, 2.26 | |
| Ovarian/primary peritoneal | 1.09 | 0.50, 2.36 | |
| Other | 1.26 | 0.45, 3.54 | |
|
| |||
| Disease status† | |||
| NED (reference category) | <0.01 | ||
| Progressive/stable | 3.10 | 1.34, 7.21 | |
| Newly diagnosed | 1.13 | 0.41, 3.14 | |
|
| |||
| Abdominal pain (no/yes) | 1.54 | 0.58, 4.07 | 0.38 |
|
| |||
| Fever (no/yes) | 1.64 | 0.83, 3.23 | 0.15 |
|
| |||
| Nausea/vomiting (no/yes) | 0.91 | 0.41, 2.01 | 0.82 |
|
| |||
| Bowel movements | |||
| Normal (reference) | 0.96 | ||
| Abnormal | 0.98 | 0.47, 2.05 | |
|
| |||
| WBC (per 1,000 WBCs/μL) † | 1.04 | 1.01, 1.07 | 0.02 |
|
| |||
| HCO3 (per mEQ/L)† | 0.92 | 0.86, 1.00 | 0.04 |
|
| |||
| Albumin (g/dL) | 0.86 | 0.54, 1.37 | 0.52 |
|
| |||
| APACHE II† | 1.20 | 1.12, 1.29 | <0.01 |
|
| |||
| Treatment of perforation† | |||
| Conservative (reference) | 0.01 | ||
| Surgical | 0.29 | 0.11, 0.76 | |
|
| |||
| Suspected perforation cause | |||
| Iatrogenic (reference)§ | 0.17 | ||
| Tumor | 2.00 | 0.63, 6.36 | |
| Unknown | 1.74 | 0.65, 4.66 | |
| Colitis/appendicitis/proctitis | 0.56 | 0.13, 2.36 | |
|
| |||
| Location of perforation | |||
|
| |||
| Small bowel (reference) | 0.32 | ||
| Ascending/Transverse/Descending Colon | 1.94 | 0.80, 4.72 | |
| Sigmoid/Rectum | 1.23 | 0.54, 2.79 | |
Variables included in multivariate Cox regression analysis
Bowel surgery/injury at the time of most recent abdominal surgery prior to intestinal perforation
Abbreviations: BMI, body mass index; XRT, radiation therapy; WBC, white blood cells; HCO3, bicarbonate; NED, no evidence of disease.
Iatrogenic causes include those diagnosed within 2 weeks of after staging surgery, colonoscopy, or intraperitoneal catheter placement
Figure 1.
Kaplan Meier Estimates of Survival Time
Discussion
Scoring systems are important tools necessary to allow objective and systematic assessment of disease severity and prognostic prediction. The choice of therapy may be influenced after consideration of the clinical assessment in conjunction with disease severity according to these scoring systems. However, no ideal or generally accepted scoring system exists for intestinal perforation. The APACHE II score was originally calculated as an admission score to intensive care units independent of treatment. The initial utility of the scoring system was not intended to evaluate the efficacy of therapy or interventions. However, an increasing number of studies are utilizing APACHE II longitudinally for patient evaluation since the patient’s status and APACHE II score may alter after treatment. In our study, we found disease status, treatment approach of intestinal perforation, APACHE II score and BMI to be significantly associated with prolonged survival time after intestinal perforation, but after multivariate analysis, only APACHE II scores remained statistically significant.
Several studies have examined potential prognostic factors which influence patient outcome after intestinal perforation. Renal function, white blood cell count, and acid-base status have been found to be potential markers for prognosis.[13] Scoring systems including APACHE II, Mannheim peritonitis index (MPI), and peritonitis index of Altona (PIA II) have also been evaluated to predict mortality in patients with peritonitis.[12, 14–16] However, only the APACHE II scoring system has been validated to assess prognosis with pre-operative data.[12]
APACHE was a physiologically based classification system initially designed in the 1970’s as a method to stratify patients based on severity of illness in an intensive care setting. [17] This system incorporated 33 physiologic characteristics and was viewed to be too complex thus allowing for the evolution of the revision, APACHE II. The new version incorporates a point-based system evaluating 12 routine physiologic measurements (temperature, blood pressure, respiratory rate, heart rate, serum sodium, hematocrit, WBC count, serum creatinine, and arterial blood gases) as well as age and health status.[12] The presence of severely compromised cardiopulmonary, hepatic, renal, or immunologic function adds points to the APACHE II score. The Glasgow Coma Scale (GCS) to assess neurologic function and the presence of acute renal failure also contribute to the final score. The maximum APACHE II score is 71, but the highest calculated APACHE II score to date is 55.[12]
Studies have found that increasing APACHE II scores correlate with subsequent risk of hospital death in the intensive care setting, as well as with several other disease processes, including intestinal perforation.[12, 14, 18–21] APACHE II scores can be used to compare studies evaluating patients of similar physiologic changes and diseases and is a useful marker to predict mortality rates in defined patient groups and diagnostic categories. Several studies have attempted to evaluate the ability of APACHE II to predict outcome for the individual patient in an intensive care setting. [15, 22–24] Marks et al. conducted a prospective study of 568 patients admitted to the intensive care unit (ICU) comparing outcome predictions based on APACHE II scores with the subjective assessment by a physician and nurse at the time of admission.[24] They found the clinician’s evaluation to be a more powerful outcome predictor than the APACHE II scores, emphasizing that the APACHE II score can be applied to stratify patient groups in an ICU setting to predict overall outcome but should not be used for the individual patient. However, this study evaluated a heterogenous patient population and included patients admitted to a mixed medical and surgical intensive therapy unit. The application of APACHE II scores to predict individual patient outcome in a more homogenous population requires further exploration.
Previously, Ohmann et al. conducted a large prospective multi-centered trial of 271 patients with confirmed peritonitis at laparotomy and reported that the APACHE II was superior to the MPI and PIA II in its ability to define risk groups and its reliability.[15] A significant correlation and linear relationship between APACHE II score and mortality was detected. Additionally, when measured preoperatively, the APACHE II score accurately risk stratified patients with duodenal perforation and was found to predict both mortality and morbidity after multivariate analysis.[21] Horiuchi et al. evaluated 26 patients who underwent emergency surgery for colorectal perforation over 12 years and found that survivors had significantly lower mean APACHE II score of 10.4 compared to 19.3 in non-survivors (p <0.001).[25] Patients with untreated abscesses and APACHE II scores < 15 had a 1.7% mortality risk compared to 78% in patients who had scores ≥15 (p<0.0001).[26] These data are consistent with the results observed in our study. We found that increasing APACHE II scores were correlated with shorter survival times from the date of diagnosis of intestinal perforation to the date of death or last contact. Patients with APACHE II scores < 15 had a median survival time of 28 months compared to a median survival time of 3 months in patients with scores ≥ 15.
During the time of initial patient presentation, clinicians often inquire about specific symptoms to assist in patient diagnosis, treatment, and risk stratification. When we compared patients with APACHE II scores < 15 to those with scores ≥15, there did not appear to be a statistically significant difference in age or presenting symptoms such as abdominal pain, fever, nausea/vomiting, or abnormal bowel movements prior to intestinal perforation diagnosis (Table 3). However, patients with APACHE II scores ≥15 did have a significantly higher mean BMI compared to those with lower APACHE II scores. Ironically, the albumin levels and nutritional status between the two groups was not significantly different. This indicates that although nutritional status is important in a patient’s ability to recover overall, other co-morbidities associated with elevated BMI levels may play a more significant role in the mortality risk after intestinal perforation.
Table 3.
Comparison of Patients with APACHE II scores < 15 versus scores ≥ 15
| Characteristic | APACHE II < 15 | APACHE II ≥ 15 | p-value |
|---|---|---|---|
|
| |||
| Age (years)* | 55.47 | 56.71 | 0.761 |
|
| |||
| BMI (kg/m2)* | 24.28 | 28.72 | 0.012 |
|
| |||
| LOS (days)* | 25.59 | 18.65 | 0.299 |
|
| |||
| Albumin (g/dL)* | 2.65 | 2.44 | 0.331 |
|
| |||
| WBC (103/μL)* | 10.29 | 18.06 | 0.011 |
|
| |||
| ANC (103/μL)* | 8.31 | 15.07 | 0.011 |
|
| |||
| HCO3− (mEQ/L)* | 25.56 | 21.12 | 0.002 |
|
| |||
| Creatinine (mg/dL)* | 0.74 | 1.72 | <0.001 |
|
| |||
| Disease status | |||
| NED | 13 | 3 | 0.059 |
| Stable/Progressive | 12 | 12 | |
| Newly Diagnosed | 9 | 2 | |
|
| |||
| Active treatment | |||
| No | 23 | 6 | 0.038 |
| Yes | 11 | 11 | |
Mean values
BMI = body mass index, LOS = length of hospital stay, WBC = white blood cell count, ANC = absolute neutrophil count, HCO3− = bicarbonate, NED = no evidence of disease
In addition to patient demographics and presenting symptoms, most clinicians also examine and consider baseline laboratory values to aid in diagnosis and clinical management. We found that patients with normal WBC counts and normal acid/base status tended to have longer median survival times from time of diagnosis of perforation compared to those with abnormal levels. However, after multivariate analysis, these factors did not appear to influence survival with the same significance as the APACHE II score. Additionally, patients with APACHE II scores ≥ 15 had higher mean WBC and creatinine levels and lower mean bicarbonate levels than those with scores <15 (Table 3). Furthermore, the odds of patients with higher APACHE II scores being actively treated for their disease at the time of intestinal perforation was 3.88 times greater than those with lower APACHE II scores.
Due to its retrospective nature, there are inherent limitations to this study. Unmeasured potentially confounding factors may exist which influence patient health status and outcome. It is difficult to ascertain the relationship between exact timing of symptom onset with patient presentation and perforation diagnosis. Patients may have had symptoms associated with perforation prior to the time of presentation. Those who sought medical attention earlier in their disease course likely received medical intervention sooner and, thereby, may have had better outcomes. Additionally, arterial blood gas values were not available for all patients, and acid/base status for those patients was estimated utilizing measured bicarbonate levels. Although substitution with bicarbonate is appropriate, it may not reflect the true APACHE II score.[12] While it is difficult to make definitive conclusions based on the overall small patient population included in this study, our results are similar to those demonstrated by prior investigators.[21, 25, 26]
Gynecologic oncologists traditionally consider the possibility of intestinal perforation in the differential diagnosis of patients presenting with abdominal pain and associated symptoms. However, several factors must be considered when determining the management approach, such as potential immunosuppression with recent chemotherapy, global health status, and disease status. As healthcare resources become increasing limited, the identification of potential mortality risk factors after intestinal perforation becomes essential since they would help guide treatment plans, and the implementation of a prognostic risk stratification system would aid in patient counseling after such a life-threatening event. We found that disease status, BMI within normal range, and surgical management of perforations were found to have improved survival times after perforation. However, after multivariate analysis, none of these factors play as significant a role as the APACHE II score. Our data indicate that patients with higher APACHE II scores at the time of intestinal perforation have shorter survival times after diagnosis of perforation. Further studies are needed to validate the prognostic ability of APACHE II scores in gynecologic oncology patients with intestinal perforations and to examine additional potential prognostic factors which may help guide treatment management of perforation in this patient population.
Footnotes
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bielecki K, Kaminski P, Klukowski M. Large bowel perforation: morbidity and mortality. Tech Coloproctol. 2002;6:177–82. doi: 10.1007/s101510200039. [DOI] [PubMed] [Google Scholar]
- 2.Torosian MH, Turnbull AD. Emergency laparotomy for spontaneous intestinal and colonic perforations in cancer patients receiving corticosteroids and chemotherapy. J Clin Oncol. 1988;6:291–6. doi: 10.1200/JCO.1988.6.2.291. [DOI] [PubMed] [Google Scholar]
- 3.Nespoli A, Ravizzini C, Trivella M, Segala M. The choice of surgical procedure for peritonitis due to colonic perforation. Arch Surg. 1993;128:814–8. doi: 10.1001/archsurg.1993.01420190110014. [DOI] [PubMed] [Google Scholar]
- 4.Yamazawa K, Matsui H, Sekiya S. Gastric perforation induced by combination chemotherapy in a patient with long-term use of corticosteroids. Int J Gynaecol Obstet. 2002;78:165–6. doi: 10.1016/s0020-7292(02)00133-9. [DOI] [PubMed] [Google Scholar]
- 5.Ramirez PT, Levenback C, Burke TW, Eifel P, Wolf JK, Gershenson DM. Sigmoid perforation following radiation therapy in patients with cervical cancer. Gynecol Oncol. 2001;82:150–5. doi: 10.1006/gyno.2001.6213. [DOI] [PubMed] [Google Scholar]
- 6.Yamashita H, Nakagawa K, Tago M, Igaki H, Shiraishi K, Nakamura N, Sasano N, Yamakawa S, Ohtomo K. Small bowel perforation without tumor recurrence after radiotherapy for cervical carcinoma: report of seven cases. J Obstet Gynaecol Res. 2006;32:235–42. doi: 10.1111/j.1447-0756.2006.00382.x. [DOI] [PubMed] [Google Scholar]
- 7.Seewaldt VL, Cain JM, Goff BA, Tamimi H, Greer B, Figge D. A retrospective review of paclitaxel-associated gastrointestinal necrosis in patients with epithelial ovarian cancer. Gynecol Oncol. 1997;67:137–40. doi: 10.1006/gyno.1997.4842. [DOI] [PubMed] [Google Scholar]
- 8.Rose PG, Piver MS. Intestinal perforation secondary to paclitaxel. Gynecol Oncol. 1995;57:270–2. doi: 10.1006/gyno.1995.1140. [DOI] [PubMed] [Google Scholar]
- 9.de Haan D, van den Berg M. Colonic perforation secondary to taxol therapy: an unusual presentation. Onkologie. 2006;29:541–2. doi: 10.1159/000096150. [DOI] [PubMed] [Google Scholar]
- 10.Kouroussis C, Samonis G, Androulakis N, Souglakos J, Voloudaki A, Dimopoulos MA, Kotsakis T, Kakolyris S, Kalbakis K, Georgoulias V. Successful conservative treatment of neutropenic enterocolitis complicating taxane-based chemotherapy: a report of five cases. Am J Clin Oncol. 2000;23:309–13. doi: 10.1097/00000421-200006000-00021. [DOI] [PubMed] [Google Scholar]
- 11.Han ES, Monk BJ. What is the risk of bowel perforation associated with bevacizumab therapy in ovarian cancer? Gynecol Oncol. 2007;105:3–6. doi: 10.1016/j.ygyno.2007.01.038. [DOI] [PubMed] [Google Scholar]
- 12.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 13.Komatsu S, Shimomatsuya T, Nakajima M, Amaya H, Kobuchi T, Shiraishi S, Konishi S, Ono S, Maruhashi K. Prognostic factors and scoring system for survival in colonic perforation. Hepatogastroenterology. 2005;52:761–4. [PubMed] [Google Scholar]
- 14.Kulkarni SV, Naik AS, Subramanian N., Jr APACHE-II scoring system in perforative peritonitis. Am J Surg. 2007;194:549–52. doi: 10.1016/j.amjsurg.2007.01.031. [DOI] [PubMed] [Google Scholar]
- 15.Ohmann C, Wittmann DH, Wacha H. Prospective evaluation of prognostic scoring systems in peritonitis. Peritonitis Study Group. Eur J Surg. 1993;159:267–74. [PubMed] [Google Scholar]
- 16.Kologlu M, Elker D, Altun H, Sayek I. Validation of MPI and PIA II in two different groups of patients with secondary peritonitis. Hepatogastroenterology. 2001;48:147–51. [PubMed] [Google Scholar]
- 17.Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med. 1981;9:591–7. doi: 10.1097/00003246-198108000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Larvin M, McMahon MJ. APACHE-II score for assessment and monitoring of acute pancreatitis. Lancet. 1989;2:201–5. doi: 10.1016/s0140-6736(89)90381-4. [DOI] [PubMed] [Google Scholar]
- 19.Hsieh HF, Chen TW, Yu CY, Wang NC, Chu HC, Shih ML, Yu JC, Hsieh CB. Aggressive hepatic resection for patients with pyogenic liver abscess and APACHE II score > or =15. Am J Surg. 2008;196:346–50. doi: 10.1016/j.amjsurg.2007.09.051. [DOI] [PubMed] [Google Scholar]
- 20.Han SH, Chin BS, Lee HS, Jeong SJ, Choi HK, Kim CO, Yong D, Choi JY, Song YG, Lee K, Kim JM. Vancomycin-resistant enterococci bacteremia: risk factors for mortality and influence of antimicrobial therapy on clinical outcome. J Infect. 2009;58:182–90. doi: 10.1016/j.jinf.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 21.Lee FY, Leung KL, Lai BS, Ng SS, Dexter S, Lau WY. Predicting mortality and morbidity of patients operated on for perforated peptic ulcers. Arch Surg. 2001;136:90–4. doi: 10.1001/archsurg.136.1.90. [DOI] [PubMed] [Google Scholar]
- 22.Ohmann C, Hau T. Prognostic indices in peritonitis. Hepatogastroenterology. 1997;44:937–46. [PubMed] [Google Scholar]
- 23.Rutledge R, Fakhry SM, Rutherford EJ, Muakkassa F, Baker CC, Koruda M, Meyer AA. Acute Physiology and Chronic Health Evaluation (APACHE II) score and outcome in the surgical intensive care unit: an analysis of multiple intervention and outcome variables in 1,238 patients. Crit Care Med. 1991;19:1048–53. doi: 10.1097/00003246-199108000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Marks RJ, Simons RS, Blizzard RA, Browne DR. Predicting outcome in intensive therapy units--a comparison of Apache II with subjective assessments. Intensive Care Med. 1991;17:159–63. doi: 10.1007/BF01704720. [DOI] [PubMed] [Google Scholar]
- 25.Horiuchi A, Watanabe Y, Doi T, Sato K, Yukumi S, Yoshida M, Yamamoto Y, Sugishita H, Kawachi K. Evaluation of prognostic factors and scoring system in colonic perforation. World J Gastroenterol. 2007;13:3228–31. doi: 10.3748/wjg.v13.i23.3228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levison MA, Zeigler D. Correlation of APACHE II score, drainage technique and outcome in postoperative intra-abdominal abscess. Surg Gynecol Obstet. 1991;172:89–94. [PubMed] [Google Scholar]