Abstract
Purpose
To report a case of bilateral glaucoma related to pseudophacomorphic mechanism in one eye and pupillary block in the other eye after Visian Implantable Collamer Lens (ICL, STAAR Surgical) insertion.
Methods
A 44 year-old female with high myopia underwent bilateral ICL implantation of MICL12.6 after sulcus diameter measurements were performed by Pentacam.
Results
Pseudophacomorphic glaucoma-related angle closure occurred due to lens oversizing in the right eye. The mechanism was relieved via ICL explantation. In the left eye, pupillary block developed in a subacute manner after closure of the peripheral iridotomy (PI). The attack was ameliorated by reestablishing patency of the iridotomy.
Conclusions
ICL-related glaucomatous attacks may result from improper sizing as well as from placement of a single PI. Identification of the proper mechanism is vital as treatments differ significantly. In pseudophacomorphic glaucoma, explantation is needed. In pupillary block glaucoma, treatment involves establishment of a patent PI.
Keywords: Pseudophacomorphic, Glaucoma, Visian ICL, Pupillary Block
Introduction
Phakic intraocular lenses (pIOLs) play an important role in the arsenal of the refractive surgeon, particularly in patients with high levels of myopia.[1] Placement of pIOLs has a relatively high safety profile when patients are appropriately screened, and careful preoperative planning guides high quality intraoperative execution.[2] Deviating from this approach can lead to significant problems.
The Visian implantable collamer lens (ICL; STAAR Surgical, Monrovia, California) is a posterior chamber pIOL. Its plate haptics are supported by the ciliary sulcus, allowing for an anteriorly vaulted configuration between the natural lens and iris. This positioning puts the patient at risk for pupillary block. Peripheral iridotomies (PI), two per eye, must be placed preoperatively with adequate time to confirm patency.[3]
Appropriate lens size selection is also important. The sulcus-to-sulcus diameter can be estimated using the white-to-white measurement, or measured using imaging technologies including the rotating Scheimpflug camera and high-frequency ultrasound.[4, 5, 6] Oversized lenses can vault anteriorly causing pupillary block or pigment dispersion syndrome. Undersized lenses may decentrate or rotate increasing the risk for refractive error and PI occlusion.[7]
We report a case of bilateral glaucoma secondary to a pseudophacomorphic mechanism with compressive angle closure accompanied by corneal edema, atonic pupil, and cataract formation along with pupillary block.
Case Report
A 44 year-old highly myopic female (− 13.75 D right eye, −13.25 D left eye) with no past ocular history presented for evaluation of refractive surgical candidacy. Due to the patient’s high refractive error and associated high ablative requirement, it was determined that implantation of an ICL represented the best corrective option. A single PI was performed in each eye at 12 oclock using a neodymium:YAG (Nd:YAG) laser 1.5 weeks preoperatively. MICL12.6 Visian ICLs were selected bilaterally based on sulcus diameters measured by the Pentacam (Oculus Optikgerate GmbH). A 3.2 mm peripheral temporal clear corneal wound was created. ICL implantation was executed in an uncomplicated fashion under topical anesthesia.
Three hours after completion of the procedure, the patient complained of a severe headache and nausea with associated intraocular pressures (IOP) of 36 mm Hg in the right eye and 20 mm Hg in the left eye (measured by Goldmann applanation tonometry). Moderate right eye cell-and-flare were also present. ICLs appeared well-positioned in the posterior chamber. Right eye pupillary block was diagnosed, and the patient was given cyclopentolate, scopolamine, and taken to the emergency department for administration of intravenous mannitol.
On postoperative day 1, uncorrected visual acuities were hand motion in the right eye and 20/20 in the left eye. Right eye wound dehiscence with iris prolapse was present along with moderate corneal edema and iris synechiae to the ICL. The patient was taken to the operative room immediately for synechiolysis, iris and ICL repositioning, and suturing of the operative wound.
On postoperative day 2, the patient demonstrated a moderate degree of diffuse right eye corneal edema along with a mid-dilated nonreactive pupil and trace cell/flare. Uncorrected visual acuities were hand motion in the right eye and 20/20 in the left eye. Intraocular pressure was 11 in both eyes. Right eye ICL position could not be accurately determined; left eye examination showed no signs of complication with a ICL vault distance of 1.5 units of corneal thickness. Durezol (Alcon Laboratories, Fort Worth, Texas), Vigamox (Alcon Laboratories, Fort Worth, Texas), and Combigan (Allergan, Irvine, California) were initiated three times per day in the right eye at this time.
The patient’s postoperative course continued without incident until approximately 2 weeks later, at which point she developed periocular pain, a headache, and temporary subjective loss of vision in the left eye. Uncorrected visual acuity surprisingly declined from 20/20 to 20/400. Tonometric values were 17 mm Hg in the right eye, and 33 mm Hg in the left eye. It was discovered that there was no transillumination of the left peripheral iridotomy. A repeat laser PI was attempted without success. The patient was taken to the operating room, and a surgical iridectomy was performed in the left eye. The patient was then discharged home with Combigan TID and Lumigan (Allergan, Irvine, California) QHS in the left eye. Over the next 2 weeks vision in the left eye returned to baseline.
Intraocular pressure normality was sustained thereafter in both eyes, although the patient began to undergo rapid development of right eye anterior subcapsular cataract along with iris atrophy and atonic pupil. Combined ICL explantation and cataract extraction with posterior chamber intraocular lens implantation was performed on the right eye approximately 1 month following initial ICL insertion. No overt complications were observed postoperatively, and the visual acuity began to improve to 20/50. Gradual resolution of central corneal edema ensued yielding 2+ temporal corneal edema extending into the visual axis.
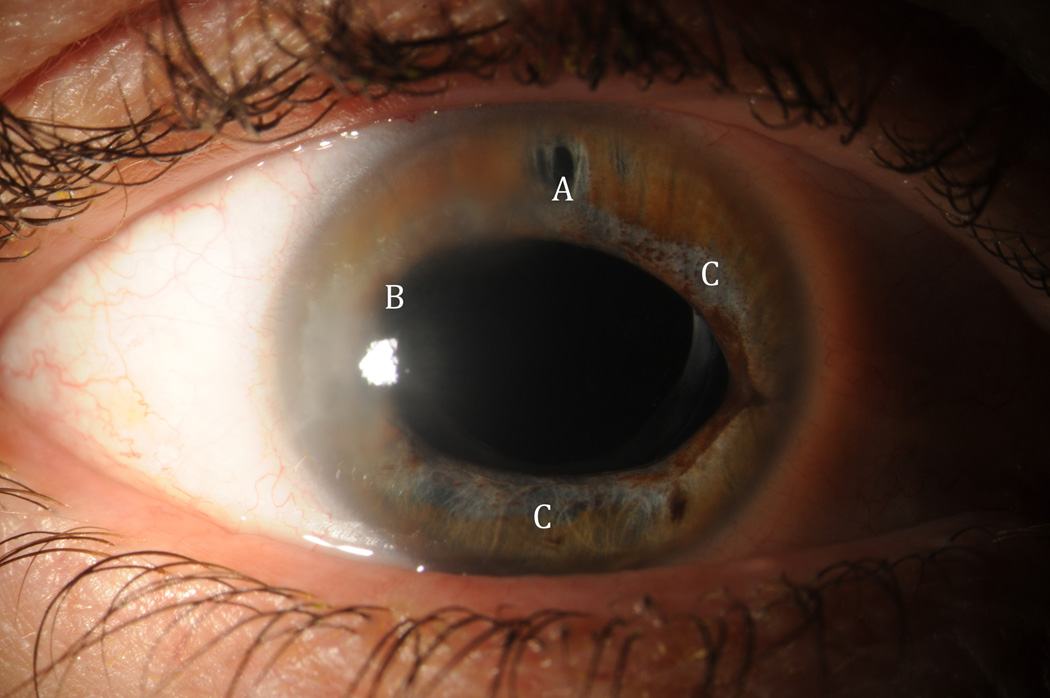
Approximately 4 months after primary ICL insertion, the patient was referred to our institution for evaluation and management of right eye corneal edema and atonic pupil (Figure 1) with associated glare and photophobia. Best-corrected visual acuities were 20/50 +2 in the right eye, and 20/20 +2 in the left eye; tonometric values were 20 mm Hg in the right eye, and 14 mm Hg in the left eye. The patient was not on any IOP lowering medications at this point. On slit lamp examination, right eye moderate temporal corneal edema and as well as atonic pupil and irregularity were observed. The PCIOL was well centered within the capsule. A large surgical sectoral iridectomy (Figure 2) was observed in the left eye. The Visian ICL was appropriately vaulted and positioned OS. Myopic fundi were noted on dilated fundus exam with mild macular thickening in the right eye. Ocular coherence tomography (OCT) confirmed a central macular thickness of 270 microns in the right eye and 220 microns in the left eye.
Figure 1.
A slit-lamp photograph showing a patient PI (A), temporal corneal edema (B) , traumatic mydriasis, and iris atrophy (C)
Figure 2.
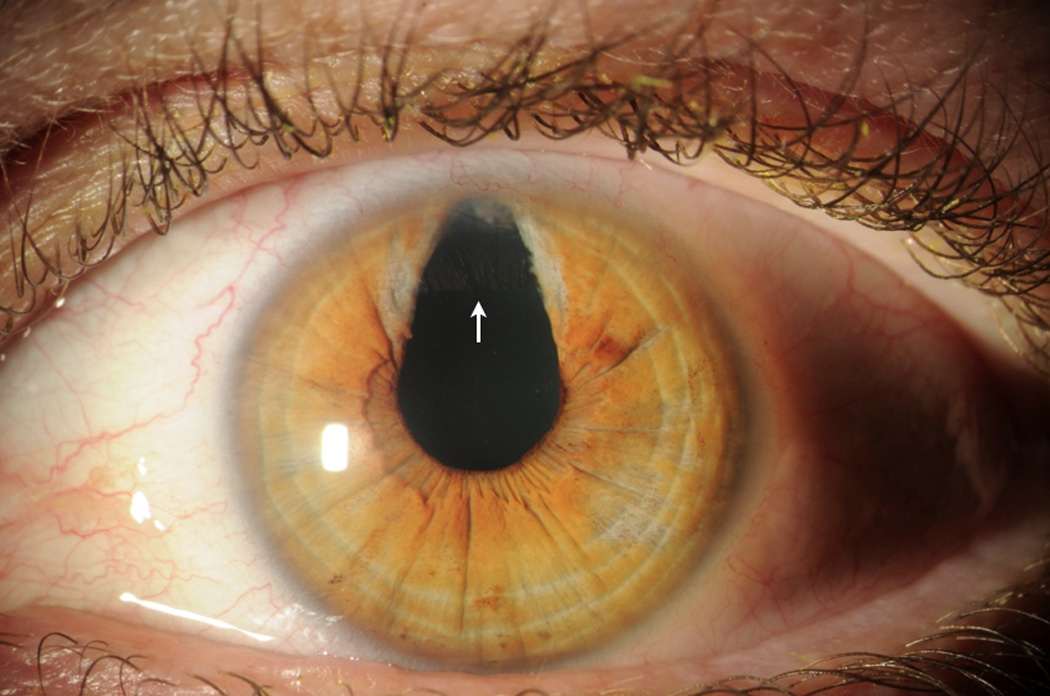
A slit-lamp photograph showing a large sectoral surgical iridectomy exposing the edge of the Visian ICL (white arrow)
Ketorolac BID along with daily Lotemax (Bausch + Lomb, Rochester, New York) were prescribed for treatment of post-surgical macular edema. During two subsequent visits over 6 months, the right eye corneal edema had diminished significantly and the macular edema resolved with a resultant improvement of uncorrected visual acuity to 20/25. The vision in the left eye improved to 20/15. Specular microscopy was performed, demonstrating an endothelial cell count of < 600 in the right eye, and > 2,000 in the left eye. An option of right eye pupilloplasty versus cosmetic colored contact lens was discussed with the patient. In order to reduce glare and halo, she chose use of a colored contact lens due to the risk of surgical intervention precipitating further endothelial decompensation. Descemet’s stripping automatic endothelial keratoplasty (DSAEK) was also discussed should surgical intervention become necessary.
Discussion
The placement of ICLs for the correction of high refractive error is not without risk. The first posterior chamber phakic intraocular lenses encountered complications including decentration, cataract formation, glaucoma, and uveitis.[3] Advancements in surgical technique, lens design, and materials have significantly improved results. However, complications may still occur.
ICL-related pupillary block is one of the most concerning complications associated with implantation and has been reported in the literature.[8, 9] The posterior iris margin and ICL optic may establish contact in such a way as to prevent posterior to anterior transpupillary flow of aqueous and subsequent iris bombé configuration with blockage of trabecular outflow and elevated intraocular pressure. This form of pupillary block – which is analogous to primary angle closure – may occur in the acute, subacute, or chronic settings following ICL placement, and may be prevented by means of PI placement. Experts recommend the placement of two PIs in each eye, each separated by 80–90 degrees, in order to have one patent PI if the other is occluded or nonfunctional.[3, 10] In the presented surgical case, only one PI was placed per eye.
PI obstruction may occur if lens undersizing leads to rotation or decentration, resulting in a haptic blocking a PI. A study of the phakic refractive lens (PRL) (Carl Zeiss Meditec) documented a median lens rotation of 18 degrees at one year with a range of 0 to 98 degrees.[11] PI obstruction can also occur secondary to blood clot formation, or healing of a small or perhaps imperforate PI.[10]
In the presented case, only one PI was placed in each eye. As a result of PI closure in the left eye, pupillary block glaucoma developed. As the lenses were likely not undersized, it is more likely that occlusion occurred secondary to blood clot, healing, or imperforate PI, rather than secondary to lens rotation.
An oversized ICL can lead to angle closure via an additional glaucoma mechanism that can be difficult to differentiate from pupillary block. Oversizing results in excessive lens vault, which can push the iris forwards into the trabecular meshwork via a direct compressive mechanism.[12, 13] This resembles the entity of phacomorphic glaucoma that is familiar to many clinicians. We call this pseudophacomorphic glaucoma, which can only achieve permanent resolution through ICL explantation, and will not resolve with PI. Anterior segment OCT or ultrasound biomicroscopy can demonstrate significant ICL vaulting and direct compressive pseudophacomorphic angle closure.[12] Nevertheless, the diagnosis of pseudophacomorphic angle closure can be made clinically if the angle is closed despite patent PI.
Temporary resolution can occur with cycloplegia in cases where the ICL is not severely oversized. Cycloplegia widens the ciliary body ring and thus increases the diameter of the ciliary sulcus; this can reduce ICL vaulting, which may in turn result in reversal of angle closure.[13] Observing this reversal can be helpful diagnostically, but is not a sensitive test because severe oversizing will not respond favorably to cycloplegia. Thus, all oversized lenses producing pseudophacomorphic glaucoma with or without cycloplegia must be removed.
We speculate that this patient suffered from glaucomatous attacks of two different etiologies. The acute right eye episode, which occurred in the immediate postoperative period, was secondary to pseudophacomorphic glaucoma. The left eye episode occurred in a subacute manner as a result of a non-patent PI. The situation was easily ameliorated by reestablishing patency of the original PI by means of sectoral iridectomy.
It is likely that this patient developed wound dehiscence with iris prolapse as a result of ICL oversizing. The expansive force of the ICL within the sulcus likely gaped the operative peripheral clear corneal wound. Elevated intraocular pressure secondary to pseudophacomorphic glaucoma may also have contributed to wound dehiscence. We believe this is the first report of wound dehiscence secondary to placement of an oversized ICL.
Despite successful cataract extraction with intraocular lens placement and resolution of macular edema, the patient continued to have severe glare and photophobia most likely related to the pupillary abnormalities including permanent mydriasis that may have resulted from high IOP. Surgical and nonsurgical options were discussed including pupilloplasty and/or colored contact lens fitting.[14, 15] It was concluded that further intraocular manipulation would likely result in additional endothelial decompensation due to the low cell count. In order to avoid this scenario, the patient opted for a colored contact lens trial. Pupilloplasty remained an option with the knowledge that further corneal decompensation may necessitate a descemets stripping automated endothelial keratoplasty (DSAEK) in the future.
ICL-related glaucoma mechanisms are conditions that can be avoided with the appropriate preoperative planning. Paramount in importance is the establishment of two patent PIs 80–90 degrees apart.[3, 10] Lack of correspondence between the white-to-white interval and ciliary sulcus diameter poses a risk for inappropriate lens oversizing.[5] Preoperative evaluation through use of high frequency ultrasound biometry should be standardized to provide greater accuracy for determining the most patient-appropriate ICL size.[4] If pressure elevation does occur, PIs should be inspected for patency and enlarged if transillumination is not observed. Angle closure in the setting of patent PI necessitates explantation of ICLs due to the aggressive pseudophacomorphic glaucoma mechanism.
References
- 1.Huang D, Schallhorn SC, Sugar A, et al. Phakic intraocular lens implantation for the correction of myopia: a report by the American Academy of Ophthalmology. Ophthalmology. 2009;116:2244–2258. doi: 10.1016/j.ophtha.2009.08.018. http://dx.doi.org/10.1016/j.ophtha.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 2.Igarashi A, Shimizu K, Kamiya K. Eight-year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Am J Ophthalmol. 2014;157:532–539. doi: 10.1016/j.ajo.2013.11.006. http://dx.doi.org/10.1016/j.ajo.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 3.Azar DT. Refractive Surgery. 2nd Edition. New York, New York: Elsevier Inc; 2007. [Google Scholar]
- 4.Kojima T, et al. Optimization of an implantable collamer lens sizing method using high-frequency ultrasound biomicroscopy. Am J Ophthalmol. 2012;153(4):632–637. doi: 10.1016/j.ajo.2011.06.031. http://dx.doi.org/10.1016/j.ajo.2011.06.031. [DOI] [PubMed] [Google Scholar]
- 5.Reinstein DZ, Lovisolo CF, Archer TJ, Gobbe M. Comparison of postoperative vault height predictability using white-to-white or sulcus diameter-based sizing for the visian implantable collamer lens. J Refract Surg. 2013;29(1):30–35. doi: 10.3928/1081597X-20121210-02. http://dx.doi.org/10.3928/1081597X-20121210-02. [DOI] [PubMed] [Google Scholar]
- 6.Baumeister M, Buhren J, Kohnen T. Position of angle-supported, iris-fixated, and ciliary sulcus-implanted myopic phakic intraocular lenses evaluated by Scheimpflug photography. Am J Ophthalmol. 2004;138(5):723–731. doi: 10.1016/j.ajo.2004.06.009. http://dx.doi.org/10.1016/j.ajo.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 7.Kohnen T, Kook D, Morral M, Güell JL. Phakic intraocular lenses part 2: results and complications. J Cataract Refract Surg. 2010;36:2168–2194. doi: 10.1016/j.jcrs.2010.10.007. http://dx.doi.org/10.1016/j.jcrs.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Smallman DS, Probst L, Rafuse PE. Pupillary block glaucoma secondary to posterior chamber phakic intraocular lens implantation for high myopia. J Cataract Refract Surg. 2004;30(4):905–907. doi: 10.1016/j.jcrs.2003.09.019. http://dx.doi.org/10.1016/j.jcrs.2003.09.019. [DOI] [PubMed] [Google Scholar]
- 9.Bylsma SS, Zalta AH, Foley E, Osher RH. Phakic posterior chamber intraocular lens pupillary block. J Cataract Refract Surg. 2002;28(12):2222–2228. doi: 10.1016/s0886-3350(02)01303-2. http://dx.doi.org/10.1016/S0886-3350(02)01303-2. [DOI] [PubMed] [Google Scholar]
- 10.Chun YS, Park IK, Lee HI, Lee JH, Kim JC. Iris and trabecular meshwork pigment changes after posterior chamber phakic intraocular lens implantation. J Cataract Refract Surg. 2006;32(9):1452–1458. doi: 10.1016/j.jcrs.2006.04.023. http://dx.doi.org/10.1016/j.jcrs.2006.04.023. [DOI] [PubMed] [Google Scholar]
- 11.Koivula A, Taube M, Zetterstrom C. Phakic Refractive Lens: Two-year Results. Journal of Refractive Surgery. 2008;24:507–515. doi: 10.3928/1081597X-20080501-09. [DOI] [PubMed] [Google Scholar]
- 12.Kahlifa YM, Goldsmith J, Moshirfar M. Bilateral Explantation of Visian Implantable Collamer Lenses Secondary to Bilateral Acute Angle Closure Resulting From a Non-pupillary Block Mechanism. J Refract Surg. 2010;26:991–994. doi: 10.3928/1081597X-20100521-01. http://dx.doi.org/10.3928/1081597X-20100521-01. [DOI] [PubMed] [Google Scholar]
- 13.Chan KC, Birchall W, Gray TB, Wells AP. Acute angle closure after implantable contact lens insertion unresponsive to surgical peripheral iridectomy. J Cataract Refract Surg. 2008;34(4):696–699. doi: 10.1016/j.jcrs.2007.10.048. http://dx.doi.org/10.1016/j.jcrs.2007.10.048. [DOI] [PubMed] [Google Scholar]
- 14.Behndig A. Small incision single-suture-loop pupilloplasty for postoperative atonic pupil. J Cataract Refract Surg. 1998;24:1429–1431. doi: 10.1016/s0886-3350(98)80161-2. http://dx.doi.org/10.1016/S0886-3350(98)80161-2. [DOI] [PubMed] [Google Scholar]
- 15.Olali C, Mohammed M, Ahmed S, Gupta M. Contact lens for failed pupilloplasty. J Cataract Refract Surg. 2008;34(11):1995–1996. doi: 10.1016/j.jcrs.2008.06.040. http://dx.doi.org/10.1016/j.jcrs.2008.06.040. [DOI] [PubMed] [Google Scholar]