Abstract
Introduction
Standard treatment for patients with primary immunodeficiency (PID) is monthly intravenous immunoglobulin (IVIG), or weekly/biweekly subcutaneous immunoglobulin (SCIG) infusion. We used population pharmacokinetic modeling to predict immunoglobulin G (IgG) exposure following a broad range of SCIG dosing regimens for initiation and maintenance therapy in patients with PID.
Methods
Simulations of SCIG dosing were performed to predict IgG concentration–time profiles and exposure metrics [steady-state area under the IgG concentration–time curve (AUC), IgG peak concentration (C max), and IgG trough concentration (C min) ratios] for various infusion regimens.
Results
The equivalent of a weekly SCIG maintenance dose administered one, two, three, five, or seven times per week, or biweekly produced overlapping steady-state concentration–time profiles and similar AUC, C max, and C min values [95% confidence interval (CI) for ratios was 0.98–1.03, 0.95–1.09, and 0.92–1.08, respectively]. Administration every 3 or 4 weeks resulted in higher peaks and lower troughs; the 95% CI of the AUC, C max, and C min ratios was 0.97–1.04, 1.07–1.26, and 0.86–0.95, respectively. IgG levels >7 g/L were reached within 1 week using a loading dose regimen in which the weekly maintenance dose was administered five times in the first week of treatment. In patients with very low endogenous IgG levels, administering 1.5 times the weekly maintenance dose five times in the first week of treatment resulted in a similar response.
Conclusions
The same total weekly SCIG dose can be administered at different intervals, from daily to biweekly, with minimal impact on serum IgG levels. Several SCIG loading regimens rapidly achieve adequate serum IgG levels in treatment-naïve patients.
Electronic supplementary material
The online version of this article (doi:10.1007/s13554-014-0018-0) contains supplementary material, which is available to authorized users.
Keywords: Biological therapy, Dosing regimen, Hizentra®, Immunoglobulin replacement therapy, Loading dose, Pharmacokinetic model, Primary immunodeficiency, Subcutaneous immunoglobulin, Skipped doses
Introduction
Patients with primary immunodeficiency (PID), including those with common variable immunodeficiency (CVID) and X-linked agammaglobulinemia (XLA), are predisposed to recurrent and persistent infections [1–7]. Immunoglobulin G (IgG) replacement therapy provides an effective prophylaxis, and for 30 years, monthly intravenous immunoglobulin (IVIG) has been the standard treatment. However, subcutaneous immunoglobulin (SCIG) given at weekly or biweekly (i.e., every 2 weeks) intervals has become an increasingly popular alternative, which has been boosted by the development of increasingly concentrated formulations (as high as 20%) enabling reduced infusion volumes and increased infusion rates [8–21].
By comparison with monthly IVIG infusion, patients receiving a weekly SCIG dose experience similar protection and infection rates, but demonstrate increased consistency in steady-state IgG levels (reduced peak/trough variation) and suffer fewer systemic adverse events [9, 15, 16, 22–24]. In addition, SCIG preparations can be self-administered at home by most patients. This reduces treatment cost and increases patient convenience, reflected by a measured improvement in patient quality of life [25, 26].
Subcutaneous immunoglobulin regimens typically divide the total monthly IgG dose into 4 weekly infusions. However, greater patient convenience would be achieved by increasing the flexibility of the dosing regimen and enabling individualized dosing schedules. A few clinical trials exploring alternative SCIG dosing regimens have been published [27–29], but testing numerous regimens clinically would be time and cost intensive, and may be burdensome for patients. A powerful approach to test a broad range of dosing regimens is population pharmacokinetic (PK) modeling and simulation [30–35]. By implementing PK models based upon existing clinical data, it is possible to simulate the kinetics of IgG following modification of variables defining a dosing regimen.
We recently developed and validated a population PK model to predict IgG concentration metrics for SCIG and IVIG dosing [36]. Model-based simulations pharmacokinetically supported that a switch from weekly SCIG to biweekly SCIG infusion at double the weekly dose maintained equivalent plasma IgG levels. The biweekly dosing regimen has recently been approved by both the US Food and Drug Administration and the European Medicines Agency for Hizentra® (20% SCIG; CSL Behring AG, Bern, Switzerland) based on this modeling and simulation [37, 38]. The aim of this investigation was to use the same model to make a broader range of predictions to address the flexibility of SCIG administration. First, the model was used to predict IgG kinetics following dosing regimens ranging from daily to monthly administrations, including the influence of skipped doses. Second, various loading regimens were simulated to measure the time to steady-state IgG concentrations in treatment-naïve patients commencing SCIG therapy.
Methods
This article does not contain any new studies with human or animal subjects performed by the authors.
Pharmacokinetic Model Development
A PK model was developed using IgG concentration data obtained from four Phase III trials (Clinicaltrials.gov: NCT00168025, NCT00419341, NCT00322556, NCT00542997) in patients with PID treated with either Privigen® (CSL Behring AG, Bern, Switzerland) IVIG and/or Hizentra® SCIG, as previously described [36]. In brief, a total of 3,837 IgG concentrations from 151 unique study patients were used to develop two reference models: RM1.5, assuming a baseline (endogenous) IgG concentration of 1.5 g/L (as expected in predominantly XLA patient populations) and RM4.0, assuming an endogenous IgG level of 4 g/L (representative for PID population with mostly patients with CVID). The PK model is a standard two-compartment model, with SCIG absorption modeled as a first-order process (Fig. 1). Evaluation of the reference models was performed using sensitivity analyses, visual predictive checks, and external validation [36].
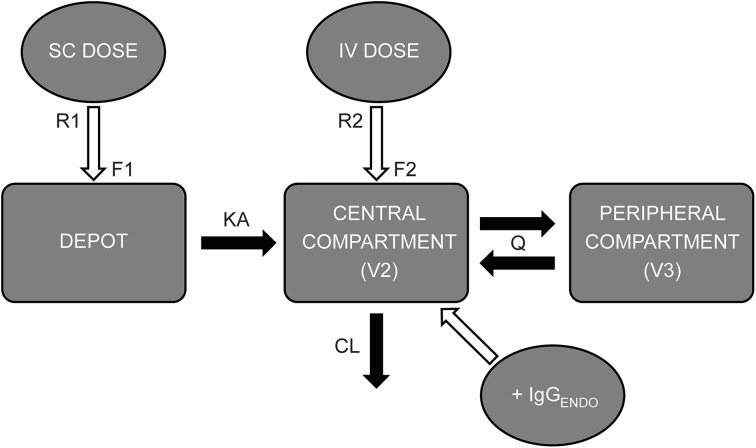
Fig. 1.
Schematic diagram of the two-compartment population PK model. CL clearance (L/day), F1 bioavailability of subcutaneous (SC) immunoglobulin, F2 bioavailability of intravenous (IV) immunoglobulin (=1.00), IgG ENDO endogenous serum IgG concentration (g/L), KA absorption rate constant of subcutaneous dose (day−1), Q inter-compartmental clearance (L/day), R1 rate of subcutaneous dose administration (g/day), R2 rate of intravenous administration (g/day), V2 volume of distribution of central compartment (L), V3 volume of distribution of peripheral compartment (L). Reprinted from Postgraduate Medicine, 125, Landersdorfer CB, Bexon M, Edelman J, et al. Pharmacokinetic modeling and simulation of biweekly subcutaneous immunoglobulin dosing in primary immunodeficiency, page 55, Copyright 2013, with permission from JTE Multimedia, LLC
Simulations
Reference population PK models, RM4.0 and RM1.5, were used to simulate several subcutaneous Hizentra® dosing regimens for evaluation of steady-state IgG concentration–time profiles and IgG exposure metrics. The same total dose (100 mg/kg/week in a 60-kg patient with PID) was applied when simulating different dosing frequency regimens.
Simulations were performed with NONMEM v7.2, using either S+ (SolutionMetrics, Sydney, NSW, Australia) or R for data management and graphic creation.
Variable Dose Frequency
A trial consisting of 2,500 patients was simulated to compare steady-state IgG concentration–time profiles between a weekly SCIG administration regimen, with more frequent (daily, five times a week, three times a week, and twice a week) and less frequent (biweekly, every 3 weeks, and every 4 weeks) dosing regimens. Simulations for more frequent dosing assumed daily dosing Monday–Sunday; five times per week (e.g., dosing daily Monday–Friday); three times a week (e.g., dosing on Monday, Wednesday, and Friday); and twice a week infusions (e.g., on Monday and Thursday).
In addition, 300 trials, each with 25 patients, were simulated to derive steady-state IgG PK parameters [area under the curve (AUC), maximum concentration (C max) and minimum concentration (C min)] for each regimen. For each exposure metric, the mean of individual ratios of weekly SCIG versus an alternative regimen was calculated for each simulated trial. The median, 5th, and 95th percentiles of the within-trial means were subsequently derived.
Impact of Skipped Doses
Steady-state IgG concentration profiles were simulated (1 trial consisting of 2,500 patients, using reference model RM4.0), in which doses were skipped during daily, weekly and biweekly dosing regimens. For a daily dosing regimen, two or three consecutive skipped doses were simulated, with or without dose replacement. For simulations in which skipped doses were included when dosing was resumed, the following dose would be three times the daily dose following two consecutive skipped doses, or four times the daily dose following three consecutive skipped doses. A weekly dosing regimen was simulated in which one, two, or three consecutive doses were skipped and replaced when dosing was resumed. For biweekly dosing, a single skipped dose was simulated. For both weekly and biweekly dosing regimens additional simulations were performed to predict the effect of a double dose followed by a single skipped dose, without dose replacement of the skipped dose.
To assess poor compliance, the effect of a daily dosing regimen, in which one or two doses were skipped without replacement every week for an extended period of time, was simulated.
Loading Dose Regimens
A study consisting of 2,500 patients was simulated to measure and compare IgG concentration–time profiles for different SCIG loading dose strategies in IgG treatment-naïve patients. Six SCIG loading dose regimens were explored, as summarized in Table 1, with 100 mg/kg/week considered as a reference dose. Following the specified loading dose, simulations proceeded with a weekly maintenance regimen.
Table 1.
Simulated loading SCIG regimens for treatment-naïve subjects
| Regimena | Day (Week 1) | Day (Week 2) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
| 100 mg/kg 5 times a week 1WK | 100 | 100 | 100 | 100 | 100 | |||||||||
| 150 mg/kg 5 times a week 1WK | 150 | 150 | 150 | 150 | 150 | |||||||||
| 100 mg/kg 2 times a week 2WK | 100 | 100 | 100 | 100 | ||||||||||
| 150 mg/kg 2 times a week 2WK | 150 | 150 | 150 | 150 | ||||||||||
| 100 mg/kg 3 times a week 2WK | 100 | 100 | 100 | 100 | 100 | 100 | ||||||||
| 100 mg/kg 5 times a week 2WK | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | ||||
SCIG subcutaneous immunoglobulin
aAll loading dose regimens maintained with 100 mg/kg weekly SCIG from day 15 onwards
Results
Predicted Pharmacokinetic Outcomes of Varied SCIG Dosing Regimens
A broad range of SCIG dosing regimens was simulated to predict steady-state serum IgG exposures relative to a weekly SCIG regimen. While the frequency of dose administration was varied, the cumulative simulated dose remained constant (100 mg/kg/week).
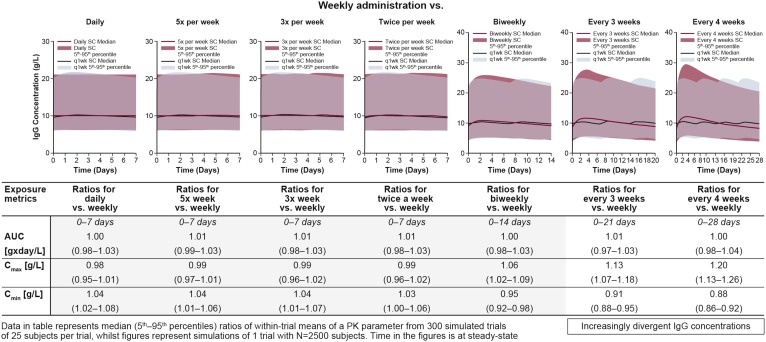
Using the RM4.0 model, simulations showed that higher dosing frequency regimens provided similar IgG concentration profiles to weekly dosing, with minimal differences in either median steady-state IgG concentration or the concentration distribution (Fig. 2). This was reflected in the exposure metric data, where median AUC0–7 days ratios for treatment intervals more frequent than weekly were within 3% of those for weekly administration, and C max ratios within 5%. The minimum IgG exposure was consistently greater for the more frequent dosing regimens, but not by more than 8%. This indicates that SCIG dosing regimens administered more frequently than once a week, in which the same total weekly dose is administered, would provide equivalent steady-state IgG exposures.
Fig. 2.
Steady-state IgG concentration–time profiles for various simulated subcutaneous immunoglobulin dosing regimens, using the RM4.0 reference model. Median IgG concentrations (black line) with 5th and 95th percentile (blue shaded area) for weekly dosing, compared with median concentrations (red line) and 5th to 95th percentiles (red shaded area) of IgG concentration for alternative dosing regimens. C min and C max values are also displayed in tabulated form. AUC area under the concentration–time curve, IgG immunoglobulin G, C min minimum concentration, C max maximum concentration, PK pharmacokinetic, SC subcutaneous
With regard to regimens less frequent than weekly dosing, predicted IgG concentration profiles were similar to those for weekly and biweekly dosing, but deviations were more apparent when dosing was every 3 or 4 weeks (Fig. 2). The average IgG exposure was consistent with frequent dosing regimens, in which median AUC ratios were within 4% of that for the weekly dose regimen, though C max and C min were notably more divergent. While median C min ratios for biweekly dosing were within 8% of weekly dosing, dosing every 3 or every 4 weeks was predicted to result in minimum exposure up to 12 and 14% lower than weekly dosing, respectively. By contrast, maximum IgG concentration when dosing every 4 weeks was up to 26% higher than experienced when dosing weekly.
This indicates that, while weekly and biweekly dosings provide comparable IgG exposure, IgG concentrations following dosing every 3 or 4 weeks may drop to less than 90% of steady-state levels toward the end of the dosing interval. Simulations performed with the RM1.5 model gave similar results (not shown).
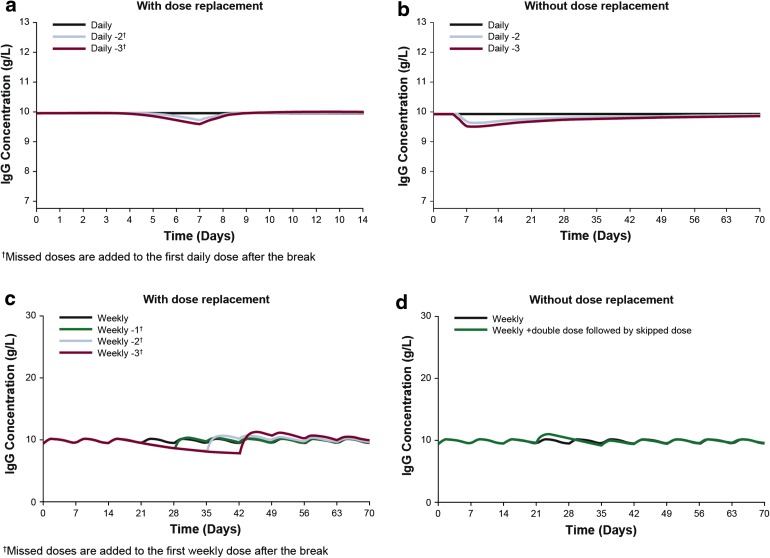
On a daily dosing regimen, skipped or missed doses can be replaced with minimal impact on plasma IgG levels: simulated steady-state concentration profiles showed that the influence of up to three consecutive skipped doses resulted in only a 4% reduction in average concentrations relative to consistent daily dosing (Fig. 3a, b). Exposure recovered within 2 to 3 days when administration was resumed and the next doses increased to administer the same total weekly dose (Fig. 3a). When the skipped doses were not replaced, there was a small, but long-lasting decrease in steady-state IgG levels (Fig. 3b). If doses were repeatedly missed and not replaced, the deficit accumulated. For example, if a patient on a daily dosing schedule regularly missed one or two doses per week over a period of several months, a new steady-state IgG level was reached; the average was 9 or 18% below the original target level, respectively.
Fig. 3.
Simulations for skipped doses during daily and weekly subcutaneous immunoglobulin. Median steady-state IgG concentrations simulating a daily dosing regimen (black line) in which either two (blue line) or three (red line) consecutive doses are skipped, and where there is (a) compensation or (b) no compensation for skipped doses upon resumption of daily dosing. c Median steady-state IgG concentrations for a weekly dosing regimen (black line) in which either one (green line), two (blue line), or three (red line) doses are skipped from day 21 and compensated for upon resuming therapy, or (d) a double dose administered on day 21 and a dose skipped on day 28, without compensation. IgG immunoglobulin G
On a simulated weekly dosing regimen, one, two or three skipped doses led to a decrease in average trough levels by 9, 15, and 19%, respectively. This recovered rapidly upon replacement of the skipped dose at the next infusion (Fig. 3c). A skipped dose on a biweekly schedule led to an average decrease in trough level by 13%, which also recovered rapidly after replacement. In anticipation of a skipped dose, a double dose can be administered during a weekly or biweekly regimen. The average peak concentration after the double dose was increased by 8% on weekly, and 16% on biweekly dosing, compared with the peak concentration achieved with a standard dose. However, the impact on subsequent trough levels was small (average 3% decrease on weekly and 5% on biweekly regimens) (Fig. 3d).
Loading Regimens for Initiating SCIG Therapy
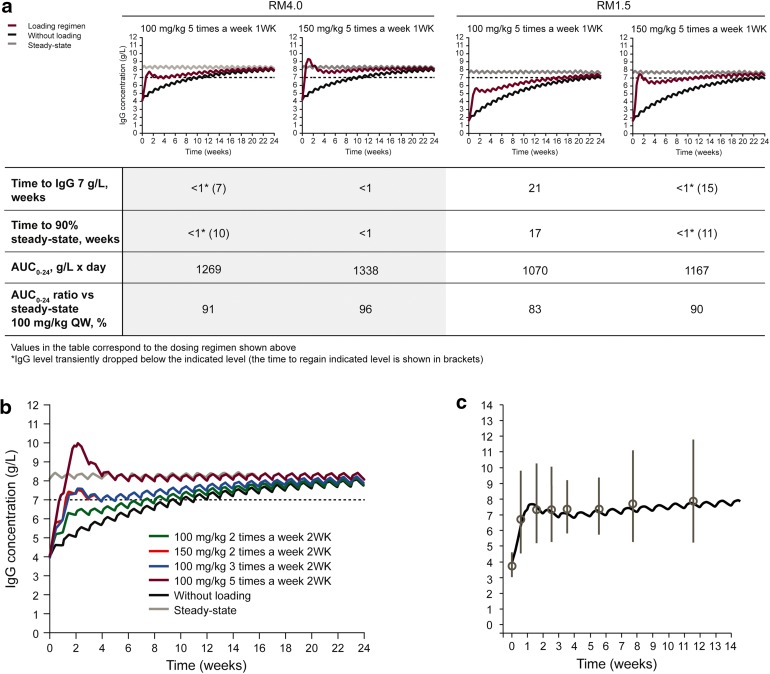
When SCIG therapy initiation was simulated in IgG treatment-naïve patients in the absence of a loading phase, the predicted time to achieve IgG levels of 7 g/L was 13 weeks when endogenous IgG was 4 g/L, and in excess of 24 weeks, when endogenous IgG was 1.5 g/L (Fig. 4a, b). The respective times to achieve 90% of steady-state IgG levels were 15 weeks and 22 weeks.
Fig. 4.
Simulated IgG concentration–time profiles for various subcutaneous immunoglobulin (SCIG) loading regimens. Steady-state (gray line) and SCIG without a loading phase (black line) are shown as comparators for different loading dose regimen. a 1-week loading phase using models RM4.0 and RM1.5 and (b) 2-week loading phase using model RM4.0. c Loading regimen of 5 × 100 mg/kg WK1 using model RM4.0 (black line) overlaid on observed clinical data (gray circles mean IgG concentration; gray lines standard error of the mean) reported by Borte et al. [39]. AUC area under the concentration–time curve, IgG immunoglobulin G, QW once a week
In simulations with endogenous IgG level of 4 g/L, the time to 7 g/L and 90% steady state was reduced to less than 1 week when the weekly SCIG maintenance dose of 100 mg/kg was administered five times during the first week of treatment (100 mg/kg 5 times a week 1WK), or a dose of 150 mg/kg was administered five times during the first week of treatment (150 mg/kg 5 times a week 1WK), before adopting weekly maintenance dosing (Fig. 4a). With the 100 mg/kg 5 times a week 1WK loading phase, there was a transient drop of IgG below 7 g/L when switching to the maintenance dose. However, this drop was relatively minor and sustained levels over 7 g/L were achieved by Week 7.
In simulations with endogenous IgG level of 1.5 g/L, the 150 mg/kg 5 times a week 1WK loading phase provided IgG levels above 7 g/L and 90% steady-state concentrations within 1 week, with a small transient drop in IgG levels when switching to weekly maintenance dose. By comparison, the 100 mg/kg 5 times a week 1WK regimen did not achieve IgG levels above 7 g/L until week 21.
An intensive loading regimen of 100 mg/kg administered five times a week during the first 2 weeks of treatment (100 mg/kg 5 times a week 2WK) was predicted to rapidly achieve and maintain IgG levels above 7 g/L (Fig. 4b). Less intensive 2-week loading regimens of either 100 mg/kg administered three times per week during the first 2 weeks of treatment (100 mg/kg 3 times a week 2WK) or 150 mg/kg administered two times per week during the first 2 weeks of treatment (150 mg/kg 2 times a week 2WK) were able to achieve IgG levels above 7 g/L in 2 weeks in simulations with an endogenous IgG level of 4.0 g/L (Fig. 4b). A small transient drop in IgG level, when switching to the maintenance dose, was recovered by Week 6.
As developed models were applied to a new patient population (i.e., treatment-naïve subjects) in this simulation study, it was important to compare simulated data with previously published data in such patients. For this reason, we overlaid the clinical IgG concentrations following loading of five consecutive SCIG daily doses of 100 mg/kg Vivaglobin® (CSL Behring GmbH, Marburg, Germany) in previously untreated patients obtained by Borte et al. [39], with our equivalent simulated data (Fig. 4c). The overlay suggests that the two sets of data are comparable, both with respect to the initial loading phase in the first week and the subsequent maintenance phase.
Discussion
Infused IgG has an elimination half-life of approximately 36 days [40]. Therefore, any dosing regimen with a frequency greater than monthly administration appears feasible from a PK point of view. While the recommended dosing for SCIG is weekly or biweekly administration, more frequent dosing regimens (up to daily) have been adopted by some patients [27, 28]. To assess the IgG kinetics for dosing regimens of higher and lower frequency than weekly dosing, we used a previously validated PK model to simulate events [36]. PK model-based simulations indicated that so long as the total dose of IgG remained constant, there is little difference in IgG exposure metrics when dosing as frequently as daily and up to biweekly. These data support the effectiveness of the varied dosing regimens already used by some patients.
The clinical advantage of frequent dosing is that serum IgG concentrations are more stable, resulting in somewhat higher IgG trough concentrations and reduced peak-to-trough variation. Due to the lack of low IgG trough levels in the days before the next infusion, patients receiving weekly SCIG therapy do not report the wear-off effects experienced by those receiving IVIG toward the end of the 3- or 4-week interval. Simulations presented here showed that SCIG dosing intervals could be extended to biweekly with minimal influence upon serum IgG concentration, whereas 3-weekly and 4-weekly dosing resulted in divergent C max and C min values. For this reason, and in terms of maintaining relative equivalency to weekly dosing, we recommend dosing regimens from daily to biweekly (in which the same weekly total dose is administered), but would not recommend dosing intervals from 3-weekly and beyond. Although this reasoning is somewhat subjective, a further consideration concerning the extension of the dosing interval is that greater subcutaneous injection volumes are required, which can become uncomfortable. However, given the variability of IgG half-life among individuals, a 3-weekly or 4-weekly regimen maybe suitable for some patients requiring a rather low dose. Flexibility in the dosing regimen from daily to biweekly enables patients to choose a regimen based on convenience or lifestyle. Possibly this can also improve compliance.
Clear benefits exist for patients offered individualized dosing regimens, tailored to their convenience. Conventional SCIG administration is by infusion pump. However, push administration, using a syringe and butterfly needle, offers a simple alternative at a lower cost (no requirement for a pump). This technique is more suited to frequent administration of lower dose volumes. Retrospective analyses have shown that push administration is preferred by patients as an easier and more convenient approach [26, 27]. In these studies, patients chose to dose on average every 2–3 days regardless of administration procedure, showing that even when patients were administering IgG by pump, they had a preference for a frequent dosing schedule. Some patients administering by pump also reported feeling better when infusing smaller volumes more frequently, although, this may be anecdotal [27].
There is also some flexibility within the dosing regimens as demonstrated by the small impact of 2–3 skipped doses on IgG levels during daily dosing, so long as the doses skipped are compensated for. These data show that if for whatever reason patients are unable to adhere strictly to their dosing regimen, it is simple and practical to compensate. For patients on a weekly or biweekly dosing regimen, trough IgG levels also recovered rapidly upon replacement of skipped doses. However, there is a greater impact on IgG trough levels when doses are skipped on these less frequent regimens, with a risk of IgG levels dropping below a protective level. It would, therefore, not be recommended to skip more than a single dose on a weekly regimen. In addition, the extra volume required to replace these doses during the following infusion could be an issue. By contrast, a double dose before a planned skipped dose had a minimal impact on the trough IgG levels for both weekly and biweekly dosing regimens. Therefore, this would be a feasible option for patients for whom on certain occasions it may be inconvenient to maintain their usual dosing pattern. For example, patients who are traveling or on vacation may take advantage of this option.
If skipped doses are not compensated when the regular daily dosing is resumed, it takes up to 5–6 weeks to return to steady-state levels. For patients with low IgG levels, or who require higher IgG levels for protection against infection, skipped doses should be compensated for as soon as possible. However, this practice should be advised for all patients. If doses are repeatedly skipped and not replaced, the deficit will accumulate. Within a few months of consistently missing one or two doses per week on a daily regimen, predicted IgG trough concentrations dropped to levels which may be under-protective. Compliance with the treatment regimen is, therefore, essential.
The data generated to determine the flexibility within dosing regimens were consistent between the two reference models, RM4.0 and RM1.5, for all simulated dosing regimens. These models represent endogenous IgG concentrations of 4 and 1.5 g/L and are reflective of the average endogenous IgG concentrations for predominantly CVID and XLA patient populations, respectively, thereby indicating that the flexibility within the dosing regimens is applicable to both patient populations.
An initial IVIG loading period before SCIG is not always practical and can be more problematic in children and the elderly, where venous accessibility may be an issue. In addition, treatment-naïve patients are more likely to experience adverse events to IVIG during the first and second infusions [41]. However, in treatment-naïve patients, SCIG therapy started at a constant weekly dose may take up to 6 months to achieve steady-state IgG levels [42]. Obviously, achieving adequate IgG concentrations as quickly as feasible is desirable for clinical efficacy. Borte et al. [39] have described a loading regimen, in which the weekly dose of 100 mg/kg was delivered five times during the first week, before adjusting the patient to a weekly dosing regimen. Nearly, all patients achieved IgG concentrations ≥5 g/L by day 12. An additional advantage of this loading regimen is that the loading phase can be used for training the patient in self-administration, the five loading doses being administered under the supervision of a nurse.
IgG concentration above 7 g/L (representing the lower limit of IgG in healthy adults [43, 44]) is considered to provide adequate protection from infection, and was recommended by a Canadian consensus guideline as the minimum IgG trough level to achieve in most patients [45, 46], although it is recognized that some patients may need a higher IgG level [47]. Our simulation data predicted that, in the absence of a loading dose, IgG concentrations of 7 g/L for SCIG dosing would only be attained after a period of 13 weeks if endogenous IgG was 4 g/L, or after more than 24 weeks if endogenous IgG was as low as 1.5 g/L. Three loading regimens were identified, which ensured that IgG concentrations were rapidly raised to protective quasi-steady-state levels. The first of these regimens was the delivery of the weekly dose of 100 mg/kg for 5 consecutive days during the first week of treatment, as also described by Borte et al. [39]. RM4.0 model simulations were highly comparable to these clinical data, and predicted that this would raise IgG concentrations above 7 g/L within 1 week of treatment initiation and thus provide rapid protection against infection for newly diagnosed patients. However, in the RM1.5 model, these levels were reached only after 21 weeks. This loading regimen may, therefore, be suitable for patients with higher endogenous (pre-therapy) IgG levels, such as patients with CVID, but not in patients with more severe disease or lower endogenous IgG, such as XLA. In such patients, a loading regimen of 150 mg/kg IgG administered five times during the first week of treatment, or 100 mg/kg administered five times during each of the first 2 weeks of treatment achieved IgG levels above 7 g/L within 2 weeks. These loading regimens would obviously also work for endogenous IgG levels of 4 g/L.
In addition, less intensive loading schedules of either 100 mg/kg three times a week or 150 mg/kg two times a week, administered over a 2-week period were able to raise IgG levels above 7 g/L within 2 weeks, when endogenous IgG was 4.0 g/L. These loading regimens might serve as alternatives for patients and physicians who prefer to use a less condensed dosing schedule. When determining clinical recommendations for loading dose regimens, non-PK factors related to clinical feasibility should be considered. This includes reaching IgG levels that would adequately protect the majority of the patient population, while considering patients’ convenience with respect to the required frequency of infusions, infusion volume, number of injection sites, and potential dose compliance. With this in mind, the loading dose of five consecutive infusions of 100 mg/kg during the first week, followed by the regular weekly dose of 100 mg/kg might be the most appropriate for the majority of patients.
For patients with low endogenous IgG level, a loading dose of one and a half times the weekly dose of 100 mg/kg administered five times during the first week of treatment may be considered more appropriate. Similar IgG concentration levels obtained by this more intense loading strategy may also be achieved by loading 100 mg/kg for five consecutive infusions during each of the first 2 weeks of SCIG therapy. However, this approach does not appear to offer any clinically important advantage, may place a higher burden upon patients, and is a more costly alternative. Less intense loading schedules of 150 mg/kg two times per week or 100 mg/kg three times per week for two consecutive weeks may still be appropriate for some patients with non-severe initial condition, relatively high endogenous IgG levels, or those who would like to avoid daily infusions for five consecutive days.
For the above reasons, depending upon the baseline IgG level, an SCIG loading regimen of 100 or 150 mg/kg for five consecutive days in the first week of treatment is predicted to quickly elevate the patient’s serum IgG levels to protective quasi-steady-state levels without the need for an initial IVIG loading dose. After the loading period, the SCIG dose can be adjusted on an individual basis dependent upon IgG levels and clinical response.
All simulations presented here were performed with respect to achieving levels around 7 g/L. While this level is probably protective in many patients, it is a somewhat hypothetical value. In practice it is important to identify the individual’s protective ‘biologic IgG level’, above which the patient remains essentially infection free, with the aim of achieving and maintaining this IgG concentration [47]. Dose levels have to be adapted accordingly. For a CVID patient population, we assumed an endogenous IgG concentration of 4 g/L; we did not take into account the functional status of this IgG, which can be compromised [7]. These patients may require a higher ‘biologic IgG level’. In addition, the efficacy of Ig therapy, i.e., the dose required to achieve a given increase in IgG trough levels, varies from patient to patient, making further dose adjustment necessary [48].
If, in a treatment-naïve patient, it can be anticipated that the target IgG trough level is higher than 7 g/L and, as a consequence, the maintenance dose is higher than 100 mg/kg/week, a loading regimen of the planned maintenance dose administered on five consecutive days is appropriate to bring the serum IgG concentration to the target ‘biologic IgG level’ within one week. If, in addition, this patient has a low endogenous IgG, one and a half times the planned maintenance dose administered 5 days in Week 1 may be required.
In considering the dosing regimens assessed in our work, particularly that for loading doses, a limitation to the modeling needs to be noted. The PK model on which the presented simulations were based was derived using data obtained in clinical trial subjects, all of whom had received IgG therapies prior to their study participation. As there was no PK data from IgG treatment-naïve subjects, methodological assumptions had to be made about the status of endogenous IgG levels. We chose to fix endogenous IgG in the model to a value within a range of 1.5–4.0 g/L. Consequently, confirmation of our assessments of various SCIG loading dose possibilities is warranted. However, the endogenous IgG level limitation is of much lesser importance for our assessments of various SCIG maintenance regimens, whereby a fixed endogenous level was held constant between comparative dosing regimens.
Conclusion
PK modeling predicts that similar IgG concentrations are achieved with a dosing frequency of every 2 weeks or less, so long as the cumulative total dose remains consistent. IgG levels of 7 g/L are achievable in treatment-naïve patients with several SCIG loading regimens during the first 1–2 weeks of SCIG treatment and would provide greater convenience for patients with PID.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
The authors thank Dr. Alphonse Hubsch for critical review of the manuscript. The study and article processing charges were funded by CSL Behring. Editorial assistance in the preparation of this manuscript was provided by Dr. Stuart Avery of Fishawack Communications GmbH, a member of the Fishawack Group of Companies. Support for this assistance was funded by CSL Behring. All named authors meet the ICMJE criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Conflict of interest
J. Sidhu is an employee of CSL Ltd. M. Rojavin is an employee of CSL Behring LLC. M. Pfister received consulting fees from CSL Behring. J. Edelman is an employee of CSL Behring.
Compliance with ethics guidelines
This article does not contain any new studies with human or animal subjects performed by the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
References
- 1.Buckley RH. Primary immunodeficiency diseases due to defects in lymphocytes. N Engl J Med. 2000;343(18):1313–1324. doi: 10.1056/NEJM200011023431806. [DOI] [PubMed] [Google Scholar]
- 2.Chapel H, Geha R, Rosen F. Primary immunodeficiency diseases: an update. Clin Exp Immunol. 2003;132(1):9–15. doi: 10.1046/j.1365-2249.2003.02110.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cunningham-Rundles C, Bodian C. Common variable immunodeficiency: clinical and immunological features of 248 patients. Clin Immunol. 1999;92(1):34–48. doi: 10.1006/clim.1999.4725. [DOI] [PubMed] [Google Scholar]
- 4.Lougaris V, Ferrari S, Plebani A. Ig beta deficiency in humans. Curr Opin Allergy Clin Immunol. 2008;8(6):515–519. doi: 10.1097/ACI.0b013e328314b621. [DOI] [PubMed] [Google Scholar]
- 5.Notarangelo LD, Fischer A, Geha RS, et al. Primary immunodeficiencies: 2009 update. J Allergy Clin Immunol. 2009;124(6):1161–1178. doi: 10.1016/j.jaci.2009.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ochs HD, Smith CIE, Puck JM. Primary immunodeficiency diseases: a molecular and genetic approach. New York: Oxford University Press; 1999. [Google Scholar]
- 7.Park MA, Li JT, Hagan JB, Maddox DE, Abraham RS. Common variable immunodeficiency: a new look at an old disease. Lancet. 2008;372(9637):489–502. doi: 10.1016/S0140-6736(08)61199-X. [DOI] [PubMed] [Google Scholar]
- 8.Berger M. Principles of and advances in immunoglobulin replacement therapy for primary immunodeficiency. Immunol Allergy Clin North Am. 2008;28(2):413–437. doi: 10.1016/j.iac.2008.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berger M. Subcutaneous administration of IgG. Immunol Allergy Clin North Am. 2008;28(4):779–802. doi: 10.1016/j.iac.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Busse PJ, Razvi S, Cunningham-Rundles C. Efficacy of intravenous immunoglobulin in the prevention of pneumonia in patients with common variable immunodeficiency. J Allergy Clin Immunol. 2002;109(6):1001–1004. doi: 10.1067/mai.2002.124999. [DOI] [PubMed] [Google Scholar]
- 11.Bussel JB, Eldor A, Kelton JG, et al. IGIV-C, a novel intravenous immunoglobulin: evaluation of safety, efficacy, mechanisms of action, and impact on quality of life. Thromb Haemost. 2004;91(4):771–778. doi: 10.1160/TH03-10-0650. [DOI] [PubMed] [Google Scholar]
- 12.Church JA, Borte M, Taki H, et al. Efficacy and safety of Privigen in children and adolescents with primary immunodeficiency. Pediatr Asthma Allergy Immunol. 2009;22(2):53–62. doi: 10.1089/pai.2009.0005. [DOI] [Google Scholar]
- 13.de Gracia J, Vendrell M, Alvarez A, et al. Immunoglobulin therapy to control lung damage in patients with common variable immunodeficiency. Int Immunopharmacol. 2004;4(6):745–753. doi: 10.1016/j.intimp.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 14.Eijkhout HW, van der Meer JW, Kallenberg CG, et al. The effect of two different dosages of intravenous immunoglobulin on the incidence of recurrent infections in patients with primary hypogammaglobulinemia. A randomized, double-blind, multicenter crossover trial. Ann Intern Med. 2001;135(3):165–174. doi: 10.7326/0003-4819-135-3-200108070-00008. [DOI] [PubMed] [Google Scholar]
- 15.Gardulf A, Hammarstrom L, Smith CI. Home treatment of hypogammaglobulinaemia with subcutaneous gammaglobulin by rapid infusion. Lancet. 1991;338(8760):162–166. doi: 10.1016/0140-6736(91)90147-H. [DOI] [PubMed] [Google Scholar]
- 16.Gardulf A, Nicolay U. Replacement IgG therapy and self-therapy at home improve the health-related quality of life in patients with primary antibody deficiencies. Curr Opin Allergy Clin Immunol. 2006;6(6):434–442. doi: 10.1097/01.all.0000246619.49494.41. [DOI] [PubMed] [Google Scholar]
- 17.Maeder W, Lieby P, Sebald A, Spycher M, Pedrussio R, Bolli R. Local tolerance and stability up to 24 months of a new 20% proline-stabilized polyclonal immunoglobulin for subcutaneous administration. Biologicals. 2011;39(1):43–49. doi: 10.1016/j.biologicals.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 18.Ochs HD, Gupta S, Kiessling P, Nicolay U, Berger M. Safety and efficacy of self-administered subcutaneous immunoglobulin in patients with primary immunodeficiency diseases. J Clin Immunol. 2006;26(3):265–273. doi: 10.1007/s10875-006-9021-7. [DOI] [PubMed] [Google Scholar]
- 19.Quartier P, Debre M, De Blic J, et al. Early and prolonged intravenous immunoglobulin replacement therapy in childhood agammaglobulinemia: a retrospective survey of 31 patients. J Pediatr. 1999;134(5):589–596. doi: 10.1016/S0022-3476(99)70246-5. [DOI] [PubMed] [Google Scholar]
- 20.Stein MR, Nelson RP, Church JA, et al. Safety and efficacy of Privigen©, a novel 10% liquid immunoglobulin preparation for intravenous use, in patients with primary immunodeficiencies. J Clin Immunol. 2009;29(1):137–144. doi: 10.1007/s10875-008-9231-2. [DOI] [PubMed] [Google Scholar]
- 21.Borte M, Pac M, Serban M, et al. Efficacy and safety of hizentra®, a new 20% immunoglobulin preparation for subcutaneous administration, in pediatric patients with primary immunodeficiency. J Clin Immunol. 2011;31(5):752–761. doi: 10.1007/s10875-011-9557-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berger M. Clinical focus on primary immune deficiencies: subcutaneous IgG replacement therapy in immune deficiency diseases. Immune Deficiency Foundation, Towson [online]; 2008 [updated 2012/07/04/]; 13:[1–12].
- 23.Gardulf A, Nicolay U, Asensio O, et al. Rapid subcutaneous IgG replacement therapy is effective and safe in children and adults with primary immunodeficiencies–a prospective, multi-national study. J Clin Immunol. 2006;26(2):177–185. doi: 10.1007/s10875-006-9002-x. [DOI] [PubMed] [Google Scholar]
- 24.Wasserman RL, Melamed I, Nelson RP, et al. Pharmacokinetics of subcutaneous IgPro20 in patients with primary immunodeficiency. Clin Pharmacokinet. 2011;50(6):405–414. doi: 10.2165/11587030-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 25.Gardulf A, Andersen V, Bjorkander J, et al. Subcutaneous immunoglobulin replacement in patients with primary antibody deficiencies: safety and costs. Lancet. 1995;345(8946):365–369. doi: 10.1016/S0140-6736(95)90346-1. [DOI] [PubMed] [Google Scholar]
- 26.Nicolay U, Kiessling P, Berger M, et al. Health-related quality of life and treatment satisfaction in North American patients with primary immunedeficiency diseases receiving subcutaneous IgG self-infusions at home. J Clin Immunol. 2006;26(1):65–72. doi: 10.1007/s10875-006-8905-x. [DOI] [PubMed] [Google Scholar]
- 27.Shapiro R. Subcutaneous immunoglobulin therapy by rapid push is preferred to infusion by pump: a retrospective analysis. J Clin Immunol. 2010;30(2):301–307. doi: 10.1007/s10875-009-9352-2. [DOI] [PubMed] [Google Scholar]
- 28.Shapiro RS. Subcutaneous immunoglobulin therapy given by subcutaneous rapid push vs infusion pump: a retrospective analysis. Ann Allergy Asthma Immunol. 2013;111(1):51–55. doi: 10.1016/j.anai.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 29.Gustafson R, Gardulf A, Hansen S, et al. Rapid subcutaneous immunoglobulin administration every second week results in high and stable serum immunoglobulin G levels in patients with primary antibody deficiencies. Clin Exp Immunol. 2008;152(2):274–279. doi: 10.1111/j.1365-2249.2008.03620.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Girgis IG, Nandy P, Nye JS, et al. Pharmacokinetic-pharmacodynamic assessment of topiramate dosing regimens for children with epilepsy 2 to <10 years of age. Epilepsia. 2010;51(10):1954–1962. doi: 10.1111/j.1528-1167.2010.02598.x. [DOI] [PubMed] [Google Scholar]
- 31.Hariharan S, Madabushi R. Clinical pharmacology basis of deriving dosing recommendations for dabigatran in patients with severe renal impairment. J Clin Pharmacol. 2012;52(1 Suppl):119S–125S. doi: 10.1177/0091270011415527. [DOI] [PubMed] [Google Scholar]
- 32.Madabushi R, Cox DS, Hossain M, et al. Pharmacokinetic and pharmacodynamic basis for effective argatroban dosing in pediatrics. J Clin Pharmacol. 2011;51(1):19–28. doi: 10.1177/0091270010365550. [DOI] [PubMed] [Google Scholar]
- 33.Tornoe CW, Tworzyanski JJ, Imoisili MA, Alexander JJ, Korth-Bradley JM, Gobburu JV. Optimising piperacillin/tazobactam dosing in paediatrics. Int J Antimicrob Agents. 2007;30(4):320–324. doi: 10.1016/j.ijantimicag.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 34.Yim DS, Zhou H, Buckwalter M, Nestorov I, Peck CC, Lee H. Population pharmacokinetic analysis and simulation of the time-concentration profile of etanercept in pediatric patients with juvenile rheumatoid arthritis. J Clin Pharmacol. 2005;45(3):246–256. doi: 10.1177/0091270004271945. [DOI] [PubMed] [Google Scholar]
- 35.Zhang L, Boulton DW, Pfister M. A pharmacometric approach to quantify the impact of chronic kidney disease and hemodialysis on systemic drug exposure: application to saxagliptin. J Clin Pharmacol. 2012;52(1 Suppl):126S–133S. doi: 10.1177/0091270011415627. [DOI] [PubMed] [Google Scholar]
- 36.Landersdorfer CB, Bexon M, Edelman J, et al. Pharmacokinetic modeling and simulation of biweekly subcutaneous immunoglobulin dosing in primary immunodeficiency. Postgrad Med. 2013;125(6):53–61. doi: 10.3810/pgm.2013.11.2712. [DOI] [PubMed] [Google Scholar]
- 37.FDA. FDA Hizentra® US Package Insert. http://www.fda.gov/downloads/BiologicsBloodVaccines/BloodBloodProducts/ApprovedProducts/LicensedProductsBLAs/FractionatedPlasmaProducts/UCM203150.pdf. Accessed 05 Aug 2014.
- 38.EMA. European Medicines Agency: Hizentra® Product Information (EU SPC). http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002127/WC500107057.pdf. Accessed 05 Aug 2014.
- 39.Borte M, Quinti I, Soresina A, et al. Efficacy and safety of subcutaneous Vivaglobin® replacement therapy in previously untreated patients with primary immunodeficiency: a prospective, multicenter study. J Clin Immunol. 2011;31(6):952–961. doi: 10.1007/s10875-011-9588-5. [DOI] [PubMed] [Google Scholar]
- 40.Wasserman RL, Church JA, Peter HH, et al. Pharmacokinetics of a new 10% intravenous immunoglobulin in patients receiving replacement therapy for primary immunodeficiency. Eur J Pharm Sci. 2009;37(3–4):272–278. doi: 10.1016/j.ejps.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 41.Skoda-Smith S, Torgerson TR, Ochs HD. Subcutaneous immunoglobulin replacement therapy in the treatment of patients with primary immunodeficiency disease. Ther Clin Risk Manag. 2010;6:1–10. doi: 10.1057/rm.2009.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Waniewski J, Gardulf A, Hammarstrom L. Bioavailability of gamma-globulin after subcutaneous infusions in patients with common variable immunodeficiency. J Clin Immunol. 1994;14(2):90–97. doi: 10.1007/BF01541341. [DOI] [PubMed] [Google Scholar]
- 43.Gonzalez-Quintela A, Alende R, Gude F, et al. Serum levels of immunoglobulins (IgG, IgA, IgM) in a general adult population and their relationship with alcohol consumption, smoking and common metabolic abnormalities. Clin Exp Immunol. 2008;151(1):42–50. doi: 10.1111/j.1365-2249.2007.03545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rose ME, Lang DM. Evaluating and managing hypogammaglobulinemia. Cleve Clin J Med. 2006;73(2):133–137. doi: 10.3949/ccjm.73.2.133. [DOI] [PubMed] [Google Scholar]
- 45.Ballow M, Notarangelo L, Grimbacher B, et al. Immunodeficiencies. Clin Exp Immunol. 2009;158(Suppl 1):14–22. doi: 10.1111/j.1365-2249.2009.04023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shehata N, Palda V, Bowen T, et al. The use of immunoglobulin therapy for patients with primary immune deficiency: an evidence-based practice guideline. Transfus Med Rev. 2010;24(Suppl 1):S28–S50. doi: 10.1016/j.tmrv.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 47.Bonagura VR, Marchlewski R, Cox A, Rosenthal DW. Biologic IgG level in primary immunodeficiency disease: the IgG level that protects against recurrent infection. J Allergy Clin Immunol. 2008;122(1):210–212. doi: 10.1016/j.jaci.2008.04.044. [DOI] [PubMed] [Google Scholar]
- 48.Gouilleux-Gruart V, Chapel H, Chevret S, et al. Efficiency of immunoglobulin G replacement therapy in common variable immunodeficiency: correlations with clinical phenotype and polymorphism of the neonatal Fc receptor. Clin Exp Immunol. 2013;171(2):186–194. doi: 10.1111/cei.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.