Abstract
Objective
This study was designed to determine if a rising intraoperative parathyroid hormone (ioPTH) level following parathyroid resection indicates multiple hyperfunctioning glands and to determine the appropriate intraoperative management.
Summary Background Data
IoPTH monitoring is commonly utilized to guide parathyroid surgery. A significant rise in the ioPTH immediately after resection of a single parathyroid is often perceived to be indicative of the presence of additional hyperfunctioning glands.
Methods
797 consecutive patients underwent parathyroidectomy for primary hyperparathyroidism with ioPTH monitoring. Patients with an elevated 5 minute ioPTH were extensively studied. Operative success was defined as normocalcemia 6 months after surgery.
Results
Of the 797 patients, 108 (14%) had a rising ioPTH 5 minutes after resection of a single parathyroid. Of these 108 patients, 36 (33%) continued to have elevated ioPTH levels and further exploration revealed additional hyperfunctioning glands. Importantly, in the majority of patients (n = 72 or 67%), the ioPTH started to fall after an additional 5 minutes (10 minutes after resection). The ioPTH declined by more than 50% from the 5 minute elevated value in 30%, 89% and 99% of patients at 10, 15, and 20 minutes after resection, respectively. Importantly this fall correctly predicted operative success in 100% of patients after removal of a single abnormal gland.
Conclusions
A rising ioPTH level immediately after parathyroidectomy is observed in 14% of patients. The majority of these patients do not have additional hyperfunctioning glands. The vast majority of patients fell below 50% of the 5 minute elevated value within 20 minutes of gland resection and in all cases this fall correctly predicted operative success.
Introduction
Primary hyperparathyroidism (HPT) is the third most common endocrine disorder in the United States with an incidence of 28 per 100,000 people and approximately 100,000 new cases each year. Surgical treatment is the mainstay of therapy with high success rates when performed by an experienced surgeon. In recent years, minimally invasive parathyroidectomy with intraoperative parathyroid hormone (ioPTH) monitoring has gained favor 1-7. This emphasis on a minimally invasive procedures has reduced operative times and hospital stay length as well as hospital costs in properly selected patients 8.
A significant amount of work has focused on defining the appropriate interpretation of ioPTH values. Previous reports have shown that a 50% drop in the ioPTH level from a preincision baseline is highly predictive of surgical cure, defined as normocalcemia 6 months postoperatively 9, 10. Others have additionally shown that this 50% drop rule is superior to waiting for the ioPTH to reach a normal value11, 12.
However, a subset of patients exists in whom the 50% rule is more difficult to apply. These patients experience a 5 minute ioPTH measurement that is actually elevated from the preincision baseline. While multiple hypotheses have been advanced to explain this elevation, perhaps the most likely is surgical manipulation of the hyperfunctioning gland(s) 13, 14. In this situation, recommendations are that the surgeon should wait for the ioPTH to fall below 50% of the pre-incision baseline value13. On the other hand, checking additional levels prolongs operative time and perhaps leads to unnecessary bilateral neck exploration 13.
The aims of this study were to document the frequency of an elevated 5 minute ioPTH level and determine if this rising 5 minute ioPTH predicts the presence of multiple hyperfunctioning glands. Additionally, we sought to define criteria for the optimal surgical management of patients with a rising 5 minute ioPTH after resection of an initial single parathyroid gland.
Patients and Methods
This study was retrospectively performed on a prospectively maintained database collected between March 2001 and August 2008. In this time, 797 patients underwent surgical resection with ioPTH monitoring for primary HPT at the University of Wisconsin. Baseline PTH levels were drawn prior to skin incision and then at least 5, 10 and 15 minutes after excision of a suspicious parathyroid adenoma.
Our protocol for ioPTH testing has been previously described15. Briefly, blood was collected prior to incision (pre-incision) as well as 5, 10 and 15 minutes after resection of the parathyroid gland. We terminate the operation if the ioPTH falls>50% from the baseline at any of the time points (5, 10, or 15 minutes). If the level has not fallen below 50% of the preincision level by 15 minutes, we would then proceed with further exploration to identify and resect additional hyperfunctioning parathyroid gland.
However, if the 5 minute post-resection value was elevated above the pre-incision value, two additional ioPTH samples were drawn at successive 5 minute intervals (at approximately 20 and 25 mintues after resection of the initial parathyroid). Curative parathyroidectomy was defined as normocalcemia (serum calcium ≤ 10.2 mg/dl) 6 months after the operation, while persistent disease was defined as patients with an elevated calcium (greater than 10.2 mg/dl) within 6 months of follow-up.
For the purposes of this study, patients with single gland disease were defined as those who had a greater than 50% fall in their ioPTH after resection of a single gland and were normocalcemic at 6 months. Those with multi-gland disease were considered to be patients who did have at least a 50% fall in their ioPTH, and additional exploration revealed other enlarged parathyroid glands. In patients with multi-gland disease, resection of more than one gland was needed to observe a >50% drop in the ioPTH, and normocalcemia at 6 months. In addition, patients with an elevated 5 minute post-resection ioPTH were identified and extensively studied. Results are expressed as the mean ± SEM.
Statistical analysis was performed using Microsoft Excell (2003 for Microsoft Windows, Microsoft, Redmond WA) and Graphpad online calculator (Graphpad Software, Inc. La Jolla, CA). Throughout the statistical analysis, the significance level was set as P ≤ 0.05.
Results
When the 797 patients in this study were examined, 108 patients (14%) had a rising ioPTH 5 minutes after resection of a single gland when compared to their pre-incision baseline. The demographics and pre-operative laboratory characteristics of these patients are described in TABLE 1. No significant differences were noted between the total patient population and the patients with an elevated 5 minute ioPTH in terms of age, gender distribution, pre-operative calcium, or pre-operative PTH when compared with an unpaired t-test (P>0.5 for all).
TABLE 1.
Demographics and Laboratory Data
| Total | Elevated 5 min ioPTH | |
|---|---|---|
| N (%) | 797 | 108 (14%) |
| Mean age (range) | 61 (10-91) | 60 (17-90) |
| Female (%) | 599 (75.1%) | 83 (75.4%) |
| Preoperative calcium (mg/dL) | 11.2 ± 0.03 | 11.2 ± 0.09 |
| Prenperative PTH (pg/mL) | 130 ± 3 | 118 ± 8 |
Mean ± standard error of mean.
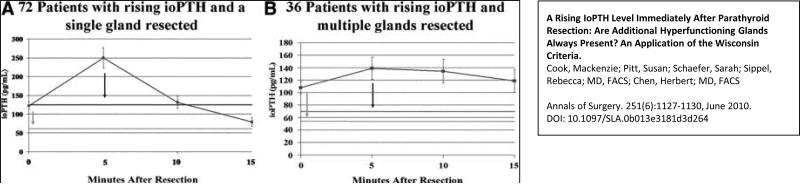
The ioPTH trend of these 108 patients with a rising 5 minute ioPTH was examined. In patients with a rising 5 minute ioPTH after resection, we routinely have used this higher ioPTH level as the new “baseline” level and a new threshold value for curative resection was defined as a >50% in ioPTH from this elevated 5 minute ioPTH. That is, we would definte an adequate drop in ioPTH as a >50% drop at 5, 10, or 15 minutes after this peak level (or 10, 15, or 20 minutes after resection of the initial gland). In this group of 108 patients, 72 (67%) fell below the newly defined baseline value within 20 minutes of the resection of the initial gland, (FIG. 1A), while 36 patients (33%) did not (FIG. 1B). Patients who fell below 50% of their elevated 5 minute ioPTH had their operation ended, while the 36 patients without a fall in their ioPTH at 20 minutes after resection were more extensively explored. In the 36 patients whose ioPTH failed to fall >50% within 20 minutes of resection (15 minutes after the peak 5 minute ioPTH level), additional exploration in 35 patients revealed other enlarged, hyperfunctioning parathyroid glands. After resection of these additional glands, the ioPTH level fell by >50% from the peak 5 minute ioPTH level with 15 minutes of the removal of the additional parathyroids. However, in 1 of the 36 patients, additional resection of 2.5 glands (a total of 3.5 glands removed) did not lead to a drop in ioPTH, but the operation was terminated due to failure to find the 5th abnormal gland. The patient was not cured, and later found to have a 5th mediastinal enlarged parathyroid which was successfully resected at a later date.
Figure 1.
The elevated 5 minute ioPTH value can be used as a new baseline to discriminate between patients with a single and multiple abnormal parathyroid glands. Patients with a single abnormal gland and a rising 5 minute ioPTH rapidly fall below 50% of this elevated value, though not 50% of the pre-incision value (A). In contrast, patients with multiple abnormal glands do not decline below 50% of the elevated 5 minute newly set ioPTH threshold (B). Data is plotted a mean ± SEM.
The mean peak ioPTH values of the 72 patients who had a subsequent fall in their ioPTH (249 ± 28 pg/ml) was significantly greater than the 36 patients who did not have a subsequent fall in their ioPTH (154 ± 5 pg/ml) (p <0.02). Though, when individual patients were examined, no clear division point either in fold increase or total increase was found between the two groups. There also were no significant differences in either the 6 month calcium or PTH values when the 72 patients who eventually fell and the 36 who required additional exploration were examined (P ≥ 0.05).
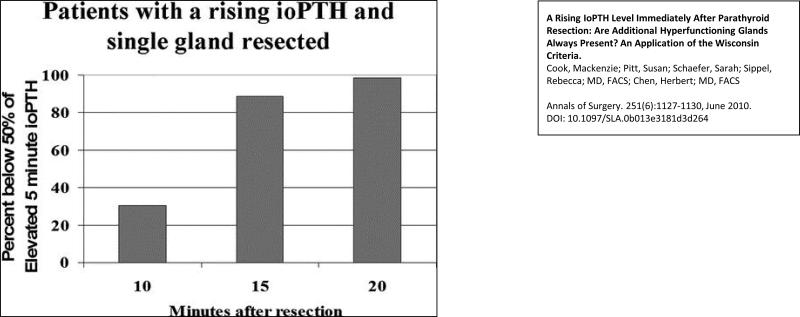
When the 72 patients with a rising 5 minute ioPTH that subsequently fell were studied more closely, we observed that 100% of patients fell below 50% of the elevated 5 minute value within 25 minutes of gland resection though 89% and 99% of patients fell below this new threshold within 15 and 20 minutes of gland resection, respectively (FIG 2).
Figure 2.
Patients with a single abnormal gland rapidly fall below a threshold defined as 50% of the elevated 5 minute ioPTH. If the elevated 5 minute ioPTH value is defined as the new baseline, a 50% decline from this point may be used to discriminate between single and multiple gland disease. Patients with only a single abnormal gland fall rapidly below this threshold.
The vast majority of the 108 patients with a rise in their 5 minute ioPTH level (n = 107, 99%) were normocalcemic at 6 months postoperatively. Importantly, of the patients who had a rising 5 minute ioPTH and a subsequent fall below our newly defined threshold, 72 (100%) were normocalcemic 6 months post-operatively. This is consistent with a 99% cure rate for the entire group of 797 patients. The outcomes for these patients are shown in TABLE 2. The patient who was not cured 6 months post-operatively was in the group of 36 patients who had an initial rise in their ioPTH at 5 minutes after resection of a single gland and subsequently failed to fall. This patient underwent a subtotal parathyroidectomy, had a persistently elevated ioPTH, and was later found to have an ectopic 5th parathyroid in the mediastinum. Subsequent cure was achieved with video assisted thorascopic surgery16.
TABLE 2.
Six Month Outcomes for 108 Patients With a Rising 5 Minutes loPTH
| Single Gland Removed | Multiple Glands Removed | |
|---|---|---|
| Cure (%) | 72 (100%) | 35 (97%) |
| Postoperative calcium (mg/dL) | 9.5 ± 0.04 | 9.2 ± 0.14 |
| Postoperative PTH (pg/mL) | 46 ± 3 | 40 ± 4 |
Mean ± standard error of mean.
Discussion
The surgical approach to parathyroidectomy has been in constant evolution since the original description by Felix Mandl in 1925 17. Minimally invasive parathyroidectomy has been proposed as a viable alternative to the traditional bilateral neck dissection. Several groups have reported that minimally invasive parathyroidectomy leads to lower hospital costs, shorter lengths of stays, a lower incidence of transient hypocalcaemia and an equally high cure rate with lower complication rates18-20. The ioPTH assay has augmented this surgical technique and proper application has been shown to be the most accurate predictor of multi-gland disease and lead to an increased cure rate when compared to bilateral neck dissection 18-20. In this study, we sought to further define the interpretation of this assay when a rising ioPTH is observed.
We show that in a series of 797 patients 14% have a 5 minute post-resection ioPTH that is elevated above their respective pre-incision baseline. It is thought that this spike can be related to surgical manipulation as opposed to multi-gland disease 13. Our findings confirm this notion as 67% of our patients with a rising 5 minute ioPTH went on to be normocalcemic at 6 months following resection of only a single gland. The lack of additional hyperfunctioning tissue in the majority of patients with an elevated 5 minute ioPTH then raises the question over proper surgical management. Bilateral neck dissection in all patients with a rising 5 minute ioPTH is clearly unnecessary.
In the setting of a rising 5 minute ioPTH level, others have proposed that the surgeon must wait until the ioPTH falls to below 50% of the pre-incision value to terminate the operation13. However, as many as 25 minutes may elapse before the ioPTH falls to less than 50% of the pre-incision level13. In this manuscript, we propose a new criteria (the “Wisconsin rule”) to determine when all additional hyperfunctioning tissue has been excised.
We propose than when the 5 minute ioPTH level is increased above the pre-incision value, the “baseline” should be reset to this peak (5 minute) value. Curative resection is then predicted by a ≥50% fall in the ioPTH level from the redefined 5 minute ioPTH peak within 15 minutes of this peak (approximately 20 minutes after resection of the initial gland). The threshold for an appropriate fall of ioPTH remains at 50%, but of this reset baseline. In our group of 108 patients, 72 fell below our newly defined threshold within 25 minutes of gland resection and had their operation terminated after removal of just one gland. It is important to note that the vast majority of these 72 patients fell below 50% of the newly defined baseline much more rapidly. Indeed, 89% fell appropriately within 15 minutes of gland excision, necessitating the drawing of no additional ioPTH values (FIG. 2). When the post-operative course of these patients was examined, 100% were found to be normocalcemic at 6 months, and, thus, presumably no additional hyperfunctioning tissue was missed. When the operative course of the 36 patients who had multiple glands removed is examined in detail, the ioPTH remains persistently elevated until the resection of all the hyperfunctioning tissue, at which time the ioPTH rapidly falls below 50% within 15 minutes of the 5 minute elevated ioPTH.
In a number of different studies, suggestions have been made that the appropriate management may be to draw both a pre-incision and pre-excision value, and then calculate the appropriate decline in ioPTH from the higher of these two values 12, 19. However, Chiu et al. show in a retrospective study that using the pre-incision baseline may actually catch more abnormal glands, thus reducing operative failures 12. Furthermore, Carniero and colleagues describe a number of patients in their experience in whom the pre-excision value has already fallen below the pre-incision value, potentially due to inadvertent devascularization 19. We present our data to suggest that it is possible to manage patients with a rising 5 minute ioPTH without a pre-excision value.
In summary, patients with an increased 5 minute ioPTH generally do not have multiple hyperfunctioning glands. Moreover, we show that it is reasonable to use this elevated 5 minute ioPTH value as a new baseline with a 50% decline over the next 5 to 15 minutes being highly predictive of surgical cure. We have termed this newly proposed guideline for ioPTH interpretation as the Wisconsin Criteria. Thus, the benefit of understanding the “Wisconsin Criteria” is that if the ioPTH has risen at 5 minutes but then drops by 50% within 25 minutes after removing the abnormal gland, the surgeon should feel comfortable that the patient has a single gland adenoma.
Therefore, we would make the following suggestions. Approximately 14% of patients will have a rising 5 minute ioPTH level after resection of a single parathyroid adenoma. At this time, an additional ioPTH level should be drawn (approximately 20 minutes after resection of the initial gland), and the new “baseline” ioPTH level should be set as this peak 5 minute ioPTH level. If the ioPTH then falls by >50% within an additional 10 minutes (at either 10 or 15 minutes after initial gland resection), then the operation is terminated. In this series, 89% of patients with a single gland will fall>50% from the peak 5 minutes ioPTH within this 10 minutes. However, if the ioPTH has not dropped by 50%, the surgeon should wait for the result of the additional ioPTH that was sent approximately 20 minutes after gland resection. (This requires about an additional 5 minutes of waiting time). If the fall is >50% from the 5 minute peak at this time point, the operation is terminated. In this series, 99% of patients with a single adenoma will fall >50% from the peak 5 minute ioPTH by this time point. If the ioPTH is still elevated, then further operative exploration should be pursued to resection additional hyperfunctioning glands.
Acknowledgments
Funding Support
Howard Hughes Medical Institute NIH grant: T32 CA009614
Footnotes
The authors would like to acknowledge the assistance of Rajarajan Paneerslavan, BS in data acquisition and preparation.
References
- 1.Chen H, Sokoll L, Udelsman R. Outpatient minimally invasive parathyroidectomy: a combination of sestamibi-SPECT localization, cervical block anesthesia, and intraoperative parathyroid hormone assay. Surgery. 1999;126(6):1016–21. doi: 10.1067/msy.2099.101433. discussion 1021-2. [DOI] [PubMed] [Google Scholar]
- 2.Chen H. Surgery for primary hyperparathyroidism: what is the best approach? Ann Surg. 2002;236(5):552–3. doi: 10.1097/00000658-200211000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ito F, Sippel R, Lederman J, et al. The utility of intraoperative bilateral internal jugular venous sampling with rapid parathyroid hormone testing. Ann Surg. 2007;245(6):959–63. doi: 10.1097/01.sla.0000255578.11198.ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen H, Zeiger MA, Gordon TA, et al. Parathyroidectomy in Maryland: effects of an endocrine center. Surgery. 1996;120(6):948–52. doi: 10.1016/s0039-6060(96)80039-0. discussion 952-3. [DOI] [PubMed] [Google Scholar]
- 5.Chen H, Parkerson S, Udelsman R. Parathyroidectomy in the elderly: do the benefits outweigh the risks? World J Surg. 1998;22(6):531–5. doi: 10.1007/s002689900431. discussion 535-6. [DOI] [PubMed] [Google Scholar]
- 6.Chen H, Mack E, Starling JR. Radioguided parathyroidectomy is equally effective for both adenomatous and hyperplastic glands. Ann Surg. 2003;238(3):332–7. doi: 10.1097/01.sla.0000086546.68794.9a. discussion 337-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Egan KR, Adler JT, Olson JE, et al. Parathyroidectomy for primary hyperparathyroidism in octogenarians and nonagenarians: a risk-benefit analysis. J Surg Res. 2007;140(2):194–8. doi: 10.1016/j.jss.2007.01.027. [DOI] [PubMed] [Google Scholar]
- 8.Udelsman R. Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg. 2002;235(5):665–70. doi: 10.1097/00000658-200205000-00008. discussion 670-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Irvin GL, 3rd, Dembrow VD, Prudhomme DL. Operative monitoring of parathyroid gland hyperfunction. Am J Surg. 1991;162(4):299–302. doi: 10.1016/0002-9610(91)90135-z. [DOI] [PubMed] [Google Scholar]
- 10.Nussbaum SR, Thompson AR, Hutcheson KA, et al. Intraoperative measurement of parathyroid hormone in the surgical management of hyperparathyroidism. Surgery. 1988;104(6):1121–7. [PubMed] [Google Scholar]
- 11.Jaskowiak N, Sugg S, Helke J, et al. Pitfalls of intraoperative quick parathyroid hormone monitoring and gamma probe localization in surgery for primary hyperparathyroidism. Arch Surg. 2002;137(6):659–68. doi: 10.1001/archsurg.137.6.659. discussion 668-9. [DOI] [PubMed] [Google Scholar]
- 12.Chiu B, Sturgeon C, Angelos P. Which intraoperative parathyroid hormone assay criterion best predicts operative success? A study of 352 consecutive patients. Arch Surg. 2006;141(5):483–7. doi: 10.1001/archsurg.141.5.483. discussion 487-8. [DOI] [PubMed] [Google Scholar]
- 13.Riss P, Kaczirek K, Bieglmayer C, et al. PTH spikes during parathyroid exploration--a possible pitfall during PTH monitoring? Langenbecks Arch Surg. 2007;392(4):427–30. doi: 10.1007/s00423-006-0125-6. [DOI] [PubMed] [Google Scholar]
- 14.Yang GP, Levine S, Weigel RJ. A spike in parathyroid hormone during neck exploration may cause a false-negative intraoperative assay result. Arch Surg. 2001;136(8):945–9. doi: 10.1001/archsurg.136.8.945. [DOI] [PubMed] [Google Scholar]
- 15.Chen H, Pruhs Z, Starling JR, et al. Intraoperative parathyroid hormone testing improves cure rates in patients undergoing minimally invasive parathyroidectomy. Surgery. 2005;138(4):583–7. doi: 10.1016/j.surg.2005.06.046. discussion 587-90. [DOI] [PubMed] [Google Scholar]
- 16.Wild J, Weigel T, Chen H. The need for intraoperative parathyroid hormone monitoring during radioguided parathyroidectomy by video-assisted thoracoscopy (VATS). Clin Nucl Med. 2006;31(1):9–12. doi: 10.1097/01.rlu.0000192133.01825.77. [DOI] [PubMed] [Google Scholar]
- 17.Mandl F. Therapeutisher versuch bein falls von ostitis fibrosa generalisata mittles. Extirpation eines epithelkorperchen tumors. Wien Klin Wochenshr Zentral. 1926;143:245–284. [Google Scholar]
- 18.Sugg S, Krzywda E, Demeure M, et al. Detection of multiple gland primary hyperparathyroidism in the era of minimally invasive parathyroidectomy. Surgery. 2004;136(6):1303–9. doi: 10.1016/j.surg.2004.06.062. [DOI] [PubMed] [Google Scholar]
- 19.Carneiro DM, Solorzano CC, Nader MC, et al. Comparison of intraoperative iPTH assay (QPTH) criteria in guiding parathyroidectomy: which criterion is the most accurate? Surgery. 2003;134(6):973–9. doi: 10.1016/j.surg.2003.06.001. discussion 979-81. [DOI] [PubMed] [Google Scholar]
- 20.Irvin Gr, Solorzano C, Carneiro D. Quick intraoperative parathyroid hormone assay: surgical adjunct to allow limited parathyroidectomy, improve success rate, and predict outcome. World J Surg. 2004;28(12):1287–92. doi: 10.1007/s00268-004-7708-6. [DOI] [PubMed] [Google Scholar]