Abstract
The homeostatic control of blood pressure hinges upon the delicate balance between prohypertensinogenic and antihypertensinogenic systems. D1-like dopamine receptors [dopamine D1 and D5 receptors (D1Rs and D5Rs, respectively)] and the α1A-adrenergic receptor (α1A-AR) are expressed in the renal proximal tubule and engender opposing effects on Na+ transport, i.e., natriuresis (via D1Rs and D5Rs) or antinatriuresis (via α1A-ARs). We tested the hypothesis that the D1R/D5R regulates the α1A-AR. D1-like dopamine receptors coimmunoprecipitated, colocalized, and cofractionated with α1A-ARs in lipid rafts in immortalized human renal proximal tubule cells. Long-term treatment with the D1R/D5R agonist fenoldopam resulted in decreased D1R and D5R expression but increased α1A-AR abundance in the plasma membrane. Short-term fenoldopam treatment stimulated the translocation of Na+-K+-ATPase from the plasma membrane to the cytosol that was partially reversed by an α1A-AR agonist, which by itself induced Na+-K+-ATPase translocation from the cytosol to the plasma membrane. The α1A-AR-specific agonist A610603 also minimized the ability of fenoldopam to inhibit Na+-K+-ATPase activity. To determine the interaction among D1Rs, D5Rs, and α1A-ARs in vivo, we used phenylephrine and A610603 to decrease Na+ excretion in several D1-like dopamine receptor knockout mouse strains. Phenylephrine and A61603 treatment resulted in a partial reduction of urinary Na+ excretion in wild-type mice and its abolition in D1R knockout, D5R knockout, and D1R-D5R double-knockout mice. Our results demonstrate the ability of the D1-like dopamine receptors to regulate the expression and activity of α1A-AR. Elucidating the intricacies of the interaction among these receptors is crucial for a better understanding of the crosstalk between anti- and pro-hypertensive systems.
Keywords: adrenergic receptor, dopamine receptor, knockout mice, renal proximal tubule cells, sodium transport
the intricate control of Na+ and fluid balance and vasomotor tone, two cornerstones in blood pressure regulation, is carried out by several systems, including renin-angiotensin-aldosterone, dopaminergic, and autonomic nervous systems (1–10, 43, 54, 76, 77). Under conditions of moderate Na+ excess, the dopaminergic system engenders natriuresis by inhibiting both renal proximal and distal tubule Na+ reabsorption (1–3, 6–9, 11, 34, 66, 77). Locally generated dopamine acts on renal dopamine receptors to decrease Na+ transport by at least 50% (3, 6, 34, 66, 77). The dopamine receptors consist of D1-like dopamine receptors [dopamine D1 and D5 receptors (D1R and D5R, respectively)] and D2-like dopamine receptors [dopamine D2, D3, and D4 receptors (D2R, D3R, and D4Rs, respectively)] (6, 34, 66). The natriuretic effect of dopamine is primarily exerted through D1Rs/D5Rs by inhibiting both the entry and egress of Na+ in renal epithelial cells via inhibition of multiple Na+ transporters along the nephron (6). Dopamine inhibits Na+-K+-ATPase, Na+/H+ exchanger (NHE)3, Na-Pi cotransporters, Na+-Cl− cotransporters, and epithelial Na+ channels (1–3, 6, 7, 11, 21, 37, 42, 43, 57, 66, 77). By simultaneously inhibiting the activity of Na+-K+-ATPase at the basolateral membrane and NHE3 and other Na+ transporters at the apical membrane, dopamine can effectively decrease vectorial Na+ transport in the renal proximal tubule (1–3, 6–9, 11, 15–17, 20, 27–29, 34, 37, 42, 43, 57, 66, 77).
The sympathetic nervous system increases blood pressure through cardiovascular, adrenal, and renal mechanisms (6, 8, 12, 25, 26, 31, 35, 36, 40, 43, 46, 49, 51, 64, 66). These effects are mediated by the hormones epinephrine and norepinephrine (NE). Both hormones act by binding to adrenergic receptors (ARs), which are classified as α1-ARs (α1A, α1B, and α1D), α2-ARs (α2A, α2B, and α2C), and β-ARs (β1, β2, β3, and β4). A fourth AR (α1L-AR) represents a functional phenotype of α1A-ARs (19). Of the three α1-ARs, the α1A-AR is the major receptor subtype that is expressed in renal proximal and distal renal tubules, although to a lesser degree compared with arteries, in the human renal cortex (48). The α1A-AR is the predominant α1-AR subtype that mediates vasoconstrictor responses to exogenous NE in rats (55). Both α1-ARs and α2-ARs have been reported to stimulate renal Na+ or Cl− transport and mediate antinatriuresis (5, 73). The α1-AR stimulates the activity of Na+-K+-ATPase (5, 12, 31) and NHE1 and NHE3 in renal proximal tubule cells (51).
The present study explored the interactions between prohypertensinogenic α1A-ARs and anti-hypertensinogenic D1-like dopamine receptors in immortalized human renal proximal tubule cells (hRPTCs) and in mice. We demonstrated the biophysical interaction among these receptors and the functional control of D1-like dopamine receptors over the α1A-AR using the appropriate knockout mouse models. Understanding the molecular pathways involved in blood pressure regulation is essential for cogent drug design and development to better control hypertension.
MATERIALS AND METHODS
Animal care and ethics statement.
D1R knockout (Drd1−/−), D5R knockout (Drd5−/−), and D1R-D5R double-knockout (Drd1−/−/Drd5−/−) mice and their wild-type littermates were identified by DNA genotyping. These experiments were conducted in accordance with National Institutes of Health guidelines for the ethical treatment and handling of animals in research and were approved by the University of Maryland School of Medicine Institutional Animal Care and Use Committee.
Materials.
The materials used were as follows: DMEM-F-12, DMEM, FBS, geneticin (Neomycin, G418), and Dynabeads (GIBCO, Grand Island, NY); EGF, dexamethasone, and triiodothyronine (Sigma-Aldrich, St. Louis, MO); Nonidet P-40 (NP-40) lysis buffer (Boston Bioproducts, Ashland, MA); Halt Protease Inhibitor Cocktail and Pierce Cell Surface Protein Isolation Kit (Thermo Scientific, Rockford, IL); 2× Laemmli buffer and 10% Mini-POTEAN precast gels (Bio-Rad, Hercules, CA); rabbit polyclonal anti-α1A-AR antibody (Bioworld, Dublin, OH); rabbit polyclonal anti-α-subunit of Na+-K+-ATPase (Millipore, Billerica, MA); proprietary rabbit polyclonal anti-D1R antibody (59); rabbit polyclonal anti-D5R antibody (Genetex, Irvine, TX); human kidney sections (Zyagen, San Diego, CA); MagneHis Protein Purification Kit (Promega; Madison, WI); and sodium green tetraacetate (Molecular Probes, Grand Island, NY).
Cell lines and cell culture.
hRPTCs were obtained from normotensive nephrectomized Caucasian men and have been previously used to study renal dopamine function (27, 28, 59, 60). Cells were maintained in DMEM-F-12 with 10% FBS, 10 ng/ml EGF, 4 ng/μl dexamethasone, and 2 ng/ml triiodothyronine at 37°C in an incubator with humidified 5% CO2 and 95% air. Cells tested negative for Mycoplasma infection.
Coimmunoprecipitation.
hRPTCs were grown in 150-mm tissue culture dishes until 90% confluent and serum starved for 2 h before treatment with fenoldopam (1 μM, 15 min) or vehicle as a control. Total cell lysates were prepared using NP-40 lysis buffer with protease inhibitors. Magnetic Dynabeads were conjugated with D1R and D5R antibodies and then incubated with cell lysates for 1 h at room temperature on a rocking platform. Proteins were eluted using 2× Laemmli buffer. Samples were resolved in 10% polyacrylamide gels, electrotransferred onto nitrocellulose membranes, and probed for α1A-ARs.
For the His pulldown assays, hRPTCs were transfected with pCMV6/α1A-AR-myc,His plasmid. Cells were grown until 90% confluent, and cell lysates were prepared using NP-40 lysis buffer. His pulldown was then performed using the MagneHis Protein Purification Kit. Lysates were incubated with Ni+ particles, which bind to the 6x-His tag of α1A-AR-myc,His. After incubation for 1 h, Ni+ beads were washed three times, and bound proteins were eluted using 2× Laemmli buffer. Samples were resolved in 10% polyacrylamide gels and immunoblotted using proprietary D1R and D5R primary antibodies.
Laser scanning confocal microscopy.
hRPTCs were grown to 50% confluence on poly-d-lysine-coated coverslips and then serum starved for 1 h before treatment with fenoldopam at the given time points. Cells were then fixed with 4% paraformaldehyde, permeabilized with 0.03% Triton X-100 in PBS, and immunostained for D1Rs or D5Rs and α1A-ARs. Cholera toxin subunit B conjugated with Alexa fluor 647 and 4′,6-diamidino-2-phenylindole were used to target lipid rafts in the plasma membrane and nuclei, respectively. Coverslips were mounted using Vectashield mounting medium. Formalin-fixed, paraffin-embedded sections of the human kidney were antigen retrieved using heat and pressure and immunostained for α1A-ARs, D1Rs, or D5Rs. Sections were mounted on glass slides using Vectashield mounting medium. To determine the in vivo interaction of these receptors, we administered fenoldopam (2 μg·kg body wt−1·min−1) (23) and/or phenylephrine (0.17 μg/kg body wt) (58) or vehicle for 30 min via the femoral vein of C57Bl/6J mice. Kidneys were then flash frozen in isopentane and prepared for immunofluorescence using an anti-Na+-K+-ATPase α-subunit antibody.
Confocal and differential interference contrast images of the cells and kidney were obtained sequentially in separate channels to avoid bleedthrough using Carl Zeiss LSM 510 META with a ×63/1.4 numerical aperture oil immersion objective and processed using Zeiss 510 META with Physiology Software (version 3.5) and Multiple Time Series Software (version 3.5). The final images were prepared using Zen 2011 software.
Sucrose gradient ultracentrifugation.
To prepare lipid raft and nonlipid raft fractions, sucrose gradient centrifugation was performed using a detergent-free protocol (65) with slight modifications (75). hRPTCs were grown in 150-mm dishes until 80–90% confluent. Cells were subjected to various drug treatments, i.e., PBS (vehicle), fenoldopam (1 μM), phenylephrine (10 μM), and methyl-β-cyclodextrin for 15 min. Cell were washed two times with PBS, lysed in 1.5 ml of 500 mmol/l sodium carbonate (pH 11), homogenized, and then sonicated in clear ultracentrifuge tubes. One milliliter of the homogenate was diluted with 2 ml of 80% sucrose, overlaid with 6 ml of 35% sucrose and 3 ml of 5% sucrose, and spun at 160,000 g in a Beckman SW40 rotor at 4°C for 18 h. Sucrose solutions were prepared in 25 mM MES (pH 6.7) and 150 mM NaCl solution. Twelve 1-ml fractions were then collected and labeled as fractions 1–12 from top to bottom. Aliquots of each fraction were mixed with 2× Laemmli buffer, boiled, and subjected to immunoblot analysis for D1Rs, D5Rs, α1A-ARs, Na+-K+-ATPase, and caveolin-1 to visualize their distribution in lipid and nonlipid raft fractions.
Preparation of the plasma membrane-enriched fraction.
Serum-starved hRPTCs were treated with fenoldopam and ascorbic acid as an antioxidant at different time points (0, 3, 6, 8, and 24 h) to determine the expression profiles of D1Rs, D5Rs, α1A-ARs, and Na+-K+-ATPase. Another set of experiments involved hRPTCs treated with fenoldopam and/or phenylephrine (10 μM) to determine the effect of the treatment on Na+-K+-ATPase plasma membrane translocation. Cells were pelleted at 2,000 rpm for 5 min at room temperature. Pelleted cells were homogenized by 10 strokes of a Dounce homogenizer, sonicated with 20 3-s bursts, and spun at 2,000 rpm for 5 min to pellet out the nuclei. The supernatant was collected and respun at 40,000 g for 30 min to separate the plasma membrane-enriched fraction from the cytosol. The protein concentration of plasma membrane and cytosolic fractions was quantified using a BCA kit, and uniform amounts of protein samples were resolved using 10% SDS-PAGE, electrotransferred onto nitrocellulose membranes, and immunoblotted for the proteins of interest. β-Actin was used for normalization.
Biotinylation experiments.
To confirm the changes in the subcellular protein abundance of D1Rs, D5Rs, and α1A-ARs in response to long-term fenoldopam treatment, plasma membrane-bound receptors were evaluated via the Pierce Cell Surface Protein Isolation Kit. Briefly, cells were treated with plasma membrane-impermeant sulfo-NSS-SS-biotin for 30 min, and the reaction was quenched thereafter. Cells were collected, lyzed, and sonicated via five 1-s bursts. Biotinylated proteins were isolated from different samples with a uniform protein concentration using NeutrAvidin agarose in a column and eluted via sample buffer with 50 mM DTT. Proteins were resolved using 10% SDS-PAGE and probed for D1Rs, D5Rs, and α1A-ARs.
Na+ transport assay.
hRPTCs grown in Transwell 12-well inserts to 100% confluence were serum starved for 2 h before the following 30-min treatments: 5-(N-ethyl-N-isopropyl)amiloride (EIPA; 500 nM, added to the apical side), fenoldopam (1 μM, apical and basolateral), and/or A61603 (10 nM, apical and basolateral). Some cells were treated with ouabain (50 μM, basolateral) for 1 h and served as controls. Cells were then washed three times before the sodium green tetraacetate assay was performed (60). The fluorescence emission of each well was measured using a VICTOR3 1420 multilabel counter.
Clearance experiments in dopamine receptor knockout mice.
Adult (10–12 mo) male Drd1−/−, Drd5−/−, and Drd1−/−/Drd5−/− mice and wild-type littermates were prepared for renal clearance experiments. Mice were housed individually in metabolic cages and allowed to acclimatize for 3 days. Twenty-four-hour urine was collected on the fourth day. Mice were then treated with the α1-AR agonist phenylephrine (50 mg/kg body wt ip) (33) and, after a 24-h washover period, with the α1A-AR agonist A61603 (25 ng/kg body wt ip) (39). Doses were chosen to minimally increase blood pressure. Twenty-four-hour urine was collected during each treatment period. Urine Na+ was analyzed using a Synchron EL-ISE Electrolyte system (Beckman). Urinary Na+ excretion was calculated as urine volume × Na+ (in meq/l).
Statistical analysis.
Numeric data are expressed as means ± SE. A significant difference between two groups was determined by Student's t-test, whereas that among three or more groups was determined by one-way ANOVA followed by a Holm-Sidak post hoc test. P values of <0.05 were considered significant. Statistical analysis was performed using SigmaPlot 11 (Richmond, CA).
RESULTS
D1-like dopamine receptors interact with the α1A-AR.
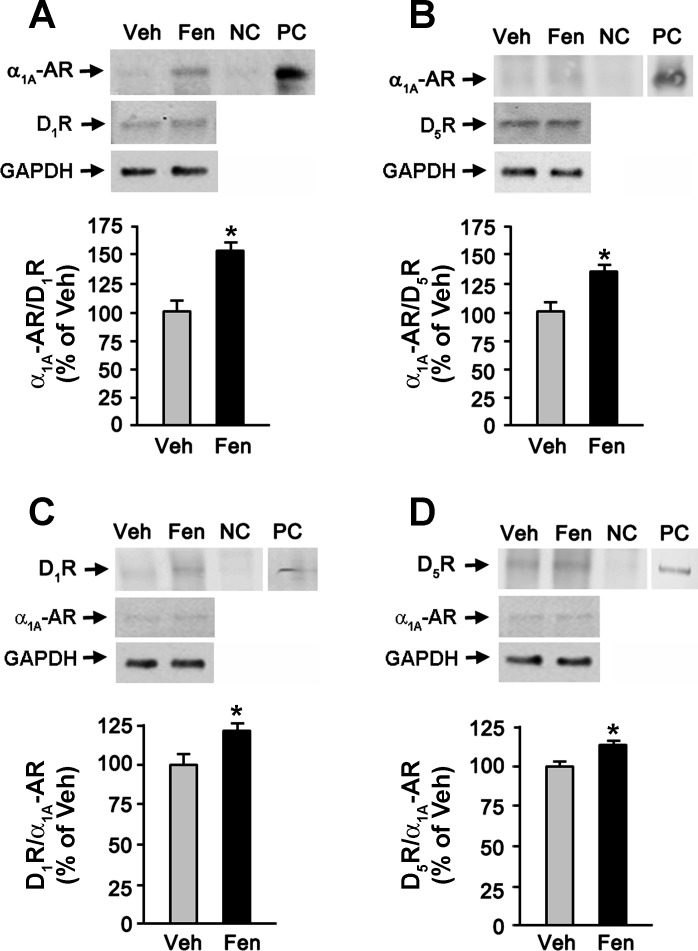
D1Rs, D5Rs, and α1A-ARs are endogenously expressed in the kidney, with dopamine receptors distributed in almost the entire nephron except the medullary collecting duct in some species and thin limbs of Henle (6, 70) and α1A-ARs mainly in proximal and distal convoluted tubules (25, 26). All three receptors are expressed in rat renal proximal tubule cells (63, 70). Through coimmunoprecipitation, a 60-kDa band corresponding to the endogenous α1A-AR was visualized in cell lysates precipitated with either D1R- or D5R-specific antibody (Fig. 1, A and B). Treatment with the D1R/D5R agonist fenoldopam enhanced the interaction between α1A-ARs and D1Rs (154.2 ± 3.6% vs. 100 ± 5.9% for vehicle) or D5Rs (131.8 ± 3.6% vs. 100 ± 4.2% for vehicle). We confirmed this interaction via His pulldown and found that these receptors interact and that fenoldopam enhanced this process (121.6 ± 1.1% vs. 100 ± 1.5% for D1Rs and 118.6 ± 3% vs. 100 ± 1.9% for D5Rs; Fig. 1, C and D).
Fig. 1.
Physical interaction between D1-like dopamine receptors and α1A-adrenergic receptors (α1A-ARs) in human renal proximal tubule cells (hRPTCs). A and B: cells were serum starved for 1 h before treatment with fenoldopam (Fen; 1 μM, 15 min) or vehicle (Veh). Endogenous dopamine D1 receptors (D1Rs) and dopamine D5 receptors (D5Rs) were immunoprecipitated using receptor-specific rabbit polyclonal antibodies or normal rabbit IgG as a negative control (NC). The immunoprecipitate was probed for α1A-ARs (∼60 kDa). Total cell lysates were used a positive control (PC). The D1R or D5R was used for normalization. GAPDH indicates uniform loading of samples. n = 3. C and D: hRPTCs were transiently transfected with His-tagged α1A-ARs or “empty vector” as the NC for 48 h. Cell lysates were subjected to His pulldown and then probed for D1Rs and D5Rs (∼55 kDa). Total cell lysates were used the PC. The α1A-AR was used for normalization. GAPDH indicates uniform loading of the samples. n = 3.
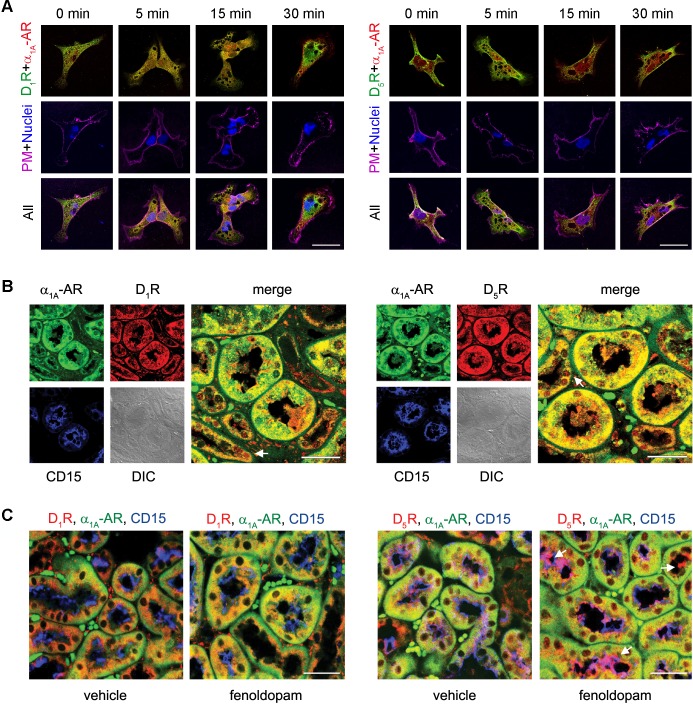
We next determined the spatial and temporal dynamics of the interaction and found that, under basal condition, the receptors were distributed to some extent in the plasma membrane but to a great extent in the cytoplasm, where they partially colocalized (Fig. 2A). Treatment with fenoldopam redistributed some of the D1-like dopamine receptors to the submembrane area [we have previously reported that only around 50% of D5Rs internalized upon agonist activation (69)] and enhanced their colocalization with α1A-ARs. In a nonpathological section of the human kidney, all three receptors were expressed abundantly at the cytoplasm of proximal tubules, as indicated by the positive staining for the proximal tubule marker CD15, where the receptors colocalized strongly, and at the distal convoluted tubules (Fig. 2B). In the kidneys of untreated C57Bl/6J mice, D1Rs and D5Rs were localized mainly to the cytoplasm and subapical area, whereas α1A-ARs were found mostly at the basal portion of the cytoplasm (Fig. 2C). Fenoldopam treatment enhanced the colocalization of D1Rs and α1A-ARs at the perinuclear area and the movement of D5Rs to the brush border and greater colocalization with α1A-ARs at the perinuclear area.
Fig. 2.
Colocalization of D1-like dopamine receptors and α1A-ARs in hRPTCs and human and mouse kidneys. A: hRPTCs were grown on coverslips, serum starved for 1 h, and treated with Fen (1 μM) at the indicated time points. Cells were then fixed, double immunostained for D1Rs or D5Rs (pseudocolored green) and α1A-ARs (pseudocolored red), and visualized via confocal microscopy. Around 30–40 cells were scored, and 5–10 cells were imaged per experiment. The lipid rafts of the plasma membrane were visualized using cholera toxin subunit B (CTxB) conjugated with Alexa fluor 647, and nuclei were visualized using 4′,6-diamidino-2-phenylindole (DAPI). Colocalization between D1-like dopamine receptors and α1A-ARs is denoted by yellow punctate areas, whereas colocalization of these receptors with the plasma membrane (PM) is denoted by white in the merged images. B: human kidney sections were antigen retrieved and double immunostained for D1Rs or D5Rs (pseudocolored red) and α1A-ARs (pseudocolored green). Proximal tubules were visualized using brush border-localized CD15 (pseudocolored blue) as a marker. Distal convoluted tubules are indicated with white arrows. DIC, differential interference contrast. C: C57Bl/6J mice were treated with Fen (2 μg·kg−1·min−1 iv) or Veh for 30 min, and kidneys were collected and prepared for immunofluorescence to evaluate the distribution and colocalization of D1Rs or D5Rs (pseudocolored red) and α1A-ARs (pseudocolored green). Proximal tubules were visualized using CD15 (pseudocolored blue) as a marker. The localization of D5Rs at the brush border is indicated by the white arrows. Magnification: ×600. Scale bars = 10 μm. n = 3.
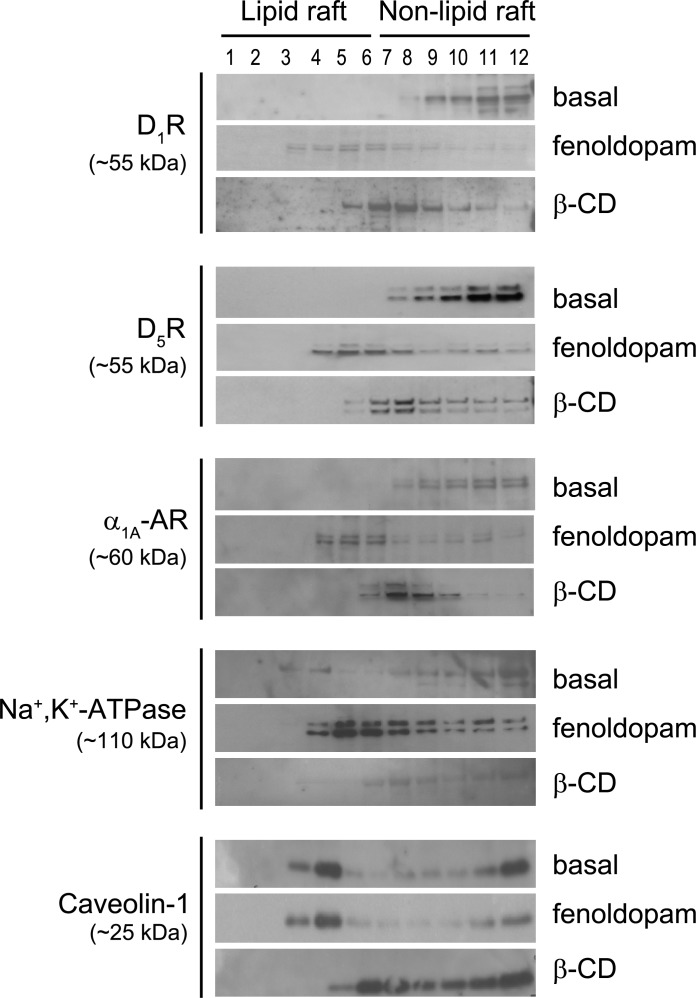
D1-like dopamine receptors cofractionate with the α1A-AR.
In the plasma membrane, distinct cholesterol-enriched islands collectively known as lipid rafts provide a cohesive platform for G protein-coupled receptors and signaling molecules for a fast, high-fidelity activation of signal transduction (56). In hRPTCs, all three receptors were distributed in nonlipid rafts, whereas Na+-K+-ATPase was localized to both lipid and nonlipid raft fractions at the basal state (Fig. 3). Fenoldopam stimulation redistributed the receptors and Na+-K+-ATPase to lipid raft fractions. The appearance of duplets may be due to the presence of native and glycosylated “active” forms of the receptors (13, 61, 62) in the plasma membrane. The membrane-bound α-subunit of Na+-K+-ATPase is phosphorylated and ubiquitinylated before endocytosis (18). The lipid raft marker caveolin-1 was found in lipid as well as nonlipid rafts basally and after fenoldopam treatment. Treatment with the cholesterol-depleting drug methyl-β-cyclodextrin, which disrupts lipid rafts, resulted in the redistribution of caveolin-1 and other components to the less buoyant nonlipid raft microdomain.
Fig. 3.
Cofractionation of D1-like dopamine receptors and α1A-ARs in hRPTCs. Serum-starved (1 h) hRPTCs were treated with Fen (1 μM, 15 min) or with methyl-β-cyclodextrin (β-CD) to disrupt lipid raft microdomains. PM-enriched cellular pellets were then subjected to sucrose gradient ultracentrifugation, and 12 fractions were obtained. The most buoyant fractions (fractions 1–6) represent lipid rafts, whereas the rest (fractions 7–12) represent nonlipid rafts. The various fractions were then probed for proteins of interest. Caveolin-1 was used as a marker for lipid raft microdomains. n = 4.
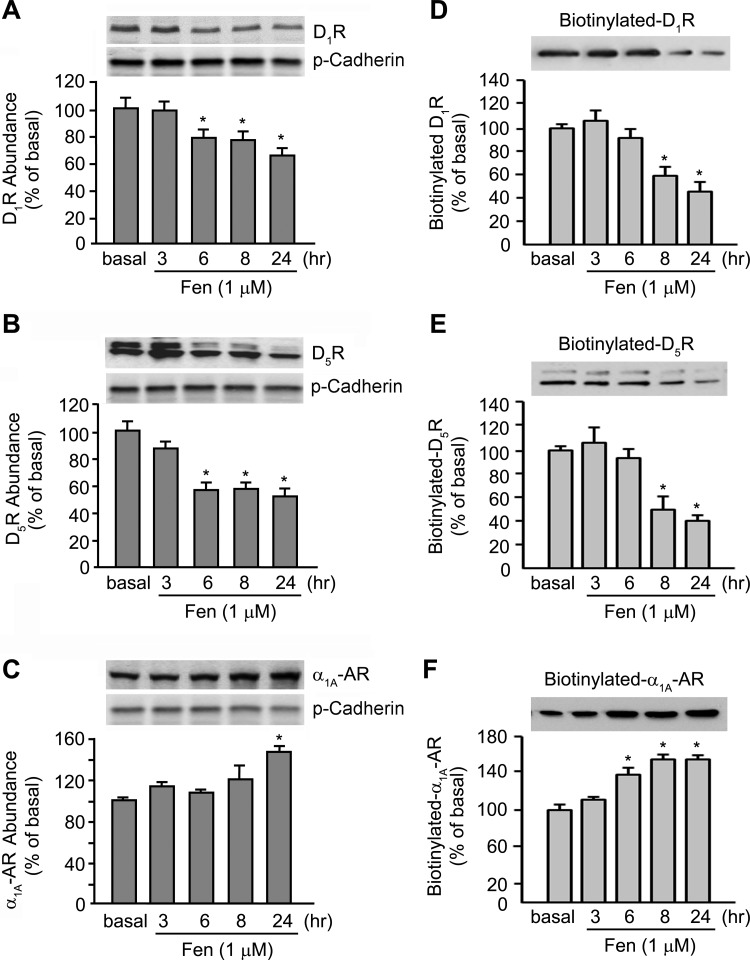
D1-like dopamine receptor stimulation downregulates α1A-AR expression.
Since these receptors interact with one another but engender contrasting effects on renal Na+ transport (6, 12, 31, 51), we next determined if D1-like dopamine receptors regulate the α1A-AR. Long-term fenoldopam treatment (6–24 h) resulted in decreased abundance of D1Rs and D5Rs but increased α1A-AR abundance in plasma membrane-enriched fractions from hRPTCs (Fig. 4, A–C). To corroborate our initial findings, we performed biotinylation experiments using a plasma membrane-impermeant biotin. Fenoldopam-treated hRPTCs were labeled with biotin, and biotinylated surface proteins were isolated using avidin agarose columns and then probed for the receptors of interest. Fenoldopam reduced the abundance of biotinylated D1Rs and D5Rs but increased that of α1A-ARs (Fig. 4, D–F). This shows the ability of dopamine receptors to negatively regulate the expression of ARs, which increased when the D1R/D5R abundance was reduced. The Na+-K+-ATPase abundance was unchanged throughout the treatment period (data not shown).
Fig. 4.
Protein expression profiles after D1-like dopamine receptor treatment in hRPTCs. Serum-starved (1 h) hRPTCs were treated with Fen (1 μM) at the indicated time points. A–C: PM-enriched fractions were prepared for immunoblot analysis using uniform amounts of protein. Pan (p)-cadherin was used for normalization. D–F: in a separate set of experiments, Fen-treated hRPTCs were labeled with cell membrane-impermeant sulfo-NSS-SS-biotin, and surface proteins were isolated using an avidin column and then probed for D1Rs, D5Rs, and α1A-ARs. Numeric data are expressed as means ± SE. Representative blots are shown above the graphs. *P < 0.05 vs. the other groups (by one-way ANOVA and a Holm-Sidak post hoc test). n = 3–4/group.
D1-like dopamine receptors and α1A-ARs regulate Na+-K+-ATPase internalization and activity.
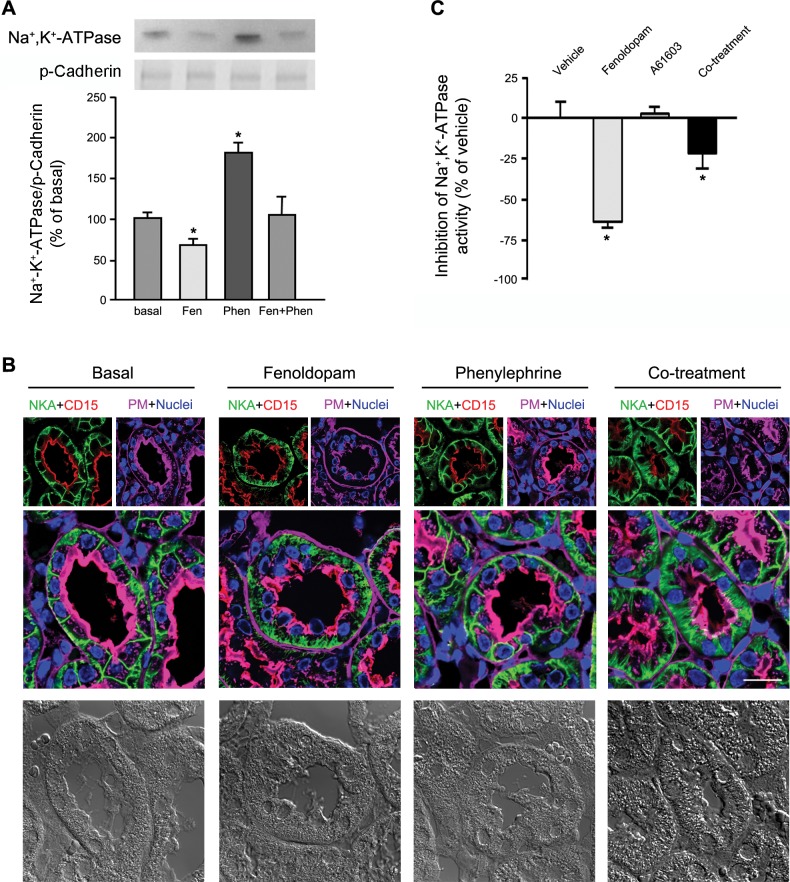
We next evaluated the effect of agonist-activated D1Rs/D5Rs and α1A-ARs on Na+-K+-ATPase translocation by measuring the abundance of plasma membrane-bound Na+-K+-ATPase (the fraction that actively transports Na+ out of the cell in exchange for K+). Stimulation with fenoldopam decreased the plasma membrane abundance of Na+-K+-ATPase by 30%, whereas stimulation with the α1A-AR agonist phenylephrine increased it almost twofold (Fig. 5A). Cotreatment with fenoldopam and phenylephrine did not change the Na+-K+-ATPase abundance in the plasma membrane, indicating the ability of one receptor to cancel the effect of the other receptor. We next corroborated the effect of agonist treatment on Na+-K+-ATPase translocation by visualizing its distribution in the proximal tubules of C57Bl/6J mice. Na+-K+-ATPase was distributed mainly at the basolateral membrane of CD15+ proximal tubules at the basal state (Fig. 5B). Fenoldopam treatment promoted the endocytosis and redistribution of Na+-K+-ATPase into the cytoplasm, whereas phenylephrine treatment resulted in the retention of Na+-K+-ATPase at the basolateral membrane in most proximal tubules, presumably by preventing Na+-K+-ATPase endocytosis. Cotreatment resulted in the endocytosis of Na+-K+-ATPase in some tubules but not in others. We next evaluated the effect of D1R/D5R and α1A-AR stimulation on Na+-K+-ATPase activity in hRPTCs grown in a polarized state and treated with EIPA to inhibit Na+ influx through NHE3. Fenoldopam treatment resulted in 65 ± 6% inhibition of ouabain-inhibitable Na+ transport, similar to that observed in Wistar-Kyoto rat renal proximal tubule cells treated with fenoldopam (100 nM, 15 min) (15). Cotreatment with the α1A-AR-selective agonist A61603 reduced the extent of inhibition of Na+ transport to 30% (Fig. 5C). There was no marked increase in Na+ transport in cells treated with A61603 because a suboptimal dose was used (10 nM) (52).
Fig. 5.
Distribution and translocation of Na+-K+-ATPase. A: hRPTCs were serum starved for 1 h and then treated with Fen and/or phenylephrine (Phen) or Veh (basal) for 30 min. PM-enriched fractions were isolated and immunoblotted for Na+-K+-ATPase. p-Cadherin was used for normalization. One group of blots is shown above the graph. *P < 0.05 vs. the other groups (by one-way ANOVA and a Holm-Sidak post hoc test). n = 3. B: C57BL/6J mice were treated with Fen (2 μg·kg−1·min−1 iv) and/or Phen (0.17 μg·kg−1·min−1 iv) or Veh (basal) for 30 min. Mice were then euthanized, and kidneys were perfused with normal saline before fixation and immunostaining for Na+-K+-ATPase (pseudocolored green) and CD15 (a proximal tubule marker, pseudocolored red). Wheat germ agglutinin tagged with Alexa fluor 647 was used to target lectins at the brush border and around the tubules (pseudocolored magenta), whereas DAPI was used to visualize nuclei (pseudocolored blue). DIC images are shown at the bottom. Magnification: ×600. Scale bar = 10 μm. C: hRPTCs grown to confluence in Transwell 12-well inserts were serum starved for 2 h before treatment with Fen (1 μM) and/or A61603 (100 nM) for 30 min. Cells treated with ouabain (50 μM) for 1 h served as controls and were used to calculate the percentage of ouabain-inhibitable Na+ activity. *P < 0.05 vs. the other groups (by one-way ANOVA and a Holm-Sidak post hoc test). n = 3.
Mice lacking D1-like dopamine receptors have diminished Na+ excretion upon α1A-AR stimulation.
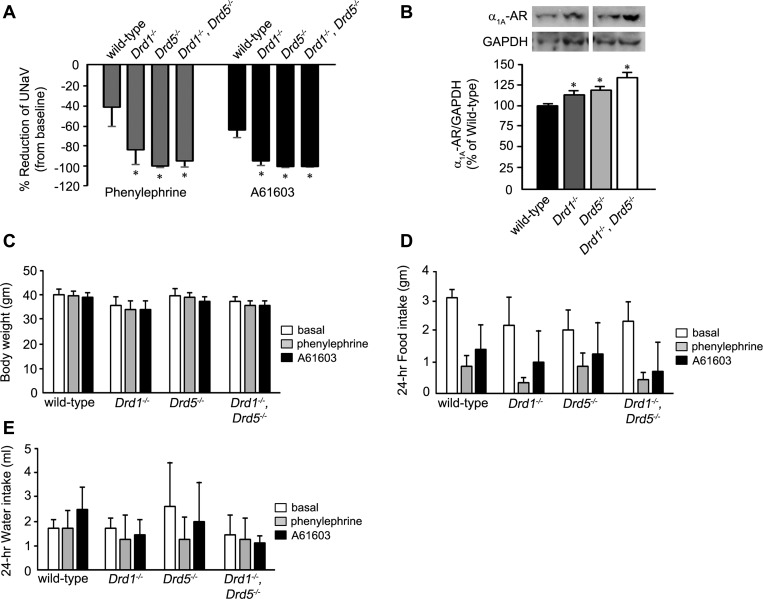
We next evaluated the ability of D1Rs/D5Rs to regulate the function of α1A-ARs in vivo by treating 10-mo-old male Drd1−/−, Drd5−/−, and Drd1−/−/Drd5−/− mice housed in metabolic cages with α1-AR agonists, which should decrease renal Na+ excretion. Treatment with phenylephrine and A61603 resulted in 42.4 ± 17.1% and 59.6 ± 5.6% reductions of 24-h urinary Na+ excretion in wild-type mice and 83 ± 14.9% and 95 ± 3.8% reductions in Drd1−/− mice, respectively (Fig. 6A). The same treatment resulted in the abrogation of Na+ excretion in Drd5−/− and Drd1−/−/Drd5−/− mice. The protein expression of renal α1A-ARs, compared with wild-type control mice, was 115.3 ± 2.1%, 120.9 ± 2.3%, and 135.0 ± 5.2% in Drd1−/−, Drd5−/−, and Drd1−/−/Drd5−/− mice (Fig. 6B). These data demonstrate the ability of D1-like dopamine receptors to counterregulate the α1A-AR-induced decrease in renal Na+ excretion in mice. There were no differences in body weight (Fig. 6C), food intake (Fig. 6D), or water consumption (Fig. 6E) among these mice before and after the treatment.
Fig. 6.
Effect on urinary Na+ excretion (UNaV) of α1A-AR stimulation in D1R knockout (Drd1−/−), D5R knockout (Drd5−/−), and D1R-D5R double-knockout (Drd1−/−/Drd5−/−) mice. Adult male Drd1−/−, Drd5−/−, and Drd1−/−/Drd5−/−, and wild-type mice were placed individually in metabolic cages for 3 days before and during pharmacological treatment with Phen (50 mg/kg body wt ip) and A61603 (25 ng/kg body wt ip). The 24-h urine voided before and after treatment was collected, and urine Na+ was measured to determine the amount of UNaV (A). Renal α1A-AR expression was quantified in whole kidney homogenates via Western blot analysis using rabbit anti-α1A-AR antibody and normalized for GAPDH (B). Body weight (C) and 24-h food (D) and water (E) intakes were measured before and after treatment. Numeric data are expressed as means ± SE. *P < 0.05 vs. the other groups (by one-way ANOVA and a Holm-Sidak post hoc test). n = 3–4/group.
DISCUSSION
Blood pressure homeostasis is carried out by the intricate interaction among various physiological mechanisms. In the kidney, both natriuretic and antinatriuretic factors work in tandem and often counterregulate one another's activity to keep Na+, water, and blood pressure in balance (5, 6, 31, 34, 38, 40). Among the various hormonal and humoral factors, the natriuretic hormone dopamine (via dopamine receptors) and antinatriuretic hormones ANG II [via the ANG II type 1 receptor (AT1R)] and NE (via the α-AR) are important in maintaining Na+ and water balance and blood pressure homeostasis (6, 7, 34, 38, 64, 66). While the interaction between dopamine receptors and AT1Rs in the kidney has been extensively studied (6, 45, 66, 76), the interaction between renal dopamine receptors and ARs has not been as rigorously pursued.
D1-like dopamine receptor interactions with and regulation of the α1A-AR.
A model of bidirectional regulation of renal Na+ transport by dopamine receptors and α-ARs has been previously described (5–7, 43, 46, 64, 66). In this model, dopamine coordinates the effects of natriuretic and antinatriuretic factors (3, 6). Thus, dopamine opposes the effects of antinatriuretic factors, such as those of the α-AR. In human mononuclear cells, activation of D1Rs/D5Rs suppresses catecholamine production by inhibiting the expression of tyrosine hydroxylase, the rate-limiting enzyme in neural dopamine synthesis (24). Dopamine, via D2-like dopamine receptors, inhibits the release of NE in gastric and uterine arteries (53). However, only 30% of urinary NE and 21% of urinary dopamine are derived from renal nerves (8).
Stimulation of D1Rs, D5Rs, and D3Rs inhibits the proliferation of vascular smooth muscle cells induced by NE (50). In the present study, we showed that long-term treatment with the D1-like dopamine receptor agonist decreased the expression of D1Rs and D5Rs but increased that of α1A-ARs, indicating that the D1R/D5R keeps the expression of the α1A-AR in the kidney under control. In contrast, dopamine acts cooperatively with other natriuretic factors, such as the β-AR in the proximal tubule. The β-AR has similar effects as the D1R/D5R in the renal proximal tubule since all are coupled to adenylyl cyclase, increase cAMP production, and inhibit tubular Na+-K+-ATPase activity (6, 41). The activation of β-AR sensitizes the D1R and, together, inhibit Na+-K+-ATPase in renal proximal tubule cells (14). Conversely, α2-AR blockade results in enhanced dopamine output in the prefrontal cortex in rats (39, 71). The α2-AR attenuates the inhibitory effect of D1-like dopamine receptors on NHE3 activity in renal brush border membranes (2).
One of the hallmarks of D1-like dopamine receptor activation is the inhibition of Na+-K+-ATPase activity in almost all segments of the nephron (6, 7, 34, 66). In the proximal tubule, this negative regulation involves PKC- or PKA-mediated phosphorylation of the catalytic α-subunit of Na+-K+-ATPase (29, 42, 57, 74) as well as the internalization of the α-subunit from the plasma membrane to the cytosol (16, 27, 28, 45, 57). Removal of catalytic subunits from the plasma membrane and their transport along the endosomal network effectively abrogate the active transport of Na+ across the basolateral membrane (22). We now report that D1R/D5R stimulation inhibits Na+-K+-ATPase activity, in part, by decreasing the abundance of the α-subunit in the plasma membrane via endocytosis (9, 22, 45), whereas α1A-AR activation increases its abundance by recruiting more Na+-K+-ATPase to the plasma membrane. Costimulation of these receptors did not increase Na+-K+-ATPase abundance in the plasma membrane, demonstrating the ability of D1-like dopamine receptors to counterbalance the effect of the α1A-AR. Dopamine can antagonize NE-mediated Na+ transport (11).
Although we did not explore the mechanism involved in the cross-talk between the D1R/D5R and α1A-AR, there are two ways by which these receptors can regulate the translocation of Na+-K+-ATPase, i.e., direct protein-protein interactions and through secondary messengers and G protein subunits involved in the signal transduction of each receptor (6, 11, 42, 57, 66). The D1R can directly interact with Na+-K+-ATPase at the plasma membrane and markedly decrease its activity even in the absence of a ligand (37, 45). Since agonist stimulation brings together D1R/D5R, α1A-AR, and Na+-K+-ATPase in lipid raft microdomains, it is conceivable that these proteins form a cohesive signaling complex where one protein may directly suppress the function of the others via structural hindrance (37), e.g., D1Rs/D5Rs may directly dampen the activity of both α1A-ARs and Na+-K+-ATPase. It is also possible that the activation of D1-like dopamine receptors may uncouple the α1A-AR, analogous to how the D1R inhibits the AT1R (45, 76), preventing its stimulatory effect on Na+-K+-ATPase.
Heightened Na+ retention in D1R/D5R-deficient mice.
Costimulation of D1- and D2-like dopamine receptors results in synergism between these receptors to promote diuresis and natriuresis in rats (44). As previously indicated, D1-like dopamine receptors and α-ARs have opposing effects on Na+ transport (4, 17, 20, 73). In the absence of D1-like dopamine receptors, the inhibitory effect of D1-like receptors on Na+ transport is diminished (1), whereas the α1A-AR predominates (present study). Both Drd1−/− and Drd5−/− mice are hypertensive and exhibit defects in renal Na+ excretion (1, 72). The lack of functional D1Rs and/or D5Rs in these mice should result to unfettered Na+ retention after agonist stimulation of α1A-ARs. Indeed, we showed that stimulation with the α1A-AR agonist phenylephrine and the α1A-AR agonist A61603 resulted in the abrogation of Na+ excretion in these knockout mice but only 42% and 60% reduction in wild-type littermates, respectively. The slight difference in the reduction of Na+ excretion between phenylephrine and A61603 treatments could be attributed to the activity of other α1-ARs. There were no differences between D1Rs and D5Rs in terms of the extent of regulation over α1A-ARs. Our group has previously reported that Drd5−/− mice manifest with an elevated urinary epinephrine-to-NE ratio and that these mice have greater reduction in blood pressure after adrenalectomy or α-adrenergic blockade compared with wild-type littermates (40). Interestingly, Drd2−/− mice develop hypertension that is secondary to increased sympathetic and endothelin B receptor activity, decreased renal dopamine production, and impaired Na+ excretion (49, 54, 67).
Taken together, our data contribute to the concept of an organized signaling complex that is composed of the D1R, D5R, α1A-AR, and α-subunit of Na+-K+-ATPase in plasma membrane microdomains. We found that D1Rs and D5Rs are basally distributed in nonlipid rafts, in contrast to our previous report (32), which used total cell lysates instead of just the plasma membrane in this study, and that these receptors are found in both lipid and nonlipid rafts. It is conceivable that intracellular D1Rs and D5Rs are distributed in lipid raft microdomains of intracellular vesicles, whereas surface D1Rs and D5Rs are in nonlipid raft microdomains in the plasma membrane at the basal state.
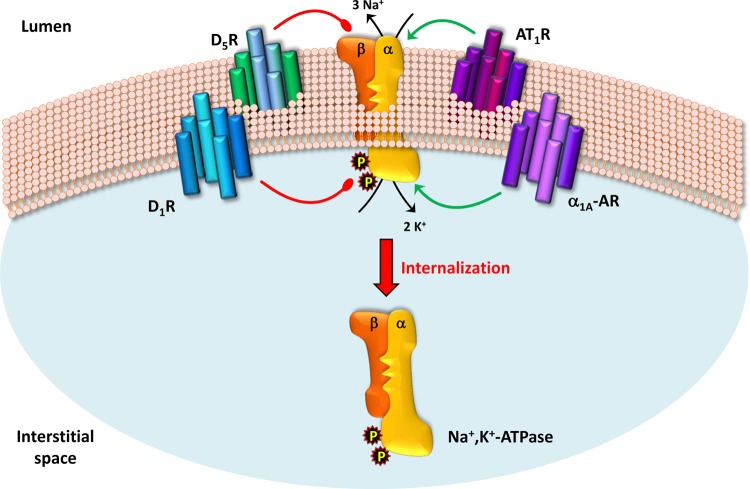
The receptor cross-talk facilitates a dynamic interaction among the receptors, e.g., natriuretic receptors D1R and D5R interact to possibly augment each other's activity and, at the same time, antagonize antinatriuretic receptors α1A-AR and AT1R and inhibit Na+-K+-ATPase through direct physical hindrance or through signal transduction (Fig. 7). Agonist-activated D1Rs and D5Rs dimerize in renal epithelial cells (P. Yu and P. Jose, unpublished observations), and the impairment of one receptor results in the total absence of cAMP production in response to agonist stimulation (68, 69), indicating a collaborative association between D1Rs and D5Rs. These receptors dimerize with ANG II type 2 receptors to cooperatively inhibit Na+ transport in hRPTCs (28). Alternatively, α1A-ARs and AT1Rs may synergize to balance the activity of dopamine receptors and, directly or indirectly, stimulate Na+-K+-ATPase activity. AT1Rs can dimerize with α1D-ARs in rats with pregnancy-induced hypertension (18a) and with β-ARs, in which the inhibition of one receptor can transinhibit the other (10).
Fig. 7.
Model of the dynamic interaction among the D1-like dopamine receptors, α1A-AR, and ANG II type 1 receptor (AT1R). The activity of these endogenously expressed receptors is ultimately governed by salt homeostasis. In salt-replete states, natriuretic D1Rs and D5Rs, along with ANG II type 2 receptors (not shown), may act cooperatively to inhibit anti-natriuretic α1A-ARs and AT1Rs and impede Na+-K+-ATPase activity via phosphorylation of the catalytic α-subunit and internalization. However, during salt-depleted states, α1A-ARs and AT1Rs stimulate Na+-K+-ATPase activity and overcome the decreased activity of dopamine receptors.
In summary, we have demonstrated the dynamic interaction of D1-like dopamine receptors and α1A-ARs in hRPTCs and in mouse and human kidneys as well as the antagonism of D1Rs/D5Rs on the expression and activity of α1A-ARs in hRPTCs and on renal Na+ handling in several dopamine receptor-deficient mice. Our findings highlight the importance of a comprehensive understanding of the cross-talk between functionally opposing systems in the control of Na+ homeostasis to facilitate improved therapeutic management and rational drug design for hypertension.
GRANTS
This work was supported, in part, by National Institutes of Health Grants R01-DK-039308, R01-HL-092196, R37-HL-023081, and R01-DK-090918.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
AUTHOR CONTRIBUTIONS
Author contributions: R.C.E., I.A., X.W., D.R.S., P.A.J., and V.A.M.V. conception and design of research; R.C.E., L.D.A., I.A., J.Y., J.B.F., J.A.J., C.S.E., P.Y., X.W., and V.A.M.V. performed experiments; R.C.E., L.D.A., I.A., J.Y., J.B.F., J.A.J., C.S.E., P.Y., P.A.J., and V.A.M.V. interpreted results of experiments; R.C.E. and V.A.M.V. drafted manuscript; R.C.E., L.D.A., I.A., J.Y., J.B.F., J.A.J., C.S.E., P.Y., X.W., D.R.S., P.A.J., and V.A.M.V. approved final version of manuscript; I.A., J.Y., J.B.F., J.A.J., C.S.E., P.Y., P.A.J., and V.A.M.V. analyzed data; I.A., J.A.J., X.W., D.R.S., and P.A.J. edited and revised manuscript.
REFERENCES
- 1.Albrecht FE, Drago J, Felder RA, Printz MP, Eisner GM, Robillard JE, Sibley DR, Westphal HJ, Jose PA. Role of the D1A dopamine receptor in the pathogenesis of genetic hypertension. J Clin Invest 97: 2283–2288, 1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Albrecht FE, Xu J, Moe OW, Hopfer U, Simonds WF, Orlowski J, Jose PA. Regulation of NHE3 activity by G protein subunits in renal brush-border membranes. Am J Physiol Regul Integr Comp Physiol 278: R1064–R1073, 2000. [DOI] [PubMed] [Google Scholar]
- 3.Aperia AC. Intrarenal dopamine: a key signal in the interactive regulation of sodium metabolism. Annu Rev Physiol 62: 621–647, 2000. [DOI] [PubMed] [Google Scholar]
- 4.Aperia A, Fryckstedt J, Holtbäck U, Belusa R, Cheng XJ, Eklöf AC, Li D, Wang ZM, Ohtomo Y. Cellular mechanisms for bi-directional regulation of tubular sodium reabsorption. Kidney Int 49: 1743–1747, 1996. [DOI] [PubMed] [Google Scholar]
- 5.Aperia A, Ibarra F, Svensson LB, Klee C, Greengard P. Calcineurin mediates α-adrenergic stimulation of Na+,K+-ATPase activity in renal tubule cells. Proc Natl Acad Sci USA 89: 7394–7397, 1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Armando I, Villar VA, Jose PA. Dopamine and renal function and blood pressure regulation. Compr Physiol 1: 1075–1117, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bacic D, Kaissling B, McLeroy P, Zou L, Baum M, Moe OW. Dopamine acutely decreases apical membrane Na/H exchanger NHE3 protein in mouse renal proximal tubule. Kidney Int 64: 2133–2141, 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baines AD. Effects of salt intake and renal denervation on catecholamine catabolism and excretion. Kidney Int 21: 316–322, 1982. [DOI] [PubMed] [Google Scholar]
- 9.Baines AD, Ho P, Drangova R. Proximal tubular dopamine production regulates basolateral Na-K-ATPase. Am J Physiol Renal Fluid Electrolyte Physiol 262: F566–F571, 1992. [DOI] [PubMed] [Google Scholar]
- 10.Barki-Harrington L, Luttrell LM, Rockman HA. Dual inhibition of β-adrenergic and angiotensin II receptors by a single antagonist: a functional role for receptor-receptor interaction in vivo. Circulation 108: 1611–1618, 2003. [DOI] [PubMed] [Google Scholar]
- 11.Baum M, Quigley R. Inhibition of proximal convoluted tubule transport by dopamine. Kidney Int 54: 1593–1600, 1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beguin P, Beggah A, Cotecchia S, Geering K. Adrenergic, dopaminergic, and muscarinic receptor stimulation leads to PKA phosphorylation of Na-K-ATPase. Am J Physiol Cell Physiol 270: C131–C137, 1996. [DOI] [PubMed] [Google Scholar]
- 13.Bergson C, Mrzljak L, Lidow MS, Goldman-Rakic PS, Levenson R. Characterization of subtype-specific antibodies to the human D5 dopamine receptor: studies in primate brain and transfected mammalian cells. Proc Natl Acad Sci USA 92: 3468–3472, 1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brismar H, Agrèn M, Holtbäck U. β-Adrenoceptor agonist sensitizes the dopamine-1 receptor in renal tubular cells. Acta Physiol Scand 175: 333–340, 2000. [DOI] [PubMed] [Google Scholar]
- 15.Chen Y, Asico LD, Zheng S, Villar VA, He D, Zhou L, Zeng C, Jose PA. Gastrin and D1 dopamine receptor interact to induce natriuresis and diuresis. Hypertension 62: 927–933, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chibalin AV, Ogimoto G, Pedemonte CH, Pressley TA, Katz AI, Féraille E, Berggren PO, Bertorello AM. Dopamine-induced endocytosis of Na+,K+-ATPase is initiated by phosphorylation of Ser-18 in the rat α subunit and is responsible for the decreased activity in epithelial cells. J Biol Chem 274: 1920–1927, 1999. [DOI] [PubMed] [Google Scholar]
- 17.Cunningham R, Biswas R, Brazie M, Steplock D, Shenolikar S, Weinman EJ. Signaling pathways utilized by PTH and dopamine to inhibit phosphate transport in mouse renal proximal tubule cells. Am J Physiol Renal Physiol 296: F355–F361, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dada LA, Welch LC, Zhou G, Ben-Saadon R, Ciechanover A, Sznajder JI. Phosphorylation and ubiquitination are necessary for Na,K-ATPase endocytosis during hypoxia. Cell Signal 19: 1893–1898, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18a.de Lourdes González-Hernández M, Godínez-Hernández D, Bobadilla-Lugo RA, López-Sánchez P. Angiotensin-II type 1 receptor (AT1R) and alpha-1D adrenoceptor form a heterodimer during pregnancy-induced hypertension. Auton Autacoid Pharmacol 30: 167–172, 2010. [DOI] [PubMed] [Google Scholar]
- 19.Docherty JR. Subtypes of functional α1-adrenoceptor. Cell Mol Life Sci 67: 405–417, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Du Z, Yan Q, Wan L, Weinbaum S, Weinstein AM, Wang T. Regulation of glomerulotubular balance. I. Impact of dopamine on flow-dependent transport. Am J Physiol Renal Physiol 303: F386–F395, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Efendiev R, Bertorello AM, Pressley TA, Rousselot M, Féraille E, Pedemonte CH. Simultaneous phosphorylation of Ser11 and Ser18 in the α-subunit promotes the recruitment of Na+,K+-ATPase molecules to the plasma membrane. Biochemistry 39: 9884–9892, 2000. [DOI] [PubMed] [Google Scholar]
- 22.Efendiev R, Pedemonte CH. Contrary to rat-type, human-type Na,K-ATPase is phosphorylated at the same amino acid by hormones that produce opposite effects on enzyme activity. J Am Soc Nephrol 17: 31–38, 2006. [DOI] [PubMed] [Google Scholar]
- 23.Escano CS, Armando I, Wang X, Asico LD, Pascua A, Yang Y, Wang Z, Lau YS, Jose PA. Renal dopaminergic defect in C57Bl/6J mice. Am J Physiol Regul Integr Comp Physiol 297: R1660–R1669, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferrari M, Cosentino M, Marino F, Bombelli R, Rasini E, Lecchini S, Frigo G. Dopaminergic D1-like receptor-dependent inhibition of tyrosine hydroxylase mRNA expression and catecholamine production in human lymphocytes. Biochem Pharmacol 67: 865–873, 2004. [DOI] [PubMed] [Google Scholar]
- 25.Gesek FA. α1- and α2-Adrenoceptor control of sodium transport reverses in developing hypertension. Hypertension 33: 524–529, 1999. [DOI] [PubMed] [Google Scholar]
- 26.Gesek FA, Cragoe EJ, Jr, Strandhoy JW. Synergistic alpha-1 and alpha-2 adrenergic stimulation of rat proximal nephron Na+/H+ exchange. J Pharmacol Exp Ther 249: 694–700, 1989. [PubMed] [Google Scholar]
- 27.Gildea JJ, Israel JA, Johnson Zhang J, Jose PA, Felder RA. Caveolin-1 and dopamine-mediated internalization of NaKATPase in human renal proximal tubule cells. Hypertension 54: 1070–1076, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gildea JJ, Wang X, Shah N, Tran H, Spinosa M, Van Sciver R, Sasaki M, Yatabe J, Carey RM, Jose PA, Felder RA. Dopamine and angiotensin type 2 receptors cooperatively inhibit sodium transport in human renal proximal tubule cells. Hypertension 60: 396–403, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gomes P, Soares-da-Silva P. Dopamine-induced inhibition of Na+-K+-ATPase activity requires integrity of actin cytoskeleton in opossum kidney cells. Acta Physiol Scand 175: 93–101, 2002. [DOI] [PubMed] [Google Scholar]
- 31.Gopalakrishnan SM, Chen C, Lokhandwala MF. Alpha1-adrenoceptor subtypes mediating stimulation of Na+,K+-ATPase activity in rat renal proximal tubules. Eur J Pharmacol 288: 139–147, 1995. [DOI] [PubMed] [Google Scholar]
- 32.Han W, Li H, Villar VA, Pascua AM, Dajani MI, Wang X, Natarajan A, Quinn MT, Felder RA, Jose PA, Yu P. Lipid rafts keep NADPH oxidase in the inactive state in human renal proximal tubule cells. Hypertension 51: 481–487, 2008. [DOI] [PubMed] [Google Scholar]
- 33.Harbison RD, Stedeford T, Muro-Cacho C, Mosquera DI, Banasik M. Activation of α1-adrenergic receptors potentiates the nephrotoxicity of ethylene dibromide. Toxicology 186: 181–189, 2003. [DOI] [PubMed] [Google Scholar]
- 34.Harris RC, Zhang MZ. Dopamine, the kidney, and hypertension. Curr Hypertens Rep 14: 138–143, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harrison DG. The mosaic theory revisited: common molecular mechanisms coordinating diverse organ and cellular events in hypertension. J Am Soc Hypertens 7: 68–74, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hayashi Y, Chiba K, Matsuoka T, Suzuki-Kusaba M, Yoshida M, Hisa H, Satoh S. Renal nerve stimulation induces α2-adrenoceptor-mediated antinatriuresis under inhibition of prostaglandin synthesis in anesthetized dogs. Tohoku J Exp Med 188: 335–346, 1999. [DOI] [PubMed] [Google Scholar]
- 37.Hazelwood LA, Free RB, Cabrera DM, Skinbjerg M, Sibley DR. Reciprocal modulation of function between the D1 and D2 dopamine receptors and the Na+,K+-ATPase. J Biol Chem 283: 36441–36453, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Herrera M, Coffman TM. The kidney and hypertension: novel insights from transgenic models. Curr Opin Nephrol Hypertens 21: 171–178, 2012. [DOI] [PubMed] [Google Scholar]
- 39.Hertel P, Fagerquist MV, Svensson TH. Enhanced cortical dopamine output and antipsychotic-like effects of raclopride by α2 adrenoceptor blockade. Science 286: 105–107, 1999. [DOI] [PubMed] [Google Scholar]
- 40.Hollon TR, Bek MJ, Lachowicz JE, Ariano MA, Mezey E, Ramachandran R, Wersinger SR, Soares-da-Silva P, Liu ZF, Grinberg A, Drago J, Young WS, 3rd, Westphal H, Jose PA, Sibley DR. Mice lacking D5 dopamine receptors have increased sympathetic tone and are hypertensive. J Neurosci 22: 10801–10810, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Holtbäck U, Ohtomo Y, Förberg P, Sahlgren B, Aperia A. Neuropeptide Y shifts equilibrium between α- and β-adrenergic tonus in proximal tubule cells. Am J Physiol Renal Physiol 275: F1–F7, 1998. [DOI] [PubMed] [Google Scholar]
- 42.Horiuchi A, Takeyasu K, Mouradian MM, Jose PA, Felder RA. D1A dopamine receptor stimulation inhibits Na+/K+-ATPase activity through protein kinase A. Mol Pharmacol 43: 281–285, 1993. [PubMed] [Google Scholar]
- 43.Ibarra F, Aperia A, Svensson LB, Eklöf AC, Greengard P. Bidirectional regulation of Na+,K+-ATPase activity by dopamine and an α-adrenergic agonist. Proc Natl Acad Sci USA 90: 21–24, 1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jose PA, Asico LD, Eisner GM, Pocchiari F, Semeraro C, Felder RA. Effects of costimulation of dopamine D1- and D2-like receptors on renal function. Am J Physiol Regul Integr Comp Physiol 275: R986–R994, 1998. [DOI] [PubMed] [Google Scholar]
- 45.Khan F, Spicarová Z, Zelenin S, Holtbäck U, Scott L, Aperia A. Negative reciprocity between angiotensin II type 1 and dopamine D1 receptors in rat renal proximal tubule cells. Am J Physiol Renal Physiol 295: F1110–F1116, 2008. [DOI] [PubMed] [Google Scholar]
- 46.Kim JK, Linas SL, Schrier RW. Catecholamines and sodium transport in the kidney. Pharmacol Rev 31: 169–178, 1979. [PubMed] [Google Scholar]
- 47.Knepper SM, Buckner SA, Brune ME, DeBernardis JF, Meyer MD, Hancock AA. A-61603, a potent α1-adrenergic receptor agonist, selective for the α1A receptor subtype. J Pharmacol Exp Ther 274: 97–103, 1995. [PubMed] [Google Scholar]
- 48.Kurooka Y, Moriyama N, Nasu K, Kameyama S, Fukasawa R, Yano J, Kawabe K. Distribution of α1-adrenoceptor subtype mRNAs in human renal cortex. BJU Int 83: 299–304, 1999. [DOI] [PubMed] [Google Scholar]
- 49.Li XX, Bek M, Asico LD, Yang Z, Grandy DK, Goldstein DS, Rubinstein M, Eisner GM, Jose PA. Adrenergic and endothelin B receptor-dependent hypertension in dopamine receptor type-2 knockout mice. Hypertension 38: 303–308, 2001. [DOI] [PubMed] [Google Scholar]
- 50.Li Z, Yu C, Han Y, Ren H, Shi W, Fu C, He D, Huang L, Yang C, Wang X, Zhou L, Asico LD, Zeng C, Jose PA. Inhibitory effect of D1-like and D3 dopamine receptors on norepinephrine-induced proliferation in vascular smooth muscle cells. Am J Physiol Heart Circ Physiol 294: H2761–H2768, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu F, Gesek FA. α1-Adrenergic receptors activate NHE1 and NHE3 through distinct signaling pathways in epithelial cells. Am J Physiol Renal Physiol 280: F415–F425, 2001. [DOI] [PubMed] [Google Scholar]
- 52.Luo DL, Gao J, Fan LL, Tang Y, Zhang YY, Han QD. Receptor subtype involved in α1-adrenergic receptor-mediated Ca2+ signaling in cardiomyocytes. Acta Pharmacol Sin 28: 968–974, 2007. [DOI] [PubMed] [Google Scholar]
- 53.Morgadinho MT, Fontes Ribeiro CA, Macedo TR. Presynaptic dopamine receptors involved in the inhibition of noradrenaline and dopamine release in the human gastric and uterine arteries. Fundam Clin Pharmacol 13: 662–670, 1999. [DOI] [PubMed] [Google Scholar]
- 54.Ozono R, Ueda A, Oishi Y, Yano A, Kambe M, Katsuki M, Oshima T. Dopamine D2 receptor modulates sodium handling via local production of dopamine in the kidney. J Cardiovasc Pharmacol 42, Suppl 1: S75–S79, 2003. [DOI] [PubMed] [Google Scholar]
- 55.Passmore JC, Joshua IG, Rowell PP, Tyagi SC, Falcone JC. Reduced α adrenergic mediated contraction of renal preglomerular blood vessels as a function of gender and aging. J Cell Biochem 96: 672–681, 2005. [DOI] [PubMed] [Google Scholar]
- 56.Patel HH, Murray F, Insel PA. G-protein-coupled receptor-signaling components in membrane raft and caveolae microdomains. Handb Exp Pharmacol 186: 167–184, 2008. [DOI] [PubMed] [Google Scholar]
- 57.Pedemonte CH, Efendiev R, Bertorello AM. Inhibition of Na,K-ATPase by dopamine in proximal tubule epithelial cells. Semin Nephrol 25: 322–327, 2005. [DOI] [PubMed] [Google Scholar]
- 58.Powers J, Bernstein D. The mouse as a model of cardiovascular adaptations to microgravity. J Appl Physiol 97: 1686–1692, 2004. [DOI] [PubMed] [Google Scholar]
- 59.Sanada H, Jose PA, Hazen-Martin D, Yu PY, Xu J, Bruns DE, Phipps J, Carey RM, Felder RA. Dopamine-1 receptor coupling defect in renal proximal tubule cells in hypertension. Hypertension 33: 1036–1042, 1999. [DOI] [PubMed] [Google Scholar]
- 60.Sasaki S, Siragy HM, Gildea JJ, Felder RA, Carey RM. Production and role of extracellular guanosine cyclic 3′,5′ monophosphate in sodium uptake in human proximal tubule cells. Hypertension 43: 286–291, 2004. [DOI] [PubMed] [Google Scholar]
- 61.Sawutz DG, Lanier SM, Warren CD, Graham RM. Glycosylation of the mammalian α1-adrenergic receptor by complex type N-linked oligosaccharides. Mol Pharmacol 32: 565–571, 1987. [PubMed] [Google Scholar]
- 62.Sidhu A. A novel affinity purification of D-1 dopamine receptors from rat striatum. J Biol Chem 265: 10065–10072, 1990. [PubMed] [Google Scholar]
- 63.Simão S, Fraga S, Jose PA, Soares-da-Silva P. Oxidative stress and α1-adrenoceptor-mediated stimulation of the Cl−/HCO3− exchanger in immortalized SHR proximal tubular epithelial cells. Br J Pharmacol 153: 1445–1455, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Soares-da-Silva P. Renal tubular dopamine outward transfer during Na+-H+ exchange activation by α1- and α2-adrenoceptor agonists. Br J Pharmacol 109: 569–576, 1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Song KS, Li Shengwen Okamoto T, Quilliam LA, Sargiacomo M, Lisanti MP. Co-purification and direct interaction of Ras with caveolin, an integral membrane protein of caveolae microdomains. Detergent-free purification of caveolae microdomains. J Biol Chem 271: 9690–9697, 1996. [DOI] [PubMed] [Google Scholar]
- 66.Tayebati SK, Lokhandwala MF, Amenta F. Dopamine and vascular dynamics control: present status and future perspectives. Curr Neurovasc Res 8: 246–257, 2011. [DOI] [PubMed] [Google Scholar]
- 67.Ueda A, Ozono R, Oshima T, Yano A, Kambe M, Teranishi Y, Katsuki M, Chayama K. Disruption of the type 2 dopamine receptor gene causes a sodium-dependent increase in blood pressure in mice. Am J Hypertens 16: 853–858, 2003. [DOI] [PubMed] [Google Scholar]
- 68.Villar VA, Armando I, Sanada H, Frazer LC, Russo CM, Notario PM, Lee H, Comisky L, Russell HA, Yang Y, Jurgens JA, Jose PA, Jones JE. Novel role of sorting nexin 5 in renal D1 dopamine receptor trafficking and function: implications for hypertension. FASEB J 27: 1808–1819, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Villar VA, Jones JE, Armando I, Asico LD, Escano CS, Jr, Lee H, Wang X, Yang Y, Pascua-Crusan AM, Palmes-Saloma CP, Felder RA, Jose PA. Sorting nexin 1 loss results in D5 dopamine receptor dysfunction in human renal proximal tubule cells and hypertension in mice. J Biol Chem 288: 152–163, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang X, Villar VA, Armando I, Eisner GM, Felder RA, Jose PA. Dopamine, kidney, and hypertension: studies in dopamine receptor knockout mice. Pediatr Nephrol 23: 2131–2146, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Weikop P, Kehr J, Scheel-Krüger J. The role of α1- and α2-adrenoreceptors on venlafaxine-induced elevation of extracellular serotonin, noradrenaline and dopamine levels in the rat prefrontal cortex and hippocampus. J Psychopharmacol 18: 395–403, 2004. [DOI] [PubMed] [Google Scholar]
- 72.Wang X, Luo Y, Escano CS, Yang Z, Asico L, Li H, Jones JE, Armando I, Lu Q, Sibley DR, Eisner GM, Jose PA. Upregulation of renal sodium transporters in D5 dopamine receptor-deficient mice. Hypertension 55: 1431–1437, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wong KR, Berry CA, Cogan MG. α1-Adrenergic control of chloride transport in the rat S1 proximal tubule. Am J Physiol Renal Fluid Electrolyte Physiol 270: F1049–F1056, 1996. [DOI] [PubMed] [Google Scholar]
- 74.Yao LP, Li XX, Yu PY, Asico LD, Jose PA. Dopamine D1 receptor and protein kinase C isoforms in spontaneously hypertensive rats. Hypertension 32: 1049–1053, 1998. [DOI] [PubMed] [Google Scholar]
- 75.Yu P, Yang Z, Jones JE, Wang Z, Owens SA, Mueller SC, Felder RA, Jose PA. D1 dopamine receptor signaling involves caveolin-2 in HEK-293 cells. Kidney Int 66: 2167–2180, 2004. [DOI] [PubMed] [Google Scholar]
- 76.Zeng C, Wang Z, Hopfer U, Asico LD, Eisner GM, Felder RA, Jose PA. Rat strain effects of AT1 receptor activation on D1 dopamine receptors in immortalized renal proximal tubule cells. Hypertension 46: 799–805, 2005. [DOI] [PubMed] [Google Scholar]
- 77.Zhang MZ, Yao B, Wang S, Fan X, Wu G, Yang H, Yin H, Yang S, Harris RC. Intrarenal dopamine deficiency leads to hypertension and decreased longevity in mice. J Clin Invest 121: 2845–2854, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]