Summary
Background
International research for acute myocardial infarction lacks comparisons of whole health systems. We assessed time trends for care and outcomes in Sweden and the UK.
Methods
We used data from national registries on consecutive patients registered between 2004 and 2010 in all hospitals providing care for acute coronary syndrome in Sweden and the UK. The primary outcome was all-cause mortality 30 days after admission. We compared effectiveness of treatment by indirect casemix standardisation. This study is registered with ClinicalTrials.gov, number NCT01359033.
Findings
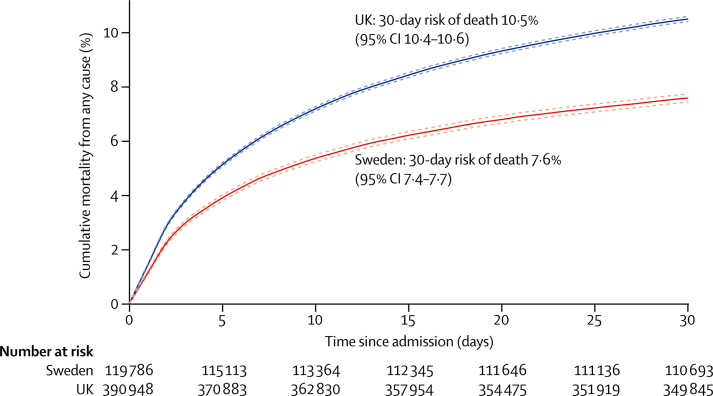
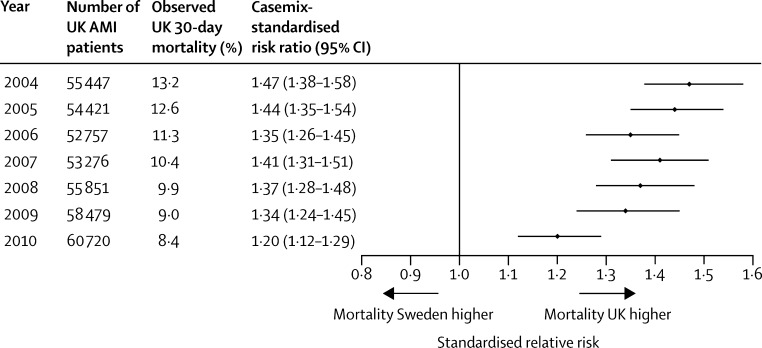
We assessed data for 119 786 patients in Sweden and 391 077 in the UK. 30-day mortality was 7·6% (95% CI 7·4–7·7) in Sweden and 10·5% (10·4–10·6) in the UK. Mortality was higher in the UK in clinically relevant subgroups defined by troponin concentration, ST-segment elevation, age, sex, heart rate, systolic blood pressure, diabetes mellitus status, and smoking status. In Sweden, compared with the UK, there was earlier and more extensive uptake of primary percutaneous coronary intervention (59% vs 22%) and more frequent use of β blockers at discharge (89% vs 78%). After casemix standardisation the 30-day mortality ratio for UK versus Sweden was 1·37 (95% CI 1·30–1·45), which corresponds to 11 263 (95% CI 9620–12 827) excess deaths, but did decline over time (from 1·47, 95% CI 1·38–1·58 in 2004 to 1·20, 1·12–1·29 in 2010; p=0·01).
Interpretation
We found clinically important differences between countries in acute myocardial infarction care and outcomes. International comparisons research might help to improve health systems and prevent deaths.
Funding
Seventh Framework Programme for Research, National Institute for Health Research, Wellcome Trust (UK), Swedish Association of Local Authorities and Regions, Swedish Heart-Lung Foundation.
Introduction
Recognition is growing of the need for comparative effectiveness research to improve the quality and outcomes of health care. International comparisons of cancer survival1 and years of life lost to ischaemic heart disease2 from 1990–2010 suggest that the performance of the UK health system needs to be improved. However, studies that simultaneously examine care and outcomes are lacking. The Institute of Medicine identified health-care delivery systems and cardiovascular care as among the highest priorities for comparative effectiveness research.3 The efficacy of treatments for acute myocardial infarction has been extensively studied in randomised trials,4, 5 but uptake and use of these treatments vary within and between the UK (England and Wales) and Sweden.6, 7, 8, 9, 10 A study in patients with ST-segment-elevation myocardial infarction (STEMI) in 12 European countries reported increasing use of primary percutaneous coronary intervention (PCI) but showed striking differences between countries.11 Attributes of care systems, including organisational culture, care pathways, and programmes to improve quality, are not assessed in trials but might be associated with outcome.12 30-day mortality for acute myocardial infarction is an important indicator of hospital performance, and delivery of care has more immediate potential to improve outcomes than treatment innovations.13 International comparisons of whole health-care delivery systems, therefore, might yield important, actionable insights to guide development of policies and clinical practice.14
International comparative effectiveness research for acute myocardial infarction has had three main limitations. First is a lack of comparison of whole health systems. Existing studies lack population coverage because they are based on selected samples of hospital patients reported in voluntary registries,8, 9, 10 one-off surveys,15 or trials16 that are known to differ from the national population in treatments and outcomes.17 Second, international studies have compared only care8 or outcomes18 or have been restricted to patients with either STEMI7, 8, 9 or non-STEMI.10 Third, attempts have not been made to standardise the mortality of patients in one country by the casemix in another. As a result, there are few studies between health systems from which to set benchmark outcome goals.
A crucial feature of the health systems in Sweden and the UK is that they are the only two countries worldwide that have continuous national clinical registries for acute coronary syndrome with mandated participation for all hospitals.19, 20 Comparison of these two countries is facilitated by the similarity of their health systems (universal, funded from taxation, and free at the point of use), proportion of gross domestic product spent on health, and national policy guidance provided for the evidence-based management of acute myocardial infarction.21, 22 Differences are that Sweden has more rapid diffusion of some new technologies,23 more complete use of evidence-based practice,9 and a more established system for evaluating and reporting the quality and outcomes of care24 than the UK.
In the absence of previous international comparisons, our objectives in this study were as follows: first, to assess the validity of comparing data from the two nationwide clinical registries; second, to compare time trends for proportions of patients in receipt of effective interventions while in hospital and at discharge between 2004 and 2010; third, to compare crude and casemix-standardised 30-day mortality between the two countries and between clinically important subgroups; fourth to estimate time trends in casemix-standardised mortality and compare them between Sweden and the UK; and fifth, to explore the contribution of clinical care to any difference in mortality.
Methods
Study population
All hospitals providing care for acute myocardial infarction in Sweden and the UK contribute data on consecutive patients to the Swedish Web-System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies (SWEDEHEART)/Register of Information and Knowledge about Swedish Heart Intensive care Admissions (RIKS-HIA) and the UK Myocardial Ischaemia National Audit Project (MINAP), respectively. RIKS-HIA and MINAP comply with the Cardiology Audit and Registration Data Standards (for acute coronary syndrome in Europe.7, 25, 26 We obtained data for all patients who were admitted to hospital because of acute myocardial infarction between Jan 1, 2004, and Dec 31, 2010. For patients with multiple admissions we used the earliest record. Acute myocardial infarction diagnosis was based on guidelines from the European Society of Cardiology/American College of Cardiology/American Heart Association.27 The study was approved by the MINAP Academic Group and the steering group of SWEDEHEART.
Casemix and treatment measures
The definitions of casemix, evidence-based hospital treatment, and discharge medications in SWEDEHEART/RIKS-HIA and MINAP were compared (appendix pp 2–9). The 17 casemix characteristics were demographic factors (age, sex, year of admission), risk factors (smoking, history of diabetes mellitus, and hypertension), severity of acute myocardial infarction (troponin concentrations, systolic blood pressure at admission, heart rate at admission), history of heart failure, cardiac arrest at admission, history of cerebrovascular disease, or history of acute myocardial infarction, and previous procedures or use of medication (antiplatelet treatment with aspirin, clopidogrel, or both, PCI, coronary artery bypass graft surgery). Features of hospital treatment for STEMI were reperfusion therapy (primary PCI or fibrinolytic therapy before or during hospital stay), delay between symptom onset and primary PCI or fibrinolysis, coronary intervention other than primary PCI, intravenous glycoprotein IIb/IIIa inhibitors, and use of anticoagulants. Discharge medications assessed were antiplatelet therapy (aspirin, clopidogrel, or both), β blockers, angiotensin-converting-enzyme (ACE) inhibitors or angiotensin-receptor blockers (ARBs), and statins. Validation of SWEDEHEART/RIKS-HIA (each year a trained monitor compares data with a chart review in 30 randomly selected patients within each hospital) showed a 96·1% agreement.20 Validation of MINAP data (compared with reaudit data, generated from each hospital annually by the re-entering of 20 data items on 20 randomly selected patients) showed a median agreement of 89·5%.19
Mortality
The primary clinical outcome was all-cause mortality within 30 days after hospital admission. National unique identifiers were used to link patients with the National Death Registry in Sweden or the Office for National Statistics in the UK. We accessed these registries to ascertain vital status or date of death at 30 days.
Statistical analysis
We compared troponin I and T concentrations, casemix, hospital treatment, and medication at discharge between Swedish and UK patients. Data are shown as proportion (95% CI) for categorical variables and mean (SD) or median (IQR) for continuous variables. To further investigate the comparability of acute myocardial infarction diagnosis in the two registries, we compared the propensity of acute myocardial infarction diagnosis between UK and Sweden patients (appendix pp 12–13). Treatments for acute myocardial infarction were also compared by year of hospital admission.
We compared mortality outcomes with Kaplan-Meier analysis in clinically important subgroups (STEMI or non-STEMI, troponin concentration, systolic blood pressure at admission, heart rate at admission, sex, age, year of admission, diabetes status, and smoking), after casemix standardisation, and by propensity-score matching. In casemix standardisation, we modelled 30-day mortality for the two countries with the 17 casemix variables then applied the Sweden model to the UK acute myocardial infarction population to estimate the casemix-standardised relative risk of observed UK 30-day mortality for each study year and overall. In propensity matching, we estimated the propensity of being a STEMI patient and the propensity of being a non-STEMI patient in Sweden and the UK, according to logistic regression, and then matched patients on the basis of propensity scores (appendix pp 12–14).
Casemix models incorporated a random effect for participant hospital. The extent of missing values was assessed and then managed by multiple imputation (appendix pp 16–19). Analyses were performed with SAS (version 9.3), R (version 2.9.2), and Matlab (version 7.14). This study is registered with ClinicalTrials.gov, number NCT01359033.
Role of the funding source
The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. S-CC had full access to all the data in the study. TJ and HH had final responsibility for the decision to submit for publication.
Results
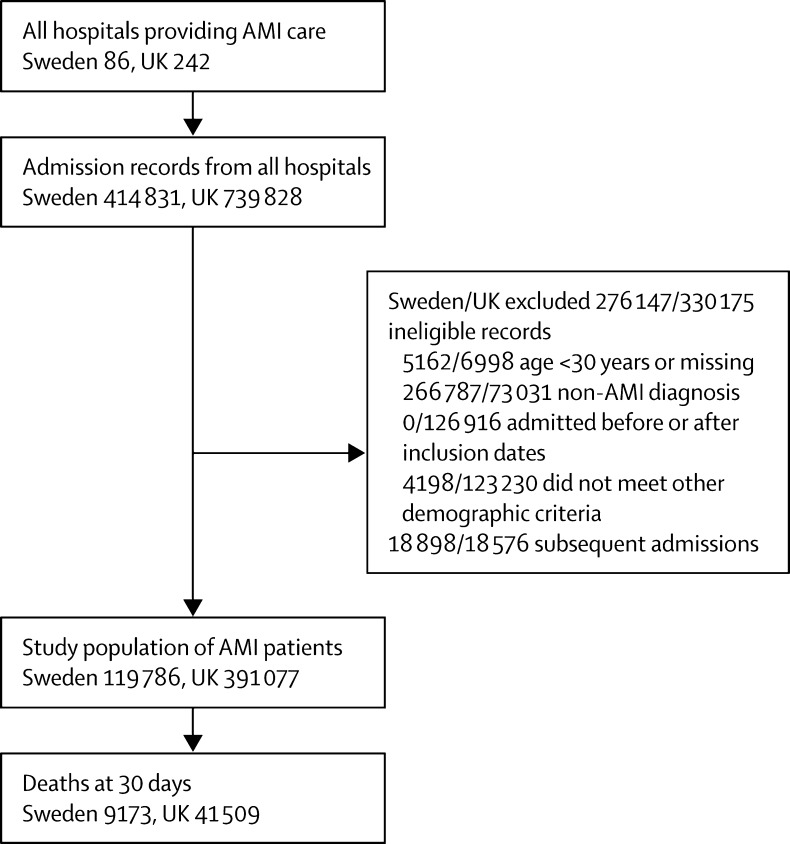
The study population was drawn from 86 hospitals in Sweden and 242 in the UK. 119 786 patients were eligible in Sweden and 391 077 in the UK (figure 1) and data on 30-day mortality were available for 119 786 (100%) and 390 951 (99·97%) of these, respectively.
Figure 1.
Study population
AMI=acute myocardial infarction. ID=identifier.
Median concentrations (IQR) maximum troponin I and troponin T were similar in Sweden and the UK overall (table 1) and for STEMI and non-STEMI patients by year (appendix pp 10–11).
Table 1.
Casemix and treatment for patients with AMI in Sweden and the UK
| Sweden (n=119 786) | UK (n=391 077) | ||
|---|---|---|---|
| Casemix | |||
| STEMI | 38 432 (32·1%, 31·8–32·3) | 157 418 (40·3%, 40·1–40·4) | |
| Mean (SD) age (years) | 71·2 (12·3) | 69·5 (13·6) | |
| Female | 43 512 (36·3%, 36·1–36·6) | 135 664 (34·8%, 34·7–34·9) | |
| Median (IQR) AMI severity | |||
| Systolic blood pressure (mm Hg) | 145 (125–165) | 139 (120–158) | |
| Heart rate (beats per min) | 78 (65–93) | 79 (66–94) | |
| Troponin I (μg/L) | 4·2 (0·8–18·0) | 4·4 (0·8–21·7) | |
| Troponin T (μg/L) | 0·7 (0·2–2·3) | 0·65 (0·2–2·3) | |
| Risk factor | |||
| Current smoker | 25 085 (23·3%, 23·0–23·5) | 104 522 (29·5%, 29·3–29·6) | |
| History of diabetes | 26 992 (22·7%, 22·4–22·9) | 65 458 (17·6%, 17·4–17·7) | |
| History of hypertension | 53 155 (45·2%, 44·9–45·5) | 173 342 (47·3%, 47·2–47·5) | |
| Cardiovascular disease history | |||
| Heart failure | 10 859 (9·7%, 9·5–9·8) | 18 944 (5·3%, 5·2–5·4) | |
| Cardiac arrest before admission | 1578 (1·3%, 1·3–1·4) | 8478 (2·3%, 2·2–2·3) | |
| Cerebrovascular disease | 9816 (10·1%, 9·9–10·3) | 30 091 (8·5%, 8·4–8·5) | |
| Myocardial infarction | 26 526 (22·4%, 22·1–22·6) | 67 346 (18·3%, 18·1–18·4) | |
| Prehospital treatment | |||
| Antiplatelet monotherapy | 43 485 (36·6%, 36·3–36·9) | 98 247 (26·4%, 26·3–26·6) | |
| Antiplatelet dual therapy | 4788 (4·0%, 3·9–4·1) | 10 931 (2·9%, 2·9–3·0) | |
| PCI | 9475 (8·0%, 7·8–8·2) | 19 473 (5·4%, 5·4–5·5) | |
| CABG | 9192 (7·7%, 7·6–7·9) | 17 383 (4·8%, 4·8–4·9) | |
| Hospital treatment | |||
| STEMI patients | |||
| Total reperfusion treatment | 27 354 (71·2%, 70·7–71·6) | 118 880 (76·6%, 76·4–76·8) | |
| Prehospital fibrinolysis | 1533 (4·1%, 3·9–4·4) | 13 903 (9·3%, 9·2–9·5) | |
| In-hospital fibrinolysis* | 4539 (11·8%, 11·5–12·1) | 84 112 (54·2%, 54·0–54·5) | |
| Primary PCI | 22 773 (59·3%, 58·8–59·8) | 34 695 (22·4%, 22·2–22·6) | |
| Median (IQR) delay from symptom to fibrinolysis (min) | 177 (108–322) | 150 (94–285) | |
| Median (IQR) delay from symptom to primary PCI (min) | 198 (129–365) | 199 (140–328) | |
| Non-STEMI and STEMI patients | |||
| Coronary intervention other than primary PCI | 34 288 (28·6%, 28·4–28·9) | 58 492 (17·3%, 17·2–17·5) | |
| IV glycoprotein IIb/IIIa receptor inhibitors | 24 993 (21·0%, 20·8–21·2) | 28 389 (8·6%, 8·5–8·7) | |
| Anticoagulants | 87 271 (73·2%, 73·0–73·5) | 28 3344 (83·0%, 82·9–83·1) | |
| Median (IQR) duration of hospital stay (days) | 5 (3–7) | 6 (3–10) | |
| Discharge medication | |||
| Antiplatelet monotherapy | 30 409 (27%, 26·8–27·3) | 103 218 (34·2%, 34·1–34·4) | |
| Antiplatelet dual therapy | 76 099 (67·6%, 67·3–67·9) | 183 753 (60·9%, 60·8–61·1) | |
| β blocker | 99 779 (88·7%, 88·5–88·9) | 231 505 (78·2%, 78–78·3) | |
| ACE inhibitor or ARB | 63 102 (56·2%, 55·9–56·5) | 242 300 (82·3%, 82·2–82·5) | |
| Statin | 89 767 (79·7%, 79·5–79·9) | 276 335 (92·8%, 92·7–92·9) | |
Values are number (%, 95% CI) unless stated otherwise. STEMI=ST-segment-elevation myocardial infarction. AMI=acute myocardial infarction. PCI=percutaneous coronary intervention. CABG=coronary artery bypass graft surgery. IV=intravenous. ACE=angiotensin-converting enzyme. ARB=angiotensin-receptor blocker.
Prehospital and in-hospital fibrinolysis are not mutually exclusive.
The proportion of patients with STEMI was lower in Sweden than in the UK (32% vs 40%). The distributions of age and sex were similar in the two countries (table 1). Swedish patients had more favourable risk profiles than UK patients for some factors (eg, lower prevalence of current smoking and higher systolic blood pressure at admission), but worse risk profiles for other factors (eg, higher prevalence of diabetes, heart failure, and cerebrovascular disease). Previous use of antiplatelet and β-blocker therapy was greater in Sweden, but use of statins on admission was lower (table 1).
Total reperfusion for STEMI was more common in the UK than in Sweden (77% vs 71%). Fibrinolysis was also more common in the UK (54% vs 12%), but primary PCI was notably more common in Sweden (59% vs 22%; table 1). The median delay from symptom onset to hospital admission was similar in the two countries. The median delay from symptom onset to primary PCI in STEMI patients was similar, but for fibrinolysis the delay was longer in Sweden (table 1). Overall, coronary interventions (other than primary PCI) and use of intravenous glycoprotein IIb/IIIa agents were higher in Sweden than in the UK. For patients who survived to hospital discharge, those in Sweden were more likely than those in the UK to be prescribed dual antiplatelet therapy or β blockers, but less likely to be prescribed ACE inhibitors or ARBs and statins (table 1).
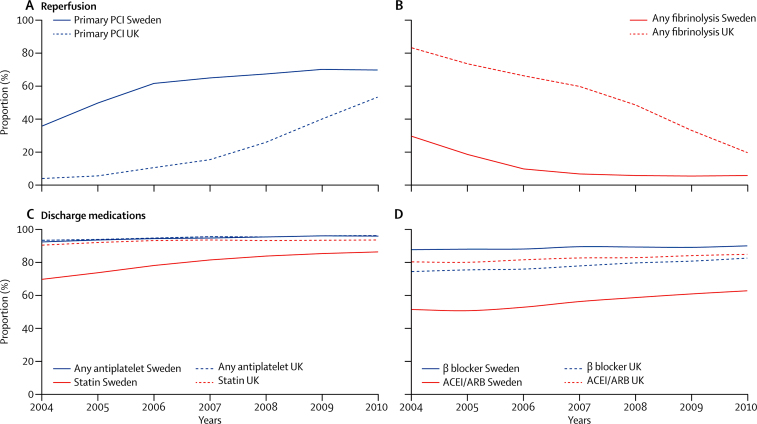
In both countries the use of primary PCI to treat STEMI increased over time and use of fibrinolysis decreased (figure 2, appendix p 20). In 2004, almost all STEMI patients in the UK received fibrinolysis, but this decreased substantially over time and use of primary PCI reached the Swedish 2004 rate in 2009. Over time, the use of any antiplatelet medication at discharge was similar in the two countries. Use of dual antiplatelet therapy at discharge was initially low in the UK but increased over time and had exceeded that in Sweden by 2009 (appendix p 20). Use of β blockers at discharge was constantly higher in Sweden, whereas use of ACE inhibitors or ARBs and use of statins were higher in the UK (figure 2).
Figure 2.
Use of reperfusion or fibrinolysis to treat STEMI and medication at discharge among all patients, by year
(A) Primary PCI and (B) fibrinolysis, including any given before admission or in hospital. (C) Any antiplatelet therapy and statin and (D) use of β blockers and ACEI or ARBs among all acute myocardial infarction patients who survived to discharge. STEMI=ST-segment-elevation myocardial infarction. PCI=percutaneous coronary intervention. ACEI=angiotensin-converting-enzyme inhibitor. ARB=angiotensin-receptor blocker.
Cumulative 30-day mortality was higher in the UK than in Sweden (figure 3). When assessed according to troponin concentrations, acute infarct severity (heart rate and blood pressure at admission), age, sex, year of admission, smoking, and diabetes status, 30-day mortality in the UK remained consistently higher than that in Sweden (table 2). The strength and direction of casemix-adjusted associations between 30-day mortality and age, year of admission, blood pressure, heart rate, diabetes status, history of cardiovascular disease, and previous revascularisation were similar in Sweden and the UK (appendix p 18). In-hospital mortality was also higher in the UK (8·8%, 8·7–8·9) than in Sweden (5·8%, 5·7–5·9). In clinically important subgroups, in-hospital mortality was consistently higher in the UK than in Sweden (appendix p 21).
Figure 3.
Kaplan-Meier curves for cumulative mortality at 30 days after admission with acute myocardial infarction in Sweden and the UK
*Time of censoring or vital status at 30 days missing for 129 patients in the UK.
Table 2.
30-day mortality in patients with acute myocardial infarction in Sweden and the UK, by clinically relevant subgroups
|
Number of deaths/patients |
30-day mortality (%, 95% CI) |
||||
|---|---|---|---|---|---|
| Sweden (n=119 786) | UK (n=391 077) | Sweden (n=119 786) | UK (n=391 077) | ||
| ST-segment elevation | |||||
| STEMI | 3248/37 937 | 17 681/15 7365 | 8·6% (8·3–8·8) | 11·2% (11·1–11·4) | |
| Non-STEMI | 5923/80 724 | 23 828/23 3586 | 7·3% (7·2–7·5) | 10·2% (10·1–10·3) | |
| Severity of myocardial infarction | |||||
| Troponin I (μg/L) | |||||
| <5·0 | 1487/29 793 | 5994/80 991 | 5·0% (4·7–5·2) | 7·4% (7·2–7·6) | |
| 5·0–9·9 | 484/6725 | 1670/17 524 | 7·2% (6·6–7·8) | 9·5% (9·1–10·0) | |
| 10·0–20·0 | 487/6256 | 1560/16 342 | 7·8% (7·1–8·5) | 9·5% (9·1–10·0) | |
| ≥20·0 | 1404/13 255 | 4630/40 765 | 10·6% (10·1–11·1) | 11·4% (11·1–11·7) | |
| Troponin T (μg/L) | |||||
| <0·2 | 724/12 846 | 2382/30 756 | 5·6% (5·3–6·0) | 7·7% (7·5–8·0) | |
| 0·2–0·5 | 598/10 263 | 2060/23 937 | 5·8% (5·4–6·3) | 8·6% (8·3–9·0) | |
| 0·5–1·0 | 559/7963 | 1674/17 774 | 7·0% (6·5–7·6) | 9·4% (9·0–9·9) | |
| ≥1·0 | 2453/22 921 | 6038/50 485 | 10·7% (10·3–11·1) | 12·0% (11·7–12·2) | |
| Admission systolic blood pressure (mm Hg) | |||||
| <110 | 2279/9729 | 10 532/47 796 | 23·4% (22·6–24·3) | 22·0% (21·7–22·4) | |
| 110–140 | 2882/31 750 | 13 331/123 072 | 9·1% (8·8–9·4) | 10·8% (10·7–11) | |
| ≥140 | 2732/62 743 | 11 406/166 274 | 4·4% (4·2–4·5) | 6·9% (6·7–7·0) | |
| Admission heart rate (beats per min) | |||||
| <90 | 4143/73 584 | 18 307/230 648 | 5·6% (5·5–5·8) | 7·9% (7·8–8·0) | |
| 90–120 | 2760/24 235 | 12694/82674 | 11·4% (11–11·8) | 15·4% (15·1–15·6) | |
| ≥120 | 1103/7933 | 4418/24 525 | 13·9% (13·2–14·7) | 18·0% (17·5–18·5) | |
| Demographic characteristics | |||||
| Male | 5069/75 406 | 22 549/25 4110 | 6·7% (6·5–6·9) | 8·9% (8·8–9·0) | |
| Female | 4102/43 255 | 18 823/135 608 | 9·5% (9·2–9·8) | 13·9% (13·7–14·1) | |
| Age | |||||
| <65 years | 717/35 262 | 4487/142 392 | 2·0% (1·9–2·2) | 3·2% (3·1–3·2) | |
| 65–75 years | 1385/29 859 | 7651/94 442 | 4·6% (4·4–4·9) | 8·1% (7·9–8·3) | |
| 75–85 years | 3731/36 324 | 16 288/101 943 | 10·3% (10–10·6) | 16·0% (15·8–16·2) | |
| ≥85 years | 3338/17 216 | 13 083/52 174 | 19·4% (18·8–20) | 25·1% (24·7–25·4) | |
| Year of admission | |||||
| 2004 | 1803/18 294 | 7300/55 447 | 9·9% (9·4–10·3) | 13·2% (12·9–13·4) | |
| 2005 | 1568/17 274 | 6842/54 421 | 9·1% (8·7–9·5) | 12·6% (12·3–12·9) | |
| 2006 | 1368/16 865 | 5966/52 757 | 8·1% (7·7–8·5) | 11·3% (11–11·6) | |
| 2007 | 1224/17 601 | 5547/53 276 | 7·0% (6·6–7·3) | 10·4% (10·2–10·7) | |
| 2008 | 1145/16 647 | 5505/55 851 | 6·9% (6·5–7·3) | 9·9% (9·6–10·1) | |
| 2009 | 1010/15 796 | 5237/58 479 | 6·4% (6–6·8) | 9·0% (8·7–9·2) | |
| 2010 | 1053/16 184 | 5112/60 720 | 6·5% (6·1–6·9) | 8·4% (8·2–8·6) | |
| Risk factors | |||||
| Diabetes | 2657/26 769 | 8444/65 424 | 9·9% (9·6–10·3) | 12·9% (12·7–13·2) | |
| No diabetes | 6371/91 275 | 29 647/307 409 | 7·0% (6·8–7·1) | 9·6% (9·5–9·7) | |
| Current smoker | 1086/24 651 | 5765/104 503 | 4·4% (4·2–4·7) | 5·5% (5·4–5·7) | |
| Non-smoker | 5939/82 205 | 26 463/249 814 | 7·2% (7–7·4) | 10·6% (10·5–10·7) | |
STEMI=ST-segment-elevation myocardial infarction.
After standardisation with the Swedish casemix model, UK mortality was lower than the unadjusted, crude estimates (appendix p 22). After standardisation, the forecast mean 30-day mortality between 2004 and 2010 was 7·7% (95% CI 7·3–8·2). If the same casemix was assumed in Sweden and the UK, the standardised mortality ratio was 1·37 (1·30–1·45), which corresponded to an estimated 11 263 (9620–12 827) more deaths in the UK between 2004 and 2010 than in Sweden. The greatest annual difference between countries in mortality was seen in 2004, when the standardised mortality ratio was 1·47 (1·38–1·58), but decreased significantly over time to 1·20 (1·12–1·29) in 2010 (figure 4). The propensity-matched analyses gave similar findings (appendix p 15). We explored the extent to which mortality differences between countries might be explained by differences in medical care, by casemix standardisation and treatment in hospital and also by estimating what might have differed if the UK had the same level of use of primary PCI and β blockers as Sweden from 2004 onwards, assuming treatment benefits reported in randomised clinical trials. If the level of use of primary PCI and β blockers had been the same in the UK as in Sweden, we estimate the standardised mortality ratio would have reduced from 1·37 to 1·31 (95% CI 1·30–1·33; appendix pp 22, 24). When in-hospital treatments were included in addition to casemix, the standardised mortality ratio decreased from 1·37 to 1·21 (1·15–1·29 appendix pp 22–23).
Figure 4.
30-day mortality of UK patients admitted in each study year, standardised according to the Swedish casemix model
p=0·01 for linear trend across years for the relative risks. AMI=acute myocardial infarction.
Discussion
We found greater mortality among patients with acute myocardial infarction in the UK than similar patients in Sweden. The differences in the care and outcomes of acute myocardial infarction are a cause for concern. Uptake of effective treatments, especially primary PCI to treat STEMI and β blockers at discharge, was slower in the UK than in Sweden. The greater cumulative 30-day mortality in the UK was much improved after standardisation with the Swedish casemix. This approach suggests that more than 10 000 deaths at 30 days would have been prevented or delayed had UK patients experienced the care of their Swedish counterparts.
Several lines of evidence support the validity of comparing care and outcomes across these registries. First, by design we captured data on the whole system in both countries (all hospitals and consecutive patients) and have used common data definitions. That these data are comparable is supported by our finding that the associations between casemix variables and mortality were similar in the two countries. Second, the diagnosis of acute myocardial infarction was comparable, with troponin values and propensity to make a diagnosis being similar. Third, differences in 30-day mortality between countries were consistent within strata defined by troponin values and other clinically important subgroups.
The use of primary PCI to treat STEMI in the UK lagged behind that in Sweden; the rate in 2010 in the UK (53%) was similar to that in Sweden in 2005 (50%). Primary PCI was more effective than fibrinolysis in a meta-analysis,28 and this finding was reflected in guideline recommendations in the USA in 2004,29 and in Europe in 2005.30 The UK did not have a national policy for primary PCI until October, 2008,31 which could explain the rapid increase in the use of this treatment from 2008 onwards, but it took until 2011–12 for rates to exceed 90%.32
The use of evidence-based secondary prevention showed a mixed pattern, with statin therapy and ACE inhibitors or ARBs being more commonly prescribed in the UK than in Sweden, whereas use of β blockers at discharge was more common in Sweden. β blockers have been reported to be efficacious for secondary prevention of acute myocardial infarction in randomised, controlled trials, and have been included in guideline recommendations for acute myocardial infarction in Europe33 and the USA34 since 1996, but their use was not recommended in the UK until 2001.35
Our findings suggest that these differences in clinical care contributed to international differences in patients' outcomes. The mortality gap between Sweden and the UK decreased over time, which is consistent with the narrowing gap between treatments. Application of Swedish rates of primary PCI and β blocker use to the UK population or inclusion of in-hospital treatments in the standardisation were associated separately with reduced differences in mortality between the two countries.
Other features of health care are not measured in these registries (eg, why particular patients do or do not receive particular types of care), and these features probably contribute to explaining the mortality gap. We show that improved understanding of selection processes in the two countries is needed (appendix p 23). Mortality might be affected by multiple unmeasured features of care, including doses, timing, adherence to drugs, differences in operator experience, shared and specialty care pathways, use of decision-support tools, and organisational culture.12
In all countries, patients, payers and policymakers could ask how outcomes in their health systems compare with our results. Policy initiatives are required to identify, understand, and reduce gaps between treatment use and outcomes in different health systems. We suggest that progress towards this goal is achievable because the narrowing of the gap between mortality in Sweden and the UK indicates that differences are reversible. Between-country comparisons of nationwide care and outcomes is a novel approach; most quality-outcome initiatives so far have been concentrated on within-country and within-system metrics. For Sweden our results highlight the value of quality of sustained, system-wide initiatives to improve quality, including the public reporting of outcomes at hospital level. For the UK our results suggest the usefulness of learning from systems that seem to be performing better.1, 2
Our study has several limitations. First, we cannot exclude the possibility that unmeasured features of casemix contributed to the differences in mortality. However, standardisation, stratification, and analysis of propensity scores all reported similar results, which supports an actual and significant difference between countries. Our casemix model is as comprehensive as the registries allow and included 17 variables in demography, acute myocardial infarction severity, risk factor, comorbidity, and prehospital treatment. Second, we could not assess the care received by patients who died before reaching hospital, although we believe this is unlikely to explain the higher mortality in the UK because the time from symptom onset to admission was similar to that in Sweden and differences in mortality became apparent after the first day in hospital. Third, the registries do not capture all patients admitted with acute myocardial infarction and, in the UK, missed patients are likely to be older and less likely to be under the care of a cardiologist than patients recorded in the registry.36 Because the nationwide registries in Sweden have been established longer than in the UK, missed cases might be less frequent in Sweden, which suggests the actual difference in mortality could be wider. Fourth, the quality and completeness of data (in themselves markers of quality of care) might introduce bias in our casemix model. In sensitivity analyses, however, estimates for the associations between casemix variables and 30-day mortality based on complete case analysis verified the results from multiple imputed data (appendix pp 18–19).
Our comparison of international outcomes suggests a novel research agenda (panel).37 First, additional patient-level health-care factors that are not measured might explain differences between countries. International harmonisation of detailed measures of quality of care in clinical registries, such as pathways of care, is needed. Second, at the national level, whether initiatives, such as national policies, financial incentives, organisation, and leadership, affect the delivery of care is unclear. Third, outcomes should be compared with those in other countries, such as France, Hungary, Poland, and the USA, through assessment of national, albeit voluntary, registries. Fourth, with linkage to national electronic health records, there are opportunities to extend comparisons to include ambulatory care before and after admission for heart attack, non-fatal events, and longer-term outcomes.38
Panel. Research in context.
Systematic review
We searched Medline via PubMed with the medical subject headings “myocardial infarction”, “Outcome Assessment (Health Care)”, and “internationality” and identified studies published in English from January, 1990 to September, 2013. Additional references from identified studies, reviews, or relevant citations provided by experts were manually checked to supplement the literature searches. We identified six closely relevant studies reporting substantial variation in the use and uptake of evidence-based medicine for care of acute myocardial infarction between countries.8, 9, 10, 11, 15, 16 These studies, however, were based on selected samples of hospital patients in voluntary registries,8, 9, 10 cross-sectional surveys,15 a clinical trial,16 or with only ST-segment-elevation acute myocardial infarction (STEMI)8, 9, 11 or non-STEMI.10 One study reported important between-countries differences in acute myocardial infarction mortality18 and the uptake of some evidence-based medicine. Our search revealed no previous studies comparing quality of care between two countries with nationwide coverage and taking into account heterogeneity in patients' casemix.
Interpretation
We found evidence of clinically important international differences in the uptake of effective treatments for and outcomes from AMI. 30-day mortality after AMI was higher among UK patients than among Swedish patients. Differences in mortality were not explained by differences in casemix, but were partly attributable to recorded differences in clinical care. International comparisons of care and outcome registries might yield important, actionable insights to guide health-care policy and clinical practice to improve the quality of health systems and prevent avoidable deaths from acute myocardial infarction.
We found clinically important differences in the care and outcomes of patients with acute myocardial infarction in Sweden and the UK. International comparisons of care and outcome registries might inform new research and policy initiatives to improve the quality of health systems.
This online publication has been corrected. The corrected version first appeared at thelancet.com on August 15, 2014
Acknowledgments
Acknowledgments
This study was done on behalf of the Swedish web-system for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies/The Swedish Register of Information and Knowledge about Swedish Health Intensive Care Admissions, the National Institute for Cardiovascular Outcomes Research/Myocardial Ischaemia National Audit Project, the Clinical Research Using Linked Bespoke Studies and Electronic Health Records programme, and the European Implementation Score project. This study was funded by the European Union Seventh Framework Programme for Research (CW, PH, and HH, grant 223153), National Institute for Health Research ([NIHR] AT and HH, grant RP-PG-0407–10314), Wellcome Trust (AT and HH, grant 086091/Z/08/Z), and the Medical Research Council Prognosis Research Strategy (PROGRESS) Partnership (AT and HH, grant G0902393/99558), and by awards to establish the Farr Institute of Health Informatics Research at UCL Partners, from the Medical Research Council, Arthritis Research UK, British Heart Foundation, Cancer Research UK, Chief Scientist Office, Economic and Social Research Council, Engineering and Physical Sciences Research Council, NIHR, National Institute for Social Care and Health Research, and Wellcome Trust. CW was supported by the NIHR Biomedical Research Centre at Guy's and St Thomas' National Health Service Foundation Trust and King's College London, funded by the NIHR. AT was supported by Barts and The London NIHR Cardiovascular Biomedical Research Unit, funded by the National Institute for Health Research. SJ, AJ, LW, and TJ were supported by the Swedish Heart and Lung Foundation. RG is employed at the Medical Products Agency in Sweden. The views expressed in this paper do not necessarily represent the views of the funding bodies.
Contributors
S-CC, RG, and ON analysed the data. All authors contributed to the preparation of the manuscript. TJ and HH oversaw the study and provided important scientific input, leadership, and collaboration in the study.
Conflicts of interest
We declare that we have no conflicts of interest.
Contributor Information
Tomas Jernberg, Email: tomas.jernberg@karolinska.se.
Harry Hemingway, Email: h.hemingway@ucl.ac.uk.
Supplementary Material
References
- 1.Coleman MP, Forman D, Bryant H, for the ICBP Module 1 Working Group Cancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995-2007 (the International Cancer Benchmarking Partnership): an analysis of population-based cancer registry data. Lancet. 2011;377:127–138. doi: 10.1016/S0140-6736(10)62231-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJ, Richards MA, Newton JN. UK health performance: findings of the Global Burden of Disease Study 2010. Lancet. 2013;381:997–1020. doi: 10.1016/S0140-6736(13)60355-4. [DOI] [PubMed] [Google Scholar]
- 3.Iglehart JK. Prioritizing comparative-effectiveness research—IOM recommendations. N Engl J Med. 2009;361:325–328. doi: 10.1056/NEJMp0904133. [DOI] [PubMed] [Google Scholar]
- 4.Wright RS, Anderson JL, Adams CD, for the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines 2011 ACCF/AHA focused update incorporated into the ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in collaboration with the American Academy of Family Physicians, Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;57:e215–e367. doi: 10.1016/j.jacc.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Kushner FG, Hand M, Smith SC., Jr 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54:2205–2241. doi: 10.1016/j.jacc.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 6.Gavalova L. Myocardial Ischaemia National Audit Project (MINAP) 2011 report. National Institute for Cardiovascular Outcomes Research; London: 2012. [Google Scholar]
- 7.Jernberg T, Johanson P, Held C, Svennblad B, Lindbäck J, Wallentin L, for the SWEDEHEART/RIKS-HIA Association between adoption of evidence-based treatment and survival for patients with ST-elevation myocardial infarction. JAMA. 2011;305:1677–1684. doi: 10.1001/jama.2011.522. [DOI] [PubMed] [Google Scholar]
- 8.Eagle KA, Goodman SG, Avezum A, Budaj A, Sullivan CM, López-Sendón J, for the GRACE Investigators Practice variation and missed opportunities for reperfusion in ST-segment-elevation myocardial infarction: findings from the Global Registry of Acute Coronary Events (GRACE) Lancet. 2002;359:373–377. doi: 10.1016/S0140-6736(02)07595-5. [DOI] [PubMed] [Google Scholar]
- 9.Widimsky P, Wijns W, Fajadet J, for the European Association for Percutaneous Cardiovascular Interventions Reperfusion therapy for ST elevation acute myocardial infarction in Europe: description of the current situation in 30 countries. Eur Heart J. 2010;31:943–957. doi: 10.1093/eurheartj/ehp492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yusuf S, Flather M, Pogue J, for the OASIS (Organisation to Assess Strategies for Ischaemic Syndromes) Registry Investigators Variations between countries in invasive cardiac procedures and outcomes in patients with suspected unstable angina or myocardial infarction without initial ST elevation. Lancet. 1998;352:507–514. doi: 10.1016/s0140-6736(97)11162-x. [DOI] [PubMed] [Google Scholar]
- 11.Laut KG, Gale CP, Lash TL, Kristensen SD. Determinants and patterns of utilization of primary percutaneous coronary intervention across 12 European countries: 2003–2008. Int J Cardiol. 2013;168:2745–2753. doi: 10.1016/j.ijcard.2013.03.085. [DOI] [PubMed] [Google Scholar]
- 12.Curry LA, Spatz E, Cherlin E. What distinguishes top-performing hospitals in acute myocardial infarction mortality rates? A qualitative study. Ann Intern Med. 2011;154:384–390. doi: 10.7326/0003-4819-154-6-201103150-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.White HD, Chew DP. Acute myocardial infarction. Lancet. 2008;372:570–584. doi: 10.1016/S0140-6736(08)61237-4. [DOI] [PubMed] [Google Scholar]
- 14.Levy AR, Mitton C, Johnston KM, Harrigan B, Briggs AH. International comparison of comparative effectiveness research in five jurisdictions: insights for the US. Pharmacoeconomics. 2010;28:813–830. doi: 10.2165/11536150-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 15.Schiele F, Hochadel M, Tubaro M. Reperfusion strategy in Europe: temporal trends in performance measures for reperfusion therapy in ST-elevation myocardial infarction. Eur Heart J. 2010;31:2614–2624. doi: 10.1093/eurheartj/ehq305. [DOI] [PubMed] [Google Scholar]
- 16.Kociol RD, Lopes RD, Clare R. International variation in and factors associated with hospital readmission after myocardial infarction. JAMA. 2012;307:66–74. doi: 10.1001/jama.2011.1926. [DOI] [PubMed] [Google Scholar]
- 17.Terkelsen CJ, Lassen JF, Nørgaard BL. Mortality rates in patients with ST-elevation vs. non-ST-elevation acute myocardial infarction: observations from an unselected cohort. Eur Heart J. 2005;26:18–26. doi: 10.1093/eurheartj/ehi002. [DOI] [PubMed] [Google Scholar]
- 18.Abildstrom SZ, Rasmussen S, Rosén M, Madsen M. Trends in incidence and case fatality rates of acute myocardial infarction in Denmark and Sweden. Heart. 2003;89:507–511. doi: 10.1136/heart.89.5.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Herrett E, Smeeth L, Walker L, Weston C, the MINAP Academic Group The Myocardial Ischaemia National Audit Project (MINAP) Heart. 2010;96:1264–1267. doi: 10.1136/hrt.2009.192328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jernberg T, Attebring MF, Hambraeus K. The Swedish Web-system for enhancement and development of evidence-based care in heart disease evaluated according to recommended therapies (SWEDEHEART) Heart. 2010;96:1617–1621. doi: 10.1136/hrt.2010.198804. [DOI] [PubMed] [Google Scholar]
- 21.Sweden National Board of Health and Welfare National guidelines for cardiac care. http://www%20socialstyrelsen%20se/nationellariktlinjerforhjartsjukvard (accessed Nov 12, 2013; in Swedish).
- 22.The National Archives Evaluation of the Coronary Heart Disease National Service Framework. http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/FreedomOfInformation/Freedomofinformationpublicationschemefeedback/FOIreleases/DH_126679 (accessed Nov 12, 2013).
- 23.Packer C, Simpson S, Stevens A, for the EuroScan: the European Information Network on New and Changing Health Technologies International diffusion of new health technologies: a ten-country analysis of six health technologies. Int J Technol Assess Health Care. 2006;22:419–428. doi: 10.1017/S0266462306051336. [DOI] [PubMed] [Google Scholar]
- 24.Carlsson P. Health technology assessment and priority setting for health policy in Sweden. Int J Technol Assess Health Care. 2004;20:44–54. doi: 10.1017/s0266462304000777. [DOI] [PubMed] [Google Scholar]
- 25.Flynn MR, Barrett C, Cosío FG. The Cardiology Audit and Registration Data Standards (CARDS), European data standards for clinical cardiology practice. Eur Heart J. 2005;26:308–313. doi: 10.1093/eurheartj/ehi079. [DOI] [PubMed] [Google Scholar]
- 26.Birkhead JS, Walker L, Pearson M, Weston C, Cunningham AD, Rickards AF, for the National Audit of Myocardial Infarction Project Steering Group Improving care for patients with acute coronary syndromes: initial results from the National Audit of Myocardial Infarction Project (MINAP) Heart. 2004;90:1004–1009. doi: 10.1136/hrt.2004.034470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thygesen K, Alpert JS, White HD, for the Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction Universal definition of myocardial infarction. Eur Heart J. 2007;28:2525–2538. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 28.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 29.Antman EM, Anbe DT, Armstrong PW, for the American College of Cardiology. the American Heart Association Task Force on Practice Guidelines. the Canadian Cardiovascular Society ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction) Circulation. 2004;110:e82–292. [PubMed] [Google Scholar]
- 30.Silber S, Albertsson P, Avilés FF, the Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology Guidelines for percutaneous coronary interventions. Eur Heart J. 2005;26:804–847. doi: 10.1093/eurheartj/ehi138. [DOI] [PubMed] [Google Scholar]
- 31.Improvement NHS. National roll-out of Primary PCI for patients with ST segment elevation myocardial infarction: an interim report. 2010. http://system.improvement.nhs.uk/ImprovementSystem/ViewDocument.aspx?path=Cardiac%2FNational%2FWebsite%2FReperfusion%2FInterim%20Report%20text%20final.doc.pdf (acccessed Jan 13, 2014).
- 32.National Health Service Growth of primary PCI for the treatment of heart attack patients in England 2008–2011: the role of NHS Improvement and the cardiac network. 2012. http://webarchive.nationalarchives.gov.uk/20130221101407/http://www.improvement.nhs.uk/LinkClick.aspx?fileticket=PWttejHG45M%3D&tabid=63 (accessed Jan 13, 2014).
- 33.The Task Force on the Management of Acute Myocardial Infarction of the European Society of Cardiology Acute myocardial infarction: pre-hospital and in-hospital management: The Task Force on the Management of Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 1996;17:43–63. doi: 10.1093/oxfordjournals.eurheartj.a014691. [DOI] [PubMed] [Google Scholar]
- 34.Ryan TJ, Anderson JL, Antman EM. ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction) J Am Coll Cardiol. 1996;28:1328–1428. doi: 10.1016/s0735-1097(96)00392-0. [DOI] [PubMed] [Google Scholar]
- 35.NICE . A prophylaxis for patients who have experienced a myocardial infarction. National Institute for Clinical Excellence; London: 2001. [Google Scholar]
- 36.Herrett E, Shah AD, Boggon R. Completeness and diagnostic validity of recording acute myocardial infarction events in primary care, hospital care, disease registry, and national mortality records: cohort study. BMJ. 2013;346:f2350. doi: 10.1136/bmj.f2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hemingway H, Croft P, Perel P, the PROGRESS Group Prognosis research strategy (PROGRESS) 1: a framework for researching clinical outcomes. BMJ. 2013;346:e5595. doi: 10.1136/bmj.e5595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Denaxas SC, George J, Herrett E. Data resource profile: cardiovascular disease research using linked bespoke studies and electronic health records (CALIBER) Int J Epidemiol. 2012;41:1625–1638. doi: 10.1093/ije/dys188. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.