Abstract
This prospective before‐and‐after survey of hypertensive patients visiting government‐run outpatient health facilities in the Yaroslavl Region of Russia assessed blood pressure (BP)–related endpoints following initiation of a comprehensive health system improvement program for hypertension. Two cross‐sectional surveys, one at baseline and the other approximately 1 year after program initiation, evaluated the primary measure of BP control rate. Secondary measures included mean BP levels and distribution, cardiovascular risk factors, and associated conditions, heart rate levels, and antihypertensive therapy. From the 2011 survey (n=1794) to the 2012 survey (n=2992), BP control rate (<140/90 mm Hg) significantly increased from 16.8% to 23.0%, reflecting a 37% relative improvement (P<.0001). Mean BP level was significantly reduced from 151/90 mm Hg to 147/88 mm Hg (P<.0001). Severe uncontrolled hypertension (systolic BP ≥180 mm Hg) was reduced from 9.7% to 6.4% (P<.0001). Implementing a guidelines‐based treatment protocol with medical and patient education programs resulted in physician behavior change and improved patient BP control.
Cardiovascular (CV) diseases remain the leading cause of mortality in Russia, accounting for 57% of all deaths.1 In 2010, the crude (non‐age and non‐sex standardized) mortality rate from all CV diseases in Russia was 805.9 per 100,000 population, mostly attributed to ischemic heart disease, and the mortality rate from cerebrovascular diseases was 260.4 per 100,000, mostly attributed to stroke. In some regions of Russia, such as Yaroslavl, there is an even higher CV disease mortality rate (1009.1 per 100,000).1
Hypertension is highly prevalent in Russia, affecting approximately 40% of adults. The hypertension control rate is estimated to be 24% of treated hypertensive patients and has been stable over the past 10 years (23.1% in 2003–2004).2 Notably, the prevalence of hypertension in Russia is substantially higher and control rates substantially lower compared with many other countries, including the United Kingdom (28% to 31% [prevalence] and 61% to 63% [control]),3 the United States (29% and 53%, respectively),4 and France (31% and 51%, respectively).5 In Canada, hypertension prevalence and control rates are estimated to be 22% and 66%, respectively.6 The 66% control rate reflects improvement over that reported in the 1990s (13%),7, 8 and the increase observed coincided with implementation of the country‐wide, evidence‐based Canadian Hypertension Education Program (CHEP).9 The CHEP was initiated in 2000 and includes 3 task forces: (1) a Clinical Recommendations Task Force that uses a rigorous and systematic process for developing recommendations, which are regularly updated; (2) an Implementation Task Force that develops recommendation summaries and highlights key prevention and control messages and strengthens the response by developing extensive partnerships and developing and disseminating materials tailored to various audiences; and (3) an Outcomes Research Task Force that assesses the success of the recommendations and identifies priority areas for further improvement.
Due to the role of hypertension as the major risk factor for total mortality, reducing the incidence and improving control of hypertension in Russia is imperative. To achieve this, a comprehensive health system improvement program for hypertension was undertaken in the Yaroslavl Region of Russia. This initiative was a joint program between clinicians, the Department of Health and Pharmacy of the Yaroslavl region, and Novartis, under the framework of the Memorandum of Understanding between the government of the Yaroslavl Region and Novartis Pharma LLC, Russia. A cross‐sectional survey evaluated blood pressure (BP) control rates among patients of general practitioners (GPs) and cardiologists of the Yaroslavl Region at baseline and then again a year after initiating the program.
Assessment of the Problem
A cross‐sectional survey was conducted to assess baseline BP control rates and medical practices.10 This was conducted over a period of 2 months (from May to June 2011). A total of 39 ambulatory institutions of the Yaroslavl Region healthcare system participated, including 180 physicians (154 GPs and 26 cardiologists). Physicians were asked to submit data from charts on 10 consecutive hypertension patients. All patients were at least 18 years of age, as the participating institutions were adult outpatient clinics. The following data were extracted: patients' history of hypertension, associated clinical conditions, BP and heart rate, use of antihypertensive therapy, and CV risk factors (including smoking, dyslipidemia, obesity, and family history of CV disease [Table]). No additional examinations, tests, interventions, or specific procedures were performed during data collection. Only medical data in the patient's outpatient record and obtained during a routine examination at the visit were recorded (anonymously) and analyzed. BP measurements were performed by participating physicians using the same methodology as in their regular clinical practice for the purpose of patient evaluation during the clinic visit. Most often, BP was assessed with manual aneroid sphygmomanometers, although no guidance or limitations on the types of devices used was provided. Patient diaries included more than 50 reported parameters, and physicians were unaware that the BP control parameter was the one of greatest interest.
Table 1.
Demographics, Hypertension History, and Patient Risk Factors, End Organ Disease, and Associated Clinical Conditions
| Characteristic | Year of Survey (Patients Surveyed, No.) | |
|---|---|---|
| 2011 (N=1794) | 2012 (N=2992) | |
| Men/women/not specified,% | 37/60/3 | 36/62/2 |
| Mean age, y | 60 | 59 |
| Patient distribution by age group (y),% | ||
| Younger than 50 | 19 | 22 |
| 50–59 | 34 | 30 |
| 60–69 | 25 | 26 |
| 70 and older | 23 | 22 |
| Patient population of working age, %a | 50 | 46 |
| Patient distribution by duration of hypertension and hospitalizations, % | ||
| ≤1 y | 18 | 17 |
| 2–9 y | 40 | 47 |
| ≥10 y | 42 | 36 |
| Patient distribution by risk factors, end organ disease, and associated clinical conditions, % | ||
| Left ventricular hypertrophy | 72 | 69 |
| Abdominal obesity | 54 | 48 |
| Dyslipidemia | 48 | 45 |
| Regular alcohol consumption | 37 | 36 |
| Family history of premature CVD | 33 | 36 |
| Current or previous smoker | 24 | 26 |
| Type 2 diabetes | 21 | 18 |
| Carotid artery changes | 17 | 17 |
| Peripheral artery disease | 6 | 3 |
| Diabetic nephropathy | 3 | 4 |
| Microalbuminuria | 3 | 4 |
| Heart diseases | 48 | 43 |
| Chronic heart failure | 38 | 29 |
| Angina pectoris | 29 | 22 |
| Myocardial infarction | 11 | 10 |
| Hypertensive retinopathy | 20 | 21 |
| Cerebrovascular diseases | 15 | 18 |
| Stroke | 6 | 7 |
| TIA | 6 | 8 |
Abbreviations: CVD, cardiovascular diseases; TIA, transient ischemic attack. aIn Russia, “working age” is defined as younger than 60 years for men and younger than 55 years for women.
The original sample size was based on an estimated BP control rate near the reported Russian average of 25%, with a 25% oversampling to ensure sufficient (80%) power for establishing the BP control rate within this population of known hypertensive patients. The survey was approved by the Department of Health and Pharmacy of the Yaroslavl Region and performed within the Memorandum of Understanding between the government of the Yaroslavl Region and Novartis Pharma LLC, Russia.
Results of the Baseline Assessment
A total of 1794 diaries (1525 from GPs; 269 from cardiologists) were analyzed.10 Demographic and baseline characteristics of this generally high‐risk patient population are reported in the Table. Most patients (97%) were prescribed antihypertensive therapy, with 83% prescribed >1 drug. The most frequently used agents included β‐blockers (50% of patients), angiotensin‐converting enzyme (ACE) inhibitors (49%), and diuretics (40%).10 Mean BP was 151/90 mm Hg and 17% of patients had normal BP (<140/90 mm Hg) (Figure 1). The distribution of patients' systolic BP (SBP) was 20% controlled (<140 mm Hg), 44% SBP 140 mm Hg to 159 mm Hg, 26% SBP 160 mm Hg to 179 mm Hg, and 10% SBP ≥180 mm Hg (Figure 2).
Figure 1.
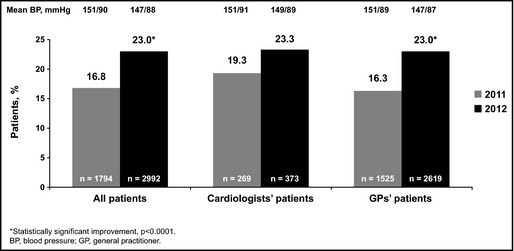
Blood pressure control rates (<140/90 mm Hg). BP indicates blood pressure; GP, general practitioner. *Statistically significant improvement, P<.0001.
Figure 2.
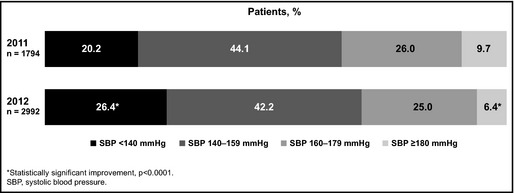
Patient distribution according to systolic blood pressure (SBP) level.
Strategy for Change
Our approach was a novel private‐government partnership engaging a variety of stakeholders. It was led by the Yaroslavl Department of Health but included input from Canadian Health Care Professionals involved in the CHEP and Novartis International's Healthcare Systems team. The program followed a structured approach of convening a cross‐sectoral steering committee to guide the project team through the various phases of health‐systems change, including a technical diagnostic‐phase assessment with an evaluation of root causes and the design and prioritization of potential interventions and improvements. This was followed by an implementation phase with regular reporting and performance‐management techniques. The program followed a similar approach to that used by the CHEP, where a central technical committee reviews the evidence‐based National Guidelines for the Diagnosis and Treatment of Hypertension11 and then makes specific recommendations for implementing the program8 (eg, medical and patient‐educational interventions) and for measuring and evaluating interventions and their impact (eg, BP control rate). The program also evaluated and suggested improvements in local clinical operating pathways (eg, concentrating care for hypertensive patients in specific clinics, establishing referral criteria for complex cases), performance measurement and management systems, and ways to improve the skills, mindsets, and behaviors of both clinicians and patients.
CHEP materials for patients, physicians, and other healthcare workers were made available for translation and cultural modification to reflect national differences. Many sections of the CHEP medical education materials for clinicians were translated and used to strengthen the Russian medical education program. In addition, CHEP patient education brochures and BP‐tracking logs were shared with clinicians and then translated and modified for use with Russian patients. CHEP clinicians visited the Yaroslavl Region, made on‐site observations, met with clinicians and Department of Health officials, and shared technical advice on how to implement effective medical education programs, as well as how to communicate the clinical evidence and overall importance of hypertension management in reducing CV‐ and all‐cause mortality. Specific “best practice” examples were shared with the Yaroslavl Department of Health and key institutions in terms of setting up a patient registry that identified and tracked patients with hypertension and the high‐priority modifiable CV risk factors. This database was eventually used to monitor and report clinic‐specific BP control rates on a quarterly basis, allowing the Department of Health to target medical education initiatives and small‐group clinical discussions to those sites performing below the mean. The program is ongoing, and continues to be modified and adapted.
A variety of interventions were explored that addressed physician knowledge, attitudes and practices, clinical staffing and patient throughput measures, patient education, coaching and adherence support programs, general public awareness, and lifestyle modification programs. These were then prioritized and sequenced by the Steering Committee. Interventions were approved by the Department of Health of Yaroslavl Region.
Specific aspects of the program included: (1) making hypertension a priority for the Yaroslavl Region by setting up a high‐level Steering Committee to oversee the project (ie, coordinating and evaluating the impact of interventions) and by creating a regional Center of Excellence for Hypertension to make organizational and methodological improvements and monitor progress; (2) focusing first on improving BP treatment by agreeing on a target for BP control and then measuring and monitoring site‐level hypertension and BP control rates, developing a simplified protocol of hypertension treatment (based on 2010 Russian National Hypertension Guidelines),11 and communicating this information to physicians via an intensive educational program, targeted in the first year at GPs. Cardiologists were excluded from the initial wave of the program because they see a minority of patients in the Yaroslavl Region, and they had reported better BP control rates than GPs, despite seeing more complex cases. The educational program consisted of a series of small‐group, case‐based discussions led by local clinical experts that addressed the barriers to care and built clinicians' context‐specific knowledge of evidence‐based guidelines, individualized treatment selection, and how to support patients getting to their BP‐treatment goal; and (3) increasing community awareness, engagement, adherence and persistence with therapy, and the rate of hypertension diagnosis through a public‐education campaign.
In early 2012, three “improvement” pilot sites were also selected by the Order of the Department of Health to not only implement the treatment protocol but also to trial other interventions including a manual tracking and call‐back system for patients with hypertension (especially those with poor BP control or who were at higher risk), as well as measurement and self‐reporting of clinic‐level BP control rates on a quarterly basis.
The program operated under the oversight of a formal Steering Committee with monthly meetings chaired by the Department of Health and Pharmacy of the Yaroslavl Region and involving the Regional Chief Specialists in Cardiology and General Medicine. Novartis personnel provided project‐management support as well as nonbranded medical education materials and lessons learned from international best practice case examples.
Effects of Change
A second cross‐sectional survey was conducted from May to July 2012, 13 months after the baseline survey and after approximately 6 months of intensive interventions. Physicians were asked to provide data on 15 consecutive hypertension patients. A total of 38 ambulatory institutions of the Yaroslavl Region healthcare system participated in the second survey, with 2992 diaries (2619 from GPs; 373 from cardiologists) analyzed. The apparent loss of one participating institution after the first survey was the result of an administrative restructuring in 2012, which resulted in two institutions to be considered as one. Although the same methodology and sampling were used in both surveys, the sample size was augmented in the second survey to increase the power for estimating the BP control rate at individual sites and to be able to adjust for any increase in newly diagnosed patients being included in the sample as a result of physician‐ and public‐awareness campaigns. This was conducted as a site‐based cross‐sectional survey to align it with other population‐based surveys that similarly track BP control rates over time. Because of this methodology, although most participating physicians were the same, patients and some physicians in the two surveys were not necessarily identical.
The patient population of the second survey was similar to that of the first (Table). Most patients (90%) were prescribed antihypertensive therapy, and 71% were prescribed >1 drug. The most frequently used agents included β‐blockers (45% of patients), ACE inhibitors (43%), and diuretics (32%). The slight decrease in the relative frequency of antihypertensive therapy utilization compared with 2011 (90% vs 97%) can be explained by the increased sample size and execution of the program, with more awareness leading to more newly diagnosed patients being included in the sample.
Compared with the first survey, mean BP in the second survey showed a significant decrease to 147/88 mm Hg (P<.0001). Goal BP (<140/90 mm Hg) was found in 23% of patients, demonstrating a statistically significant increase from the baseline survey (P<.0001) and a 37% relative improvement (Figure 1). The distribution of patients' SBP was: (1) 26% controlled (<140 mm Hg); (2) 42% SBP 140 mm Hg to 159 mm Hg; 25% SBP 160 mm Hg to 179 mm Hg; and (3) 6% SBP ≥180 mm Hg, demonstrating a statistically significant increase in the percentage of patients with SBP <140 mm Hg and a statistically significant decrease in the percentage of patients with SBP ≥180 mm Hg (ie, severe uncontrolled hypertension) (both P<.0001; Figure 2).
Although our data demonstrated that the general approach to drug therapy did not substantively change from the first to the second survey (factoring in the larger sample size of the second survey), an increase in volume of antihypertensive prescriptions filled for patients in the Yaroslavl Region was reported in an IMS database (Figure 3) (unpublished data sourced from an IMS database subscription accessible to the authors [www.imshealth.com]). Thus, it is possible that an increase in the antihypertensive therapy volume growth may be associated with improved patient adherence to prescribed therapy, likely caused by patient‐education efforts, including use of control logs to track BP, hypertension education leaflets, and physician‐directed patient education. These approaches could be important contributors to the improved BP control rate seen in our second survey.
Figure 3.
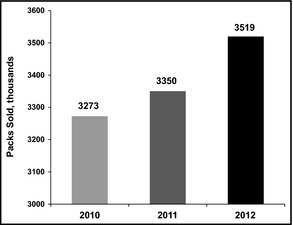
Volume of antihypertensive therapies dispensed (retail channel), Yaroslavl Region 2010–2012. Source: IMS Health Database accessed March 2013 (from author subscription).
Of note, during the years following initiation of the Canadian program (CHEP), improved compliance, as measured by evaluation of prescription databases and by a patient self‐report survey (ie, the Survey of Living With Chronic Diseases in Canada, hypertension module), was also found.12, 13 Importantly, improved adherence to antihypertensive therapy not only results in better BP control but has also been shown to have a positive effect on reducing hospitalization rates and overall medical costs.14, 15, 16, 17 Conversely, poor adherence and persistence increases hypertension complications risks, such as stroke (estimated 28% increased risk) and myocardial infarction (estimated 15% increased risk).14, 15, 16, 17
Discussion
Hypertension is a global issue, with the World Health Organization including it as one of the few priority recommendations in their Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020.18 A recent global survey of current hypertension management practices found substantial consistency across the 31 participating countries (including Russia).19 This survey found that almost all countries extensively use ACE inhibitors, angiotensin receptor blockers, calcium channel blockers, and diuretics, with β‐blockers no longer regarded as first‐line drugs.19 This is in contrast to what was found in our prior evaluation of hypertensive medication use in the Yaroslavl Region, with β‐blockers being the most frequently prescribed treatment (in 50% of patients), along with ACE inhibitors (in 49% of patients).10
Much has been studied and written regarding clinical improvement initiatives in other countries and also in demonstrating the correlation between improved management of hypertension and reduced rates of CV‐related mortality.6, 7, 8, 9, 20 Many studies have also clearly laid out the excess morbidity and mortality in Russia and the disproportionate burden caused by CV disease.21, 22, 23, 24, 25, 26 Relatively little has been published regarding clinical improvement initiatives in Russia beyond documentation of changes over time in BP epidemiology and control.2 Interestingly, the role of hypertension as a major modifiable determinant of poor health in Russia has been previously reported, with a clinic‐based program demonstrating a modest decrease in BP in 192 patients. However, the authors concluded that an effort beyond the clinic was needed.27
This project identified some of the root causes for poor hypertension management in a region of Russia. Some of the key root causes identified for the low rate of BP control initially measured included: (1) lack of awareness in front‐line clinics of evidence‐based guidelines for BP diagnosis and management; (2) no BP control target set or communicated to health workers; (3) BP control rate by clinician or clinic was not measured or reported; and (4) patients not understanding the value of controlling hypertension. We were then able to design a custom purpose improvement program for the Region, taking many elements of other hypertension and chronic disease management programs, aligning them with local guidelines, and effectively applying them in a typical Russian setting. Our experience in the Yaroslavl Region demonstrates that implementing a guidelines‐based treatment protocol and a small‐group, case‐based, medical education campaign specifically targeted to GPs, along with site‐specific patient tracking and monitoring of BP control rates with feedback, may be associated with improvements in hypertension control. Some of the benefits may have been related to improved patient engagement through physician counseling, as well as educational materials and self‐monitoring and recording of BP levels. During the course of the project, we gathered additional third‐party data indicating increased use of antihypertensive therapies that coincides with the improved BP control rates. The addition of a basic monitoring and evaluation system was effective in measuring and reinforcing the impact of the program. While we are pleased to report the progress made and our results to date, we acknowledge that region‐wide improvement in addressing the significant CV disease and all‐cause mortality risk factors of hypertension will take sustained effort over many years.
Limitations
Limitations in the methodological approach include the potential for selection bias (as selection for patient diaries was sequential and not random) and observation bias (as physicians self‐reported BP control measures). This study approach was taken in a relatively resource‐constrained health system but was partially mitigated by requiring that a prespecified number of consecutive patients be included and also by sampling a significant proportion of physicians and clinics within the region. Although it would have been ideal if both surveys included the same patients, the cross‐sectional, population‐based approach that we took is common,28, 29 and is an economical way to collect large amounts of data from a large number of patients.
There was also difficulty in measuring individual patient adherence and persistence to behavioral modification and medications because the surveys were cross‐sectional and not cohort‐based. Another limitation is the dissociation between information collected for medical records, prescriptions written, and prescriptions filled for each patient, which made it very difficult to track physician‐prescribing practices and to evaluate the impact of individual patient‐level dosing and adherence or persistence with therapy. Additional challenges encountered included high physician turnover and low staffing levels at some sites (as reported via informal communications from the regional Department of Health officials to the authors).
Currently, this program is being expanded and “scaled up” across the other clinics of the Yaroslavl Region, with lessons learned in pilot sites and in the Yaroslavl Region being shared with the Federal Ministry of Health and other interested regional governments across Russia through presentation of these data at national congresses and conferences on CV diseases. Although this program is still relatively early in its development, particularly when set against the historical background of the enormous burden of CV disease in Russia, we are encouraged by the magnitude and pace of improvement in a leading indicator of better CV disease risk management. Therefore, we posit that if the improved BP control rates continue to be observed and improve further, then a similar structured approach to improving the diagnosis and treatment of hypertension could be applied nationwide on a region‐by‐region basis. Additionally, a similar approach could be applied to other diseases—particularly those with similar characteristics (eg, more common, noncommunicable diseases with a robust body of knowledge such as evidence‐based guidelines and where a track record of performance improvement over time [eg, CHEP] is available). A similar approach could be tailored to the Russian situation and then implemented by Regional Departments of Health across Russia.
Additional studies should look at how to accelerate the pace of change and also more clearly define patient and/or geographic subsets to identify ways to more effectively engage with patient and/or clinician subgroups to optimize and tailor behavioral interventions to more effectively and rapidly improve the BP control rate. We also believe there would be value in extending the interventions to include better diagnosis and treatment of other known CV risk factors with the end goal of reducing the burden of CV disease and improving survival and quality of life.
In addition to scaling up and implementing the described initiatives region‐wide, lessons learned from the CHEP suggest that engaging more stakeholders could help reach even higher levels of sustained BP control. It is hoped that further improvements may be achieved, such as those seen across the Kaiser Permanente network where BP control rates of >80% have been reported in California.30 The third annual regional cross‐sectional survey is being conducted in 2013 and will provide general and detailed clinic‐by‐clinic analysis of the implemented changes at the end of the program.
Conclusions
A guidelines‐based approach to hypertension can be effectively applied to improve BP control by setting a specific BP control target that is crucial for changing the mindsets and attitudes of physicians and healthcare systems. Measuring and reporting results and progress will be key components of tracking system performance and reinforcing change and improvements in clinics. It is likely that aspects of our comprehensive health system improvement program and Canada's education program (CHEP) can be used to guide the development of successful hypertension programs in other parts of Russia and the world.
Disclosure
Maria Mozheyko has received lecturer's honoraria and travel support and participated in research conducted by Novartis Pharma LLC Russia. Sergey Eregin has received lecturer's honoraria and travel support from Novartis Pharma LLC Russia. Alexey Vigdorchik is an employee of Novartis Pharma LLC, Russia. Sheldon Tobe has received lecturer's honoraria and travel support from Novartis Pharma LLC Russia. Norman Campbell has received travel support from Novartis Pharma LLC Russia. Farhad Riahi is an employee of Novartis International AG, Switzerland. David Hughes is an employee of Novartis International AG, Switzerland. These surveys were initiated by the Department of Health and Pharmacy of Yaroslavl Region, designed and reviewed by all authors, conducted by the International Institute for Market Research GFK Rus, and funded by Novartis International AG, Basel, Switzerland. Editorial assistance was provided by Fran Karo, PhD, CMPP, of Oxford PharmaGenesis, for her help in editing and preparing the manuscript for submission. Editorial assistance was funded by Novartis International AG, Basel.
Author Contributions
All authors had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. The draft manuscript was prepared by David Hughes and Alexey Vigdorchik with input from Maria Mozheyko, Sergey Eregin, Sheldon Tobe, Norman Campbell, and Farhad Riahi.
Acknowledgements
The authors would like to thank Olga Chernichenko, Andrey Karasev, and Ekaterina Germanova of International Institute for Market Research GFK Rus for assistance in planning, conducting, and preliminary analysis of these surveys. The medical interventions are consistent with Russia National Guidelines and accepted medical practice and approved by the Department of Health and Pharmacy of Yaroslavl Region. According to the policy regarding activities that constitute research at the Department of Health and Pharmacy of Yaroslavl Region this work met criteria for operational improvement activities and was exempt from ethics review.
J Clin Hypertens (Greenwich). 2013;15:918–924. DOI: 10.1111/jch.12214. ©2013 Wiley Periodicals, Inc.
References
- 1. Russian Federal Service of State Statistics . Healthcare in Russia [Russian]. 2011. Russia: http://www.gks.ru/bgd/regl/b11_34/IssWWW.exe/Stg/d01/01-86.htm; Yaroslavl: http://www.gks.ru/bgd/regl/b11_34/IssWWW.exe/Stg/d01/01-94.htm. Accessed March 18, 2013.
- 2. Oganov RG, Timofeeva TN, Koltunov IE, et al. Arterial hypertension epidemiology in Russia; the results of 2003–2010 federal monitoring. Cardiovasc Ther Prev. 2011;10:9–13. [Google Scholar]
- 3. The Health and Social Care Information Centre . Hypertension. In: Health Survey for England 2011: Health, Social Care and Lifestyles: Summary of Key Findings. Leeds, UK: The Health and Social Care Information Centre; 2012:1–34. [Google Scholar]
- 4. Yoon SS, Burt V, Louis T, Carroll MD. Hypertension Among Adults in the United States, 2009–2010. NCHS data brief, no 107. Hyattsville, MD: National Center for Health Statistics. 2012. [PubMed] [Google Scholar]
- 5. Godet‐Mardirossian H, Girerd X, Vernay M, et al. Patterns of hypertension management in France (ENNS 2006–2007). Eur J Prev Cardiol. 2012;19:213–220. [DOI] [PubMed] [Google Scholar]
- 6. Wilkins K, Campbell NRC, Joffres MR, et al. Blood pressure in Canadian adults. Health Rep. 2010;21:37–46. [PubMed] [Google Scholar]
- 7. Joffres MR, Hamet P, MacLean DR, et al. Distribution of blood pressure and hypertension in Canada and the United States. Am J Hypertens. 2001;14(11 Pt 1):1099–1105. [DOI] [PubMed] [Google Scholar]
- 8. Campbell NR, Chen G. Canadian efforts to prevent and control hypertension. Can J Cardiol. 2010;26(Suppl C):14C–17C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Campbell NR, Brant R, Johansen H, et al. For the Canadian Hypertension Education Program Outcomes Research Task Force . Increases in antihypertensive prescriptions and reductions in cardiovascular events in Canada. Hypertension. 2009;53:128–134. [DOI] [PubMed] [Google Scholar]
- 10. Mozheyko M, Eregin S, Vigdorchik A, et al. A cross‐sectional survey of hypertension diagnosis and treatment practices among primary care physicians and cardiologists of Yaroslavl Region in Russia. Adv Ther. 2012;29:1016–1025. [DOI] [PubMed] [Google Scholar]
- 11. Chazova IE, Ratova LG, Boytsov SA, et al. For the Experts Committee, Russian Medical Society of Hypertension and Russian Scientific Society of Cardiology . Diagnostics and treatment of arterial hypertension. Russian Guidelines (4th review): Systemic Hypertension. 2010;3:5–26.
- 12. Gee ME, Campbell NR, Gwadry‐Sridhar F, et al. Antihypertensive medication use, adherence, stops, and starts in Canadians with hypertension. Can J Cardiol. 2012;28:383–389. [DOI] [PubMed] [Google Scholar]
- 13. Friedman O, McAlister FA, Yun L, et al. Antihypertensive drug persistence and compliance among newly treated elderly hypertensives in Ontario. Am J Med. 2010;123:173–181. [DOI] [PubMed] [Google Scholar]
- 14. Yiannakopoulou E, Papadopulos J, Cokkinos D, et al. Adherence to antihypertensive treatment: a critical factor for blood pressure control. Eur J Cardiovasc Prev Rehabil. 2005;12:243–249. [DOI] [PubMed] [Google Scholar]
- 15. Sokol M, McGuigan K, Verbrugge R, et al. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. [DOI] [PubMed] [Google Scholar]
- 16. Breekveldt‐Postma N, Penningvan‐Beest FJA, Siiskonen SJ, et al. Effect of persistent use of antihypertensives on blood pressure goal attainment. Curr Med Res Opin. 2008;24:1025–1031. [DOI] [PubMed] [Google Scholar]
- 17. Elliott WJ. Improving outcomes in hypertensive patients: focus on adherence and persistence with antihypertensive therapy. J Clin Hypertens (Greenwich). 2009;11:376–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Health Organization Executive Board . Draft action plan for the prevention and control of noncommunicable diseases 2013–2020. 11 January 2013. http://apps.who.int/gb/ebwha/pdf_files/EB132/B132_7-en.pdf. Accessed August 19, 2013.
- 19. Chalmers J, Arima H, Harrap S, et al. Global survey of current practice in management of hypertension as reported by societies affiliated with the International Society of Hypertension. J Hypertens. 2013;31:1043–1048. [DOI] [PubMed] [Google Scholar]
- 20. Moser M. Hypertension treatment–a success story. J Clin Hypertens (Greenwich). 2006;8:313–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shkolnikov V, Meslé F, Leon DA. Premature cardiovascular mortality in Russia in the light of population‐ and individual‐level evidence. In: Weidner G, Kopp SM, Kristenson M, eds. Heart Disease: Environment, Stress and Gender. Nato Science Series, Series I: Life and Behavioural Sciences, vol. 327. Amsterdam: NATO; 2001:39–68. [Google Scholar]
- 22. Shkolnikov VM, Andreev EM, Leon DA, et al. Mortality reversal in Russia: the story so far. Hygiea Internationalis. 2004;4:29–80. [Google Scholar]
- 23. Roberts B, Stickley A, Balabanova D, et al. Irregular treatment of hypertension in the former Soviet Union. J Epidemiol Community Health. 2010;66:482–488. [DOI] [PubMed] [Google Scholar]
- 24. Roberts B, Stickley A, Balabanova D, et al. The persistence of irregular treatment of hypertension in the former Soviet Union. J Epidemiol Community Health. 2012;66:1079–1082. [DOI] [PubMed] [Google Scholar]
- 25. Grassi G, Cifkova R, Laurent S, et al. Blood pressure control and cardiovascular risk profile in hypertensive patients from central and eastern European countries: results of the BP‐CARE study. Eur Heart J. 2011;32:218–225. [DOI] [PubMed] [Google Scholar]
- 26. Rechel B, Roberts B, Richardson E, et al. Health and health systems in the Commonwealth of Independent States. Lancet. 2013;381:1145–1155. [DOI] [PubMed] [Google Scholar]
- 27. Greenberg HM, Galyavich AS, Ziganshina LE, et al. Identification and management of patients with hypertension in the polyclinic system of the Russian Federation. Am J Hypertens. 2005;18:943–948. [DOI] [PubMed] [Google Scholar]
- 28. Cutler JA, Sorlie P, Wolz M, et al. Trends in hypertension prevalence, awareness, treatment, and control rates in the United States between 1988–2004 and 1999–2004. Hypertension. 2008;52:818–827. [DOI] [PubMed] [Google Scholar]
- 29. Cifkova R, Skodova Z, Bruthans J, et al. Longitudinal trends in major cardiovascular risk factors in the Czech population between 1985 and 2007/8. Czech MONICA and Czech post‐MONICA. Atherosclerosis. 2010;211:676–681. [DOI] [PubMed] [Google Scholar]
- 30. Jaffe MG, Young JD. The Permanente Medical Group. The Kaiser Permanente Northern California Hypertension Project 2001–2009: how an integrated care delivery system increased blood pressure control rates from 44% to 80% in 8 years. [abstract OR‐13.]. J Clin Hypertens (Greenwich). 2011;13(Suppl 1):A6. [Google Scholar]


