Abstract
Fear arousal—vividly showing people the negative health consequences of life-endangering behaviors—is popular as a method to raise awareness of risk behaviors and to change them into health-promoting behaviors. However, most data suggest that, under conditions of low efficacy, the resulting reaction will be defensive. Instead of applying fear appeals, health promoters should identify effective alternatives to fear arousal by carefully developing theory- and evidence-based programs. The Intervention Mapping (IM) protocol helps program planners to optimize chances for effectiveness. IM describes the intervention development process in six steps: (1) assessing the problem and community capacities, (2) specifying program objectives, (3) selecting theory-based intervention methods and practical applications, (4) designing and organizing the program, (5) planning, adoption, and implementation, and (6) developing an evaluation plan. Authors who used IM indicated that it helped in bringing the development of interventions to a higher level.
Keywords: Fear appeals, Intervention Mapping, Program planning, Health promotion
Fear arousal—vividly showing people the negative health consequences of life-endangering behaviors— has been suggested as a method to raise awareness of risk behaviors and to change them into health-promoting behaviors. Using fear may be intuitively appealing to the health promoter, and research on fear-arousing communication has a long tradition in social psychology and public health education. Most relevant theories and the available empirical data suggest that fear, as a result of subjective appraisals of personal susceptibility and severity, motivates an individual to action. However, a person's self-efficacy and outcome expectations moderate the type of action (protection motivation theory, Norman, Boer, & Seijdel, 2005; health belief model, Champion & Skinner, 2008; health action process approach, Schwarzer, 2008; extended parallel process model, Ruiter, Kessels, Peters, & Kok, 2014, this issue; Witte, Meyer, & Martell, 2001; I-change model, De Vries, Mesters, Van de Steeg, & Honing, 2005). For instance, smokers may become afraid of cancer when they recognize their own susceptibility to cancer and the severity of the disease. Their fear may motivate them to stop smoking, but only when they are convinced that quitting is really effective in preventing cancer (response efficacy or outcome expectation) and when they feel confident that they are able to quit (self-efficacy). In this particular example, low self-efficacy may be the most important barrier to quitting for most smokers. The meta-analysis by Peters, Ruiter, & Kok (2013) supports these theoretical predictions.
What happens when people are threatened but they are not convinced of their self-efficacy or of the effectiveness of the alternative behavior? Most data suggest that, under those conditions, the resulting behavior may be defensive, more oriented toward avoidance of the anti-smoking fear message than action to quit smoking (Albarracín et al., 2005; De Hoog, Stroebe, & De Wit, 2007; Earl & Albarracín, 2007; Floyd & Prentice-Dunn, 2000; Milne, Orbell, & Sheeran, 2002; Peters et al., 2013; Ruiter, Abraham, & Kok, 2001; Ruiter et al, 2014, this issue; Witte & Allen, 2000). Messages that arouse extreme fear may cause people to deny cancer risks and may inadvertently result in more smoking (Brown & Smith, 2007).
What does this mean for the use of fear-arousing communication as a theory-based behavior change method? First, fear is a potential motivator of behavior change. Second, fear can stimulate health-promoting behavior; however, this effect is more likely if the individual has high outcome and self-efficacy expectations. In cases in which people are not aware of their risk, some confrontation with undeniable negative consequences of the risky behavior may be effective, but that message does not have to be emotionally arousing (De Hoog et al., 2007). When people are aware of their risk but lack self-efficacy for engaging in a health-promoting alternative behavior, messages should focus on improving self-efficacy—which is easier said than done (Ruiter & Kok, 2012).
Peters, Ruiter, & Kok (2014, this issue) report on a qualitative study of fear appeal effectiveness beliefs among intervention developers, policymakers, politicians, scientists and advertisers. They observe that interviewees who were closer to actual intervention development often had a general idea that there was something wrong with inducing fear (though they rarely grasped the underlying dynamics). Interviewees who were further removed from the intervention development activities often did not have this basic heuristic belief. Peters et al. conclude that intervention developers should be better trained in, and more insistent on (1) performing adequate determinant analyses, (2) applying theory- and evidence-based behavior change methods, and (3) convincing their managers and collaborating organizations to implement well-planned alternatives to fear appeals. Godin Gagnon, Alary, Levy, & Otis (2007), in a study analyzing the quality of program planning of 50 funded community-based health promotion projects in Canada, also observed a lack of careful determinant analyses and insufficient use of theories in program development. Finally, risk perception is rarely a major determinant of behavior (Hospers & Kok, 1995; Peters et al., 2013); most relevant generic theories of behavior and behavior change do not mention risk perception as a separate determinant (McAlister, Perry, & Parcel, 2008; Montaño & Kasprzyk, 2008).
We agree with Ruiter et al. (2014, this issue):
Current evidence shows that information about the severity of possible negative consequences from risk behavior may prompt defensive responses. These counterproductive responses may be avoided by providing instruction on how to successfully implement the recommended actions as well as convincing people that they are personally susceptible to the threat.
In the following we will describe a program planning protocol, Intervention Mapping (IM), which can guide the program planner to optimize chances for effectiveness and, among others, finding effective alternatives for fear appeals.
INTERVENTION MAPPING
IM was developed as a program planning framework for the development of theory- and evidence-based health promotion interventions (Bartholomew, Parcel, Kok, Gottlieb, & Fernández, 2011). IM provides guidelines and tools for the empirical and theoretical foundation of health promotion programs, for the application of theory, for the translation of theory into actual intervention activities and materials, for the management of program adoption and implementation, and for the collaboration between health educators, researchers, priority groups and stake-holders. IM enables health promoters to develop interventions that include theory-based intervention strategies and materials that may accomplish program objectives, and that match priority populations and intervention contexts.
IM guides program planners to map the path of intervention development from recognizing a need or problem to testing solutions. It describes the intervention development process in six steps (see Table 1). In everyday language (Schaalma & Kok, 2009): (1) What is the problem? What are the causes? Who are those at risk? What are the resources for change? (2) What does the program planner need to change, and why? (3) How can these changes be accomplished with theory- and evidence-based methods that can be expected to work? (4) How can the methods be delivered in a way that makes sense and will be implemented? (5) How can we facilitate sustained implementation? (6) Did the program work out the way we planned?
TABLE 1.
Intervention Mapping steps and tasks (Bartholomew et al., 2011)
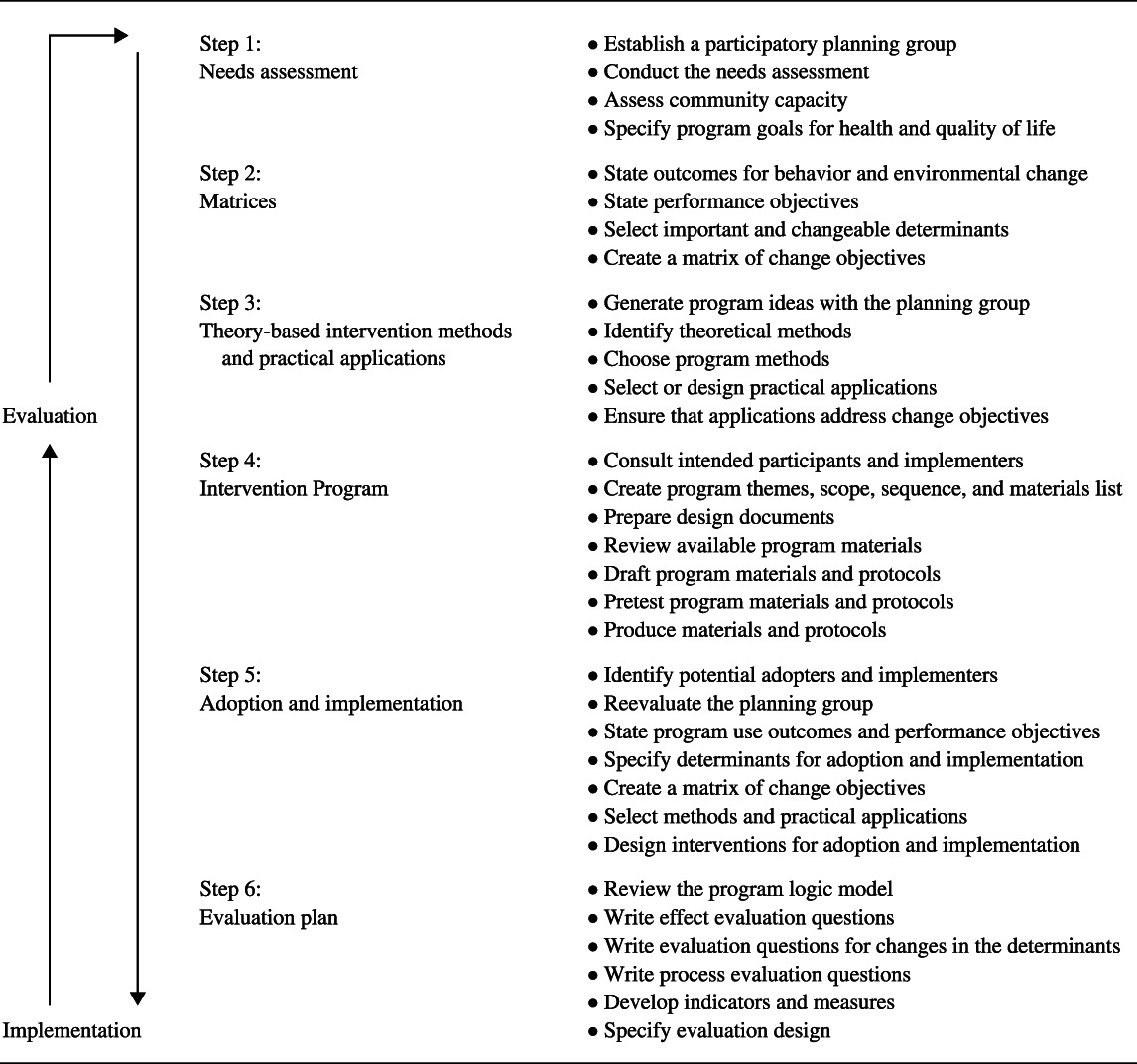
IM describes the iterative path from problem identification to problem solving or mitigation. Each of the six steps comprises several tasks, and completing of the tasks in a step creates a foundation for the subsequent step. The completion of all of the steps serves as a blueprint for designing, implementing and evaluating an intervention based on a foundation of theoretical, empirical and practical information. Table 1 shows the six steps and related tasks of the IM process.
An IM approach is characterized by four perspectives that are applied during the entire program planning process and in all steps (Bartholomew et al., 2011). From a participation perspective, the framework suggests that the priority population and program implementers should be involved in all aspects of decision making to make sure that the program is based on the needs of the community. From a multi-theory perspective, IM stimulates an eclectic use of theories. Because theories are by definition abstractions of reality, and therefore explain only part of it, IM suggests that real-life problems should be approached from multiple theories (Buunk & Van Vugt, 2008). From a systems perspective, interventions are seen as events occurring in systems, with other factors within a system possibly reinforcing or dampening the influence of an intervention on the target behavior or environmental change. Finally, from an ecological perspective, planning with IM recognizes the relevance of social and physical environmental conditions that influence behaviors. These social and physical environmental conditions may have a much stronger impact on the target behavior than individual-related factors (Kok, Gottlieb, Commers, & Smerecnik, 2008).
In this paper, we focus on IM Steps 2, 3, 4, and 5 because they are most relevant for the main question of this paper: what are alternatives to fear appeals? We assume that in conducting Step 1 the program planner will focus on the analysis of the problem behaviors and environmental conditions and will have no reason to be focusing on intervention. Therefore, the issue of whether to use fear appeals will not be relevant. Likewise, evaluation (Step 6) focuses on whatever has been developed in 1–5 and decisions regarding fear appeals are not made in this last step. In Step 2, program planners may focus on the wrong behaviors or determinants. In Step 3, program planners may choose inadequate methods or applications. In Step 4, fear appeals may be introduced by other professionals involved in text writing and materials development. And in Step 5, implementers and decision makers in health promotion organizations may overrule program planners in a misguided preference for fear appeals. A full example of an IM application on adolescent HIV/STI prevention can be found at the web address given in the Schaalma and Kok (2011) reference.
Step 2: Adequate determinants' analyses
In applying IM, determinants have a function in understanding behavior and in changing behavior. In Step 2, the determinants of the risky as well as the health-promoting behaviors are analyzed, while in Step 3, theoretical methods for change are identified that may effectively change these determinants.
The first impression of the causes of a health behavior problem does not always represent the correct definition of the problem. An example of poorly explored causation is an intended campaign to increase child restraint devices (CRDs) to protect young children against the consequences of an automobile accident. At first program planners began to plan a campaign based on the assumption that parents did not use the devices based on underestimation of risk. As it turned out, the reasons for parents not using CRDs was not an underestimation of risk (more than 90% intended to use CRDs) but a lack of self-efficacy and skills for coping when a child becomes restless and disruptive (Pieterse, Kok, & Verbeek, 1992). A fear appeal intervention would have made the situation for the parents even worse; what they needed instead was skills training and self-efficacy improvement.
A second example is about HIV prevention; specifically, why do adolescents have sexual intercourse without using condoms? One explanation, of course, is that they do not recognize the severity of an HIV infection and their own susceptibility to become infected with HIV. However, as it turns out, the major determinants of using or not using condoms are outcome expectations, subjective norms, self-efficacy, responsibility, and embarrassment (Bartholomew et al., 2011, p. 27). Underestimation of risk is found, but in relation to misconceptions about personal susceptibility. Fear appeals would not promote condom use; what is needed is interventions increasing skills and self-efficacy.
How to find the right determinants to target in an intervention? Intervention Mapping suggests four core processes: (1) brainstorming in the planning group involving representatives from the target population, stakeholders, and implementers; (2) searching the empirical literature for determinants of behavior; (3) identifying and applying appropriate theories on determinants; and (4) conducting additional qualitative and quantitative research for unanswered questions (Bartholomew et al., 2011, pp. 25–33). How to identify appropriate theories? By searching the literature on the topic for theories, by matching constructs from the brainstorm to theories, and by applying frequently used theories (Buunk & Van Vugt, 2008). For example, a construct from the brainstorm could be “lack of confidence.” This construct might lead to the theoretical construct of “self-efficacy” in social cognitive theory (McAllister et al., 2008).
Regarding frequently used theories, some agreement is emerging in the health promotion and behavioral health fields regarding important determinants of behavior, based on theoretical constructs across theories. Five major behavioral science theorists agreed on a set of eight variables as key determinants of behavior, later called the integrated behavioral model (Montaño & Kasprzyk, 2008). The determinants from the integrated behavioral model are presented in Table 2 with the first three variables thought to be necessary and sufficient for behavior change and the remaining five as influencing the direction and strength of behavioral intention. Risk perception is seen as a part of the determinant outcome expectations or attitude. Lack of fear—not perceiving the negative health consequences of life-endangering behaviors—is very seldom an important determinant of risky behavior.
TABLE 2.
Determinants of behavior from the integrated behavioral model (Montaño & Kasprzyk, 2008)
| 1. | The person has formed a strong positive intention (or made a commitment) to perform the behavior (intention). |
| 2. | No environmental constraints make it impossible for the behavior to occur (environmental constraints). |
| 3. | The person has the skills necessary to perform the behavior (skills). |
| 4. | The person believes that the advantages of performing the behavior outweigh the disadvantages (attitude). |
| 5. | The person perceives more social (normative) pressure to perform the behavior than not to do so. |
| 6. | The person perceives that performing the behavior is more consistent than inconsistent with his or her own self-image (personal norms, personal standards). |
| 7. | The person's affective reaction to performing the behavior is more positive than negative. |
| 8. | The person perceives that he or she has the capability to perform the behavior under a number of different circumstances (perceived self-efficacy, perceived behavioral control). |
Step 3: Theory- and evidence-based behavior change methods
A number of systematic reviews and meta-analyses in the health promotion field show that adequate use of theory-based methods increases the effectiveness of interventions to change behavior (Albarracín et al., 2005; De Bruin et al., 2010b; Fisher, Fisher, Bryan, & Misovich, 2002; Mullen, Green, & Persinger, 1985; Peters et al., 2013; Van Achterberg et al., 2011). In the third step of IM, all program objectives are organized by determinant. Then theoretical methods are identified that may help reach the program objectives, which in turn are translated into practical applications. A theory-based change method is a technique for changing a behavioral determinant of individuals or environmental agents, while a practical application delivers the method to fit with the priority group and the program setting. There are no ‘magic bullets’; some methods can be used for a range of determinants, some only for a specific determinant.
There is increasing interest in systematic descriptions of health promotion interventions, the theoretical methods they contain, and the determinants that are targeted for change. For instance, Abraham and Michie (2008) provide a theory-linked taxonomy of generally applicable individual health behavior change techniques. Those behavior change techniques derived from reviews were then linked with theory-based determinants (Michie, Johnston, Francis, Hardeman, & Eccles, 2008), comparable to the IM approach. Other authors combined the taxonomy with the IM approach, to develop a checklist for coding methods in patient education interventions (De Bruin et al., 2010a; Van Achterberg et al., 2011). At higher environmental levels, Khan et al. (2009) described processes (and their measures) for use by communities and local governments in planning and monitoring environmental and policy-level interventions for obesity prevention. However, these taxonomies define behavior change methods; they do not describe whether that method is used appropriately or inappropriately: the parameters for use or the conditions under which methods are effective.
Bartholomew et al. (2011) provide tables with theoretical methods and their limiting conditions for every major determinant and for all higher environmental levels. See Table 3 for examples of basic theoretical methods at the individual level, Table 4 for methods to change risk perception, and Table 5 for methods to improve self-efficacy and skills.
TABLE 3.
Examples of basic methods at the individual level (adapted from Bartholomew et al., 2011, pp. 327–329)
| Methods and definitions | Parameters for use | Examples |
|---|---|---|
| Tailoring | ||
| Matching the intervention or components to previously measured characteristics of the participant. | Tailoring variables or factors related to behavior change (such as stage) or to relevance (such as culture or socioeconomic status). | A patient educator motivates her patients to engage in vigorous physical activity by giving different messages based on the stage of change of each patient, for example developing an action plan for those in action. |
| Modeling | ||
| Providing an appropriate model being reinforced for the desired action. | Attention, remembrance, self-efficacy and skills, reinforcement of model, identification with model, coping model instead of mastery model. | The health promoter finds a role model from the at-risk group who will encourage identification and serve as a coping model: “I tried to quit smoking several times and was not successful, then I tried … Now I have been off cigarettes for … ” |
| Facilitation | ||
| Creating an environment that makes the action easier or reduces barriers to action. | Requires real changes in the environment; identification of barriers and facilitators; power for making changes; and usually intervention at a higher environmental level to facilitate conditions on a lower level. | A program that targets improvement in drug users' self-efficacy for using clean needles must also facilitate accessibility of clean needles. |
TABLE 4.
Examples of methods to change awareness and risk perception (adapted from Bartholomew et al., 2011, pp. 333–334)
| Methods and definitions | Parameters for use | Examples |
|---|---|---|
| Consciousness raising | ||
| Providing information, feedback, or confrontation about the causes, consequences, and alternatives for a problem or a problem behavior. | Can use feedback and confrontation; however, raising awareness must be quickly followed by increase in problem-solving ability and (collective) self-efficacy. | An HIV counselor reminds a person of recent episodes of failure to use condoms when having sex and the potential consequences of that behavior on significant others. |
| Personalize risk | ||
| Providing information about personal costs or risks of action or inaction with respect to target behavior. | Present messages as individual and undeniable, and compare them with absolute and normative standard. | Individuals receive personal risk feedback on their fat intake, indicating whether it is higher than their self-rated level. |
| Scenario-based risk information | ||
| Providing information that may aid the construction of an image of the ways in which a future loss or accident might occur. | Plausible scenario with a cause and an outcome; imagery. Most effective when people generate their own scenario or when multiple scenarios are provided. | Peer models in an HIV-prevention program present a series of scenarios in which they describe how they found themselves in risky situations, for example, a sexual relationship over the summer holidays. |
TABLE 5.
Examples of methods to change skills, capability, and self-efficacy and to overcome barriers (adapted from Bartholomew et al., 2011, pp. 342–344)
| Methods and definitions | Parameters for use | Examples |
|---|---|---|
| Cue altering | ||
| Teaching changing a stimulus, either consciously or unconsciously perceived, that elicits or signals a behavior. | Existing positive intention. | Dieters change the route they take, walking to work in order to avoid easy access to snack shops. |
| Goal setting | ||
| Prompting planning what the person will do, including a definition of goal-directed behaviors that result in the target behavior. | Commitment to the goal; goals that are difficult but available within the individual's skill level. | Dietician and patient discuss the weight loss goal for the next meeting, deciding on a goal that is acceptable to the patient and to the dietician. |
| Planning coping responses | ||
| Prompting participants to list potential barriers and ways to overcome these. | Identification of high-risk situations and practice of coping response. | The HIV nurse and the patient define the causes of nonadherence. Then the HIV nurse and the patient formulate solutions to solve or avoid the causes for nonadherence. |
It is important to bear in mind that theoretical methods are only effective under certain conditions (Schaalma and Kok, 2009). Modeling, for instance, is only effective when the model is reinforced, and observers pay attention, have sufficient self-efficacy and skills, identify with the model, and observe a coping model instead of a mastery model (McAlister et al., 2008). Under those conditions, modeling is a very effective method to change many determinants. Other theoretical methods have other conditions that need to be met; for example, goal setting is effective when the chosen goal is challenging but feasible (Latham and Locke, 2007). As mentioned earlier, fear arousal as a method requires high self-efficacy expectations about the behavior; a condition that is very rare because of the complex nature of most behavior change settings. However, it may be clear from these examples that many potential alternative methods are available.
Step 4: Designing and organizing the program
Step 4 of IM concerns the actual development of the program, integrating the various applications that were chosen in the previous step. Program planners decide about the overall structure of the program, themes, channels, and vehicles of the program. They design and produce materials while striving for cultural sensitivity. They work with other professionals and they pilot-test the relevant elements of the program. Even when program planners are aware of the limitations of fear appeals, the other professionals that contribute to this step in program production may not be. Fear appeals may appear in the text writing, the choice of illustrations, or in the filming. Also in the actual delivery of the program by program peer educators or implementers, the message may be ‘colored’ in a way that reflects the naïve trust in fear appeals. There is always a moment in the program planning process where someone will suggest using a “harder” or “tougher” approach. Within the program development team, the program planner is the one responsible for the correct translation of theoretical methods into practical applications based on the parameters of the methods and is often the only team member who is sufficiently trained to do so. Program planners should respect other professionals' expertise but at the same time be able to effectively communicate their own expertise.
Essential in Step 4 is pilot-testing, which is meant as a guarantee against implementing inadequate program materials. Individual components of the intervention program should be pilot-tested on their effectiveness before final production and implementation, which can be done relatively easily using experimental research designs (Whittingham, Ruiter, Castermans, Huiberts, & Kok, 2008).
Step 5: Implementation of theory- and evidence-based interventions: Organizational change
Program implementers are the people who participate in program activities to deliver the program to participants or beneficiaries. For example, teachers present health education programs to students, and nurses often deliver programs to patients. Gate-keepers, even though they are not program implementers, may be program adopters because they are necessary to get the program to the program participants. For example, school principals may not be the user of a health education curriculum, but their support is critical for program adoption. The health promoters in the study of Peters et al. (2014, this issue) experienced difficulties in convincing their managers and collaborating organizations to implement well-planned alternatives to fear appeals. In the implementation step, fear appeals may be promoted by program implementers and gatekeepers or decision makers, who have insufficient knowledge of the available evidence.
Implementation is an essential step in program development. Effective health education and promotion programs will have little impact if they are never used or if they are discontinued while still needed to create the desired health impact (Durlak & DuPre, 2008; Oldenburg & Glanz, 2008; Rogers, 2003). In Step 5 of IM, the focus is on planning an implementation protocol to ensure that the program developed in the previous steps will be used and maintained over time, for as long as it is needed. Program planners may have to convince implementers and decision makers in their own organization and in collaborating organizations that fear appeals are ineffective and that alternatives are available. That is a process at the environmental level of organizations.
The methods discussed above and illustrated in Tables 5 can be applied to interventions to accomplish program adoption, implementation, and sustainability. Program planners can address personal determinants of implementers such as knowledge of program compatibility and relative advantage, outcome expectations for the program, and self-efficacy for doing the program activities with methods at the individual level, such as persuasive communication, tailoring, and modeling. However, implementation almost always involves organizational change, and program planners have to apply methods at environmental levels as well. Organizational theory can be used to understand the determinants of implementation and to select methods for organizational change that will support program implementation (Rutten, Roger, Abu-Omar, & Frahsa, 2009; Weiner, Lewis, & Linnan, 2009). Examples of basic methods at the environmental level are presented in Table 6 and examples of methods at the organizational level in Table 7 (Bartholomew et al., 2011).
TABLE 6.
Examples of basic methods at the environmental level (adapted from Bartholomew et al., 2011, pp. 347–348)
| Methods and definitions | Parameters for use | Examples |
|---|---|---|
| Participatory problem solving | ||
| Diagnosing the problem, generating potential solutions, developing priorities, making an action plan, and obtaining feedback after implementing the plan. | Requires willingness by the health promoter or convener to accept the participants as equals and as having a high level of influence; requires target group to possess appropriate motivation and skills. | A health promotion consultant assists employees of a small company to identify the level and sources of stress and develop a plan with management to address and monitor work stress. |
| Advocacy and lobbying | ||
| Arguing and mobilizing resources on behalf of a particular change; giving aid to a cause; active support for a cause or position. | Form of advocacy must match style and tactics of the people, communities or organizations represented, and the nature of the issue; includes policy advocacy; often tailored to a specific environmental agent. | Members of the American Public Health Association use the organization's action alert system to contact their legislators to urge them to vote for pending health care reform legislation. |
| Technical assistance | ||
| Providing technical means to achieve desired behavior. | Nature of technical assistance will vary by environmental level but must fit needs, culture, and resources of recipient. | A health department liaison helps a community health center design recruitment procedures, training, and supervisory guidelines as they establish a new lay health worker program. |
TABLE 7.
Examples of methods to change organizations (adapted from Bartholomew et al., 2011, pp. 352–353)
| Methods and definitions | Parameters for use | Examples |
|---|---|---|
| Sense-making | ||
| Leaders reinterpret and relabel processes in organization, create meaning through dialogue, and model and redirect change. | Used for continuous change, including culture change. | A supervisor in a hospital talks to his staff about the positive aspects of finding and correcting mistakes in documentation of medication administration. |
| Organizational diagnosis and feedback | ||
| Assessing of organizational structures and employees' beliefs and attitudes, desired outcomes and readiness to take action, using surveys and other methods. | Methods appropriate to organizational characteristics, for example, size and information technology. | An organizational consultant conducts a survey of employees' health behaviors and determinants and holds focus groups of employees to review the results and plan for health promotion programs. |
| Increasing stakeholder influence | ||
| Increase stakeholder power, legitimacy, and urgency, often by forming coalitions and using community development and social action to change an organization's policies. | The focal organization perceives that the external organization or group is one of its stakeholders. | A community group uses media advocacy to highlight the groundwater pollution by gas storage tanks located in the community and to demand that the tanks be moved by the gas company that owns them. |
Finding alternatives to fear appeals: Intervention Mapping
We elaborated on aspects of IM that would foster our objectives that intervention developers should be better trained in, and more insistent on (1) performing adequate determinant analyses, (2) applying theory- and evidence-based behavior change methods, and (3) convincing their program implementers, managers and collaborating organizations to implement well-planned alternatives to fear appeals.
Non-behavioral scientists think that fear appeals will trigger people's risk awareness and motivate them to change based on the assumption that risky or unhealthy behavior is determined by a lack of risk awareness. Even if that is the case, underestimation of the severity of consequences is often less important that underestimation of personal susceptibility (Ruiter et al., 2001). Moreover, most risk behavior is determined by other determinants—intentions, skills, and environmental factors—while intention is determined by attitude, social norms, personal norms, affective reactions, and self-efficacy. Exposing at-risk people to fear appeals while the actual determinants of the risky behavior are, for example, environmental factors, self-efficacy, and skills, will lead to defensive reactions, including less attention to the fear-arousing message (Kessels, Ruiter, & Jansma, 2010; Ruiter & Kok, 2012). Before considering fear appeals, program planners should carefully identify important and changeable determinants of the behavior they want to change, using theory and qualitative and quantitative research (Bartholomew et al., 2011).
For example, Schaalma and colleagues developed an STD/HIV prevention program for 13-15 year old school students (Schaalma & Kok, 2011). Of course they mentioned the severity of STD/HIV infections, but not in an emotional way. The focus of the program was on personal susceptibility, condom use as response efficacy, and the promotion of self-efficacy regarding carrying condoms, negotiating with the partner, correct condom use and maintenance of condom use (Schaalma & Kok, 2011). They applied theoretical methods such as modeling, scenario-based risk information, and guided practice. To get the schools to implement the program, they applied technical assistance and increasing stakeholder influence, in this case through the municipal public health services. Their program was shown to be effective for all targeted determinants, and led to an increase in condom use. As another example, De Bruin and colleagues developed a program for HIV nurses to increase therapy adherence with HIV + − patients (De Bruin, Hospers, Van den Borne, Kok, & Prins, 2005). Again, they explained the health consequences of low adherence, but not in an emotional way. The focus of the program was on self-management and coping with difficult situations. De Bruin and colleagues applied theoretical methods such as participation and tailoring, self-monitoring, goal setting, and planning coping responses. To get the hospital and the nurses to implement the program, they applied participatory problem solving, technical assistance, and organizational diagnosis and feedback. The program was shown to be effective in improving adherence (De Bruin et al., 2010a).
Changing behavior is a challenging task for health promoters. The IM protocol helps program planners to identify methods and applications for raising risk awareness and for changing any other determinant: not like a cook book, but by suggesting theory- and evidence-based behavior change methods linked with determinants, and by providing the conditions under which these method will be more or less effective. IM has been described as tiresome, complex, elaborate, expensive and time-consuming. To a degree, that may be true. At the same time, however, all authors who assessed IM critically also indicated that IM helped in bringing the development of interventions to a higher level. In the end, advantages outweighed disadvantages (Kok & Mesters, 2011).
Developing high-quality programs is one thing, getting them implemented another. Developing a program includes planning the implementation. Implementation almost always involves organizational change, schools, worksites, hospitals, local governments, etc. But it also involves gatekeepers at the organizations of the health promoters. The same IM process that guides program planners in developing interventions for the at-risk populations and environmental decision makers also guides program planners to develop interventions for dissemination, adoption, implementation, and sustainability.
CONCLUSIONS
Fear appeals in health education are effective rarely, and only under exceptional circumstances of high efficacy. Instead of applying fear appeals, health promoters should identify effective alternatives for fear arousal and carefully develop theory- and evidence-based programs, specifically: identify important and changeable determinants of the risk behavior, choose appropriate intervention methods and applications, and develop interventions for dissemination, adoption, implementation and sustainability of those theory- and evidence-based programs. The Intervention Mapping protocol helps program planners to optimize chances for effectiveness.
REFERENCES
- Abraham C. Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychology. 2008;27:379–387. doi: 10.1037/0278-6133.27.3.379. [DOI] [PubMed] [Google Scholar]
- Albarracín D, Gillette JC, Earl AN, Glasman LR, Durantini MR. Ho M-H. A test of major assumptions about behavior change: A comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychological Bulletin. 2005;131:856–897. doi: 10.1037/0033-2909.131.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartholomew LK, Parcel GS, Kok G, Gottlieb NH. Fernández ME. Planning health promotion programs: An Intervention Mapping approach. 3rd ed. San Francisco, CA: Jossey-Bass; 2011. [Google Scholar]
- Brown SL. Smith EZ. The inhibitory effect of a distressing anti-smoking message on risk perceptions in smokers. Psychology & Health. 2007;22:255–268. [Google Scholar]
- Buunk AP. van Vugt M. Applying social psychology: From problems to solutions. London: Sage; 2008. [Google Scholar]
- Champion VL. Skinner CS. The health belief model. In: Viswanath K, editor; Glanz K, Rimer BK, editors. Health behavior and health education: Theory, research, and practice. 4th ed. San Francisco, CA: Jossey-Bass; 2008. pp. 45–65. [Google Scholar]
- De Bruin M, Hospers HJ, Van den Borne HW, Kok G. Prins J. Theory-and evidence-based intervention to improve adherence to antiretroviral therapy among HIV-infected patients in the Netherlands: A pilot study. AIDS Patient Care and STDs. 2005;19:384–394. doi: 10.1089/apc.2005.19.384. [DOI] [PubMed] [Google Scholar]
- De Bruin M, Hospers HJ, Van Breukelen GJP, Kok G, Koevoets WM. Prins JM. Electronic monitoring-based counseling to enhance adherence among HIV-infected patients: A randomized controlled trial. Health Psychology. 2010a;29:421–428. doi: 10.1037/a0020335. [DOI] [PubMed] [Google Scholar]
- De Bruin M, Viechtbauer W, Schaalma HP, Kok G, Abraham C. Hospers HJ. Standard care impact on effects of highly active antiretroviral therapy adherence interventions: A meta-analysis of randomized controlled trials. Archives of Internal Medicine. 2010b;170:240–250. doi: 10.1001/archinternmed.2009.536. [DOI] [PubMed] [Google Scholar]
- De Hoog N, Stroebe W. De Wit JBF. The impact of vulnerability to and severity of a health risk on processing and acceptance of fear-arousing communications: A meta-analysis. Review of General Psychology. 2007;11:258. [Google Scholar]
- De Vries H, Mesters I, Van de Steeg H. Honing C. The general public's information needs and perceptions regarding hereditary cancer: An application of the Integrated Change Model. Patient Education and Counseling. 2005;56:154–165. doi: 10.1016/j.pec.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Durlak JA. DuPre EP. Implementation matters: A review of research on the influence of implementation on program outcomes and the factors affecting implementation. American Journal of Community Psychology. 2008;41:327–350. doi: 10.1007/s10464-008-9165-0. [DOI] [PubMed] [Google Scholar]
- Earl A. Albarracín D. Nature, decay, and spiraling of the effects of fear-inducing arguments and HIV counseling and testing: A meta-analysis of the short-and long-term outcomes of HIV-prevention interventions. Health Psychology. 2007;26:496–506. doi: 10.1037/0278-6133.26.4.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Bryan AD. Misovich SJ. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychology. 2002;21:177–186. [PubMed] [Google Scholar]
- Floyd DL. Prentice-Dunn S. A meta-analysis of research on protection motivation theory. Journal of Applied Social Psychology. 2000;30:407–429. [Google Scholar]
- Godin G, Gagnon H, Alary M, Levy JJ. Otis J. The degree of planning: An indicator of the potential success of health education programs. Promotion & Education, XIV. 2007;((3)):138–142. [PubMed] [Google Scholar]
- Hospers HJ. Kok G. Determinants of safe and risk taking behavior among gay men: A review. AIDS Education and Prevention. 1995;7:74–96. [PubMed] [Google Scholar]
- Khan LK, Sobush K, Keener D, Goodman K, Lowry A, Kakietek J, et al. Recommended community strategies and measurements to prevent obesity in the United States. Morbidity and Mortality Weekly Report. 2009;58:1–26. (RR07) [PubMed] [Google Scholar]
- Kok G, Gottlieb NH, Commers M. Smerecnik C. The ecological approach in health promotion programs: A decade later. American Journal of Health Promotion. 2008;22:437–442. doi: 10.4278/ajhp.22.6.437. [DOI] [PubMed] [Google Scholar]
- Kok G. Mesters I. Getting inside the black box of health promotion programs using intervention mapping. Chronic Illness. 2011;7(3):176–180. doi: 10.1177/1742395311403013. [DOI] [PubMed] [Google Scholar]
- Latham GP. Locke EA. New developments in and directions for goal-setting research. European Psychologist. 2007;12:290–300. [Google Scholar]
- McAlister AL, Perry CL. Parcel GS. How individuals, environments, and health behaviors interact: Social Cognitive Theory. In: Viswanath K, editor; Glanz K, Rimer BK, editors. Health Behavior and Health Education: Theory, research, and practice. 4th ed. San Francisco, CA: Jossey-Bass; 2008. pp. 169–188. [Google Scholar]
- Michie S, Johnston M, Francis J, Hardeman W. Eccles M. From theory to intervention: Mapping theoretically derived behavioral determinants to behavior change techniques. Applied Psychology. 2008;57:660–680. [Google Scholar]
- Milne S, Orbell S. Sheeran P. Combining motivational and volitional interventions to promote exercise participation: Protection Motivation Theory and implementation intentions. British Journal of Health Psychology. 2002;7:163–184. doi: 10.1348/135910702169420. [DOI] [PubMed] [Google Scholar]
- Montaño DE. Kasprzyk D. Theory of Reasoned Action, Theory of Planned Behavior, and the Integrated Behavioral Model. In: Viswanath K, editor; Glanz K, Rimer BK, editors. Health behavior and health education: Theory, research, and practice. 4th ed. San Francisco, CA: Jossey-Bass; 2008. pp. 67–96. [Google Scholar]
- Mullen PD, Green LW. Persinger GS. Clinical trials of patient education for chronic conditions: A comparative meta-analysis of intervention types. Preventive Medicine. 1985;14:753–781. doi: 10.1016/0091-7435(85)90070-2. [DOI] [PubMed] [Google Scholar]
- Norman P, Boer H. Seijdel ER. Protection motivation theory. In: Norman P, editor; Conner M, editor. Predicting health behaviour: Research and practice with social cognitive models. 2nd ed. Maiden-head: Open University Press; 2005. pp. 170–222. [Google Scholar]
- Oldenburg B. Glanz K. Diffusion of innovations. In: Lewis FM, editor; Glanz K, Rimer BK, editors. Health behavior and health education: Theory, research, and practice. 4th ed. San Francisco, CA: Jossey-Bass; 2008. pp. 313–333. [Google Scholar]
- Peters GJY, Ruiter RAC. Kok G. Threatening communication: A critical re-analysis and a revised meta-analytic test of fear appeal theory. Health Psychology Reviews. 2013;7:S8–S31. doi: 10.1080/17437199.2012.703527. doi: 10.1080/17437199.2012.703527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters G-JY, Ruiter RAC. Kok G. Threatening communication: A qualitative study of fear appeal effectiveness beliefs among intervention developers, policymakers, politicians, scientists, and advertising professionals. International Journal of Psychology. 2014;49:71–79. doi: 10.1002/ijop.12000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters LHW, Kok G, Ten Dam GTM, Buijs GJ. Paulussen TGWM. Effective elements of school health promotion across behavioral domains: A systematic review of reviews. BMC Public Health. 2013;9:182. doi: 10.1186/1471-2458-9-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieterse ME, Kok G. Verbeek J. Determinants of the acquisition and utilization of automobile child restraint devices: A survey among Dutch parents. Health Education Research. 1992;7:349–358. [Google Scholar]
- Rogers EM. Diffusion of innovations. 5th ed. New York, NY: Free Press; 2003. [Google Scholar]
- Ruiter RAC, Abraham C. Kok G. Scary warnings and rational precautions: A review of the psychology of fear appeals. Psychology and Health. 2001;16:613–630. [Google Scholar]
- Ruiter RAC, Kessels LTE, Peters G-JY. Kok G. Sixty years of fear appeal research: Current state of the evidence. International Journal of Psychology. 2014;49:63–70. doi: 10.1002/ijop.12042. [DOI] [PubMed] [Google Scholar]
- Ruiter RAC. Kok G. Planning to frighten people? Think again. In: Kools M, editor; Abraham C, editor. Writing health communication. London: Sage; 2012. pp. 117–133. [Google Scholar]
- Rutten A, Roger U, Abu-Omar K. Frahsa A. Assessment of organizational readiness for health promotion policy implementation: Test of a theoretical model. Health Promotion International. 2009;24:243–251. doi: 10.1093/heapro/dap016. [DOI] [PubMed] [Google Scholar]
- Schaalma H. Kok G. Decoding health education interventions: The times are a-changin'. Psychology and Health. 2009;24:5–9. doi: 10.1080/08870440903126348. [DOI] [PubMed] [Google Scholar]
- Schaalma H. Kok G. 2011. Case study 3: A school HIV-prevention program in the Netherlands. Case study on the companion site for Bartholomew et al. (2011). Retrieved from http://bcs.wiley.com/he-bcs/Books?action=index&itemId=0470528516&bcsId=6246.
- Schwarzer R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Applied Psychology. 2008;57:1–29. [Google Scholar]
- Van Achterberg T, Huisman-De Waal GGJ, Ketelaar NABM, Oostendorp RA, Jacobs JE. Wollersheim HCH. How to promote healthy behavior in patients? An overview of evidence for behaviour change techniques. Health Promotion International. 2011;26:148–162. doi: 10.1093/heapro/daq050. doi: 10.1093/heapro/daq050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner BJ, Lewis MA. Linnan LA. Using organization theory to understand the determinants of effective implementation of worksite health promotion programs. Health Education Research. 2009;24:292–305. doi: 10.1093/her/cyn019. [DOI] [PubMed] [Google Scholar]
- Whittingham JR, Ruiter RAC, Castermans D, Huiberts A. Kok G. Designing effective health education materials: Experimental pre-testing of a theory-based brochure to increase knowledge. Health Education Research. 2008;23:414–426. doi: 10.1093/her/cym018. [DOI] [PubMed] [Google Scholar]
- Witte K. Allen M. A meta-analysis of fear appeals: Implications for effective public health campaigns. Health Education & Behavior. 2000;27:591–615. doi: 10.1177/109019810002700506. [DOI] [PubMed] [Google Scholar]
- Witte K, Meyer G. Martell D. Effective health risk messages: A step-by-step guide. Thousand Oaks, CA: Sage; 2001. [Google Scholar]


