Abstract
Objective
To assess 2004–08 ectopic pregnancy rates among Medicaid recipients in 14 states and 2000–08 time trends in 3 states, and to identify differences in rate by race/ethnicity.
Design
Secondary analysis of Medicaid administrative claims data.
Setting
United States.
Subjects
Women ages 15–44 enrolled in Medicaid in Arizona, California, Colorado, Florida, Illinois, Indiana, Iowa, Louisiana, Massachusetts, Michigan, Minnesota, Mississippi, New York, or Texas in 2004–08 (n=19,135,106), and in California, Illinois and New York in 2000–03.
Interventions
None.
Main Outcome Measure
Number of ectopic pregnancies divided by the number of total pregnancies (spontaneous abortions, induced abortions, ectopic pregnancies, and all births).
Results
The 2004–08 Medicaid ectopic pregnancy rate for all 14 states combined was 1.40% of all reported pregnancies. Adjusted for age, the rate was 1.47%. Ectopic pregnancy incidence was 2.3 per 1,000 woman-years. In states for which longer-term data were available (California, Illinois and New York), the rate declined significantly 2000–08. In all 14 states, Black women were more likely to experience an ectopic pregnancy compared to whites (Relative Risk 1.46, 95% Confidence Interval 1.45–1.47).
Conclusions
Ectopic pregnancy remains an important health risk for women enrolled in Medicaid. Black women are at consistently higher risk than whites.
Keywords: Ectopic pregnancy, Health status disparities, Medicaid
Ectopic pregnancy poses a serious health risk to women. Defined as implantation of a fertilized ovum outside the uterine endometrium, the condition can cause hemorrhage and death if not treated promptly. Approximately 4% of pregnancy-related death in the United States (1998–2005) is due to ectopic pregnancy (1). Primary risk factors for ectopic pregnancy include smoking and a history of chlamydia (2), and other factors such as prior tubal surgery or assisted reproductive technologies also increase risk. As with other causes of maternal morbidity and mortality (1, 3, 4), African American women face higher rates of ectopic pregnancy than whites (5, 6). The relationship between race and socioeconomic status in maternal health is poorly understood. Some studies demonstrating racial disparities have not taken socioeconomic status into account (7) while others have found race to be significant even controlling for socioeconomic status (8,3).
In recent years, quantifying ectopic pregnancy in the United States has become difficult because ectopic pregnancies treated during multiple outpatient visits cannot be reliably identified and tracked using traditional surveillance data; this has left administrative claims data as an important surveillance tool (9). Medicaid is an important data source for maternal health epidemiology since it includes low-income women, a population at high risk for maternal morbidity and mortality (3, 10). We previously reported ectopic pregnancy rates among Medicaid beneficiaries in three large states – California (2.07% of all reported pregnancies), Illinois (2.43%), and New York (2.38%) – from 2000 through 2003 (6). These rates were generally higher than those reported in other studies based on insurance data, including the MarketScan nationwide database of commercial insurers (1.6% in 2002–07 if all ectopic pregnancy diagnoses were counted, or 0.64% if only those with a documented treatment were included), (11) Kaiser Permanente Northern California (2.07% in 1997–2000) (12) and Group Health Cooperative in Idaho and Washington state (1.36% in 2005–07)(13). We also found that within the Medicaid population, African American women had significantly higher risk of ectopic pregnancy than whites in the three states studied (California, Illinois, New York); trends for other race/ethnicity groups varied by state. Ectopic pregnancy rates in the Medicaid population from other states and more recent years are unknown.
We conducted this study to assess recent ectopic pregnancy rates and incidence (2004–08) in a 14-state population that includes an estimated 58% of the US population of female Medicaid beneficiaries of reproductive age (14). We also aimed to assess whether there was a time trend in rates among women in California, Illinois and New York, the three states we had previously studies, from 2000 to 2008. Finally we examined disparities by race/ethnicity in this large population of low-income women.
MATERIALS AND METHODS
We received Medicaid Analytic Extract data files from the Centers for Medicare and Medicaid Services (CMS) under an approved Data Use Agreement. The study’s institutional review board acknowledged the study as exempt from review since it constituted a secondary analysis of deidentified data. The authors had no conflicts of interest. We examined Medicaid claims for all female beneficiaries 10–55 years of age in Arizona, California, Colorado, Florida, Illinois, Indiana, Iowa, Louisiana, Massachusetts, Michigan, Minnesota, Mississippi, New York and Texas, 2004–08. We selected these states to maximize number of enrollees, geographic spread and racial diversity, given that we could purchase data for 14 states. These data files include person-level information on Medicaid enrollees and encounter-level information for Medicaid claims from all sources of care, including inpatient, outpatient, physician services, radiology, and clinic visits. We did not examine long-term care files or pharmacy prescription claims for this study since our previous research found these did not contribute valuable information about ectopic pregnancy. We included women aged 15–44 in our analysis in order to make it comparable to other studies of women of reproductive age.
Analysis was conducted in the same manner as was previously reported for Medicaid 2000–03 rates in three states (6). We identified ectopic pregnancy cases from both inpatient and outpatient claims containing the International Classification of Diseases 9th revision (ICD9) diagnosis code 633.xx as principal diagnosis. We calculated the ectopic pregnancy rate among beneficiaries aged 15–44 as the number of ectopic pregnancies (by principal diagnosis code) divided by the number of total pregnancies, identified using ICD9 diagnosis codes for all pregnancy-related care and outcomes. The denominator included codes for spontaneous and induced abortion (63x.xx), pregnancy complications (64x.xx), normal and complicated birth (65x.xx and 66x.xx), routine and high-risk prenatal care (V22.xx and V23.xx), outcome of delivery (V27.xx), and antenatal screening (V28.xx). Encounters with one of these codes in any diagnosis field–principal, secondary, or other–were included in the denominator. This strategy was designed to produce the most conservative (lowest) estimate of the ectopic pregnancy rate, because the case definition for the numerator required a principal diagnosis of ectopic pregnancy, whereas any possible pregnancy would be captured in the denominator. For both the numerator and denominator counts, repeat pregnancy-related encounters within 9 months (270 days) were considered part of the same pregnancy. Repeat pregnancy-related encounters for the same beneficiary after 9 months were treated as a new pregnancy episode and each pregnancy episode (in 9-month groupings of claims) was counted separately. Age-adjusted and race-adjusted ectopic pregnancy rates were computed using the female, aged 15–44, Medicaid population for the named 14 states as the standard population. We also calculated the incidence of ectopic pregnancy as the number of ectopic pregnancies divided by the number of person-years (female Medicaid beneficiaries aged 15–44).
We examined ectopic pregnancy rates by race/ethnicity using the race/ethnicity variable in Medicaid files, which is coded as: white, black, Hispanic, Asian, American Indian/Alaskan native, native Hawaiian/Pacific Islander, or multiracial. Because the outcome variable was a rate, we used Poisson multivariable regression models to estimate the relative risks for ectopic pregnancy by race/ethnicity within each state, adjusting for age and for all states combined, adjusting for age and state. We tested for a time trend in the rate of ectopic pregnancy, from the year 2000 to 2008, for the three states (California, Illinois, New York) for which we had previously reported 2000 to 2003 rates.
Finally, we conducted post-hoc exploratory analyses to identify possible explanations of state-level variation in ectopic pregnancy rates. We tested for correlation between state Medicaid ectopic pregnancy rate and various factors that we speculated might be associated. We used Spearman’s rank correlation coefficient, ρ (rho), with state as the unit of analysis. First, we explored the timing of enrollment in Medicaid relative to ectopic pregnancy episodes, to test whether ectopic pregnancy rates are attributable to local Medicaid enrollment practices (such as greater or less likelihood of a woman signing up for Medicaid when she learns she is pregnant). We also searched publicly available state-level variables that might contribute to state variation in ectopic pregnancy: rates of chlamydia (15) and smoking (16) among women; median household income (17), income inequality (Gini coefficient),(18) and population density (19). We also assessed whether the rate of chlamydia diagnosis within our Medicaid state data (% of female Medicaid beneficiaries ages 15–44 who had any claim with an ICD9 diagnosis code for chlamydia infection) correlated with state ectopic pregnancy rate. Finally, we explored whether proportion of Medicaid-covered births (20), or Medicaid coverage of induced abortion (which we assessed qualitatively by reviewing state policies)(21), might be associated with state ectopic pregnancy rates because these might affect the number of total pregnancies counted in the denominator.
RESULTS
There were 45,201,325 person-years of enrollment in Medicaid among women aged 15–44 in Arizona, California, Colorado, Florida, Illinois, Indiana, Iowa, Louisiana, Massachusetts, Michigan, Minnesota, Mississippi, New York and Texas combined during the 2004–08 period (Table 1), representing 19,135,106 unique individuals. Overall, there were 101,892 unique cases of ectopic pregnancy in this population (with 99,267 unique individuals having at least one ectopic pregnancy) and 7,271,430 total pregnancies, for an ectopic pregnancy rate (ectopic pregnancies/total pregnancies) of 1.40%, an age-adjusted rate of 1.47% and race-adjusted rate of 1.43%. There was marked variation in ectopic pregnancy rate and incidence by state (Table 2).
Table 1.
Person-Years and Racial Distribution, 2004–2008, women aged 15–44 in Medicaid
| State | Total | % White | % Black | % American Indian/Alaskan Native | % Asian | % Hispanic | % Native Hawaiian/Pacific Islander | % Unknown |
|---|---|---|---|---|---|---|---|---|
| AZ | 1,827,440 | 35.33 | 5.61 | 10.80 | 1.26 | 46.03 | 0.00 | 0.98 |
| CA | 19,350,690 | 20.30 | 8.47 | 0.47 | 4.54 | 60.56 | 2.65 | 3.02 |
| CO | 625,295 | 31.15 | 5.34 | 0.69 | 0.83 | 26.18 | 0.40 | 35.40 |
| FL | 3,079,865 | 37.53 | 33.17 | 0.11 | 0.73 | 24.98 | 0.00 | 3.49 |
| IA | 462,475 | 68.91 | 8.04 | 0.58 | 0.69 | 4.35 | 0.02 | 17.41 |
| IL | 2,620,430 | 40.73 | 40.77 | 0.21 | 1.74 | 14.45 | 0.00 | 2.10 |
| IN | 1,182,310 | 66.65 | 23.91 | 0.06 | 0.37 | 8.13 | 0.00 | 0.88 |
| LA | 1,116,610 | 35.69 | 58.69 | 0.32 | 0.54 | 0.89 | 0.02 | 3.85 |
| MA | 1,436,270 | 41.26 | 10.72 | 0.17 | 3.22 | 17.72 | 0.00 | 26.91 |
| MI | 2,032,470 | 57.06 | 35.21 | 0.55 | 1.19 | 5.20 | 0.00 | 0.78 |
| MN | 931,200 | 62.17 | 17.84 | 4.28 | 5.69 | 7.02 | 0.08 | 2.92 |
| MS | 878,385 | 31.13 | 56.97 | 0.36 | 0.36 | 0.64 | 0.02 | 10.52 |
| NY | 6,005,890 | 33.34 | 25.91 | 0.99 | 6.73 | 26.23 | 0.39 | 6.41 |
| TX | 3,651,995 | 27.07 | 20.60 | 0.41 | 1.09 | 50.35 | 0.00 | 0.47 |
| Al States | 45,201,325 | 31.18 | 19.21 | 0.97 | 3.45 | 39.47 | 1.19 | 4.52 |
Table 2.
Ectopic Pregnancy Incidence and Rates among Medicaid beneficiaries aged 15–44, 2004–08
| State | Incidencea | Unadjusted Rateb | Age-adjusted Rate | Race-adjusted Rate |
|---|---|---|---|---|
| AZ | 1.8 | 0.93% | 1.00% | 0.96% |
| CA | 1.7 | 1.79% | 1.83% | 1.89% |
| CO | 2.3 | 0.87% | 0.91% | 0.90% |
| FL | 2.2 | 0.95% | 1.02% | 1.02% |
| IA | 2.4 | 1.02% | 1.09% | 1.05% |
| IL | 2.9 | 1.54% | 1.65% | 1.60% |
| IN | 2.4 | 1.06% | 1.13% | 1.10% |
| LA | 3.5 | 1.34% | 1.44% | 1.38% |
| MA | 1.3 | 1.47% | 1.54% | 1.46% |
| MI | 2.9 | 2.02% | 2.12% | 2.06% |
| MN | 2.3 | 1.09% | 1.12% | 1.06% |
| MS | 2.3 | 1.11% | 1.21% | 1.16% |
| NY | 2.8 | 1.75% | 1.82% | 1.88% |
| TX | 3.6 | 1.04% | 1.06% | 1.11% |
| All States | 2.3 | 1.40% | 1.47% | 1.43% |
Incidence = number of ectopic pregnancies / 1,000 person-years
Rate = number of ectopic pregnancies / number of total pregnancies
In all 14 states, the age-adjusted risk of ectopic pregnancy was statistically significantly higher among African American women in comparison to white women (Table 3). The statespecific relative risks ranged from 1.25 (95% CI 1.19 – 1.32) in Massachusetts to 1.95 in Illinois (CI 1.91 – 2.00). Asian American women experienced significantly lower ectopic pregnancy rates in all states studied except New York. There was no consistent pattern across states in the ectopic pregnancy rates for Hispanic, American Indian/Alaskan Native, and Native Hawaiian/Pacific Islander women relative to white women.
Table 3.
Relative Risk of Ectopic Pregnancy by Race/Ethnicity, Medicaid beneficiaries aged 15–44, 2004–08
| State | White | Blacka | American Indian/Alaskan Nativea | Asiana | Hispanica | Native Hawaiian/Pacific Islandera |
|---|---|---|---|---|---|---|
| AZ | Ref | 1.41 (1.36, 1.47) <0.0001 |
0.45 (0.42, 0.47) <0.0001 |
0.66 (0.60, 0.74) <0.0001 |
0.67 (0.65, 0.69) <0.0001 |
---- |
| CA | Ref | 1.47 (1.45, 1.49) <0.0001 |
0.94 (0.88, 1.00) 0.0502 |
0.61 (0.59, 0.63) <0.0001 |
0.79 (0.78, 0.80) <0.0001 |
0.62 (0.60, 0.65) <0.0001 |
| CO | Ref | 1.42 (1.30, 1.54) <0.0001 |
1.01 (0.81, 1.25) 0.9415 |
0.43 (0.33, 0.55) <0.0001 |
0.78 (0.74, 0.82) <0.0001 |
0.74 (0.48, 1.14) 0.1740 |
| FL | Ref | 1.39 (1.36, 1.41) <0.0001 |
1.36 (1.16, 1.59) 0.0001 |
0.58 (0.54, 0.63) <0.0001 |
0.97 (0.95, 0.99) 0.0008 |
---- |
| IA | Ref | 1.46 (1.37, 1.56) <0.0001 |
0.79 (0.60, 1.04) 0.0907 |
0.73 (0.58, 0.93) 0.0907 |
0.54 (0.49, 0.58) <0.0001 |
---- |
| IL | Ref | 1.95 (1.91, 2.00) <0.0001 |
0.74 (0.52, 1.04) 0.0813 |
0.87 (0.80, 0.96) 0.0045 |
1.35 (1.31, 1.39) <0.0001 |
1.43 (1.05, 1.97) 0.0249 |
| IN | Ref | 1.56 (1.52, 1.61) <0.0001 |
1.96 (1.32, 2.88) 0.0007 |
0.55 (0.46, 0.66) <0.0001 |
0.49 (0.46, 0.51) <0.0001 |
---- |
| LA | Ref | 1.65 (1.60, 1.69) <0.0001 |
1.08 (0.88, 1.34) 0.4449 |
0.81 (0.69, 0.95) 0.0088 |
0.72 (0.65, 0.81) <0.0001 |
0.71 (0.34, 1.51) 0.3786 |
| MA | Ref | 1.25 (1.19, 1.32) <0.0001 |
0.86 (0.56, 1.31) 0.4734 |
0.77 (0.69, 0.84) <0.0001 |
1.04 (0.88, 1.09) 0.0857 |
---- |
| MI | Ref | 1.43 (1.40, 1.47) <0.0001 |
0.59 (0.50, 0.71) <0.0001 |
0.88 (0.79, 0.97) 0.0118 |
0.98 (0.93, 1.03) 0.3967 |
---- |
| MN | Ref | 1.46 (1.41, 1.51) <0.0001 |
1.04 (0.96, 1.12) 0.3704 |
0.72 (0.66, 0.78) <0.0001 |
1.06 (1.00, 1.13) 0.0457 |
---- |
| MS | Ref | 1.51 (1.46, 1.56) <0.0001 |
1.54 (1.31, 1.81) <0.0001 |
0.46 (0.33, 0.65) <0.0001 |
0.64 (0.55, 0.75) <0.0001 |
---- |
| NY | Ref | 1.52 (1.50, 1.55) <0.0001 |
0.81 (0.75. 0.89) <0.0001 |
1.01 (0.98, 1.04) 0.5030 |
1.21 (1.19, 1.23) <0.0001 |
1.05 (0.94, 1.18) 0.4101 |
| TX | Ref | 1.33 (1.31, 1.35) <0.0001 |
0.89 (0.81, 0.97) 0.0063 |
0.72 (0.68, 0.76) <0.0001 |
0.69 (0.68, 0.69) <0.0001 |
---- |
| All Statesb | Ref | 1.46 (1.45, 1.47) <0.0001 |
0.72 (0.70, 0.74) <0.0001 |
0.86 (0.84, 0.87) <0.0001 |
0.95 (0.94, 0.95) <0.0001 |
0.92 (0.90, 0.95) <0.0001 |
Data are Relative Risk (95% Confidence Interval) p-value
Model additionally controlled for state
When we examined the nine-year trend in the three states for which we had a longer data series, California, Illinois and New York, there was significant variation in the ectopic pregnancy rate by year (Figure 1) with a significant overall downward trend for each state from 2000 to 2008.
Figure 1. Ectopic Pregnancy Rates in the Medicaid Population, 2000–2008.
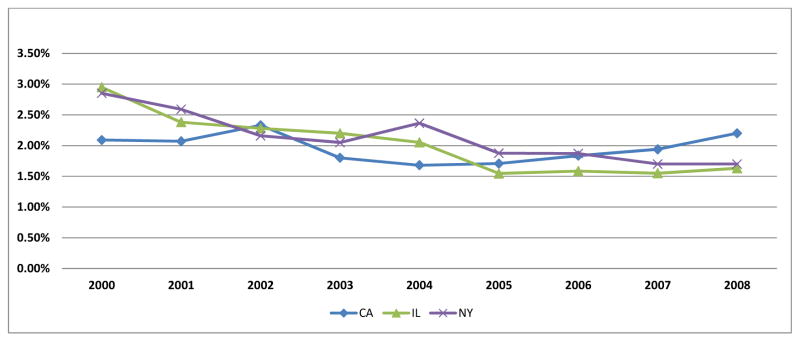
For all states: p-trend <0.0001
In exploratory analysis to explain state-level variation in ectopic pregnancy rates, the only factor significantly correlated with state Medicaid ectopic pregnancy rate was population density (ρ=0.64, p=0.01). We found moderate non-significant correlation (ρ=0.39, p=0.17) between ectopic pregnancy rate and the percent of ectopic pregnancy cases in which the woman was Medicaid-eligible in the months prior to developing an ectopic pregnancy. We found moderate non-significant correlation with published statewide chlamydia rate (ρ=0.39, p=0.16) and Gini coefficient (ρ=0.31, p=0.28) but not smoking (ρ=0.02, p=0.95) or median household income (ρ=0.16, p=0.59) by state. There was low correlation (ρ=−0.09, p=0.76) with state chlamydia rates within our Medicaid population, and also low correlation (ρ=0.14, p=0.64) with state proportion of births covered by Medicaid; there was no qualitative association with state Medicaid policy on abortion coverage.
DISCUSSION
African American women enrolled in Medicaid in 2004–08 were at significantly higher risk of ectopic pregnancy than white women in the 14 states studied. Age-adjusted ectopic pregnancy rates ranged from 0.91% of all pregnancies in Colorado, to 2.12% in Michigan, rates similar to those reported in other public and private insurance databases. In California, Illinois and New York, Medicaid ectopic pregnancy rates declined from 2000 to 2008.
The strength of our approach is that it provides a complete population count of ectopic pregnancy cases among women with Medicaid insurance in this 14-state population, using the most recently available Medicaid data. Medicaid covered 40% of all U.S. births in 2008 (22). The 14 states included in this study comprised nearly 60% of female Medicaid recipients of reproductive age in the United States.
Our study also has several limitations. First, we lacked clinician-or patient-reported information to validate the administrative claims data. Therefore, some of the ectopic pregnancies reported may be errors in coding or “rule-out” diagnoses. However, because our denominator captures all pregnancies with an even more permissive definition, we believe the risk of over-counting is at least as high in the denominator as the numerator, thereby decreasing the risk that we are overestimating the ectopic pregnancy rate. We were also unable to identify treatment modalities (surgical, medical, or expectant) for the ectopic pregnancies included. There is no reliable ICD9 diagnosis or procedure code for medical treatment of ectopic pregnancy (9); and Medicaid pharmacy files do not report medications that are dispensed the way methotrexate usually is for ectopic pregnancy: directly to the patient in a clinic, physician’s office, hospital, or emergency room. However, the study captured ectopic pregnancies treated in both inpatient and outpatient settings, in the same method as previously published for the Medicaid population (6). Another limitation is the possible exclusion of women within Medicaid who are enrolled in prepaid managed care programs. Medicaid managed care programs are obligated to submit claims data to CMS, however this reporting may be incomplete. Since capitated managed care providers do not rely on encounter-level claims to receive payment, their incentive to submit diagnosis and procedure codes by encounter is less than for fee-for-service providers. However, many individuals enrolled in Medicaid managed care programs participate in limited-scope programs, such as for the management of behavioral health care, or inpatient care. Pregnancy-related care could still be paid on a fee-for-service basis. Finally, it’s important to keep in mind that observed ectopic pregnancy rates can be affected by policy and demographic factors that affect the denominator (pregnancy among Medicaid beneficiaries). For example, we included induced abortion procedure codes in our denominator where they were reported, but lack of insurance coverage for induced abortion and under-use of insurance even where abortion is covered, is a concern in this and other ectopic pregnancy surveillance relying on claims data (6, 11). Furthermore, since we are unable to observe spontaneous abortions in which the woman does not seek health care, if women from different racial/ethnic groups varied in their likelihood of presenting for care during early pregnancy losses, this could affect our total pregnancy count in the denominator and thus our calculated ectopic pregnancy rates. However, in previous analyses (6), we demonstrated that adding or removing spontaneous and induced abortion diagnosis and procedure codes to our total pregnancy ascertainment method had no significant effect on overall rate calculations. We also previously found that changes to the time period defined as a single pregnancy episode had minimal effect on rate calculations. Our method used a 270-day (9-month) cut-off for a single pregnancy, and we cannot rule out that repeat early pregnancy losses (ectopic or intrauterine) and terminations may be missed in the denominator if, for example, two full episodes of care occurred within 9 months. However, when we previously compared this approach to 180-and 300-day cut-offs, we found similar results (6).
The marked state-by-state variation we observed in ectopic pregnancy rates (which was present even controlling for age and race) was surprising. We explored ecologic correlations between several state-level factors and the ectopic pregnancy rates. Because the sample size is very small, with only 14 states, we consider these analyses exploratory. While we found significant correlation between ectopic pregnancy rate and state population density, we cannot say if this relationship is meaningful. Overall state population density does not say anything about how the population is distributed. However, it may be reasonable to think that people living in densely populated areas have environmental exposures or behavior patterns that contribute to ectopic pregnancy risk. The moderate correlation with Medicaid eligibility rates prior to developing ectopic pregnancy may suggest that states with lower ectopic pregnancy rates represent under-reporting, if women who became eligible because of their ectopic pregnancy were less likely to become enrolled (and thus have their ectopic pregnancy reported) in some states compared to others. The moderate correlation (0.39) with statewide chlamydia rates was not surprising given that chlamydia is a recognized risk factor for ectopic pregnancy. These state-level correlations are intended to explore state-level factors that might be related to the variation we observe across states and are not intended to address individual-level risk factors for ectopic pregnancy, a topic beyond the scope of this study. Finally, the lack of association between ectopic pregnancy rates and either state policy on Medicaid abortion coverage or state proportion of births covered by Medicaid suggest that the observed state variation in ectopic pregnancy rate is not driven by these factors affecting total pregnancy counts in the denominator.
The implications of our findings are mixed. We are encouraged to see that in the states for which we have nine years’ worth of data (2000–08), ectopic pregnancy rates decreased slightly during this time period. This may be evidence of the benefits of clinical and preventive programs such as safer sex campaigns to prevent sexually transmitted infections, screening efforts to detect and treat these infections early, and smoking prevention and cessation programs. We cannot rule out other explanations.
The most striking finding is the persistent and consistent elevated risk of ectopic pregnancy faced by African American women. Medicaid eligibility was available to women in our study’s states at an income range from 150% of the federal poverty line (in Arizona) to 200% (in California, Colorado, Louisiana, and New York, among others), creating a population with a relatively narrow income distribution (20). Within this low-income population, across 14 states that vary greatly in their demographic makeup, the consistency of the black-white ectopic pregnancy disparity is remarkable. Elevated rates of chlamydia among African Americans compared to whites have been documented and may contribute to this disparity. Other factors that are more difficult to measure, such as possible delay in the diagnosis and treatment of sexually transmitted infections, causing fallopian tube scarring, may also play a role. Finally, chronic maternal stress has been associated with increased rates of preterm birth and low birth-weight (23, 24). This may contribute to racial disparities in maternal morbidity, including ectopic pregnancy.
Overall, this study suggests a lower total ectopic pregnancy rate among Medicaid recipients than we previously reported, since the previous study happened to only include highrate states, and even in those states, rates declined between the previous study period (2000–03) and this one (20004–08). However, ectopic pregnancy remains a serious health threat for all women, and among the Medicaid population African American women are at higher risk.
Acknowledgments
Financial Support: This work is supported by a career development award to Dr. Stulberg (1 K08 HD060663) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development
Footnotes
Disclosure: The authors report no conflict of interest
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy-related mortality in the United States, 1998 to 2005. Obstet Gynecol. 2010;116(6):1302–9. doi: 10.1097/AOG.0b013e3181fdfb11. [DOI] [PubMed] [Google Scholar]
- 2.Bouyer J, Coste J, Shojaei T, Pouly JL, Fernandez H, Gerbaud L, et al. Risk factors for ectopic pregnancy: a comprehensive analysis based on a large case-control, populationbased study in France. Am J of Epidemiol. 2003;157(3):185–94. doi: 10.1093/aje/kwf190. [DOI] [PubMed] [Google Scholar]
- 3.Creanga AA, Bateman BT, Kuklina EV, Callaghan WM. Racial and Ethnic Disparities in Severe Maternal Morbidity: a Multi-State Analysis, 2008–2010. Am J Obstet Gynecol. 2013 doi: 10.1016/j.ajog.2013.11.039. [DOI] [PubMed] [Google Scholar]
- 4.Callaghan WM, Creanga AA, Kuklina EV. Severe Maternal Morbidity Among Delivery and Postpartum Hospitalizations in the United States. Obstet Gynecol. 2012;120(5):1029–36. doi: 10.1097/aog.0b013e31826d60c5. [DOI] [PubMed] [Google Scholar]
- 5.Goldner TE, Lawson HW, Xia Z, Atrash HK. Surveillance for ectopic pregnancy--United States, 1970–1989. MMWR Weekly Report. 1993;42(6):73–85. [PubMed] [Google Scholar]
- 6.Stulberg DB, Cain LR, Dahlquist I, Lauderdale DS. Ectopic pregnancy rates in the Medicaid population. Am J Obstet Gynecol. 2013 Apr;208(4):274.e1–7. doi: 10.1016/j.ajog.2012.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Race, ethnicity, and nativity differentials in pregnancy-related mortality in the United States: 1993–2006. Obstet Gynecol. 2012 Aug;120(2 Pt 1):261–8. doi: 10.1097/AOG.0b013e31825cb87a. [DOI] [PubMed] [Google Scholar]
- 8.Goffman D, Madden RC, Harrison EA, Merkatz IR, Chazotte C. Predictors of maternal mortality and near-miss maternal morbidity. J Perinatol. 2007;27(10):597–601. doi: 10.1038/sj.jp.7211810. [DOI] [PubMed] [Google Scholar]
- 9.Zane SB, Kieke BA, Jr, Kendrick JS, Bruce C. Surveillance in a time of changing health care practices: estimating ectopic pregnancy incidence in the United States. Matern Child Health J. 2002;6(4):227–36. doi: 10.1023/a:1021106032198. [DOI] [PubMed] [Google Scholar]
- 10.Stulberg DB, Zhang JX, Lindau ST. Socioeconomic disparities in ectopic pregnancy: predictors of adverse outcomes from Illinois hospital-based care, 2000–2006. Matern Child Health J. 2011;15(2):234–41. doi: 10.1007/s10995-010-0579-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoover KW, Tao G, Kent CK. Trends in the diagnosis and treatment of ectopic pregnancy in the United States. Obstet Gynecol. 2010;115(3):495–502. doi: 10.1097/AOG.0b013e3181d0c328. [DOI] [PubMed] [Google Scholar]
- 12.Van Den Eeden SK, Shan J, Bruce C, Glasser M. Ectopic pregnancy rate and treatment utilization in a large managed care organization. Obstet Gynecol. 2005;105(5 Pt 1):1052–7. doi: 10.1097/01.AOG.0000158860.26939.2d. [DOI] [PubMed] [Google Scholar]
- 13.Trabert B, Holt VL, Yu O, Van Den Eeden SK, Scholes D. Correction. Am J Prev Med. 2012;42(1):107–8. doi: 10.1016/j.amepre.2010.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sonfield A. More Reproductive-Age Women Covered by Medicaid-But More Are Also Uninsured. Guttmacher Policy Review. 2007;10(1) [Google Scholar]
- 15.Centers for Disease Control and Prevention (CDC) [Accessed Jan. 3, 2014];Sexually Transmitted Disease Surveillance 2011, Figure A Data, All States. Available at: http://www.cdc.gov/std/Chlamydia2011/statesA.htm.
- 16.Centers for Disease Control and Prevention (CDC) State-Specific Prevalence of Cigarette Smoking Among Adults and Quitting Among Persons Aged 18–35 Years-United States, 2006, [Table 1] [Accessed Jan. 3, 2014];MMWR Mob Mortal Wkly. 2007 56(38):993–996. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5638a2.htm#tab1. [PubMed] [Google Scholar]
- 17.U.S. Census Bureau and Social Explorer. American Community Survey. (1-Year Estimates). Median Household Income. 2011 Available at: http://www.socialexplorer.com.proxy.uchicago.edu/tables/ACS2011/R10630234.
- 18.U.S. Census Bureau. Census. [Accessed Jan. 10, 2014];Population Density. 2000 Available at: http://old.socialexplorer.com.proxy.uchicago.edu/pub/reportdata/HtmlResults.aspx?reportid=R10640589.
- 19.U.S Census Bureau. Census. [Accessed Jan. 10, 2014];Population Density. 2000 Available at: http://old.socialexplorer.com.proxy.uchicago.edu/pub/reportdata/HtmlResults.aspx?reportid=R10640589.
- 20.Ranji U, Salganicoff A, Stewart AM, Cox M, Doamekpor L. State Medicaid coverage of perinatal services: Summary of state survey findings. Henry J. Kaiser Family Foundation; 2009. [Google Scholar]
- 21.Sonfield A, Gold RB. FY 1980–2010. New York: Guttmacher Institute; 2012. Public funding for family planning, sterilization and abortion services. [Google Scholar]
- 22.Markus AR, Andres E, West KD, Garro N, Pellegrini C. Medicaid covered births, 2008 through 2010, in the context of the implementation of health reform. Womens Health Iss. 2013;23(5):e273–80. doi: 10.1016/j.whi.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 23.Borders AE, Grobman WA, Amsden LB, Holl JL. Chronic stress and low birth weight neonates in a low-income population of women. Obstet Gynecol. 2007;109(2 Pt 1):331–8. doi: 10.1097/01.AOG.0000250535.97920.b5. [DOI] [PubMed] [Google Scholar]
- 24.Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM, McMahon MJ, Buekens P. Maternal stress and preterm birth. Am J Epidemiol. 2003;157(1):14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]


