Abstract
As the importance of providing patient-centered palliative care for patients with advanced illnesses gains attention, standard dialysis delivery may be inconsistent with the goals of care for many patients with ESRD. Many dialysis patients with life expectancy of <1 year may desire a palliative approach to dialysis care, which focuses on aligning patient treatment with patients’ informed preferences. This commentary elucidates what comprises a palliative approach to dialysis care and describes its potential and appropriate use. It also reviews the barriers to integrating such an approach into the current clinical paradigm of care and existing infrastructure and outlines system-level changes needed to accommodate such an approach.
Keywords: dialysis, end of life, palliative care
Introduction
In response to the high burden of physical and psychologic symptoms among individuals with ESRD, recent commentary has called for policies to promote palliative care (1). However, among the ESRD population undergoing maintenance dialysis, much of the symptom burden may be attributable to dialysis therapy itself, particularly for those nearing the end of life. Also needed, then, is a palliative approach to how dialysis care itself is provided, but the current system of dialysis delivery and regulatory oversight in the United States is not well suited to accommodate such an approach.
Defining a Palliative Approach to Dialysis Care
We define a palliative approach to dialysis care as a transition from a conventional disease-oriented focus on dialysis as rehabilitative treatment to an approach prioritizing comfort and alignment with patient preferences and goals of care to improve quality of life and reduce symptom burden for maintenance dialysis patients in their final year of life. This transition aligns with palliative care in general as well as with the current demographic of the United States dialysis population.
The Centers for Medicare & Medicaid Services (CMS) recognize palliative care as “patient- and family-centered care that optimizes quality of life by anticipating, preventing and treating suffering” (2). Provision of palliative care is appropriate at any age and at any stage in serious illness and it is not exclusively reserved for patients who have exhausted or decided to forgo life-prolonging therapies (3). CMS further states that “as age or illness progress, and cure or rehabilitation are no longer realistic expectations, care focuses increasingly on palliation” (2).
ESRD is a unique illness in that while there is no cure and it portends a higher mortality rate than do some cancers, some patients with ESRD survive decades while receiving dialysis or following transplantation (4). Therefore, a one-size-fits-all approach to dialysis care cannot be expected to meet the needs of such a heterogeneous demographic. This heterogeneity reflects a dramatic change in the ESRD patient population over the past 4 decades. A similar shift in how we approach dialysis care should follow suit.
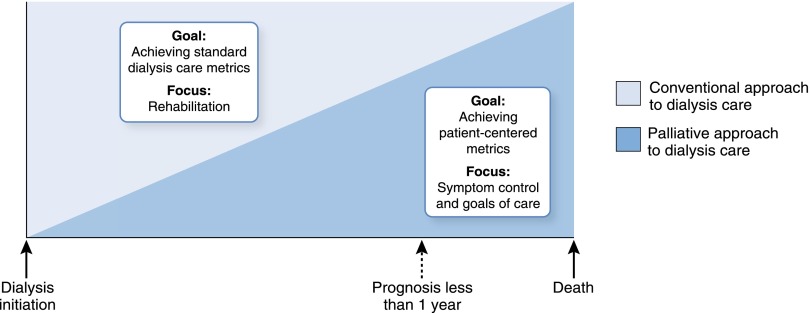
At the inception of the ESRD Medicare Entitlement Program in 1972, the ESRD population was predominantly young and not experiencing progressive comorbid disorders, such as diabetes. Accordingly, the primary goal of care beyond merely extending life was rehabilitation—to enable patients disabled by ESRD to return to work or normal activities. Currently, however, more than half of patients initiating dialysis are >60 years of age and have multiple chronic illnesses in addition to ESRD, so the predominant goal is often restricted to prolongation of life. Patients have a wide spectrum of prognoses, including many with a life expectancy of <1 year (4,5). For this group, the burdens of dialysis care may outweigh its benefits, thus making desirable a palliative approach to dialysis care in which the emphasis is shifted toward minimizing physical and psychologic burdens of standard maintenance dialysis schedules (such as fatigue and travel to and from dialysis), and away from achieving standard performance metrics (such as creation of an arteriovenous fistula or intensification of the dialysis prescription to achieve a target Kt/V) (Figure 1) (6).
Figure 1.
As the patient nears the end of life (dashed arrow), there is an increasing focus on symptom control and patient goals of care and a shift in the approach to dialysis care from conventional to palliative. Adapted from Institute of Medicine (59).
Several domains of care apply within a palliative approach to dialysis care. While the rigorous quality measurement framework outlined by National Quality Forum (NQF) is directly applicable to developing standards of care for conventional dialysis, the current specific measures endorsed by the organization have less relevance to a palliative approach to dialysis (7). Patient-centered metrics, such as those focused on quality of life, psychosocial health, and satisfaction with care, are not currently established by CMS or NQF for patients with CKD or ESRD. However, broad palliative care metrics endorsed by NQF and reported by the Center to Advance Palliative Care could be adapted to a palliative approach to dialysis care (1,8). Potential key domains include eliciting patient goals of care; physical, psychological, and spiritual symptom management; patient and caregiver satisfaction; and caregiver support (8).
Within this framework, dialysis care providers must assume responsibility for initiating discussion of goals and prognosis and encouraging patient-family communication, with the broad understanding that the goals of a palliative approach to dialysis care are to ameliorate symptoms and minimize suffering (9). Once identified, patient preferences for care should routinely be written as medical orders to ensure that patients receive the treatment they want throughout the health care system. The Physician Orders for Life-Sustaining Treatment (POLST) program has been validated and recommended as a best practice for patients whose physicians would not be surprised if they died in the next year (10,11). The POLST is intended to serve as a living documentation of patient preferences for current care among the seriously ill, in addition to medical orders for future end-of-life care (12). Because goals of care may change over time, this should be an iterative process, revisited over time (13). Similarly, it is imperative that symptoms, quality of life, and clinical status be regularly assessed and evaluated within a palliative approach to dialysis care.
Patient and caregiver satisfaction with care is also an important patient-centered domain for maintenance dialysis but has only recently been evaluated. Studies suggest patient satisfaction with care correlates with perceived quality of life and disease burden, thus supporting its relevance to a palliative approach to dialysis care (14,15).
Finally, social support for caregivers is linked to improvements in psychological health, adherence with treatment, and survival among dialysis patients (16). Whether the patient is undergoing in-center or home dialysis, the quality of life for the caregiver correlates strongly with the patients’ level of dependency (16,17). Patients choosing a palliative approach to dialysis care may be in the midst of substantial functional decline, and as this process unfolds, there will likely be more demands and stress on their caregivers (18).
Why a Palliative Approach to Dialysis Care Is Needed
In justifying the need for a palliative approach to dialysis care, it is important to underscore the substantial morbidity and mortality among maintenance dialysis patients. The mean age for prevalent dialysis patients in the United States is now 62.7 years, and the prevalence of maintenance dialysis among patients≥75 years of age has doubled during the last 2 decades (4). The dialysis population has an adjusted 76% 1-year survival rate and only a 36% 5-year survival rate (4). The adjusted mortality rate of maintenance dialysis patients is nearly twice that of adults with cancer and more than twice that of adults with congestive heart failure or stroke (4).
Patients treated with maintenance dialysis have a high prevalence of debilitating symptoms, which are multifactorial in origin and include uremia, other complications of ESRD, demands of routine dialysis, or comorbid conditions (19). Physical and emotional symptoms are highly prevalent, are often severe and undertreated, and correlate directly with impaired quality of life among maintenance dialysis patients (19–21). Using the Edmonton Symptom Assessment System, Davison et al. (22) found a mean of 7.5 symptoms per maintenance dialysis patient, 4.5 of which were characterized as moderate or severe on average. Using the Dialysis Symptom Index, Weisbord et al. (20) found a median of 9.0 symptoms among dialysis patients, with >50% reporting dry skin, fatigue, itching, and joint/bone pain.
In addition to the burdens of the dialysis procedure itself, initiation of dialysis often means that patients are committing themselves to intensive patterns of health care utilization, in many instances without full understanding and adequate discussion of the implications (23). Only 6%–35% of dialysis patients complete advance directives planning; the default then becomes intensive care patterns, including multiple admissions, surgical procedures, and resuscitation attempts at the end of life (13).
Most older dialysis patients in the United States initiate dialysis in the hospital, and many experience high rates of subsequent hospitalization (23). In a study of older Medicare patients starting dialysis, patients were classified into five levels of intensity of care, with the highest level being those who had longer than a 2-week hospital stay and received at least one intensive procedure, such as cardiopulmonary resuscitation, mechanical ventilation, or a feeding tube. In patients≥85 years who received the highest intensity of care, the median duration of survival after dialysis initiation was <6 months, with more than a third of that time spent in the hospital (23).
Many older adults treated with maintenance dialysis in the United States continue to receive aggressive care focused on life prolongation toward the end of their lives. Almost half (45%) of older United States dialysis patients die in a hospital setting as compared with 35% of Medicare beneficiaries with other severe chronic illness (including congestive heart failure, advanced liver disease, dementia, and chronic obstructive pulmonary disease) (24). Rates of hospitalization (76%) and intensive care unit (ICU) admission (49%) during the final month of life are also substantially higher than reported for other older Medicare beneficiaries, including those with cancer (of whom 61% are hospitalized and 24% are admitted to an ICU) and heart failure (of whom 64% are hospitalized and 19% are admitted to an ICU). Additionally, older dialysis patients spend twice as many days in the hospital during the last month of life as do Medicare recipients with cancer (9.8 versus 5.1 days) and are three times more likely to undergo an intensive procedure (29% versus 9%). In contrast, rates of palliative care and hospice utilization among dialysis patients at the end of life are extremely low (24). Compared with hospice use in patients with terminal cancer (55%) and heart failure (39%), hospice is used in only 20% among dialysis patients and is often only initiated within the last days of life (24–26).
These current patterns of death and treatment intensity do not appear congruent with patient wishes when actively elicited. In a study of United States maintenance dialysis patients, only 18% preferred to live as long as possible even if suffering (27). Similarly, in a study of patients with advanced CKD in Canada, a majority preferred their care to focus on decreasing pain and suffering, while only 18% favored dialysis to extend their lives (28). More patients wished to die at home (36%) or in an inpatient hospice (29%) than in a hospital (27%) (28).
Appropriate Use of a Palliative Approach to Dialysis Care
Given the high prevalence of advanced age, severe comorbid conditions, and high mortality rate among the ESRD population, a substantial proportion of patients undergoing maintenance dialysis may be nearing the end of life and could be candidates for a palliative approach to dialysis care (4,5,19). Such patients may have difficulty tolerating conventional dialysis regimens, and conversations with patients about preferences and goals of care are warranted. While a discussion of dialysis withdrawal may be considered, many patients and family members may not feel ready to discontinue dialysis completely because of concerns about suffering from ESRD-related symptoms or death within the mean 8-day time frame following dialysis cessation in patients with no residual kidney function (26,29–31). A palliative approach would not inevitably lead to withdrawal but could provide a transition to this option.
Specific clinical scenarios of maintenance dialysis patients with limited life expectancy in which a palliative approach to dialysis care may be considered include (1) the maintenance dialysis patient who develops a severe illness that causes an abrupt decline in life expectancy, (2) the patient started on dialysis in the setting of AKI with unclear life expectancy and goals of care, and (3) the maintenance dialysis patient with progressive functional or cognitive decline. In a palliative approach to dialysis care, the transition of care for each of these scenarios would begin with a conversation about the goals of care.
Barriers to a Palliative Approach to Dialysis
Provider Barriers
Several factors pose barriers to a palliative approach to dialysis care for appropriate patients. For example, while patients with ESRD prefer to be given information about their prognosis by their physicians and those who participate in end-of-life discussions tend to prefer less aggressive care, few dialysis patients report having had even limited discussions about their wishes (28,32–34). The dearth of discussions is likely fueled by provider uncertainty about prognosis and a lack of attention during training (35–37). However, reliable instruments have been developed to identify dialysis patients at highest risk of death, and fellowship training programs have been encouraged to attend more to building this skill (36,38,39).
A lack of understanding of palliative care and/or negative perceptions among patients, caregivers, and providers alike may also function as a barrier to a palliative approach to dialysis care (40,41). While current guidelines and practice standards have resulted in most dialysis staff being highly trained to recognize signs of underdialysis and fluid overload, few if any are trained to identify or manage symptoms that may be addressed with palliative care. Even small changes in protocols, such as relaxation of biochemical targets (e.g., for serum phosphorus) or flexibility around dialysis time/prescription, may be viewed as improper or inadequate care, thus leading to conflict among providers who strictly adhere to standard dialysis quality metrics versus those advocating for treatment aligned with the patient’s goals.
Fiscal Barriers
Economic and regulatory factors also pose barriers. As the payer of 90% of prevalent dialysis patients, CMS establishes the targets for dialysis care through its performance standards and frequently includes incentives to ensure an acceptable level of care (4,42). Within the ESRD Prospective Payment System, these incentives exist in the Quality Incentive Program, which is composed of performance metrics that include measures of dialysis dose, avoidance of high hemoglobin levels, and maximizing arteriovenous fistula use while minimizing central venous catheter use (43,44). End-of-life goals seldom conform to disease-focused incentivized metrics (Table 1), but the failure of a facility to achieve adequate performance on the Quality Incentive Program measures can result in up to a 2% loss of reimbursement for all Medicare beneficiaries in the facility (45). Therefore, the juxtaposition of incentivized metrics and individualized, patient-centered care may create conflict among the facility management (who bear the financial penalty for unmet metrics), physicians and other dialysis staff (who have an interest in seeing the facility succeed financially but are also charged with advocating for the best interests of the individual patient), and the patient (for whom goals may not align with quantifiable metrics).
Table 1.
Examples of approaches to common issues among maintenance dialysis patients in the current disease-focused dialysis delivery model versus a palliative approach to dialysis care model
| Issue | Current Disease-Focused Metrics for Conventional Delivery of Dialysis Care | A Patient-Centered Palliative Approach to Dialysis Care |
|---|---|---|
| Vascular access | Creation and maintenance of an AV fistula | Central venous catheter acceptable |
| Dialysis adequacy | Target small solute clearance based on current standards (Kt/V>1.2 for HD and Kt/V>1.7 for PD), intensifying the dialysis prescription as needed to achieve targets | Lower clearance acceptable if changes in dialysis prescription increase demands inconsistent with patient preference |
| Cardiovascular disease | Treat CV risk factors, potentially targeting BP and dyslipidemia | Tolerate hypertension to avoid symptoms; no indication for dyslipidemia treatment |
| Mineral and bone disorder | Dietary counseling; binders to control hyperphosphatemia; vitamin D analogues with or without calcimimetics for secondary hyperparathyroidism | Limited restrictions; more permissive hyperphosphatemia and hyperparathyroidism |
| Nutrition | Encourage dietary protein intake while limiting potassium (if HD), sodium, and phosphorus intake | Reduce dietary restrictions |
| Laboratory monitoring | Routine monthly laboratory tests | Minimal necessary |
AV, arteriovenous; HD, hemodialysis; PD, peritoneal dialysis.
Care Delivery Barriers
The lack of wide-scale infrastructure or universal reimbursement for providing staff-assisted home hemodialysis or peritoneal dialysis (PD) contributes to the underuse of a palliative approach to dialysis. Staff-assisted home dialysis, which involves the delivery of hemodialysis or PD with the aid of visiting nurses who assist to varying degrees in the tasks needed for the patient and/or caregiver to safely and effectively perform maintenance dialysis at home, is well established and supported by governments in Canada, France, Belgium, and Demark, but not in the United States (46–49). Staff-assisted home dialysis may be particularly attractive over facility-based hemodialysis for elderly, frail patients who would need varying degrees of assistance to perform dialysis at home, thus serving as a palliative approach to dialysis care by avoiding potentially lengthy transportation to and from the dialysis facility and potentially allowing the dose of dialysis to be better tailored to the needs of patients with variable uremic symptoms.
Finally, CMS policy regarding provision of hospice benefits for patients in whom ESRD is the primary terminal condition contributes to the underuse of a palliative approach to dialysis care by requiring that hospice agencies pay for the costs of continuing dialysis care in such cases (50). Such a proposition is not financially tenable for hospice providers, thus potentially depriving such patients who have a life expectancy consistent with hospice requirements (<6 months) an important aspect of supportive care services.
Recommendations for Implementing a Palliative Approach to Dialysis Care
Achieving the most effective use of a palliative approach to dialysis care requires several system-wide changes. We suggest the following recommendations to accommodate this approach (Table 2):
Table 2.
Proposed recommendations and barriers addressed
| Recommendation | Barriers Addressed |
|---|---|
| Nephrologists and nephrology fellows should develop expertise in discussing prognosis and goals of care | Nephrologists often lack skills to address prognosis and goals of care for patients with ESRD |
| Infrequent end-of-life discussions among dialysis patients | |
| Develop metrics for a palliative approach to dialysis care | Current standard-of-care metrics disease-focused rather than patient-centered |
| Determine the fiscal impact of a palliative approach to dialysis care | Inflexible in-center hemodialysis schedules |
| Lack of reimbursement for staff-assisted home dialysis | |
| Hospice benefit covers dialysis only if terminal illness other than ESRD |
Recommendation #1: Nephrologists and Nephrology Fellows Should Develop Expertise in Discussing Prognosis and Goals of Care
Reliable instruments have been developed to help identify dialysis patients at highest risk of death within a 6- and 12-month time frame and should be used widely (38,39). Nephrology organizations have long advocated shared decision-making and discussion of prognosis for patients with AKI, advanced CKD, and ESRD (51). Palliative care physicians have recommended that nephrologists and other physicians providing primary care to specific disease populations develop generalist palliative care skill sets (37). These skill sets include basic management of symptoms and comfort with discussions about patients’ preferences for goals of treatment.
It is commonly assumed by clinicians that they do not have the time to discuss end-of-life issues with their patients and families and that sufficient space and privacy are not possible in the open dialysis unit. However, improved expertise would allow clinicians to facilitate such discussions with greater ease and efficiency. Further, patient and family members could be invited to have such discussions as part of care plan conferences that are already required by CMS.
Improving knowledge gaps in this area would require incorporation of skill sets into training program curricula for fellows (such as NephroTalk) and could be achieved through continuing medical education requirements for practicing nephrologists (52). Dialysis social workers and nursing staff may be tasked with following up with end-of-life discussions, the assignment of health care proxies, and completion of living wills, but nephrologists must remain primarily responsible for discussion of prognosis and goals of care with patients and families. Involvement of the dialysis team can facilitate the implementation of a palliative approach into dialysis care (41,53).
Recommendation #2: Develop Metrics for a Palliative Approach to Dialysis Care
Although important guidelines, working group publications, and initiatives focusing on palliative care in the ESRD population have increased awareness among nephrology providers, additional research and evidence is needed to inform appropriate standards of care for patients undergoing a palliative approach to dialysis care (51,54,55). Many questions remain unanswered, including better identification of patients who could benefit from a palliative approach, dosing and timing of dialysis, optimizing symptom management, and establishing patient-centered goals of care. Nevertheless, given the magnitude of burdens associated with dialysis near the end of life, implementing a palliative approach to dialysis care based on expert opinion is reasonable (56,57). Codifying quality metrics for a palliative approach to dialysis care could alleviate concerns of substandard care that does not align with the current disease-focused metrics, thereby promoting patient goals and improving utilization of appropriate services near the end of life.
Key domains for a palliative approach to dialysis care include elicitation of patient goals of care; physical, psychological, and spiritual symptom management; patient and caregiver satisfaction; and caregiver support. Potential metrics within these domains are summarized in Table 3.
Table 3.
Key domains and suggested quality metrics for a palliative approach to dialysis care
| Domain | Potential Metrics |
|---|---|
| Elicitation of patient goals of care | Documentation of discussion of prognosis |
| Frequency of documentation in medical orders, such as POLST, of patient goals of current care and preferences for life-sustaining treatments at the end of life | |
| Physical, psychological, and spiritual symptoms | Frequency of documentation of symptoms by the dialysis care team |
| Change in symptom scores over time | |
| Caregiver support | Documentation of discussion and offering of peer support programs and relevant social service programs to caregivers |
| Patient and caregiver satisfaction | Frequency of documentation of satisfaction by the dialysis care team |
| Change in satisfaction scores over time |
POLST, Physician Orders for Life-Sustaining Treatment.
Recommendation #3: Determine the Fiscal Impact of a Palliative Approach to Dialysis Care
A palliative approach to dialysis care by definition targets maintenance dialysis patients nearing the end of life who want to minimize the intensity of care in order to focus on living as comfortably as possible, rather than on meeting current standard-of-care metrics for maximal rehabilitation and survival. However, given the inflexibility of the in-center hemodialysis environment, deviations from conventional thrice-weekly dialysis treatment schedules to variable once- or twice-weekly dialysis treatments would be both inefficient and expensive since utilization of and hence reimbursement for each potential treatment in each shift would not be maximized. This further underscores the value of incorporating the option of staff-assisted home dialysis, which could be a way to circumvent the issue of inflexible schedules for in-center hemodialysis as well as be an option for patients for whom travel to a dialysis facility is burdensome. Existing models of delivering and funding staff-assisted home hemodialysis or PD should be explored for implementation in the United States (46,58).
Finally, facility-specific standardized mortality ratios and quality measures for dialysis patients should be distinct and reported separately for those undergoing a palliative approach to dialysis care versus those seeking aggressive therapy and rehabilitation. Current practices of aggregating data for all dialysis patients regardless of their goals of care misrepresent the delivered quality of care as reported on public reporting sites, discourage a palliative approach and may have negative financial consequences for dialysis providers (45,51). A failure to implement a separate reporting mechanism representing achievement of standards specific to patients choosing a palliative approach could lead to dialysis providers “cherry-picking” and, worse, subjecting patients nearing the end of life to unwanted and possibly detrimental treatment.
Conclusion
A palliative approach to dialysis care could be an important aspect of treating selected patients on maintenance dialysis. As a patient-centered rather than disease-oriented approach to the delivery of dialysis care among patients with limited life expectancy, a palliative approach to dialysis care could alleviate the suffering of such patients. Much work is needed to facilitate incorporation of this approach into the existing dialysis delivery infrastructure in the United States in order to realize its most effective use.
Disclosures
V.G. received investigator-initiated research funding from Valeant Pharmaceuticals. S.V.J. received investigator-initiated research funding from Fresenius and speaker fees from Amgen. J.P. received speaking honoraria from Baxter Healthcare, Amgen Canada, and DaVita Healthcare Partners; consulting fees from Baxter Healthcare, Shire, Takeda, Janssen Inc.; and research support from Baxter Healthcare. D.W. received research funding from Dialysis Clinic, Inc. and was site principal investigator for clinical trials by Keryx (completed) and Janssen. R.M. received grant support and/or honoraria from Baxter Healthcare and DaVita.
Acknowledgments
V.G. was supported by grant 1K23-DK093710-01A1 from the National Institute of Diabetes and Digestive and Kidney Disease and by the Harold Amos Medical Faculty Development Program of the Robert Wood Johnson Foundation. L.M.C. and M.G. are supported by a grant from the Patient Centered Outcomes Research Institute on Shared Decision-Making and Renal Supportive Care.
V.G., M.J.F., J.P., and R.M. are members of the Dialysis Advisory Group of the American Society of Nephrology. D.W. was a member of the Dialysis Advisory Group at the time of manuscript conception, and S.V.J. and M.J.G. are members of the Geriatric Nephrology Advisory Group of the American Society of Nephrology (ASN). The opinions expressed in this manuscript are those of the authors and not necessarily the opinions of their institutions or of all the members of the ASN. The members of the ASN’s Dialysis and Geriatric Nephrology Advisory Groups and Communication Committee reviewed this manuscript prior to submission.
The following were the members of the Dialysis Advisory Group of the ASN at the time of writing this editorial: Gregory L. Braden (Springfield, MA), Christopher Chan (Toronto, ON, Canada), David Charytan (Boston, MA), Michael J. Fischer (Chicago, IL), Jennifer E. Flythe (Boston, MA), Vanessa Grubbs (San Francisco, CA), Adriana Hung (Nashville, TN), Frank Hurst (Silver Spring, MD), Mark Lukaszewski (Washington, DC; ASN Staff), Rajnish Mehrotra (Seattle, WA; Advisory Group Chair), Timothy W. Meyer (Palo Alto, CA), Sharon M. Moe (Indianapolis, IN; ASN Council liaison), Amy Barton Pai (Albany, NY), Jeffrey Perl (Toronto, ON, Canada), Shuvo Roy (San Francisco, CA), Michael J. Somers (Boston, MA), Isaac Teitelbaum (Denver, CO), and Leslie Wong (Cleveland, OH).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Tamura MK, Meier DE: Five policies to promote palliative care for patients with ESRD. Clin J Am Soc Nephrol 8: 1783–1790, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Medicare & Medicaid Services: Center for Clinical Standards and Quality/Survey & Certification Group. Ref: S&C 12-48-NH. 2012. Available at: http://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-12-48.pdf. Accessed February 20, 2014
- 3.Center to Advance Palliative Care: Defining palliative care: Building a palliative care program. 2013. Available at: http://www.capc.org/building-a-hospital-based-palliative-care-program/case/definingpc. Accessed October 23, 2013
- 4.U.S. Renal Data System: USRDS 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD, 2013. [Google Scholar]
- 5.Kurella M, Covinsky KE, Collins AJ, Chertow GM: Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med 146: 177–183, 2007 [DOI] [PubMed] [Google Scholar]
- 6.Trivedi DD: Palliative dialysis in end-stage renal disease. Am J Hosp Palliat Care 28: 539–542, 2011 [DOI] [PubMed] [Google Scholar]
- 7.The National Quality Forum: Measures, reports, and tools. 2013.http://www.qualityforum.org/Measures_Reports_Tools.aspx. Accessed November 17, 2013.
- 8.Weissman DE, Morrison RS, Meier DE: Center to Advance Palliative Care palliative care clinical care and customer satisfaction metrics consensus recommendations. J Palliat Med 13: 179–184, 2010 [DOI] [PubMed] [Google Scholar]
- 9.Holley JL: Palliative care in end-stage renal disease: Focus on advance care planning, hospice referral, and bereavement. Semin Dial 18: 154–156, 2005 [DOI] [PubMed] [Google Scholar]
- 10.Citko J, Moss AH, Carley M, Tolle SW: The National POLST Paradigm Initiative, 2nd ed. Fast Facts and Concepts. 2010. Available at:http://www.eperc.mcw.edu/EPERC/FastFactsIndex/ff_178.htm. Accessed November 1, 2013.
- 11.Hickman SE, Nelson CA, Moss AH, Tolle SW, Perrin NA, Hammes BJ: The consistency between treatments provided to nursing facility residents and orders on the physician orders for life-sustaining treatment form. J Am Geriatr Soc 59: 2091–2099, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bomba PA, Kemp M, Black JS: POLST: An improvement over traditional advance directives. Cleve Clin J Med 79: 457–464, 2012 [DOI] [PubMed] [Google Scholar]
- 13.Davison SN: Facilitating advance care planning for patients with end-stage renal disease: the patient perspective. Clin J Am Soc Nephrol 1: 1023–1028, 2006 [DOI] [PubMed] [Google Scholar]
- 14.Kimmel PL: Psychosocial factors in adult end-stage renal disease patients treated with hemodialysis: Correlates and outcomes. Am J Kidney Dis 35[Suppl 1]: S132–S140, 2000 [DOI] [PubMed] [Google Scholar]
- 15.Kirchgessner J, Perera-Chang M, Klinkner G, Soley I, Marcelli D, Arkossy O, Stopper A, Kimmel PL: Satisfaction with care in peritoneal dialysis patients. Kidney Int 70: 1325–1331, 2006 [DOI] [PubMed] [Google Scholar]
- 16.Patel SS, Peterson RA, Kimmel PL: The impact of social support on end-stage renal disease. Semin Dial 18: 98–102, 2005 [DOI] [PubMed] [Google Scholar]
- 17.Belasco A, Barbosa D, Bettencourt AR, Diccini S, Sesso R: Quality of life of family caregivers of elderly patients on hemodialysis and peritoneal dialysis. Am J Kidney Dis 48: 955–963, 2006 [DOI] [PubMed] [Google Scholar]
- 18.Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE: Functional status of elderly adults before and after initiation of dialysis. N Engl J Med 361: 1539–1547, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen LM, Moss AH, Weisbord SD, Germain MJ: Renal palliative care. J Palliat Med 9: 977–992, 2006 [DOI] [PubMed] [Google Scholar]
- 20.Weisbord SD, Fried LF, Arnold RM, Fine MJ, Levenson DJ, Peterson RA, Switzer GE: Prevalence, severity, and importance of physical and emotional symptoms in chronic hemodialysis patients. J Am Soc Nephrol 16: 2487–2494, 2005 [DOI] [PubMed] [Google Scholar]
- 21.Feldman R, Berman N, Reid MC, Roberts J, Shengelia R, Christianer K, Eiss B, Adelman RD: Improving symptom management in hemodialysis patients: Identifying barriers and future directions. J Palliat Med 16: 1528–1533, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davison SN, Jhangri GS, Johnson JA: Cross-sectional validity of a modified Edmonton symptom assessment system in dialysis patients: A simple assessment of symptom burden. Kidney Int 69: 1621–1625, 2006 [DOI] [PubMed] [Google Scholar]
- 23.Wong SP, Kreuter W, O’Hare AM: Healthcare intensity at initiation of chronic dialysis among older adults. J Am Soc Nephrol 25: 143–149, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wong SP, Kreuter W, O’Hare AM: Treatment intensity at the end of life in older adults receiving long-term dialysis. Arch Intern Med 172: 661–663, discussion 663–664, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murray AM, Arko C, Chen SC, Gilbertson DT, Moss AH: Use of hospice in the United States dialysis population. Clin J Am Soc Nephrol 1: 1248–1255, 2006 [DOI] [PubMed] [Google Scholar]
- 26.O’Connor NR, Dougherty M, Harris PS, Casarett DJ: Survival after dialysis discontinuation and hospice enrollment for ESRD. Clin J Am Soc Nephrol 8: 2117–2122, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hines SC, Glover JJ, Babrow AS, Holley JL, Badzek LA, Moss AH: Improving advance care planning by accommodating family preferences. J Palliat Med 4: 481–489, 2001 [DOI] [PubMed] [Google Scholar]
- 28.Davison SN: End-of-life care preferences and needs: Perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol 5: 195–204, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baumrucker SJ, Carter GT, Stolick M, Oertli KA, Sheldon JE, Morris GM: The case for “palliative dialysis.” Am J Hosp Palliat Care 26: 303–307, 2009 [DOI] [PubMed] [Google Scholar]
- 30.Fissell RB, Bragg-Gresham JL, Lopes AA, Cruz JM, Fukuhara S, Asano Y, Brown WW, Keen ML, Port FK, Young EW: Factors associated with “do not resuscitate” orders and rates of withdrawal from hemodialysis in the international DOPPS. Kidney Int 68: 1282–1288, 2005 [DOI] [PubMed] [Google Scholar]
- 31.Murtagh FE, Addington-Hall JM, Edmonds PM, Donohoe P, Carey I, Jenkins K, Higginson IJ: Symptoms in advanced renal disease: A cross-sectional survey of symptom prevalence in stage 5 chronic kidney disease managed without dialysis. J Palliat Med 10: 1266–1276, 2007 [DOI] [PubMed] [Google Scholar]
- 32.Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, Mitchell SL, Jackson VA, Block SD, Maciejewski PK, Prigerson HG: Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 300: 1665–1673, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Holley JL, Hines SC, Glover JJ, Babrow AS, Badzek LA, Moss AH: Failure of advance care planning to elicit patients’ preferences for withdrawal from dialysis. Am J Kidney Dis 33: 688–693, 1999 [DOI] [PubMed] [Google Scholar]
- 34.Fine A, Fontaine B, Kraushar MM, Rich BR: Nephrologists should voluntarily divulge survival data to potential dialysis patients: A questionnaire study. Perit Dial Int 25: 269–273, 2005 [PubMed] [Google Scholar]
- 35.Davison SN, Jhangri GS, Holley JL, Moss AH: Nephrologists’ reported preparedness for end-of-life decision-making. Clin J Am Soc Nephrol 1: 1256–1262, 2006 [DOI] [PubMed] [Google Scholar]
- 36.Holley JL, Carmody SS, Moss AH, Sullivan AM, Cohen LM, Block SD, Arnold RM: The need for end-of-life care training in nephrology: National survey results of nephrology fellows. Am J Kidney Dis 42: 813–820, 2003 [DOI] [PubMed] [Google Scholar]
- 37.Quill TE, Abernethy AP: Generalist plus specialist palliative care—creating a more sustainable model. N Engl J Med 368: 1173–1175, 2013 [DOI] [PubMed] [Google Scholar]
- 38.Cohen LM, Ruthazer R, Moss AH, Germain MJ: Predicting six-month mortality for patients who are on maintenance hemodialysis. Clin J Am Soc Nephrol 5: 72–79, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moss AH, Ganjoo J, Sharma S, Gansor J, Senft S, Weaner B, Dalton C, MacKay K, Pellegrino B, Anantharaman P, Schmidt R: Utility of the “surprise” question to identify dialysis patients with high mortality. Clin J Am Soc Nephrol 3: 1379–1384, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Davison SN, Jhangri GS, Koffman J: Knowledge of and attitudes towards palliative care and hospice services among patients with advanced chronic kidney disease [published online ahead of print June 10, 2014]. BMJ Support Palliat Care 10.1136/bmjspcare-2013-000610 [DOI] [PubMed] [Google Scholar]
- 41.Thompson KF, Bhargava J, Bachelder R, Bova-Collis R, Moss AH: Hospice and ESRD: knowledge deficits and underutilization of program benefits. Nephrol Nurs J 35: 461–466, 502, quiz 467–468, 2008 [PubMed] [Google Scholar]
- 42.Chambers JD, Weiner DE, Bliss SK, Neumann PJ: What can we learn from the U.S. expanded end-stage renal disease bundle? Health Policy 110: 164–171, 2013 [DOI] [PubMed] [Google Scholar]
- 43.Centers for Medicare & Medicaid Services: ESRD Quality Incentive Program. 2013. Available at: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/ESRDQIP/index.html. Accessed November 17, 2013.
- 44.Centers for Medicare & Medicaid Services : Final CY, End-Stage Renal Disease Prospective Payment System. ; 2013, pp 1352–F2012 [Google Scholar]
- 45.Weiner DE: The 2011 ESRD prospective payment system: Welcome to the bundle. Am J Kidney Dis 57: 539–541, 2011 [DOI] [PubMed] [Google Scholar]
- 46.Brown EA, Dratwa M, Povlsen JV: Assisted peritoneal dialysis—an evolving dialysis modality. Nephrol Dial Transplant 22: 3091–3092, 2007 [DOI] [PubMed] [Google Scholar]
- 47.Castrale C, Evans D, Verger C, Fabre E, Aguilera D, Ryckelynck JP, Lobbedez T: Peritoneal dialysis in elderly patients: Report from the French Peritoneal Dialysis Registry (RDPLF). Nephrol Dial Transplant 25: 255–262, 2010 [DOI] [PubMed] [Google Scholar]
- 48.Brown EA: Peritoneal dialysis in the elderly. Contrib Nephrol 163: 264–269, 2009 [DOI] [PubMed] [Google Scholar]
- 49.Oliver MJ, Quinn RR, Richardson EP, Kiss AJ, Lamping DL, Manns BJ: Home care assistance and the utilization of peritoneal dialysis. Kidney Int 71: 673–678, 2007 [DOI] [PubMed] [Google Scholar]
- 50.Centers for Medicare & Medicaid Services: Medicare Benefit Policy Manual. Rev. 177, 12-13-13. Available at http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c11.pdf. Accessed April 4, 2014 [Google Scholar]
- 51.Renal Physicians Association and American Society of Nephrology: Shared Decision-Making in the Appropriate Initiation of and Withdrawal from Dialysis, 2nd Ed. Washington, DC, Renal Physicians Association and American Society of Nephrology, 2010 [Google Scholar]
- 52.Schell JO, Green JA, Tulsky JA, Arnold RM: Communication skills training for dialysis decision-making and end-of-life care in nephrology. Clin J Am Soc Nephrol 8: 675–680, 2013 [DOI] [PubMed] [Google Scholar]
- 53.Singh P, Germain MJ, Cohen L, Unruh M: The elderly patient on dialysis: Geriatric considerations. Nephrol Dial Transplant 29: 990–996, 2014 [DOI] [PubMed] [Google Scholar]
- 54.Moss AH, Holley JL, Davison SN, Dart RA, Germain MJ, Cohen L, Swartz RD: Palliative care. Am J Kidney Dis 43: 172–173, 2004 [DOI] [PubMed] [Google Scholar]
- 55.Germain M, Cohen LM: Renal supportive care: View from across the pond: the United States perspective. J Palliat Med 10: 1241–1244, 2007 [DOI] [PubMed] [Google Scholar]
- 56.Churchill DN, Jassal SV: Dialysis: destination or journey [Published online ahead of print May 15, 2014]. J Am Soc Nephrol 10.1681/ASN.2014040390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vandecasteele SJ, Kurella Tamura M: A patient-centered vision of care for ESRD: Dialysis as a bridging treatment or as a final destination? [published online ahead of print May 15, 2014] J Am Soc Nephrol 10.1681/ASN.2013101082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Agraharkar M, Barclay C, Agraharkar A: Staff-assisted home hemodialysis in debilitated or terminally ill patients. Int Urol Nephrol 33: 139–144, 2002 [DOI] [PubMed] [Google Scholar]
- 59.Institute of Medicine: Improving palliative care for cancer: Summary and recommendations. 2003 Available at: http://iom.edu/~/media/Files/Report Files/2003/Improving-Palliative-Care-for-Cancer-Summary-and-Recommendations/PallativeCare8pager.pdf. Accessed February 20, 2014