Abstract
Background and objectives
Patients undergoing hemodialysis have an elevated risk of cardiovascular disease–related morbidity and mortality compared with the general population. Intradialytic hypotension (IDH) is estimated to occur during 20%–30% of hemodialysis sessions. To date, no large studies have examined whether IDH is associated with cardiovascular outcomes. This study determined the prevalence of IDH according to interdialytic weight gain (IDWG) and studied the association between IDH and outcomes for cardiovascular events and mortality to better understand its role.
Design, setting, participants, & measurements
This study retrospectively examined records of 39,497 hemodialysis patients during 2007 and 2008. US Renal Data System claims and dialysis provider data were used to determine outcomes. IDH was defined by current Kidney Disease Outcomes Quality Initiative guidelines (≥20 mmHg fall in systolic BP from predialysis to nadir intradialytic levels plus ≥2 responsive measures [dialysis stopped, saline administered, etc.]). IDWG was measured absolutely (in kilograms) and relatively (in percentages).
Results
IDH occurred in 31.1% of patients during the 90-day exposure assessment period. At baseline, the higher the IDWG (relative or absolute), the greater the frequency of IDH (P<0.001). For all-cause mortality, the median follow-up was 398 days (interquartile range, 231–602 days). Compared with patients without IDH, IDH was associated with all-cause mortality (7646 events; adjusted hazard ratio, 1.07 [95% confidence interval, 1.01 to 1.14]), myocardial infarction (2396 events; 1.20 [1.10 to 1.31]), hospitalization for heart failure/volume overload (8896 events; 1.13 [1.08 to 1.18]), composite hospitalization for heart failure/volume overload or cardiovascular mortality (10,805 events; 1.12 [1.08 to 1.17]), major adverse cardiac events (MACEs; myocardial infarction, stroke, cardiovascular mortality) (4994 events, 1.10 [1.03 to 1.17]), and MACEs+ (MACEs plus arrhythmia or hospitalization for heart failure/volume overload) (12,221 events; 1.14 [1.09 to 1.19]).
Conclusions
IDH was potently associated with cardiovascular morbidity and mortality. Clinical trials to ascertain causality are needed and should consider reduction in IDWG as a potential means to reduce IDH.
Keywords: cardiovascular disease, hemodialysis, ESRD, hypotension
Introduction
Patients with ESRD undergoing hemodialysis (HD) are at greater risk of cardiovascular (CV) disease–related morbidity and mortality compared with the general population, with published estimates suggesting that the differential risk is as high as 8- to 20-fold (1,2).
The higher burden of CV disease–related events may be due in part to episodic tissue hypoxia resulting from intradialytic hypotension (IDH). The National Kidney Foundation Kidney Disease Outcomes Quality Initiative (KDOQI) defines IDH as “a decrease in systolic BP by ≥ 20 mmHg or a decrease in mean arterial pressure by 10 mmHg associated with symptoms that include abdominal discomfort; yawning; sighing; nausea; vomiting; muscle cramps; restlessness; dizziness or fainting; and anxiety” (3). On the basis of the KDOQI definition, IDH occurs in approximately 20%–30% of all HD sessions (4).
IDH mainly occurs during dialysis when plasma fluid removal through ultrafiltration outpaces the rate of refilling (5). Although all patients undergoing HD are at risk of IDH due to the change in blood volume caused by ultrafiltration, some patients are at greater risk, including elderly individuals (aged >65 years), those with diabetes, those who are CV compromised, and those who present with low predialysis systolic BP (<100 mmHg) (6).
In addition to a reduced sense of well-being caused by the symptoms of IDH, patients who experience IDH have been shown to be at higher risk of mortality (7).
To date, no large-scale studies have examined whether IDH is associated with CV clinical outcomes. We do know that IDH is related to interdialytic weight gain (IDWG), which has been associated with higher risk of all-cause mortality, CV events, and CV mortality (8,9). Greater IDWG implies the need for more rapid fluid removal because dialysis time is essentially fixed for individual patients. Thus, it stands to reason that greater IDWG is related to greater IDH. Therefore, we measured the frequency of IDH according to IDWG, a potentially modifiable variable, and the association between IDH and CV events or mortality.
Materials and Methods
Data were obtained from a large dialysis organization’s (LDO’s) centralized data warehouse (CDW) and the US Renal Data System (USRDS) claims data. The CDW is the repository for the integrated electronic health records of nearly 150,000 patients with ESRD per year. These health records capture 100% of patient demographic information, laboratory values, dialysis treatment records, insurer, quality-of-life evaluation results, and comorbidity information. Use of in-center HD was defined using CDW data, which provides treatment-by-treatment records of the modality delivered. Comorbidities were assessed based on data from the US Centers for Medicare and Medicaid Services (CMS) Form 2728 (from the USRDS), which is submitted for all patients at the time of dialysis initiation, and supplemented with CMS claims data (from the USRDS) and electronic health record data (from the CDW) to capture comorbidities that manifest between dialysis initiation and the start of the at-risk period. Death data were taken from the CDW.
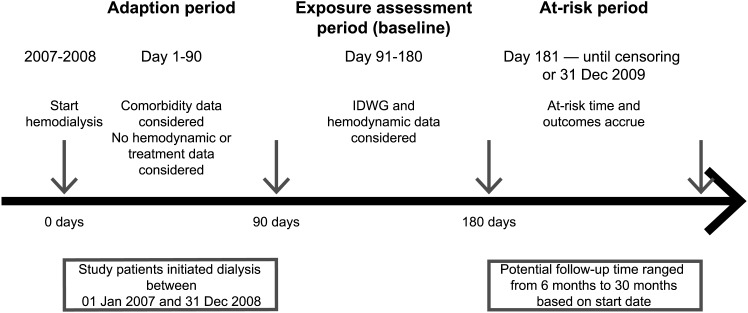
This study examined patients with ESRD who began in-center HD at the LDO between January 1, 2007, and December 31, 2008, within 30 days of first dialysis. Observation was restricted to patients who remained on in-center HD until the start of at-risk time (day 181 of dialysis to allow for 90 days of equilibration to dialysis followed by an additional 90 days over which exposures were assessed; Figure 1). Patients were considered at risk for outcome beginning on day 181 of dialysis and continuing until death, transfer of care away from the LDO (including voluntary withdrawals), modality change (including transplant, recovery of renal function), or the end of the study period (December 31, 2009). Because outcome data were ascertained from Medicare claims files, inclusion was limited to patients with Medicare Part A primary insurance.
Figure 1.
Schema depicting timing of study periods.
IDH was defined as patients having at least one treatment during the period dialysis day 91 to dialysis day 180 that met both of the following criteria: a fall in systolic BP of ≥20 mmHg from predialysis to nadir intradialytic levels (3), accompanied by at least two responsive measures (reduction in ultrafiltration rate, reduction in HD blood flow rate, saline administration, or premature cessation of dialysis according to guidelines).
Absolute IDWG was defined as predialysis weight from one treatment minus postdialysis weight from the prior treatment. This represents fluid accumulation between dialysis treatments (1 kg of weight gain for approximately 1 liter of fluid accumulated). Each patient’s mean value was calculated over dialysis days 91–180. Relative IDWG was defined as a percentage of postdialysis weight. This measure described the amount of fluid accumulated between dialysis treatments as a function of the patient’s body size. Each patient’s mean absolute and relative IDWG was calculated over dialysis days 91–180.
Outcomes were defined based on claims data from the USRDS. Patients were considered at risk beginning on day 181 of dialysis and continuing until death, transfer of care away from the LDO (including voluntary withdrawals), modality change (including transplant, recovery of renal function), or end of the study period (December 31, 2009). Outcomes included the following: all-cause mortality; CV mortality (death attributed to myocardial infarction, atherosclerotic heart disease, cardiac arrhythmia, congestive heart failure, cardiomyopathy, cardiac arrest, valvular heart disease, pulmonary edema, cerebrovascular accident including intracranial hemorrhage, or ischemic brain damage/anoxic encephalopathy); myocardial infarction; hospitalization for heart failure/fluid overload, composite heart failure/fluid overload hospitalization, or CV mortality; major adverse cardiac events (MACEs), including nonfatal myocardial infarction, nonfatal ischemic stroke, and CV death; MACEs+ (events comprising MACEs as well as arrhythmia, nonfatal hemorrhagic stroke, or hospitalization for heart failure); and hospitalization for atrial fibrillation.
Baseline cross-sectional associations were estimated for each exposure with demographic factors and comorbid conditions to estimate the burden of illness that might confound associations with outcomes by t testing and chi-squared testing as dictated by data type. Associations between exposures and outcomes were estimated using proportional hazards regression. Estimation was done on a crude basis as well as adjusted for baseline differences in demographic and comorbid conditions.
Results
A total of 39,497 patients receiving treatment between January 1, 2007, and December 31, 2008, were considered in this study. These patients are characterized in Table 1. Compared with patients who did not experience IDH during the exposure assessment period of the study (n=27,212), patients with IDH (n=12,285) were younger (60.9 versus 62.7 years), less frequently women (53.7% versus 57.2%), less frequently white (44.4% versus 46.8%), and more frequently black (34.3% versus 30.5%). The most common causes of ESRD were diabetes (46.0% for controls versus 49.6% for patients with IDH) and hypertension (31.0% for controls versus 29.1% for patients with IDH). The modality of vascular access was similar between patients with IDH and controls, with 61.3% and 63.3% having a central venous catheter, 28.3% and 27.4% having an arteriovenous fistula, and 10.4% and 9.3% having an arteriovenous graft, respectively. Comorbidity presence between patients with IDH and controls was similar for uncontrolled hypertension (95.9% versus 94.5%), heart failure (39.6% versus 40.0%), myocardial infarction (24.5% versus 25.5%), CV disease (8.6% versus 8.8%), and atrial fibrillation (4.9% versus 6.4%). Patients with IDH had more diabetes (70.7%) than controls (67.1%). Prior kidney transplant history was present in 1.8% of patients without IDH, and 1.7% of patients with IDH. Compared with patients who did not experience IDH, patients with IDH had greater absolute (4.52 kg versus 4.15 kg) and relative (3.30% versus 3.11% of body weight) IDWG.
Table 1.
Characteristics of study participants (n=39,497)
| Characteristic | IDH Absent | IDH Presenta | P |
|---|---|---|---|
| Participants | 27,212 (68.9) | 12,285 (31.1) | |
| IDH frequency (% of treatment) | Not applicable | ||
| >0 to ≤5 | 6096 (15.4) | ||
| >5 to ≤10 | 3789 (9.6) | ||
| >10 | 2400 (6.1) | ||
| Age, yr | 62.7±15.3 | 60.9±15.1 | <0.001 |
| Women | 15,564 (57.2) | 6598 (53.7) | <0.001 |
| Race/ethnicity | <0.001 | ||
| White | 12,728 (46.8) | 5459 (44.4) | |
| Black | 8302 (30.5) | 4214 (34.3) | |
| Hispanic | 4088 (15.0) | 1709 (13.9) | |
| Other/unknown | 2094 (7.7) | 903 (7.4) | |
| Cause of ESRD | 0.001 | ||
| Diabetes | 12,514 (46.0) | 6094 (49.6) | |
| Hypertension | 8434 (31.0) | 3579 (29.1) | |
| Glomerular disease | 1988 (7.3) | 860 (7.0) | |
| Other | 4276 (15.7) | 1752 (14.3) | |
| Prior transplant | 488 (1.8) | 209 (1.7) | 0.50 |
| Access type | <0.001 | ||
| Catheter | 17,216 (63.3) | 7535 (61.3) | |
| Fistula | 7442 (27.4) | 3476 (28.3) | |
| Graft | 2533 (9.3) | 1272 (10.4) | |
| Prevalent diabetesb | 18,246 (67.1) | 8691 (70.7) | <0.001 |
| Prevalent HFb | 10,871 (40.0) | 4864 (39.6) | 0.50 |
| Prevalent MIb | 6970 (25.6) | 3012 (24.5) | 0.02 |
| Prevalent atrial fibrillationb | 1733 (6.4) | 606 (4.9) | <0.001 |
| Prevalent CVDc | 2375 (8.8) | 1049 (8.6) | 0.50 |
| Uncontrolled hypertensiond | 25,725 (94.5) | 11,777 (95.9) | <0.001 |
| IDWG | |||
| Absolute (kg) | 4.15±2.44 | 4.52±2.24 | <0.001 |
| Relative ( %) | 3.11±1.80 | 3.30±1.60 | <0.001 |
Data are presented as the mean±SD or n (%). IDH, intradialytic hypotension; HF, heart failure; MI, myocardial infarction; CVD, cerebrovascular disease; IDWG, interdialytic weight gain; CMS, US Centers for Medicare and Medicaid Services; EMR, electronic medical record.
IDH is defined as one or more episodes during which systolic BP fell by at least 20 mmHg (predialysis to nadir intradialytic) accompanied by at least two responsive measures (premature cessation of dialysis, administration of saline, reduction in ultrafiltration rate, reduction in blood flow rate) over the period dialysis day 91 through dialysis day 180.
Defined based on CMS Medical Evidence Form 2728 data, claims (one inpatient or two outpatient), or DaVita EMR records before dialysis day 180.
Defined based on CMS Medical Evidence Form 2728 data, claims (one inpatient or two outpatient), or DaVita EMR record before dialysis day 180. Includes ischemic stroke, hemorrhagic stroke, and transient ischemic attack.
Defined as mean predialysis BP>140/90 mmHg or postdialysis BP>130/85 mmHg during the exposure assessment period (dialysis days 91–180).
BPs were considered for patients over dialysis days 91–180 of the exposure assessment study period. During this baseline assessment phase, 31.1% of patients experienced IDH at least once. When an alternative definition of IDH was considered based on the same BP change plus one responsive measure (rather than two), 90.4% of patients experienced IDH during the assessment period (data not shown). Because this proportion of patients was grossly inconsistent with clinical experience, the alternative definition was not considered in subsequent analyses.
Mean predialysis systolic BP was greater among patients with IDH than controls (150.9 mmHg versus 146.8 mmHg, respectively), postdialysis systolic BP was similar (141 mmHg in both groups), and nadir intradialytic systolic BP was lower for those with IDH (113.4 mmHg versus 115.4 mmHg). Mean predialysis diastolic BP was higher for patients with IDH than controls (78.9 mmHg versus 76.9 mmHg), postdialysis diastolic BP was the same for both groups (74 mmHg), and nadir intradialytic diastolic pressure was lower for patients with IDH (64.5 mmHg versus 65.1 mmHg).
Event rates for outcomes of interest during the at-risk period (on or after dialysis day 181) are provided in Table 2. Hospitalizations for heart failure/volume overload occurred at a rate of 243.9 events/1000 patient-years. All-cause mortality occurred at a rate of 141.9 deaths/1000 patient-years, CV mortality at 55.8 deaths/1000 patient-years, MACEs (including nonfatal myocardial infarction, nonfatal ischemic stroke, and CV death) at 107.7 events/1000 patient-years, and MACEs+ (plus arrhythmia, nonfatal hemorrhagic stroke, and heart failure) at 325.0 events/1000 patient-years. The median duration of study over the at-risk period varied according to outcome; for all-cause mortality, the median follow-up was 398 days (interquartile range, 231–602 days).
Table 2.
Incidence rates and cumulative incidence of outcomes during the at-risk period (n=39,782)
| Variablea | Affected Patients, n (%) | Incidence Rate per 1000 Patient-Years (95% CI) |
|---|---|---|
| Hospitalization for HF/volume overload | 8896 (22.4) | 243.9 (238.9 to 249.1) |
| Composite hospitalization for HF/volume overload or CV mortality | 10,805 (27.2) | 278.3 (272.9 to 283.7) |
| CV mortalityb | 2976 (7.5) | 55.8 (53.6 to 58.2) |
| All-cause mortality | 7646 (19.2) | 141.9 (138.3 to 145.6) |
| Myocardial infarction | 2396 (6.0) | 59.5 (57.1 to 61.9) |
| MACEc | 4994 (12.6) | 107.7 (104.6 to 111.0) |
| MACE+d | 12,221 (30.7) | 325.0 (319.2 to 331.0) |
| Hospitalization for atrial fibrillation | 2789 (7.0) | 69.7 (67.2 to 72.4) |
HF, heart failure; CV, cardiovascular; MACE, major adverse cardiovascular event; 95% CI, 95% confidence interval.
At-risk period began on dialysis day 181 and continued until death or censoring (as described in the text).
CV deaths defined as those attributed to myocardial infarction, atherosclerotic heart disease, cardiac arrhythmia, congestive HF, cardiomyopathy, cardiac arrest, valvular heart disease, pulmonary edema, cerebrovascular accident including intracranial hemorrhage, or ischemic brain damage/anoxic encephalopathy.
MACE is nonfatal myocardial infarction, nonfatal ischemic stroke, and CV death.
MACE+ is MACE plus arrhythmia, nonfatal hemorrhagic stroke, and HF.
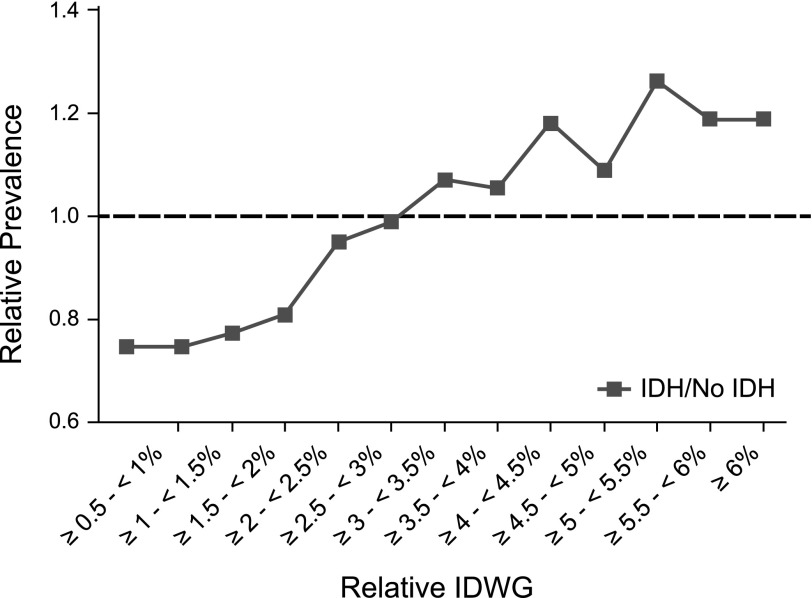
Table 3 provides a cross-sectional analysis of absolute and relative IDWG and IDH at baseline. Results demonstrated a potent and statistically significant association between IDH and IDWG (P<0.001). This was true for both absolute IDWG, which was defined as predialysis weight from one treatment minus postdialysis weight from the prior treatment, and relative IDWG, defined as a percentage of postdialysis weight. When IDWG metrics were considered dichotomously, 30.32% of patients with IDH experienced IDWG≥3 kg compared with 24.67% of patients without IDH (P<0.001). When expressed as a relative value, 40.33% of patients with IDH had relative IDWG≥3.5% compared with 35.61% of patients who did not experience IDH (P<0.001).
Table 3.
Cross-sectional associations of baseline absolute and relative IDWG with baseline IDH
| Absolute IDWG (n=39,497)a | Relative IDWG (n=39,497)b | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| IDWG (kg) | n | IDH Absent | IDH Present | P | IDWG (%) | n | IDH Absent | IDH Present | P |
| <0.5 | 1418 | 1060 (3.90) | 358 (2.91) | <0.001 | <0.5 | 922 | 690 (2.54) | 232 (1.89) | <0.001 |
| ≥0.5 to <1.0 | 2436 | 1866 (6.86) | 570 (4.64) | ≥0.5 to <1.0 | 1260 | 941 (3.46) | 319 (2.60) | ||
| ≥1.0 to <1.5 | 4729 | 3500 (12.86) | 1229 (10.00) | ≥1.0 to <1.5 | 2251 | 1670 (6.14) | 581 (4.73) | ||
| ≥1.5 to <2.0 | 6638 | 4674 (17.18) | 1964 (15.99) | ≥1.5 to <2.0 | 3851 | 2825 (10.38) | 1026 (8.35) | ||
| ≥2.0 to <2.5 | 7360 | 5048 (18.55) | 2312 (18.82) | ≥2.0 to <2.5 | 5081 | 3554 (13.06) | 1527 (12.43) | ||
| ≥2.5 to <3.0 | 6456 | 4332 (15.92) | 2124 (17.29) | ≥2.5 to <3.0 | 5851 | 4042 (14.85) | 1809 (14.73) | ||
| ≥3.0 to <3.5 | 4525 | 2948 (10.83) | 1577 (12.84) | ≥3.0 to <3.5 | 5635 | 3799 (13.96) | 1836 (14.95) | ||
| ≥3.5 to <4.0 | 2834 | 1825 (6.71) | 1009 (8.21) | ≥3.5 to <4.0 | 4870 | 3297 (12.12) | 1573 (12.80) | ||
| ≥4.0 to <4.5 | 1539 | 971 (3.57) | 568 (4.62) | ≥4.0 to <4.5 | 3448 | 2253 (8.28) | 1195 (9.73) | ||
| ≥4.5 to <5.0 | 737 | 439 (1.61) | 298 (2.43) | ≥4.5 to <5.0 | 2258 | 1514 (5.56) | 744 (6.06) | ||
| ≥5.0 to <5.5 | 377 | 255 (0.94) | 122 (0.99) | ≥5.0 to <5.5 | 1521 | 968 (3.56) | 553 (4.50) | ||
| ≥5.5 to <6.0 | 183 | 120 (0.44) | 63 (0.51) | ≥5.5 to <6.0 | 957 | 623 (2.29) | 334 (2.72) | ||
| ≥6.0 | 265 | 174 (0.64) | 91 (0.74) | ≥6.0 | 1592 | 1036 (3.81) | 556 (4.53) | ||
| <3.0 | 29,058 | 20,498 (75.33) | 8560 (69.98) | <0.001 | <3.5 | 24,851 | 17,521 (64.39) | 7330 (59.67) | <0.001 |
| ≥3.0 | 10,439 | 6714 (24.67) | 3725 (30.32) | ≥3.5 | 14,646 | 9691 (35.61) | 4955 (40.33) | ||
Data are presented as n (%) unless otherwise specified.
IDWG and IDH defined during the exposure assessment period (dialysis days 91–180). The primary definition of IDH is defined as a fall in systolic BP (predialysis to nadir intradialytic) of ≥20 mmHg or more accompanied by at least two responsive measures (reduction in ultrafiltration rate, reduction in blood flow rate, administration of saline, or premature cessation of dialysis). n=27,212 (68.9%) for IDH absent and n=12,285 (31.1%) for IDH present.
IDWG and IDH defined during the exposure assessment period (dialysis days 91–180). Relative IDWG is defined as IDWG as a percentage of postdialysis weight. Primary definition of IDH defined as a fall in systolic BP (predialysis to nadir intradialytic) of ≥20 mmHg accompanied by at least two responsive measures (reduction in ultrafiltration rate, reduction in blood flow rate, administration of saline, or premature cessation of dialysis). n=27,212 (68.9%) for IDH absent and n=12,285 (31.1%) for IDH present.
Figure 2 displays the prevalence of IDH as a function of relative IDWG. IDH was incrementally greater with greater IDWG. According to this analysis, IDH was least prevalent in patients who experienced relative IDWG<3%.
Figure 2.
Association between relative IDWG and IDH. Relative prevalence of IDH by relative IDWG category (P<0.001) is defined as the ratio of the proportion of patients who experienced IDH to the proportion of patients who did not within each relative IDWG category. IDH, intradialytic hypotension; IDWG, interdialytic weight gain; Rel, relative.
Table 4 presents the crude and adjusted associations between IDH and incident outcomes during the at-risk period (dialysis day 181, continuing until death or censoring). Unadjusted associations of IDH showed higher hazard ratios (HRs [95% confidence intervals]) for myocardial infarction (1.14 [1.04 to 1.24]), hospitalization for heart failure/volume overload (1.08 [1.04 to 1.13]), composite hospitalization for heart failure/volume overload or CV mortality (1.08 [1.03 to 1.12]), and MACEs+ (1.08 [1.04 to 1.12]), than for those without IDH. Findings were not significant for all-cause mortality, CV mortality, MACEs, or hospitalization for atrial fibrillation.
Table 4.
Unadjusted and adjusted associations of IDH with incident clinical outcomes (n=39,497)
| IDHa | Crude | Adjustedb | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| All-cause mortality (7646 qualifying events) | ||||
| IDH absent | 1 (ref) | — | 1 (ref) | — |
| IDH present overall (versus absent) | 1.00 (0.95 to 1.06) | 0.94 | 1.07 (1.01 to 1.14) | 0.01 |
| >0% to ≤5% of treatments (versus absent) | 1.05 (0.98 to 1.13) | 0.17 | ||
| >5% to ≤10% of treatments (versus absent) | 1.04 (0.95 to 1.14) | 0.41 | ||
| >10% of treatments (versus absent) | 1.19 (1.06 to 1.34) | 0.004 | ||
| CV mortality (2976 qualifying events)c | ||||
| IDH absent | 1 (ref) | — | 1 (ref) | — |
| IDH present overall (versus absent) | 0.93 (0.85 to 1.02) | 0.14 | 1.00 (0.91 to 1.10) | 0.99 |
| >0 to ≤5% of treatments (versus absent) | 0.96 (0.85 to 1.09) | 0.55 | ||
| >5 to ≤10% of treatments (versus absent) | 0.94 (0.81 to 1.10) | 0.46 | ||
| >10% of treatments (versus absent) | 1.22 (1.02 to 1.48) | 0.03 | ||
| Myocardial infarction (2396 qualifying events) | ||||
| IDH absent | 1 (ref) | — | 1 (ref) | — |
| IDH present overall (versus absent) | 1.14 (1.04 to 1.24) | 0.01 | 1.20 (1.10 to 1.31) | <0.001 |
| >0 to ≤5% of treatments (versus absent) | 1.15 (1.04 to 1.30) | 0.01 | ||
| >5 to ≤10% of treatments (versus absent) | 1.27 (1.10 to 1.45) | 0.001 | ||
| >10% of treatments (versus absent) | 1.20 (1.00 to 1.45) | 0.05 | ||
| Hospitalization for HF/volume overload (8896 qualifying outcomes) | ||||
| IDH absent | 1 (ref) | — | 1 (ref) | — |
| IDH present overall (versus absent) | 1.08 (1.04 to 1.13) | <0.001 | 1.13 (1.08 to 1.18) | <0.001 |
| >0% to ≤5% of treatments (versus absent) | 1.09 (1.03 to 1.15) | 0.01 | ||
| >5% to ≤10% of treatments (versus absent) | 1.16 (1.08 to 1.25) | <0.001 | ||
| >10% of treatments (versus absent) | 1.22 (1.11 to 1.34) | <0.001 | ||
| Composite hospitalization for HF/volume overload or CV mortality (10,805 qualifying outcomes)c | ||||
| IDH absent | 1 (ref) | — | 1 (ref) | — |
| IDH present overall (versus absent) | 1.08 (1.03 to 1.12) | <0.001 | 1.12 (1.08 to 1.17) | <0.001 |
| >0% to ≤5% of treatments (versus absent) | 1.08 (1.02 to 1.14) | 0.01 | ||
| >5% to ≤10% of treatments (versus absent) | 1.14 (1.06 to 1.22) | <0.001 | ||
| >10% of treatments (versus absent) | 1.26 (1.15 to 1.37) | <0.001 | ||
| MACEs (4994 qualifying events)d | ||||
| IDH absent | 1 (ref) | — | 1 (ref) | — |
| IDH present overall (versus absent) | 1.04 (0.97 to 1.11) | 0.27 | 1.10 (1.03 to 1.17) | 0.01 |
| >0% to ≤5% of treatments (versus absent) | 1.06 (0.97 to 1.15) | 0.18 | ||
| >5% to ≤10% of treatments (versus absent) | 1.09 (0.98 to 1.22) | 0.10 | ||
| >10% of treatments (versus absent) | 1.23 (1.08 to 1.41) | 0.002 | ||
| MACEs+ (12,221 qualifying events)e | ||||
| IDH absent | 1 (ref) | — | 1 (ref) | — |
| IDH present overall (versus absent) | 1.08 (1.04 to 1.12) | <0.001 | 1.14 (1.09 to 1.19) | <0.001 |
| >0% to ≤5% of treatments (versus absent) | 1.08 (1.02 to 1.14) | 0.004 | ||
| >5% to ≤10% of treatments (versus absent) | 1.17 (1.10 to 1.25) | <0.001 | ||
| >10% of treatments (versus absent) | 1.29 (1.19 to 1.40) | <0.001 | ||
| Hospitalization for atrial fibrillation (2789 qualifying events) | ||||
| IDH absent | 1 (ref) | — | 1 (ref) | — |
| IDH present overall (versus absent) | 0.89 (0.82 to 0.97) | 0.01 | 1.04 (0.95 to 1.13) | 0.38 |
| >0% to ≤5% of treatments (versus absent) | 1.00 (0.90 to 1.11) | 0.98 | ||
| >5% to ≤10% of treatments (versus absent) | 1.03 (0.89 to 1.18) | 0.72 | ||
| >10% of treatments (versus absent) | 1.19 (1.00 to 1.42) | 0.07 | ||
Estimates reported as HRs (95% CIs). n=27,212 (68.9%) for IDH absent and n=12,285 (31.1%) for IDH present. HR, hazard ratio.
IDH defined during the exposure assessment period (dialysis days 91–180) as a fall in systolic BP (predialysis to nadir intradialytic) of ≥20 mmHg accompanied by at least two responsive measures (reduction in ultrafiltration rate, reduction in blood flow rate, administration of saline, or premature cessation of dialysis).Outcomes considered beginning on dialysis day 181 and continuing until death or censoring (as described in the text). Cumulative patient-years at risk were 26,245 for hospitalization for HF/volume overload, 26,206 for composite hospitalization for HF/volume overload or CV mortality, 29,249 for CV mortality, 29,210 for all-cause mortality, 30,595 for myocardial infarction, 29,594 for MACEs, 25,891 for MACEs+, 29,062 for postdialytic complications, and 27,105 for hospitalization for atrial fibrillation.
Adjusted for age, race, sex, cause of ESRD, prior renal transplant, access type, uncontrolled hypertension (mean predialysis BP>140/90 mmHg or mean postdialysis BP>130/85 mmHg during exposure period; dialysis days 91–180), and the following prevalent at baseline (on or before dialysis day 180): diabetes, HF, myocardial infarction, atrial fibrillation, and cerebrovascular disease (ischemic/hemorrhagic stroke or transient ischemic attack).
CV deaths defined as those attributed to myocardial infarction, atherosclerotic heart disease, cardiac arrhythmia, congestive HF, cardiomyopathy, cardiac arrest, valvular heart disease, pulmonary edema, cerebrovascular accident including intracranial hemorrhage, or ischemic brain damage/anoxic encephalopathy.
MACEs defined as nonfatal myocardial infarction, nonfatal stroke, or CV mortality.
MACEs+ defined as nonfatal myocardial infarction, nonfatal stroke, CV mortality, arrhythmia, nonfatal hemorrhagic stroke, or hospitalization for HF/volume overload.
Upon adjustment for baseline differences in age, race, sex, cause of ESRD, prior renal transplant, access type, uncontrolled hypertension, prevalent diabetes, heart failure, myocardial infarction, atrial fibrillation, and cerebrovascular disease (ischemic/hemorrhagic stroke or transient ischemic attack), the magnitude of association between IDH and outcomes was potentiated. Significant associations were observed of IDH with all-cause mortality (1.07 [1.01 to 1.14]), myocardial infarction (1.20 [1.10 to 1.31]), hospitalization for heart failure/volume overload (1.13 [1.08 to 1.18]), composite hospitalization for heart failure/volume overload or CV mortality (1.12 [1.08 to 1.17]), MACEs (1.10 [1.03 to 1.17]), and MACEs+ (1.14 [1.09 to 1.19]) (P<0.01). Findings were not significant for CV mortality or atrial fibrillation. When patients were subcategorized based on the frequency of IDH measured during the exposure assessment period, a dose-response association was observed for most outcomes. This was most apparent for MACEs, MACEs+, hospitalizations for heart failure and volume overload, and the composite measure for heart failure/volume overload, and CV mortality (Table 4).
Discussion
This retrospective study found a significant association between IDH and IDWG and that IDH was associated with CV events. These findings could have widespread implications in the treatment of patients with ESRD undergoing HD, considering that IDH is estimated to occur in 20%–30% of all dialysis treatments (depending on the definition used for IDH) (4), and that IDWG has been shown to increase the risk of CV events and mortality (10,11).
According to the USRDS, 37.9% of deaths among incident HD patients and 42.3% among prevalent HD patients are due to CV disease, including acute myocardial infarction, congestive heart failure, arrhythmia and cardiac arrest, cerebrovascular accidents, and other cardiac and vascular disease (1). Individuals with CKD have up to a 10- to 20-fold greater risk of cardiac death than age- and sex-matched controls without CKD (12,13).
Preventing or controlling for hypertension can reduce CV risk in the general population. Strict BP control, however, is challenging in the ESRD population, and the relationship between IDH and predialysis and postdialysis BP is complex (9,14). One study examined strict control of BP to minimize the risk of hypertension. The researchers found that patients had higher rates of IDH at dialysis centers that achieved postdialysis BP targets (130/80 mmHg) than patients at clinics that did not achieve these targets (15).
A possible explanation is the relationship between IDH and myocardial stunning. Myocardial stunning refers to transient abnormalities in cardiac regional wall motion that occur in the presence of coronary hypoperfusion. Because coronary flow is dependent on central arterial pressure, rapid reductions in BP predispose to myocardial stunning, which has been shown to be predictive of CV events. Burton et al. found that 28% of patients with evidence of myocardial stunning died within a year, whereas those without evidence of myocardial stunning had a 100% survival rate for the same time period. They also found that myocardial stunning occurred in 60% of their HD patients and that myocardial hypoperfusion may lead to repeated episodes of subclinical hypoxic damage to the myocardium, as evidenced by intradialytic troponin leak; this has also been associated with adverse outcomes (16).
At baseline, there was a statistically significant association between IDWG and IDH; compared with patients with lower IDWG, greater IDWG (both absolute and relative) was associated with a higher likelihood of IDH. It is presumed that greater IDWG may predispose patients to IDH by virtue of a greater implied volume of fluid that must be removed in a fixed period. This clinic and patient-centered challenge is evident in this study because when further adjustments were made for dialysis session length, associations between IDH and outcome risks were unchanged. However, in many instances, dialysis session length is limited by patient symptoms. Davenport et al. found that 7% of all treatments were complicated by symptomatic hypotension and that this was more common in patients with large IDWG and lower predialysis BPs and pulse pressures (15). Using a different operational definition (>30 mmHg decrease in systolic BP to <90 mmHg), Sands et al. observed that IDH occurred in 17.2% of dialysis treatments (17). And as we found, IDH in their study was strongly associated with risk of hospitalization and death compared with patients who did not experience IDH. IDH definitions that include symptoms largely preclude large-scale study because symptoms data are not captured in large data sets.
In prior studies, the operational definition of IDH has varied widely; definitions have considered combinations of variables such as decreases in BP during dialysis, nadir BP with respect to prespecified thresholds, symptomatology, and therapeutic responses. We selected our operational definition to be closely aligned with KDOQI guidelines and because it is readily applied to data commonly available in large clinical data sets. As such, it is possible that IDH defined else wise may be more potently associated with outcomes; to the degree that this is true, our estimates are conservative. Additional study is needed to identify the optimal definition of IDH.
In this study, IDH was associated with a higher risk of heart failure, composite heart failure/CV mortality, myocardial infarction, and all-cause mortality (P<0.001). This observation supports earlier research showing a higher mortality risk with IDH. Shoji et al. found that the lowest intradialytic systolic BP was a significant risk factor for higher mortality and that intradialytic diastolic BP<59 mmHg was associated with a significantly higher risk of death from CV and cerebrovascular disease (7). This effect has also been seen in patients who experience perioperative hypotension (18,19) and peripartum hypotension (20). However, given the alarmingly high prevalence of hypotensive events and the poor underlying CV substrate for many dialysis patients, the relationship between hypotension and mortality may be more important for dialysis patients. Although no significant association was seen for IDH with CV mortality or atrial fibrillation, point estimates for atrial fibrillation were in the direction of higher risk.
It was previously demonstrated that patients who shorten their dialysis sessions have worse outcomes (13). The mechanisms for this phenomenon are unknown, although it may be related to inadequate fluid removal and greater IDWG. It is likely that longer dialysis treatments provide enhanced solute clearance beyond what is reflected by clearance of urea. It is also possible that prolonged dialysis sessions allow ultrafiltration to proceed slowly and in a manner that improves BP control and allows for consistent dry weight achievement (11).
We were able to demonstrate that greater IDWG is associated with a greater risk of IDH, likely as a result of the implied cyclical changes in extracellular volume. However, IDH is probably multifactorial. Unfortunately, available data precluded study of the effects of dialysis sodium concentration and dialysate temperature, both of which may also affect IDH (21). Furthermore, prior studies indicate that fluid status with respect to extracellular euvolemia may be an important determinant in IDH (22,23). In time, emerging technologies may enable real-time consideration of volume status to ameliorate IDH and downstream CV events. These technologies are not currently routinely used in the United States (and therefore could not be studied here). To date, analyses regarding the effect of such technologies have yielded mixed findings, possibly based on differences in protocolized responses to IDH. Further study is needed to optimally translate data on extracellular volume into clinical responses (23).
Observational analyses are valuable tools for studying population-level trends using real-world data derived from clinical patient databases; however, they have limitations. A limitation to our study is that residual urine output was not captured in the clinical database studied, and incident patients with urine output would have attenuated IDWG. It is reassuring, however, that the association between IDH and outcomes was constant over time and statistical tests for time×IDH interaction were nonsignificant (data not shown). In addition, our study did not consider the effects of oral medications to treat hypertension among patients with IDH. We feel that adjusting for antihypertensive medications, such as β-blockers, would implicitly assume effects on IDH, and analytical reparations for cardioprotective medication use might systematically bias findings. The nature of these study limitations demonstrates the need for prospective studies designed to examine cause and effect.
Looking forward, clinical trials are needed to determine whether amelioration of IDH improves patient outcomes. Such investigations may focus on patient sodium exposure from dialysate and diet or other strategies to mitigate IDWG. Current studies are looking at biofeedback or medication to control BP during dialysis, dialysate cooling, and increasing the frequency of dialysis to lower ultrafiltration rates and volumes (4,24–26).
Disclosures
B.V.S., C.C., D.R., and N.-O.S. are employees of AstraZeneca Inc. S.M.B., E.A., K.R., and D.E.J. are employees of DaVita Clinical Research. D.R. is employed by Ardelyx. The study on which this article was based, as well as manuscript development, was funded by Ardelyx Inc. and AstraZeneca Inc.
Acknowledgments
We thank DaVita Clinical Research for providing technical support for this research project. We also thank Michele G. Scheid of DaVita Clinical Research for medical writing and editorial support. DaVita Clinical Research is committed to advancing the knowledge and practice of kidney care.
This study was sponsored by Ardelyx Inc./AstraZeneca Inc.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Fluid Management: The Challenge of Defining Standards of Care,” on pages 2033–2035.
References
- 1.US Renal Data System: 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Available at http://www.usrds.org/atlas.aspx. Accessed October 10, 2013
- 2.Flythe JE, Kimmel SE, Brunelli SM: Rapid fluid removal during dialysis is associated with cardiovascular morbidity and mortality. Kidney Int 79: 250–257, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Kidney Foundation: KDOQI Clinical Practice Guidelines for Cardiovascular Disease in Dialysis Patients. Available at http://www.kidney.org/professionals/kdoqi/guidelines_cvd/intradialytic.htm. Accessed October 16, 2013 [PubMed]
- 4.Palmer BF, Henrich WL: Recent advances in the prevention and management of intradialytic hypotension. J Am Soc Nephrol 19: 8–11, 2008 [DOI] [PubMed] [Google Scholar]
- 5.Leypoldt JK, Cheung AK, Delmez JA, Gassman JJ, Levin NW, Lewis JA, Lewis JL, Rocco MV: Relationship between volume status and blood pressure during chronic hemodialysis. Kidney Int 61: 266–275, 2002 [DOI] [PubMed] [Google Scholar]
- 6.van der Sande FM, Kooman JP, Leunissen KM: Intradialytic hypotension—new concepts on an old problem. Nephrol Dial Transplant 15: 1746–1748, 2000 [DOI] [PubMed] [Google Scholar]
- 7.Shoji T, Tsubakihara Y, Fujii M, Imai E: Hemodialysis-associated hypotension as an independent risk factor for two-year mortality in hemodialysis patients. Kidney Int 66: 1212–1220, 2004 [DOI] [PubMed] [Google Scholar]
- 8.Kalantar-Zadeh K, Regidor DL, Kovesdy CP, Van Wyck D, Bunnapradist S, Horwich TB, Fonarow GC: Fluid retention is associated with cardiovascular mortality in patients undergoing long-term hemodialysis. Circulation 119: 671–679, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flythe JE, Inrig JK, Shafi T, Chang TI, Cape K, Dinesh K, Kunaparaju S, Brunelli SM: Association of intradialytic blood pressure variability with increased all-cause and cardiovascular mortality in patients treated with long-term hemodialysis. Am J Kidney Dis 61: 966–974, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stegmayr BG, Brannstrom M, Bucht S, Dimeny E, Ekspong A, Granroth B, Grontoft KC, Hadimeri H, Holmberg B, Ingman B, Isaksson B, Johansson G, Lindberger K, Lundberg L, Lundstrom O, Mikaelsson L, Mortzell M, Olausson E, Persson B, Svensson L, Wikdahl AM: Minimized weight gain between hemodialysis contributes to a reduced risk of death. Int J Artif Organs 29: 675–680, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Flythe JE, Curhan GC, Brunelli SM: Disentangling the ultrafiltration rate-mortality association: The respective roles of session length and weight gain. Clin J Am Soc Nephrol 8: 1151–1161, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foley RN, Parfrey PS, Sarnak MJ: Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis 32[Suppl 3]: S112–S119, 1998 [DOI] [PubMed] [Google Scholar]
- 13.Weiner DE, Tighiouart H, Amin MG, Stark PC, MacLeod B, Griffith JL, Salem DN, Levey AS, Sarnak MJ: Chronic kidney disease as a risk factor for cardiovascular disease and all-cause mortality: A pooled analysis of community-based studies. J Am Soc Nephrol 15: 1307–1315, 2004 [DOI] [PubMed] [Google Scholar]
- 14.Agarwal R: Interdialytic hypertension-an update. Adv Chronic Kidney Dis 18: 11–16, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davenport A, Cox C, Thuraisingham R: Achieving blood pressure targets during dialysis improves control but increases intradialytic hypotension. Kidney Int 73: 759–764, 2008 [DOI] [PubMed] [Google Scholar]
- 16.Burton JO, Jefferies HJ, Selby NM, McIntyre CW: Hemodialysis-induced cardiac injury: Determinants and associated outcomes. Clin J Am Soc Nephrol 4: 914–920, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sands JJ, Usvyat LA, Sullivan T, Segal JH, Zabetakis P, Kotanko P, Maddux FW, Diaz-Buxo JA: Intradialytic hypotension: Frequency, sources of variation and correlation with clinical outcome. Hemodial Int 18: 415–422, 2014 [DOI] [PubMed] [Google Scholar]
- 18.Bijker JB, Persoon S, Peelen LM, Moons KG, Kalkman CJ, Kappelle LJ, van Klei WA: Intraoperative hypotension and perioperative ischemic stroke after general surgery: A nested case-control study. Anesthesiology 116: 658–664, 2012 [DOI] [PubMed] [Google Scholar]
- 19.Walsh M, Devereaux PJ, Garg AX, Kurz A, Turan A, Rodseth RN, Cywinski J, Thabane L, Sessler DI: Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: Toward an empirical definition of hypotension. Anesthesiology 119: 507–515, 2013 [DOI] [PubMed] [Google Scholar]
- 20.Bánhidy F, Acs N, Puhó EH, Czeizel AE: Hypotension in pregnant women: A population-based case-control study of pregnancy complications and birth outcomes. Hypertens Res 34: 55–61, 2011 [DOI] [PubMed] [Google Scholar]
- 21.Kumar S, Khosravi M, Massart A, Potluri M, Davenport A: Are serum to dialysate sodium gradient and segmental bioimpedance volumes associated with the fall in blood pressure with hemodialysis? Int J Artif Organs 37: 21–28, 2014 [DOI] [PubMed] [Google Scholar]
- 22.Booth J, Pinney J, Davenport A: Do changes in relative blood volume monitoring correlate to hemodialysis-associated hypotension? Nephron Clin Pract 117: c179–c183, 2011 [DOI] [PubMed] [Google Scholar]
- 23.Dasselaar JJ, van der Sande FM, Franssen CF: Critical evaluation of blood volume measurements during hemodialysis. Blood Purif 33: 177–182, 2012 [DOI] [PubMed] [Google Scholar]
- 24.Breidthardt T, McIntyre CW: Dialysis-induced myocardial stunning: The other side of the cardiorenal syndrome. Rev Cardiovasc Med 12: 13–20, 2011 [DOI] [PubMed] [Google Scholar]
- 25.Jefferies HJ, Virk B, Schiller B, Moran J, McIntyre CW: Frequent hemodialysis schedules are associated with reduced levels of dialysis-induced cardiac injury (myocardial stunning). Clin J Am Soc Nephrol 6: 1326–1332, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Locatelli F, Altieri P, Andrulli S, Bolasco P, Sau G, Pedrini LA, Basile C, David S, Feriani M, Montagna G, Di Iorio BR, Memoli B, Cravero R, Battaglia G, Zoccali C: Hemofiltration and hemodiafiltration reduce intradialytic hypotension in ESRD. J Am Soc Nephrol 21: 1798–1807, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]