Abstract
Objective
Octogenarians (aged ≥ 80 years) are increasingly being referred for cardiac surgery. We aimed to describe the morbidity, mortality, and health services utilization of octogenarians undergoing elective cardiac surgery.
Methods
Retrospective population-based cohort study of adult patients receiving elective cardiac surgery between January 1 2004 and December 31 2009. Primary exposure was age ≥80 years. Outcomes were 30-day, 1- and 5-year mortality, post-operative complications, and ICU/hospital lengths of stay. Multi-variable logistic and Cox regression analyses were used to explore the association between older age and outcome.
Results
Of 6,843 patients receiving cardiac surgery, 544 (7.9%) were octogenarians. There was an increasing trend in the proportion of octogenarians undergoing surgery during the study period (0.3% per year, P = 0.073). Octogenarians were more likely to have combined procedures (valve plus coronary artery bypass or multiple valves) compared with younger strata (p < 0.001). Crude 30-day, 1-year and 5-year mortality for octogenarians were 3.7%, 10.8% and 29.0%, respectively. Compared to younger strata, octogenarians had higher adjusted 30-day (OR 4.83, 95%CI 1.30-17.92; P = 0.018) and 1-year mortality (OR 4.92; 95% CI, 2.32-10.46. P<0.001). Post-operative complications were more likely among octogenarians. Octogenarians had longer post-operative stays in ICU and hospital, and higher rates of ICU readmission (P < 0.001 for all). After multi-variable adjustment, age ≧ 80 years was an independent predictor of death at 30-days and 1 year.
Conclusions
Octogenarians are increasingly referred for elective cardiac surgery with more combined procedures. Compared to younger patients, octogenarians have a higher risk of post-operative complications, consume greater resources, and have worse but acceptable short and long-term survival.
Electronic supplementary material
The online version of this article (doi:10.1186/s13019-014-0177-6) contains supplementary material, which is available to authorized users.
Keywords: Octogenarian, Cardiac Surgery, Complication, Mortality
Background
Population aging is a global phenomenon with significant implications for health care systems in the developed world. In 2012, over 5.2 million people in Canada were aged over 65 years, representing 14.9% of total population. Of these, approximately 1.4 million (4.2% of total population) were octogenarians (aged ≥80 years) [1]. Associated with this increasingly older population, the demand for surgery, in particular cardiac surgery, is expected to markedly increase [2],[3].
Prior studies evaluating the course and outcomes of older patient receiving cardiac surgery have notable limitations, including being relatively small, only investigating certain type or types of cardiac procedures, failing to include adjusted analyses of outcomes relative to younger age strata, and reporting only on short-term outcomes [4]-[7].
We hypothesized that octogenarians undergoing cardiac surgery would have higher perioperative mortality and complication rates and consume greater health resources. Our objectives were to describe the population-based short-term and long-term mortality, major morbidity, and health services utilization in patients aged ≥80 years undergoing elective cardiac surgery.
Methods
The study was approved by the Health Research Ethics Board at the University of Alberta prior to commencement. The requirement for written consent was waived.
Study design, setting, population
This was a retrospective population-based cohort study performed at the Mazankowski Alberta Heart Institute (MAHI), University of Alberta (Edmonton, Canada) between January 1 2004 and December 31 2009. The MAHI is the only referral center for adult cardiac surgery in northern Alberta. There are nine adult cardiac surgeons at the MAHI performing approximately 1100–1200 adult open cardiac surgery procedures annually (excluding heart transplant, lung transplant, and mechanical assist device implantation).
All adult patients receiving elective cardiac surgery were potentially eligible. We excluded those patients receiving heart and lung transplantation, emergent cardiac surgery, mechanical assist device implantation and those aged less than 18 years. Octogenarians were defined by an age ≥80 years according to their age on the day of surgery. For the purpose of analyses, the entire cohort was categorized into four age strata: 18–49 years, 50–64 years, 65–79 and ≥80 years, respectively.
Study protocol
Patients were identified by interrogation of the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease (APPROACH)) registry. The APPROACH registry prospectively captures detailed clinical information on adult patients with known or suspected coronary artery disease (CAD) investigated in the province of Alberta (more information can be found at http://www.approach.org/). Patients entered into the registry are longitudinally followed after cardiac catheterization for all cardiac-specific investigations, interventions (i.e. percutaneous coronary intervention [PCI] or coronary artery bypass grafting surgery [CABG]) and outcomes. Data elements in the registry include socio-demographic features (i.e. age, sex), cardiovascular risk factors and co-morbidities (i.e. hypertension, dyslipidemia, stroke, congestive heart failure (CHF), chronic pulmonary disease, end stage kidney disease (ESKD) on dialysis, peripheral vascular disease (PVD), diabetes mellitus, liver and gastrointestinal disease, malignancy), coronary anatomy as defined by the Duke Index [8], left ventricular ejection fraction (EF), prior thrombolytic therapy, prior myocardial infarction (MI), prior CABG surgery, and prior angioplasty. In addition, the registry also captures several peri-operative variables specific for cardiac surgery (i.e. procedure type, cardiopulmonary bypass and aortic cross clamp time, use of intra-operative balloon pump [IABP]) and surgery specific complications and outcomes. Quarterly merges of the APPROACH registry with the Bureau of Vital Statistics was used for ascertainment of vital status.
Operational definitions
Post-operative major bleeding was defined as blood loss from chest tubes greater than 400 ml × 1 hr or 300 ml × 2 hrs or 200 ml × 3 hrs. Surgical wound infection was defined as purulent discharge from sternal wounds and/or positive culture results from blood, urine, sputum/lungs and incisions. Cardiac arrest was defined as a recorded cardiac arrest or pulseless electric arrest (PEA) in the post-operative period that required cardiopulmonary resuscitation. Heart block was defined as second degree type 2 or third degree heart block occurring beyond post-operative day 3. Pulmonary complication was defined as post-operative ventilation time greater than 48 hours or need for re-intubation. Neurologic complication was defined as post-operative transient ischemic attack (TIA), stroke or seizure. Acute kidney injury (AKI) was defined as an increase of ≥50% in serum creatinine (Cr) from pre-operative baseline value, or post-operative urine output <0.5 ml/kg/hr x 12 hours.
Statistical analysis
The primary exposure of interest across all analyses was octogenarians (i.e. age ≥80 years). The outcomes were 30-day, 1-year and 5-year mortality, post-operative complications (i.e. bleeding, infection, neurologic events, pulmonary complications, AKI, atrial fibrillation, cardiac arrest, heart block) and health service utilization (ICU stay, hospital stay and ICU re-admission). Continuous data were reported as means ± standard deviations (SD) and were compared by Student’s t-test and analysis of variance (ANOVA) where appropriate. Categorical data were reported as proportions and compared using χ2 test or Fisher’s exact test where appropriate. Multivariate logistic regression analysis was used to identify independent risk factors for 30-day and 1-year mortality in all patients with age strata. Initial covariates considered included sex, pre-operative co-morbid illnesses, procedure type, CPB and/or aortic cross clamp time, and post-operative complications. Data were presented as adjusted odds ratios (ORs) with 95% confidence intervals (CIs). Kaplan-Meier survival curve was used for survival analysis. Cox regression analysis was used to explore the association of long-term mortality across age strata while controlling for potential confounding covariates. The associations were reported as hazard ratios (HR) with 95% CIs. A p-value of <0.05 was considered statistically significant for all comparisons. All analysis was performed by using IBM SSPS software.
Results
Of 7,302 patients receiving cardiac surgery during the study, 23 (0.3%) were excluded due to age <18 years; 384 (5.3%) excluded due to emergent surgery, and 52 (0.7%) excluded due to missing data on the primary outcome. (Figure 1) The final cohort comprised of 6,843 patients undergoing elective cardiac surgery. Of these, 752 (11.0%) were aged between 18 to 49 years; 2,500 (36.5%) between 50 to 64 years; 3,047 (44.5%) between 65 to 79 years and 544 (7.9%) were aged ≥80 years. The median (range) age of those ≥80 years was 82.5 years (80.0-92.1), with 19.1% (n = 104) ≥85 years and 1.3% (n = 7) ≥90 years, respectively. Linear regression showed a trend for a greater proportion of patients aged ≥80 years receiving cardiac surgery during the study period (estimated relative annual increase 3%; P = 0.073) (Figure 2).
Figure 1.
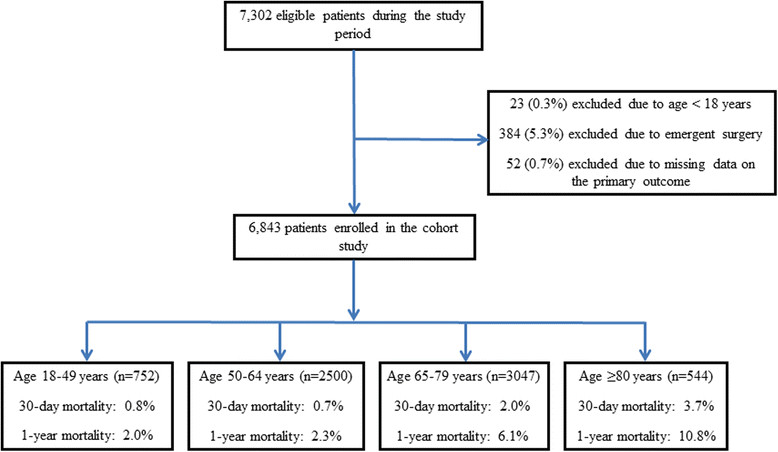
Flow diagram of study patients.
Figure 2.
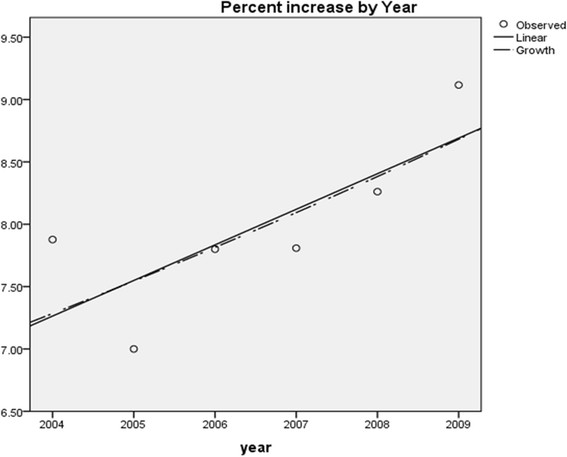
Annual proportions of octogenarians receiving cardiac surgery within the study period.
Baseline characteristics
Octogenarians had higher prevalence of hypertension, prior MI, CHF, stroke, and malignancy when compared with younger strata (Table 1). Octogenarians had lower prevalence of ESKD and had lower BMI values when compared with younger groups. Octogenarians were also less likely to be undergoing re-operation.
Table 1.
Pre-operative characteristics and type of surgery across the four age strata
| Variables | Age 18–49 (n = 752) | Age 50–64 (n = 2500) | Age 65–79 (n = 3047) | Age ≥80 (n = 544) | P value |
|---|---|---|---|---|---|
| Age (year) | 40.6 ± 8.9 | 58.5 ± 4.1 | 72.4 ± 4.3 | 83.1 ± 2.4 | <0.001 |
| Male (%) | 71.5% | 80.9% | 74.7% | 73.0% | <0.001 |
| Hypertension (%) | 42.9% | 77.6% | 84.3% | 86.0% | <0.001 |
| Hyperlipidemia (%) | 64.5% | 94.9% | 94.0% | 90.9% | <0.001 |
| Diabetes (%) | 14.9% | 33.8% | 34.0% | 26.1% | <0.001 |
| Previous MI (%) | 32.3% | 50.7% | 51.7% | 53.8% | <0.001 |
| CHF (%) | 12.0% | 11.7% | 17.8% | 24.5% | <0.001 |
| PVD (%) | 2.7% | 6.7% | 11.6% | 11.8% | <0.001 |
| Stroke (%) | 7.0% | 8.9% | 16.3% | 21.8% | <0.001 |
| CRF on dialysis (%) | 2.4% | 1.3% | 1.5% | 0.4% | 0.028 |
| Malignancy (%) | 1.3% | 2.0% | 5.6% | 7.2% | <0.001 |
| BMI | 29.4 ± 5.8 | 30.1 ± 5.9 | 28.8 ± 5.1 | 26.8 ± 4.5 | <0.001 |
| Re-operation (%) | 21.5% | 6.4% | 6.9% | 4.5% | <0.001 |
| Re-op adult congenital (%) | 10.2% | 0.3% | 0.1% | 0.0% | <0.001 |
| Pre-op Cr (μmol/L) | 108.1 ± 107.1 | 103.1 ± 79.0 | 112.1 ± 83.7 | 109.3 ± 39.5 | 0.04 |
| Type of Surgery | |||||
| CABG | 42.0% | 73.2% | 67.8% | 52.4% | <0.001 |
| AVR | 16.0% | 5.0% | 4.4% | 3.9% | <0.001 |
| MVR | 15.6% | 5.8% | 5.3% | 4.4% | <0.001 |
| Combined surgery | 9.8% | 12.6% | 21.2% | 36.3% | <0.001 |
| AVR + CABG | 1.2% | 4.6% | 11.1% | 24.3% | <0.001 |
| MVR + CABG | 1.3% | 4.1% | 5.5% | 5.0% | <0.001 |
| 2 or more valves | 7.3% | 3.9% | 4.6% | 7.0% | <0.001 |
| PVR/TVR | 10.6% | 1.0% | 0.5% | 0.0% | <0.001 |
| Others | 6.0% | 2.3% | 0.8% | 1.3% | <0.001 |
| CPB time (min) | 123.0 ± 62.1 | 115.9 ± 52.4 | 123.9 ± 55.2 | 129.6 ± 55.3 | <0.001 |
| Cross Clamp time (min) | 79.1 ± 54.9 | 78.7 ± 44.3 | 85.8 ± 47.9 | 92.0 ± 48.4 | <0.001 |
| off-pump surgery | 9.6% | 1.3% | 0.9% | 0.4% | <0.001 |
MI: myocardial infarct; CHF: congestive heart failure; PVD: peripheral vascular disease; ESKD: end stage kidney disease; BMI: body mass index; Cr: creatinine, EF: ejection fraction; CABG: coronary artery bypass grafting; AVR: aortic valve repair/replacement; MVR: mitral valve repair/replacement; PVR: pulmonary valve repair/replacement; TVR: tricuspid valve repair/replacement; CPB: cardiopulmonary bypass.
Surgery type
Octogenarians were more likely to undergo combined cardiac procedures, in particular aortic value replacement and coronary artery bypass, when compared with younger strata. This was associated with comparatively longer durations of CPB and aortic cross-clamp (Table 1).
Mortality
Crude 30-day, 1-year and 5-year mortality for octogenarians were 3.7%, 10.8% and 29.0%, respectively. The OR of adjusted 30-day and 1-year mortality in octogenarians were 4.83 (95% CI 1.30-17.92, P = 0.018) and 4.92 (95%CI 2.32-10.46, P < 0.001), respectively (referent group 18–49 years).
Post-operative complications
Octogenarians had significant higher risk for all major post-operative complications (bleeding, infection, neurologic events, pulmonary complications, AKI, atrial fibrillation, cardiac arrest, heart block). Octogenarians also had higher utilization of post-operative continuous renal replacement therapy (CRRT) and a trend for higher utilization of peri-operative IABP (Table 2).
Table 2.
Post-operative complications and health service utilization
| Variables | Age 18–49 (n = 752) | Age 50–64 (n = 2500) | Age 65–79 (n = 3047) | Age ≥80 (n = 544) | P value |
|---|---|---|---|---|---|
| Bleeding (re-exploration) | 2.0% | 1.4% | 2.3% | 2.8% | 0.04 |
| Infection | 6.2% | 7.4% | 11.4% | 13.4% | <0.001 |
| Neurologic events | 1.3% | 1.3% | 3.7% | 7.4% | <0.001 |
| Pulmonary complications | 14.1% | 12.7% | 20.5% | 30.3% | <0.001 |
| AKI | 6.5% | 4.7% | 11.2% | 16.2% | <0.001 |
| Atrial fibrillation | 15.1% | 28.0% | 41.1% | 45.8% | <0.001 |
| Cardiac arrest | 1.5% | 1.8% | 3.4% | 5.5% | <0.001 |
| Heart block | 2.7% | 1.8% | 2.9% | 5.0% | <0.001 |
| IABP | 3.0% | 3.1% | 3.9% | 4.2% | 0.27 |
| CRRT | 2.7% | 1.7% | 4.1% | 6.4% | <0.001 |
| CVICU LOS (hr) | 87.5 ± 385.6 | 67.7 ± 145.0 | 107.7 ± 248.7 | 158.8 ± 343.6 | <0.001 |
| Hospital LOS | 8.7 ± 14.4 | 8.1 ± 14.7 | 11.3 ± 17.7 | 15.8 ± 24.2 | <0.001 |
| CVICU re-admission | 3.9% | 2.6% | 4.6% | 9.0% | <0.001 |
| Discharge location | |||||
| Home | 92.1% | 90.6% | 77.1% | 56.1% | <0.001 |
| Other facilities | 7.9% | 9.4% | 22.9% | 43.9% | <0.001 |
AKI: acute kidney injury; IABP: intra-aortic balloon pump; CRRT: continuous renal replacement therapy; LOS: length of stay.
Health service utilization
Octogenarians had longer durations of stay in ICU and hospital (Table 2). Octogenarians were also considerably more likely to require ICU readmission. The crude 30-day, 1-year and 5-year mortality in octogenarians who had cardiovascular surgical ICU (CVICU) re-admission were 10.2%, 40.8% and 59.2%. The likelihood of not being discharged home or to a skilled nursing facility was higher for octogenarians (Table 2).
Factors associated with 30-day, 1-year and 5-year mortality
In multi-variable analysis, age ≥80 years was independently associated with increased risk of death at 30 days (adjusted OR 4.83, 95% CI 1.30-17.92, P = 0.0018) and at 1-year (adjusted OR 4.92, 95% CI 2.32-10.46, P < 0.001) (Tables 3 and 4).
Table 3.
Significant independent predictive variables for 30-day mortality by multivariate logistic regression analysis
| Factors | OR (95% CI) | P value |
|---|---|---|
| Pre-operative factors | ||
| Male sex | 3.00 (1.75-5.15) | <0.001 |
| Age ≥80 (referent group 18–49 years) | 4.83 (1.30-17.92) | 0.018 |
| ESKD on dialysis | 6.54 (2.52-16.94) | <0.001 |
| EF 35-50% (referent group EF > 50%) | 2.29 (1.08-4.86) | 0.032 |
| EF < 35% (referent group EF > 50%) | 4.07 (1.70-9.74) | 0.002 |
| Intra-operative factors | ||
| CPB time | 1.01 (1.01-1.02) | <0.001 |
| Post-operative complications | ||
| Pulmonary complications | 2.39 (1.30-4.41) | 0.005 |
| Cardiac arrest | 20.20 (10.64-38.34) | <0.001 |
| Acute kidney injury on CRRT | 5.13 (2.57-10.21) | <0.001 |
OR: odds ratio; CI: confidence interval; CRF: chronic renal failure; EF: ejection fraction; CPB: cardiopulmonary bypass; CRRT: continuous renal replacement therapy.
Table 4.
Significant independent predictive variables for 1-year mortality by multivariate logistic regression analysis
| Factors | OR (95% CI) | P value |
|---|---|---|
| Pre-operative factors | ||
| Age 65–79 (referent group 18–49 years) | 3.01 (1.52-5.98) | 0.002 |
| Age ≥80 (referent group 18–49 years) | 4.92 (2.32-10.46) | <0.001 |
| CHF | 2.13 (1.54-2.94) | <0.001 |
| Peripheral vascular disease | 2.04 (1.40-2.96) | <0.001 |
| ESKD on dialysis | 6.80 (3.68-12.55) | <0.001 |
| EF < 35% (referent group EF > 50%) | 1.83 (1.12-3.01) | 0.017 |
| Intra-operative factors | ||
| CPB time | 1.01 (1.00-1.01) | 0.001 |
| Post-operative complications | ||
| Neurologic events | 1.82 (1.13-2.93) | 0.014 |
| Pulmonary complications | 2.14 (1.53-3.00) | <0.001 |
| Cardiac arrest | 5.38 (3.36-8.62) | <0.001 |
| CVICU re-admission | 1.61 (1.04-2.48) | 0.034 |
| Acute kidney injury on CRRT | 6.27 (4.03-9.75) | <0.001 |
OR: odds ratio; CI: confidence interval; CHF: congestive heart failure; CRF: chronic renal failure; EF: ejection fraction; CPB: cardiopulmonary bypass; CRRT: continuous renal replacement therapy; CVICU: cardiovascular surgical intensive care unit.
Age ≥80 years was the strongest independent factor affecting long-term survival (hazard ratio [HR] 5.30, 95% CI 3.70-7.59, P < 0.001) (Table 5; Figure 3). While procedure type was not independently associated with short or mid-term mortality; those receiving combined procedures had worse long term survival.
Table 5.
Significant risk factors for long-term survival by Cox regression analysis
| Factors | HR (95% CI) | P value |
|---|---|---|
| Age 65–79 (referent group 18–49 years) | 2.81 (2.02-3.90) | <0.001 |
| Age ≥80 (referent group 18–49 years) | 5.30 (3.70-7.59) | <0.001 |
| Pre-operative co-morbidities | ||
| Type 1 Diabetes | 1.98 (1.17-3.34) | 0.011 |
| Type 2 Diabetes | 1.43 (1.25-1.64) | <0.001 |
| Smoking | 1.52 (1.25-1.86) | <0.001 |
| CHF | 1.72 (1.47-2.00) | <0.001 |
| PVD | 1.47 (1.24-1.74) | <0.001 |
| Stroke | 1.33 (1.14-1.56) | <0.001 |
| ESKD on dialysis | 3.61 (2.64-4.94) | <0.001 |
| Malignancy | 2.08 (1.66-2.61) | <0.001 |
| EF 35-50% (referent group EF > 50%) | 1.20 (1.00-1.43) | 0.045 |
| EF < 35% (referent group EF > 50%) | 1.54 (1.23-1.94) | <0.001 |
| Surgery type | ||
| AVR + CABG (referent group isolated CABG) | 1.61 (1.29-2.00) | <0.001 |
| MVR + CABG (referent group isolated CABG) | 1.31 (1.00-1.70) | 0.047 |
| 2 or more valves (referent group isolated CABG) | 1.48 (1.08-2.04) | 0.015 |
| Post-operative complications | ||
| Infection | 1.28 (1.07-1.53) | 0.007 |
| Neurologic events | 1.45 (1.12-1.88) | 0.004 |
| Pulmonary complications | 1.27 (1.08-1.50) | 0.004 |
| Acute kidney injury on CRRT | 2.10 (1.74-2.54) | <0.001 |
| Cardiac arrest | 2.72 (2.07-3.58) | <0.001 |
| CVICU re-admission | 1.32 (1.05-1.67) | 0.019 |
HR: hazard ratio; CI: confidence interval; PCI: percutaneous coronary intervention; CHF: congestive heart failure; PVD: peripheral vascular disease; CVA: cerebral vascular attack; CRF: chronic renal failure; EF: ejection fraction; CABG: coronary artery bypass grafting; AVR: aortic valve repair/replacement; MVR: mitral valve repair/replacement; CRRT: continuous renal replacement therapy; CVICU: cardiovascular surgical intensive care unit.
Figure 3.
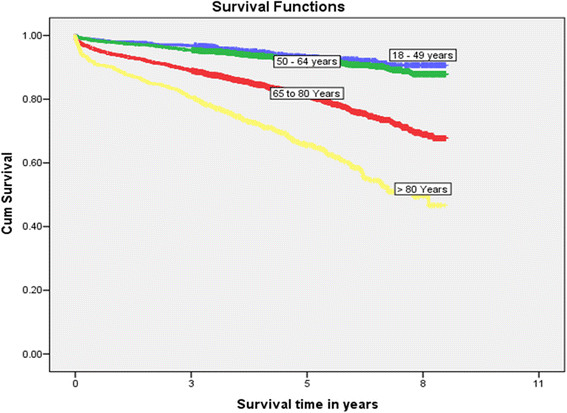
Kaplan-Meier survival curve for long-term survival.
Discussion
We performed a large population-based cohort study evaluating the incidence, clinical course, outcomes and health utilization of octogenarians undergoing elective cardiac surgery.
Key findings
Our study had several notable findings. Firstly, the proportion of octogenarians receiving cardiac surgery appears to be increasing. Secondly, octogenarians had significantly higher short and long-term mortality compared with younger patients after adjustment for relevant confounders. Thirdly, octogenarians were more likely to require combined procedures, resulting in longer exposure to cardiopulmonary bypass. Moreover, despite octogenarians having fewer selected comorbid diseases (i.e. ESKD) or undergoing re-operation, the rate of post-operative complications, including ICU readmission, was considerably higher when compared with younger age strata. Finally, octogenarians had markedly longer durations of stay in ICU and hospital and were far less likely to return home after surgery.
Strengths and limitations
There are important limitations to our study. Firstly, our cohort was assembled from a single center’s experience in Canada, was retrospective, and considered only patients referred for elective surgery. This may limit the generalizability of our study and we recognize the process of selection of octogenarians for elective surgery may be variable within and across institutions and jurisdictions. However, our study utilizes a large catchment from a relatively isolated geographical region of Canada, our cohort was relatively large with complete ascertainment of long-term vital status, and we utilized the high fidelity data prospectively captured with the APPROACH database. Secondly, while we were able to capture hospital discharge disposition and long-term vital status, we were unable to describe quality-adjusted survival or perform more formal cost analyses associated with elective cardiac surgery in octogenarians.
Interpretation and context with prior literature
Owing to the demographic change worldwide, the relative proportion of older persons is increasing. Data from Australia and New Zealand demonstrated a 5.6% annual increase of octogenarians admitted to ICU [9]. It is not surprising that elderly patients are more commonly referred to cardiac surgery. In fact, the average age for patients undergoing isolated CABG has increased from 55.8 (1990) to 68.6 year (2007) in Germany [10]. In large observational studies, Bhamidipati et al. and Alexander et al. reported 6.7-7.0% of all patients undergoing cardiac surgeries were aged ≥80 years. In our study cohort, the rate of octogenarians was modestly higher at 7.9%. Precise estimates of the numbers of octogenarians receiving cardiac surgery and their course are vital for resource planning, as our study has clearly shown these patients have longer more complicated post-operative stays that consumer greater resources that will likely impact cardiac surgical capacity and throughput. Although there was no previous data demonstrating the trend of octogenarians undergoing cardiac surgery, our study showed a small but steady annual increase in the number of octogenarians receiving surgery. As aging is a global phenomenon involved both developed and developing countries, we believe this trend of increasing numbers of octogenarians undergoing cardiac surgery would be evidenced by all high volume cardiac surgery centres in the near future.
As a consequence of older patient referral for cardiac surgery, cardiac pathology is often more considerable. Indeed, we found 36.3% of octogenarians received combined cardiac procedures (predominantly AVR and CABG), which is among the highest rates compared to previous studies [10]-[12] and associated with longer CPB and aortic cross clamp time. It is not surprising that octogenarians with more complex procedures have higher risk for major post-operative complications and consequently greater health service utilization (i.e. longer hospital stay, higher ICU re-admission and greater utilization of organ support) and overall costs. Cox regression analysis also suggested combined surgery was associated with worse long term survival. This will present a challenge for cardiac surgical programs to maintain capacity and accommodate the growing demand of this demographic coupled with their higher resource utilization. It is likely that improved and transparent mechanisms for risk assessment and prioritization are needed.
One concern with increasing numbers of octogenarians undergoing more combined cardiac surgery is the high operational mortality. Operating on this specific demographic is not only a challenge to cardiac surgeons but also a challenge to cardiologists, anesthesiologists, CVICU intensivists, and the whole medical system [11]. Previous studies have shown that the in-hospital mortality in octogenarians undergoing isolated CABG, AVR and MVR were 6.8%-14.3% [5],[12]-[14], 4.5%-12.6% [6],[15]-[17], and 2.7%-18.5% [7],[18], respectively. In a multi-center retrospective study gathering data from 22 high volume cardiac centers in the United States, the reported in-hospital mortality rates for octogenarians after cardiac surgery were 8.1% for isolated CABG, 10.1% for combined CABG and AVR, and 19.6% for combined CABG and MVR [19]. In our study, despite more combined cardiac procedures and longer CPB/cross clamp time, the crude 30-day mortality was only 3.7%, and the 1-year and 5-year mortality were 10.8% and 29.0% among octogenarians, respectively. Although still significantly higher than patients of younger age groups, the short-term and long-term survival in octogenarians are better than previous studies. Indeed, the 29.0% 5-year mortality in octogenarians (mean age 83.1 years) undergoing cardiac surgery is lower than the 5-year estimated mortality of an average Canadian at age of 83 years (40.5% in male and 30.4% in female) [20]. These observations confirm that informed selection of older patients for cardiac surgery can translate into acceptable post-operative survival.
Post-operative complications are a source of major morbidity and a driver of health resource use. Across the entire spectrum of complications, the rates are markedly higher among octogenarians [21]. While some occur commonly in the post-operative period, many translate into need for increased intensity of support, downstream morbidity and disability. Indeed, post-operative complications contribute to higher ICU readmission rates and longer durations of ICU and hospital stay. For those octogenarians requiring ICU readmission, in hospital death was 35% and only 41% were discharged home. In addition, post-operative complications were independently associated with 30-day and 1-year mortality.
In our opinion, thoughtful patient selection is necessary to optimize post-operative outcomes, in particular in older patients. The vulnerability to less favorable outcomes after cardiac surgery may not be age-specific, but rather reflect “physiologic age”. Pre-operative risk assessment may need to consider the emerging concept of frailty as a modifying factor for post-operative course and outcome. Observational data have shown in patients undergoing cardiac surgery that frailty is an independent risk factor for post-operative complications, mortality and institutionalization, after adjusting for age [22]. In our study, we found that in addition to age ≥80 years, pre-operative low EF and pre-operative dialysis dependence were also significant independent risk factors predictive of 30-day mortality. These may be important additional variables to consider when constructing novel clinical risk assessment tools unique to older frail patients referred for surgery, as well as informed decision-making about undergoing surgery and appropriate resource planning.
Conclusions
The number of octogenarians referred for cardiac surgery is increasing. Age ≥80 years was associated with higher risk of post-operative complications and short and long-term mortality. Octogenarians also have greater post-operative health service utilization. While clinical outcomes may be acceptable with careful patient selection, these data should be utilized to better inform discussions about prognosis, recovery and ultimate resource planning.
Authors’ contributions
WW: Study design, data collecting and manuscript writing. SMB: Study design, statistical analysis and interpretation, and manuscript writing. CMN: Statistical analysis and interpretation. RZ: Data collecting. MZ: Study design and data collecting. RM: Study design and manuscript writing. All authors read and approved the final manuscript.
Acknowledgements
This study was unfunded.
Dr. Bagshaw holds a Canada Research Chair in Critical Care Nephrology and is a Clinical Investigator supported by Alberta Innovates – Health Solutions (AI-HS).
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Contributor Information
Wei Wang, Email: wei.wang@ualberta.ca.
Sean M Bagshaw, Email: bagshaw@ualberta.ca.
Colleen M Norris, Email: cnorris@ualberta.ca.
Rami Zibdawi, Email: zibdawi@ualberta.ca.
Mohamad Zibdawi, Email: Mohamad.Zibdawi@albertahealthservices.ca.
Roderick MacArthur, Email: Roderick.MacArthur@albertahealthservices.ca.
References
- 1.Statistics Canada: Annual demographic estimates: Canada, provinces and territories 2012. Available at: ., [www.statcan.gc.ca/pub/91-215-x/91-215-x2012000-eng.pdf]
- 2.Bettelli G. Preoperative evaluation in geriatric surgery: comorbidity, functional status and pharmacological history. Minerva Anestesiol. 2011;77:637–646. [PubMed] [Google Scholar]
- 3.Neragi-Miandoab S, Wayne M, Cioroiu M, Zank LM, Mills C. Preoperative evaluation and a risk assessment in patients undergoing abdominal surgery. Surg Today. 2010;40:108–113. doi: 10.1007/s00595-009-3996-7. [DOI] [PubMed] [Google Scholar]
- 4.Krane M, Voss B, Hiebinger A, Deutsch MA, Wottke M, Hapfelmeier A, Badiu CC, Bauernschmitt R, Lange R. Twenty years of cardiac surgery in patients aged 80 years and older: risks and benefits. Ann Thorac Surg. 2011;91:506–513. doi: 10.1016/j.athoracsur.2010.10.041. [DOI] [PubMed] [Google Scholar]
- 5.Scott BH, Seifert FC, Grimson R, Glass PS. Octogenarians undergoing coronary artery bypass graft surgery: resource utilization, postoperative mortality, and morbidity. J Cardiothorac Vasc Anesth. 2005;19:583–588. doi: 10.1053/j.jvca.2005.03.030. [DOI] [PubMed] [Google Scholar]
- 6.Leontyev S, Walther T, Borger MA, Lehmann S, Funkat AK, Rastan A, Kempfert J, Falk V, Mohr FW. Aortic valve replacement in octogenarians: utility of risk stratification with EuroSCORE. Ann Thorac Surg. 2009;87:1440–1445. doi: 10.1016/j.athoracsur.2009.01.057. [DOI] [PubMed] [Google Scholar]
- 7.Nloga J, Hénaine R, Vergnat M, Wautot F, Desebbe O, Robin J, Ninet J, Obadia JF. Mitral valve surgery in octogenarians: should we fight for repair? A survival and quality-of-life assessment. Eur J Cardiothorac Surg. 2011;39:875–880. doi: 10.1016/j.ejcts.2010.11.019. [DOI] [PubMed] [Google Scholar]
- 8.Mark DB, Nelson CL, Califf RM, Harrell FE, Jr, Lee KL, Jones RH, Fortin DF, Stack RS, Glower DD, Smith LR. Continuing evolution of therapy for coronary artery disease. Initial results from the era of coronary angioplasty. Circulation. 1994;89:2015–2025. doi: 10.1161/01.CIR.89.5.2015. [DOI] [PubMed] [Google Scholar]
- 9.Bagshaw SM, Webb SA, Delaney A, George C, Pilcher D, Hart GK, Bellomo R. Very old patients admitted to intensive care in Australia and New Zealand: a multi-centre cohort analysis. Crit Care. 2009;13:R45. doi: 10.1186/cc7768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Friedrich I, Simm A, Kotting J, Tholen F, Fischer B, Silber RE. Cardiac surgery in the elderly patient. Dtsch Arztebl Int. 2009;106:416–422. doi: 10.3238/arztebl.2009.0416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gelsomino S, Lorusso R, Livi U, Masullo G, Lucà F, Maessen J, Gensini GF. Cost and cost-effectiveness of cardiac surgery in elderly patients. J Thorac Cardiovasc Surg. 2011;142:1062–1073. doi: 10.1016/j.jtcvs.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 12.Pivatto Júnior F, Kalil RA, Costa AR, Pereira EM, Santos EZ, Valle FH, Bender LP, Trombka M, Modkovski TB, Nesralla IA. Morbimortality in octogenarian patients submitted to coronary artery bypass graft surgery. Arq Bras Cardiol. 2010;95:41–46. doi: 10.1590/S0066-782X2010005000071. [DOI] [PubMed] [Google Scholar]
- 13.Sen B, Niemann B, Roth P, Aser R, Schonburg M, Boning A. Short- and long-term outcomes in octogenarians after coronary artery bypass surgery. Eur J Cardiothorac Surg. 2012;42:e102–e107. doi: 10.1093/ejcts/ezs410. [DOI] [PubMed] [Google Scholar]
- 14.Maganti M, Rao V, Brister S, Ivanov J. Decreasing mortality for coronary artery bypass surgery in octogenarians. Can J Cardiol. 2009;25:e32–e35. doi: 10.1016/S0828-282X(09)70481-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Di Eusanio M, Fortuna D, Cristell D, Pugliese P, Nicolini F, Pacini D, Gabbieri D, Lamarra M. Contemporary outcomes of conventional aortic valve replacement in 638 octogenarians: insights from an Italian Regional Cardiac Surgery Registry (RERIC) Eur J Cardiothorac Surg. 2012;41:1247–1252. doi: 10.1093/ejcts/ezr204. [DOI] [PubMed] [Google Scholar]
- 16.Langanay T, Flécher E, Fouquet O, Ruggieri VG, De La Tour B, Félix C, Lelong B, Verhoye JP, Corbineau H, Leguerrier A. Aortic valve replacement in the elderly: the real life. Ann Thorac Surg. 2012;93:70–77. doi: 10.1016/j.athoracsur.2011.07.033. [DOI] [PubMed] [Google Scholar]
- 17.Filsoufi F, Rahmanian PB, Castillo JG, Chikwe J, Silvay G, Adams DH. Excellent early and late outcomes of aortic valve replacement in people aged 80 and older. J Am Geriatr Soc. 2008;56:255–261. doi: 10.1111/j.1532-5415.2007.01535.x. [DOI] [PubMed] [Google Scholar]
- 18.Nagendran J, Norris C, Maitland A, Koshal A, Ross DB. Is mitral valve surgery safe in octogenarians? Eur J Cardiothorac Surg. 2005;28:83–87. doi: 10.1016/j.ejcts.2004.12.067. [DOI] [PubMed] [Google Scholar]
- 19.Alexander KP, Anstrom KJ, Muhlbaier LH, Grosswald RD, Smith PK, Jones RH, Peterson ED. Outcomes of cardiac surgery in patients > or =80 years: results from the National Cardiovascular Network. J Am Coll Cardiol. 2000;35:731–738. doi: 10.1016/S0735-1097(99)00606-3. [DOI] [PubMed] [Google Scholar]
- 20.Statistics Canada: Life Tables, Canada, Provinces and Territories 2005 to 2007. Available at: ., [http://www.statcan.gc.ca/pub/84-537-x/2013001/tbl-eng.htm]
- 21.Barnett SD, Halpin LS, Speir AM, Albus RA, Akl BF, Massimiano PS, Burton NA, Collazo LR, Lefrak EA. Postoperative complications among octogenarians after cardiovascular surgery. Ann Thorac Surg. 2003;76:726–731. doi: 10.1016/S0003-4975(03)00676-3. [DOI] [PubMed] [Google Scholar]
- 22.Lee DH, Buth KJ, Martin BJ, Yip AM, Hirsch GM. Frail patients are at increased risk for mortality and prolonged institutional care after cardiac surgery. Circulation. 2010;121:973–978. doi: 10.1161/CIRCULATIONAHA.108.841437. [DOI] [PubMed] [Google Scholar]


