Abstract
This study aims to assess the validity of maternal recall for several perinatal variables 8–10 years after pregnancy in a twin sample. Retrospective information was collected 8–10 years after the delivery event in a cohort of mothers from the University of Southern California Twin Study (N = 611) and compared with medical records for validity analysis. Recall of most variables showed substantial to perfect agreement (κ = 0.60–1.00), with notable exceptions for specific medical problems during pregnancy (κ ≤ 0.40) and substance use when mothers provided continuous data (e.g., number of cigarettes per day; r ≤ 0.24). With the exception of delivery method, neonatal intensive care unit admission, birth weight, neonatal information, and post-delivery complications were also recalled with low accuracy. For mothers of twins, maternal recall is generally a valid measure for perinatal variables 10 years after pregnancy. However, caution should be taken regarding variables such as substance use, medical problems, birth length, and post-delivery complications.
Keywords: twin, maternal recall, recall validity, recall reliability, perinatal pregnancy, birth complication
Research has increasingly shown that prenatal and perinatal events have an important effect on later and lifelong health outcomes of offspring. Complications during pregnancy, delivery, and early childhood have all been associated with neurological, developmental, and neuropsychiatric disorders (Cannon et al., 2002; Liu et al., 2009; Rice et al., 2007), as well as chronic diseases such as obesity, metabolic syndromes, cardiovascular disease, cancer, and neurocognitive disorders (Rice et al., 2007; Sou et al., 2006; Troude et al., 2008). Early life factors are also associated with the development of chronic diseases and increased rates of cognitive, behavioral, and emotional problems (Buka et al., 2004; Liu, 2011; Rice et al., 2007; Tomeo et al., 1999). For instance, recent studies have suggested an association between birth weight and cardiovascular diseases in adulthood (Frontini et al., 2004; Mzayek et al., 2007) that is not confounded by genetic and environmental factors (Bergvall et al., 2007). Furthermore, maternal health-related behaviors, such as substance use during pregnancy, are known to have important implications on offspring health and development.
Researchers are increasingly interested in obtaining information from the perinatal period and often do so through maternal recall. Although medical records are often considered to be the most accurate sources of information, using medical records and charts can be impractical due to time and cost restraints, and in some instances health registries and records may not even exist (Troude et al., 2008). Furthermore, recording errors can occur, medical criteria may vary from hospital to hospital, and abstraction of information may be difficult due to the Health Insurance Portability and Accountability Act (HIPAA) policies as well as inconsistencies in record organization (Elliott et al., 2010; Hewson & Bennett, 1987; Joffe & Grisso, 1985). As a result, pregnancy and neonatal information is commonly obtained through cost-effective, self-report questionnaires or interviews. However, the validity and reliability of maternal report are still debated, and despite the number of studies suggesting maternal recall is sufficiently reliable for some pregnancy and early life characteristics (D’Souza-Vazirani et al., 2005; Launer et al., 1992; Li et al., 2005; McCormick & Brooks-Gunn, 1999; Olson et al., 1997; Quigley et al., 2007; Reich et al., 2003; Tomeo et al., 1999), evidence still suggests poor to moderate recall for information including lifestyle during pregnancy (Jaspers et al., 2010), complications and disease diagnosis (Coolman et al., 2010; Sou et al., 2006), and procedures during delivery (Quigley et al., 2007). These inconsistencies are in part attributed to the current literature’s varied sample populations, methodology, length of recall, and measures of interest. Importantly, most studies have focused on the recall of one or a few related variables, such as birth weight (Catov et al., 2006; Lumey et al., 1994), and specific procedures or complications during delivery (Coolman et al., 2010; Quigley et al., 2007; Sou et al., 2006). Thus, it is unclear whether inconsistencies in findings actually reflect differences in the accuracy of maternal report for different variables or whether they are due to methodological variations (i.e., sample characteristics, questionnaire wording, measurement). Few studies have looked comprehensively at recall validity for perinatal, prenatal, and post-natal data, and those which have often use small samples (Githens et al., 1993; Rice et al., 2007; Tomeo et al., 1999). Even fewer studies have addressed maternal recall of pregnancy, delivery, or postnatal complications, and those that have often do so very broadly (Tomeo et al., 1999; Yawn et al., 1998). On the other hand, studies which have studied the recall validity for specific complications often leave out other important perinatal factors (Buka et al., 2004; Coolman et al., 2010; Sou et al., 2006). Finally, and importantly, validity has not been assessed in a large sample of mothers of twins who are asked to recall information for both twins simultaneously. To our knowledge, only Reich et al. (2003) have examined maternal recall with a focus on mothers of twins. In their study, mothers were re-interviewed 6–18 months after the initial interview, but comparison to medical records was not available. Thus, while the use of twins allowed for maternal recall to be assessed for reliability, validity of this information was not established.
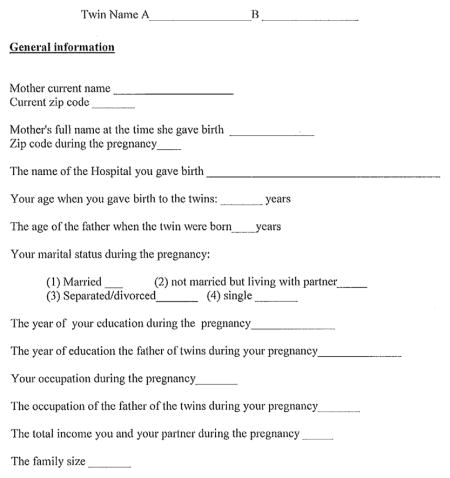
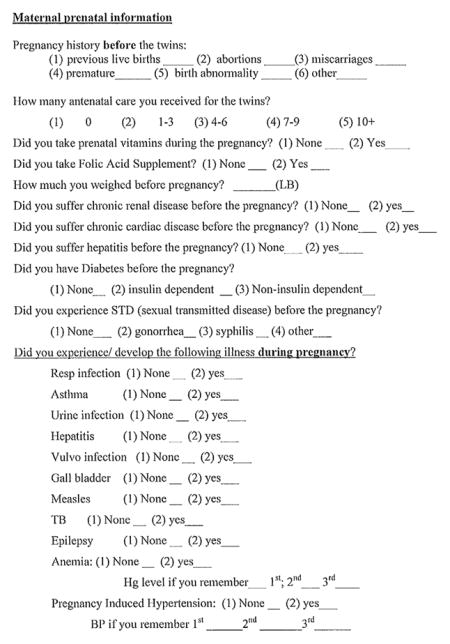
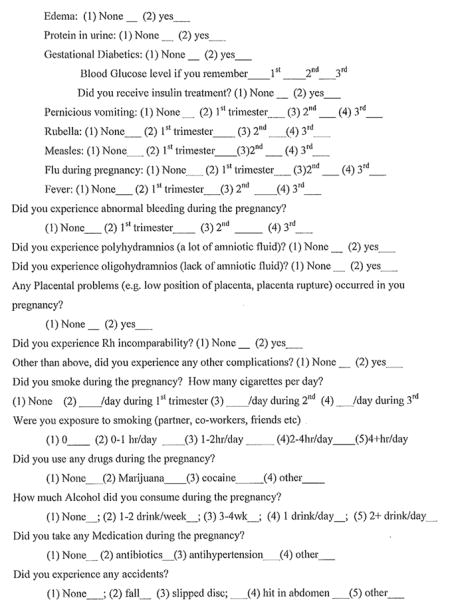
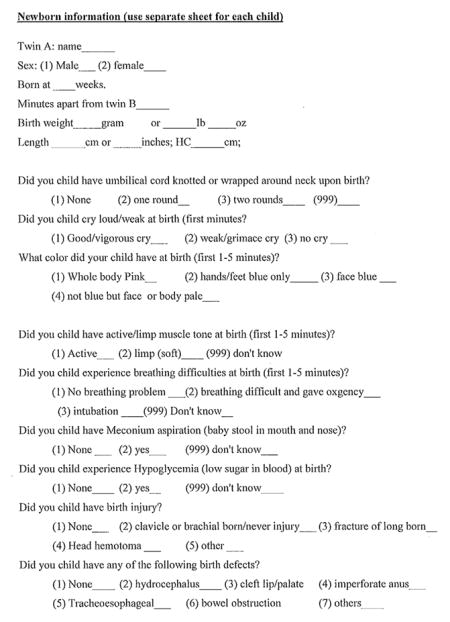
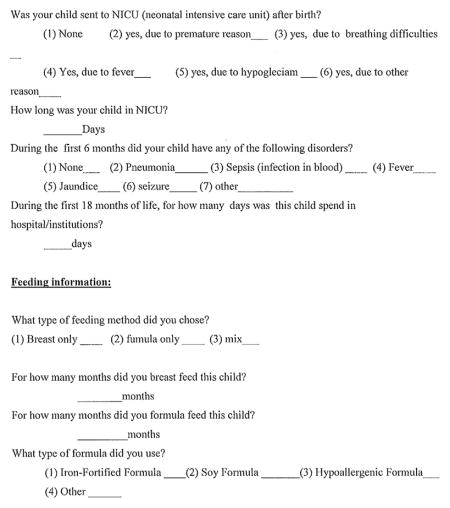
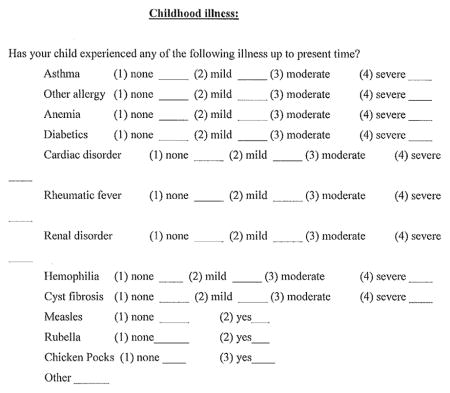
This study aims to help bridge the gaps in the existing literature by examining the validity of maternal recall in a large twin cohort. Mothers of twins were asked to complete a questionnaire that was developed by the first author and asked mothers to report on pregnancy and birth-related events including maternal history, medical problems during pregnancy, substance and vitamin use, delivery procedures, neonatal information for both twins, and post-delivery complications for both twins. The validity of the data was obtained by comparing questionnaire answers to medical records.
Methods
Study Sample
The subjects were participants in the University of Southern California (USC) Risk Factors for Antisocial Behavior (RFAB) twin study, which is an ongoing prospective longitudinal study of the interplay of genetic, environmental, social, and biological factors on the development of antisocial behavior from childhood to early adulthood. The twins and their parents were recruited from the larger Los Angeles community and the sample is representative of the ethnic and socio-economic diversity of the greater Los Angeles area. On the first assessment (Wave 1), the twins were 9–10 years old (mean age = 9.59, SD = 0.58). On the second assessment (Wave 2), the twins were 11–13 years old (mean age = 11.79, SD = 0.92). On the third assessment (Wave 3), the twins were 14–15 years old (mean age = 14.82, SD = 0.83), and during Wave 4 the twins were 16–18 years old (mean age = 17.22, SD = 1.23). The total sample contains 1,564 subjects (781 twin pairs), including 169 monozygotic (MZ) male, 171 MZ female, 121 dizygotic (DZ) male, 120 DZ female, and 200 DZ opposite-sex twin pairs. Complete details on the procedures and measures can be found elsewhere (Baker et al., 2006, 2007, 2013).
Caregiver participation was primarily by the biological mothers (>90%). Information on prenatal recall was collected from 611 of the twins’ mothers. The mean age of pregnancy among the women in this sample was 29.5 years.
Study Measures
Retrospective birth complications recall questionnaire
Birth complications recall was measured with a retrospective questionnaire developed by the first author who has a master degree in Maternal-Child Health Nursing (see the Appendix). It was developed from the birth complications-medical records instrument (see below), which asked mothers about birth complications on a more general level. The form includes questions regarding three main areas: prenatal (during pregnancy), perinatal (during birth), and post-natal (newborn) complications. Mothers were asked to fill in a computerized version of the birth complications questionnaire at their visit to the USC laboratory.
Birth complications-medical records instrument
We developed the Birth Complications-Medical Records Instrument, which incorporated more detailed birth complications information. This was derived from two well-established instruments: the Lewis–Murray Obstetric Complication Scale (Lewis & Murray, 1987; Lewis et al., 1989) and the McNeil–Sjöström Scale for Obstetric Complications (McNeil & Sjöström, 1995). In this study, we asked for the mother’s permission to obtain the children’s medical records, which were stored at the birth hospitals. We then contacted each hospital and the records were mailed to the laboratory.
Statistical Analyses
Items were grouped into those events occurring prior to the pregnancy of interest (maternal history), during the pregnancy (medical problems during pregnancy; substance use during pregnancy; vitamins during pregnancy), during delivery (medical procedures), information on the infant (neonatal information), and events occurring after delivery (post-delivery complications); see Table 1.
TABLE 1.
Agreement Between Medical Records and Maternal Reports
| Medical records (%) | Frequency | Prenatal recall (%) | Frequency | Mother (N = 611)
|
Twin A (N = 287)
|
Twin B (N = 287)
|
|
|---|---|---|---|---|---|---|---|
| κ(95% CI)/ Pearson correlations | κ (95% CI)/ Pearson correlations | κ (95% CI)/ Pearson correlations | |||||
| Maternal history | |||||||
| Previous live births | |||||||
| No | 25.00 | 48 | 25.00 | 48 | |||
| Yes | 75.00 | 144 | 75.00 | 144 | 1.00 (1.00–1.00) | ||
| Medical problems during pregnancy | |||||||
| Respiratory infection | 16.7 | 1 | 0 | 0 | |||
| Urine infection | 66.7 | 4 | 66.7 | 4 | |||
| Asthma | 16.7 | 1 | 33.3 | 2 | 0.67 (0.24–1.00) | ||
| Bleeding during pregnancy | |||||||
| No | 73.20 | 30 | 80.50 | 33 | |||
| Yes | 26.80 | 11 | 19.50 | 8 | 0.39 (0.06–0.71) | ||
| Edema during the pregnancy (any swelling in face, fingers, legs or feet) | |||||||
| None | 48.19 | 40 | 44.58 | 37 | |||
| Yes | 51.81 | 43 | 55.42 | 46 | 0.30 (0.09–0.50) | ||
| Proteinuria during the pregnancy | |||||||
| None | 24.68 | 19 | 85.71 | 66 | |||
| Yes | 75.32 | 58 | 14.29 | 11 | 0.10 (0.03–0.17) | ||
| Pre-elampsia vs pre-elampsia + hypertension | |||||||
| No | 65.71 | 46 | 74.29 | 52 | |||
| Yes | 34.29 | 24 | 25.71 | 18 | 0.60 (0.39–0.80) | ||
| Medication taken during the pregnancy | |||||||
| Antibiotics | 71.43 | 5 | 71.43 | 5 | |||
| Anti-hypertension | 28.57 | 2 | 28.57 | 2 | 1.00 (−1.00–1.00) | ||
| Nausea and vomiting during pregnancy | |||||||
| No | 43.10 | 28 | 63.10 | 41 | |||
| Yes | 56.90 | 37 | 36.90 | 24 | 0.38 (0.17–0.58) | ||
| Weight gain during pregnancy | 0.30* | ||||||
| Substance use during pregnancy (continuous) | |||||||
| Smoking (number of cigarettes per day) | |||||||
| During the pregnancy | 0.25 | ||||||
| During the first trimester | 0.24 | ||||||
| During the second trimester | 0.001 | ||||||
| During the third trimester | 0.01 | ||||||
| Alcohol (number of alcoholic drinks per month) | |||||||
| During the pregnancy | −0.09 | ||||||
| During the first trimester | −0.07 | ||||||
| During the second trimester | −0.06 | ||||||
| During the third trimester | −0.07 | ||||||
| Substance use during pregnancy (dichotomized) | |||||||
| Smoking during pregnancy | |||||||
| No | 70.27 | 26 | 75.68 | 28 | |||
| Yes | 29.73 | 11 | 24.32 | 9 | 0.73 (0.48–0.98) | ||
| Smoking during the first trimester | |||||||
| No | 80.00 | 40 | 86.00 | 43 | |||
| Yes | 20.00 | 10 | 14.00 | 7 | 0.79 (0.56–1.00) | ||
| Smoking during the second trimester | |||||||
| No | 83.33 | 30 | 83.33 | 30 | |||
| Yes | 16.67 | 6 | 16.67 | 6 | 0.80 (0.53–1.00) | ||
| Smoking during the third trimester | |||||||
| No | 80.43 | 37 | 82.61 | 38 | |||
| Yes | 19.57 | 9 | 17.39 | 8 | 0.78 (0.55–1.00) | ||
| Alcohol during pregnancy | |||||||
| No | 72.97 | 27 | 94.59 | 35 | |||
| Yes | 27.03 | 10 | 5.41 | 2 | 0.08 (−0.18–0.35) | ||
| Alcohol in the first trimester | |||||||
| No | 85.71 | 42 | 93.88 | 43 | |||
| Yes | 14.29 | 7 | 6.12 | 6 | 0.13 (−0.22–0.47) | ||
| Alcohol in the second trimester | |||||||
| No | 86.49 | 32 | 97.30 | 36 | |||
| Yes | 13.51 | 5 | 2.70 | 1 | −0.05 (−0.13–0.03) | ||
| Alcohol in the third trimester | |||||||
| No | 82.98 | 39 | 95.74 | 45 | |||
| Yes | 17.02 | 8 | 4.26 | 2 | −0.073 (−0.16–0.01) | ||
| Vitamins during pregnancy | |||||||
| Prenatal vitamins | |||||||
| No | 0.82 | 1 | 12.30 | 15 | |||
| Yes | 99.18 | 121 | 87.70 | 107 | 0.11 (−0.09–0.31) | ||
| Iron supplement during the pregnancy | |||||||
| No | 1.56 | 1 | 37.50 | 24 | |||
| Yes | 98.44 | 63 | 62.50 | 40 | 0.05 (0.05–0.15) | ||
| Folic acid during the pregnancy | |||||||
| No | 16.67 | 1 | 66.67 | 4 | |||
| Yes | 83.33 | 5 | 33.33 | 2 | 0.18 (−0.19–0.56) | ||
| Medical procedures/method of delivery | |||||||
| Method of delivery (Twin A) | |||||||
| Vaginal | 38.20 | 100 | 37.80 | 99 | |||
| C-section | 61.80 | 162 | 62.20 | 163 | 0.94 (0.90–0.98) | ||
| Method of delivery (Twin B) | |||||||
| Vaginal | 32.90 | 85 | 34.50 | 89 | |||
| C-section | 67.10 | 173 | 65.50 | 169 | 0.97 (0.93–1.00) | ||
| Neonatal information | |||||||
| Birth weight | 0.84* | 0.82* | |||||
| Birth length | 0.17 | 0.21* | |||||
| Meconium (Twin A) | |||||||
| No | 91.40 | 170 | 97.80 | 182 | |||
| Yes | 8.6 | 16 | 2.20 | 4 | 0.17 (−0.06–0.4) | ||
| Meconium (Twin B) | |||||||
| No | 91.80 | 169 | 98.90 | 182 | |||
| Yes | 8.2 | 15 | 1.10 | 2 | −0.02 (−0.04—0.00) | ||
| Muscle tone (Twin A) | |||||||
| Limp and some flexion | 7.50 | 12 | 9.40 | 15 | |||
| Active motion | 92.50 | 147 | 90.60 | 144 | 0.70 (0.51–0.89) | ||
| Muscle tone (Twin B) | |||||||
| Limp and some flexion | 11.9 | 19 | 13.1 | 21 | |||
| Active motion | 88.1 | 141 | 86.9 | 139 | 0.26 (0.05–0.46) | ||
| Apgar score — Color (Twin A) | |||||||
| Pale/blue/body pink extra blue | 95.55 | 156 | 19.39 | 32 | |||
| All pink | 5.45 | 9 | 80.61 | 133 | −0.04 (−0.08–0.01) | ||
| Apgar score — Color (Twin B) | |||||||
| Pale/blue/ body pink extra blue | 94.71 | 161 | 22.35 | 38 | |||
| All pink | 5.29 | 9 | 77.65 | 132 | −0.03 (−0.08–0.02) | ||
| Respiratory distress (Twin A) | |||||||
| No | 67.80 | 139 | 83.90 | 172 | |||
| Yes | 32.20 | 66 | 16.10 | 33 | 0.32 (0.18–0.45) | ||
| Respiratory distress (Twin B) | |||||||
| No | 75.50 | 154 | 81.40 | 166 | |||
| Yes | 24.50 | 50 | 18.60 | 38 | 0.34 (0.19–0.49) | ||
| Post-delivery complications | |||||||
| Jaundice (Twin A) | |||||||
| No | 60.60 | 137 | 79.60 | 180 | |||
| Yes | 39.40 | 89 | 20.40 | 46 | 0.18 (0.06–0.30) | ||
| Jaundice (Twin B) | |||||||
| No | 58.3 | 127 | 78.0 | 170 | |||
| Yes | 41.7 | 91 | 22.0 | 48 | 0.28 (0.16–0.40) | ||
| NICU (Twin A) | |||||||
| No | 64.50 | 138 | 61.70 | 132 | |||
| Yes | 35.50 | 76 | 38.30 | 82 | 0.80 (0.72–0.88) | ||
| NICU (Twin B) | |||||||
| No | 67.90 | 146 | 59.10 | 127 | |||
| Yes | 32.10 | 69 | 40.90 | 88 | 0.65 (0.55–0.76) | ||
Note:
p < .05.
κ is not calculated for this dataset because observed concordance is smaller than mean-chance concordance.
NICU = neonatal intensive care unit.
In the prenatal recall record, seven different illnesses were combined into one variable (0 = none, 1 = respiratory infection, 2 = urinary tract infection, 3 = gall bladder inflammation, 4 = measles, 5 = TB, 6 = epilepsy, 7 = asthma). Due to limited data for some diseases, we only kept respiratory infection, urinary tract infection, and asthma when calculating the κ statistic. Two variables in prenatal record, pre-eclampsia and hypertension, were combined and paired with pre-eclampsia in medical records.
Measures of agreement for both categorical and continuous measures are presented. For the continuous variables (e.g., birth weight and birth length), we computed Pearson’s correlation coefficient along with p values. The κ statistic was calculated for categorical variables. The κ statistic measures the extent of exact agreement, adjusting for chance agreement. All analyses were performed using the statistical software SAS (SAS, 2005).
Results
Recall validity for several perinatal factors obtained from the USC Twin Study is presented in Table 1.
Prenatal
Perfect agreement was obtained for maternal history (previous live births; κ 1.00). Poor agreement was found among medical problems during pregnancy, such as bleeding (0.39), edema (0.30), proteinuria (0.10), and nausea and vomiting (0.38). Substance use during pregnancy, specifically alcohol use and vitamin use, was very poorly recalled. However, smoking during pregnancy showed moderate agreement. Information regarding substance use was collected as continuous data (e.g., number of cigarettes per day), and validity analysis was repeated after dichotomizing these data, where any answer >0 would, for example, represent having ever smoked during pregnancy. This produced better recall accuracy for smoking throughout pregnancy (κ 0.73, 95% CI 0.48–0.98) as well as during the first, second, and third trimesters (0.79, 0.80, 0.78, respectively), but validity recall of alcohol use remained poor (0.08, 95% CI 0.18–0.35).
Perinatal and Postnatal
For both twins (A, B), near-perfect (κ ≥ 0.80) agreement was obtained for medical procedures/method of delivery (0.94, 0.97) and birth weight (κ 0.84, 0.82), but not birth length (0.17, 0.21). Recall of specific delivery procedures such as the use of forceps and oxytocin to induce labor was excluded from validity analyses due to low frequency. Recall accuracy was generally low for neonatal information and post-delivery complications. Mothers generally recalled neonatal information for both twins with similar accuracy, and without consistently more accurate recall of information for twin A than B or vice versa. A notably pronounced difference in recall accuracy was, however, found in muscle tone: agreement between recall and medical records was substantial for Twin A (κ 0.70, 95% CI 0.51–0.89) but poor for Twin B (κ 0.26, 95% CI 0.05–0.46).
Discussion
This study examined the validity of maternal recall for peri-natal variables in a large twin sample 8–10 years after birth. Overall, the data obtained from questionnaires completed by mothers around 9 years after pregnancy showed substantial agreement (κ ≥ 0.60) with medical records for most pre-, peri-, and postnatal variables. Exceptions included poor validity for medical problems during pregnancy (e.g., bleeding, edema, proteinuria), substance and vitamin use, and some neonatal information (e.g., birth length, meconium, respiratory distress, and jaundice).
To our knowledge, these findings are the first that use medical records to demonstrate that that maternal recall is a valid method for obtaining neonatal information in twins. Although Reich et al. (2003) looked at reliability and stability of maternal report using a twin sample, this study’s design compared sets of interview responses and did not assess validity through comparison with medical records. The findings for a number of pregnancy and neonatal factors are further discussed below.
Prenatal
The recall validity of medical problems such as bleeding, edema, and nausea and vomiting during pregnancy was mostly poor to moderate. Low rates of recall for ante partum vaginal bleeding and edema have been reported previously (Bryant et al., 1989; Buka et al., 2000; Olson et al., 1997; Sou et al., 2006). Low rates of maternal recall for these particular problems may reflect the fact that these complications may not be severe enough to warrant major actions (i.e., diet change, medications) and are thus less memorable to mothers (Sou et al., 2006). Indeed, the few women whose complications did require them to take medications recalled this information with near-perfect accuracy. The moderate recall of hypertension versus pre-eclampsia in our sample (κ 0.60, 95% CI 0.39–0.80) is in line with previous reports, which have generally promoted more accurate patient–doctor communication in order to address the reduced maternal recall (Coolman et al., 2010; Rice et al., 2007). Previous work has also suggested recall of hypertension to be particularly time-sensitive (Olson et al., 1997).
Our initial findings suggest very poor recall validity and reliability for both smoking and alcohol use. While our findings are in line with existing evidence that maternal recall for alcohol use is poor (Delgado-Rodriguez et al., 1995; Jaspers et al., 2010; Rice et al., 2007), these and other findings have demonstrated accurate recall for smoking (Tomeo et al., 1999; Yawn et al., 1998), which was not observed in our initial analysis. This discrepancy in recall validity for smoking likely reflects the fact that we asked mothers to provide continuous data (e.g., cigarettes per day for overall pregnancy and during each trimester). In contrast to the present study, other studies have generally used dichotomized categories (e.g., ‘ever’/‘never’) when comparing maternal recall data to medical records. Repeating our validity analysis with dichotomous data produced results more in line with the existing evidence with substantial to near perfect agreement for smoking but poor recall of alcohol use.
In addition to poor recall for substance use, we also found very poor recall (κ < 0.20) for the use of prenatal vitamins, iron supplements, and folic acid during pregnancy. To our knowledge, this is the first study that examines maternal recall for vitamin use, but very poor agreement between records and self-report has been reported for prenatal vitamin use even during pregnancy (κ 0.11; Hessol et al., 2004). Due to low frequency of use for the individual vitamins mothers were asked to report on, answers for prenatal vitamins, iron supplements, and folic acid were all grouped into one category.
Perinatal and Postnatal
Our findings add to the existing evidence that birth weight and the method of delivery are among the most accurately recalled perinatal variables (Olson et al., 1997; Sou et al., 2006; Tomeo et al., 1999; Yawn et al., 1998). An accurate and consistent recall of birth weight may reflect high social value and repetition of information to others (Yawn et al., 1998). The lack of such social value could explain the poor recall for birth length in both our samples. We are aware of only one other study that reports recall of birth length, which showed accurate recall but only 6–10 weeks after delivery (Troude et al., 2008). Birth length has been demonstrated to be an independent predictor for various health outcomes (Maehle et al., 2010; Melve et al., 2000; Sun et al., 2009), and may actually serve as a better indicator of birth size than birth weight (Silva et al., 2008). Thus, while there may be growing interest in obtaining this information, our finding highlights the need for researchers to use caution when relying on maternal reports of birth length.
Recall accuracy was generally poor for neonatal information and post-delivery complications regarding both Twin A and Twin B. Meconium was especially unreliably recalled. Although meconium-stained aminiotic fluid has been associated with higher rates of stillbirths, low Apgar scores, and hypoxic ischemic encephalopathy (Carbonne et al., 1997; Starks, 1980; Steer et al., 1989), outcomes are generally good (Balchin et al., 2011) and may explain the underreporting of this complication by mothers. NICU admission tended to be over reported by mothers of the twin samples, while maternal recall of post-delivery complication factors for both twins was the most accurate. This result is similar to previous findings from the United States (Githens et al., 1993).
Limitations and Implications
Our findings are not without limitations, particularly our use of medical records as the ‘gold standard’. These records are not always valid, especially regarding behavioral or lifestyle factors (Hessol et al., 2004; Hewson & Bennett, 1987). Medical records are subject to recording errors and inconsistencies due to varying medical criteria between hospitals (Hewson & Bennett, 1987; Joffe & Grisso, 1985). Recall bias may have also affected our findings and can be caused by factors such as the child’s current physical, emotional, mental, or behavioral state. For example, McIntosh et al. (2002) found that the number of obstetric complications recalled by mothers was not related to their own schizophrenic status but was instead related to measures of abnormal child behavior, suggesting that concern for child’s behavior may affect retrospective recall. Moreover, it may be possible that pregnancy and related events were more memorable to mothers expecting twins than for those expecting a single child. Additionally, because recall accuracy may be affected by culturally influenced factors, such as the importance of events and awareness and knowledge of conditions (Olson et al., 1997), these findings should be generalized with caution. Furthermore, our sample size is small, which may explain why not all results are significant, specifically regarding more rare medical outcomes. Finally, no information on chorion type was available in the medical birth records.
Despite these limitations, this study makes important contributions to the literature on validity of maternal recall for various perinatal factors. The questionnaire developed and used in this study provides data for medical and behavioral factors that are of interest to researchers, due to their associations with important health outcomes, but have not been examined elsewhere in regard to long-term recall validity. For instance, validity for maternal recall of Apgar scores and birth length has been assessed previously but only 6–10 weeks after delivery (Troude et al., 2008). Recent studies have shown associations between low Apgar scores and a high risk for cerebral palsy in term infants born in Sweden (Thorngren-Jerneck & Herbst, 2006). Our findings suggest that researchers using maternal reports to assess Apgar scores should do so with caution because of the low validity of recall. It could be that parents do not understand the medical terminology, and the information may be unclear to parents when they recall, which in turn may affect validity. Additionally, jaundice has recently been associated with disorders of psychological development (Maimburg et al., 2010), and prenatal vitamin use has been linked to outcomes such as childhood cancers (Goh & Koren, 2008). The present study also informs researchers in the development and use of recall questionnaires. The validity of recall for behavioral factors like smoking was low when mothers were asked to report continuous data within a recall period of almost 10 years. Thus, while the frequency of smoking may be a variable of interest to researchers due to its association with many long-term outcomes in offspring (Batty et al., 2006; Brook et al., 2006, 2008; Button et al., 2005; Lambe et al., 2006; Liu et al., 2013), it may be more suitable to present mothers with categorical answers, or ask within a more immediate recall period. Furthermore, since maternal knowledge and perception of the event’s importance may also affect recall validity (Hewson & Bennett, 1987; Mitchell et al., 1986; Olson et al., 1997), as different pre-, peri-, and post-natal events become increasingly associated as risk factors for offspring health, doctors and nurses should emphasize the importance of this information at or around the time of the delivery event. Healthcare professionals should also improve communication with parents in order to clarify an understanding of how various conditions, procedures, and other factors are defined.
In conclusion, our findings support that maternal recall, even in a twin sample, could be a reliable source for many pregnancy-related variables up to 10 years after the delivery event. However, maternal recall may not be appropriate for obtaining postnatal information, especially regarding twins, aside from the method of delivery, birth weight, and NICU admissions. Furthermore, this study also highlights the need for caution when using maternal report as a sole source of information, especially for information which mothers may not deem socially valuable (e.g., birth length) or events that require little involvement or changes from the mother (e.g., medical problems not requiring medication).
Appendix. Retrospective pre/peri/post-natal data Questionnaire*

Footnotes
This questionnaire was developed by Dr. Jianghong Liu.
References
- Baker LA, Barton M, Lozano DI, Raine A, Fowler JH. The Southern California Twin Register at the University of Southern California: II. Twin Research and Human Genetics. 2006;9:933–940. doi: 10.1375/183242706779462912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker LA, Jacobson KC, Raine A, Lozano DI, Bezdjian S. Genetic and environmental bases of childhood antisocial behavior: A multi-informant twin study. Journal of Abnormal Psychology. 2007;116:219–235. doi: 10.1037/0021-843X.116.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker LA, Tuvblad C, Wang P, Gomez K, Raine A. The Southern California Twin Register at the University of Southern California: III. Twin Research and Human Genetics. 2013;16:336–343. doi: 10.1017/thg.2012.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balchin I, Whittaker JC, Lamont RF, Steer PJ. Maternal and fetal characteristics associated with meconium-stained amniotic fluid. Obstetrics and Gynecology. 2011;117:828–835. doi: 10.1097/AOG.0b013e3182117a26. [DOI] [PubMed] [Google Scholar]
- Batty GD, Der G, Deary IJ. Effect of maternal smoking during pregnancy on offspring’s cognitive ability: Empirical evidence for complete confounding in the US national longitudinal survey of youth. Pediatrics. 2006;118:943–950. doi: 10.1542/peds.2006-0168. [DOI] [PubMed] [Google Scholar]
- Bergvall N, Iliadou A, Johansson S, de Faire U, Kramer MS, Pawitan Y, Cnattingius S. Genetic and shared environmental factors do not confound the association between birth weight and hypertension — A study among Swedish twins. Circulation. 2007;115:2931–2938. doi: 10.1161/CIRCULATIONAHA.106.674812. [DOI] [PubMed] [Google Scholar]
- Brook DW, Zhang C, Rosenberg G, Brook JS. Maternal cigarette smoking during pregnancy and child aggressive behavior. American Journal on Addictions. 2006;15:450–456. doi: 10.1080/10550490600998559. [DOI] [PubMed] [Google Scholar]
- Brook JS, Zhang CS, Fagan P. Exposure to parental cigarette smoking and child problem behaviors: A longitudinal study. Journal of Child and Family Studies. 2008;17:372–384. doi: 10.1007/s10826-007-9147-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant HE, Visser N, Love EJ. Records, recall loss, and recall bias in pregnancy: A comparison of interview and medical records data of pregnant and postnatal women. American Journal of Public Health. 1989;79:78–80. doi: 10.2105/ajph.79.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buka SL, Goldstein JM, Seidman LJ, Tsuang MT. Maternal recall of pregnancy history: Accuracy and bias in schizophrenia research. Schizophrenia Bulletin. 2000;26:335–350. doi: 10.1093/oxfordjournals.schbul.a033457. [DOI] [PubMed] [Google Scholar]
- Buka SL, Goldstein JM, Spartos E, Tsuang MT. The retrospective measurement of prenatal and perinatal events: Accuracy of maternal recall. Schizophrenia Research. 2004;71:417–426. doi: 10.1016/j.schres.2004.04.004. [DOI] [PubMed] [Google Scholar]
- Button TMM, Thapar A, McGuffin P. Relationship between antisocial behaviour attention-deficit hyperactivity disorder and maternal prenatal smoking. British Journal of Psychiatry. 2005;187:155–160. doi: 10.1192/bjp.187.2.155. [DOI] [PubMed] [Google Scholar]
- Cannon M, Jones PB, Murray RM. Obstetric complications and schizophrenia: Historical and meta-analytic review. American Journal of Psychiatry. 2002;159:1080–1092. doi: 10.1176/appi.ajp.159.7.1080. [DOI] [PubMed] [Google Scholar]
- Carbonne B, Cudeville C, Sivan H, Cabrol D, Papiernik E. Fetal oxygen saturation measured by pulse oximetry during labour with clear or meconium-stained amniotic fluid. European Journal of Obstetrics and Gynecology and Reproductive Biology. 1997;72(Suppl):S51–S55. doi: 10.1016/s0301-2115(97)02718-8. [DOI] [PubMed] [Google Scholar]
- Catov JM, Newman AB, Kelsey SF, Roberts JM, Sutton-Tyrrell KC, Garcia M, Ness RB. Accuracy and reliability of maternal recall of infant birth weight among older women. Annals of Epidemiology. 2006;16:429–431. doi: 10.1016/j.annepidem.2005.09.004. [DOI] [PubMed] [Google Scholar]
- Coolman M, de Groot CJ, Jaddoe VW, Hofman A, Raat H, Steegers EA. Medical record validation of maternally reported history of preeclampsia. Journal of Clinical Epidemiology. 2010;63:932–937. doi: 10.1016/j.jclinepi.2009.10.010. [DOI] [PubMed] [Google Scholar]
- D’Souza-Vazirani D, Minkovitz CS, Strobino DM. Validity of maternal report of acute health care use for children younger than 3 years. Archives of Pediatrics and Adolescent Medicine. 2005;159:167–172. doi: 10.1001/archpedi.159.2.167. [DOI] [PubMed] [Google Scholar]
- Delgado-Rodriguez M, Gomez-Olmedo M, Bueno-Cavanillas A, Garcia-Martin M, Galvez-Vargas R. Recall bias in a case-control study of low birth weight. Journal of Clinical Epidemiology. 1995;48:1133–1140. doi: 10.1016/0895-4356(94)00241-h. [DOI] [PubMed] [Google Scholar]
- Elliott JP, Desch C, Istwan NB, Rhea D, Collins AM, Stanziano GJ. The reliability of patient-reported pregnancy outcome data. Population Health Management. 2010;13:27–32. doi: 10.1089/pop.2009.0008. [DOI] [PubMed] [Google Scholar]
- Frontini MG, Srinivasan SR, Xu J, Berenson GS. Low birth weight and longitudinal trends of cardiovascular risk factor variables from childhood to adolescence: The Bogalusa heart study. BMC Pediatrics. 2004;4:22. doi: 10.1186/1471-2431-4-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Githens PB, Glass CA, Sloan FA, Entman SS. Maternal recall and medical records: An examination of events during pregnancy, childbirth, and early infancy. Birth. 1993;20:136–141. doi: 10.1111/j.1523-536x.1993.tb00438.x. [DOI] [PubMed] [Google Scholar]
- Goh YI, Koren G. Prenatal supplementation with multivitamins and the incidence of pediatric cancers: Clinical and methodological considerations. Pediatric Blood and Cancer. 2008;50:487–489. doi: 10.1002/pbc.21403. [DOI] [PubMed] [Google Scholar]
- Hessol NA, Missett B, Fuentes-Afflick E. Lower agreement on behavioral factors than on medical conditions in self-reported data among pregnant Latina women. Archives of Medical Research. 2004;35:241–245. doi: 10.1016/j.arcmed.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Hewson D, Bennett A. Childbirth research data —Medical records or women’s reports. American Journal of Epidemiology. 1987;125:484–491. doi: 10.1093/oxfordjournals.aje.a114554. [DOI] [PubMed] [Google Scholar]
- Jaspers M, de Meer G, Verhulst FC, Ormel J, Reijneveld SA. Limited validity of parental recall on pregnancy, birth, and early childhood at child age 10 years. Journal of Clinical Epidemiology. 2010;63:185–191. doi: 10.1016/j.jclinepi.2009.05.003. [DOI] [PubMed] [Google Scholar]
- Joffe M, Grisso JA. Comparison of antenatal hospital records with retrospective interviewing. Journal of Biosocial Science. 1985;17:113–119. doi: 10.1017/s0021932000015522. [DOI] [PubMed] [Google Scholar]
- Lambe M, Hultman C, Torrang A, MacCabe J, Cnattingius S. Maternal smoking during pregnancy and school performance at age 15. Epidemiology. 2006;17:524–530. doi: 10.1097/01.ede.0000231561.49208.be. [DOI] [PubMed] [Google Scholar]
- Launer LJ, Forman MR, Hundt GL, Sarov B, Chang D, Berendes HW, Naggan L. Maternal recall of infant-feeding events is accurate. Journal of Epidemiology and Community Health. 1992;46:203–206. doi: 10.1136/jech.46.3.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis S, Owen M, Murray R. Obstetric complications and schizophrenia: Methodology and mechanisms. In: Schultz S, Tamminga C, editors. Schizophrenia: Scientific progress. New York: Oxford University Press; 1989. pp. 56–68. [Google Scholar]
- Lewis SW, Murray RM. Obstetric complications, neurodevelopmental deviance, and risk of schizophrenia. Journal of Psychiatric Research. 1987;21:413–421. doi: 10.1016/0022-3956(87)90088-4. [DOI] [PubMed] [Google Scholar]
- Li R, Scanlon KS, Serdula MK. The validity and reliability of maternal recall of breastfeeding practice. Nutrition Reviews. 2005;63:103–110. doi: 10.1111/j.1753-4887.2005.tb00128.x. [DOI] [PubMed] [Google Scholar]
- Liu J. Early health risk factors for violence: Conceptualization, review of the evidence, and implications. Aggression and Violent Behavior. 2011;16:63–73. doi: 10.1016/j.avb.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Leung PW, McCauley L, Ai Y, Pinto-Martin J. Mother’s environmental tobacco smoke exposure during pregnancy and externalizing behavior problems in children. NeuroToxicology. 2013;34:167–174. doi: 10.1016/j.neuro.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Raine A, Wuerker A, Venables P, Mednick SA. The association of birth complications and externalizing behavior in early adolescents. Journal of Research on Adolescence. 2009;19(1):93–111. doi: 10.1111/j.1532-7795.2009.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumey LH, Stein AD, Ravelli AC. Maternal recall of birthweights of adult children: Validation by hospital and well baby clinic records. International Journal of Epidemiology. 1994;23:1006–1012. doi: 10.1093/ije/23.5.1006. [DOI] [PubMed] [Google Scholar]
- McCormick MC, Brooks-Gunn J. Concurrent child health status and maternal recall of events in infancy. Pediatrics. 1999;104:1176–1181. [PubMed] [Google Scholar]
- McIntosh AM, Holmes S, Gleeson S, Burns JK, Hodges AK, Byrne MM, Johnstone EC. Maternal recall bias, obstetric history and schizophrenia. British Journal of Psychiatry. 2002;181:520–525. doi: 10.1192/bjp.181.6.520. [DOI] [PubMed] [Google Scholar]
- McNeil TF, Sjöström K. The McNeil-Sjöström scale for obstetric complications. Malmö, Sweden: Department of Psychiatry, University Hospital, Lund University; 1995. [Google Scholar]
- Maehle BO, Vatten LJ, Tretli S. Birth length and weight as predictors of breast cancer prognosis. BMC Cancer. 2010;10:115. doi: 10.1186/1471-2407-10-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maimburg RD, Bech BH, Vaeth M, Moller-Madsen B, Olsen J. Neonatal jaundice, autism, and other disorders of psychological development. Pediatrics. 2010;126:872–878. doi: 10.1542/peds.2010-0052. [DOI] [PubMed] [Google Scholar]
- Melve KK, Gjessing HK, Skjaerven R, Oyen N. Infants’ length at birth: An independent effect on perinatal mortality. Acta Obstetricia et Gynecologica Scandinavica. 2000;79:459–464. [PubMed] [Google Scholar]
- Mitchell AA, Cottler LB, Shapiro S. Effect of questionnaire design on recall of drug exposure in pregnancy. American Journal of Epidemiology. 1986;123:670–676. doi: 10.1093/oxfordjournals.aje.a114286. [DOI] [PubMed] [Google Scholar]
- Mzayek F, Hassig S, Sherwin R, Hughes J, Chen W, Srinivasan S, Berenson G. The association of birth weight with developmental trends in blood pressure from childhood through mid-adulthood — The Bogalusa heart study. American Journal of Epidemiology. 2007;166:413–420. doi: 10.1093/aje/kwm098. [DOI] [PubMed] [Google Scholar]
- Olson JE, Shu XO, Ross JA, Pendergrass T, Robison LL. Medical record validation of maternally reported birth characteristics and pregnancy-related events: A report from the Children’s Cancer Group. American Journal of Epidemiology. 1997;145:58–67. doi: 10.1093/oxfordjournals.aje.a009032. [DOI] [PubMed] [Google Scholar]
- Quigley MA, Hockley C, Davidson LL. Agreement between hospital records and maternal recall of mode of delivery: Evidence from 12,391 deliveries in the UK Millennium Cohort Study. BJOG: International Journal of Obstetrics and Gynaecology. 2007;114:195–200. doi: 10.1111/j.1471-0528.2006.01203.x. [DOI] [PubMed] [Google Scholar]
- Reich W, Todd RD, Joyner CA, Neuman RJ, Heath AC. Reliability and stability of mothers’ reports about their pregnancies with twins. Twin Research. 2003;6:85–88. doi: 10.1375/136905203321536209. [DOI] [PubMed] [Google Scholar]
- Rice F, Lewis A, Harold G, van den Bree M, Boivin J, Hay DF, Thapar A. Agreement between maternal report and antenatal records for a range of pre and peri-natal factors: The influence of maternal and child characteristics. Early Human Development. 2007;83:497–504. doi: 10.1016/j.earlhumdev.2006.09.015. [DOI] [PubMed] [Google Scholar]
- SAS. SAS/STAT software: Changes and enhancements through release 9.2. Cary, NC: SAS Institute Inc; 2005. [Google Scholar]
- Silva ID, De Stavola B, McCormack V Collaborative Group on Pre-Natal Risk Factors and Subsequent Risk of Breast Cancer. Birth size and breast cancer risk: Re-analysis of individual participant data from 32 studies. PLOS Medicine. 2008;5:1372–1386. doi: 10.1371/journal.pmed.0050193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sou SC, Chen WJ, Hsieh WS, Jeng SF. Severe obstetric complications and birth characteristics in preterm or term delivery were accurately recalled by mothers. Journal of Clinical Epidemiology. 2006;59:429–435. doi: 10.1016/j.jclinepi.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Starks GC. Correlation of meconium-stained amniotic-fluid, early intrapartum fetal Ph, and Apgar scores as predictors of perinatal outcome. Obstetrics and Gynecology. 1980;56:604–609. [PubMed] [Google Scholar]
- Steer PJ, Eigbe F, Lissauer TJ, Beard RW. Interrelationships among abnormal cardiotocograms in labor, meconium staining of the amniotic-fluid, arterial cord blood-ph, and Apgar scores. Obstetrics and Gynecology. 1989;74:715–721. [PubMed] [Google Scholar]
- Sun C, Ponsonby AL, Wong TY, Brown SA, Kearns LS, Cochrane J, Mackey DA. Effect of birth parameters on retinal vascular caliber: The twins eye study in Tasmania. Hypertension. 2009;53:487–493. doi: 10.1161/HYPERTENSIONAHA.108.125914. [DOI] [PubMed] [Google Scholar]
- Thorngren-Jerneck K, Herbst A. Perinatal factors associated with cerebral palsy in children born in Sweden. Obstetrics and Gynecology. 2006;108:1499–1505. doi: 10.1097/01.AOG.0000247174.27979.6b. [DOI] [PubMed] [Google Scholar]
- Tomeo CA, Rich-Edwards JW, Michels KB, Berkey CS, Hunter DJ, Frazier AL, Buka SL. Reproducibility and validity of maternal recall of pregnancy-related events. Epidemiology. 1999;10:774–777. [PubMed] [Google Scholar]
- Troude P, L\Helias LF, Raison-Boulley AM, Castel C, Pichon C, Bouyer J, de La Rochebrochard E. Perinatal factors reported by mothers: Do they agree with medical records? European Journal of Epidemiology. 2008;23:557–564. doi: 10.1007/s10654-008-9268-9. [DOI] [PubMed] [Google Scholar]
- Yawn BP, Suman VJ, Jacobsen SJ. Maternal recall of distant pregnancy events. Journal of Clinical Epidemiology. 1998;51:399–405. doi: 10.1016/s0895-4356(97)00304-1. [DOI] [PubMed] [Google Scholar]


