Abstract
Purpose
Trauma team activation (TTA) has been shown to have fundamental impact on trauma patients' outcomes. The purpose of this study was to evaluate the short-term outcomes of use of a new TTA protocol in the management of major trauma patients who underwent exploratory laparotomy.
Methods
The medical records of trauma patients who had been treated by the new TTA protocol (NT) over 18 months were compared with those of trauma patients treated by the old TTA protocol (OT) over 18 months. Comparisons between the two groups in terms of the time interval between accident and emergency room (ER) arrival, between ER arrival and CT scanning, between ER arrival and operating room (OR) presentation, between accident and OR presentation, mean intensive care unit (ICU) stay, mean hospital stay, mortality within 24 hours, mean mortality within one month, and overall mortality were performed using the Pearson chi-squared test and Student t-test.
Results
The time interval between accident and ER arrival, between ER arrival and CT scanning, between ER arrival and OR presentation, and between accident and OR presentation was found to have decreased significantly with the use of NT compared to OT. However, the mean ICU stay, mean hospital stay, mortality within 24 hours, mortality within one month, and overall mortality were found not to have improved.
Conclusion
While initiation of early TTA can shorten the time interval in the management of trauma patients, it may not improve patient outcomes.
Keywords: Morbidity, Mortality, Trauma centers, Trauma team activation
INTRODUCTION
Many nations have been attempting to improve the management of patients with severe trauma, the main cause of death for young people worldwide [1]. It is well known that the mortality rate of severe trauma patients who are treated in specialized trauma centers equipped with a highly qualified trauma team and medical devices is significantly lower than that of patients treated in nontrauma centers [2,3]. In addition to being equipped with hardware, specialized trauma centers use effective and rapid management techniques, such as trauma team activation (TTA). TTA is initiated by some criteria and enable trauma surgeons (TSs) to perform a multidisciplinary approach [4,5,6,7]. Although the effects of use of TTA are tremendous, there is no best TTA protocol. Each trauma center must develop its own TTA protocol because the circumstances of each trauma center are unique.
Abdominal organs are vulnerable to trauma because of the lack of protection provided by bony structures. Some patients with major abdominal trauma develop life-threatening conditions that cause death. Accordingly, timely arrest of uncontrolled hemorrhage and control of contamination is clinically important for better results. Based on this knowledge, our hospital formed a trauma team and developed modified TTA criteria based on our unique circumstances. In addition, in 2012 two surgeons were designated to perform emergency laparotomy for major abdominal trauma exclusively, and have been doing so since. The goals of these actions are to shorten the time interval between emergency room (ER) arrival and definitive surgery and improve trauma intensive care unit management and overall outcomes. The purpose of this study was to evaluate the short-term outcomes of use of new TTA and the effectiveness of appointing a designated TS in the management of major trauma patients who underwent exploratory laparotomy.
METHODS
The medical records of trauma patients treated by the old TTA protocol (OT), which had been used from October 2010 to February 2012, and the new TTA protocol (NT), which had been used from March 2012 to August 2013, respectively, were retrospectively reviewed. Cases of prehospital death and of transfer to other hospitals were excluded from the analysis. The trauma team is composed of five emergency medicine (EM) physicians, two general surgeons whose subspecialty is hepatobiliary and vascular surgery, respectively, two cardiovascular surgeons, two neurosurgeons, and two anesthesiologists.
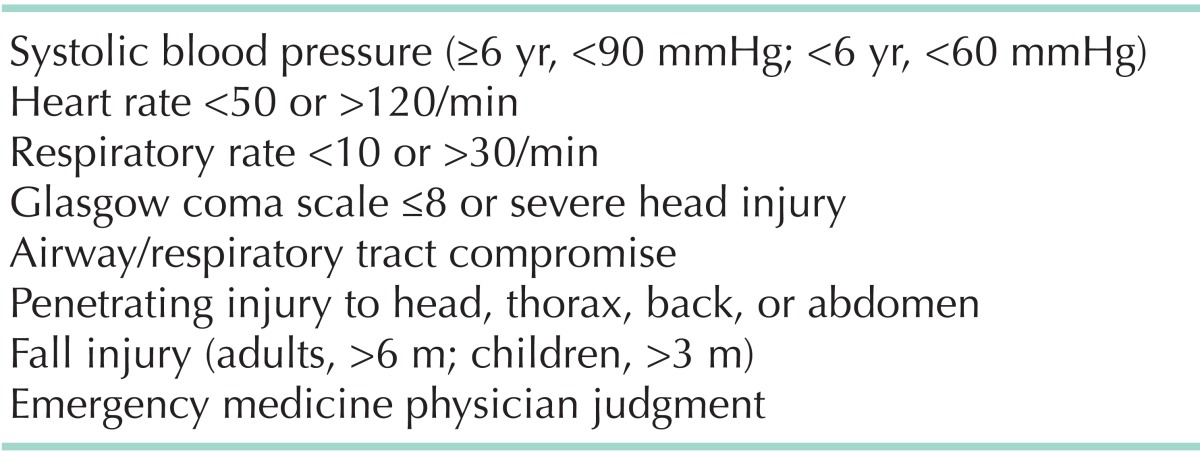
The main differences between OT and NT are the criteria of activation. Previously, an EM physician called the residents of each department according to the organ of injury, which was identified mainly by observation of patient symptoms and signs and focused assessment with sonography for trauma or CT. NT was developed according to the simplified criteria for TTA based on the field triage decision scheme outlined by American College of Surgeons Committee on Trauma [8]. NT is initiated very early in treatment based on assessment of vital signs, trauma mechanism, and injury type (Table 1). When a patient who meets the NT criteria arrives at the ER, Emergency Department resident initiates NT through the activation of electronic medical record (EMR) system. The EMR automatically texts data regarding the NT criteria, vital signs, mechanism of injury (MOI), and arrival time to three attending doctors-a general surgeon, a cardiovascular surgeon, and the trauma on-call neurosurgeon-who arrive at the ER within 15 minutes of receiving the text. After conducting a primary and secondary survey, the doctors decide on the necessity of performing preoperative CT scanning, which should be conducted within 30 minutes, and emergency surgery, which should be decided upon within 1 hour, at the ER.
Table 1.
Criteria for new trauma team activation
The Chosun University Hospital Institutional Review Board approved this study, and the need to obtain informed consent was waived because of the study's retrospective nature. Statistical analysis was performed using IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA). Comparisons between the two groups were performed using the Pearson chi-squared test and Student t-test and differences were considered statistically significant when P-value was less than 0.05.
RESULTS
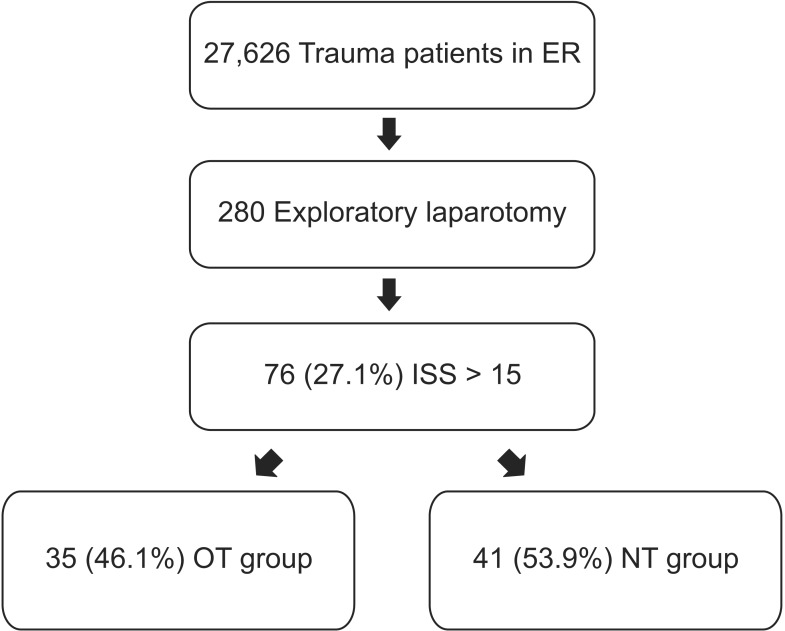
Of the 27,626 trauma patients admitted to the ER during the study period, 280 patients underwent exploratory laparotomy. Among them, 76 patients had an injury severity score (ISS) higher than 15. Thirty-five had been treated by OT and 41 by NT (Fig. 1). Of the 41 patients in the NT group, 32 were male. The mean age was 52.5 years. Thirty-eight had experienced blunt trauma, and 3 had experienced penetrating trauma. Twenty-seven had been transferred from the local hospital, and 14 had visited the ER primarily. Of the 38 patients who had undergone CT scanning in the local hospital, CT was reperformed in 18 patients (Table 2). Twelve had been traffic accident (TA) drivers, 5 TA motorcycle drivers, 3 TA passengers, 4 TA pedestrians, 1 TA cultivator (farm machine), and 1 TA bicyclist; 6 had been victims of physical assault; 5 had experienced falls; and 3 had experienced stab injuries. Nine had an injury in small intestine, 8 in liver, 6 in mesentery, 4 in spleen, 4 in blood vessel, 2 in pancreas and 1 in diaphragm, stomach, kidney, respectively (Table 3).
Fig. 1.
Patient enrollment process. ER, emergency room; ISS, injury severity score; OT, old trauma team activation protocol; NT, new trauma team activation protocol.
Table 2.
Patient demographics
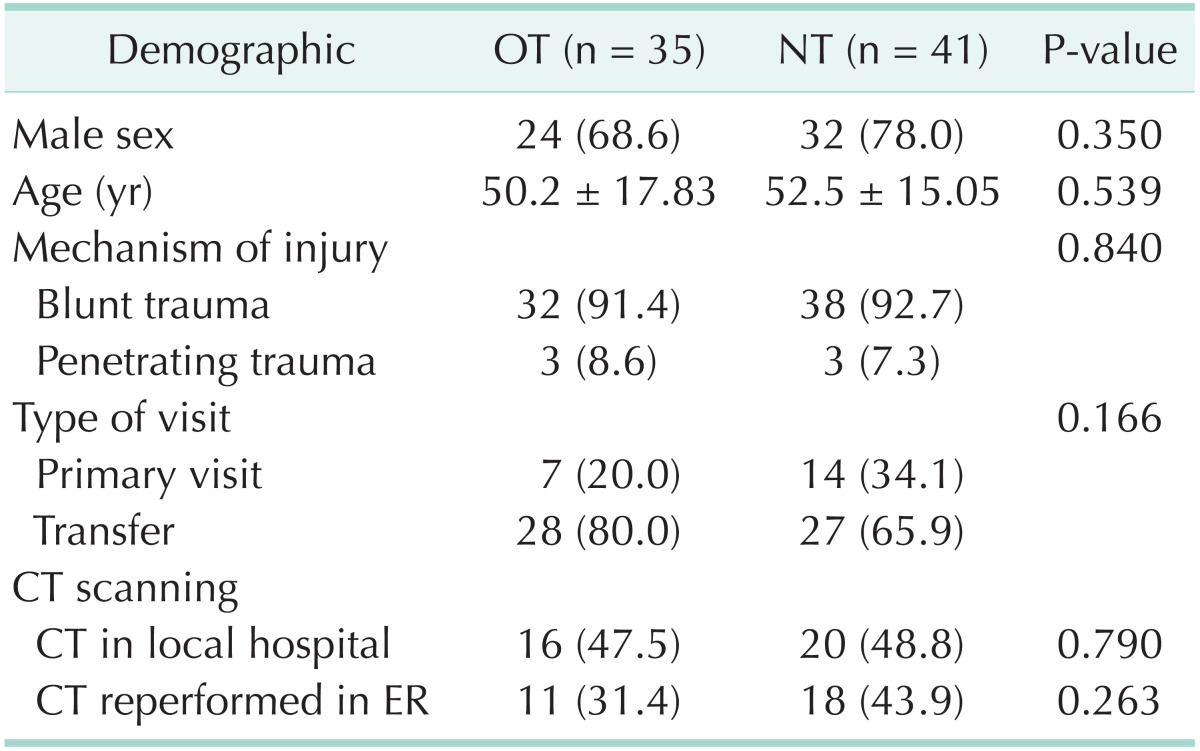
Values are presented as number (%) or mean ± standard deviation.
OT, old trauma team activation protocol; NT, new trauma team activation protocol; ER, emergency room.
Table 3.
Mechanism of injury and organ of major injury
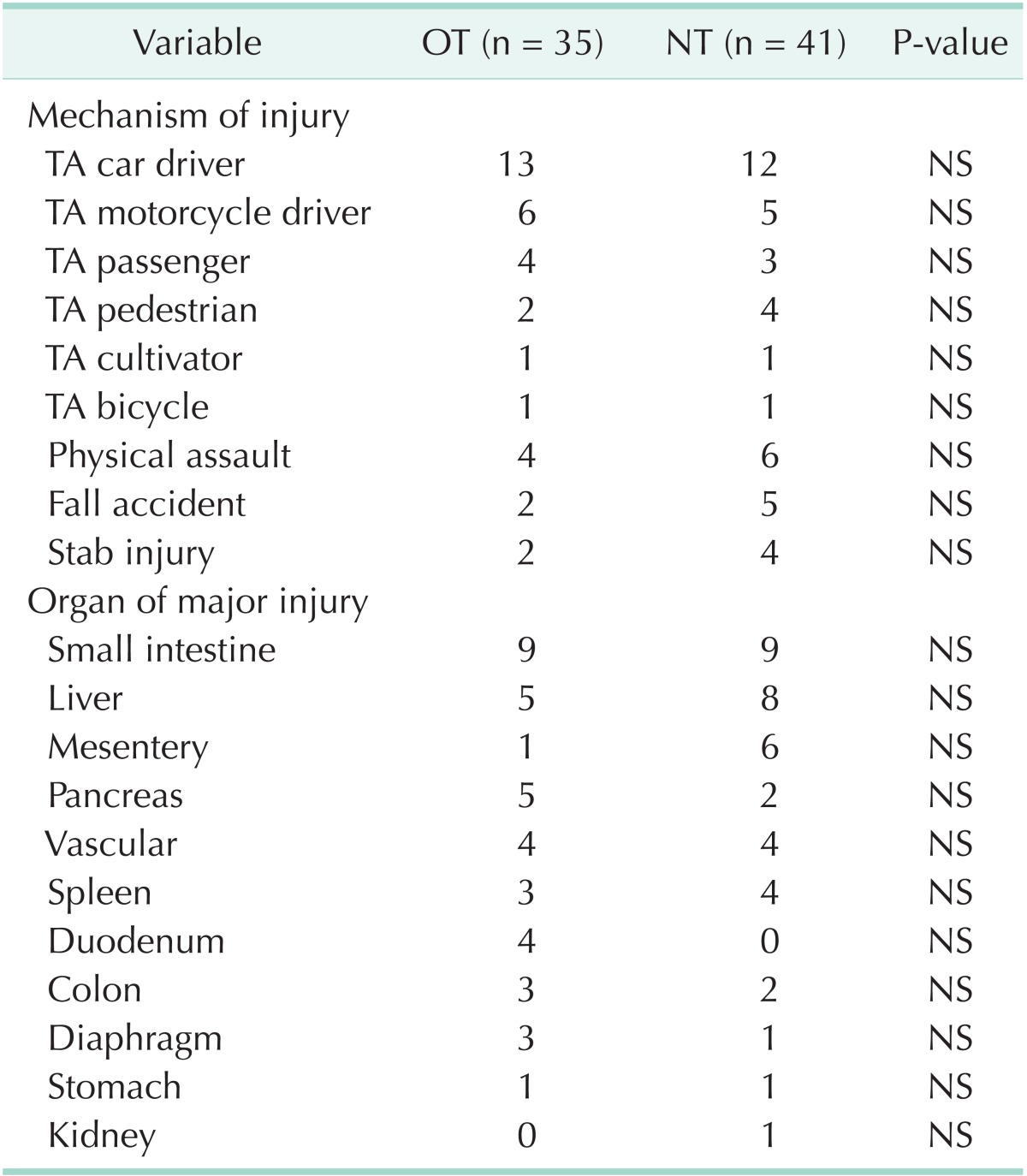
OT, old trauma team activation protocol; NT, new trauma team activation protocol; TA, traffic accident; NS, not significant.
No statistically significant differences were found between the OT and NT groups regarding mean ISS, revised trauma score (RTS), Glasgow coma scale (GCS) score, systolic blood pressure, respiratory rate, and trauma and injury severity score (Table 4). The time interval between the accident and ER arrival, between ER arrival and CT scanning, between ER arrival and operating room (OR) presentation, and between the accident and OR presentation was found to be significantly shorter for the NT group compared to the OT group. The mean surgical duration for all patients was 198.6 minutes. Four combined operations were performed in each group. The mean ICU stay and hospital stay of all patients were 4.9 and 19.2 days, respectively. The mean mortality within 24 hours, within 1 month, and overall of all patients were 6%, 9%, and 9% respectively. Although use of NT was found to have decreased the time interval between ER arrival and OR presentation by 73 minutes and between accidents to OR presentation by 147 minutes, it was not found to yield any survival benefit compared to using OT (Table 5).
Table 4.
Injury and trauma severity scores and physiological indicators
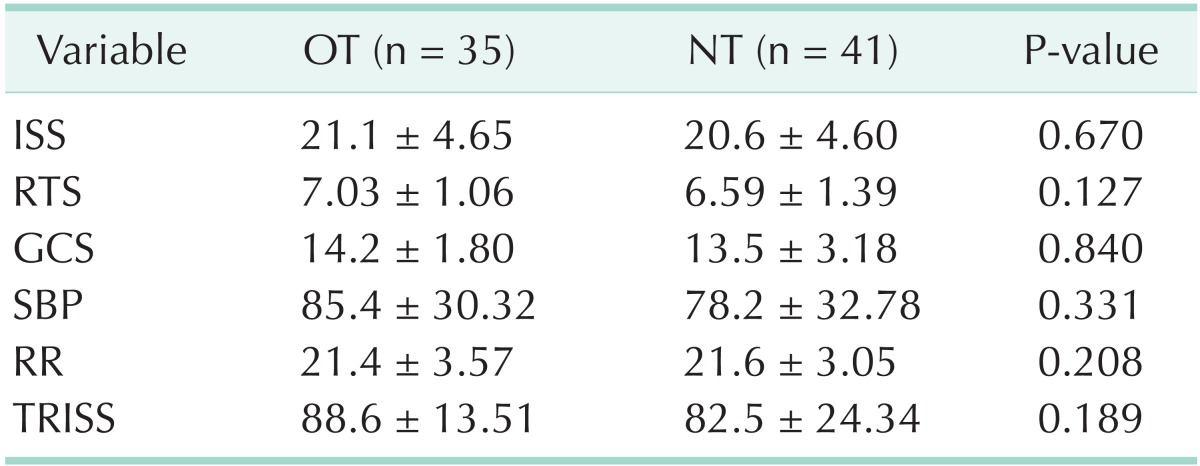
Values are presented as mean ± standard deviation.
OT, old trauma team activation protocol; NT, new trauma team activation protocol; ISS, injury severity score; RTS, revised trauma score; GCS, Glasgow coma scale; SBP, systolic blood pressure; RR, respiratory rate; TRISS, trauma and injury severity score.
Table 5.
Patient outcomes
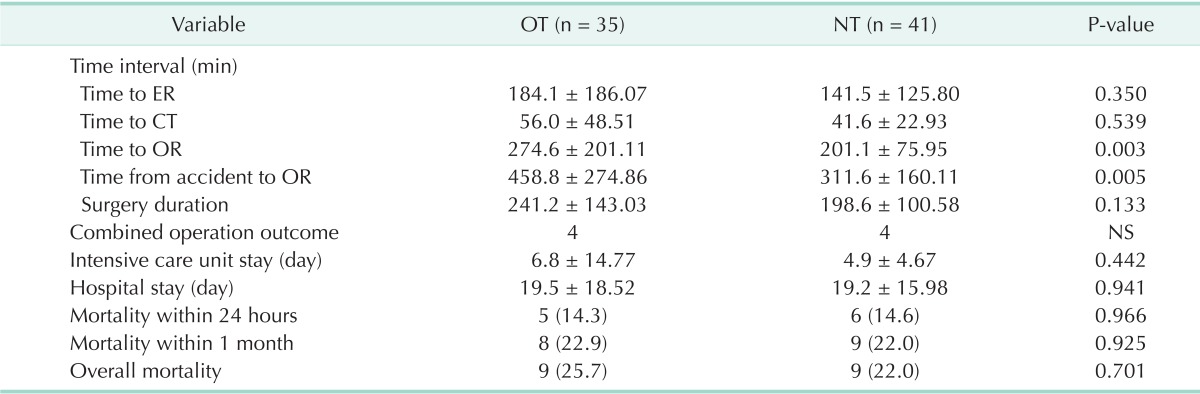
Values are presented as mean ± standard deviation or number (%).
OT, old trauma team activation protocol; NT, new trauma team activation protocol; ER, emergency room; OR, operative room.
DISCUSSION
Use of TTA is considered a fundamental element in managing trauma patients, with a recent meta-analysis reporting a 15% reduction in mortality with the use of a trauma system [9]. While trauma centers use different activation methods and criteria, TTA notification is typically performed via light panel, beeper, or cell phone text. Many trauma centers are calling for modification of existing TTA protocol to achieve better outcomes. Such modification should be based on many revisions after short-term evaluation and in consideration of the resources available to provide trauma care. Compared to those in Western nations, most trauma centers in our nation have limited resources. The findings of this study regarding the short-term results of TTA modification are thus valuable, especially for trauma centers with resources similar to those of the hospital studied here.
In the past, most TTA protocols were based on the organ of injury, the identification of which is confirmed mainly by CT scanning. While use of this anatomic indicator has improved the accuracy of major trauma activation and resulted in more cost-efficient resource use in terms of deployment of surgeons and other staff and use of the OR [10], it requires considerable time. Specifically, it requires that EM physicians decide which patients need CT scanning, which area of the body should be scanned, and which technique should be used to interpret the radiologic findings, and may require consultation with a radiologist. As TTA should be performed after completion of all these processes, it may result in the late involvement of the TS. As it is well known that early presence of a TS on the trauma team reduces resuscitation time and time to incision for emergency operations [11], many trauma centers are changing TTA protocol to promote earlier involvement of the TS. For this purpose, many current TTA protocols are based on more objective and simple criteria, such as presence of unstable vital signs, advanced age, GCS, MOI, and laboratory parameters.
The most commonly used simple TTA indicator is systolic hypotension, which has been found to be a valid indicator for TTA. One study of patients with prehospital hypotension found that nearly 50% required operative intervention and an additional 25% required ICU admission [12]. Advanced age may also be a TTA criterion, as elderly trauma patients, even those with minor or moderately severe injuries, have been found to have high mortality. Nevertheless, a significant number of elderly patients with severe injuries do not meet the standard criteria for TTA. It is thus suggested that age 70 years and over alone should be a criterion for TTA [13]. Prehospital GCS score is a reliable parameter for predicting hospital admission after motor vehicle collision (MVC). When obvious indicators, such as hypoxemia, multiple long bone fractures, or focal neurologic deficits, for TTA are lacking, prehospital GCS score may be used [14]. MOI has also been suggested for use as a criterion, regardless of physiologic indicators [15]. Use of these simple indicators may enable initiation of TTA earlier and more objectively such that even non-physicians can perform it [16].
As expected, use of NT based on these simple criteria was found to have resulted in earlier TTA initiation and reduction in the time interval between ER arrival and CT scanning compared to use of OT compared to that reported by a study of TTA in a trauma center conducted at another university hospital in our nation, the time to CT scanning and emergency surgery was found to be statistically significantly shorter in the current study (Table 6) [17,18]. Moreover, use of NT was found to have decreased the time interval between ER arrival and emergency operation by 73 minutes compared to use of OT. However, use of NT was not found to have improved patient outcomes compared to use of OT. ICU stay, hospital stay, mortality within 24 hours, mortality within one month, and overall mortality found not have been improved at a statistically significant level (Table 6). These findings may be results of the heterogeneity of MOI, injured abdominal organs, accompanying injuries, and type of surgery between two groups. In particular, we enrolled the cases of abdominal injury requiring exploratory laparotomy only. We expect the outcomes of TTA would be better if we compared the results prospectively with the same study period and better design. Although use of NT was found to have decreased the time interval between ER arrivals and OR presentation, this interval is still longer than that of Western and Japanese trauma centers. This delay is not due to TTA defects but rather lack of trauma resources, such as on-call trauma surgeons, spare anesthesiologists, and OR availability. This delay thus cannot be reduced without incurring high costs, such as by hiring additional TS and increasing the number of ORs and trauma coordinators. However, hospitals unable to incur such costs may aim to decrease the interfacility transport time. Recently, the Ministry of Health and Welfare designated 35 major trauma-specified centers (MTSCs) and prepared a budget for preparing the trauma care resources. However, many teaching hospitals failed to be designated, as they can use the TTA protocols of MTSCs but cannot prepare the trauma resources necessary for designation. Non-MTSCs need to develop effective interfacility transfer protocols in order to improve the nationwide outcomes of trauma patients [19].
Table 6.
Comparison of the effectiveness of trauma team activation protocol
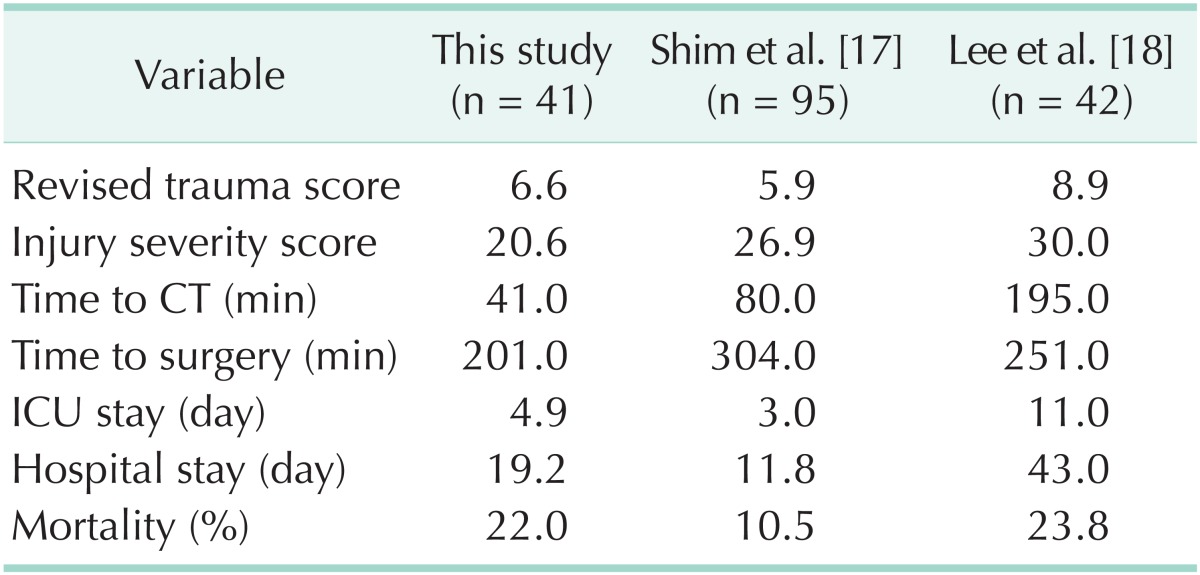
ICU, intensive care unit.
While it is difficult to define the ideal time interval between ER arrival and emergency surgery, Western trauma centers generally define it as within 2 hours. A study of the Royal London Hospital found that the mean duration from ER arrival to emergency surgery was 56 minutes for blunt trauma and 37 minutes for penetrating trauma [20]. Another study using American College of Surgeons audit filters found that performance of laparotomy more than 2 hours after admission resulted in increased mortality and longer ICU and hospital stay [21].
This study faced several limitations that should be considered when reviewing the findings. First, the cohorts examined had different time period and resultant heterogeneity. Second, the long-term outcome after hospital discharge was not examined. Third, compared to use of anatomic indicators, use of simple TTA criteria poses the risk of over-triage. Although it is important issue regarding interfacility referral, the extent of over-triage was not examined.
ACKNOWLEDGEMENTS
Present study was supported by grants from the Clinical Medicine Research Institute at Chosun University Hospital, 2012.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Rivara FP, Grossman DC, Cummings P. Injury prevention. First of two parts. N Engl J Med. 1997;337:543–548. doi: 10.1056/NEJM199708213370807. [DOI] [PubMed] [Google Scholar]
- 2.Demetriades D, Martin M, Salim A, Rhee P, Brown C, Chan L. The effect of trauma center designation and trauma volume on outcome in specific severe injuries. Ann Surg. 2005;242:512–517. doi: 10.1097/01.sla.0000184169.73614.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 4.Lehmann RK, Arthurs ZM, Cuadrado DG, Casey LE, Beekley AC, Martin MJ. Trauma team activation: simplified criteria safely reduces overtriage. Am J Surg. 2007;193:630–634. doi: 10.1016/j.amjsurg.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 5.Kouzminova N, Shatney C, Palm E, McCullough M, Sherck J. The efficacy of a two-tiered trauma activation system at a level I trauma center. J Trauma. 2009;67:829–833. doi: 10.1097/TA.0b013e3181b57b6d. [DOI] [PubMed] [Google Scholar]
- 6.Williams D, Foglia R, Megison S, Garcia N, Foglia M, Vinson L. Trauma activation: are we making the right call? A 3-year experience at a Level I pediatric trauma center. J Pediatr Surg. 2011;46:1985–1991. doi: 10.1016/j.jpedsurg.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Cherry RA, King TS, Carney DE, Bryant P, Cooney RN. Trauma team activation and the impact on mortality. J Trauma. 2007;63:326–330. doi: 10.1097/TA.0b013e31811eaad1. [DOI] [PubMed] [Google Scholar]
- 8.American College of Surgeons; Committee on Trauma. Resources for optimal care of the injured patient. Chicago, IL: ACS; 2006. [Google Scholar]
- 9.Celso B, Tepas J, Langland-Orban B, Pracht E, Papa L, Lottenberg L, et al. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60:371–378. doi: 10.1097/01.ta.0000197916.99629.eb. [DOI] [PubMed] [Google Scholar]
- 10.Krieger AR, Wills HE, Green MC, Gleisner AL, Vane DW. Efficacy of anatomic and physiologic indicators versus mechanism of injury criteria for trauma activation in pediatric emergencies. J Trauma Acute Care Surg. 2012;73:1471–1477. doi: 10.1097/TA.0b013e3182782789. [DOI] [PubMed] [Google Scholar]
- 11.Khetarpal S, Steinbrunn BS, McGonigal MD, Stafford R, Ney AL, Kalb DC, et al. Trauma faculty and trauma team activation: impact on trauma system function and patient outcome. J Trauma. 1999;47:576–581. doi: 10.1097/00005373-199909000-00028. [DOI] [PubMed] [Google Scholar]
- 12.Franklin GA, Boaz PW, Spain DA, Lukan JK, Carrillo EH, Richardson JD. Prehospital hypotension as a valid indicator of trauma team activation. J Trauma. 2000;48:1034–1037. doi: 10.1097/00005373-200006000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Demetriades D, Sava J, Alo K, Newton E, Velmahos GC, Murray JA, et al. Old age as a criterion for trauma team activation. J Trauma. 2001;51:754–756. doi: 10.1097/00005373-200110000-00022. [DOI] [PubMed] [Google Scholar]
- 14.Norwood SH, McAuley CE, Berne JD, Vallina VL, Creath RG, McLarty J. A prehospital glasgow coma scale score < or = 14 accurately predicts the need for full trauma team activation and patient hospitalization after motor vehicle collisions. J Trauma. 2002;53:503–507. doi: 10.1097/00005373-200209000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Craven JA. Paediatric and adolescent horse-related injuries: does the mechanism of injury justify a trauma response? Emerg Med Australas. 2008;20:357–362. doi: 10.1111/j.1742-6723.2008.01107.x. [DOI] [PubMed] [Google Scholar]
- 16.Qazi K, Kempf JA, Christopher NC, Gerson LW. Paramedic judgment of the need for trauma team activation for pediatric patients. Acad Emerg Med. 1998;5:1002–1007. doi: 10.1111/j.1553-2712.1998.tb02780.x. [DOI] [PubMed] [Google Scholar]
- 17.Shim H, Jang JY, Lee JG, Kim S, Kim MJ, Park YS, et al. Application of critical pathway in trauma patients. J Trauma Inj. 2012;25:159–165. [Google Scholar]
- 18.Lee DK, Lee KH, Cha KC, Park KH, Choi HJ, Kim H, et al. Effectiveness of simple trauma team activation criteria on prognosis of severe trauma patients. J Korean Soc Traumatol. 2009;22:71–76. [Google Scholar]
- 19.Cho S, Jung K, Yeom S, Park S, Kim H, Hwang S. Change of inter-facility transfer pattern in a regional trauma system after designation of trauma centers. J Korean Surg Soc. 2012;82:8–12. doi: 10.4174/jkss.2012.82.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simpson E, MacAteer E, Visram A. Review of paediatric trauma admissions at the royal london hospital (February 98 to february 99) Paediatr Anaesth. 2000;10:696–697. doi: 10.1111/j.1460-9592.2000.ab01q.x. [DOI] [PubMed] [Google Scholar]
- 21.Copes WS, Staz CF, Konvolinka CW, Sacco WJ. American College of Surgeons audit filters: associations with patient outcome and resource utilization. J Trauma. 1995;38:432–438. doi: 10.1097/00005373-199503000-00027. [DOI] [PubMed] [Google Scholar]