Abstract
Context
Lesbian, gay, bisexual, and transgender (LGBT) people are at increased risk for the adverse effects of tobacco use given their high prevalence of use, especially smoking. Evidence regarding cessation is limited. To determine if efficacious interventions are available and to aid the development of interventions, a systematic review was conducted of gray and peer-reviewed literature describing clinical, community, and policy interventions as well as knowledge, attitudes, and behaviors regarding tobacco use cessation among LGBT people.
Evidence acquisition
Eight databases for articles from 1987 to April 23, 2014 were searched. In February–November 2013, authors and researchers were contacted to identify gray literature.
Evidence synthesis
The search identified 57 records, of which 51 were relevant and 22 were from the gray literature; these were abstracted into evidence tables, and a narrative synthesis was conducted in October–May 2014. Group cessation curricula tailored for LGBT populations were found feasible to implement and show evidence of effectiveness. Community interventions have been implemented by and for LGBT communities; although these interventions showed feasibility, no rigorous outcome evaluations exist. Clinical interventions show little difference between LGBT and heterosexual people. Focus groups suggest that care is needed in selecting messaging used in media campaigns.
Conclusions
LGBT-serving organizations should implement existing evidence-based tobacco dependence treatment and clinical systems to support treatment of tobacco use. A clear commitment from government and funders is needed to investigate whether sexual orientation and gender identity moderate the impacts of policy interventions, media campaigns, and clinical interventions.
Introduction
Tobacco use among lesbian, gay, bisexual, and transgender (LGBT) people constitutes a major health inequality.1,2 Findings confirming this large and persistent disparity span study design, sampling method, geographic location, and population subgroups.1 In the U.S., LGBT adult smoking prevalence is 68% higher than that of heterosexuals.2 Although data are limited globally, similar disparities appear to be present in population-based sampling in other countries (e.g., England,3 Mexico4). Although reasons for these disparities remain unclear,5 researchers have proposed several explanations: historic exposure to community spaces6,7 and media8–10 where smoking was normative; targeted marketing by the tobacco industry11–13; pro-tobacco community norms14,15; and the impacts of stigma, discrimination, and stress.5,16
Researchers have also noted potential barriers to cessation services for LGB populations17 and preferences for LGBT-specific cessation services.18 Targeted cessation services may be needed, as some stressors are unique to LGBT lives (e.g., accepting one’s LGBT identity, prejudice against LGBT people), some cues to smoke may be unique to LGBT lives (e.g., not being accepted by family), and tobacco use may be used to rebel against or promote particular gender identities.5,19,20 At the population level, the strength of state tobacco programs may play a role in LGBT tobacco cessation,21 and there is worrisome evidence that certain evidence-based tobacco interventions may even exacerbate disparities for vulnerable populations.22–25 Indeed, a recent systematic review found that only interventions that increase the unit cost of cigarettes had a pro-equity effect, and non-targeted cessation campaigns increased disparities.23 Too little evidence addresses the impact of policy-based interventions on vulnerable populations.26,27
The need for interventions to reduce this disparity and its health consequences is compelling; yet, little is known about the need for tailored interventions for LGBT people or about the efficacy, reach, and effectiveness of existing individual, group, or policy interventions in promoting tobacco use cessation among LGBT people. Synthesis of such information can accelerate and improve intervention research, and lessons learned from community-based efforts can inform research design and intervention innovations.28 No RCTs of LGBT-specific cessation interventions were identified in the 2008 Public Health Service Clinical Update,29 and the IOM report on LGBT health30 was largely silent on this disparity and interventions to address it.31 A review of interventions among special populations from 2000 to 2005 identified only one study addressing cessation among LGBT people.32 Nonetheless, a systematic screening and assessment of LGBT community-based tobacco-related interventions indicates that LGBT-targeted tobacco interventions do exist, albeit often without peer-reviewed, published evaluations.33
This study aimed to review the literature regarding: (1) clinical treatment of tobacco dependence among LGBT populations; (2) strategies used to increase the number of LGBT tobacco users who attempt to quit and improve the success rate of LGBT tobacco users attempting to quit (e.g., community, policy, and media interventions); and (3) LGBT populations’ knowledge, attitudes, and behaviors related to tobacco cessation.
Methods
Search Strategy
Search terms were iteratively developed in PubMed until no relevant new results were identified,a and then the controlled vocabulary (i.e., medical subject headings [MeSH] terms) was translated into the controlled vocabulary of other databases providing this feature. This search was implemented on April 23, 2014, in eight electronic databases: Cochrane Central Register of Controlled Trials via Wiley Online Library; Cumulative Index to Nursing and Allied Health Literature (CINAHL), Global Health, PsycINFO, and Social Work Abstracts via EBSCO; Embase; PubMed; and Scopus. In Embase and EBSCO databases, MEDLINE records were excluded, as they are included in PubMed. The search was not restricted by date, language, or geography. Full search strings for each database and a review protocol are available from the first author.
As publication bias can result in unsuccessful interventions not being published,34 the authors decided to search for unpublished reports relating to the study aims. Program innovations are often created by practitioners (“practice-based evidence”), and documentation of these innovations can contribute to the design of interventions that are more feasible to implement in real-world settings.28,35 Thus, from January to November 2013, the first author sent e-mails to corresponding authors (n=19) of included studies and individuals (n=38) known to have an interest in LGBT tobacco treatment by the authors of this review or suggested by the researchers that were contacted. Unpublished manuscripts, manuscripts in press, conference papers, conference posters, evaluation reports, and grant close-out reports related to the key study aims were requested. Manuscripts in progress and pending submission or currently in the peer-review process were not eligible.
Inclusion Coding
Interventions were defined to include pharmacotherapy, clinical approaches, behavioral counseling, media campaigns, public policy, and combinations thereof. Studies not available in English or published prior to 1987 were excluded. Interventions focused on people living with HIV/AIDS were included if reporting specific results for men who have sex with men (MSM) or with gay or bisexual men. Survey research and qualitative research were included if they were relevant to study aims. Two authors (JGLL) and (AKM or CAM) independently reviewed each title, abstract, and, as necessary, full-text article to code for inclusion and exclusion. The authors resolved coding differences through discussion.
Data Abstraction
From October 2014 to May 2014, one author abstracted the following data from each study into evidence tables (JGLL) in Microsoft Word (Redmond WA), which were then reviewed by another author for accuracy (CAM). Study characteristics included study design, population, dates, intervention description, number of participants, attrition, outcome(s), and funding source. Where possible, both intent-to-treat and treatment-of-the-treated quit rates at the intervention endpoint and at the longest follow-up period are reported. General estimates of efficacy (i.e., abstinence at 6-month follow-up) from the Public Health Service’s “Treating Tobacco Use and Dependence: 2008 Update” report are presented for comparison.29
Results
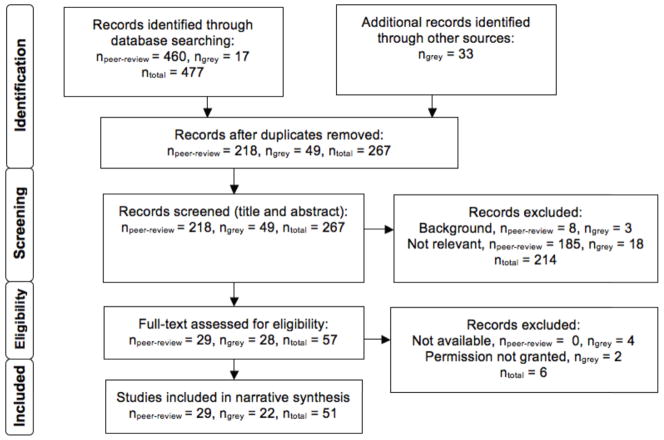
Figure 1, based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines,36 shows the inclusion process. The search identified 57 records, but copies of the full text of four records were unavailable, and permission to report on the results of two grant reports was not obtained. Twenty-nine peer-reviewed and 22 gray literature citations were included. One previous systematic review, which identified a single study, was not included in the current review.32 There were 15 citations about 14 clinical (n=9)37–46 or clinical systems–based (n=5)47–51 interventions to treat tobacco use dependence, and nine citations regarding seven community and policy interventions to increase cessation.6,52–59 Of these, five provided comparisons on LGBT versus heterosexual outcomes.37,41,50,51,56 There were 26 studies that focused on knowledge, intentions, attitudes, and behaviors regarding cessation.17,18,20,60–82 A full list of included studies, by topic area, is found in the Appendix.
Figure 1.
PRISMA flow diagram of study inclusion, April 23, 2014
Clinical Treatment of Tobacco Dependence among Lesbian, Gay, Bisexual, and Transgender Populations
The nine identified clinical interventions were predominantly cessation groups (with or without nicotine replacement therapy)33–35,37–40,46 and two clinical trials.37,41 Community organizations, notably the Coalition of Lavender Americans on Smoking and Health (CLASH), have adapted group cessation curricula into The Last Drag38,43 and Bitch to Quit programs.45 In the United Kingdom, an LGBT-tailored cessation group program showed positive results generally comparable to national results (45% abstinent [intent-to-treat] at seventh week versus 53% nationally [of those setting a quit date]),39 and this program was replicated in Zurich, Switzerland, showing a 29% quit rate at 6 months.46 Evaluations of these programs suggest heterogeneity of efficacy with quit rates (range, 6% at 3 months44 to 36% at 6 months38) both above and below other group-based interventions in the general population (14%, 95% CI=12%–16%, at 6 months)29 and highlight the feasibility of implementing smoking-cessation treatments at health centers and community organizations. These community-driven programs were conducted with diverse populations and across genders. However, one attempt at recruiting friendship networks to cessation programs found few groups of friends interested in enrolling.40 Two clinical trials were identified, which used intensive counseling and pharmacotherapy without tailoring to LGBT populations. In one,41 a post-hoc analysis of male participants showed that quit rates did not differ based on sexual orientation (59% vs 57% at the eighth week of treatment). In the other,37 LGBT and heterosexual smokers showed no difference in cessation at the 104th week of follow-up (38% vs 40%, respectively).
Clinical systems–based interventions at the organizational level for healthcare providers included adding identification systems for smokers,49,50 cultural competency trainings and implementation of sexual orientation questions for quitlines,47,48 and an analysis of receipt of physician advice to quit for LGBT smokers.51 As part of Communities Putting Prevention to Work, Howard Brown Health Center, an LGBT-serving community health center, received funding to implement tobacco screening questions as a “vital sign”83 into its electronic health record system: Ask, Advise, Refer. Evaluation results showed that of the 8,854 tracked medical visits, documentation of tobacco use status increased 30 percentage points, from 53% to 83% and, among identified smokers, receipt of cessation advice or treatment increased from 61% to 76%.49 Huber et al.50 reported on the implementation of a half-day training on tobacco dependence treatment among medical providers at a Swiss HIV clinic that also instituted a tobacco checklist at semi-annual clinic visits. Data collected 2 years after intervention showed that 84% of clients had documented smoking status and, of smokers, brief cessation counseling was reported for 80%. No difference was found for HIV-positive patients in the MSM transmission group compared with other transmission groups.50 Both percentages were slightly higher than estimates in the general population (where addition of a smoking status identification system increases clinician intervention from 39% to 66% [95% CI=58%, 73%]).29
Reminder systems such as these showed evidence of success in the U.S. 2009–2010 Adult Tobacco Survey, with 67% of U.S. adult LGBT smokers reporting receipt of advice to quit from a physician.51 There was no difference in reported receipt of physician advice to quit or follow-up between LGBT and heterosexual smokers.51
BlueCross BlueShield of Minnesota implemented an LGBT cultural competency training program for quitline coaches47,48 that focused on how to screen for LGBT identity and provide tailored coaching to LGBT people, emphasizing information on disparities, etiology of smoking in LGBT communities, and use of culturally appropriate language. Suggested strategies covered three domains: before the call (understanding barriers), during the call (creating a welcoming environment), and after the call (providing culturally relevant materials, that is, a quit guide tailored to LGBT populations with specific statistics, imagery, and suggestions for dealing with stressors specific to LGBT populations). No impact evaluation was available. Lessons learned included challenges of reluctance to have trainings for individual disparity groups and the need to address staff turnover.47
Community, Policy, and Media Interventions
Six of the seven community interventions were from the gray literature and included media campaigns with formative research,59 community assessments used to inform community media campaigns directly linked to cessation services,52–54,58 and bar-based approaches promoting quitlines.6,55,57 The one peer-reviewed paper examined the impact of increasing cigarette prices.56 Community interventions successfully leveraged earned media coverage (i.e., unpaid media coverage),6,55,59 distribution of public service announcements,58,59 print advertising,52–54,57 and outreach to LGBT organizations.52–54,58 These community interventions included only process evaluations, suggesting successful implementation but only limited evidence of impact. It is of note that a single funder, Legacy (legacyforhealth.org), supported 4 of the 7 community interventions. Only one examination of a policy intervention was identified, and this study examined the impact of French cigarette prices on smoking prevalence in an HIV cohort: for each additional Euro of price the AOR of smoking cessation increased by 10% among the homosexual transmission group, a relationship that was not found for other transmission groups.56
Knowledge, Attitudes, and Behaviors Related to Tobacco Cessation among Lesbian, Gay, Bisexual, and Transgender Populations
LGBT smokers, like heterosexual smokers, generally wish to quit, try to quit, and by far attempt to quit using unassisted or “cold turkey” approaches.18,61,63,64,70,71,76,79,80 Although tobacco use appears to be ranked low on health concerns among LGBT people,71,73 standard theories of health behavior are able to predict quit intentions among LGBT people: Burkhalter and colleagues69 found that constructs from the Theory of Planned Behavior predicted 34% of the variance in intention to quit among LGB smokers. Two studies62,79 noted a positive association between cessation and having friends who did not smoke, suggesting a role for social networks that is also found in the general population.85 Nonetheless, there may be important differences between LGBT and heterosexual smokers. Colorado smokers who are LGBT were less likely to report intent to call the quitline than heterosexual smokers,17 and there were limited and inconsistent findings regarding differences in quit attempt frequency for LGBT versus heterosexual smokers.70,77 LGBT people often reported a desire for LGBT-specific or -friendly interventions in community surveys and focus groups.64,66,72 Swiss focus groups among gay and bisexual men replicated this finding but also suggested little interest in group cessation interventions.18 Using qualitative data, Gruskin et al.20 noted unique stressors for lesbian smokers and suggest that interventions should directly address stigma and focus on social support as well as diffusion of cessation through networks.
Eight studies tested campaign messaging using focus groups and diverse populations: lesbians older than age 40 years in online forums who smoked or had recently quit,60 LGBT youth and service providers in a Midwestern U.S. city,63 San Francisco Bay area women who had quit smoking and relapsed within the prior 3 months,20 Florida LGBT smokers,71 gay or bisexual male smokers in Zurich,18 Atlanta LGBT adults,72 Salt Lake City LGBT young adults,75 and African American MSM smokers in Chicago.78 Focus groups found the following themes as relevant for message development: LGBT smokers were concerned about their health,60,63,78 the cost of tobacco products,63,71,78 the health of loved ones,60,71 addiction,60 and increasingly tobacco-free norms.78 Researchers recommended community-relevant messaging (e.g., “I didn’t survive HIV to die of lung cancer”)75 and, in one focus group, leveraging sex appeal,75 as well as a focus on being supportive, non-judgmental, and genuine.60,71 Messaging highlighting the tobacco industry’s targeting of LGBT communities performed poorly, evoking emotion but not motivation to quit,60 resulting in indifference about targeting,75 and suggesting an appreciation for targeted marketing by the industry.71 Researchers analyzing one focus group were concerned that a focus on tobacco industry malfeasance might drive smokers to brands perceived as more independent (e.g., American Spirit).60
Discussion
The included studies show interventions developed by community leaders, LGBT organizations, and local health departments leveraging community assessment, media, and engagement to deliver needed cessation services. Yet, nearly half of the evidence identified regarding tobacco dependence treatment and smoking cessation among LGBT populations is not in the peer-reviewed literature, and many interventions have very limited reach. Promising LGBT-specific group cessation curricula exist, and their implementation has been shown feasible in LGBT-serving settings. Evidence-based systems to promote assessment of tobacco use and increase counseling by healthcare providers are feasible in LGBT-serving healthcare settings. The available evidence suggests that non-tailored clinical treatments work as well for LGBT and non-LGBT populations. Yet, LGBT-specific barriers may exist to accessing cessation services. Although community interventions have documented disparities, generated substantial media coverage, and promoted cessation services, they remain largely unevaluated. It is unclear if outcomes for cessation groups, media, and policy interventions are moderated by sexual orientation and gender identity.
The existing evidence suggests that the efficacy of non-tailored clinical treatment of tobacco dependence is similar for LGBT and heterosexual populations living in large cities with a substantial LGBT population. However, it is unknown if LGBT smokers are less willing to use non-tailored tobacco treatment programs. It is also unknown if tailored interventions might outperform non-tailored interventions in this population. Group cessation curricula tailored to LGBT communities (e.g., The Last Drag38) show evidence of effectiveness in tobacco cessation. Yet, their reach appears very limited (e.g., in California, less than 0.1% of LGB smokers with a quit attempt in the past year used an LGBT-tailored cessation group).61 Additionally, although LGBT group cessation interventions have been successfully implemented among lesbians, gay men, and across diverse racial/ethnic groups, little research has directly addressed cessation among transgender people. (A best-practice guide to developing LGBT culturally competent tobacco treatment groups is available.86)
Healthcare facilities that serve members of LGBT communities should rigorously implement the Public Health Service Clinical Guidelines29 for tobacco use dependence treatment. LGBT health centers and HIV clinics not implementing these guidelines should explore barriers to successful implementation of these guidelines and engage relevant stakeholders such as LGBT people, community organizations, funders, and healthcare professionals in efforts to overcome barriers and offer effective, life-saving treatments for tobacco use.
As for community, policy, and media interventions, there is little evidence regarding effectiveness for LGBT populations or impacts on reducing disparities. Community interventions should continue to use evidence-based assessment and program planning processes.87 Workplaces and other LGBT community spaces (e.g., LGBT community centers, bars) should implement tobacco-free policies to promote cessation.88 Policies that increase the per-unit cost of tobacco products are highly effective at increasing cessation in the general population,88 show promise for increasing equity in vulnerable populations,23,25 and have limited but promising evidence from one study of HIV-positive French men.56 Efforts to link LGBT health efforts to policies at the local, state, and federal level that increase the cost of tobacco products in LGBT communities are needed (e.g., local bans on price promotions and minimum floor price policies89,90), as are strategies for engaging members of LGBT communities in policy advocacy.
In media interventions, stronger evidence is needed regarding the best messaging strategies to impact cessation efforts. Given the evidence regarding non-targeted media campaigns increasing disparities for vulnerable populations by being more effective for less vulnerable populations,23,25,91 major smoking-cessation media campaigns should include targeted sub-campaigns for LGBT people or risk the potential exacerbation of disparities. Media campaigns for LGBT smokers have emphasized the size and extent of the disparity as motivation to quit; however, Niederdeppe and colleagues24,92 have noted that there is limited yet concerning evidence that emphasizing the extent of a disparity may reduce individuals’ self-efficacy to address the health behavior involved in the disparity. It is not clear that this finding applies for LGBT populations, and if it does, which interventions might be most useful in mitigating this disparity effect. This research should be extended to LGBT populations. In the interim, targeted media campaigns should consider themes of overcoming tobacco addiction instead of emphasizing the normative nature of smoking in LGBT communities.92
The findings of focus group studies suggest that care should be taken with messaging about LGBT targeting by the tobacco industry, a strategy that has been effective in the general population,93 as this may not be effective in motivating quit attempts among LGBT individuals. Future work should also examine communication channels for disseminating cessation messages and policy-related media advocacy, especially where social/friendship networks and media can be leveraged.85
Like heterosexual people, many LGBT smokers desire to and attempt to quit,61,64,70,74,79,80 most often using “cold turkey” approaches.60,64 Evidence on whether LGBT populations are more or less likely to attempt cessation is equivocal.70,77 Some evidence suggests barriers to accessing quitline services for LGBT people.17 It is unclear to what extent LGBT tobacco cessation is influenced by factors that are unique to LGBT people or experienced at greater levels by LGBT people such as stigma, discrimination, and minority stress. Of note, no research has thoroughly investigated correlates of unassisted quitting among LGBT smokers, a topic that has been neglected in the literature generally, despite the fact that most successful quit attempts use this method.94
Limitations
There are important limitations to this study. Gray literature was included, which allows the presentation, often for the first time, of information about community-driven interventions. Yet, this strength of diverse community-based experiences also represents a weakness of the existing literature’s study designs and commitment to community-engaged research. The authors acknowledge a broad range of methodologic quality in the included studies. The process evaluations contained in foundation grant reports offer little direct evidence of efficacy or effectiveness. Many of the studies have very limited generalizability to broader LGBT communities owing to convenience sampling. Additionally, most studies focus on LGBT identity and may not generalize to populations with same-sex sexual behaviors but with heterosexual identity. Only two studies were RCTs, designed for a different purpose. Studies were not excluded based on their quality, in order to provide a broad view of the existing evidence base to inform future research. Inclusion of the gray literature may reduce the influence of publication bias, but it remains unclear to what extent publication bias is present.
Recommendations for Future Research
In sum, the authors recommend that research should examine: (1) direct comparisons of interventions between LGBT and heterosexual smokers to identify if community-desired tailored interventions improve cessation outcomes; (2) diffusion and implementation of existing best practices in LGBT-specific healthcare settings; (3) best strategies for targeted messaging in LGBT media campaigns; (4) determinants of LGBT tobacco use cessation that may be unique to LGBT individuals or experienced at greater levels by LGBT individuals; (5) investigation of within-group differences (e.g., by lesbian versus bisexual and by racial/ethnic LGBT minorities) in cessation behaviors and outcomes; and (6) the impact of policy-based interventions on disparity and LGBT tobacco use cessation. To achieve this, as suggested by the IOM30 regarding LGBT health research in general, it is clear that funding and training programs in LGBT health and LGBT tobacco intervention research are needed.95 Large cessation trials should include measures of sexual orientation and gender identity to examine outcomes for moderation.96
Conclusions
The best available evidence concerning LGBT smoking cessation demonstrates efficacy of group interventions with the least reach. Although these interventions are often desired by LGBT communities and a valuable contribution to a comprehensive cessation strategy, the investment of additional resources to identify and implement efficacious systems-based interventions, targeted media campaigns, and policy interventions is imperative. The available, albeit limited, evidence suggests that evidence-based, non-tailored clinical tobacco treatments29 work as well for LGBT people as for heterosexual people. Investment in the promotion of health and health equity for LGBT communities must turn to implementing these clinical interventions and developing effective, community-informed, and engaged interventions at all levels as well as utilizing population-level policies that promote cessation and health equity.
Supplementary Material
Acknowledgments
Thanks to Mellanye Lackey, MSI, of the University of North Carolina (UNC) Health Sciences Library for her expertise on database searching. Thanks also to all of the kind help identifying gray literature from researchers and advocates and to Legacy for assistance locating lesbian, gay, bisexual, and transgender cessation programs.
JGLL was supported by tuition support from UNC Lineberger Comprehensive Cancer Center, AKM was supported by NIH/National Institute of Drug Abuse funding (grant No. R01DA023935-01A2). CLM was supported in part by the South Carolina Clinical & Translational Research Institute (grant No. UL1 TR000062) and the Hollings Cancer Center’s Cancer Center Support Grant (No. P30 CA138313) at the Medical University of South Carolina.
Footnotes
Example search from PubMed: (homosexuality[MeSH Terms] OR homosexuality[tiab] OR homosexual[tiab] OR gay[tiab] OR LGBT[tiab] OR GLBT[tiab] OR LGB[tiab] OR “sexual minority”[tiab] OR “sexual minorities”[tiab] OR lesbian[tiab] OR bisexuality[MeSH Terms] OR bisexuality[tiab] OR bisexual[tiab] OR transsexualism[MeSH Terms] OR transsexualism[tiab] OR transgender[tiab] OR transsexual[tiab] OR transsexuality[tiab] OR msm[tiab] OR queer[tiab] OR “sexual orientation”[tiab] OR “men who have sex with men”[tiab] OR WSW[tiab] OR “women loving women”[tiab] OR “women who have sex with women”[tiab] OR lesbianism[tiab]) AND (Tobacco Use Disorder[MeSH Terms] OR “Tobacco Use Disorder”[tiab] OR smoking cessation[MeSH Terms] OR cessation[tiab] OR tobacco use cessation products[MeSH Terms] OR tobacco use cessation[MeSH Terms] OR quitline[tiab] OR “quit line”[tiab] OR quitting[tiab] OR quit[tiab] OR “stop smoking”[tiab] OR Smoking/prevention and control[MeSH Terms] OR Smoking/therapy[MeSH Terms] OR “tobacco dependence”[tiab] OR “tobacco treatment”[tiab] OR “smoking decline”[tiab] OR “smoking reduction”[tiab] OR “smoking decrease”[tiab])
No financial disclosures were reported by the authors of this paper.
The funding agencies had no role in the study design; collection, analysis, and interpretation of data; writing; and decision to submit the report for publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lee JG, Griffin GK, Melvin CL. Tobacco use among sexual minorities in the USA, 1987 to May 2007: a systematic review. Tob Control. 2009;18(4):275–282. doi: 10.1136/tc.2008.028241. [DOI] [PubMed] [Google Scholar]
- 2.King BA, Dube SR, Tynan MA. Current tobacco use among adults in the United States: findings from the National Adult Tobacco Survey. Am J Public Health. 2012;102(11):e93–e100. doi: 10.2105/AJPH.2012.301002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hagger-Johnson G, Taibjee R, Semlyen J, et al. Sexual orientation identity in relation to smoking history and alcohol use at age 18/19: cross-sectional associations from the Longitudinal Study of Young People in England (LSYPE) BMJ Open. 2013;3(8):e002810. doi: 10.1136/bmjopen-2013-002810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ortiz-Hernandez L, Tello BL, Valdes J. The association of sexual orientation with self-rated health, and cigarette and alcohol use in Mexican adolescents and youths. Soc Sci Med. 2009;69(1):85–93. doi: 10.1016/j.socscimed.2009.03.028. [DOI] [PubMed] [Google Scholar]
- 5.Blosnich J, Lee JG, Horn K. A systematic review of the aetiology of tobacco disparities for sexual minorities. Tob Control. 2013;22(2):66–73. doi: 10.1136/tobaccocontrol-2011-050181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leibel K, Lee JG, Goldstein AO, Ranney LM. Barring intervention? Lesbian and gay bars as an underutilized venue for tobacco interventions. Nicotine Tob Res. 2011;13(7):507–11. doi: 10.1093/ntr/ntr065. [DOI] [PubMed] [Google Scholar]
- 7.Gruskin E, Byrne K, Kools S, Altschuler A. Consequences of frequenting the lesbian bar. Women Health. 2006;44(2):103–20. doi: 10.1300/j013v44n02_06. [DOI] [PubMed] [Google Scholar]
- 8.Smith EA, Offen N, Malone RE. What makes an ad a cigarette ad? Commercial tobacco imagery in the lesbian, gay, and bisexual press. J Epidemiol Community Health. 2005;59(12):1086–91. doi: 10.1136/jech.2005.038760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith EA, Offen N, Malone RE. Pictures worth a thousand words: noncommercial tobacco content in the lesbian, gay, and bisexual press. J Health Commun. 2006;11(7):635–49. doi: 10.1080/10810730600934492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JG, Agnew-Brune CB, Clapp JA, Blosnich JR. Out smoking on the big screen: tobacco use in LGBT movies. Tob Control. 2000–2011 doi: 10.1136/tobaccocontrol-2013-051288. published ahead of print November 25, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Washington HA. Burning Love: big tobacco takes aim at LGBT youths. Am J Public Health. 2002;92(7):1086–95. doi: 10.2105/ajph.92.7.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stevens P, Carlson LM, Hinman JM. An analysis of tobacco industry marketing to lesbian, gay, bisexual, and transgender (LGBT) populations: strategies for mainstream tobacco control and prevention. Health Promot Pract. 2004;5(3S):129S–134S. doi: 10.1177/1524839904264617. [DOI] [PubMed] [Google Scholar]
- 13.Offen N, Smith EA, Malone RE. From adversary to target market: the ACT-UP boycott of Philip Morris. Tob Control. 2003;12(2):203–7. doi: 10.1136/tc.12.2.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Offen N, Smith EA, Malone RE. Is tobacco a gay issue? Interviews with leaders of the lesbian, gay, bisexual and transgender community. Cult Health Sex. 2008;10(2):143–57. doi: 10.1080/13691050701656284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith EA, Thomson K, Offen N, Malone RE. If you know you exist, it’s just marketing poison”: meanings of tobacco industry targeting in the lesbian, gay, bisexual, and transgender community. Am J Public Health. 2008;98(6):996–1003. doi: 10.2105/AJPH.2007.118174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hatzenbuehler ML, Wieringa NF, Keyes KM. Community-level determinants of tobacco use disparities in lesbian, gay, and bisexual youth: results from a population-based study. Arch Pediatr Adolesc Med. 2011;165(6):527–32. doi: 10.1001/archpediatrics.2011.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burns EK, Deaton EA, Levinson AH. Rates and reasons: disparities in low intentions to use a state smoking cessation quitline. Am J Health Promot. 2011;25(5S):S59–65. doi: 10.4278/ajhp.100611-QUAN-183. [DOI] [PubMed] [Google Scholar]
- 18.Schwappach DL. Queer quit: gay smokers’ perspectives on a culturally specific smoking cessation service. Health Expect. 2009;12(4):383–95. doi: 10.1111/j.1369-7625.2009.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.San Francisco Lesbian and Gay History Project. “She even chewed tobacco”: A pictoral narrative of passing women in America. In: Duberman MB, Vicinus M, Chauncey G, editors. Hidden from history: Reclaiming the gay & lesbian past. New York, NY: New American Library; 1989. [Google Scholar]
- 20.Gruskin EP, Byrne KM, Altschuler A, Dibble SL. Smoking it all away: influences of stress, negative emotions, and stigma on lesbian tobacco use. J LGBT Health Res. 2008;4(4):167–79. doi: 10.1080/15574090903141104. [DOI] [PubMed] [Google Scholar]
- 21.Hatzenbuehler ML, Keyes KM, Hamilton A, Hasin DS. State-level tobacco environments and sexual orientation disparities in tobacco use and dependence in the USA. Tob Control. 2014 doi: 10.1136/tobaccocontrol-2013-051279. published ahead of print on February 25, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frohlich KL, Potvin L. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. Am J Public Health. 2008;98(2):216–21. doi: 10.2105/AJPH.2007.114777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hill S, Amos A, Clifford D, Platt S. Impact of tobacco control interventions on socioeconomic inequalities in smoking: review of the evidence. Tob Control. 2013 doi: 10.1136/tobaccocontrol-2013-051110. published ahead of print on September 17, 2013. [DOI] [PubMed] [Google Scholar]
- 24.Niederdeppe J, Bigman CA, Gonzales AL, Gollust SE. Communication About Health Disparities in the Mass Media. J Commun. 2013;63(1):8–30. [Google Scholar]
- 25.Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health. 2013;67(2):190–3. doi: 10.1136/jech-2012-201257. [DOI] [PubMed] [Google Scholar]
- 26.Greaves L, Johnson J, Bottorff J, et al. What are the effects of tobacco policies on vulnerable populations? A better practices review. Can J Public Health. 2006;97(4):310–5. doi: 10.1007/BF03405610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Main C, Thomas S, Ogilvie D, et al. Population tobacco control interventions and their effects on social inequalities in smoking: placing an equity lens on existing systematic reviews. BMC Public Health. 2008;8:178. doi: 10.1186/1471-2458-8-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Green LW. Making research relevant: if it is an evidence-based practice, where’s the practice-based evidence? Fam Pract. 2008;25 (Suppl 1):i20–4. doi: 10.1093/fampra/cmn055. [DOI] [PubMed] [Google Scholar]
- 29.Fiore MC, Jaen CR, Baker TB. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 30.IOM. The health of lesbian, gay, bisexual, and transgender people: building a foundation for better understanding. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 31.Lee JG, Blosnich JR, Melvin CL. Up in smoke: vanishing evidence of tobacco disparities in the Institute of Medicine’s report on sexual and gender minority health. Am J Public Health. 2012;102(11):2041–3. doi: 10.2105/AJPH.2012.300746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Doolan DM, Froelicher ES. Efficacy of smoking cessation intervention among special populations: review of the literature from 2000 to 2005. Nurs Res. 2006;55(4S):S29–37. doi: 10.1097/00006199-200607001-00005. [DOI] [PubMed] [Google Scholar]
- 33.Network for LGBT Health Equity. MPOWERED: Best and Promising Practices for LGBT Tobacco Prevention and Control. Boston, MA: Fenway Institute; 2012. [Google Scholar]
- 34.Dickersin K, Min YI. Publication bias: the problem that won’t go away. Ann N Y Acad Sci. 1993;703:135–46. doi: 10.1111/j.1749-6632.1993.tb26343.x. [DOI] [PubMed] [Google Scholar]
- 35.Leviton LC, Gutman MA. Overview and rationale for the Systematic Screening and Assessment Method. New Directions for Evaluation. 2010;124:7–31. [Google Scholar]
- 36.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grady ES, Humfleet GL, Delucchi KL, Reus VI, Munoz RF, Hall SM. Smoking cessation outcomes among sexual and gender minority and nonminority smokers in extended smoking treatments. Nic Tob Res. doi: 10.1093/ntr/ntu050. published advance access on April 11, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eliason MJ, Dibble SL, Gordon R, Soliz GB. The last drag: an evaluation of an LGBT-specific smoking intervention. J Homosex. 2012;59(6):864–78. doi: 10.1080/00918369.2012.694770. [DOI] [PubMed] [Google Scholar]
- 39.Harding R, Bensley J, Corrigan N. Targeting smoking cessation to high prevalence communities: outcomes from a pilot intervention for gay men. BMC Public Health. 2004;4:43. doi: 10.1186/1471-2458-4-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miele AM, Scout N, Bradford JB, Perry D. Final Report 3/1/03– 8/31/05. Boston, MA: The Fenway Institute; 2005. Priority Populations Initiative: The LGBT Incubation Project. [Google Scholar]
- 41.Covey LS, Weissman J, LoDuca C, Duan N. A comparison of abstinence outcomes among gay/bisexual and heterosexual male smokers in an intensive, non-tailored smoking cessation study. Nicotine Tob Res. 2009;11(11):1374–7. doi: 10.1093/ntr/ntp137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Warren B. Positively smokefree: Helping HIV+ smokers to quit. Boston, MA: National LGBT Tobacco Control Network; 2010. [Google Scholar]
- 43.Walls NE, Wisneski H. Evaluation of smoking cessation classes for the lesbian, gay, bisexual, and transgender community. J Soc Serv Res. 2011;37(1):99–111. [Google Scholar]
- 44.Matthews AK, Conrad M, Kuhns L, Vargas M, King AC. Project Exhale: preliminary evaluation of a tailored smoking cessation treatment for HIV+ African American smokers. AIDS Patient Care STDS. 2013;27(1):22–32. doi: 10.1089/apc.2012.0253. [DOI] [PubMed] [Google Scholar]
- 45.Matthews AK, Li CC, Kuhns LM, Tasker TB, Cesario JA. Results from a community-based smoking cessation treatment program for LGBT smokers. J Environ Public Health. 2013;2013:984508. doi: 10.1155/2013/984508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dickson-Spillmann M, Sullivan R, Zahno B, Schaub MP. Queer quit: a pilot study of a smoking cessation programme tailored to gay men. BMC Public Health. 2014;14:126. doi: 10.1186/1471-2458-14-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Senseman SE. Making Minnesota’s quitlines accessible to LGBTQ communities: Lessons Learned. [Conference Presentation.] Bridging the Gap: 8th National LGBTQ Health Equity Summit; August 14, 2012; Kansas City, MO. [Google Scholar]
- 48.National LGBT Tobacco Control Network. Making Minnesota’s Quitlines. Accessible to LGBTs. 2008 www.lgbttobacco.org/files/SOL%20V2%20_quitlines.pdf.
- 49.Howard Brown Health Center. Grant reporting document to Respiratory Health Association (of Chicago), personal e-mail communication from Kelly Ducheny on January 7, 2013. Chicago, IL: Author; Mar 5, 2012. Chicago Tobacco Prevention Project (CTPP) Close Out Summary Questions. [Google Scholar]
- 50.Huber M, Ledergerber B, Sauter R, et al. Outcome of smoking cessation counselling of HIV-positive persons by HIV care physicians. HIV Med. 2012;13(7):387–97. doi: 10.1111/j.1468-1293.2011.00984.x. [DOI] [PubMed] [Google Scholar]
- 51.King BA, Dube SR, Babb SD, McAfee TA. Patient-reported recall of smoking cessation interventions from a health professional. Prev Med. 2013;57(5):715–7. doi: 10.1016/j.ypmed.2013.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bronx Lesbian & Gay Health Resource Consortium. Grant reporting document, personal e-mail communication from Robin Scott on January 10, 2013. Bronx, NY: Author; Jul 22, 2003. Priority Populations Initiative: “Queer and Healthy in the Bronx: Smoking Cessation for Lesbians and Their Families”. [Google Scholar]
- 53.Bronx Lesbian & Gay Health Resource Consortium. Grant reporting document to American Legacy Foundation, personal e-mail communication from Robin Scott on January 10, 2013. Bronx, NY: Author; Jun 29, 2006. Priority Populations Initiative Grant: “Queer and Healthy in the Bronx”. [Google Scholar]
- 54.Howard Brown Health Center. Grant reporting document to Amerian Legacy Foundation, personal e-mail communication from William Furmanski on January 8, 2013. Chicago, IL: Author; Mar 1, 2006. Priority Populations Initiative: Queer Tobacco Elimination and Control Collaborative (Q-TECC) [Google Scholar]
- 55.Aragon LM, Le Veque M. The Last Drag Campaign: Countering the tobacco industry’s targeting of the gay and lesbian community. [Conference poster.] Presented at 2006 World Conference on Tobacco or Health; Washington, DC. July 14, 2006; Available from: http://publichealth.lacounty.gov/tob/pdf/Banner-C.6.29.6.pdf. [Google Scholar]
- 56.Peretti-Watel P, Villes V, Duval X, et al. How do HIV-infected smokers react to cigarette price increases? Evidence from the Aproco-Copilote-ANRS CO8. Cohort Curr HIV Res. 2009;7(4):462–467. doi: 10.2174/157016209788680624. [DOI] [PubMed] [Google Scholar]
- 57.Southern Nevada Health District. Grant reporting document to American Legacy Foundation, personal e-mail communication from William Furmanski on January 8, 2013. Las Vegas, NV: Author; Jun 2, 2010. American Legacy Foundation Priority Populations Initiative II Final Report: LGBT Lifestyle Project. [Google Scholar]
- 58.Vincent M. LGBT engagement paradigm: West Virginia case study. [Conference presentation.] LGBT Health Equity Summit; August 14, 2012; Kansas City, MO. [Google Scholar]
- 59.Mautner Project. Grant reporting document to American Legacy Foundation, personal e-mail communication from William Furmanski on January 8, 2013. Washington, DC: Author; Nov 30, 2005. Priority Populations Initiative: Smoking Cessation Media Campaign for Lesbians Over 40. [Google Scholar]
- 60.Shields M, Zapert K, Ackermann S. Witeck-Combs Communications, accessed through Schlesinger Library (collection: MC 683) Radcliffe Institute, Harvard University; 2003. Mautner Project/Witeck-Combs LBT anti-smoking qualitative research summary report. [Google Scholar]
- 61.Bye LL, Gruskin EP, Greenwood G, Albright V, Krotki K. California lesbians, gays, bisexuals, and transgender (LGBT) tobacco use survey - 2004. Sacramento, CA: California Department of Health Services; 2005. [Google Scholar]
- 62.Greenwood GL, Paul JP, Pollack LM, et al. Tobacco use and cessation among a household-based sample of US urban men who have sex with men. Am J Public Health. 2005;95(1):145–51. doi: 10.2105/AJPH.2003.021451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Remafedi G, Carol H. Preventing tobacco use among lesbian, gay, bisexual, and transgender youths. Nicotine Tob Res. 2005;7(2):249–56. doi: 10.1080/14622200500055517. [DOI] [PubMed] [Google Scholar]
- 64.Sanchez JP, Meacher P, Beil R. Cigarette smoking and lesbian and bisexual women in the Bronx. J Community Health. 2005;30(1):23–37. doi: 10.1007/s10900-004-6093-2. [DOI] [PubMed] [Google Scholar]
- 65.Dibble SL, Sato N, Haller E. Asians and native Hawaiian or other Pacific Islanders midlife lesbians’ health. Women and Therapy. 2007;30(3–4):129–43. [Google Scholar]
- 66.Schwappach DL. Smoking behavior, intention to quit, and preferences toward cessation programs among gay men in Zurich, Switzerland. Nic Tob Res. 2008;10(12):1783–7. doi: 10.1080/14622200802443502. [DOI] [PubMed] [Google Scholar]
- 67.Tobacco Program Evaluation Group. Cessation barriers, attitudes and preferences among Colorado GLBT smokers. Denver, CO: University of Colorado Denver; 2008. [Google Scholar]
- 68.Aholt EC. Cognitive processing themes for smoking among lesbians [dissertation] Auburn, AL: Department of Special Education, Rehabilitation and Counseling, Auburn University; 2009. [Google Scholar]
- 69.Burkhalter JE, Warren B, Shuk E, Primavera L, Ostroff JS. Intention to quit smoking among lesbian, gay, bisexual, and transgender smokers. Nicotine Tob Res. 2009;11(11):1312–20. doi: 10.1093/ntr/ntp140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pizacani BA, Rohde K, Bushore C, et al. Smoking-related knowledge, attitudes and behaviors in the lesbian, gay and bisexual community: a population-based study from the U.S. Pacific Northwest. Prev Med. 2009;48(6):555–61. doi: 10.1016/j.ypmed.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 71.Rose J, Adams E. Focus groups with selected priority populations: Evaluation of the Florida Tobacco Prevention and Control Program. Research Triangle Park, NC: RTI International; 2009. [Google Scholar]
- 72.Bryant L, Bowman L, Damarin AK. Assessment for a better understanding of tobacco use by LGBT Atlantans. Respiratory Care Education Annual. 2011;20:63–73. https://www.aarc.org/resources/rcea/rcea11.pdf. [Google Scholar]
- 73.Burkhalter JE, Hay JL, Coups E, Warren B, Li Y, Ostroff JS. Perceived risk for cancer in an urban sexual minority. J Behav Med. 2011;34(3):157–69. doi: 10.1007/s10865-010-9296-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.McElroy JA, Everett KD, Zaniletti I. An examination of smoking behavior and opinions about smoke-free environments in a large sample of sexual and gender minority community members. Nicotine Tob Res. 2011;13(6):440–8. doi: 10.1093/ntr/ntr021. [DOI] [PubMed] [Google Scholar]
- 75.Rescue Social Change Group. Research report to Utah State Department of Health, personal e-mail communication from Jeff Jordan on January 10, 2013. San Diego, CA: Author; 2011. Lesbian, gay, bisexual and transgender young adult tobacco use in Salt Lake City, UT. [Google Scholar]
- 76.Levinson AH, Hood N, Mahajan R, Russ R. Smoking cessation treatment preferences, intentions, and behaviors among a large sample of Colorado gay, lesbian, bisexual, and transgendered smokers. Nicotine Tob Res. 2012;14(8):910–8. doi: 10.1093/ntr/ntr303. [DOI] [PubMed] [Google Scholar]
- 77.Farmer GW, Bowen DJ, Bucholz KK. A population-based comparison of smoking cessation among sexual minority and heterosexual adults. [Conference presentation.] Society for Research on Nicotine & Tobacco Annual Meeting; 2013; Boston, MA. [Google Scholar]
- 78.Matthews AK, Vargas M, Kuhns L, Shappiva N, King A. A qualitative examination of barriers and motivators to smoking cessation among HIV positive African American MSM smokers. Journal of Health Disparities Research and Practice. 2014;7(2):50–76. [Google Scholar]
- 79.Robinson WT, Brown MC, Moody-Thomas S. Smoking and experiences with tobacco cessation among men who have sex with men: New Orleans, 2011. AIDS Behav. 2014;18(Suppl 3):324–32. doi: 10.1007/s10461-013-0585-y. [DOI] [PubMed] [Google Scholar]
- 80.Matthews AK, Hotton A, DuBois S, Fingerhut D, Kuhns LM. Demographic, psychosocial, and contextual correlates of tobacco use in sexual minority women. Res Nurs Health. 2011;34(2):141–52. doi: 10.1002/nur.20427. [DOI] [PubMed] [Google Scholar]
- 81.Berg CJ, Nehl EJ, Wang X, et al. Healthcare provider intervention on smoking and quit attempts among HIV-positive versus HIV-negative MSM smokers in Chengdu, China. AIDS Care. 2014;26(9):1201–7. doi: 10.1080/09540121.2014.892565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Matthews AK, Riley BB, Everett B, Hughes TL, Aranda F, Johnson T. A Longitudinal Study of the Correlates of Persistent Smoking Among Sexual Minority Women. Nic Tob Res. doi: 10.1093/ntr/ntu051. Published advance access on April 11, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.McCullough A, Fisher M, Goldstein AO, Kramer KD, Ripley-Moffitt C. Smoking as a vital sign: prompts to ask and assess increase cessation counseling. J Am Board Fam Med. 2009;22(6):625–632. doi: 10.3122/jabfm.2009.06.080211. [DOI] [PubMed] [Google Scholar]
- 84.Lee JG, Goldstein AO, Ranney LM, Crist J, McCullough A. High tobacco use among lesbian, gay, and bisexual populations in West Virginian bars and community festivals. Int J Environ Res Public Health. 2011;8(7):2758–69. doi: 10.3390/ijerph8072758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358(21):2249–58. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Scout N, Miele AM, Bradford JB, Perry D. Running an LGBT smoking treatment group. Boston, MA: Fenway Institute; 2006. [Google Scholar]
- 87.Runyan CW, Freire KE. Developing interventions when there is little science. In: Doll LS, Bonzo SE, Mercy JA, Sleet DA, editors. Handbook of injury and violence prevention. New York, NY: Springer; 2007. [Google Scholar]
- 88.Task Force on Community Preventive Services. Recommendations regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. Am J Prev Med. 2001;20(2S):10–5. [Google Scholar]
- 89.Tynan MA, Ribisl KM, Loomis BR. Impact of cigarette minimum price laws on the retail price of cigarettes in the USA. Tob Control. 2013;22(e1):e78–85. doi: 10.1136/tobaccocontrol-2012-050554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chapman S, Freeman B. Regulating the tobacco retail environment: beyond reducing sales to minors. Tob Control. 2009;18(6):496–501. doi: 10.1136/tc.2009.031724. [DOI] [PubMed] [Google Scholar]
- 91.Niederdeppe J, Kuang X, Crock B, Skelton A. Media campaigns to promote smoking cessation among socioeconomically disadvantaged populations: what do we know, what do we need to learn, and what should we do now? Soc Sci Med. 2008;67(9):1343–55. doi: 10.1016/j.socscimed.2008.06.037. [DOI] [PubMed] [Google Scholar]
- 92.Nicholson RA, Kreuter MW, Lapka C, et al. Unintended effects of emphasizing disparities in cancer communication to African-Americans. Cancer Epidemiol Biomarkers Prev. 2008;17(11):2946–53. doi: 10.1158/1055-9965.EPI-08-0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Thrasher JF, Niederdeppe J, Farrelly MC, Davis KC, Ribisl KM, Haviland ML. The impact of anti-tobacco industry prevention messages in tobacco producing regions: evidence from the US truth campaign. Tob Control. 2004;13(3):283–8. doi: 10.1136/tc.2003.006403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chapman S, MacKenzie R. The global research neglect of unassisted smoking cessation: causes and consequences. PLoS Med. 2010;7(2):e1000216. doi: 10.1371/journal.pmed.1000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Coulter RW, Kenst KS, Bowen DJ, Scout Research funded by the National Institutes of Health on the health of lesbian, gay, bisexual, and transgender populations. Am J Public Health. 2014;104(2):e105–12. doi: 10.2105/AJPH.2013.301501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Badgett L, Goldberg N. Best practices for asking questions about sexual orientation on surveys. Los Angeles, CA: Williams Institute Sexual Minority Assessment Research Team; 2009. www.law.ucla.edu/williamsinstitute/pdf/SMART_FINAL_Nov09.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.