Introduction
The role that academic medicine has to play in a medical career has been a hotly debated topic over the last two decades. A number of initiatives have been proposed to increase the number of clinical academics, the quality of research undertaken and to preserve research in a NHS driven by service provision.1–3 These initiatives have generated discussion, solved some issues, but left a number of ongoing problems unanswered.
This review evaluates recent changes in academic medicine and describes how they apply to Northern Ireland. It also details the various opportunities for a medical undergraduate or postgraduate to access academic training to explore or enter a career in academic medicine.
In Northern Ireland, academic medicine is linked with Queen's University Belfast, the sole provider of medical education in Northern Ireland. The medical school has four research centres and one teaching and research centre: Centre for Cancer Research and Cell Biology, Centre for Experimental Medicine, Centre for Infection and Immunity and Centre for Public Health and the Centre for Medical Education which is responsible for the administration and management of the undergraduate medical course as well as education research.
What is Academic Medicine?
Most job descriptions for clinical academics include responsibilities for research, teaching and administration in addition to clinical practice. Clinical academics are often expected to have a role in inspiring and training the next generation of clinicians as well as introducing innovations in treatment and practice. Locally, new staff are appointed to a post within one of the five research or teaching centres, however, they are obliged to contribute to the overall needs of the school. These appointments are strategic to enable these centres to meet their research themes, as measured by the Research Excellence Framework, or teaching commitments, as evaluated by the General Medical Council.
The responsibilities of clinical academics evolve over the course of their careers and usually involve all of these roles. The time commitment to these different activities depends on contractual arrangements with academic clinicians having primary contracts in the NHS with honorary academic contracts or in the case of Clinician Scientists, their contract is with their university. Recently, the local preference has been for a person's substantive affiliation to be with the university and then for them to be offered an honorary position with a NHS Trust to undertake clinical work. In view of the crucial role of clinical research in the interface between basic science and clinical practice, clinical academics often make important contributions to the prevention, diagnosis and treatment of disease, teaching of medical students and the training of junior doctors.4
Who are Clinical Academics?
A recent survey of staffing levels of medical clinical academics, in medical schools, identified that approximately 6% of the NHS clinical workforce are involved in clinical academia. The survey showed that there were 3162 (full time equivalent) clinical academics employed in the UK in 34 medical schools. Although this has remained steady over the last few years, the number is still lower than in 2000.5 Since then, General Practice, Ophthalmology and Internal Medicine have seen an increase in clinical academics but all other specialties have seen a decrease, with the greatest reduction being observed in Pathology. In comparison to NHS consultants, medical academics tend to be older, however, there have been recent improvements in gender balance and diversity of ethnicity.5
What has Changed?
In 2005, the Walport report was published by the academic careers sub-committee of Modernising Medical Careers and the UK Clinical Research Collaboration.6 It highlighted three major issues that were barriers to an academic career: lack of a transparent career structure, lack of flexibility in training and a shortage of supported posts when training is completed. Building on the Savill Report7, Walport also noted that a problem for clinical academics splitting their time between NHS and academic responsibilities is that they are judged against the standard of their fulltime peers in both the hospital and university settings. This can be particularly problematic in craft specialties, where it can be a challenge to remain up-to-date, develop new technical skills in procedures or surgery and undertake the appropriate numbers of index operations/procedures as required by their respective specialty associations. They also have to meet high standards of the university with regards to lecturing, community engagement and research.
The Walport report suggested specific solutions to each of these deterrents by recommending the establishment of a distinct career pathway for those keen to pursue a career in clinical academia and increased flexibility allowing individuals to move easily between clinical and academic components. For the first time, it defined the academic pathway as consisting of three increasingly senior levels of post: Academic Clinical Fellowships, Academic Clinical Lectureships and Clinical Senior Lectureships for postgraduates, building on a more formalised undergraduate academic stream (Figure 1).
Fig 1.
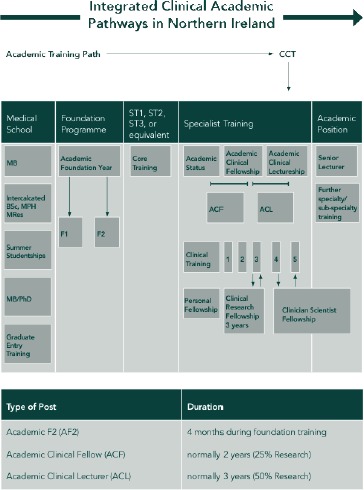
The integrated clinical academic pathway in Northern Ireland.8
Undergraduate Opportunities
A systematic review, in 2006, stated that it was the duty of medical schools to ensure that their students were trained for future advances in clinical care, research and education and that they should aim to stimulate interest in academic medicine.9 However, a recent study, based in Liverpool, found that 75% of undergraduates surveyed felt they had not been given opportunities to learn about academic medicine with 57% of students feeling that a career in academic medicine was less than ‘quite appealing’ for various reasons.4 Many medical schools now offer several opportunities to gain some exposure to an academic career path. A group of medical students at QUB have formed an academic medicine society to promote research and academia to medical and dental undergraduates.10 This society echoes the aims of INSPIRE, an initiative of the Academy of Medical Sciences, which seeks to coordinate current research opportunities and enhance the promotion of clinical academic training throughout the medical school and beyond.
Intercalated Degrees - BSc, MRes, MSc in Public Health
Intercalated degrees allow an extra year of study at the end of 2nd or 3rd year, giving students an opportunity to explore an area of particular interest in greater depth. This year focuses largely on research and provides an opportunity to submit work for publication or to attend scientific meetings. Queen's University Belfast had 60 students, in 2013-14, in one of three programmes:
a Bachelor of Science at the end of 2nd or 3rd year in one of the basic sciences related to clinical training including Anatomy, Physiology, Pharmacology etc.,
a Masters of Research in translational medicine11 which aims to inspire a new generation of innovative clinician scientists with an understanding of disease at a molecular level and a strong training in research methodologies and
a Masters of Science in Public Health, which aims to train the student in research methodology but also provides problem-solving skills to find solutions to practical health problems.12
As these options have become more popular, entry to these programmes has become more competitive. A review of a longstanding Masters' programme in Rheumatology, at another institution, highlighted that these schemes had the potential to maximize learning opportunities, to encourage critical reflection on professional practice, to promote the integration of existing knowledge and experience with new perspectives and develop the application of learning to the workplace.13
If a commitment to an entire year of further study seems too much, students can have a shorter ‘taster’ experience over the summer months through a Summer Studentship. This offers an eight-week exposure to laboratory or educational based research and could potentially be the foundation for a year-long research programme through an intercalated degree. This can be funded by the university or by some local and national charities keen to promote interest in their particular research area.
Recent studies have highlighted that students who undertake an intercalated degree had better examination results and greater success when securing their preferred Foundation posts.14 15 A recent BEME (Best Evidence Medical Education Collaboration) systematic review of the impact of an intercalated BSc on medical student performance and careers found that undertaking an intercalated degree may improve undergraduate performance, increase the likelihood of pursuing an academic career or make the student less likely to follow a career in general practice.16 The extra year increases the financial burden of a medical student's time at university and could create an extra year of debt. The review highlighted that most students felt uninformed about the benefits of undertaking an intercalated degree.16 One of the problems is that the benefits are soft and difficult to measure. At a bare minimum it is a topic to discuss at interview in which the interviewee should be an expert. More often the generic skills learnt can have a significant impact throughout a doctor's career. An attempt to introduce a compulsory intercalated degree at an Australian medical school required modification after it was found that some students lacked the maturity and autonomy required for such a programme.17 However, it is a routine part of the undergraduate medical course at Nottingham University.18
MB/PHD Programme
In some UK universities an MB/PhD programme is offered to a small numbers of students.19 20 This combines the undergraduate medical curriculum with a prolonged period of research working towards the award of a PhD. A recent review of graduates from a longstanding MB/PhD programme found that 79% of them were active in research and 90% had definite plans for further fulltime research.20 They concluded that the scheme was successful at promoting scientific discovery and sustaining academic development.20 However, some would question the optimal time at which to opt out from the undergraduate curriculum to undertake a focused period of research and would also ask whether or not it could result in the loss of recently attained clinical skills and loss of knowledge from the broad sweep of undergraduate medicine.
Academic Foundation Programme - AF2
Included in the proposals from the Walport report was an option for new graduates to undertake an integrated academic foundation programme in their first or second postgraduate years. An academic foundation programme is a four-month research or teaching-intensive placement. It is designed to enable the foundation doctor to gain insights into clinical academic medicine through regular contact with academic clinical supervisors, scientific staff and postgraduate research students. It should allow foundation doctors to develop knowledge, skills and aptitudes for academic medicine and foster an interest in a long-term clinical academic career. A major feature is an opportunity to undertake a teaching or research project under the supervision of a senior academic.8
Recent evaluation of the foundation programme has highlighted that many found academic foundation posts provided good support to junior doctors and offered a wide range of learning opportunities.21 Some, however, felt that the skills learnt were too generic and would have preferred an opportunity to focus their training at this stage.21 The programme acted as a ‘taster’, allowing foundation doctors an opportunity to gain experience through an academic specific option early in their careers rather than having to progress to advanced clinical grades before academic training was a possibility.
Academic Clinical Fellowship – ACF
Academic Clinical Fellowships are targeted at doctors in the early years of specialty training. This is a two-year funded post that attracts an NTN(a) (National Training Number - Academic) and allows an opportunity to develop clinical skills and academic skills concurrently. The ACF is expected to complete ST3+ level training or equivalent with an integrated 25% of time spent in academic research. The aim is to obtain preliminary data to prepare a competitive application for a nationally funded research training fellowship working towards a higher degree. An AF2 post is not viewed as a prerequisite for applying for an ACF post, however, it would be evidence of commitment to an academic career and it may be possible to develop a project undertaken during an AF2 into an academic clinical fellowship application.
An ACF post provides an opportunity to be trained in generic academic skills such as applied research skills, governance, communication and setting specific goals. Importantly, the scheme has a clearly defined entry point and an opportunity to exit academic training on completion of the programme.22 A recent study highlighted that fellows felt that, as well as the opportunity to undertake and develop a research project, the major positive reasons for applying for a fellowship included stimulation, challenge and the opportunity to teach. However, it also highlighted that the negative factors of a fellowship included difficulty obtaining research grants, competing pressures between research, clinical work and teaching, lack of pay parity and concerns about availability of senior posts at the end of the fellowship (Table 1).22
Table 1.
Table highlighting possible positive and negative aspects of the clinical academic pathway
| Positives | Negatives |
|---|---|
| Challenge of research | Lack of role models/mentors |
| Variety in work | Limited availability of senior academic positions |
| Intellectual environment/stimulation | Longer training period |
| Teamwork | Difficulty in obtaining funding |
| Stimulation of teaching | Lack of pay parity |
| Stimulation of supervising research teams | Increased assessment burden due to different roles |
| Recognition by peers | No perfect stage in career at which to do this |
| Travel | Research may not ‘work out’ |
| Award of higher degree | Loss of skills especially in craft specialty |
| Development of critical appraisal skills |
Academic Clinical Lecturers – ACL
Academic Clinical Lectureships are the most senior element of the integrated training pathway. They provide aspiring academic trainees with an opportunity to gain comprehensive research experience by working alongside internationally recognised researchers and clinicians. In England, these schemes are run by the National Institute for Health Research, who funded 122 of these posts in 2013. Similar schemes are run in the devolved nations. They are set up to allow 50% of time to be spent undertaking specialist clinical training and 50% undertaking research or education training. Some question whether this is enough clinical time during the final years of training in craft specialties such as surgery or anaesthetics. Applicants for these posts will be advanced in their specialty training and will have obtained a PhD/MD or equivalent or will be within three months of submission. The trainee is usually at ST3 level or above and will work towards gaining core clinical competencies to finish their training while continuing their academic development at a post-doctoral level to enable them to run an independent research group.
Northern Ireland Clinical Academic Programme
The Northern Ireland Clinical Academic Programme is administered and run by Queen's University Belfast in collaboration with the Northern Ireland Medical and Dental Training Agency (NIMDTA). This enables the scheme to be accountable to NIMDTA for training purposes and quality assurance. The scheme also receives significant support from the Belfast and South Eastern Health and Social Care Trusts. This tripartite integrated model has enabled rapid roll out of clinically relevant research.
Indeed, a recent review by the GMC to find good practice in academic training schemes throughout the UK, highlighted flexibility in the Northern Ireland programme and also the effective integration with the local Trusts and good collaboration between the University, Trusts and NIMDTA.
Considering an Academic Career?
As the Walport report has been implemented, some problems have been highlighted. One criticism of the new system is that doctors have to make decisions regarding their careers earlier than they would have historically. Consequently, some question whether clinicians who develop an academic interest later in their career are able to compete with those who have progressed along an academic career pathway since their Foundation Programme and, as such, may be excluded from the academic career pathway.23
Some further question whether the potential increase in financial burden placed on those who prolong their training through periods spent in research have been addressed adequately, potentially deterring clinicians capable of succeeding in an academic career (Table 1).23
Recent changes to medical school admissions have seen an increase in graduate entry.24 The current academic training pathway may be less attractive to this cohort, with the requirement for further years of training and the resultant increased financial burden. Other models may be needed to attract these highly motivated students into academic medicine.
The relative lack of suitable role models has been highlighted for several years and has been perceived as a key element that needs to be addressed to encourage clinicians to enter and be retained in an academic career.25 The Walport report recognised this and stated that one way to help students to understand the attractions of a career in academic medicine was to make 'sure that medical students are taught by leading clinical academics, among others'.6 This requires teaching to be formally recognised in NHS or university contracts otherwise it may become overshadowed by other commitments as there can be very few opportunities for students to gain exposure to pure researchers.
Different specialties lend themselves more easily to the blend of academic and clinical training. Craft specialties, such as surgery, rely on regular practice to acquire and maintain skills with minimum numbers often being required to ensure competency in index procedures. Studies have already shown a reduction in the amount of time all surgical trainees are able to spend learning surgical techniques following the implementation of Modernising Medical Careers. It has been recognised that, in order to provide adequate training, the reduction in working hours must be offset by implementing measures to maximise the effectiveness of the limited training opportunities, such as simulation. This is an even more acute problem for those electing to undertake an academic training pathway.26–28 The scrutiny of an individual surgeon's surgical outcome has recently increased due to national publication of these results. The Shape of Medical Training Review, chaired by Prof Greenaway (Vice Chancellor of the University of Nottingham), reported in the Autumn 2013.29 It focused on the optimum balance of specialist and generalist training. It reinforced the role of academic training, but emphasised the need for the acquisition and maintenance of generalist skills until a Certificate of Specialist Training is obtained. A smaller number of individuals would then proceed to sub-specialist training after this by credentialling. The implementation of this report will have further implications for academic training.
Strategy for Success
So, what can be done to encourage success in this field? It is vital to ensure that the academic work undertaken by clinical academics addresses questions that are of clinical significance and of personal interest. If the subject is of personal interest and relevant to clinical practice then there will be a greater desire to persevere during difficult times (unsuccessful grant applications; negative studies).
Secondly, an effective mentor is invaluable. The academic pathway, though now much clearer, still has many hurdles along the way. A mentor that can encourage, inspire, challenge and question at just the right time is indispensable in helping someone negotiate the academic training pathway.
Thirdly, cooperation between universities, health trusts and deaneries, as modelled in Northern Ireland, can enable the academic training pathway to operate effectively ensuring smooth transition between stages.
Conclusions
A career in academic medicine can be a very fulfilling one. However, time spent in academic medicine at any point in a medical career can provide an opportunity to learn valuable generic skills, improve clinical practice and provide an opportunity to develop critical thinking. These skills and experiences will be of benefit in career development but most importantly in improving the care of patients.
References
- 1.Goldacre M, Stear S, Richards R, Sidebottom E. Junior doctors' views about careers in academic medicine. Med Educ. 1999;33(5):318–26. doi: 10.1046/j.1365-2923.1999.00404.x. [DOI] [PubMed] [Google Scholar]
- 2.House of Lords Select Committee on Science and Technology. Third report. Paper 12. London: Stationery Office; 1995. Medical research and NHS reforms. [Google Scholar]
- 3.Weatherall DJ. The physician scientist: an endangered but far from extinct species. BMJ. 1991;302(6783):1002–5. doi: 10.1136/bmj.302.6783.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mulla S, Watmough S, Waddelove C. Medical students' views and understanding of a career in academic medicine. Br J Hosp Med. 2012;73(7):401–5. doi: 10.12968/hmed.2012.73.7.401. [DOI] [PubMed] [Google Scholar]
- 5.Fitzpatrick S. London: Medical Schools Council; 2012. A survey of staffing levels of Medical Clinical Academics in UK Medical Schools as at 31 July 2011, a report by the Medical Schools Council. Available online from: www.medschools.ac.uk/Publications/Documents/MSC_ Clinical_Academic_Staff_Survey_310711.pdf Last accessed June 2014. [Google Scholar]
- 6.UK Clinical Research Collaboration. London: Modernising Medical Careers; 2005. Medically- and dentally-qualified academic staff: Recommendations for training the researchers and educators of the future. Available online from: www.nihrtcc.nhs.uk/intetacatrain/copy_of_ Medically_and_Dentally-qualified_Academic_Staff_Report.pdf. Last accessed June 2014. [Google Scholar]
- 7.Savill J. London: The Academy of Medical Sciences; 2000. The tenure-track clinician scientist: a new career pathway to promote recruitment into clinical academic medicine. Available online from www.acmedsci.ac.uk/publications/ Last accessed June 2014. [Google Scholar]
- 8.Carney S. Belfast: Queen's University Belfast; 2013. Investigate further: clinical academic training at Queen's University Belfast in partnership with the Northern Ireland Deanery and the Belfast Health and Social Care Trust. Available online from: www.qub.ac.uk/schools/mdbs/pgd/Filestore/Filetoupload,308130,en.pdf. Last accessed June 2014. [Google Scholar]
- 9.Straus SE, Straus C, Tzanetos K. International Campaign to Revitalise Academic Medicine. Career choice in academic medicine: systematic review. J Gen Intern Med. 2006;21(12):1222–9. doi: 10.1111/j.1525-1497.2006.00599.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quams. org. uk [Internet]. Belfast: QUAMS. Queen's UniversityAcademic Medicine Society; 2012. [updated 2014 Jun 16; cited 2014 Jun 23]. Available online from: www.quams.org.uk. [Google Scholar]
- 11.Queen's University Belfast, School of Medicine, Dentistry and Biomedical Sciences. Belfast: Queen's University Belfast; 2013. Centre for Biomedical Sciences Education, Intercalated degrees. Available online from: www.qub.ac.uk/schools/mdbs/bms/CurrentStudents/IntercalatedDegrees/ Last accessed June 2014. [Google Scholar]
- 12.Queen's University Belfast, School of Medicine, Dentistry and Biomedical Sciences. Belfast: Queen's University Belfast; 2013. Postgraduate and professional development; Masters in Public Health. Available online from: www.qub.ac.uk/schools/mdbs/pgd/PT/MPH/. Last accessed June 2014. [Google Scholar]
- 13.Snaith ML, Adebajo AO. The value ofmasters educational programmes for specialist registrars in rheumatology. Rheumatology. 2003;42(3):481–3. doi: 10.1093/rheumatology/keg147. [DOI] [PubMed] [Google Scholar]
- 14.Mahesan N, Crichton S, Sewell H, Howell S. The effect of an intercalated BSc on subsequent academic performance. BMC Med Educ. 2011;11:76. doi: 10.1186/1472-6920-11-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cleland JA, Milne A, Sinclair H, Lee AJ. An intercalated BSc degree is associated with higher marks in subsequent medical school examinations. BMC Med Educ. 2009;9:24. doi: 10.1186/1472-6920-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones M, Hutt P, Eastwood S, Singh S. Impact of an intercalated BSc on medical student performance and careers: a BEME systematic review: BEME Guide No. 28. Med Teach. 2013;35(10):e1493–510. doi: 10.3109/0142159X.2013.806983. [DOI] [PubMed] [Google Scholar]
- 17.Collins JP, Farish S, McCalman JS, McColl GJ. Amandatory intercalated degree programme: revitalising and enhancing academic and evidence-based medicine. Med Teach. 2010;32(12):e541–6. doi: 10.3109/0142159X.2010.528807. [DOI] [PubMed] [Google Scholar]
- 18.University of Nottingham. Nottingham: University of Nottingham; 2013. Medicine: course curriculum. Available online from: www.nottingham.ac.uk/ugstudy/courses/medicine/medicine.aspx. Last accessed June 2014. [Google Scholar]
- 19.Stewart GW. An MBPhD programme in the UK: the UCL experience. Clin Med. 2012;12(6):526–9. doi: 10.7861/clinmedicine.12-6-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cox TM, Brimicombe J, Wood DF, Peters DK. The Cambridge Bachelor of Medicine (MB)/Doctor of Philosophy (PhD): graduate outcomes of the first MB/PhD programme in the UK. Clin Med. 2012;12(6):530–4. doi: 10.7861/clinmedicine.12-6-530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O'Brien M, Brown J, Ryland I, Shaw N, Chapman T, Gillies R, et al. Exploring the views of second-year Foundation Programme doctors and their educational supervisors during a deanery-wide pilot Foundation Programme. Postgrad Med J. 2006;82(974):813–6. doi: 10.1136/pgmj.2006.049676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldacre MJ, Lambert TW, Goldacre R, Hoang U. Career plans and views of trainees in the Academic Clinical Fellowship Programme in England. Med Teach. 2011;33(11):e637–43. doi: 10.3109/0142159X.2011.610842. [DOI] [PubMed] [Google Scholar]
- 23.Derham C, Vohra RS, Homer-Vanniasinkam S. Academia and MMC: uncomfortable bed-fellows? Surgeon. 2009;7(1):4–5. doi: 10.1016/s1479-666x(09)80058-9. [DOI] [PubMed] [Google Scholar]
- 24.Garrud P. Who applies and who gets admitted to UK graduate entry medicine? – An analysis of UK admission statistics. BMC Med Educ. 2011;11:71. doi: 10.1186/1472-6920-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sambunjak D, Straus SE, Marusic A. Mentoring in academic medicine: a systematic review. JAMA. 2006;296(9):1103–15. doi: 10.1001/jama.296.9.1103. [DOI] [PubMed] [Google Scholar]
- 26.Brennan PA, McCaul JA. Association of Surgeons of Great Britain and Ireland; Association of Surgeons of Training. The future of academic surgery--a consensus conference held at the Royal College of Surgeons of England, 2 September 2005. Br J Oral Maxillofac Surg. 2007;45(6):488–9. doi: 10.1016/j.bjoms.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 27.Mehmood S, Anwar S, Ahmed J, Tayyab M, O'Regan D. A survey of UK surgical trainees and trainers; latest reforms well understood but perceived detrimental to surgical training. Surgeon. 2012;10(1):9–15. doi: 10.1016/j.surge.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 28.Parsons BA, Blencowe NS, Hollowood AD, Grant JR. Surgical training: the impact of changes in curriculum and experience. J Surg Educ. 2011;68(1):44–51. doi: 10.1016/j.jsurg.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Greenaway D. Shape of Training. London: General Medical Council; 2013. Securing the future of excellent patient care: final report of the independent review. Available online from: www.shapeoftraining.co.uk/static/documents/content/Shape_of_training_FINAL_Report.pdf_53977887. pdf Last accessed June 2014. [Google Scholar]


