Abstract
Summary:
Cancer of a male breast represents less than 1% of all breast cancer. As with to female patients, mastectomy in men creates a substantial emotional burden. Breast reconstruction may improve the patient’s psychological well-being, compliance with adjuvant treatments, and overall outcome. However, due to the unique anatomy of the male breast, standard reconstructive strategies using anatomic or prosthetic modalities are not entirely applicable. We describe a case of a 68-year-old male patient who underwent successful unilateral breast reconstruction solely with fat grafting technique.
It is estimated that in 2014, about 2360 new breast cancer cases causing 430 deaths will have been diagnosed among men in the United States.1,2 The diagnosis of breast cancer creates a considerable psychological burden and reduces the quality of life.3,4 Major depressive disorder is a frequent but often unrecognized and untreated condition among breast cancer patients, which causes amplification of physical symptoms, additive functional impairment, and poor adherence to treatment regimens.3,4 The primary standard treatment in male breast cancer consists of a modified radical mastectomy with axillary node sampling and/or dissection, which leaves an asymmetrical chest.1,2,5 Because breast reconstruction reduces the disfigurement, it is appropriate to also consider restoration of the breast in the male patient. However, standard autologous and/or prosthetic reconstructive approaches may not be adequate to recreate the unique shape and symmetry of the male chest wall. We present a case of a 68-year-old psychologist and body builder who underwent a successful unilateral breast reconstruction with fat grafting.
CASE REPORT
A 68-year-old male patient was diagnosed with a 1 × 2 cm subareolar ER/PR positive and estrogen receptor (ER)/progesterone receptor (PR) positive and human epidermal growth factor receptor 2 (HER2/neu) negative invasive ductal carcinoma. There was no skin involvement or nipple discharge. The initial excisional biopsy was coupled with a sentinel lymph node biopsy, which was negative for metastases. The patient was then offered a completion mastectomy. Due to the patient’s considerable concerns about chest wall appearance after mastectomy, immediate staged breast reconstruction with fat grafting was offered. Surgical interventions were carried out approximately 5 months apart.
Staged Surgical Approach
Initially, 70 ml of fat graft from the abdomen was deposited in strands under the preserved fascia of the left pectoralis major muscle (Fig. 1). The fat graft was acquired and processed according to Coleman’s method including manual fat harvesting and centrifugation.6 The mastectomy wound was closed in standard fashion over a drain. After 5 months (Fig. 2), additional 141 ml of fat graft was injected into the tissues of the left chest wall defect. The last stage carried out after subsequent 5 months and consisted of liposuction of 70 ml of excessive tissues from the left breast and transfer of 20 ml of fat graft into a residual contour defect. During the last stage, nipple reconstruction using a modified skate flap and skin graft from the patient’s groin was performed.
Fig. 1.
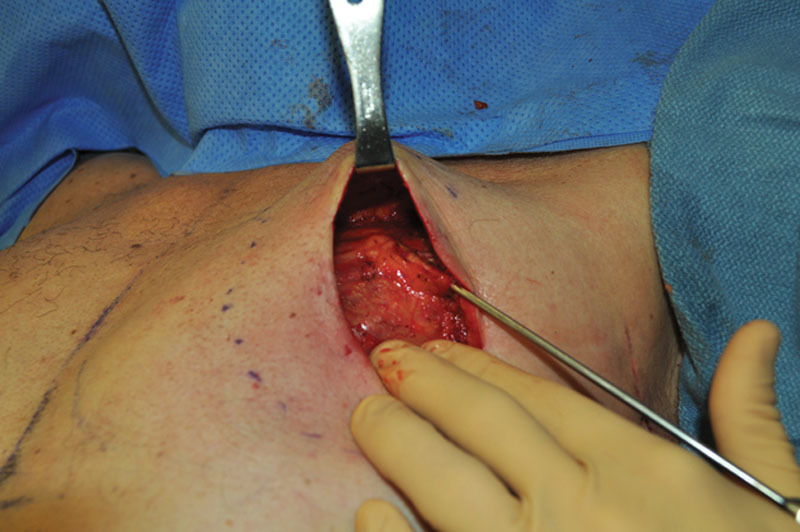
Intraoperative view of fat deposition under the fascia of the pectoralis major muscle immediately following mastectomy.
Fig. 2.

The appearance of the patient’s chest 5 months after mastectomy and 70 ml of fat graft.
Follow-up
The patient’s recovery after each procedure was uneventful. The reconstructed breast mound remained entirely soft without palpable nodules suggestive of fat necrosis. The reconstructed nipple, however, developed partial necrosis but did not require revision. At 6-month follow-up, the patient was very satisfied with his reconstructed breast, which became his preferred side (Fig. 3).
Fig. 3.

The final result 6 months after the last fat grafting session.
DISCUSSION
Treatment of breast cancer is emotionally and physically disabling regardless of sex.3,4 Moreover, impaired physical activity and emotional dysfunction associated with breast cancer negatively affect patient survival.7 On the other hand, breast reconstruction after mastectomy has been shown to reduce cancer-specific death.8 Although methods of reconstruction after mastectomy in women are well described, postmastectomy deformity of the male chest has not received sufficient attention. The likely explanation of this fact is the relative rarity of male breast cancer and different societal roles and expectations. In our patient, we achieved total breast reconstruction with 3 sessions of liposculpting, yielding a satisfactory outcome.
Fat grafting is a straightforward technique associated with low complications and minimal donor site morbidity compared with other techniques.9,10 It allows the surgeon to customize the surgical approach to address the distinctive defect of the male chest. Due to low volume demands, reconstruction of the male breast intuitively may require small graft volumes and fewer operative sessions. In addition, fat represents a filling material with ideal properties—it is cheap, biocompatible, and lacks toxicity. It can provide a natural feel and great cosmesis, and, if needed, can be easily removed.11–13
Fat grafting is not free of challenges because the “behavior” of transplanted fat is not entirely understood. Fat graft take varies greatly, frequently requiring several procedures.11,13–16 Moreover, the amount of fat transferred in 1 session is limited as overfilling results in fat necrosis leading to cyst formation and possible infection.17 Other potential complications of fat grating include necrotic lumps and calcifications thought to obscure cancer surveillance.11,13,18 However, Parikh et al19 conducted a retrospective analysis of 286 breast cancer patients reconstructed with fat grafting who underwent imaging of a palpable lesions and found that the negative predictive value for malignancy of avascular lesions with circumscribed margins (characterizing fat necrosis) was 100%. Additionally, the authors provided a detailed imaging classification of radiographic features distinguishing benign and malignant lesions.19 Similarly, the American Society of Plastic Surgeons Fat Graft Task Force recognized high reliability of imaging in ruling out malignant findings but also recommended biopsy in cases of uncertainty.14,16
The potential of fat grafting to the breast coinciding with cancer has been examined in the literature. In a study of 1112 breasts in 866 breast cancer patients reconstructed immediately with tissue expander and fat graft, there were no cases of local recurrence after over a 40-month follow-up.20 Similarly, in another series of 880 patients who underwent breast lipomodeling, there were no instances of cancer after 10-year follow-up.21 Although relationship between local cancer recurrence and fat graft is rare,20,22 the possibility for transferred adipocytes and particularly adipose-derived stem cells to cause malignant transformation has been investigated.23,24 The available data suggest that the critical factor determining whether regeneration therapy (eg, adipose-derived stem cells) enhances tumor growth is the condition of the remaining tumor: active disease is promoted, whereas dormant tumor is insensitive.23 Clearly, caution should be exercised when applying fat cells into a prior tumor bed.23,24
In conclusion, even though the behavior of transferred fat is not well understood, fat grafting is a very powerful reconstructive modality to recreate the unique shape of the male breast after mastectomy.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.American Cancer Society. Cancer Facts and Figures 2014. Available at: http://www.cancer.org/acs/groups/content/@research/documents/webcontent/acspc-042151.pdf. Accessed September 2, 2014.
- 2.Giordano SH, Buzdar AU, Hortobagyi GN. Breast cancer in men. Ann Intern Med. 2002;137:678–687. doi: 10.7326/0003-4819-137-8-200210150-00013. [DOI] [PubMed] [Google Scholar]
- 3.Strittmatter HJ, Neises M, Blecken SR. Criteria of life quality after reconstructive breast cancer surgery [article in German]. Zentralbl Gynakol. 2006;128:217. doi: 10.1055/s-2005-836887. [DOI] [PubMed] [Google Scholar]
- 4.Fann JR, Thomas-Rich AM, Katon WJ, et al. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry. 2008;30:112–126. doi: 10.1016/j.genhosppsych.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Kinne DW. Management of male breast cancer. Oncology (Williston Park) 1991;5:45–47. [PubMed] [Google Scholar]
- 6.Coleman SR. Structural Fat Grafting. St. Louis, Mo.: Quality Medical; 2004. pp. 30–175. [Google Scholar]
- 7.Quinten C, Martinelli F, Coens C, et al. Patient Reported Outcomes and Behavioral Evidence (PROBE) and the European Organization for Research and Treatment of Cancer (EORTC) Clinical Groups. A global analysis of multitrial data investigating quality of life and symptoms as prognostic factors for survival in different tumor sites. Cancer. 2014;120:302–311. doi: 10.1002/cncr.28382. [DOI] [PubMed] [Google Scholar]
- 8.Hsieh TY, Lin YN, Lin SD, et al. Immediate transverse rectus abdominis musculocutaneous flap reconstruction is associated with improved cancer-specific survival in locally advanced breast cancer. Ann Plast Surg. 2014;73(Suppl 1):S31–S36. doi: 10.1097/SAP.0000000000000251. [DOI] [PubMed] [Google Scholar]
- 9.de Blacam C, Momoh AO, Colakoglu S, et al. Evaluation of clinical outcomes and aesthetic results after autologous fat grafting for contour deformities of the reconstructed breast. Plast Reconstr Surg. 2011;128:411e–418e. doi: 10.1097/PRS.0b013e31822b669f. [DOI] [PubMed] [Google Scholar]
- 10.Losken A, Pinell XA, Sikoro K, et al. Autologous fat grafting in secondary breast reconstruction. Ann Plast Surg. 2011;66:518–522. doi: 10.1097/SAP.0b013e3181fe9334. [DOI] [PubMed] [Google Scholar]
- 11.Bucky LP, Percec I. The science of autologous fat grafting: views on current and future approaches to neoadipogenesis. Aesthet Surg J. 2008;28:313–321; quiz 322. doi: 10.1016/j.asj.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 12.Coleman SR, Saboeiro AP. Fat grafting to the breast revisited: safety and efficacy. Plast Reconstr Surg. 2007;119:775–785; discussion 786. doi: 10.1097/01.prs.0000252001.59162.c9. [DOI] [PubMed] [Google Scholar]
- 13.Delay E, Garson S, Tousson G, et al. Fat injection to the breast: technique, results, and indications based on 880 procedures over 10 years. Aesthet Surg J. 2009;29:360. doi: 10.1016/j.asj.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 14.American Society of Plastic Surgeons. 2012 Post-Mastectomy Fat Graft/Fat Transfer/ASPS Guiding Principles. Available at: http://www.plasticsurgery.org/Documents/medical-professionals/health-policy/guiding-principles/2012Post-MastectomyFatGraft-FatTransferASPSGuidingPrinciples.pdf. Accessed September 2, 2014.
- 15.Hyakusoku H, Ogawa R, Ono S, et al. Complications after autologous fat injection to the breast. Plast Reconstr Surg. 2009;123:360–370; discussion 371. doi: 10.1097/PRS.0b013e31819347ba. [DOI] [PubMed] [Google Scholar]
- 16.Gutowski KA ASPS Fat Graft Task Force. Current applications and safety of autologous fat grafts: a report of the ASPS fat graft task force. Plast Reconstr Surg. 2009;124:272–280. doi: 10.1097/PRS.0b013e3181a09506. [DOI] [PubMed] [Google Scholar]
- 17.Khouri RK, Rigotti G, Cardoso E, et al. Megavolume autologous fat transfer: part I. Theory and principles. Plast Reconstr Surg. 2014;133:550. doi: 10.1097/01.prs.0000438044.06387.2a. [DOI] [PubMed] [Google Scholar]
- 18.Missana MC, Laurent I, Barreau L, et al. Autologous fat transfer in reconstructive breast surgery: indications, technique and results. Eur J Surg Oncol. 2007;33:685–690. doi: 10.1016/j.ejso.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Parikh RP, Doren EL, Mooney B, et al. Differentiating fat necrosis from recurrent malignancy in fat-grafted breasts: an imaging classification system to guide management. Plast Reconstr Surg. 2012;130:761–772. doi: 10.1097/PRS.0b013e318262f03b. [DOI] [PubMed] [Google Scholar]
- 20.Seth AK, Hirsch EM, Kim JY, et al. Long-term outcomes following fat grafting in prosthetic breast reconstruction: a comparative analysis. Plast Reconstr Surg. 2012;130:984. doi: 10.1097/PRS.0b013e318267d34d. [DOI] [PubMed] [Google Scholar]
- 21.Delay E, Garson S, Tousson G, et al. Fat injection to the breast: technique, results, and indications based on 880 procedures over 10 years. Aesthet Surg J. 2009;29:360–376. doi: 10.1016/j.asj.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 22.Brenelli F, Rietjens M, De Lorenzi F, et al. Oncological safety of autologous fat grafting after breast conservative treatment: a prospective evaluation. Breast J. 2014;20:159–165. doi: 10.1111/tbj.12225. [DOI] [PubMed] [Google Scholar]
- 23.Donnenberg VS, Zimmerlin L, Rubin JP, et al. Regenerative therapy after cancer: what are the risks? Tissue Eng Part B Rev. 2010;16:567–575. doi: 10.1089/ten.teb.2010.0352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rowan BG, Gimble JM, Sheng M, et al. Human adipose tissue-derived stromal/stem cells promote migration and early metastasis of triple negative breast cancer xenografts. PLoS One. 2014;9:e89595. doi: 10.1371/journal.pone.0089595. [DOI] [PMC free article] [PubMed] [Google Scholar]


