Abstract
Aims
To investigate the utility of the body adiposity index (BAI) and its association with the metabolic syndrome (MetS) in older Caucasian (n=369), African-American (n=336) and Filipina (n=275) women.
Methods
Dual energy x-ray absorptiometry, anthropometric measures, plasma glucose and medical history were assessed in 1993-1999.
Results
Despite smaller body size, 32.7% of Filipina women had higher MetS compared to African-American and Caucasian women based on the National Cholesterol Education Program (NCEP) (32.7% vs 19.6% and 13.3%, respectively) or the International Diabetes Federation (IDF) (42.6% vs. 33.0% and 18.7%, respectively ps<0.05). BAI had higher positive correlations with BMI, %body fat (%BF), and %truncal fat in Caucasian than African-American and Filipina women. Adjusted for age, smoking, estrogen use, exercise, and alcohol intake, odds of the MetS (NCEP) were 2.08 (95%CI:1.52-2.85) by BAI, 3.04 (95%CI:2.11-4.38) by BMI, and 2.13 (95%CI:1.52-3.00) by %BF for Caucasian women; 0.92 (95%CI:0.69-1.23) by BAI, 1.44(95%CI:1.09-1.90) by BMI, and 1.12(95%CI:0.84-1.50) by %BF for African-American women; and 1.14 (95%CI:0.88-1.47) by BAI, 1.51 (95%CI:1.15-1.97) by BMI, and 0.96 (95%CI:0.74-1.25) by %BF for Filipinas.
Conclusion
BAI was better able to assess adiposity in postmenopausal Caucasian women compared to African-American and Filipina women. This index can distinguish ethnic differences in MetS confirmed by %BF.
Keywords: BAI, Metabolic Syndrome, Ethnic Differences, Adiposity, Postmenopausal Women
INTRODUCTION
Obesity or accumulated adiposity is an important etiological factor in the clustering of clinical conditions that comprise the metabolic syndrome (MetS) [1]. These conditions include central obesity, hypertension, hyperglycemia, and dyslipidemia [2,3]. Having the MetS in turn, predisposes individuals for more serious chronic clinical outcomes, such as cardiovascular disease (CVD), type 2 diabetes, and possibly some cancers [2,4].
Although, high precision imaging techniques, including computed tomography (CT) or dual-energy x-ray absorptiometry (DXA) imaging, are considered to be the gold standard for measuring fat distribution, their clinical value is often undermined by the cost and time burden associated with CT or DXA. Therefore, other markers including weight, waist circumference, skinfold patterns, BMI and waist-hip ratio are used as convenient and economical clinical proxies to evaluate adiposity [5,6]. While anthropometric thresholds provide a general assessment of risk, they may not provide a valid basis for comparisons between ethnic groups, and ethnic specific thresholds must be considered [7–9].
Previous reports have shown the importance of considering ethnic differences in fat distribution when assessing adiposity using BMI [10,11]. Persons from different ethnic groups with similar BMIs can be at dissimilar risks for poor health outcomes attributable to increased adiposity. For example, several studies suggest that despite similar BMI, Indians, Asians, and Filipina women living in the US have higher visceral adipose tissue compared to Caucasians. while African American women have less visceral adipose tissue despite significantly larger BMI [12,13]. Also, variations of body fat do not correlate with BMI variations in Mexican American, non-Hispanic White, and non-Hispanic Black adolescents [14].
A recent analysis by Bergman and colleagues, reported that the body adiposity index (BAI) based on hip circumference and height, was highly correlated with DXA measures of body fat in relatively young African American and Mexican American men and women (average age 35 years) [15]. The applicability of this index has been studied in various populations such as middle-aged and elderly Caucasian adults, post-menopausal Caucasian women, multi-ethnic cohorts predominantly Caucasian or African-American, and Chinese adults, however the conclusions drawn have been inconsistent [16–21]. However, there have been no studies comparing BAI and its association with the MetS in older women of Caucasian, African American, and Filipino ethnicities.
The purpose of this study is to examine the association of BAI with other adiposity markers in Caucasian, African American, and Filipina women aged 50-70 years and to investigate the utility of BAI as a risk factor for the MetS in community dwelling women of these ethnicities.
METHODS
Study population
Caucasian women in this study were members of the Rancho Bernardo Cohort who were initially enrolled in a community-based longitudinal study between 1972-1974 [22]. In 1997-99, all surviving members of the original cohort were invited to participate in a research clinic visit focused on diabetes and its risk factors; approximately 70% of the locally residing, non-institutionalized cohort attended this visit. African-American and Filipina women were enrolled as ethnic comparison groups to the Rancho Bernardo Study, using the same research protocol. African American women were participants in the Health Assessment Study of African American Women, a longitudinal study, and had been recruited between 1993-1997 [23]. Filipina women were recruited between 1995 and 1999 for the longitudinal UCSD Filipino Women's Health Study [24]. All women were residents of San Diego, California. Efforts were made to recruit African American and Filipina women of a socio-economic status similar to the Caucasian women of the Rancho Bernardo Study.
Only women aged 50-70 years at the time of their visit (n=1043) were considered for this analysis in order to obtain three ethnic cohorts of comparable age. After excluding those missing weight, height, hip, waist, and any DXA measures (n=64), the final study sample consisted of 369 Caucasian, 336 African American, and 275 Filipina women. The University of California, San Diego Human Research Protection Program approved this study; all participants gave written informed consent prior to participation.
Clinical Measures
Self-administered standardized questionnaires were used to assess demographic characteristics and lifestyle (physical activity, cigarette smoking, and alcohol use). Physical activity was assessed by asking participants if they engaged in exercise or labor for thirty minutes at least three times per week. Cigarette smoking history (current/past/never) and alcohol use (consumption of 3 or more drinks per week) were also assessed in each cohort. Previous physician diagnoses of diseases were obtained by a nurse during a structured interview. Use of prescription and over-the-counter medications during the prior month was validated by a nurse using containers and pills brought to the clinic for that purpose.
Height and weight were measured using a stadiometer and a balance beam scale respectively, and used to calculate body mass index (BMI; weight in kg divided by height in meters squared). Waist girth was measured at the minimum point between the last rib and the iliac crest with a tape measure. If the minimum waist circumference was at the iliac crest because of excessive central obesity, waist girth was measured at the umbilicus. Hip circumference was measured at the largest point of the greater trochanter area.
A nurse specially trained in the Hypertension Detection Follow-up Protocol (HDFP) measured blood pressure twice using a mercury sphygmanometer after the participant had been seated quietly for 5 minutes [25]. Blood was obtained via venipuncture after a requested minimum 8-12 hour fast. A 75g oral glucose tolerance test was administered and venous blood collected 2 hours post challenge. Fasting and post-challenge plasma glucose were measured using a glucose oxidase assay. Total cholesterol and triglycerides were measured with a biochromatic analyzer (ABA-200, Abbott Laboratories, Irving, TX. High-density-lipoprotein (HDL) and low-density-lipoprotein (LDL) were obtained according to the standard blood/lipid panel in a clinical research laboratory.
Percent total body fat content, right and left leg percent fat, and truncal percent fat were measured using dual-energy x-ray absorptiometry (model QDR-2000 X-ray bone densitometer, Hologic Inc Waltham, MA). Daily calibration was performed using a standard phantom provided by the manufacturer. Precision errors for the DXA measures used here were approximately 1.2% or less.
Statistical Analysis
BAI was calculated using formula developed by Bergman et al. where BAI=(hip circumference/height1.5) -18 [15]. High blood pressure was defined as systolic blood pressure ≥130 mm Hg, diastolic blood pressure ≥85 mmHg, or use of antihypertensive medication.
The MetS was defined using the National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III) and International Diabetes Federation (IDF) definitions [3]. According to the NCEP-ATP III definition, participants were classified as having the MetS if they had any three of the following conditions: Waist circumference >88cm, triglycerides ≥150 mg/dl, HDL cholesterol level <50 mg/dl, fasting plasma glucose ≥110 mg/dl, blood pressure >135/85 mmHg or physician diagnosed hypertension. Based on the IDF definition, participants were classified as having the MetS, if they had a waist circumference ≥80 cm and 2 of any of the following conditions: triglycerides ≥150 mg/dl, HDL cholesterol level <50 mg/dl, fasting plasma glucose ≥100 mg/dl, blood pressure >135/85 mmHg or physician diagnosed hypertension.Based on 1999 WHO criteria, Type 2 diabetes was defined as fasting plasma glucose ≥126 mg/dl or 2-hour post challenge glucose level ≥200 mg or a verified history of physician diagnosed type-2 diabetes, or reported use of insulin or oral hypoglycemic medication in the past 2 weeks.
Age-adjusted means and multiple comparisons across ethnic groups using the Caucasian women as the reference group were computed using general linear models with Tukey's test for continuous variables, χ2 tests were performed for categorical variables. Variables not normally distributed (total cholesterol, LDL, HDL, and triglycerides) were log-transformed for analysis. Pearson correlations were computed as well as Fisher's z transformation on these coefficients for comparisons across cohorts. Multivariable logistic regression models were used to assess the association between BAI, BMI, and %BF separately with the odds of having the MetS after adjusting for age, current cigarette smoking, current estrogen use, alcohol use, and physical activity. Amount of increase for each risk factor was standardized across cohorts by using a one standard deviation specific to each cohort as the measure of unit increase. All data analyses were performed using SAS version 9.2 (SAS Inc, Cary, NC); all tests were two-tailed with statistical significance defined as p<0.05.
RESULTS
After adjustment for age, there were significant weight, waist circumference, and hip girth differences across all three ethnicities (see Table 1). Mean %BF, BAI and BMI were similar across Caucasian and Filipina women. However, African American women had significantly higher levels of truncal fat, leg fat, %BF, BAI and BMI but significantly lower triglycerides and total cholesterol than women in the other two ethnic groups. African American and Filipina women had similar mean systolic blood pressures that were significantly higher than those in Caucasian women. Larger proportions of Filipina women had diabetes (36.4%) and hypertension (67.3%) compared to Caucasian women (8.4% and 47% respectively). Regardless of definition, Filipinas had the highest prevalence of the MetS followed by African Americans. More Caucasian women drank 3 or more alcoholic drinks per week and were current estrogen users compared to African American and Filipina women (see Table 1). Caucasian women had similar levels of physical activity compared to Filipina women but more physical activity than African American women.
Table 1.
Age, Age-adjusted Means and rates for characteristics in Caucasian, African American, and Filipina Participants
| Characteristics | Caucasian | African American | Filipina |
|---|---|---|---|
| N | 368 | 336 | 275 |
| Age (years) | 60.8 | 59.2a | 60.1 |
| Anthropometric Measures | |||
| Height (m) | 1.63 | 1.63b | 1.53 |
| Weight (kg) | 66.9 | 78.6ab | 59.8a |
| Waist circumference (cm) | 79.2 | 88.2ab | 81.4a |
| Hip girth (cm) | 102.5 | 107.1ab | 97.1a |
| Waist:hip ratio | 0.77 | 0.82ab | 0.84a |
| Body fat (%) | 34.1 | 37.6ab | 33.4 |
| Truncal fat (%) | 29.7 | 33.8ab | 31.4a |
| Right leg fat (%) | 41.4 | 43.5ab | 37.3a |
| Left leg fat (%) | 41.2 | 43.6ab | 37.1a |
| BAI (%) | 31.4 | 33.8ab | 33.3 |
| BMI (kg/m2) | 25.2 | 29.7ab | 25.5 |
| Clinical Measures | |||
| Systolic Blood Pressure (mmHg) | 125.4 | 136.9a | 135.8a |
| Diastolic blood pressure (mmHg) | 76.6 | 78.0b | 79.9a |
| Triglycerides (mg/dl) | 124.8 | 95.16ab | 161.5a |
| LDL cholesterol (mg/dl) | 129.4 | 128.3b | 136.1a |
| HDL cholesterol (mg/dl) | 64.3 | 61.8ab | 53.2a |
| Total cholesterol (mg/dl) | 218.6 | 209.4ab | 222.8 |
| Fasting plasma glucose (mg/dl) | 93.4 | 99.8ab | 110.7a |
| Behaviors | |||
| Alcohol intake (3+drink/week) (%) | 40.2 | 12.1ab | 0.7a |
| Physical Activity (3 times per week) (%) | 67.1 | 58.3a | 62.9 |
| Current Smoker (%) | 12.6 | 12.1b | 6.2a |
| Currently taking estrogen (%) | 59.0 | 42.3ab | 19.3a |
| Comorbidities | |||
| Hypertension (%) | 47.0 | 72.9a | 67.3a |
| MetS (NCEP)(%) | 13.3 | 19.6ab | 32.7a |
| MetS (IDF)(%) | 18.7 | 33.0ab | 42.6a |
| Diabetes (%) | 8.4 | 15.2ab | 36.4a |
p-value <0.05 with Caucasian as the Reference Group
p-value <0.05 between African American and Filipina
Pearson correlations of BAI and BMI with each adiposity measure are shown in Table 2. BAI had significantly higher correlations with other adiposity measures (BMI, weight, %BF, and percent truncal fat) in Caucasians, compared to African-Americans and Filipinas. BAI had the highest correlations with BMI in all groups, followed by %BF among Caucasians, right leg fat in African Americans and truncal fat among Filipinas. Correlations between BMI and %BF were similar in Caucasian and African American women, but significantly lower in Filipina women. The correlations coefficients between BMI and %BF had higher values compared to those between BAI and %BF. As shown in Table 2, correlations between BMI and other adiposity measures were consistent across ethnic groups whereas correlations between BAI and other adiposity measures were stronger for the Caucasian group but less consistent across the other ethnic groups.
Table 2.
Pearson Correlation Coefficients between BAI, BMI, and Other Adiposity Markers
| BAI | BMI | |||||
|---|---|---|---|---|---|---|
| Caucasian | African American | Filipina | Caucasian | African American | Filipina | |
| BMI | 0.876* | 0.786*a | 0.797*a | – | – | – |
| Weight | 0.641* | 0.592* | 0.473*a | – | – | – |
| Height | – | – | – | – | – | – |
| Hip circumference | – | – | – | 0.881* | 0.793*ab | 0.854* |
| Waist circumference | 0.638* | 0.507*a | 0.587* | 0.837* | 0.847* | 0.840* |
| Waist:hip ratio | 0.186* | −0.115*ab | 0.170* | 0.421* | 0.336* | 0.423* |
| Body fat | 0.818* | 0.750*a | 0.695*a | 0.831* | 0.819*b | 0.690*a |
| Truncal fat | 0.805* | 0.700*a | 0.708*a | 0.856* | 0.834*b | 0.732*a |
| Right leg fat | 0.678* | 0.753*b | 0.476*a | 0.607* | 0.673*b | 0.393*a |
| Left leg fat | 0.700* | 0.728*b | 0.462*a | 0.622* | 0.668*b | 0.371*a |
Correlation coefficient statistically significant (p<0.05)
Statistically different correlation coefficients with Caucasian as the Reference Group
Statistically different correlation coefficients between African American and Filipina groups
Correlations not obtained for measures used to calculate BAI and BMI
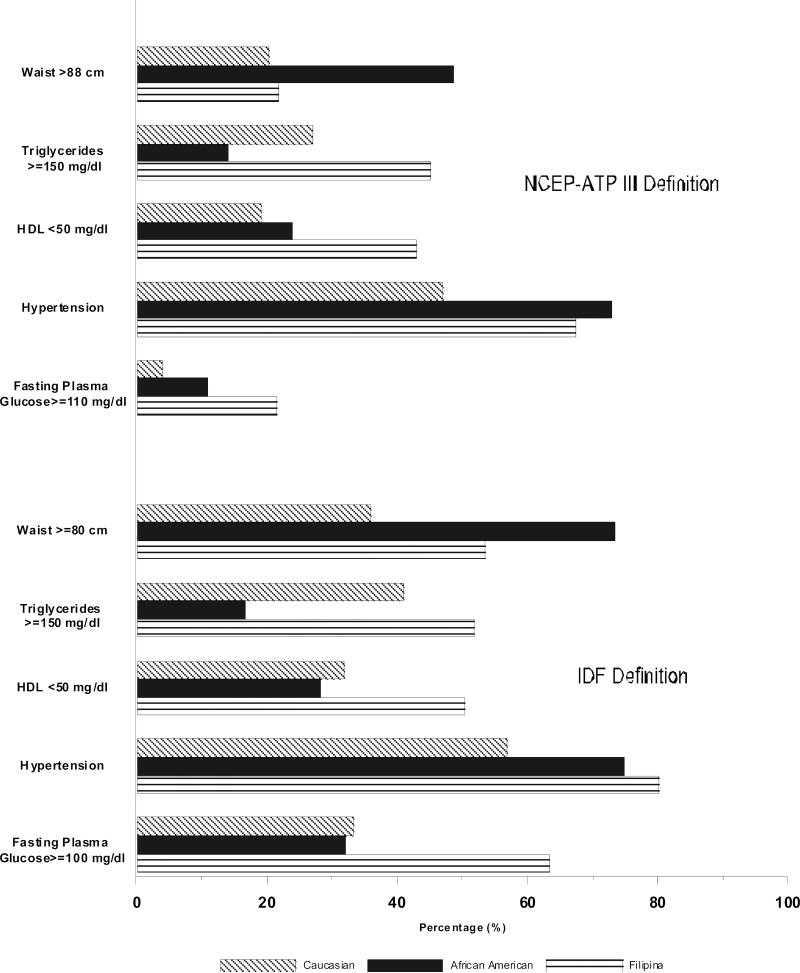
Ethnic differences were observed in the components of the MetS (Figure 1). Using the NCEP definition the three most common factors in Caucasians and Filipina were high triglycerides, low HDL, and hypertension, while in African American women, large waist, low HDL, and hypertension were more prevalent. Using the IDF definition the two most common factors in Caucasian women were high triglycerides and hypertension, while in African American and Filipina women, hypertension and high FPG were more prevalent (p<0.05). A significantly higher proportion of African American women (73.5%) had a waist circumference above 80 cm compared to the other two ethnic groups (p<0.05).
Figure 1.
Prevalence of the MetS Components in Caucasian, African American, and Filipina Women
Table 3 shows comparisons of mean BAI, BMI and %BF by MetS status. Caucasian women with the MetS by either definition had the highest BAI, while BAI was lower and similar among African-American and Filipina women with the MetS, despite their disparate BMI and %BF. Mean BAI differed significantly among Caucasian women with versus without MetS by either NCEP (BAI: 35.2 vs 30.9) or IDF criteria (BAI: 35.1 vs 30.6, p<0.05), mean BAI only differed by MetS status among Filipina by IDF criteria (BAI: 34.6 vs. 32.4), however it did not differ by MetS among African American women (Table 3). In fact, BAI, BMI, and %BF were all significantly higher among Caucasians with MetS (by either definition) versus those without MetS. Whereas, among Filipina and African-American women, only BMI was significantly higher among women with MetS compared to those without MetS, by either criteria, while %BF was significantly higher among those with MetS by IDF criteria only.
Table 3.
Mean Obesity Measures by MetS Status in Caucasian, African American, and Filipina Women
| Caucasian | African American | Filipina | |||||
|---|---|---|---|---|---|---|---|
| MetS | No MetS | MetS | No MetS | MetS | No MetS | ||
| NCEP | BAI (%) | 35.2 ± 6.1* | 30.9 ± 4.4 | 33.7 ± 4.6 | 33.7 ± 5.7 | 33.8 ± 4.1 | 33.1 ± 4.1 |
| BMI (kg/m2) | 29.5 ± 5.2* | 24.6 ± 3.6 | 31.9 ± 4.4* | 29.2 ± 6.1 | 26.5 ± 3.8* | 25.0 ± 3.3 | |
| Body Fat (%) | 38.8 ± 7.4* | 33.5 ± 6.3 | 38.9 ± 6.8 | 37.3 ± 8.4 | 33.4 ± 4.7 | 33.4 ± 5.2 | |
| IDF | BAI (%) | 35.1 ± 5.3* | 30.6 ± 4.3 | 34.4 ± 5.6 | 33.4 ± 5.5 | 34.6 ± 4.0* | 32.4 ± 3.9 |
| BMI (kg/m2) | 29.5 ± 4.1* | 24.2 ± 3.6 | 31.5 ± 4.8* | 28.8 ± 6.1 | 27.4 ± 3.2* | 24.1 ± 3.1 | |
| Body Fat (%) | 39.8 ± 6.4* | 32.9 ± 6.1 | 39.0 ± 7.5* | 36.9 ± 8.4 | 34.8 ± 4.4* | 32.4 ± 5.2 | |
Data is Mean ± Standard Deviation
p<0.05
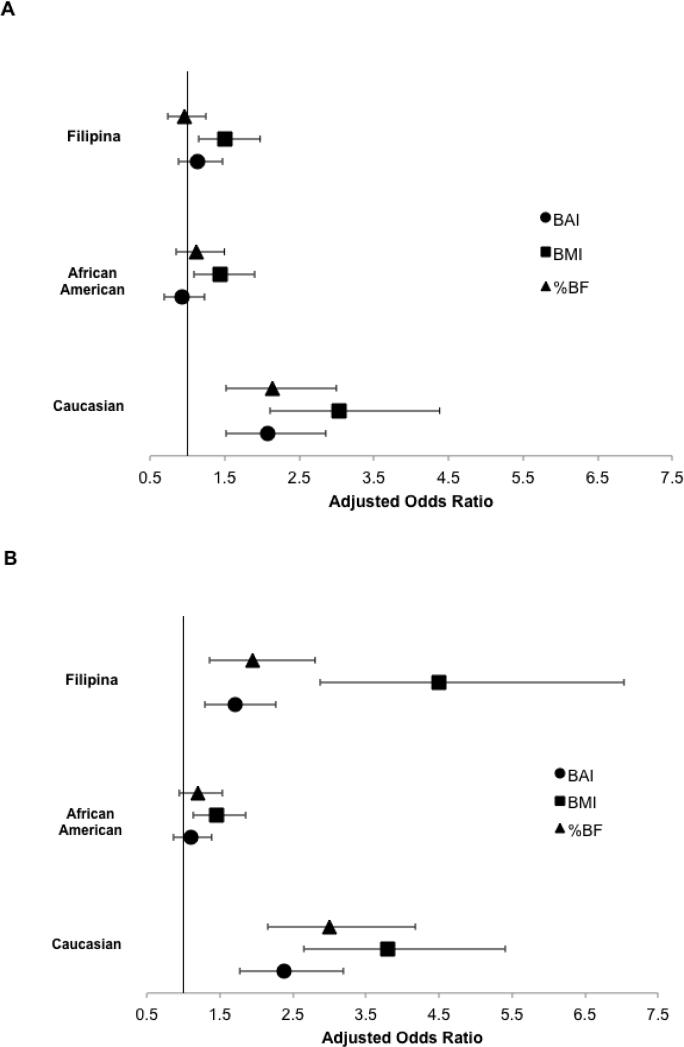
Odds ratios for presence of MetS by each adiposity measure after adjustment for current smoking status, current estrogen use, alcohol use, physical activity, and age are presented in Figure 2. Using the NCEP criteria, BAI was associated with the MetS among Caucasians only; using the IDF criteria, BAI was associated with the MetS among both Filipinas and Caucasians. Neither BAI nor %BF were associated with the MetS (by either definition) in the African American cohort. Using standardized unit increases, all odds ratios of having the MetS obtained using BMI as a risk factor were higher than those obtained using %BF or BAI as risk factors for women in all three ethnic groups. Moreover, odds ratios using BAI as a predictor had values similar to those obtained using DXA measured %BF for all women. These trends persisted when analyses were repeated after excluding those with Type 2 diabetes (analysis not shown).
Figure 2.
Associations between Having the MetS and Obesity Markers of Interest in Caucasian, African American, and Filipina Women A. NCEP-ATP III definition of MetS. B. IDF definition of MetS.
DISCUSSION
This study shows that BAI was more similar to DXA measured %BF than BMI when estimating the association with MetS. There were ethnic differences in the relation between adiposity and prevalent clinical conditions. In this analysis, African American women had significantly higher mean values for adiposity, including weight, BMI, BAI, %BF, and waist circumference than Caucasian and Filipina women. However, they had lower MetS prevalence compared to Filipina women.
To our knowledge, this is the first study to examine the utility of BAI in older women across three different ethnic groups and its applicability in evaluating the likelihood of the MetS in comparison to other adiposity measures; previous studies only examined the correlation of BAI with single risk factors for the MetS [26,27].
In this multi-ethnic cohort of women aged 50-70, BAI was positively associated with DXA measures, waist circumference and BMI across Caucasian, African American, and Filipina women. However, the correlations between BAI, %BF, and BMI varied by ethnicity and were significantly higher in Caucasian than in African American and Filipina women. Unlike BMI, which was significantly associated with the MetS in women of all ethnicities, BAI was associated with the MetS in Caucasian women regardless of definition, but only when the definition was based on IDF criteria in Filipina women. BAI was not associated at all with the MetS among African-American women.
In establishing the equation for BAI, Bergman and colleagues used a patient population of Mexican American men and women aged 18 to 65 years [15]. They validated their measure with a convenience sample of African American individuals aged 18-50 years and concluded that the performance of BAI as a predictor of %BF was optimal when the latter ranged from 15-35% [15]. Results of this study of women with diverse ethnicities are in accord with those of Bergman and colleagues showing high positive correlations between BAI and DXA derived body fat measures. Moreover, the results of this study are consistent with another published study among 18 to 69 year old men and women that showed BAI had higher correlations with %BF in Caucasian compared to African American women [28], but no association between BAI and BMI was reported. Other studies of women specific results showed conflicting trends of correlations between BAI and %BF as compared to BMI [17,21,29,30]. In contrast to the present study, these reports sampled younger and/or predominantly Caucasian cohorts.
BAI may be a less robust measure for the extremes in body adiposity, especially in Caucasian women with %BF higher than 38%. BAI was previously shown to diverge from %BF measurements at the extremities of the range in Caucasian adults [29]. Previous studies showed increased insulin resistance in African American compared to Caucasian women [31]. However, hip circumference in African American women can be wider than in Caucasian and Filipina women without manifestation of any characteristics of the MetS, thus hip circumference may be a less accurate indicator of body adiposity in older African American women because of differences in fat distribution [32]. Results from this study are also in accord with others showing that adiposity measures are heterogeneous across ethnicities [8,14,33]. This study further emphasizes that ethnic and age group specific thresholds should be developed for BAI to enhance its clinical utility.
This study has several limitations. These results may not be applicable to other cohorts of 50-70 year old women as participants in this study were selected to be of middle-class socioeconomic status. However, this homogeneity in socio-economic status across ethnicities was similar by design in order to reduce the confounding effects of disparate access to healthcare. Women in these cohorts were not randomly selected from the general population; they were part of a community-based convenience sample for a research study. Enrollment of Caucasian women was population-based for residents of Rancho Bernardo, however, population-based sampling of Filipinos was not possible because the 1990 census data reported all Asians collectively. Finally, this study included only women and was not able to examine the associations of BAI by gender . Some studies of BAI that included men and women did not stratify for sex in evaluating BAI, although it has been previously established that adiposity is gender dependent [34]. Strengths of this study include the ability to tease out ethnic differences in applicability and analytical outcome between two MetS definitions. This is also the first study to apply BAI as a risk factor for the MetS and compared to a wide range of adiposity measures including gold standard body adiposity measurements using DXA as well as other clinically used but simpler measures such as BMI, waist circumference, and waist-hip ratio [10,28,34].
In conclusion, BAI did not outperform BMI in correlations with other adiposity measures such as waist circumference and %BF. However, unlike BMI, BAI mimicked the specific ethnic differences found when using the more costly DXA %BF in association with the MetS. This suggests the utility of BAI as a quick, economical method to estimate body fat in selected ethnic groups, such as Asian women, who paradoxically manifest adverse metabolic outcomes despite normal or small body size [35]. BAI may be a less costly alternative to DXA measures when evaluating patients of various ethnic backgrounds, however before using BAI and creating clinical relevant cutoffs, additional studies with randomly selected individuals of both sexes as well as different age and ethnic cohorts should be performed.
ACKNOWLEDGEMENTS
The data analyzed in this article was collected with support from the American Heart Association Grant 0070088Y, NIH/National Institute of Diabetes and Digestive and Kidney Diseases Grant R03 DK60575, NIH/National Institute on Aging Grant 5R01AG07181, and NIH/National Institute of Diabetes and Digestive and Kidney Diseases Grant 5R01DK31801.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare that there is no conflict of interests regarding the publication of this article.
REFERENCES
- 1.Haslam DW, James WPT. Obesity. Lancet. 2005;366:1197–209. doi: 10.1016/S0140-6736(05)67483-1. [DOI] [PubMed] [Google Scholar]
- 2.Grundy SM, Brewer HB, Cleeman JI, et al. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–8. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 3.Alberti KGMM, Zimmet P, Shaw J. The metabolic syndrome--a new worldwide definition. Lancet. 2004;366:1059–62. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 4.Khaodhiar L, McCowen K, Blackburn G. Obesity and its comorbid conditions. Clin Cornerstone. 1999;2:17–31. doi: 10.1016/s1098-3597(99)90002-9. [DOI] [PubMed] [Google Scholar]
- 5.Keys A, Fidanza F, Karvonen MJ, et al. Indices of relative weight and obesity. J Chronic Dis. 1972;25:329–43. doi: 10.1016/0021-9681(72)90027-6. [DOI] [PubMed] [Google Scholar]
- 6.Eknoyan G. Historical Note Adolphe Quetelet (1796 – 1874)— the average man and indices of obesity. Nephrol Dial Transpl. 2008;23:47–51. doi: 10.1093/ndt/gfm517. [DOI] [PubMed] [Google Scholar]
- 7.Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004;79:379–84. doi: 10.1093/ajcn/79.3.379. [DOI] [PubMed] [Google Scholar]
- 8.Deurenberg P, Yap M, van Staveren W. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Relat Metab Disord. 1998;22:1164–71. doi: 10.1038/sj.ijo.0800741. [DOI] [PubMed] [Google Scholar]
- 9.Katzmarzyk PT, Bray GA, Greenway FL, et al. Ethnic-Specific BMI and Waist Circumference Thresholds. Obesity. 2011;19:1272–8. doi: 10.1038/oby.2010.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cornier M-A, Després J-P, Davis N, et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011:124. doi: 10.1161/CIR.0b013e318233bc6a. [DOI] [PubMed] [Google Scholar]
- 11.Stommel M, Schoenborn CA. Variations in BMI and prevalence of health risks in diverse racial and ethnic populations. Obesity. 2010;18:1821–6. doi: 10.1038/oby.2009.472. [DOI] [PubMed] [Google Scholar]
- 12.Raji A, Seely E, Arky R, et al. Body fat distribution and insulin resistance in healthy Asian Indians and Caucasians. J Clin Endocrinol Metab. 2001;86:5366–71. doi: 10.1210/jcem.86.11.7992. [DOI] [PubMed] [Google Scholar]
- 13.Araneta MRG, Barrett-Connor E. Ethnic differences in visceral adipose tissue and type 2 diabetes: Filipino, African-American, and white women. Obes Res. 2005;13:1458–65. doi: 10.1038/oby.2005.176. [DOI] [PubMed] [Google Scholar]
- 14.Dugas LR, Cao G, Luke AH, et al. Adiposity is not equal in a multi-race/ethnic adolescent population: NHANES 1999-2004. Obesity. 2011:10–2. doi: 10.1038/oby.2011.52. [DOI] [PubMed] [Google Scholar]
- 15.Bergman RN, Stefanovski D, Buchanan TA, et al. A better index of body adiposity. Obesity. 2011;19:1083–9. doi: 10.1038/oby.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang Z-Q, Liu Y-H, Xu Y, et al. The validity of the Body Adiposity Index in predicting percentage body fat and cardiovascular risk factors among Chinese. Clin Endocrinol (Oxf) 2013 doi: 10.1111/cen.12351. [DOI] [PubMed] [Google Scholar]
- 17.Chang H, Simonsick EM, Ferrucci L, et al. Validation study of the Body Adiposity Index as a predictor of percent body fat in older individuals: findings from the BLSA. J Gerontol A Biol Sci Med Sci. 2013:1–7. doi: 10.1093/gerona/glt165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vinknes KJ, Elshorbagy AK, Drevon CA, et al. Evaluation of the Body Adiposity Index in a Caucasian Population: The Hordaland Health Study. Am J Epidemiol. 2013;177:586–92. doi: 10.1093/aje/kws271. [DOI] [PubMed] [Google Scholar]
- 19.Gomez-Ambrosi J, Silva C, Catalan V, et al. Clinical Usefulness of a New Equation for Estimating Body Fat. Diabetes Care. 2012;35:383–8. doi: 10.2337/dc11-1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Freedman DS, Thornton J, Pi-Sunyer FX, et al. The body adiposity index (hip circumference ÷ height(1.5)) is not a more accurate measure of adiposity than is BMI, waist circumference, or hip circumference. Obesity. 2012 doi: 10.1038/oby.2012.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suchanek P, Lesna IK, Mengerova O, et al. Which index best correlates with body fat mass: BAI, BMI, waist or WHR? Neuroendocr Lett. 2012;33:78–82. [PubMed] [Google Scholar]
- 22.Barrett-Connor E. The prevalence of diabetes mellitus in an adult community as determined by history of fasting hyperglycemia. Am J Epidemiol. 1980;111:705–12. doi: 10.1093/oxfordjournals.aje.a112948. [DOI] [PubMed] [Google Scholar]
- 23.Eskridge SL, Morton DJ, Kritz-Silverstein D, et al. Estrogen therapy and bone mineral density in African-American and Caucasian women. Am J Epidemiol. 2010;171:808–16. doi: 10.1093/aje/kwp460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Araneta MRG, Wingard DL, Barrett-Connor E. Type 2 diabetes and metabolic syndrome in Filipina-American women: a high-risk nonobese population. Diabetes Care. 2002;25:494–9. doi: 10.2337/diacare.25.3.494. [DOI] [PubMed] [Google Scholar]
- 25.The hypertension detection and follow-up program: hypertension detection and follow-up program cooperative group. Prev Med. 1976;5:207–15. doi: 10.1016/0091-7435(76)90039-6. [DOI] [PubMed] [Google Scholar]
- 26.De Lima JG, Nobrega LHC, de Souza ABC. Body Adiposity Index Indicates Only Total Adiposity, Not Risk. Obesity. 2012;20:1140. doi: 10.1038/oby.2012.3. [DOI] [PubMed] [Google Scholar]
- 27.Snijder MB, Nicolaou M, van Valkengoed IGM, et al. Newly Proposed Body Adiposity Index (BAI) by Bergman et al. Is Not Strongly Related to Cardiovascular Health Risk. Obesity. 2012;20:1138–9. doi: 10.1038/oby.2011.338. [DOI] [PubMed] [Google Scholar]
- 28.Barreira T, Harrington D, Staiano A, et al. Research letter: body adiposity index, body mass index, and body fat in White and Black adults. JAMA. 2011;306:828–30. doi: 10.1001/jama.2011.1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Johnson W, Chumlea WC, Czerwinski SA, et al. Concordance of the Recently Published Body Adiposity Index With Measured Body Fat Percent in European-American Adults. Obesity. 2012;20:900–3. doi: 10.1038/oby.2011.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Freedman DS, Blanck HM, Dietz WH, et al. Is the body adiposity index (hip circumference/height(1.5)) more strongly related to skinfold thicknesses and risk factor levels than is BMI? The Bogalusa Heart Study. Brit J Nut. 2013;109:338–45. doi: 10.1017/S0007114512000979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ingram KH, Lara-Castro C, Gower BA, et al. Intramyocellular lipid and insulin resistance: differential relationships in European and African Americans. Obesity. 2011;19:1469–75. doi: 10.1038/oby.2011.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Osei K. Metabolic syndrome in blacks: are the criteria right? Curr Diab Rep. 2010;10:199–208. doi: 10.1007/s11892-010-0116-4. [DOI] [PubMed] [Google Scholar]
- 33.Lear SA, Humphries KH, Kohli S, et al. Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M-CHAT). Am J Clin Nutr. 2007;86:353–9. doi: 10.1093/ajcn/86.2.353. [DOI] [PubMed] [Google Scholar]
- 34.Schulze MB, Stefan N. The body adiposity index and the sexual dimorphism in body fat. Obesity. 2011;19:1729. doi: 10.1038/oby.2011.153. [DOI] [PubMed] [Google Scholar]
- 35.Palaniappan L, Wong E, Shin J, et al. Asian Americans have greater prevalence of metabolic syndrome despite lower body mass index. Int J Obes. 2011;35:393–400. doi: 10.1038/ijo.2010.152. [DOI] [PMC free article] [PubMed] [Google Scholar]