Abstract
Background
The Warfarin versus Aspirin in Reduced Cardiac Ejection Fraction trial found no difference between warfarin and aspirin in patients with low ejection fraction in sinus rhythm for the primary outcome: first to occur of 84 incident ischemic strokes (IIS), 7 intracerebral hemorrhages or 531 deaths. Prespecified secondary analysis showed a 48% hazard ratio reduction (p = 0.005) for warfarin in IIS. Cardioembolism is likely the main pathogenesis of stroke in heart failure. We examined the IIS benefit for warfarin in more detail in post hoc secondary analyses.
Methods
We subtyped IIS into definite, possible and noncardioembolic using the Stroke Prevention in Atrial Fibrillation method. Statistical tests, stratified by prior ischemic stroke or transient ischemic attack, were the conditional binomial for independent Poisson variables for rates, the Cochran-Mantel-Haenszel test for stroke subtype and the van Elteren test for modified Rankin Score (mRS) and National Institute of Health Stroke Scale (NIHSS) distributions, and an exact test for proportions.
Results
Twenty-nine of 1,142 warfarin and 55 of 1,163 aspirin patients had IIS. The warfarin IIS rate (0.727/100 patient-years, PY) was lower than for aspirin (1.36/100 PY, p = 0.003). Definite cardioembolic IIS was less frequent on warfarin than aspirin (0.22 vs. 0.55/100 PY, p = 0.012). Possible cardioembolic IIS tended to be less frequent on warfarin than aspirin (0.37 vs. 0.67/100 PY, p = 0.063) but noncardioembolic IIS showed no difference: 5 (0.12/100 PY) versus 6 (0.15/100 PY, p = 0.768). Among patients experiencing IIS, there were no differences by treatment arm in fatal IIS, baseline mRS, mRS 90 days after IIS, and change from baseline to post-IIS mRS. The warfarin arm showed a trend to a lower proportion of severe nonfatal IIS [mRS 3–5; 3/23 (13.0%) vs. 16/48 (33.3%), p = 0.086]. There was no difference in NIHSS at the time of stroke (p = 0.825) or in post-IIS mRS (p = 0.948) between cardioembolic, possible cardioembolic and noncardioembolic stroke including both warfarin and aspirin groups.
Conclusions
The observed benefits in the reduction of IIS for warfarin compared to aspirin are most significant for cardioembolic IIS among patients with low ejection fraction in sinus rhythm. This is supported by trends to lower frequencies of severe IIS and possible cardioembolic IIS in patients on warfarin compared to aspirin.
Keywords: Aspirin, Cardiac embolism, Heart failure, Stroke prevention
Introduction
Heart failure (HF) ranks second as a cause of cardiogenic stroke after atrial fibrillation (AF) with approximately 60,000 strokes per year [1]. HF however affects more than twice as many individuals in the population in the USA (almost 6 million) as are affected by AF (2.3 million). Cardioembolism is likely the main pathogenesis of stroke in HF as it is in AF. Like the dysfunctional left atrial appendage, the dilated left ventricle may be a site of thrombus formation.
HF is likely a prothrombotic state with a higher plasma viscosity, soluble P-selectin, von Willebrand factor and fibrinogen [2]. There is an increased incidence of left ventricular mural thrombi of up to 36% in cardiomyopathy [3].
The Warfarin versus Aspirin in Reduced Cardiac Ejection Fraction (WARCEF) trial [4] was designed to evaluate the efficacy of warfarin compared to aspirin among patients with reduced ejection fraction and normal sinus rhythm. Overall, there was no difference in the primary outcome of first to occur of ischemic stroke, intracerebral hemorrhage or death from any cause over 3.5 ± 0.8 years. However, there was a significant benefit for warfarin over aspirin in terms of time to incident ischemic stroke (IIS; HR 0.52; 95% confidence interval 0.33–0.82; p = 0.005 in a stratified cause-specific Cox model) [5]. This is similar to the risk reduction with warfarin in AF [6] supporting a cardiogenic embolic etiology for stroke in HF in sinus rhythm. In the current post hoc analysis we explore differential effects between warfarin and aspirin on stroke subtype and severity. Since warfarin has a differential effect over warfarin for cardioembolic stroke in AF, we wanted to determine if a similar effect pertains to HF in sinus rhythm [7].
Methods
The methodology and results of the primary WARCEF analysis have been previously published [4, 5]. Here we further analyze data from the 84 patients with IIS. It is difficult to diagnose noncardioembolic stroke with ORG-10172 in Acute Stroke Trial criteria [8] , which classify dilated cardiomyopathy as a high-risk cardioembolic source. In the presence of cardiomyopathy, patients who also fulfill criteria for a noncardioembolic stroke subtype (e.g. lacunar) are classified as stroke of undetermined etiology (2 causes identified). Stroke subtyping in the WARCEF trial was therefore performed using the Stroke Prevention in Atrial Fibrillation (SPAF) method [9] , with a minor modification. The SPAF method divides stroke in cardioembolic versus other subtypes without using echocardiographic data. Subtyping was performed by an adjudication committee of 5 stroke neurologists and the clinical events committee chairperson, with 2 neurologists serving as the primary reviewers and final adjudication by consensus of all adjudicators. Since a diagnosis of definite cardioembolic stroke according to the SPAF criteria requires carotid imaging and 38 patients with IIS (36%) did not have carotid imaging but had symptoms or imaging suggestive of cardioembolism, we renamed the SPAF ‘uncertain’ group as ‘possible cardioembolic’. Justification for this is given in the Results. Patients with ‘noncardioembolic’ stroke met criteria for lacunar stroke or atherothrombotic stroke.
We present median scores and interquartile ranges (IQR) for warfarin and aspirin arms on outcome measures. Statistical comparisons were stratified by prior ischemic stroke or transient ischemic attack status. All tests were performed at the α = 0.05 level. We used a stratified exact conditional binomial test for two independent Poisson variables to compare rates, a stratified Cochran-Mantel-Haenszel test to compare stroke subtype distributions, the van Elteren test (a stratified Wilcoxon rank sum test) to compare modified Rankin Score (mRS) and National Institute of Health Stroke Scale (NIHSS) distributions, and the stratified exact test of two independent proportions to compare proportions.
Results
Eighty-four of the 2,305 randomized patients had IIS. Thirty-one (37%) of these were classified as having a definite cardioembolic etiology, 42 (50%) a possible cardioembolic etiology, and 11 (13%) a noncardioembolic one (table 1). Among the 42 patients with possible cardioembolic stroke, 13 (31%) had a >2 cm cortical lesion on imaging, 23 (55%) had symptoms of cortical involvement, and in 24 (57%) the deficit was maximal at onset. Twenty-one patients (50%) had 2 or more of these 3 findings and 9 (21%) had all 3.
Table 1.
Ischemic stroke subtype by treatment
| Type | Aspirin | Warfarin | Total |
|---|---|---|---|
| Definite cardioembolic | 22 (40.0) | 9 (31.0) | 31 (36.9) |
| Noncardioembolic | 6 (10.9) | 5 (17.2) | 11 (13.1) |
| Possible cardioembolic | 27 (49.1) | 15 (51.7) | 42 (50.0) |
| Total | 55 (100.0) | 29 (100.0) | 84 (100.0) |
Results are presented as numbers of patients, with percentages in parentheses; percentages may not sum to 100 because of rounding.
p value = 0.583, Cochran-Mantel-Haenszel test stratified by ischemic stroke or transient ischemic attack prior to baseline.
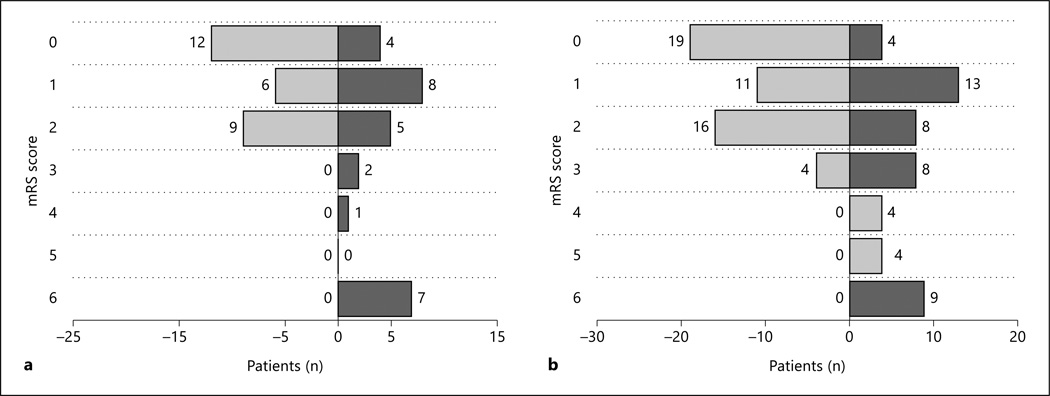
Twenty-nine (2.5%) of 1,142 patients on warfarin and 55 (4.7%) of 1,163 on aspirin had IIS. The warfarin IIS rate (0.72/100 patient years, PY) was lower than for aspirin (1.36/100 PY; p = 0.003). There were no differences between warfarin and aspirin IIS patients in baseline mRS (median 1, IQR 0–2, n = 29 vs. median 1, IQR 0–2, n = 55, p = 0.241), fatal (within 30 days) IIS (3/29, 10.3% vs. 6/55, 10.9%, p = 1.0), or post-IIS (after 90 ± 30 days) mRS (median 2, IQR 1–4, n = 23 vs. median 2, IQR 1–4, n = 48, p = 0.437; fig. 1). There were also no differences between warfarin and aspirin in change from baseline to post-IIS mRS (median 1, IQR 0–3, n = 23 vs. median 1, IQR 0–3, n = 48, p = 0.884). Definite cardioembolic IIS was significantly less frequent on warfarin than on aspirin [9 events (0.22/100 PY) vs. 22 (0.55/100 PY), p = 0.012; table 2]. The warfarin arm showed trends to fewer severe (post-IIS mRS 3–5) IIS [3/23 (13.0%) vs. 16/48 (33.3%), p = 0.086; fig. 1 ], and to a lower rate of IIS of possible cardioembolic etiology [15 (0.37/100 PY) vs. 27 (0.67/100 PY), p = 0.063; table 2]. There was no difference between warfarin and aspirin in rate of noncardioembolic IIS [5 (0.12/100 PY) vs. 6 (0.15/100 PY), p = 0.768; table 2 ]. There was no difference in NIHSS at stroke (p = 0.825) or in post-IIS mRS (p = 0.948) between cardioembolic, possible cardioembolic and noncardioembolic stroke including both warfarin and aspirin groups.
Fig. 1.
Split bar graphs comparing baseline (light) and follow-up (dark) mRS scores for patients with outcome ischemic stroke or intracerebral hemorrhage. a Warfarin patients (n = 27). b Aspirin patients (n = 50).
Table 2.
Stroke subtype rates by treatment
| Type | Aspirin (4,032.8 PY) events |
Warfarin (4,044.7 PY) events |
p value |
|---|---|---|---|
| Definite cardioembolic | 22 (0.55) | 9 (0.22) | 0.012 |
| Noncardioembolic | 6 (0.15) | 5 (0.12) | 0.768 |
| Possible cardioembolic | 27 (0.67) | 15 (0.37) | 0.063 |
| Total | 55 (1.36) | 29 (0.72) | 0.003 |
Figures in parentheses indicate the rate per 100 PY. For p values, exact conditional binomial test for 2 independent Poisson variables, stratified by prior ischemic stroke or transient ischemic attack.
Discussion
The WARCEF trial found no difference in heart failure patients in sinus rhythm between warfarin and aspirin treatment for the outcome of first to occur of 84 IISs, 7 intracerebral hemorrhages or 531 deaths. Warfarin, as compared with aspirin, was however associated with a significant reduction in the rate of IIS throughout the follow-up period [5]. Although the WARCEF trial was reported as a negative study overall, an accompanying editorial did suggest that there may be subgroups of patients, such as those at risk of cardioembolic IIS, who could benefit from warfarin [10]. The marked reduction between the rates of cardioembolic IIS between warfarin and aspirin we found (0.55 vs. 0.22/100 PY) shows a stronger risk reduction effect in cardioembolic IIS than in all stroke subtypes, and suggests that in stroke of cardioembolic etiology, the reduction of IIS may be clinically significant.
We found 37% of IIS in patients with HF in sinus rhythm to be definitely of cardioembolic etiology, but a further 50% were of possible cardioembolic etiology. Half of the patients in the ‘possible cardioembolic’ group had at least 2 criteria of cardioembolic stroke, which supports the ‘possible’ cardioembolic etiology of this group and justifies the renaming of this SPAF ‘uncertain’ group as ‘possible cardioembolic’. It is likely that up to half of this group actually had cardioembolic stroke, but they were not included in the ‘definite’ cardioembolic group because they had no carotid imaging. The frequency of cardioembolic stroke in AF has been estimated to be about 65–70%, and our findings suggest that the frequency may be similar in patients with HF in sinus rhythm. Further confirmation is needed however.
The SPAF-II trial showed a differential effect of warfarin over aspirin in cardioembolism in AF [9] and our findings are similar. Aspirin decreases platelet aggregation which is encouraged by the higher shear rates in the arterial circulation. Warfarin is more effective in the reduction of red thrombus in the venous circulation and has been shown to be effective in reducing stroke secondary to left atrial appendage thrombus in AF. In HF in sinus rhythm, the enlarged poorly functioning left ventricle probably predisposes to thrombus formation and our results suggest that warfarin is effective in preventing the consequences of such mural thrombi. Cardioembolic stroke is the most disabling stroke subtype, and a differential reduction of this subtype is therefore extremely important.
Some [10] have suggested that the beneficial effect of warfarin in reducing the risk of IIS in the WARCEF trial was offset by the major hemorrhage rates. There is much discussion about whether a risk of systemic hemorrhage which is potentially completely treatable should negate treatment with an agent (warfarin) that reduces the permanent disability associated with stroke. This is even more questionable if warfarin is reducing the frequency of the more disabling strokes. In the treatment of AF equipoise has moved to treating with warfarin even if there are significant risks of systemic hemorrhage, on the basis that stroke is likely to lead to permanent disability whereas systemic hemorrhage, even if severe, is not. For this reason, it is important to look further at the use of warfarin in HF in sinus rhythm and identify subgroups in whom stroke prevention would be clinically relevant and indicated. The new anticoagulants [11] also need to be studied as they may offer advantages over warfarin in HF in sinus rhythm.
Acknowledgments
Funding was offered by U01-NS-043975 (S. Homma) and U01-NS-039143 (J.L.P. Thompson) from the National Institute of Neurological Diseases and Stroke. Warfarin and warfarin placebo were provided by Taro Pharmaceuticals USA Inc., Hawthorne, N.Y., USA, and aspirin and aspirin placebo by Bayer HealthCare LLC, Morristown, N.J., USA.
References
- 1.Pullicino P, Homma S, Thompson JLP, Freudenberger RS, Sacco RL, Mohr JP. Oral anticoagulation in patients with cardiomyopathy or heart failure in sinus rhythm. Cerebrovasc Dis. 2008;26:322–327. doi: 10.1159/000149581. [DOI] [PubMed] [Google Scholar]
- 2.Gibbs CR, Blann AD, Watson RD, Lip GY. Abnormalities of hemorheological, endothelial, and platelet function in patients with chronic heart failure in sinus rhythm: effects of angiotensin-converting enzyme inhibitor and beta-blocker therapy. Circulation. 2001;103:1746–1751. doi: 10.1161/01.cir.103.13.1746. [DOI] [PubMed] [Google Scholar]
- 3.Gottdiener JS, Gay JA, Van Voorhees L, Di Bianco R, Fletcher RD. Frequency and embolic potential of left ventricular thrombus in dilated cardiomyopathy: assessment by 2-dimensional echocardiography. Am J Cardiol. 1983;52:1281–1285. doi: 10.1016/0002-9149(83)90588-x. [DOI] [PubMed] [Google Scholar]
- 4.Pullicino P, Thompson JLP, Barton B, Levin B, Graham S, Freudenberger RS WARCEF Investigators. Warfarin versus Aspirin in Patients with Reduced Cardiac Ejection Fraction (WARCEF): rationale, objectives and design. J Cardiac Fail. 2006;12:39–46. doi: 10.1016/j.cardfail.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 5.Homma S, Thompson JLP, Pullicino PM, Levin B, Freudenberger RS, Teerlink JR, Ammon SE, Graham S, Sacco RL, Mann DL, Mohr JP, Massie BM, Labovitz AJ, Anker SD, Lok DJ, Ponikowski P, Estol CJ, Lip GY, Di Tullio MR, Sanford AR, Mejia V, Gabriel AP, del Valle ML, Buchsbaum R. Warfarin and aspirin in patients with heart failure and sinus rhythm. N Engl J Med. 2012;366:1859–1869. doi: 10.1056/NEJMoa1202299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hart RG, Benavente O, McBride R, Pearce LA. Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a metaanalysis. Ann Intern Med. 1999;131:492–501. doi: 10.7326/0003-4819-131-7-199910050-00003. [DOI] [PubMed] [Google Scholar]
- 7.Miller VT, Pearce LA, Feinberg WM, Rothrock JF, Anderson DC, Hart RG Stroke Prevention in Atrial Fibrillation Investigators. Differential effect of aspirin versus warfarin on clinical stroke types in patients with atrial fibrillation. Neurology. 1996;46:238–240. doi: 10.1212/wnl.46.1.238. [DOI] [PubMed] [Google Scholar]
- 8.Adams HP, Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE, III TOAST Investigators. Classification of subtype of acute ischemic stroke: definitions for use in a multicenter clinical trial. Stroke. 1993;24:35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 9.Hart RG, Pearce LA, Miller VT, Anderson DC, Rothrock JF, Albers GW, Nasco E SPAF Investigators. Cardioembolic vs noncardioembolic strokes in atrial fibrillation: frequency and effect of antithrombotic effect in the stroke prevention in atrial fibrillation studies. Cerebrovasc Dis. 2000;10:39–43. doi: 10.1159/000016023. [DOI] [PubMed] [Google Scholar]
- 10.Eikelboom JW, Connolly SJ. Warfarin in heart failure. N Engl J Med. 2012;366:1936–1938. doi: 10.1056/NEJMe1202504. [DOI] [PubMed] [Google Scholar]
- 11.Marrone LCP, Marrone ACH. Acute ischemic stroke and new anticoagulants – how to act in the acute phase of stroke. Cerebrovasc Dis. 2013;35:91. doi: 10.1159/000346079. [DOI] [PubMed] [Google Scholar]