Abstract
Background
Childhood obesity and asthma are increasing worldwide. A possible link between the two conditions has been postulated.
Methods
Cross-sectional studies of stratified random samples of 8–12-year-old children (n = 10 652) (16 centres in affluent and 8 centres in non-affluent countries) used the standardized methodology of ISAAC Phase Two. Respiratory and allergic symptoms were ascertained by parental questionnaires. Tests for allergic disease were performed. Height and weight were measured, and overweight and obesity were defined according to international definitions. Prevalence rates and prevalence odds ratios were calculated.
Results
Overweight (odds ratio = 1.14, 95%-confidence interval: 0.98; 1.33) and obesity (odds ratio = 1.67, 95%-confidence interval: 1.25; 2.21) were related to wheeze. The relationship was stronger in affluent than in non-affluent centres. Similar results were found for cough and phlegm, rhinitis and eczema but the associations were mostly driven by children with wheeze. There was a clear association of overweight and obesity with airways obstruction (change in FEV1/FVC, −0.90, 95%-confidence interval: −1.33%; −0.47%, for overweight and −2.46%, 95%-confidence interval: −3.84%; −1.07%, for obesity) whereas the results for the other objective markers, including atopy, were null.
Conclusions
Our data from a large international child population confirm that there is a strong relation of body mass index with wheeze especially in affluent countries. Moreover, body mass index is associated with an objective marker of airways obstruction (FEV1/FVC) but no other objective markers of respiratory and allergic disorders.
Introduction
The prevalence of obesity in childhood is increasing in many countries worldwide. Secular trends of increased obesity and asthma prevalence in adults and children during the past decades have led to a debate about potential links between both conditions. Suggested mechanisms to explain this association includes mechanical, lifestyle, dietary, immunological, hormonal, and common genetic factors [1].
There is evidence from cross-sectional studies [2], [3] that obesity is associated with asthma in childhood [4]–[6]. Prospective cohort studies show associations between obesity and incidence [7], [8] and persistence of asthma [9]. In a cohort study, overweight children had higher risk of asthma symptoms and bronchial hyper-responsiveness (BHR) at 8 years [10]. Although there is evidence of a link between obesity and asthma in children from predominantly western populations, little is known about less affluent regions and the under-lying mechanisms [11]. A recent report from the International Study of Asthma and Allergies in Childhood (ISAAC) Phase Three, a cross-sectional study, revealed associations between overweight and obesity and symptoms of asthma and eczema but not rhinoconjunctivitis [12]. However, no systematic evaluation of the association of objectively measured weight and height, with questionnaire reports together with objective measures of allergy and lung function has been available.
Despite the growing research over the obesity/asthma relationship, little is known about worldwide variation in the relationship of excess body mass index (BMI) and the prevalence of respiratory symptoms and allergic disease, and even less regarding objective markers for allergy and respiratory function. The ISAAC Phase Two study is ideally suited to address these issues because it includes a large number of children in geographically and economically diverse regions with data on various objective markers, and measured BMI in addition to a range of reported symptoms.
Methods
Study populations and field work
The methods of ISAAC Phase Two have been described in detail elsewhere [13]. Briefly, random samples of at least 10 schools from defined geographical areas were chosen and children (n>1 000 per centre) attending classes with a majority of 9–11-year-olds were invited to participate. Standardized parental questionnaires were used. In three countries (Ghana, Brazil and India) the questions were posed by trained interviewers because illiteracy was common.
The ISAAC Phase Two methodology allowed objective measurements to be performed either in the full sample (option A) or in random subsamples of children, generally stratified by wheeze (option B) [13]. Most centres invited all children to participate in the skin prick testing, while blood sampling, BHR tests and anthropometric measurements were carried out mostly in stratified random subsamples of children with and without reports of wheeze in the past year (targeting 100 per centre in each stratum).
Fuller details of the skin examination, lung function measurements and BHR, total immunglobulin E (IgE) measurements and skin prick tests to six aeroallergens (Dermatophagoides pteronyssinus, D. farinae, cat dander, Alternaria tenuis, mixed tree pollen and mixed grass pollen) have been published elsewhere [13] and can be found at http://isaac.auckland.ac.nz/phases/phasetwo/phasetwo.html.
Symptoms data
Standardized parental questionnaires, including detailed questions on the occurrence and severity of symptoms of asthma (wheeze), rhinitis (with and without conjunctivitis) and flexural eczema were administered. In this context, wheezing is regarded as indicator symptom for asthma. These were identical to those used in ISAAC Phase One for parents of children aged 6–7 years [13]. In addition, in many (but not all) centres, questions about cough and phlegm were asked (http://isaac.auckland.ac.nz/phases/phasetwo/phasetwo.html and Online-Repository in File S1).
Assessment of adiposity
Weight and height were measured without shoes and BMI was calculated. We used the age and sex specific BMI cut points for overweight and obesity derived from an international data set by Cole et al [14]. These cut points are based on age and sex specific percentile curves that were shown to correspond to the adult cut points of 25 and 30 kg/m2 for overweight and obesity, respectively. This procedure has the advantage of being independent of the prevalence of obesity in the individual study centres, thereby enabling their comparison and combining of results.
Statistical analysis
Prevalence, population means and linear and logistic regression for health outcomes were calculated with the SURVEY-procedures of SAS (V9.2) using the appropriate weighting and variance estimation to account for stratified subsampling [15] where necessary. Total IgE as an outcome was dichotomized at the median (4.17 kU/l). Separate regression models were fitted for each centre and combined estimates of the effect estimates were derived using random effects meta-analysis [16]. Associations are presented as odds ratios (OR) or change in the parameter of interest. Forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) as measured during spirometry were used in the statistical analysis, adjusting for age, gender and height, rather than using predicted values which may not be applicable in a large global setting with different child populations [17].
Potential confounders were tested by including them one by one in the centre-specific models and only those that resulted in a notable (10% or greater) change of the combined estimate were retained. The potential confounders included sex, age, diet (fruit and vegetable intake), Mediterranean diet, physical activity, reported parental allergic disease, maternal education, birth weight, breastfeeding, maternal smoking in pregnancy, anybody smoking in the child’s home, and damp spots or moulds in the child’s home. Based on the change-in-parameter criterion, only sex was retained in the fully adjusted model. Adjustment with physical activity and diet did not result in any change of the estimates but reduced the study population by about half. Results using adjustment for all other tested factors are presented in table S2 in File S2. Models for lung function (FEV1, FVC) were adjusted for age, sex and height.
The influence of potential effect modifiers was investigated by performing stratified centre-specific analyses, calculating the combined effect for each stratum and evaluating the difference between strata-specific estimates. Due to small cell counts in some centres in specific strata, the number of centres contributing to the stratum-specific estimates may differ from the number of centres in the corresponding unstratified analyses.
Centres classified by the World Bank as ‘high income countries’ (i.e. gross national income (GNI) per capita per year in 2001 ≧ 9 200 US $) were combined in a group called ‘affluent countries’ and the remaining centres in a group called ‘non-affluent countries’ [18].
Ethics statement
All centres obtained approval by local ethics committees and investigators were trained in one location to assure comparable data quality. Almeria, Cartagena, Madrid, Valencia (all Spain): Ethics Committee of the “12 de Octubre” Hospital in Madrid; Tirana (Albania): National Ethics Committee; Tallinn (Estonia): The Medical Research Ethics Committee of Estonian Institute of Experimental and Clinical Medicine; Creteil (France): Comite Consultatif de Protection des Personnes dans la recherché biomedicale- Marseille 2; Dresden, Munich (both Germany): Ethics Committee of the University of Münster; Athens, Thessaloniki (both Greece): Hippokration General Hospital Ethical Committee; Rome (Italy): Ethic Committee of catholic University, Rome; Reykjavik (Iceland): National Bioethics Committee; Utrecht (Netherlands): Medical Ethical Committee of Wageningen University; Tromso (Norway): Regional Medical Ethics Committeee Norwegian Data Inspectorate; Linkoeping, Oestersund (both Sweden): Ethics committee at Linköping and Umea University; Ankara (Turkey): Ethics committee of Hacettepe University Faculty of Medicine; Ethics committee of the Turkish Ministry of Health; West Sussex (UK): Local Research Ethics Committee for Mid-Downs Health Authority; Hawkes Bay (New Zeland): Hawkes Bay Ethics Committee; Hong Kong (China): Ethics Committee of the Chinese University of Hong Kong; Beijing (China): Ethics Committee of Capital Institute of Paediatrics, Beijing; Guangzhou (China): Ethics Committee of Guangzhou Institute of Respirating Diseases; Kintampo (Ghana): London school of Hygiene and Tropical Medicine Ethics Committee; Mumbai (India): Jaslok Hospital; Uruguaiana (Brazil): Comite de Etica e Pesquisa da Pontificia Universidade Catolica do RGS; Pichincha (Ecuador): Saludesa/Hospital Pedro Vicente Maldonado Ad Hoc Ethics Committee; Tbilisi (Georgia): Bioethics National Counsil of Ministry of Labor, Health and Social Affairs of Georgia; Ramallah (Palestine): Palestinian Ministry of education; Palestinian Ministry of health; United Nations Relief and works Agency (UNRWA) school education dept.; Riga (Latvia): Ethics Committee of Riga Stradins University. The international coordination and collaboration has been approved by the ethics committees of the universities of Münster and Ulm, Germany [13]. Participation was voluntary and written consent from the parents was obtained for each child.
Results
Table 1 presents mean BMI and the prevalence of overweight/obesity and the 12-months prevalence of wheeze for each study centre. An expanded version of the table, including all health-related outcomes, is included in Table S1 in File S2. Mean BMI was highest in Almeria (Spain) with 21 kg/m2 and lowest in Mumbai (India) with 15 kg/m2. The percentage of overweight children (excluding obese children) ranged from 0.6% in Kintampo (Ghana) to 38.7% in Uruguaiana (Brazil), and the percentage of obese children from 0 in Kintampo and Mumbai to 22.1% in Almerìa. Within Europe, there was a gradient with children from the Mediterranean region being more frequently obese. Wheeze was most frequent in Brazil (25.6%) and least prevalent in Athens, Greece (5.6%).
Table 1. Description of the study population: estimates referring to the full sample mean and prevalence are reported (implying appropriate weighting for stratified subsamples).
| Centre | N | Age | BMI | Overweight | Obese | Wheeze | |||
| Mean (95%-CI) | Mean (95%-CI) | N | % (95%-CI) | N | % (95%-CI) | N | % (95%-CI) | ||
| Brazil, Uruguaiana$ | 953 | 9.63 (9.58;9.68) | 19.8 (19.6;20.0) | 368 | 38.7 (35.6;41.8) | 105 | 11.1 (9.1;13.1) | 245 | 25.6 (23.7;27.6) |
| Estonia, Tallinn* | 241 | 10.09 (10.05;10.13) | 17.8 (17.5;18.1) | 37 | 15.8 (10.9;20.8) | 7 | 2.8 (0.6;5.0) | 55 | 8.4 (6.7;10.2) |
| Georgia, Tbilisi* | 169 | 10.41 (10.31;10.50) | 18.8 (18.2;19.3) | 31 | 20.1 (13.3;27.0) | 12 | 6.4 (2.3;10.5) | 54 | 9.2 (7.4;11.1) |
| Germany, Dresden§ | 694 | 9.87 (9.84;9.91) | 17.4 (17.2;17.6) | 100 | 14.4 (11.8;17.0) | 21 | 3.0 (1.7;4.3) | 52 | 7.9 (6.9;8.8) |
| Germany, Munich§ | 886 | 9.55 (9.51;9.59) | 17.9 (17.7;18.1) | 168 | 19.0 (16.4;21.5) | 40 | 4.5 (3.1;5.9) | 75 | 8.3 (7.3;9.2) |
| Ghana, Kintampo* | 241 | 10.37 (10.28;10.46) | 16.1 (16.0;16.3) | 1 | 0.6 (0;1.7) | 0 | 0 | 81 | 6.4 (5.1;7.7) |
| Greece, Athens* | 193 | 9.79 (9.72;9.85) | 19.9 (19.4;20.5) | 54 | 27.7 (21.0;34.4) | 30 | 15.4 (10.0;20.9) | 37 | 5.6 (4.2;7.1) |
| Greece, Thessaloniki* | 211 | 9.74 (9.66;9.82) | 20.2 (19.7;20.6) | 73 | 35.8 (28.4;43.3) | 40 | 15.0 (9.6;20.4) | 73 | 8.4 (6.7;10.1) |
| India, Mumbai* | 119 | 9.77 (9.63;9.92) | 15.0 (14.6;15.5) | 7 | 4.9 (0.6;9.2) | 0 | 0 | 33 | 6.1 (4.9;7.3) |
| Italy, Rome$ | 1307 | 10.02 (9.99;10.04) | 19.4 (19.2;19.6) | 402 | 30.8 (28.3;33.3) | 137 | 10.5 (8.8;12.1) | 103 | 7.9 (6.5;9.4) |
| Latvia, Riga§ | 156 | 10.54 (10.45;10.63) | 18.0 (17.5;18.4) | 20 | 12.8 (7.5;18.1) | 3 | 1.9 (0;4.1) | 16 | 6.9 (5.3;8.6) |
| Netherlands, Utrecht$ | 2638 | 9.50 (9.45;9.54) | 17.8 (17.7;17.9) | 413 | 15.7 (14.3;17.0) | 98 | 3.7 (3.0;4.4) | 238 | 8.7 (7.8;9.6) |
| New Zealand, Hawkes Bay* | 222 | 10.76 (10.69;10.83) | 19.8 (19.3;20.3) | 52 | 22.4 (16.1;28.7) | 25 | 9.5 (5.2;13.7) | 111 | 21.9 (19.7;24.1) |
| Norway, Tromso* | 637 | 9.94 (9.89;10.00) | 17.9 (17.7;18.1) | 106 | 16.0 (13.2;18.9) | 25 | 3.4 (2.1;4.8) | 131 | 14.0 (12.9;15.2) |
| Palestine, Ramallah* | 216 | 9.73 (9.54;9.91) | 17.8 (17.4;18.2) | 25 | 12.2 (7.6;16.8) | 10 | 4.0 (1.4;6.6) | 43 | 8.8 (7.6;9.9) |
| Spain, Almeria* | 208 | 10.26 (10.15;10.37) | 21.0 (20.4;21.7) | 65 | 33.1 (25.2;41.1) | 45 | 22.1 (15.1;29.1) | 105 | 15.5 (13.4;17.7) |
| Spain, Cartagena* | 160 | 9.53 (9.44;9.63) | 18.6 (18.0;19.2) | 42 | 21.7 (14.2;29.2) | 17 | 10.2 (4.6;15.8) | 70 | 11.9 (10.2;13.6) |
| Spain, Madrid* | 408 | 9.21 (9.15;9.27) | 19.3 (18.9;19.6) | 114 | 27.5 (23.1;31.9) | 59 | 14.7 (11.1;18.2) | 80 | 11.6 (9.6;13.7) |
| Spain, Valencia* | 192 | 9.32 (9.22;9.42) | 19.3 (18.8;19.7) | 68 | 35.4 (28.5;42.3) | 20 | 10.4 (6.0;14.8) | 28 | 9.1 (7.6;10.7) |
| Sweden, Linkoeping* | 181 | 10.72 (10.61;10.82) | 19.4 (18.9;19.9) | 42 | 23.6 (16.5;30.7) | 14 | 5.6 (2.0;9.2) | 59 | 7.9 (6.2;9.7) |
| Sweden, Oestersund* | 278 | 10.70 (10.60;10.80) | 18.7 (18.3;19.0) | 49 | 15.5 (10.6;20.4) | 17 | 3.8 (1.4;6.2) | 109 | 10.2 (8.5;12.0) |
| Turkey, Ankara* | 342 | 9.09 (9.03;9.14) | 17.7 (17.4;18.1) | 52 | 17.0 (12.0;22.0) | 21 | 6.9 (3.5;10.3) | 160 | 10.9 (9.8;12.0) |
Full sample;
*Stratified random subsample: 100 children with and 100 children without wheeze were invited.
Random sample: a random sample without stratification by wheeze was invited.
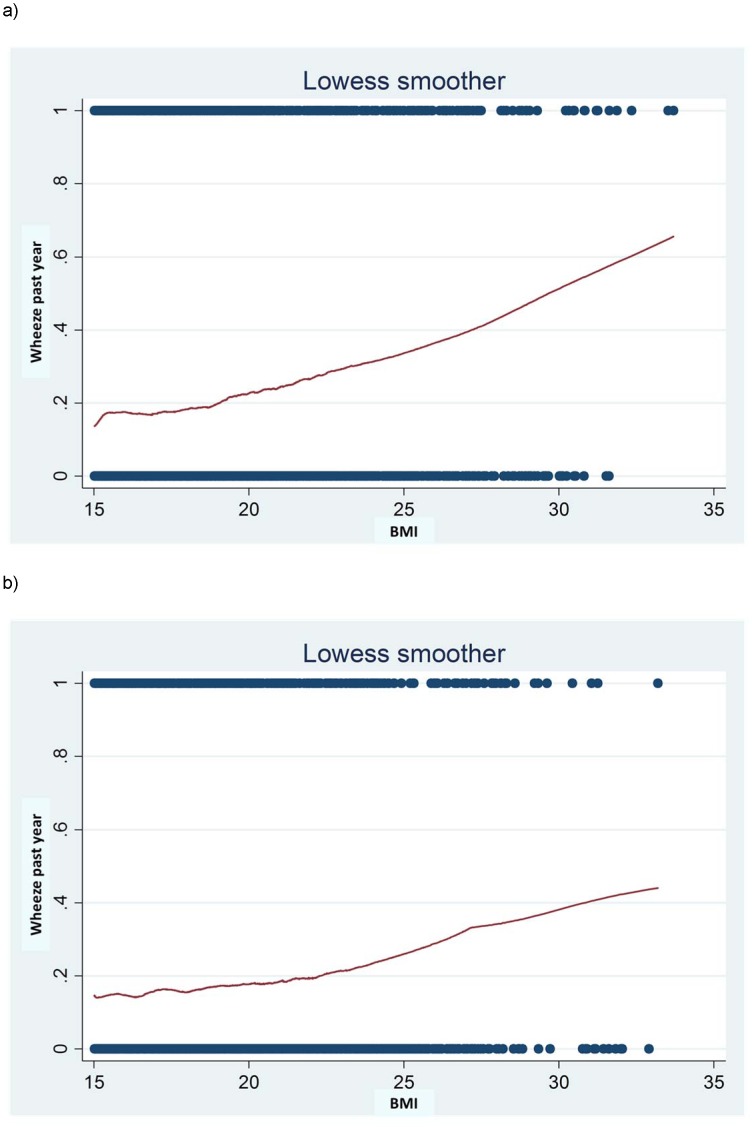
Figure 1 shows the relation between BMI and proportion of wheeze in the past year including children from all centres. A monotonic increase of wheeze with increase in BMI was seen with no deviation from linearity. There was a slight indication for a stronger slope for boys than for girls. When we calculated combined ORs for all centres from meta-analysis, there were no statistically significant differences between boys and girls. We therefore report results for boys and girls combined, but also provide additional sex-specific results in Table S7 in File S2.
Figure 1. Lowess plots i.e. smoothed curves of the average proportion of wheeze in the past year in relation to BMI (a: boys; b: girls).
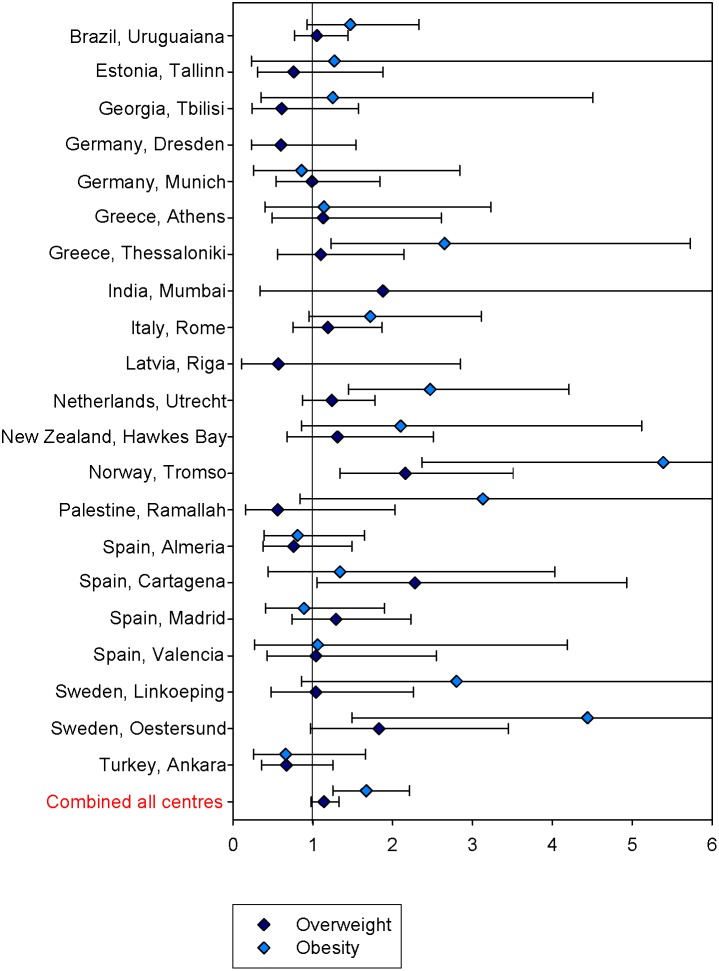
The combined OR for wheeze in the past year in relation to overweight and to obesity was 1.14 (95% confidence interval (CI): 0.98; 1.33) and 1.67 (95%-CI: 1.25; 2.21), respectively (Table 2). The greater part of the centres showed positive ORs with wheeze for overweight and even more so for obesity (Figure 2). There was a stronger association in affluent centres than in non-affluent centres (Tables 2 and 3). This difference between affluent and non-affluent centres was statistically significant for overweight (p = 0.024) where no association was seen in the non-affluent countries, but not for obesity (p = 0.267). Within affluent European centres, there was an indication of a stronger association with obesity among centres from North-Central Europe (2.84, 95%-CI: 1.67; 4.82) as opposed to Southern Europe, but much less so for overweight (1.31, 95%-CI: 0.91; 1.89, Table S3 in File S2).
Table 2. Association of wheeze, respiratory and allergy related outcomes and eczema symptoms with overweight and obesity: combined estimates from meta-analysis, adjusted for sex.
| Overweight | Obese | ||||||
| OR (95%-CI) | N | n* | OR (95%-CI) | N | n* | ||
| Wheeze past year | All centres | 1.14 (0.98;1.33) | 9658 | 21 | 1.67 (1.25;2.21) | 7274 | 18 |
| Affluent | 1.27 (1.08;1.50) | 7623 | 14 | 1.80 (1.28;2.53) | 5869 | 13 | |
| Nonaffluent | 0.86 (0.65;1.16) | 2035 | 7 | 1.34 (0.91;1.98) | 1405 | 5 | |
| Wheeze with exercise | All centres | 1.24 (1.01;1.52) | 7221 | 17 | 1.65 (1.19;2.29) | 5995 | 16 |
| Affluent | 1.33 (1.06;1.66) | 5580 | 12 | 1.58 (1.04;2.38) | 4801 | 12 | |
| Nonaffluent | 0.88 (0.47;1.63) | 1641 | 5 | 1.64 (1.00;2.70) | 1194 | 4 | |
| Wheeze without exercise | All centres | 1.10 (0.80;1.52) | 5359 | 13 | 1.20 (0.81;1.77) | 4323 | 12 |
| Affluent | 1.15 (0.76;1.73) | 3870 | 9 | 1.12 (0.74;1.67) | 3329 | 9 | |
| Nonaffluent | 0.98 (0.49;1.98) | 1489 | 4 | 1.48 (0.31;6.99) | 994 | 3 | |
| Sleep disturbing wheeze | All centres | 1.36 (0.99;1.86) | 7447 | 15 | 2.15 (1.21;3.82) | 6338 | 13 |
| Affluent | 1.30 (0.77;2.18) | 5981 | 11 | 2.27 (1.16;4.44) | 5566 | 11 | |
| Nonaffluent | 1.44 (0.93;2.21) | 1466 | 4 | 2.04 (0.46;9.09) | 772 | 2 | |
| Dry cough at night | All centres | 1.13 (1.00;1.29) | 9498 | 21 | 1.28 (1.07;1.54) | 7729 | 19 |
| Affluent | 1.21 (1.05;1.40) | 7487 | 14 | 1.34 (1.08;1.65) | 6341 | 14 | |
| Nonaffluent | 0.93 (0.73;1.19) | 2011 | 7 | 1.32 (0.63;2.79) | 1388 | 5 | |
| Woken with shortness of breath | All centres | 1.01 (0.84;1.20) | 4221 | 14 | 1.35 (0.89;2.04) | 2949 | 11 |
| Affluent | 1.06 (0.76;1.48) | 2417 | 8 | 1.18 (0.62;2.24) | 1816 | 7 | |
| Nonaffluent | 0.94 (0.59;1.50) | 1804 | 6 | 1.70 (0.80;3.61) | 1133 | 4 | |
| Severe wheeze | All centres | 1.29 (1.02;1.64) | 8525 | 20 | 1.69 (1.19;2.38) | 6599 | 19 |
| Affluent | 1.37 (1.03;1.80) | 6968 | 14 | 1.99 (1.31;3.03) | 5338 | 13 | |
| Nonaffluent | 0.93 (0.43;2.04) | 1557 | 6 | 1.17 (0.73;1.88) | 1261 | 6 | |
| Severe wheeze among wheezers | All centres | 1.14 (0.87;1.50) | 1562 | 18 | 1.08 (0.77;1.51) | 1298 | 17 |
| Affluent | 1.09 (0.81;1.47) | 1066 | 13 | 1.08 (0.71;1.65) | 878 | 12 | |
| Nonaffluent | 1.12 (0.57;2.20) | 496 | 5 | 1.10 (0.59;2.07) | 420 | 5 | |
| BHR yes/no | All centres | 1.05 (0.88;1.26) | 5056 | 19 | 1.09 (0.81;1.47) | 3916 | 16 |
| Affluent | 1.13 (0.93;1.36) | 4135 | 14 | 1.10 (0.80;1.50) | 3515 | 14 | |
| Nonaffluent | 0.57 (0.32;1.01) | 921 | 5 | 1.05 (0.42;2.63) | 401 | 2 | |
| Skin prick test | All centres | 1.04 (0.91;1.18) | 7891 | 21 | 1.13 (0.91;1.42) | 6194 | 18 |
| Affluent | 1.03 (0.90;1.19) | 5954 | 14 | 1.07 (0.87;1.33) | 5004 | 14 | |
| Nonaffluent | 1.05 (0.77;1.44) | 1937 | 7 | 1.49 (0.61;3.67) | 1190 | 4 | |
| Total IgE $ | All centres | 0.95 (0.80;1.12) | 4451 | 15 | 1.07 (0.82;1.39) | 3709 | 15 |
| Affluent | 0.97 (0.81;1.15) | 4144 | 13 | 1.07 (0.81;1.39) | 3571 | 14 | |
| Nonaffluent | 0.76 (0.40;1.44) | 307 | 2 | Only one centre left | |||
| Rhinitis | All centres | 0.99 (0.88;1.11) | 9522 | 21 | 1.19 (0.90;1.56) | 7746 | 19 |
| Affluent | 0.95 (0.83;1.09) | 7506 | 14 | 1.07 (0.79;1.45) | 6358 | 14 | |
| Nonaffluent | 1.11 (0.87;1.41) | 2016 | 7 | 1.71 (0.94;3.11) | 1388 | 5 | |
| Rhinitis with wheeze | All centres | 1.10 (0.93;1.32) | 7161 | 21 | 1.73 (1.26;2.38) | 5379 | 18 |
| Affluent | 1.12 (0.91;1.38) | 5752 | 14 | 1.65 (1.10;2.46) | 4426 | 13 | |
| Nonaffluent | 1.06 (0.76;1.48) | 1409 | 7 | 1.99 (1.24;3.19) | 953 | 5 | |
| Rhinitis without wheeze | All centres | 0.99 (0.86;1.13) | 7878 | 21 | 1.13 (0.85;1.51) | 6243 | 18 |
| Affluent | 0.96 (0.83;1.12) | 6408 | 14 | 1.03 (0.75;1.42) | 5274 | 13 | |
| Nonaffluent | 1.07 (0.80;1.43) | 1470 | 7 | 1.56 (0.79;3.08) | 969 | 5 | |
| Reported eczema past year | All centres | 1.19 (1.02;1.39) | 9376 | 20 | 1.45 (0.94;2.24) | 7471 | 18 |
| Affluent | 1.26 (1.06;1.50) | 7494 | 14 | 1.62 (0.95;2.79) | 6236 | 13 | |
| Nonaffluent | 0.98 (0.71;1.35) | 1882 | 6 | 0.84 (0.49;1.47) | 1235 | 5 | |
| Reported eczema without wheeze | All centres | 1.18 (0.99;1.41) | 7667 | 19 | 1.24 (0.88;1.75) | 5900 | 15 |
| Affluent | 1.26 (1.03;1.54) | 6290 | 13 | 1.34 (0.93;1.92) | 5260 | 12 | |
| Nonaffluent | 0.94 (0.64;1.37) | 1377 | 6 | 1.01 (0.35;2.94) | 640 | 3 | |
| Eczema by examination | All centres | 1.36 (0.98;1.87) | 6348 | 14 | 1.18 (0.70;2.00) | 4292 | 11 |
| Affluent | 1.39 (0.98;1.98) | 5505 | 10 | 1.19 (0.69;2.06) | 4154 | 10 | |
| Nonaffluent | 1.06 (0.40;2.81) | 843 | 4 | Only one centre left | |||
| Examined eczema without wheeze | all centres | 1.27 (0.88;1.82) | 5366 | 14 | 2.07 (1.03;4.17) | 2656 | 7 |
| affluent | 1.29 (0.85;1.96) | 4802 | 10 | 2.25 (1.08;4.68) | 2565 | 6 | |
| nonaffluent | 1.15 (0.39;3.40) | 564 | 4 | Only one centre left | |||
| Mean change (%) (95%-CI) | N | n* | Mean change (%) (95%-CI) | N | n* | ||
| FEV1/FVC&# | All centres | −0.90 (−1.33;−0.47) | 5439 | 9 | −2.46 (−3.84;−1.07) | 4746 | 9 |
| Affluent | −0.94 (−1.43;−0.44) | 4970 | 7 | −1.59 (−2.31;−0.86) | 4324 | 7 | |
| Nonaffluent | −0.79 (−2.28;0.70) | 469 | 2 | −5.39 (−9.46;−1.31) | 422 | 2 | |
| Mean change (ml) | N | n* | Mean change (ml) | N | n* | ||
| FEV1 & | All centres | 80.84 (48.09;113.58) | 7926 | 21 | 80.26 (52.79;107.74) | 6544 | 19 |
| Affluent | 61.34 (42.69;79.99) | 6498 | 14 | 82.96 (49.28;116.64) | 5586 | 14 | |
| Nonaffluent | 123.40 (37.86;208.95) | 1428 | 7 | 53.80 (−38.70;146.30) | 958 | 5 | |
| Mean change (ml) | N | n* | Mean change (ml) | N | n* | ||
| FVC & | All centres | 105.57 (84.57;126.56) | 5494 | 9 | 172.05 (125.68;218.42) | 4790 | 9 |
| Affluent | 105.73 (83.97;127.49) | 5023 | 7 | 157.17 (113.64;200.69) | 4367 | 7 | |
| Nonaffluent | 103.30 (23.49;183.12) | 471 | 2 | 265.25 (137.21;393.29) | 423 | 2 | |
*Number of centres.
Dichotomized at 4.17 kU/l.
Adjusted for age, sex and height.
Exclusion of children with difference of FEV1 and FVC>200 ml or difference = −12 000 ml.
Figure 2. Odds ratios with 95%-confidence intervals (adjusted for sex) for the association of wheeze in the past year with overweight and obesity.
Table 3. Association of overweight and obesity with wheeze and effect modification: OR with 95%-confidence intervals adjusted for sex.
| OR | N | n(centres) | OR | N | n(centres) | P-value for difference | |
| Affluent countries | Nonaffluent countries | ||||||
| Overweight | 1.27 (1.08;1.50) | 7623 | 14 | 0.86 (0.65;1.16) | 2035 | 7 | 0.024 |
| Obese | 1.80 (1.28;2.53) | 5869 | 13 | 1.34 (0.91;1.98) | 1405 | 5 | 0.27 |
| Boys | Girls | ||||||
| Overweight | 1.26 (1.05;1.53) | 4801 | 20 | 0.98 (0.71;1.34) | 4628 | 19 | 0.17 |
| Obese | 1.94 (1.45;2.60) | 3768 | 18 | 1.47 (1.08;2.00) | 3068 | 16 | 0.20 |
| Atopics | Nonatopics | ||||||
| Overweight | 1.22 (0.95;1.56) | 2095 | 20 | 1.05 (0.87;1.27) | 5328 | 20 | 0.35 |
| Obese | 1.65 (1.14;2.39) | 1403 | 14 | 1.70 (1.08;2.66) | 3537 | 16 | 0.92 |
| Parental allergic disease | No parental allergic disease | ||||||
| Overweight | 1.10 (0.86;1.41) | 4753 | 18 | 1.21 (0.98;1.49) | 4496 | 19 | 0.57 |
| Obese | 1.97 (1.49;2.62) | 3757 | 17 | 1.48 (1.05;2.08) | 3190 | 15 | 0.20 |
| Parental asthma | No parental asthma | ||||||
| Overweight | 1.18 (0.84;1.67) | 1126 | 16 | 1.14 (0.96;1.36) | 8078 | 20 | 0.86 |
| Obese | 1.88 (1.13;3.12) | 772 | 12 | 1.65 (1.24;2.19) | 6066 | 17 | 0.66 |
| BHR | No BHR | ||||||
| Overweight | 1.02 (0.73;1.44) | 1126 | 18 | 1.12 (0.84;1.49) | 3918 | 19 | 0.69 |
| Obese | 1.37 (0.82;2.28) | 825 | 14 | 1.94 (1.19;3.16) | 2607 | 14 | 0.34 |
| Mother smoked in pregnancy | No maternal smoking in pregnancy | ||||||
| Overweight | 1.21 (0.87;1.68) | 1427 | 10 | 1.16 (0.98;1.37) | 6873 | 19 | 0.85 |
| Obese | 1.93 (1.24;2.99) | 1171 | 10 | 1.52 (1.19;1.94) | 5063 | 16 | 0.35 |
| Fresh fruits intake* | No fresh fruits intake | ||||||
| Overweight | 1.20 (0.94;1.53) | 4233 | 15 | 0.88 (0.52;1.49) | 414 | 10 | 0.29 |
| Obese | 1.53 (1.04;2.25) | 3227 | 13 | 1.35 (0.59;3.07) | 252 | 7 | 0.78 |
| Med score first tertile§ | Med score second and third tertile | ||||||
| Overweight | 1.33 (1.03;1.72) | 1918 | 13 | 1.15 (0.81;1.64) | 1841 | 13 | 0.51 |
| Obese | 1.50 (1.05;2.14) | 1449 | 11 | 1.41 (0.95;2.10) | 1380 | 11 | 0.82 |
| Physical activity + | Physical activity− | ||||||
| Overweight | 1.32 (1.01;1.74) | 2656 | 13 | 0.93 (0.63;1.38) | 817 | 11 | 0.15 |
| Obese | 1.69 (1.04;2.76) | 2075 | 12 | 1.07 (0.61;1.88) | 676 | 11 | 0.23 |
| Urban$ | Rural$ | ||||||
| Overweight | 1.08 (0.81;1.45) | 3401 | 18 | 1.22 (0.91;1.62) | 2095 | 15 | 0.58 |
| Obese | 1.24 (0.92;1.66) | 2262 | 13 | 2.05 (1.22;3.45) | 1470 | 13 | 0.10 |
| Low birth weight& | Normal birth weight& | ||||||
| Overweight | 1.65 (0.89;3.06) | 417 | 11 | 1.09 (0.83;1.42) | 2746 | 17 | 0.23 |
| Obese | 2.54 (0.86;7.50) | 159 | 4 | 1.35 (0.82;2.23) | 1996 | 14 | 0.30 |
| High birthweight& | Normal birth weight& | ||||||
| Overweight | 1.40 (1.08;1.82) | 1816 | 15 | 1.09 (0.83;1.42) | 2746 | 17 | 0.18 |
| Obese | 2.10 (1.49;2.98) | 1508 | 15 | 1.35 (0.82;2.23) | 1996 | 14 | 0.15 |
Physical activity: 2 times a week or more often; *Fresh fruits are consumed 1 time per week or more often; §Med.Score: higher scores for more frequent consumption of vegetables (raw green and cooked), fruit, fruit juice and fish, and lower scores for more frequent consumption of meat, burger and fizzy drinks (for details see File S1 and S2); &Low birthweight: less than 2500 g, normal: 2500–3499 g, high: more than 3500 g; $urban: suburban, with few parks or gardens or urban with no parks or gardens, rural: rural, open spaces or fields nearby or suburban, with many parks or gardens.
When looking at wheeze characteristics, we found that wheeze with exercise was statistically significantly associated with overweight and obesity, especially in affluent centres, whereas wheeze in the absence of exercise was not. Children reporting more often dry cough at night and those woken with tightness of chest were more often obese. Effects were most pronounced in North-Central Europe (Table S3 in File S2). There was no strong evidence for an association with children woken with shortness of breath. Also, among wheezers, there was no indication of more severe wheeze in overweight or obese children.
Except for affluence in overweight children, none of the tested potential effect modifiers gave a statistically significant result (Table 3). For some factors, there was a slight indication with p-values ≤0.2 and with a statistically significant positive associations only in one stratum, namely in physically active children, children with high birth weight and boys. For rural and urban surroundings, effect estimates were both positive but higher for rural (p = 0.1).
None of the three objective measures of BHR, skin prick tests, and total IgE was conclusively associated with overweight or obesity (Table 2). ORs were close to one for skin prick test and total IgE, and, while there was an indication of a positive association with BHR in Northern-Central Europe, an inverse association with overweight was observed in non-affluent centres. There was a statistically significantly lower FEV1/FVC in relation with overweight and obesity in affluent centres and even more so with obesity in non-affluent centres. FEV1 and FVC adjusted for age, sex and height, on the contrary, showed an increase of approximately 80 ml (overweight and obese) for FEV1 and 106 ml (overweight) and 172 ml (obese) for FVC.
Regarding other allergic disease symptoms (Table 2 and Table S4 in File S2), rhinitis was not associated with overweight and obesity. For eczema (reported and examined), there was an association with overweight and obesity in affluent countries but not in non-affluent countries. The figures for examined eczema in obese children should be viewed with caution due to the reduced number of centres (and children) in the analysis. Looking at respiratory symptoms (Table 4 and Table S5 in File S2), the association of coughed up phlegm with overweight and obesity was observed mostly when occurring in the absence of a cold or frequently among children from affluent countries. All associations were moderately stronger in children who also reported wheeze at the same time (Table S6 in File S2).
Table 4. Association of cough and phlegm with overweight and obesity: combined estimates from meta-analysis adjusted for sex.
| Overweight | Obese | |||||
| OR (95%-CI) | N | n* | OR (95%-CI) | N | n* | |
| Coughed up phlegm with colds | ||||||
| All centres | 1.11 (0.94;1.30) | 7646 | 17 | 1.26 (0.96;1.66) | 6251 | 16 |
| Affluent | 1.19 (1.00;1.43) | 5824 | 11 | 1.32 (0.95;1.83) | 4908 | 11 |
| Nonaffluent | 0.96 (0.77;1.21) | 1822 | 6 | 0.86 (0.37;1.99) | 1343 | 5 |
| Coughed up phlegm with colds without wheeze | ||||||
| All centres | 1.03 (0.84;1.26) | 6255 | 17 | 1.25 (0.98;1.59) | 4949 | 15 |
| Affluent | 1.06 (0.82;1.38) | 4946 | 11 | 1.27 (0.95;1.70) | 4158 | 11 |
| Nonaffluent | 0.94 (0.72;1.22) | 1309 | 6 | 1.11 (0.71;1.74) | 791 | 4 |
| Coughed up phlegm without colds | ||||||
| All centres | 1.17 (0.98;1.40) | 7541 | 17 | 1.64 (1.15;2.34) | 5840 | 14 |
| Affluent | 1.30 (0.99;1.71) | 5755 | 11 | 1.73 (1.10;2.71) | 4859 | 11 |
| Nonaffluent | 1.12 (0.80;1.58) | 1786 | 6 | 1.13 (0.38;3.30) | 981 | 3 |
| Coughed up phlegm without colds without wheeze | ||||||
| All centres | 1.07 (0.83;1.37) | 5375 | 13 | 1.86 (1.32;2.63) | 4418 | 10 |
| Affluent | 1.10 (0.78;1.56) | 4176 | 8 | 1.88 (1.27;2.80) | 3846 | 8 |
| Nonaffluent | 1.13 (0.63;2.05) | 1199 | 5 | 1.78 (0.76;4.17) | 572 | 2 |
| Congested in chest/coughed up phlegm frequently § | ||||||
| All centres | 1.44 (1.15;1.79) | 6935 | 15 | 2.28 (1.70;3.07) | 5482 | 13 |
| Affluent | 1.70 (1.29;2.25) | 5363 | 10 | 2.53 (1.62;3.93) | 4546 | 10 |
| Nonaffluent | 0.91 (0.49;1.68) | 1572 | 5 | 2.01 (1.26;3.22) | 936 | 3 |
| Congested in chest/coughed up phlegm frequently § without wheeze | ||||||
| All centres | 1.52 (1.00;2.30) | 4947 | 11 | 2.71 (1.76;4.17) | 3824 | 9 |
| Affluent | 1.87 (1.24;2.82) | 3915 | 7 | 2.93 (1.55;5.52) | 3270 | 7 |
| Nonaffluent | 0.85 (0.46;1.60) | 1032 | 4 | 2.65 (1.28;5.50) | 554 | 2 |
*Number of centres.
On 4 or more days a week for as much as 3 months a year.
Discussion
This large international multi-centre study, including both affluent and non-affluent countries, provides evidence that excess weight is associated with asthmatic symptoms as well as eczema, and rhinitis in combination with asthmatic symptoms. No association was observed for objective measures of allergic disease such as BHR, skin prick test, or total IgE. BMI was inversely associated with FEV1/FVC, an indicator of airway obstruction.
In our study, we found a linear association between BMI and wheeze indicating a dose-response relationship. However, other authors observed a U-shaped BMI-asthma relationship, when applying BMI categories [19]. We found a stronger association with wheeze for overweight in affluent countries and within Europe an indication for a stronger association with obesity in Northern-Central than in Southern European centres. A dose response pattern was also found for coughed up phlegm. Stronger associations due to more power could be attributed to higher prevalence of weight excess in western countries [20].
A lower FEV1/FVC was observed in overweight and obese children from both, affluent and non-affluent countries. However, it should be acknowledged that data on FVC was only available in a subset. Literature examining the association between obesity and lung function is conflicting. Height has been identified as the important independent predictor of spirometric variables and the therefore resulting collinearity of FEV1 and FVC with BMI limits the interpretation of these parameters on their own [21]. Our observation that the effects of obesity on FEV1/FVC are related to an increase in FVC, rather than a decrease in FEV1 has therefore to be interpreted with caution. In a certain proportion of children, BMI may reflect increased muscular mass and be correlated with higher lung volumes and therefore influence the observed relationship with FVC and FEV1, respectively [22], while this effect is cancelled out in the ratio between them. Nevertheless, the reduction of FEV1/FVC but no increase of BHR could suggest that overweight and obesity are not related to the common asthma phenotype associated with BHR. Indeed, there is cumulating evidence that asthma is a heterogeneous disease with different phenotypes and potential different pathological mechanisms [23], [24]. Obesity and asthma are believed to share common genetic determinates [25] and it has been suggested that obesity results in a distinct asthma phenotype [26], characterized by more severe disease, with increased exacerbation, poorer asthma control and steroid responsiveness. In our study, wheeze with exercise, dry cough at night, woken at night with tightness of chest and coughed up phlegm without a cold were found more frequently among overweight and obese children. This could reflect differential patterns of asthma phenotypes between normal weight as opposed to overweight/obese children. The stronger association of wheeze with overweight/obesity in affluent countries, in particular countries from Northern-Central Europe, may possibly reflect an increased prevalence of an obesity-related asthma phenotype.
In our study, the association between excess weight and wheeze was not related to atopic status. This contradicts some previous reports on stronger associations for non-atopic asthma, but is in line with the observations that have not found an effect modification by atopy [2]. Consistent with the literature, we found no evidence that overweight and obesity is associated with allergic sensitization [27]. Our observation of mixed results for BHR in affluent countries and non-affluent countries fits with the heterogeneous results from former publications [10], [19], [28]. For reported eczema we observed increased prevalence among obese children with asthma symptoms in agreement with cross-sectional and longitudinal studies [12], [29], and the data for clinical examination of eczema seem to corroborate these results.
We did not find strong evidence for an association between overweight and obesity and allergic disease, since only rhinitis in combination with wheeze and none of the objective measures for allergy was associated with overweight and obesity. This is in line with other studies including objective markers [29] suggesting a non-eosinophil inflammatory mechanism is associated with asthma. Obesity is thought to be linked with asthma by obesity-related systemic inflammation, which could promote exaggerated responses to environmental triggers [1]. Obesity is associated with low-grade inflammation and adipokines, which have been found to be related to asthma symptoms [30].
In our study, the association of overweight and obesity with asthma symptoms did not differ between girls and boys. In previous cross-sectional and longitudinal studies, gender-differences have been reported in some [8], [11], [29] but not in other studies [2], [9], [12], [27], [29].
We observed stronger associations between overweight and asthma in affluent and in particular Northern-Central European countries than in non-affluent countries. Differences of asthma prevalence according to affluence status are well established [31]. Lifestyle and standards of living are suggested to contribute to these disparities, and may also reflect partly different structures of residual confounding as indicated by former ISAAC II publications on breastfeeding [32], diet [33], infections [34], and dampness [35]. The existence of different asthma phenotypes [24] may also contribute to the observed pattern. Epidemiological studies in adults and also children revealed ethnic differences in fat deposits [36] which can also apply in different relationships of the fat mass and fat free mass in children. The differences could contribute to geographic changes in the associations of BMI with asthma and allergic diseases.
Several possible limitations of the study need to be considered. Parental reporting on disease symptoms, in particular for asthma, could have been influenced by obesity, since in adults over-diagnosis of asthma has been matter of concern [30]. In our study, however, the positive associations between obesity and wheeze were also present when considering lung function. Residual confounding could have affected the associations. However, by further adjustment for dietary factors such as fruit and vegetable intake, Mediterranean diet score or physical activity the associations between obesity and asthma symptoms did not change. Other comorbid conditions related to obesity could have influenced the occurrence of asthma [37]. As we investigated a number of outcomes, we cannot exclude the possibility of a sporadic chance finding among the findings which are, however, quite consistent in their overall pattern. In large worldwide studies, a difficulty is that information may not be comparable across geographical regions and therefore covariates may not reflect exactly the same underlying confounders. This may have limited our ability to find and adjust for relevant confounders, so that we cannot exclude fully the possibility of residual confounding. On the other hand the presence of quite consistent associations across these geographical regions is reassuring, decreasing the probability that the overall result is due to residual confounding, only.
Further strengths of the study are the use of the standardized ISAAC questionnaires and methodology in all centres and the inclusion of non-affluent countries. Another strength is that BMI has been measured according to a standard protocol extending the work from ISAAC Phase Three which was largely based on reported values [12]. Furthermore, we were able to investigate standardized objective measurements for lung function and allergic disease in a large international study. However, due to the cross-sectional study design reverse causation cannot be completely excluded.
Conclusion
Our observations in a large international child population strengthen previous reports that overweight and obesity are associated with wheeze and asthma in childhood as well as objective evidence of airways obstruction. No other objective markers of respiratory and allergic disorders were involved. The significance of these observations needs to be confirmed in prospective studies and experimental trials.
Supporting Information
Contains detailed information of additional outcomes.
(DOC)
Additional Tables: Table S1: Mean and prevalence of investigated outcomes with 95% confidence interval. Table S2: Test for confounding: results from fully adjusted model including all potential factors tested. Table S3: Association of wheeze and related symptoms with overweight and obesity: combined estimates from meta-analysis, adjusted for sex. Table S4: Association of respiratory and allergy related outcomes and eczema with overweight and obesity, adjusted for sex. Table S5: Association of cough and phlegm with overweight and obesity: combined estimates from meta-analysis adjusted for sex. Table S6: Association of overweight and obesity with respiratory and allergy related outcomes and eczema in the absence/presence of wheeze: combined estimates with 95%-confidence intervals from meta-analysis adjusted for sex. Table S7: Association of respiratory and allergy related outcomes and eczema with overweight and obesity: analysis by sex.
(DOC)
Acknowledgments
We wish to thank all children, parents, teachers, field workers and lab workers for their enormous contributions to this collaborative study. ALK generously provided reagents for field work in several low income countries without charge.
The ISAAC Phase Two Study group consists of:
The ISAAC Phase Two Coordinating and Data Centre: S.K. Weiland † (Director), G. Büchele, C. Dentler, A. Jaensch, P. Rzehak, G. Weinmayr (1).
Phase Two Principal Investigators: A. Priftanji, A. Shkurti, J. Simenati, E. Grabocka, K. Shyti, S. Agolli, A. Gurakuqi (2); R.T. Stein, M. Urrutia de Pereira, M.H. Jones, P.M. Pitrez (3); P.J. Cooper, M. Chico (4); Y.Z. Chen (5); N.S Zhong (6); C.K.W. Lai (7); G.W.K. Wong (8); M-A. Riikjärv, T. Annus (9); I. Annesi-Maesano (10); M. Gotua, M. Rukhadze, T. Abramidze, I. Kvachadze, L. Karsanidze, M. Kiladze, N. Dolidze (11); W. Leupold (12); U. Keil (13); E. von Mutius (14); S.K. Weiland † (1); P. Arthur †, E. Addo-Yobo (15); C. Gratziou (16); K. Priftis (17); A. Papadopoulou, C. Katsardis (18); J. Tsanakas, E. Hatziagorou, F. Kirvassilis (19); M. Clausen (20); J.R. Shah, R.S. Mathur, R.P. Khubchandani, S. Mantri (21); F. Forastiere, R. Di Domenicantonio, M. De Sario, S. Sammarro (22); R. Pistelli, M.G. Serra, G. Corbo, C.A. Perucci (23); V. Svabe, D. Sebre, G. Casno, I. Novikova, L. Bagrade (24); B. Brunekreef (25); D. Schram (26); G. Doekes, P.H.N. Jansen-van Vliet (27); N.A.H. Janssen (28); F.J.H. Aarts, G. de Meer (29); J. Crane, K. Wickens (30); D. Barry (31); W. Nystad (32); R. Bolle (33); E. Lund (34); J. Batlles Garrido, T. Rubi Ruiz, A. Bonillo Perales, Y. Gonzalez Jiménez, J. Aguirre Rodriguez, J. Momblan de Cabo, A. Losilla Maldonado, M. Daza Torres (35); L. García-Marcos (36); A. Martinez Torres, J.J. Guillén Pérez, A. Piñana López, S. Castejon Robles (37); G. García Hernandez, A. Martinez Gimeno, A.L. Moro Rodríguez, C. Luna Paredes, I. Gonzalez Gil (38); M.M. Morales Suarez-Varela, A. Llopis González (39); A. Escribano Montaner (40); M. Tallon Guerola (41); L. Bråbäck, A. Sandin (42); M. Kjellman (43); L. Nilsson, X-M. Mai (44); Y. Saraçlar, A. Tuncer, C. Saçkesen, V. Sumbulglu, P. Geyik, C. Kocabas (45); S. Kuyucu (46); D.P. Strachan, B. Kaur (47); N. El-Sharif, F. Barghuthy, S. Abu Huij, M. Qlebo (48); B. Nemery (49).
The ISAAC Steering Committee: N. Aït-Khaled (50); H.R. Anderson (51); N. Pearce (52); D.P. Strachan* (47); C. Flohr* (53); H. Williams (54); F. Forastiere* (22); M.I. Asher, P. Ellwood, A. Stewart and E. Mitchell (55); J. Crane (30); R. Beasley (56); B. Björkstén (57); B. Brunekreef* (25); S. Foliaki (58); L. García-Marcos (36); E. von Mutius* (14); U. Keil (13); S.K. Weiland*†, G. Weinmayr* (1); C.K.W. Lai (7); G.W.K. Wong (8); J. Mallol (59); S. Montefort (60); J. Odhiambo† (61); and C. Robertson (62).
* also members of the ISAAC Phase Two Steering Group, † deceased.
Lead author for the ISAAC Phase Two Study Group: D.P. Strachan (sgjd950@sgul.ac.uk).
1 Institute of Epidemiology and Medical Biometry, Ulm University, Ulm, Germany;
2 Service of Allergology & Clinical Immunology, UHC “Mother Teresa”, Tirana, Albania;
3 Pediatric Pulmonary Unit, Department of Pediatrics, Pontificia Universidade Catolica RS, Porto Alegre, Brazil;
4 Laboratorio de Investigaciones, Hospital Pedro Vicente Maldonado, Quito, Ecuador;
5 Clinical and Education Centre for Asthma, Capital Institute of Pediatrics, Beijing, China;
6 Guangzhou Medical College, Guangzhou, China;
7 Department of Medicine and Therapeutics, The Chinese University of Hong Kong, Hong Kong, China;
8 Department of Paediatrics, Prince of Wales Hospital, Chinese University of Hong Kong, Hong Kong, China;
9 Tallinn Children’s Hospital, Tallinn, Estonia;
10 INSERM, Faculte de Medecine St-Antoine, Universite Pierre et Marie Curie, Paris, France;
11 Center of Allergy & Immunology, Tbilisi, Georgia;
12 Klinik und Poliklinik für Kinder- und Jugendmedizin, Universitätsklinikum Carl Gustav Carus, Dresden, Germany;
13 Institut für Epidemiologie und Sozialmedizin, Westfälische Wilhelms Universität, Muenster, Germany;
14 Dr. von Haunersches University Children's Hospital, Ludwig-Maximilians University, Munich, Germany;
15 Department of Child Health, Komfo Anokye Teaching Hospital (KATH), Kintampo, Ghana;
16 Pulmonary and Critical Care, Medical School, Athens University, Asthma and Allergy Centre, Eugenidio Hospital, Athens, Greece;
17 Allegiology and Pneumonology, 3rd Department of Pediatrics, “Attikon” Hospital, Athens University, Athens, Greece;
18 Pedetrician Asthma and Allergy Unit, Pediatric Department, ‘‘KAT’’ General Hospital, Athens, Greece;
19 Paediatric Respiratory Unit, 3rd Department of Paediatrics, Hippokration General Hospital, Thessaloniki, Greece;
20 Department of Paediatrics, Landspitalinn Hákskólasjúkrahus, Reykjavik, Iceland;
21 Jaslok Hospital & Research Centre, Mumbai, India;
22 Department of Epidemiology, Rome E Health Authority, Rome, Italy;
23 Università Cattolica Sacro Cuore, Servizio Fisiopatologia Respiratoria, Complesso Integrato Columbus, Rome, Italy;
24 Childrens Clinical Hospital, Riga Stradins University, Riga, Latvia;
25 Institute for Risk Assessment Sciences, Universiteit Utrecht, Utrecht, Netherlands;
26 Environmental and Occupational Health Group, University of Utrecht, Utrecht, Netherlands;
27 Environmental and Occupational Health Group, Wageningen, Netherlands;
28 Harvard School of Public Health, Department of Environmental Health, Boston, USA;
29 Dept. Environmental Sciences, WAU Dept. of Epidemiology, Environmental & Occupational Health, Wageningen, Netherlands;
30 Wellington Asthma Research Group, University of Otago, Wellington, New Zealand;
31 Hawke's Bay Regional Hospital, Hawkes Bay, New Zealand;
32 Section of Epidemiology, Department of Health & Society, Norwegian Institute of Public Health, Oslo, Norway;
33 University Hospital Northern Norway, Tromso, Norway;
34 University of Tromso, Tromso, Norway;
35 Institute of Pediatric Neumology Unit, Torrecardenas Hospital, Almeria, Spain;
36 ‘Virgen de la Arrixaca’ University Children’s Hospital, University of Murcia, Murcia, Spain;
37 Direccion de Salud Area II, University of Murcia, Murcia, Spain;
38 Seccion de Neumologia y Alergia Pediatricas, Hospital Universitario 12 de Octubre, Madrid, Spain;
39 Department of Preventive Medicine, Faculty of Pharmacy, University of Valencia and Dr. Peset University Hospital, Valencia, Spain;
40 Pediatric Respiratory Unit, Clinic University Hospital, Valencia, Spain;
41 Pediatric Department, Dr. Peset University Hospital, Valencia, Spain;
42 Mid Sweden Research and Development Centre, Sundsvall Hospital, Sundsvall, Sweden;
43 Department of Pediatrics, Linkoeping University Hospital, Linkoeping, Sweden;
44 Department of Molecular and Clinical Medicine, Division of Pediatrics, University Hospital, Linkoeping; Sweden;
45 Pediatrics Allergy and Asthma Unit, Hacettepe University, Faculty of Medicine, Ankara, Turkey;
46 Department of Pediatrics, University of Mersin, Mersin, Turkey;
47 Division of Community Health Sciences, St George's, University of London, London, UK;
48 Medical Sciences-Epidemiology, Alquds University, Faculty of Public Health, Jerusalem, Palestine;
49 Kathoilic University of Leuven, Leuven, Belgium;
50 Asthma Division, Union Internationale Contre la Tuberculose et les Maladies Respiratoires, Paris, France;
51 Division of Community Health Sciences, St George's, University of London and MRC Centre for Environment and Health, Cranmer Terrace, Tooting, London, United Kingdom;
52 Faculty of Epidemiology and Public Health, London School of Hygiene and Tropical Medicine, London, UK;
53 Department of Paediatric Allergy & Dermatology, St John’s Institute of Dermatology, St Thomas’ Hospital, London, United Kingdom;
54 Centre for Evidence-based Dermatology, Nottingham University Hospital's Queen's Medical Centre Campus, Nottingham, United Kingdom;
55 Department of Paediatrics: Child and Youth Health, Faculty of Medical and Health Sciences, The University of Auckland, Auckland, New Zealand;
56 Medical Research Institute of New Zealand, Wellington, New Zealand;
57 National Institute of Environmental Medicine/IMM, Division of Respiratory Physiology, Karolinska Institutet, Stockholm, Sweden;
58 Massey University, Wellington Campus, Wellington, New Zealand;
59 Department of Pediatric and Respiratory Medicine, Hospital CRS El Pino, University of Santiago de Chile (USACH), Santiago, Chile;
60 Department of Medicine, University of Malta, Malta;
61 Centre for Respiratory Diseases Research, Kenya Medical Research Institute (KEMRI), Village Market, Kenya;
62 Murdoch Children’s Research Institute, Melbourne, Australia.
Data Availability
The authors confirm that, for approved reasons, some access restrictions apply to the data underlying the findings. Data are from the ISAAC Phase Two study centre who may be contacted via gudrun.weinmayr@uni-ulm.de. In order to obtain data, the ISAAC Executive needs to consent on behalf of the individual study centres. The data of all centres are contained in the international dataset created and maintained by the data centre in Ulm - therefore data requests can be responded to directly by the University of Ulm, there is no need to contact the centres individually.
Funding Statement
Coordination and central laboratory analyses of the European centres were funded by the Fifth Framework Program of European Commission, [grant number QLK4-CT-1999-01288]; Funding of local studies: Almeria: Fondo de Investigacion Sanitaria (grant code 00/1092E); Ankara*: Scientific and Technical Research council of Turkey (grant code SPAG-2237), Treatment and Research Foundation of Turkey for Allergy, Asthma and Immunology, and the Research Foundation of Hacettepe University Faculty of Medicine; Athens: the Thorax Foundation Research Centre, Greece; Cartagena: Fondo de Investigacion Sanitaria (grant code 00/1092E). Créteil: French Institute of Health and Medical Research (Institut National de la Santé et de la Recherche Médicale (INSERM) (grant codes IDS 337/4D001D and 737/69480), Ministère de l'Emploi et de la Solidarité (grant code 227/7HL02D), Mutuelle Générale de l'Education Nationale (grant code 257/8PL01F) and Agence de l'Environnement et de la Maitrise de l'Energie ADEME/PRIMEQUAL 96 (grant code FJ012B); Dresden: German Ministry of Education and Research (01 EE 9411-3); Hastings: Health Research Council of New Zealand, Asthma and Respiratory Foundation of New Zealand, and Hawkes Bay Medical Research Foundation; Kintampo*: Linköping: the Swedish Foundation for Health Care Sciences and Allergy Research; Madrid: Fondo de Investigacion Sanitaria (grant code 00/1092E); Mumbai*: Jaslok Hospital & Research Centre; Munich: German Ministry of Education and Research (01 EE 9411-3); Östersund: the Swedish Foundation for Health Care Sciences and Allergy Research; Pichincha province: Wellcome Trust; Pôrto Alegre: Rudolf und Clothilde Eberhardt Foundation, Ulm, Germany; Ramallah: Al-Quds University, Directorate General for International Cooperation and Belgian Technical Cooperation; Riga*; Rome: Lazio Regional Health Authority; Tallinn*; Tbilisi*; Thessaloníki: the Thorax Foundation Research Centre, Greece; Tirana*; Utrecht: Dutch Ministries of the Environment, of Health and of Transport, Rotterdam, the Netherlands; Valencia: Fondo de Investigacion Sanitaria (grant code 00/1092E); West Sussex: South Thames National Health Service Regional Research and Development project SPGS 573. *: centres supported, at least in part, by European members of the ISAAC Steering Committee. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Tantisira KG, Weiss ST (2001) Childhood infections and asthma: at the crossroads of the hygiene and Barker hypotheses. Respir Res 2(6):324–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Von Mutius E, Schwartz J, Neas LM, Dockery D, Weiss ST (2001) Relation of body mass index to asthma and atopy in children: the National Health and Nutrition Examination Study III. Thorax 56(11):835–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chatzi L, Torrent M, Romieu I, Garcia-Esteban R, Ferrer C, et al. (2007) Diet, wheeze, and atopy in school children in Menorca, Spain. Pediatr Allergy Immunol 18(6):480–5. [DOI] [PubMed] [Google Scholar]
- 4. Visness CM, London SJ, Daniels JL, Kaufman JS, Yeatts KB, et al. (2010) Association of childhood obesity with atopic and nonatopic asthma: results from the National Health and Nutrition Examination Survey 1999–2006. J Asthma 47(7):822–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sin DD, Sutherland ER (2008) Obesity and the lung: 4. Obesity and asthma. Thorax 63(11):1018–23. [DOI] [PubMed] [Google Scholar]
- 6. Flaherman V, Rutherford GW (2006) A meta-analysis of the effect of high weight on asthma. Arch Dis Child 91(4):334–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gilliland FD, Berhane K, Islam T, McConnell R, Gauderman WJ, et al. (2003) Obesity and the risk of newly diagnosed asthma in school-age children. Am J Epidemiol 158(5):406–15. [DOI] [PubMed] [Google Scholar]
- 8. Hancox RJ, Milne BJ, Poulton R, Taylor DR, Greene JM, et al. (2005) Sex differences in the relation between body mass index and asthma and atopy in a birth cohort. Am J Respir Crit Care Med 171(5):440–5. [DOI] [PubMed] [Google Scholar]
- 9. Guerra S, Wright AL, Morgan WJ, Sherrill DL, Holberg CJ, et al. (2004) Persistence of asthma symptoms during adolescence: role of obesity and age at the onset of puberty. Am J Respir Crit Care Med 170(1):78–85. [DOI] [PubMed] [Google Scholar]
- 10. Scholtens S, Wijga AH, Brunekreef B, Kerkhof M, Postma DS, et al. (2010) Maternal overweight before pregnancy and asthma in offspring followed for 8 years. Int J Obes (Lond) 34(4):606–13. [DOI] [PubMed] [Google Scholar]
- 11. Matricardi PM, Grüber C, Wahn U, Lau S (2007) The asthma-obesity link in childhood: open questions, complex evidence, a few answers only. Clin Exp Allergy 37(4):476–84. [DOI] [PubMed] [Google Scholar]
- 12. Mitchell EA, Beasley R, Björkstén B, Crane J, García-Marcos L, et al. (2013) The association between BMI, vigorous physical activity and television viewing and the risk of symptoms of asthma, rhinoconjunctivitis and eczema in children and adolescents: ISAAC Phase Three. Clin Exp Allergy 43(1):73–84. [DOI] [PubMed] [Google Scholar]
- 13. Weiland SK, Björkstén B, Brunekreef B, Cookson WOC, von Mutius E, et al. (2004) Phase II of the International Study of Asthma and Allergies in Childhood (ISAAC II): rationale and methods. Eur Respir J 24(3):406–12. [DOI] [PubMed] [Google Scholar]
- 14. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320(7244):1240–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Richardson DB, Rzehak P, Klenk J, Weiland SK (2007) Analyses of case-control data for additional outcomes. Epidemiology 18(4):441–5. [DOI] [PubMed] [Google Scholar]
- 16.Chambless L, Boyle K (1985) Maximum Likelihood methods for complex sample data: Logistic Regression and discrete proportional hazards models. Commun Statist-Theor Meth. 14th ed 1377–92.
- 17. Büchele G, Genuneit J, Weinmayr G, Björkstén B, Gehring U, et al. (2010) International variations in bronchial responsiveness in children: findings from ISAAC phase two. Pediatr Pulmonol 45(8):796–806. [DOI] [PubMed] [Google Scholar]
- 18.The World Bank; 2011. Available at: http://data.worldbank.org/.
- 19. Dixon AE, Holguin F, Sood A, Salome CM, Pratley RE, et al. (2010) An official American Thoracic Society Workshop report: obesity and asthma. Proc Am Thorac Soc 7(5):325–35. [DOI] [PubMed] [Google Scholar]
- 20. Wang Y, Lobstein T (2006) Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes 1(1):11–25. [DOI] [PubMed] [Google Scholar]
- 21. Pistelli R, Brancato G, Forastiere F, Michelozzi P, Corbo GM, et al. (1992) Population values of lung volumes and flows in children: effect of sex, body mass and respiratory conditions. Eur Respir J 5(4):463–70. [PubMed] [Google Scholar]
- 22. Jensen ME, Gibson PG, Collins CE, Wood LG (2013) Lean mass, not fat mass, is associated with lung function in male and female children with asthma. Pediatr Res 75(1–1):93–8. [DOI] [PubMed] [Google Scholar]
- 23. Wenzel SE (2012) Asthma phenotypes: the evolution from clinical to molecular approaches. Nat Med 18(5):716–25. [DOI] [PubMed] [Google Scholar]
- 24. Weinmayr G, Keller F, Kleiner A, du Prel JB, Garcia-Marcos L, et al. (2013) Asthma phenotypes identified by latent class analysis in the ISAAC phase II Spain study. Clin Exp Allergy 43(2):223–32. [DOI] [PubMed] [Google Scholar]
- 25. Melén E, Himes BE, Brehm JM, Boutaoui N, Klanderman BJ, et al. (2010) Analyses of shared genetic factors between asthma and obesity in children. J Allergy Clin Immunol 126(3):631–7.e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lugogo NL, Kraft M, Dixon AE (2010) Does obesity produce a distinct asthma phenotype? J Appl Physiol 108(3):729–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wickens K, Barry D, Friezema A, Rhodius R, Bone N, et al. (2005) Obesity and asthma in 11–12 year old New Zealand children in 1989 and 2000. Thorax 60(1):7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mai XM, Nilsson L, Axelson O, Bråbäck L, Sandin A, et al. (2003) High body mass index, asthma and allergy in Swedish schoolchildren participating in the International Study of Asthma and Allergies in Childhood: Phase II. Acta Paediatr 92(10):1144–8. [PubMed] [Google Scholar]
- 29. Murray CS, Canoy D, Buchan I, Woodcock A, Simpson A, et al. (2011) Body mass index in young children and allergic disease: gender differences in a longitudinal study. Clin Exp Allergy 41(1):78–85. [DOI] [PubMed] [Google Scholar]
- 30. Aaron SD, Vandemheen KL, Boulet L-P, McIvor RA, Fitzgerald JM, et al. (2008) Overdiagnosis of asthma in obese and nonobese adults. CMAJ 179(11):1121–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Von Hertzen LC, Haahtela T (2004) Asthma and atopy - the price of affluence? Allergy 59(2):124–37. [DOI] [PubMed] [Google Scholar]
- 32. Nagel G, Büchele G, Weinmayr G, Björkstén B, Chen Y-Z, et al. (2009) Effect of breastfeeding on asthma, lung function and bronchial hyperreactivity in ISAAC Phase II. Eur Respir J 33(5):993–1002. [DOI] [PubMed] [Google Scholar]
- 33. Nagel G, Weinmayr G, Kleiner A, Garcia-Marcos L, Strachan DP, et al. (2010) Effect of diet on asthma and allergic sensitisation in the International Study on Allergies and Asthma in Childhood (ISAAC) Phase Two. Thorax 65(6):516–22. [DOI] [PubMed] [Google Scholar]
- 34. Nagel G, Weinmayr G, Flohr C, Kleiner A, Strachan DP, et al. (2012) Association of pertussis and measles infections and immunizations with asthma and allergic sensitization in ISAAC Phase Two. Pediatr Allergy Immunol 23(8):737–46. [DOI] [PubMed] [Google Scholar]
- 35. Weinmayr G, Gehring U, Genuneit J, Büchele G, Kleiner A, et al. (2013) Dampness and moulds in relation to respiratory and allergic symptoms in children: results from Phase Two of the International Study of Asthma and Allergies in Childhood (ISAAC Phase Two). Clin Exp Allergy 43(7):762–74. [DOI] [PubMed] [Google Scholar]
- 36. Camhi SM, Bray GA, Bouchard C, Greenway FL, Johnson WD, et al. (2011) The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: sex and race differences. Obesity (Silver Spring) 19(2):402–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. De Groot EP, Duiverman EJ, Brand PLP (2010) Comorbidities of asthma during childhood: possibly important, yet poorly studied. Eur Respir J 36(3):671–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Contains detailed information of additional outcomes.
(DOC)
Additional Tables: Table S1: Mean and prevalence of investigated outcomes with 95% confidence interval. Table S2: Test for confounding: results from fully adjusted model including all potential factors tested. Table S3: Association of wheeze and related symptoms with overweight and obesity: combined estimates from meta-analysis, adjusted for sex. Table S4: Association of respiratory and allergy related outcomes and eczema with overweight and obesity, adjusted for sex. Table S5: Association of cough and phlegm with overweight and obesity: combined estimates from meta-analysis adjusted for sex. Table S6: Association of overweight and obesity with respiratory and allergy related outcomes and eczema in the absence/presence of wheeze: combined estimates with 95%-confidence intervals from meta-analysis adjusted for sex. Table S7: Association of respiratory and allergy related outcomes and eczema with overweight and obesity: analysis by sex.
(DOC)
Data Availability Statement
The authors confirm that, for approved reasons, some access restrictions apply to the data underlying the findings. Data are from the ISAAC Phase Two study centre who may be contacted via gudrun.weinmayr@uni-ulm.de. In order to obtain data, the ISAAC Executive needs to consent on behalf of the individual study centres. The data of all centres are contained in the international dataset created and maintained by the data centre in Ulm - therefore data requests can be responded to directly by the University of Ulm, there is no need to contact the centres individually.