Abstract
A 30-year-old, 39 weeks pregnant, multiparous woman with single fetus, attended our obstetric clinic with complete cervical dilation in intractable mentum anterior presentation. The fetus was delivered by caesarean section with vertical uterine incision under general anaesthesia and lithotomy position. After surgery, examination of the vagina revealed multiple, serious tears with severe haemorrhage. Vaginal bleeding could not be controlled by sutures and concurrently uterine atony developed, which could not be controlled with medical treatment. Owing to intractable bleeding from uterus and vagina, a complete tamponade system was used. After the instillation of the uterine balloon with 500 mL and vaginal balloon with 300 mL liquid, the bleeding was controlled. The estimated blood loss was 3200 mL. The vaginal wound healed well during the postoperative 2 weeks. A complete tamponade system may be an effective treatment method for treatment of postpartum haemorrhage owing to vaginal lacerations and uterine atony.
Background
The most frequent reasons for postpartum haemorrhage are uterine atony, genital tractus lacerations, abnormal placentation, placenta retention and coagulation disorders.1
It is difficult to control and suture haemorrhages arising from multiple mucosal lacerations. In some cases, it may not be possible to determine a submucosal bleeding vein. Therefore, it becomes difficult to prevent formation of haematomas. When haematomas occur, they generally required complex management.2 3
We have presented a postpartum haemorrhage case due to serious vaginal lacerations and uterine atony and management of the case using a complete balloon system.
Case presentation
A 30-year-old, 39 weeks pregnant woman with single living fetus, on mentum anterior presentation with complete cervical dilation was admitted to our obstetric clinic. Owing to delivery arrest, the fetus was delivered by emergent caesarean section with vertical uterine incision under lithotomy position and general anaesthesia. The abdomen was entered by median incision under the umbilicus. A 3600 g, living female neonate was delivered. The uterine incision was closed with No 1 polyglactin. After surgery, severe vaginal haemorrhage from mucosal lacerations was observed. Repair of the vaginal lacerations could not be performed with compression sutures in the form of eight; also, concurrently, uterine atony developed. A combination of uterine massage and oxytocic medications did not control the haemorrhage and the haemodynamic stability of the patient deteriorated. Systolic blood pressure was measured as 30 mm/Hg with tachycardiac (170–180 bpm) pulse rate. There was no urination during these interventions. During the restoration of hypovolaemia, a complete tamponade system with uterine and vaginal balloon (The Belfort-Dildy Obstetrical Tamponade System, trade named the ebbComplete Tamponade System (Glenveigh Medical, LLC, Chattanooga, Tennessee, USA)) was placed in the cavities. The system was inserted vaginally. After the instillation of the uterine balloon with 500 mL and of the vaginal balloon with 300 mL of liquid (figure 1), the haemorrhage was brought under control. The estimated blood loss was 3200 mL. During these procedures, 4 units of erythrocyte suspension and 3 units of fresh frozen plasma (FFP) were transfused. After transfusion of blood products, haemoglobin (Hb) value was 6.1 g/dL. During the postoperative period, 4 additional units of erythrocyte suspension were replaced and Hb and haematocrit values reached 10.2 g/dL and 29.8%, respectively. During the first postoperative 24 h, hourly urination (mL), arterial blood pressure (mm Hg) and body temperature (°C) were measured. Volume replacement and oxitocic medications were regulated according to central venous pressure value and vital findings of the patient.
Figure 1.
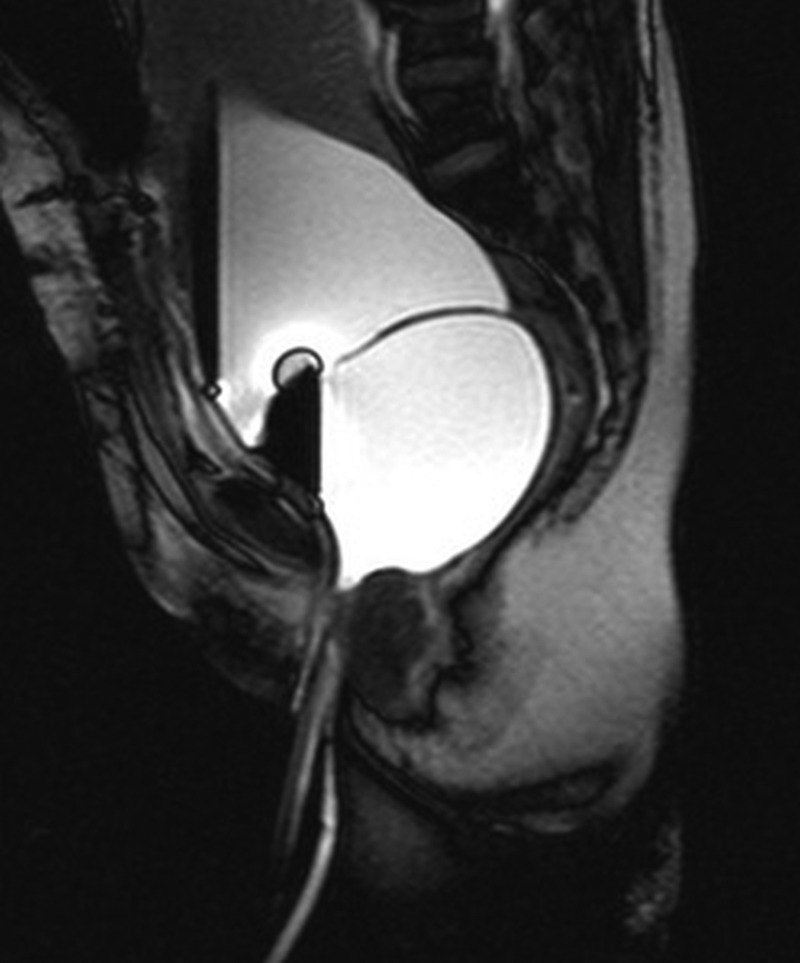
MRI of the Belfort-Dildy obstetrical tamponade system in the uterus and vagina.
A written informed and signed consent form was obtained.
Treatment
In total 40 IU oxytocin in 500 mL normal saline was administered intravenously at a 125 mL/h infusion rate. Methyl ergonovin maleat (0.5 mg) was administered intravenously.
Uterus massage and bimanual compression of the uterus was applied.
A complete tamponade system with uterine and vaginal balloons (The Belfort-Dildy Obstetrical Tamponade System) was inserted.
Anaemia was corrected by 8 U erythrocyte suspension transfusions and 3 U FFP; the haemoglobin value increased to 10.2 g/dL.
Outcome and follow-up
At 48 h postoperatively, the balloon was deflated and withdrawn. No uterine or vaginal bleeding was observed.
Postoperatively, the vaginal wounds healed well.
Discussion
We have presented the successful conservative management of a case of concomitant severe vaginal lacerations and uterine atony using a complete balloon tamponade system. A previous case successfully treated by our team using an intravaginal foley catheter-condom for treating a vaginal haematoma as a result of postpartum vaginal lacerations gave us the idea for handling the current case.
Postpartum bleeding depending on uterine atony occurs because of inability of the uterus to be contracted, and to close the veins in the myometrium. Towards the end of pregnancy, uteroplacental circulation receives 1/5 of the heartbeat (approximately 1000 mL/min) and postpartum bleeding even for a short period can threaten the life of the patient. The majority of postpartum bleedings develop due to uterine atony. The rate of birth canal injuries, including lacerations on genital tractus, inversion and rupture is approximately 20%.4
Vaginal balloons were used successfully in postpartum vaginal haematoma case series. However, these balloon systems are not basically designed for vaginal use. In order to enable the balloon to remain in the vagina, it needs to be packed with sutures.5 6 A newly developed medical tool for conservative management of postpartum uterine bleeding, The Belfort-Dildy Obstetrical Tamponade System, trade named the ebb Complete Tamponade System (Glenveigh Medical, LLC, Chattanooga, Tennessee, USA) was approved by the US Food and Drug Administration (FDA) in 2010. In this system, the upper uterine balloon can be inflated up to 750 mL and the lower vaginal balloon can be inflated up to 300 mL.7 Ghirardini et al8 suggested that a vaginal balloon tamponade may be applied easily and rapidly for treatment of a postpartum vaginal haematoma. Despite their high inflation pressure, they emphasised that the patient did not report vaginal pain during the presence of the balloons, as in our case. Our patient merely admitted mild abdominal pain due to uterine involution.
Yoong et al6 presented a patient with severe vaginal bleeding after vaginal delivery via vacuum extraction. They reported that haemorrhage control could not be performed with compression sutures in the form of eight. After insertion of 100 mL inflated Bakri balloon into the vagina, the bleeding was controlled and removal of balloon was performed after 24 h.
In some cases due to oedematous vaginal mucosa and difficulty of suturation for haemorrhage control, vaginal balloon tamponade application may be appropriate.8 In our case, vaginal repair could not be performed to completion because of severe bleeding stemming from the atonic uterus. Owing to rapid, progressive deterioration of the haemodynamics of the patient, complete balloon tamponade insertion was performed.
Severe bleeding from vaginal lacerations may cause hypovolaemic shock in a short time. In such cases, concomitant uterine atony may be catastrophic for the hypovolaemia. In cases with postpartum intractable bleeding due to atony and lacerations, a complete tamponade system may be an effective treatment method.
Learning points.
Complete balloon tamponade is a successful conservative treatment for severe vaginal laceration together with uterine atony.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ahonen J, Stefanovic V, Lassila R. Management of post-partum haemorrhage. Acta Anaesthesiol Scand 2010;54:1164–78. [DOI] [PubMed] [Google Scholar]
- 2.Mukherjee S, Arulkumaran S. Post-partum haemorrhage. Obstet Gynaecol Reprod Med 2009;19:121–26. [Google Scholar]
- 3.Ridgway LE. Puerperal emergency. Vaginal and vulvar hematomas. Obstet Gynecol Clin North Am 1995;22:275–82. [PubMed] [Google Scholar]
- 4.Prendiville W, Elbourne D. Care during the third stage of labour. In: Chambers I, Enkin M, Keirse M, eds. Effective care in pregnancy and childbirth, Vol 2 Oxford: Oxford University Press, 1989:1145–70. [Google Scholar]
- 5.Tattersall M, Braithwaite W. Balloon tamponade for vaginal lacerations causing severe postpartum haemorrhage. BJOG 2007;114:647–8. [DOI] [PubMed] [Google Scholar]
- 6.Yoong W, Ray A, Philip SA. Balloon tamponade for postpartum vaginal lacerations in a woman refusing blood transfusion. Int J Gynaecol Obstet 2009;106:261. [DOI] [PubMed] [Google Scholar]
- 7.Dildy GA., III Postpartum hemorrhage: new management options. Clin Obstet Gynecol 2002;45:330–44. [DOI] [PubMed] [Google Scholar]
- 8.Ghirardini G, Alboni C, Mabrouk M. Use of balloon tamponade in management of severe vaginal postpartum hemorrhage and vaginal hematoma: a case series. Gynecol Obstet Invest 2012;74:320–3. [DOI] [PubMed] [Google Scholar]


