Abstract
Aims
To undertake a systematic review and meta-analysis of randomized controlled trials concerned with the impact of community pharmacist-led interventions on blood pressure control in patients with hypertension.
Methods
Eight electronic databases were searched up to 30 November 2013, with no start date (Web of Science, Embase, The Cochrane Library, Medline Ovid, Biomed Central, Biosis Citation Index, CINAHL, PsycINFO). All studies included were randomized controlled trials involving patients with hypertension, with or without cardiovascular-related co-morbidities, with difference in blood pressure as an outcome. Data collected included the study design, baseline characteristics of study populations, types of interventions and outcomes. The Cochrane tool was used to assess risk of bias.
Results
From 340 articles identified on initial searching, 16 randomized controlled trials (3032 patients) were included. Pharmacist-led interventions were patient education on hypertension, management of prescribing and safety problems associated with medication, and advice on lifestyle. These interventions were associated with significant reductions in systolic [11 studies (2240 patients); −6.1 mmHg (95% confidence interval, −3.8 to −8.4 mmHg); P < 0.00001] and diastolic blood pressure [11 studies (2246 patients); −2.5 mmHg (95% confidence interval, −1.5 to −3.4 mmHg); P < 0.00001].
Conclusions
Community pharmacist-led interventions can significantly reduce systolic and diastolic blood pressure. These interventions could be useful for improving clinical management of hypertension.
Keywords: hypertension, meta-analysis, pharmacists, randomized controlled trial
What is Already Known about this Subject
Hypertension is considered to be one of the most important treatable risk factors for cardiovascular disease.
Research suggests that reduction of systolic or diastolic blood pressure is associated with a decreased risk of coronary heart disease and stroke.
Recent systematic reviews and meta-analyses pooling observational studies and randomized controlled trials have suggested important contributions of community pharmacists in the management of hypertension in a range of healthcare settings.
What this Study Adds
This systematic review and meta-analysis confined to randomized controlled trials provides evidence that community pharmacists can make a clinically important contribution to the management of hypertension in patients with or without associated cardiovascular co-morbidities.
Introduction
Despite benefits of blood pressure control for reducing risk of stroke and coronary heart disease 1,2 and other serious cardiovascular events 3, hypertension continues to be poorly controlled in the community 4. It has been reported that pharmacist-led interventions can lead to significant reductions in blood pressure in patients seen in a range of healthcare settings 5,6, including secondary care, community health clinics and community pharmacies 7,8. However, previous systematic reviews and meta-analysis of blood pressure control have been limited by including very short-term studies 5, by including observational studies 5,6, largely confining outcomes to hypertensive patients with no reported cardiovascular problems including diabetes, kidney disease, stroke, atrial fibrillation, myocardial infarction and/or heart failure 5,6 and by being unclear about the specific role of community pharmacists in improving the management of high blood pressure 8.
Increasingly in clinical practice, patients with hypertension have an associated range of cardiovascular co-morbidities. The aim of this systematic review and meta-analysis was to extend previous assessment of the impact of community pharmacist interventions on blood pressure control by limiting the analysis to randomized controlled trials (RCTs) and by evaluating studies in patients with hypertension with or without cardiovascular co-morbidities. Heterogeneity in pharmacist interventions was minimized by including data only from RCTs, by being specific about the setting for pharmacist intervention, i.e. community pharmacies, and by standardizing the nature of active pharmacist interventions considered as education about hypertension and its treatment, identifying prescribing and safety issues, and lifestyle advice.
Methods
Search strategy for identification of studies
A literature search of published articles, with no start date restrictions, was undertaken in November 2013 in eight electronic health-related databases: MEDLINE, Web of Science, the Cochrane library, EMBASE, Biosis Citation Index and Biomed Central, CINAHL and PsycINFO. Articles were retrieved up to 30 November 2013. Search terms included ‘community pharmacy’, ‘essential hypertension’, ‘hypertension’ OR ‘blood pressure’, ‘randomized controlled trial’ and ‘intervention’ (see Appendix S1 for complete search strategy).
In addition, reference lists were screened of all included articles retrieved at full paper and the first 100 results of this search strategy applied to Google Scholar. We also screened references in a further systematic review and meta-analysis published in April 2014 8 for additional eligible RCTs.
Types of studies
Randomized controlled trials and systematic reviews of RCTs evaluating the clinical impact of community pharmacist interventions on patients with essential hypertension were included. Systematic reviews were searched to identify additional eligible RCTs. Studies that did not specify the types of hypertension were also considered for inclusion provided they met the inclusion criteria. Randomized controlled trials were included if they had a control group receiving standard or usual care, compared with the care in intervention groups.
Types of participants
All participants were adults (18 years or older) participating in an RCT of treatment for their hypertension in community pharmacies. A study was included if it had a minimum of 80% of the population meeting the inclusion criteria for study participants. Studies were also included which had participants with coexisting cardiovascular-related medical conditions (e.g. high cholesterol, diabetes, renal disease and clinical cardiovascular disease, including cerebrovascular disease and peripheral arterial disease).
Types of interventions
Pharmacological interventions were defined as interventions concerning education on drug treatment of blood pressure, advice to patients to improve medication adherence, identifying drug adverse effects and drug prescribing issues, and liaising with prescribers about concerns of drug treatment. Nonpharmacological interventions were defined as those concerning education about hypertension and education about lifestyle, such as advice to patients on healthy lifestyle, including diet, weight management, alcohol consumption and smoking cessation.
Types of outcome measures
Primary outcomes
Reduction in systolic blood pressure and diastolic blood pressure measured in the community pharmacies or at home.
Secondary outcomes
Improvement in adherence to antihypertensive medications measured by tablet count, by pharmacy dispensing records, by use of the four-point Morisky questionnaire and by prescription claims data.
Identification and management of drug-related problems. Drug-related problems were defined as concerns about adverse drug effects expressed by the patient or the pharmacist. Methodology for assessing this was nonstandard across included studies. Inappropriate drug selection or dose was based on pharmacist access to formularies and guidelines; sources for these were not clear across the studies.
Impact on cardiovascular risk factors, i.e. smoking, alcohol consumption, weight, cholesterol levels (in millimoles per litre) and glycated haemoglobin (HbA1c, expressed as a percentage).
Exclusion criteria
The reviewers excluded studies with multidisciplinary interventions in which the pharmacist intervention within the team was not clearly defined, conference proceedings or abstracts only, systematic reviews of RCTs containing <50% of eligible studies, and articles published in languages other than English.
Data extraction, risk of bias and quality assessment
Two reviewers (EC and PS) independently reviewed titles and abstracts of all potentially relevant papers. Papers which met inclusion criteria were retrieved as full papers, and these two reviewers checked each paper for inclusion. Any differences were agreed through discussion or resolved by a third reviewer (DRJS). Reviewer EC independently extracted data, and PS checked all extraction sheets (see Appendix S2 for characteristics of included studies).
Criteria for quality assessment of included systematic reviews were based on those of the NHS Centre for Reviews and Dissemination (CRD) 9. Two reviewers (EC and PS) rated each paper using the Cochrane Risk of Bias tool 10 to assess RCTs on their randomization procedure, allocation concealment, blinding of participants, reporting of incomplete outcome data, selective reporting or any other biases that did not fit into the above-mentioned categories. Other sources of bias explored in this review included the possibility of cross-contamination between study arms, recruitment of participants from a selected population and noncompliance of researchers to the study protocol. For each included study, a risk-of-bias graph and a risk-of-bias summary were generated 10. The use of power calculations was recorded.
Statistical analysis
A narrative overview and analysis of included RCTs and systematic reviews was undertaken and supplemented with further meta-analyses. A cumulative meta-analysis of studies was used to identify changes in blood pressure control over time.
Meta-analyses were undertaken with random-effects models (Rev Man version 5.2; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). Mean difference [standard deviation] and 95% confidence intervals (CIs) were used to estimate effects. Because of differences in study population, sample size and methods of blood pressure measurement, a random-effects model was used, and τ2 recorded. To minimize heterogeneity in the meta-analysis, studies using three similar interventions were used (patient education on disease management, identification and management of prescribing and safety problems associated with antihypertensive medications, and advice on lifestyle). Heterogeneity was measured by Cochrane's test. Statistical heterogeneity beyond that expected through chance was investigated using I2. Heterogeneity was further explored with sensitivity analysis by repeating meta-analysis after excluding a single outlying study and by using both random- and fixed-effect models.
Results
A total of 340 studies were identified (Figure 1), 330 from electronic databases and 10 from reference lists of previous reviews. Fifty-three duplicates were removed. Two hundred and eighty-seven records were screened at title level, with 143 irrelevant titles removed. The remaining 144 records were screened at abstract level. After eliminating abstracts not meeting inclusion criteria, 70 full-text studies were assessed for eligibility. Fifty-four studies did not meet inclusion criteria (Figure 1). Reasons for exclusion included the following: not RCTs; different study settings; systematic reviews containing <50% of eligible studies; intervention not provided by community pharmacists; <80% of study population hypertensive; blood pressure not a study outcome; studies not defining details of community pharmacist roles; and studies with published protocol only. Sixteen RCTs contributed to the systematic review 11–26. Of these, 11 studies were included in the meta-analysis 11,12,14–17,19,21,24–26.
Figure 1.
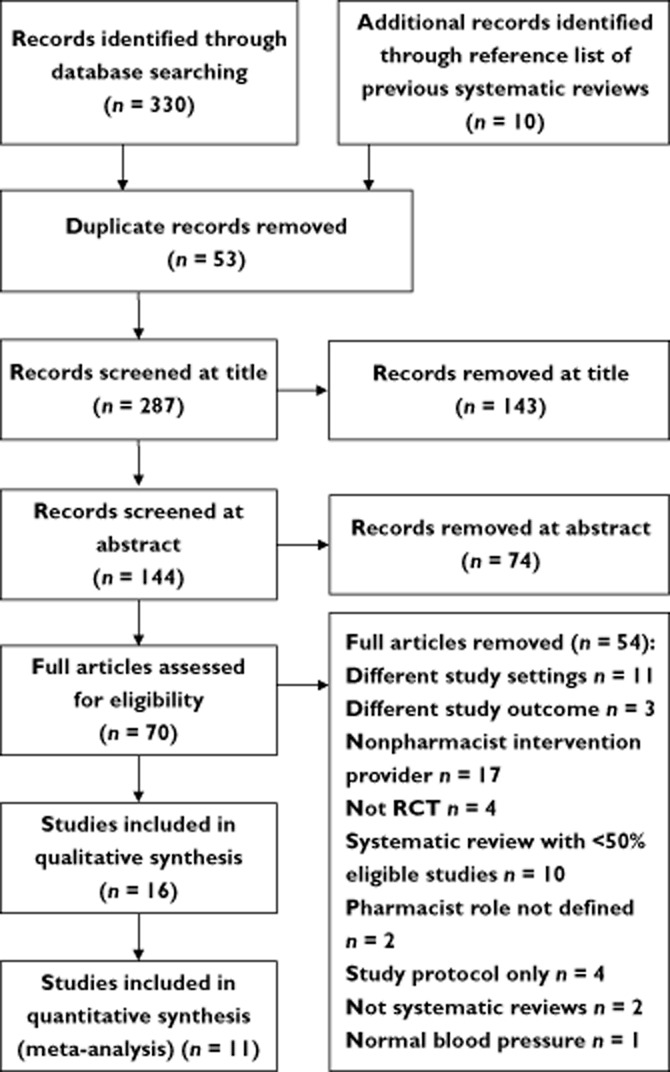
Prisma flow diagram
Study characteristics
All 16 studies included were RCTs conducted in community pharmacies. These trials were conducted in Australia 17, Canada 20,23, Portugal 16, Spain 12,15, Thailand 24, the USA 14,18,19,21,22,25,26 and the UK 11,13. All 16 studies used intervention groups receiving a selection from the following interventions by community pharmacists: patient education on disease management; identification and management of prescribing and safety problems associated with antihypertensive medications; and advice on lifestyle, compared with a control group receiving usual care. No systematic reviews meeting the inclusion criteria were identified.
The duration of intervention ranged from 3 26 to 13 months 15). The studies included 3034 patients, with individual study size ranging from 50 18 to 714 12. Mean age ranged from 53 25 to 72 years 23. Additional medical conditions included dyslipidaemia, diabetes mellitus, heart failure, angina pectoris and atrial fibrillation.
There was heterogeneity among studies for interventions, outcomes, population characteristics, study duration and methods for measuring outcomes. Only three of seven studies that measured adherence to antihypertensive medications reported using a similar assessment method (pill count) 18,21,24. Only four studies reported measuring the impact of pharmacists' interventions on other cardiovascular disease risk factors 12,14,15,17.
Study quality
The quality of included studies assessed by Cochrane Risk of Bias tool is shown in Figure 2. Only three (18%) of 16 studies reported details of allocation concealment 12,20,25. It was unclear in the remaining 13 studies whether they had used adequate allocation concealment. Only four (25%) studies reported using single blinding of participants 15,16,21,25. Only nine (56%) studies reported using power calculations 11,12,14–17,21,24,25.
Figure 2.
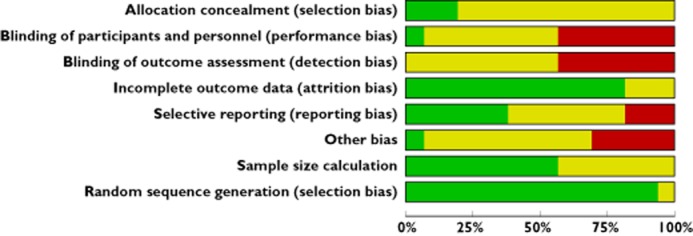
Cochrane risk-of-bias graph 10. Authors' judgements about each risk-of-bias item are presented as percentages across all included studies.  , low risk of bias;
, low risk of bias;  , unclear risk of bias;
, unclear risk of bias;  , high risk of bias
, high risk of bias
Impact of pharmacist interventions on outcome measures
All 16 studies included in this systematic review measured systolic and diastolic blood pressure at baseline and the end of the study. None measured ambulatory blood pressure. In 14 studies, measurements were in the community pharmacy, while in one study, home blood pressure recordings were used 26. One study 13 reported improved blood pressure based on measurements in general practice, but did not report quantitative blood pressure results.
Of these 16 studies, 11 were included in the meta-analysis of effects on systolic (2240 patients) and diastolic blood pressure (2246 patients) 11,12,14–17,19,21,24–26. Absence of quantitative blood pressure data (one study) 13 and limitations in interventions were reasons to exclude the remaining four studies from meta-analysis 18,20,22,23.
Meta-analysis
All 11 studies included in the meta-analysis used three similar interventions, namely patient education on hypertension and the importance of its treatment, identification of drug-related problems and lifestyle advice.
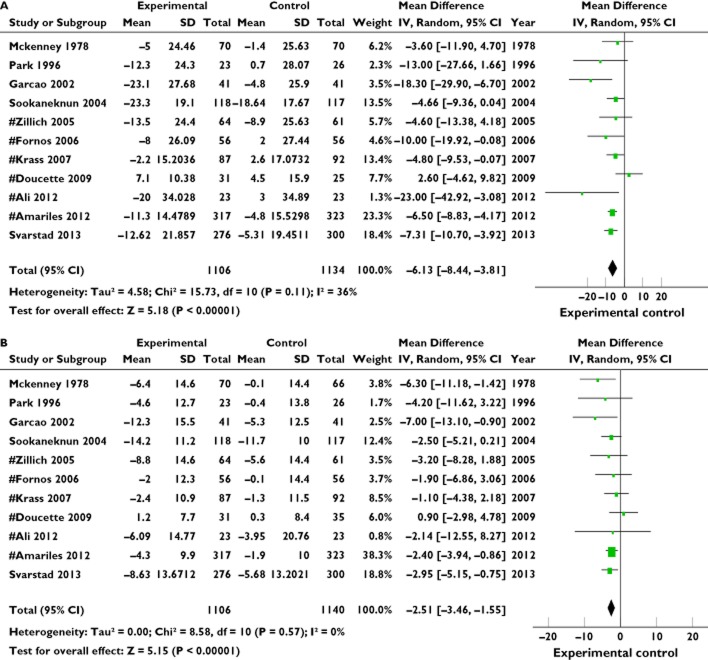
Systolic blood pressure: all subjects
Meta-analysis of data from the 11 studies showed a significant benefit in favour of community pharmacist interventions, with a pooled effect of 6.1 mmHg reduction in systolic blood pressure (95% CI −3.8 to −8.4 mmHg, P < 0.00001) using a random-effect model. Heterogeneity among studies for differences in systolic blood pressure was low to moderate (χ2 = 15.73, d.f. = 10, P = 0.11, I2 = 36%; Figure 3A).
Figure 3.
Forest plot comparisons of experimental (intervention) vs. control groups in 11 studies for systolic blood pressure (A) and diastolic blood pressure (B). #Indicates studies including patients with cardiovascular-related co-morbidities. Mckenney 19, Park 21, Garcao 16, Sookaneknun 24, Zillich 26, Fornos 15, Krass 17, Doucette 14, Ali 11, Amariles 12, Svarstad 25
Diastolic blood pressure: all subjects
Meta-analysis of data from the 11 studies showed a significant benefit in favour of community pharmacist interventions, with a pooled effect of 2.5 mmHg reduction in diastolic blood pressure (95% CI −1.5 to −3.4 mmHg, P < 0.00001) using a random-effect model. There was no heterogeneity among the studies for differences in diastolic pressure (χ2 = 8.58, d.f. = 10, P = 0.57, I2 = 0%; Figure 3B).
Sensitivity meta-analysis for blood pressure effects
Two approaches were used to test the robustness of the results 10. No significant difference was found between the results of fixed-effect model meta-analysis (systolic −6.2 mmHg, 95% CI −4.7 to −7.8 mmHg; diastolic −2.5 mmHg, 95% CI −1.6 to −3.5 mmHg) vs. the above random-effects model analysis. Results of random-effects model meta-analysis after removal of the outlier were similar for systolic (−6.6 mmHg, 95% CI −5.0 to −8.2 mmHg) and diastolic blood pressure (−2.7 mmHg, 95% CI −1.7 to −3.7 mmHg).
Cumulative meta-analysis identified no significant changes over time in the impact of pharmacist interventions on blood pressure control.
Blood pressure effects for five studies on hypertension without cardiovascular problems
Pooled reduction in systolic blood pressure with active interventions in 528 patients without cardiovascular-related co-morbidities vs. 554 control subjects 16,19,21,24,25 was 7.2 mmHg (95% CI −3.6 to −10.8 mmHg, P = 0.004). Heterogeneity was low to moderate (χ2 = 5.91, d.f. = 4, P = 0.21, I2 = 32%).
Pooled reduction in diastolic blood pressure with active interventions in 528 patients without cardiovascular-related co-morbidities vs. 550 control subjects 16,19,21,24,25 was 3.4 mmHg (95% CI −1.9 to −5.0 mmHg, P < 0.00001). There was no significant heterogeneity (χ2 = 3.32, d.f. = 4, P = 0.51, I2 = 0%).
Blood pressure effects for six studies on hypertension with cardiovascular problems
Pooled reduction in systolic blood pressure with active interventions in 578 patients with cardiovascular-related co-morbidities vs. 580 control subjects 11,12,14,15,17,26 was 5.3 mmHg (95% CI −1.7 to −8.9 mmHg, P < 0.0001). Heterogeneity was moderate (χ2 = 9.34, d.f. = 5, P = 0.10, I2 = 46%).
The pooled reduction in diastolic blood pressure with active interventions in patients with cardiovascular-related co-morbidities was 1.9 mmHg (95% CI −0.7 to −3.1 mmHg, n = 578 intervention vs. 590 control subjects, P = 0.002). There was no significant heterogeneity (χ2 = 2.88, d.f. = 5, P = 0.72, I2 = 0%).
This trend for a smaller blood pressure reduction from community pharmacist interventions in patients with co-morbidities in comparison to those without co-morbidities was not significant (systolic difference 1.9 mmHg, 95% CI −3.1 to −6.9 mmHg, P = 0.46; and diastolic difference 1.5 mmHg, 95% CI −0.4 to −3.4 mmHg, P = 0.127).
Problems with blood pressure medications
Pharmacists recorded drug-related problems in five studies. On entry to these studies, 822 medication-related problems were recorded in 337 patients; no medication-related data were recorded in 132 of the control patients. Categories of medication problems included patients not prescribed a relevant antihypertensive medicine, patients not benefiting from effects of medicine(s) and patients experiencing adverse effects from antihypertensive medications 15,16.
Within intervention groups (240 patients, five studies), pharmacists reported resolving 205 of 539 problems (38%) by advice to prescribers and patients.
Medication adherence
Seven studies reported the impact of pharmacist interventions on adherence to antihypertensive medications 13,18,19,22,24–26. Three studies used pill counting, one used pharmacy dispensing records, two used self-reported adherence questionnaires and one study used prescription claims data. One study 13 used a pharmacist-administered questionnaire based on a Medication Adherence Report Scale 27. Another study used self-reported adherence 26 using the four-item Morisky questionnaire 28. Three studies reported an increase in medication adherence in intervention compared with control groups 13,22,24. One study reported increased adherence (P < 0.005) but provided no quantitative data. For the remaining six studies, adherence in intervention groups increased from 203 (56%) to 246 (68%) of 360 participants, and from 190 (59%) to 195 (61%) of 320 participants in the control group. Thus there was an increase in adherence of 43 from 158 poorly adherent subjects in intervention groups and four of 132 poorly adherent subjects in control groups (odds ratio 12.1, 95% CI 4.2–34.6; P < 0.001).
Reduction in cardiovascular risk factors
Three studies reported results for total cholesterol levels 12,15,17. One study 15 reported a reduction in total cholesterol levels by 0.52 mmol l−1 (P < 0.001) in the intervention group. Two studies reported outcomes for low-density lipoprotein-cholesterol 14,15. All these studies reported a mean reduction in low-density lipoprotein-cholesterol for both intervention and control groups. Three studies measured HbA1c % 14,15,17. Two studies reported a mean reduction in HbA1c % by 0.5 and 1.0% in patients in intervention groups 15,17.
Discussion
These findings show that compared with usual blood pressure management, active interventions by pharmacists working in community pharmacies were associated with clinically important improvement in control of hypertension, whether or not associated with cardiovascular co-morbidities. In comparison to patients receiving usual care, both systolic and diastolic pressure decreased and adherence improved, as did control of other cardiovascular risk factors, including both diabetes mellitus and cholesterol.
Previous analyses have assessed the impact of community pharmacist interventions on blood pressure control in hypertensive patients without cardiovascular problems 5,6 or of a wide range of clinical and other pharmacists working within inpatient and outpatient settings 7,8. The present study is the first meta-analysis to evaluate the specific impact of community pharmacist interventions delivered in community pharmacies both in hypertensive patients without cardiovascular problems and in patients with cardiovascular co-morbidities, including dyslipidaemia, diabetes mellitus, chronic kidney disease and clinical vascular disease. Of note, Santschi et al. 8 do not differentiate between the impact of different types of pharmacists working across a range of healthcare settings, including primary care health centres, hospitals, army medical centres, academic health centres, community pharmacies, community-based hypertension clinics and hospital outpatient clinics. Furthermore, in our meta-analysis of 11 community pharmacy-based RCTs, in addition to all four studies in community pharmacies identified by Santschi et al., we include a further seven studies not referenced in that study 8.
The evidence presented in this review together with previous reviews 5–8 provides an important message to health professionals and policy makers about the potential for community pharmacists to ease the burden for physicians in primary and secondary care of chronic disease management in the context of hypertension. The results of this review show that interventions by community pharmacists were associated with clinically important reductions in both systolic and diastolic blood pressure within a wide range of international geographical regions from North America to Europe, South East Asia and Australia.
The improvement in blood pressure control appeared to occur irrespective of the length of intervention, across included studies whose duration ranged from 3 to 13 months. In the meta-analysis, in studies published from 1978 to 2013, there was also no obvious trend in degree of impact on blood pressure by year of publication. Community pharmacists appeared to be similarly effective in improving blood pressure control both for patients with high blood pressure alone 16,19,21,24,25 and for patients with hypertension coupled with serious cardiovascular problems 11,12,14,15,17,26.
The largest category of preventable causes of poor blood pressure control across the studies included in this review appeared to be incorrect use of medicines by prescribers and patients. In the five studies which recorded this information, it was noteworthy that pharmacists reported being able to resolve only 38% of these problems by making suggestions to prescribers and patients, although expertise in resolving these problems is an expected core usual clinical activity of community pharmacists 29. Further work is needed to investigate two major questions arising from this aspect of the meta-analysis. First, how can the initial occurrence of medication-related problems, such as errors of omission and commission, be prevented when prescribing for hypertension and and how can adverse effects from antihypertensive medications be prevented? Second, what would make interventions by community pharmacists more effective, when aiming to resolve medication-related problems? Possible reasons for the high proportion of unresolved medicine-associated problems include time pressure on community pharmacists providing clinical services within busy commercial settings 30 and challenges to effective interprofessional working arrangements between community pharmacists and other clinical practitioners 31.
There were limitations in this review. Although rigorous and systematic, the reviewers did not include unindexed and unpublished research. Studies were of variable quality, with low to moderate heterogeneity for systolic blood pressure. Home blood pressure monitoring was used in only one of studies in this systematic review 26. There is however high-quality evidence from individual RCTs and robust meta-analysis that home blood pressure monitoring resulted in better blood pressure control and greater achievements of blood pressure targets than standard blood pressure monitoring in healthcare systems 32. Furthermore, recent research suggests that home blood pressure monitoring is also a useful adjunct to pharmacist-supported management of hypertension within family doctor centres 33. Further studies using home blood pressure monitoring are needed to discover whether this would have enhanced the already important reductions in blood pressure observed in this meta-analysis. There are well-established lifestyle approaches for improving control of hypertension 34. However, details of lifestyle interventions were unclear in many of the studies in this systematic review, including whether specific advice was on reducing dietary salt, increasing fruit and vegetable intake and objective assessment of impact of this advice, e.g. from measurement of urinary electrolyte excretion. Future studies could, for example, evaluate formal use of established Dietary Approaches to Stop Hypertension Diet approaches 35 within community pharmacist interventions aimed at blood pressure control.
The reductions in systolic and diastolic blood pressure reported in this meta-analysis, if sustained in clinical practice, would have important implications for primary and secondary prevention of cardiovascular morbidity and mortality. For example, evidence from a meta-analysis involving 1 million adults in the USA reported that every 1 mmHg reduction in systolic blood pressure could prevent about 10 000 deaths related to coronary heart disease in the USA each year 3. A further analysis suggests that a sustained 2 mmHg reduction in diastolic blood pressure would be expected to result in a 6% reduction in the risk of coronary heart disease and 15% decrease in stroke 36.
There are international differences in the extent to which community pharmacy services are embedded within usual clinical care of long-term medical conditions. In the National Health Service in the UK, a new contractual framework for community pharmacies was introduced in 2005, with the intention of moving pharmacists towards a more clinical service-oriented role 37. For example, UK community pharmacies can provide Health Checks for people aged 40–74 years. Within these health checks, pharmacists can carry out a full vascular risk assessment and provide advice and support to help to reduce the risk of heart disease, strokes, diabetes and obesity 37.
However, such extensions in activities and services delivered by community pharmacists may conflict with the work of general practice and health professionals working in hospitals. There is a need for formal links to ensure coherence of treatment approaches and evidence-based integration of pharmacy-delivered services with other health services 38.
Conclusions
Effective blood pressure management requires a systematic multidisciplinary approach in the community. Provision of safe and effective medications to patients is a key role of community pharmacists. The findings of this meta-analysis highlight the significant potential benefits of community pharmacist-led interventions in the management of high blood pressure, whether or not associated with significant cardiovascular co-morbidity. These results support a greater involvement of the community pharmacist in the management of hypertension and its treatment.
Future work needed to address the policy implications of pharmacist-led interventions includes cost-effectiveness analysis of these approaches and their sustainability in the long term in clinical practice. Research is also needed into the type, mode and frequency of interventions in relation to differences in age, gender, ethnicity and other variables of potential importance in the selection and response to the management of hypertension.
Competing Interests
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
We thank Dr Peter Kimani for his statistical advice. In addition, we thank Samantha Johnson for her advice on searching the electronic databases and Warwick University library for help in retrieving the studies evaluated in this review.
References
- Collins R, MacMahon S. Blood pressure, antihypertensive drug treatment and the risks of stroke and of coronary heart disease. Br Med Bull. 1994;50:272–298. doi: 10.1093/oxfordjournals.bmb.a072892. [DOI] [PubMed] [Google Scholar]
- Gueyffier F, Bulpitt C, Boissel JP, Schron E, Ekbom T, Fagard R, Casiglia E, Kerlikowske K, Coope J. Antihypertensive drugs in very old people: a subgroup meta-analysis of randomised controlled trials. INDANA Group. Lancet. 1999;353:793–796. doi: 10.1016/s0140-6736(98)08127-6. [DOI] [PubMed] [Google Scholar]
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Collaboration PS. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- World Health Organization; Alwan A. Global Status Report on Non-Communicable Diseases 2010. Geneva: WHO; 2011. Burden, mortality, morbidity and risk factors; pp. 9–31. [Google Scholar]
- Machado M, Bajcar J, Guzzo GC, Einarson TR. Sensitivity of patient outcomes to pharmacist interventions. Part II: systematic review and meta-analysis in hypertension management. Ann Pharmacother. 2007;41:1770–1781. doi: 10.1345/aph.1K311. [DOI] [PubMed] [Google Scholar]
- Morgado MP, Morgado SR, Mendes LC, Pereira LJ, Castelo-Branco M. Pharmacist interventions to enhance blood pressure control and adherence to antihypertensive therapy: review and meta-analysis. Am J Health Syst Pharm. 2011;68:241–253. doi: 10.2146/ajhp090656. [DOI] [PubMed] [Google Scholar]
- Santschi V, Chiolero A, Burnand B, Colosimo AL, Paradis G. Impact of pharmacist care in the management of cardiovascular disease risk factors a systematic review and meta-analysis of randomized trials. Arch Intern Med. 2011;171:1441–1453. doi: 10.1001/archinternmed.2011.399. [DOI] [PubMed] [Google Scholar]
- Santschi V, Chiolero A, Colosimo AL, Platt RW, Taffé P, Burnier M, Burnand B, Paradis G. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc. 2014;3:e000718. doi: 10.1161/JAHA.113.000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHS Centre for Reviews and Dissemination. Undertaking Systematic Reviews of Research on Effectiveness: CRD Guidelines for Those Carrying out or Commissioning Reviews. York: NHS Centre for Reviews and Dissemination, University of York; 1999. CRD Report 4. [Google Scholar]
- Higgins J, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 (Updated March 2011) West Sussex, UK: The Cochrane collaboration; 2011. [Google Scholar]
- Ali M, Schifano F, Robinson P, Phillips G, Doherty L, Melnick P, Laming L, Sinclair A, Dhillon S. Impact of community pharmacy diabetes monitoring and education programme on diabetes management: a randomized controlled study. Diabet Med. 2012;29:326–333. doi: 10.1111/j.1464-5491.2012.03725.x. [DOI] [PubMed] [Google Scholar]
- Amariles P, Sabater-Hernandez D, Garcia-Jimenez E, Rodriguez-Chamorro MA, Prats-Mas R, Marin-Magan F, Galan-Ceballos JA, Jimenez-Martin J, Faus MJ. Effectiveness of dader method for pharmaceutical care on control of blood pressure and total cholesterol in outpatients with cardiovascular disease or cardiovascular risk: EMDADER-CV Randomized Controlled Trial. J Manag Care Pharm. 2012;18:311–323. doi: 10.18553/jmcp.2012.18.4.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blenkinsopp A, Phelan M, Bourne J, Dakhil N. Extended adherence support by community pharmacists for patients with hypertension: a randomised controlled trial. Int J Pharm Pract. 2000;8:165–175. [Google Scholar]
- Doucette WR, Witry MJ, Farris KB, McDonough RP. Community pharmacist-provided extended diabetes care. Ann Pharmacother. 2009;43:882–889. doi: 10.1345/aph.1L605. [DOI] [PubMed] [Google Scholar]
- Fornos JA, Andres NF, Andres JC, Guerra MM, Egea B. A pharmacotherapy follow-up program in patients with type-2 diabetes in community pharmacies in Spain. Pharm World Sci. 2006;28:65–72. doi: 10.1007/s11096-006-9003-0. [DOI] [PubMed] [Google Scholar]
- Garcao JA, Cabrita J. Evaluation of a pharmaceutical care program for hypertensive patients in rural Portugal. J Am Pharm Assoc (Washington, DC) 2002;42:858–864. doi: 10.1331/108658002762063691. [DOI] [PubMed] [Google Scholar]
- Krass I, Armour CL, Mitchell B, Brillant M, Dienaar R, Hughes J, Lau P, Peterson G, Stewart K, Taylor S, Wilkinson J. The Pharmacy Diabetes Care Program: assessment of a community pharmacy diabetes service model in Australia. Diabet Med. 2007;24:677–683. doi: 10.1111/j.1464-5491.2007.02143.x. [DOI] [PubMed] [Google Scholar]
- McKenney JM, Slining JM, Henderson HR, Devins D, Barr M. The effect of clinical pharmacy services on patients with essential hypertension. Circulation. 1973;48:1104–1111. doi: 10.1161/01.cir.48.5.1104. [DOI] [PubMed] [Google Scholar]
- McKenney J, Brown E, Necsary R. Effect of pharmacist drug monitoring and patient education on hypertensive patients. Contemp Pharm Pract. 1978;1:50–56. [Google Scholar]
- McLean DL, McAlister FA, Johnson JA, King KM, Makowsky MJ, Jones CA, Tsuyuki RT, Investigators SH. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus study of cardiovascular risk intervention by pharmacists- hypertension (SCRIP-HTN) Arch Intern Med. 2008;168:2355–2361. doi: 10.1001/archinte.168.21.2355. [DOI] [PubMed] [Google Scholar]
- Park JJ, Kelly P, Carter BL, Burgess PP. Comprehensive pharmaceutical care in the chain setting. J Am Pharm Assoc. 1996;NS36:443–451. doi: 10.1016/s1086-5802(16)30099-7. [DOI] [PubMed] [Google Scholar]
- Planas LG, Crosby KM, Mitchell KD, Farmer KC. Evaluation of a hypertension medication therapy management program in patients with diabetes. J Am Pharm Assoc. 2009;49:164–170. doi: 10.1331/JAPhA.2009.08164. [DOI] [PubMed] [Google Scholar]
- Santschi V, Lord A, Berbiche D, Lamarre D, Corneille L, Prud'homme L, Normandeau M, Lalonde L. Impact of collaborative and multidisciplinary care on management of hypertension in chronic kidney disease outpatients. J Pharm Health Serv Res. 2011;2:79–87. [Google Scholar]
- Sookaneknun P, Richards RME, Sanguansermsri J, Teerasut C. Pharmacist involvement in primary care improves hypertensive patient clinical outcomes. Ann Pharmacother. 2004;38:2023–2028. doi: 10.1345/aph.1D605. [DOI] [PubMed] [Google Scholar]
- Svarstad BL, Kotchen JM, Shireman TI, Brown RL, Crawford SY, Mount JK, Palmer PA, Vivian EM, Wilson DA. Improving refill adherence and hypertension control in black patients: Wisconsin TEAM trial. J Am Pharm Assoc (2003) 2013;53:520–529. doi: 10.1331/JAPhA.2013.12246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zillich AJ, Sutherland JM, Kumbera PA, Carter BL. Hypertension outcomes through blood pressure monitoring and evaluation by pharmacists (HOME study) J Gen Intern Med. 2005;20:1091–1096. doi: 10.1111/j.1525-1497.2005.0226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne R. The Nature, Determinants and Effects of Medication, Beliefs in Chronic Illness. London: University of London; 1997. [Google Scholar]
- Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47:533–543. [PubMed] [Google Scholar]
- De Simoni A, Mullis R, Clyne W, Blenkinsopp A. Medicines optimisation in primary care: can community pharmacies deliver? Br J Gen Pract. 2012;62:398–399. doi: 10.3399/bjgp12X653444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly DV, Bishop L, Young S, Hawboldt J, Phillips L, Keough TM. Pharmacist and physician views on collaborative practice: findings from the community pharmaceutical care project. Can Pharm J (Ott) 2013;146:218–226. doi: 10.1177/1715163513492642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ. 2004;329:145–148. doi: 10.1136/bmj.38121.684410.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, Kerby TJ, Klotzle KJ, Maciosek MV, Michels RD, O'Connor PJ, Pritchard RA, Sekenski JL, Sperl-Hillen JM, Trower NK. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. 2013;310:46–56. doi: 10.1001/jama.2013.6549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, Stevens VJ, Vollmer WM, Lin PH, Svetkey LP, Stedman SW, Young DR Group WGotPCR. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289:2083–2093. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, Simons-Morton DG, Karanja N, Lin PH. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- Cook NR, Cohen J, Hebert PR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995;155:701–709. [PubMed] [Google Scholar]
- National Pharmacy Association and British Medical Association. 2009. Improving communication between community pharmacy and general practice: a joint initiative from the General Practitioners Committee of the British Medical Association and the National Pharmacy Association Available at bma.org.uk/-/media/…/gppharmimprovingcommunicationworkbook.pdf (last accessed 27 March 2014)
- Blenkinsopp A, Bond C. Pharmacists must learn to play their part in multidisciplinary health teams. Pharm J. 2007;279:330–332. [Google Scholar]
Supporting Information
Additional Supporting Information may be found in the online version of this article at the publisher’s web-site:
Appendix S1 Search strategies used in the major electronic databases
Appendix S2 Characteristics of included studies
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Search strategies used in the major electronic databases
Appendix S2 Characteristics of included studies