Abstract
Aims
Poor communication of clinical information between healthcare settings is associated with patient harm. In 2008, the UK National Prescribing Centre (NPC) issued guidance regarding the minimum information to be communicated upon hospital discharge. This study evaluates the extent of adherence to this guidance and identifies predictors of adherence.
Methods
This was an audit of discharge summaries received by medical practices in one UK primary care trust of patients hospitalized for 24 h or longer. Each discharge summary was scored against the applicable NPC criteria which were organized into: ‘patient, admission and discharge’, ‘medicine’ and ‘therapy change’ information.
Results
Of 3444 discharge summaries audited, 2421 (70.3%) were from two teaching hospitals and 906 (26.3%) from three district hospitals. Unplanned admissions accounted for 2168 (63.0%) of the audit sample and 74.6% (2570) of discharge summaries were electronic. Mean (95% CI) adherence to the total NPC minimum dataset was 71.7% [70.2, 73.2]. Adherence to patient, admission and discharge information was 77.3% (95% CI 77.0, 77.7), 67.2% (95% CI 66.3, 68.2) for medicine information and 48.9% (95% CI 47.5, 50.3) for therapy change information. Allergy status, co-morbidities, medication history and rationale for therapy change were the most frequent omissions. Predictors of adherence included quality of the discharge template, electronic discharge summaries and smaller numbers of prescribed medicines.
Conclusions
Despite clear guidance regarding the content of discharge information, omissions are frequent. Adherence to the NPC minimum dataset might be improved by using comprehensive electronic discharge templates and implementation of effective medicines reconciliation at both sides of the health interface.
Keywords: care transition, discharge communication, discharge information, discharge summary, medicine reconciliation, NPC minimum dataset
What is Already Known about this Subject?
Previous research suggests that the quality of discharge medication information transfer is generally poor. However, limited research can be found about communication of patient, admission, discharge and therapy change information.
There is no large UK report of the extent to which discharge summaries adhere to national guidance and no indication of the predictors of performance.
What this Study Adds
Three years post-issue of the UK national standards, the majority of discharge summaries are failing to fulfil these requirements.
The audit found that the use of an electronic template incorporating all recommended national standards increased the likelihood of adherence to the requirements and thus improved discharge communication.
Introduction
Transition of patient care between settings presents an opportunity for errors and has been identified by the World Health Organization as a cause of preventable morbidity 1. The Institute of Health Improvement suggested that poor information communication at healthcare transition is responsible for over 50% of all medication errors and up to 20% of adverse events 2. Similar rates have been reported in the UK 3, Australia 4 and Europe 5. Lack of communication is not restricted to medication information and admission, discharge and patient information such as incomplete and inaccurate allergy status, co-morbidities and hospital contact information have also been reported 6,7.
Legibility has presented an additional opportunity for error at care transition. An estimated 40% to 75% of handwritten discharge summaries have been found to be completely or partially illegible 8,9. With advances in computer technology, the use of electronic discharge summaries has evolved and thus the relevance of legibility may have diminished. Evidence is, however, emerging that new types of errors maybe introduced with the use of IT systems 10. Electronic discharge summaries can however improve the timeliness of information transfer between care settings. In 2009, the UK care quality commission reported that only 53% of discharge summaries were received in sufficient time to be of use in post-discharge management 11. A recent USA report highlighted that less than 50% of discharged patients have their discharge letter prepared on the day of discharge and for one in four patients, the discharge team took over a week to complete the discharge summary 12. However, the timeliness of the discharge information being received by the next health provider was not reported.
A systematic review of deficits in communication and information transfer performed in 2007 by Kripalani et al. 13 reviewed observational studies investigating communication and information transfer at hospital discharge (n = 55) and controlled studies evaluating the efficacy of interventions to improve information transfer (n = 18). Kripalani et al. followed by a number of studies in later years, found that deficits in communication and information transfer at hospital discharge are common and may adversely affect patient care. The researchers were however unable to identify the factors associated with the deficits 4,5,7,8,12,13.
Transfer of discharge summary information is a multi-factorial process and the relationships between these factors and the quality of discharge communication are unclear 14,15. Factors which influence discharge summary information might be system related such as discharge summary template content, whether the document used to transfer information is handwritten or electronic 8,16,17, time available to collect and communicate discharge information and whether the admission was planned or unplanned 5,18. Variations in discharge information may be related to the individual such as the medical training of the person completing the discharge summary, the complexity of the patient's care and discharge medication 5,7,19.
There is limited UK evidence evaluating the quality of information received in primary care following patient discharge which currently comprises one general practitioner (GP) survey 11, two large audits 3,14 and one retrospective case note review study 6.
In response to patient safety concerns, in 2008 the UK National Prescribing Centre (NPC) stipulated a minimum dataset of information to be communicated at all transitions of patient care 20. The NPC is now a part of the UK National Institute for Health and Care Excellence (NICE) which has therefore adopted the NPC guidance as a national standard for information communication at care transition. NICE is a government funded organization that supports health professionals in providing the best possible healthcare. There are no large scale reports of the extent to which discharge summaries adhere to these guidelines and thus no indication of their impact on the quality of practice.
The aims of this study were to report the magnitude of hospital discharge summary adherence to the NPC minimum dataset and to identify the extent of adherence to different elements within the dataset. Additionally, the study aimed to determine the factors affecting the likelihood of discharge summary adherence to the NPC minimum dataset.
Methods
Setting and study design
A retrospective review of a sample of discharge summaries received by medical practices from one primary care trust was conducted between January to March 2011 in the eastern region of the UK. As an audit, ethics approval was not required. However, appropriate authorization to undertake the audit was obtained from the NHS Norfolk in August 2010.
An audit tool was developed to record either ‘yes’ or ‘no’ for the presence of each NPC minimum dataset item in a discharge summary. Table 1 describes the minimum dataset recommended by the NPC following hospital discharge.
The NPC minimum dataset of information recommended in primary care following discharge from hospital*
|
All the NPC minimum dataset criteria listed above were included in the audit standards except ‘procedures carried out’ and ‘additional information related to corticosteroid record cards or anticoagulant books’. This was because it was not possible to identify whether procedures were carried out when this information was not recorded in the discharge summary and the audit was conducted retrospectively so it was not possible to identify whether a patient was provided with the relevant record card or logbook.
Sample selection
All medical practices (n = 91) in one primary care trust were invited to participate and practices self-selected a member of the medical team to complete a piloted audit data collection form for each discharge summary. Each practice was allocated a target number of eligible discharge summaries to collect prospectively and a standardized procedure for data collection form completion was issued. Discharge summaries were selected consecutively until the allocated number was collected. The allocation was based on the assumption that a sample representing 5% of the patients registered with a practice is a reasonable work load for GP practices to audit. List sizes of the GP practices ranged from 200 to 2180 and thus practice allocated numbers ranged from 10 to 109. A total sample of 3761 discharge summaries was anticipated.
All discharge summaries of patients hospitalized for 24 h or longer were included and those for patients transferred to another trust or deceased before discharge or data collection were excluded.
Estimating discharge summary adherence to the NPC minimum dataset
Discharge summaries were scored against all NPC criteria presented in Table 1, except for ‘procedures carried out’ and ‘additional information related to corticosteroid record cards or anticoagulant books’. Discharge summaries were scored one point when a criterion was successfully fulfilled (i.e. all information was provided and/or accurate as appropriate). For example, if a patient had three allergies and only one was documented the criterion was not fulfilled. Two points were scored for each criterion not fulfilled. Discharge summaries for patients with no medication history or where no medicines were changed, initiated or discontinued were scored only against the applicable criteria and therefore the extent of adherence to the NPC minimum dataset was estimated as a percentage using the equation below:
Discharge summary adherence score (S) = Sum of the point(s) assigned to each applicable criterion
T = score representing complete adherence to all applicable criteria
The NPC minimum dataset criteria were organized into three categories: ‘patient, admission and discharge information’, ‘medication information’ and ‘therapy change information’. These are shown in Table 2.
The audit scoring criteria
| Patient, admission and discharge details |
|
| Medication information* |
|
| Therapy changes information† |
|
Based on the completeness of the medicines listed in the discharge summary, for example if five medicines were listed in the discharge summary, the criteria would have been fulfilled if all the requirements (name, dose, duration etc.) for the five medicines were recorded. To avoid double counting, if for example the same patient used six medications according to the GP and five were listed in the discharge summary. omission of the 6th pre-admission medication would be scored as ‘complete medication history’ not fulfilled with no further penalty under the ‘medication information’ criterion.
The whole discharge summary was reviewed to identify changes in therapy and rationale for change, initiation or discontinuation.
Audit quality assurance
Variations between auditors were systematically evaluated to assess the quality of the audit data. All participating medical practices were stratified by list size into five strata. Computerized random number generation was used to select five medical practices from each stratum to assess variations in audit data collection. Similarly, 20 discharge summaries were randomly selected from each of the selected practices and re-audited by the lead author (EH). Agreement for each audit question was calculated using the Kappa statistic. Kappa scores ranging from 0.01–0.40 were considered of slight to fair agreement, 0.41–0.60 of moderate agreement, 0.061–0.80 good and > 0.81 of substantial agreement 21.
Twenty handwritten discharge summaries were randomly selected using a computerized random number generator and legibility rated by a GP independent of the medical practice from which the data were collected. Agreement between the GP assessment and auditors was assessed by weighted Kappa scores which were interpreted in a similar way to unweighted Kappa scores. Cells were weighted according to the magnitude of disagreement; the method used to weight cells is the absolute error weight 22.
Data collection and outcome measurements
In addition to data describing discharge summary adherence to the NPC minimum dataset, the following data were collected from each discharge summary: dates of admission and discharge, whether it was planned or unplanned (emergency) and the role of the professional responsible for discharge, patient medical and demographic information, clinical information related to laboratory results and post-admission complications and the number of working days between discharge and receipt of the discharge summary by primary care.
From each hospital represented in the audit, a copy of the discharge summary template was obtained. For some hospitals, more than one template was available and thus the template representing the majority of the discharge summaries from that hospital was selected for analysis.
Discharge summary legibility was assessed using a four point scale 23: ‘Illegible’, ‘most words are illegible’, ‘some words illegible’ and ‘legible’.
The audit tool was piloted and face validated by two primary care pharmacists and one GP before Trust-wide distribution.
Total adherence to the NPC minimum dataset was reported as the primary outcome. Extent of discharge summary adherence to the three categories of the NPC minimum dataset was the secondary outcome.
Data analysis
Data were processed using the Statistical Package for Social Science (SPSS version 18). Descriptive statistics were reported as a mean (95% CI) and median (IQR) as appropriate. General linear models (GLM) were used to investigate the effect of factors such as, the number of prescribed medicines, type of discharge summary (handwritten or electronic) and discharge summary template on adherence to the NPC minimum dataset. Stepwise backward elimination was used to reach the most parsimonious GLM models.
Furthermore, GLM analysis was performed to determine the effect of ward speciality on discharge summary adherence to the NPC minimum dataset. Community and specialist care hospitals such as mental health hospitals were excluded from this analysis as they do not have the breadth of different ward specialities demonstrated by general hospitals. Likewise, GLM analysis was employed to determine the effect of factors and ward speciality on discharge summary adherence to each of the three categories of the NPC minimum dataset.
All models presented were checked for assumptions of linearity, multicollinearity and homoscedasticity. None of these assumptions was violated.
Results
Study sample
A small number of practices (n = 7) did not complete the audit in the specified time window. These only represented 317 (8%) of the anticipated number of discharge summaries which were therefore excluded from analysis. A total of 3444 discharge summaries representing 12 different hospitals were audited by 84 medical practices. Discharge summaries from two teaching hospitals accounted for 2421 (70.3%), three general district hospitals accounted for 906 (26.3%), 21 (0.6%) were from a mental health trust, 52 (1.5%) were from community and 40 (1.2%) were from private hospitals or hospitals beyond the region surrounding the Trust. Table 3 summarizes the audit sample characteristics. Discharge summaries were primarily electronic and arose from unplanned admissions. The audit was largely of older patients and with a relatively even gender distribution. The highest proportion of discharge summaries were from medicine for elderly wards. For more than 20% of discharge summaries there was no indication of the role of the healthcare professional responsible for preparing the discharge summary. Where profession type was provided, doctors represented the highest proportion of which 1113 (44.5%) were of an unknown training level and 853 (34.1%) were doctors in their first year of practice after qualification.
Table 3.
Audit sample characteristics
| Measure | H1 | H2 | H3 | H4 | H5 | Community hospitals | Others | Total | |
|---|---|---|---|---|---|---|---|---|---|
| n = 715 | n = 57 | n = 136 | n = 55 | n = 2368 | n = 52 | n = 61 | n = 3444 | ||
| Patient demographics | |||||||||
| Age | Median (IQR) | 67 (45–81) | 59 (46–70) | 60.5 (39.3–76.8) | 73 (57–80) | 66.0 (46–79) | 76.0 (70.3–84.8) | 65.0 (46.5–76) | 66 (46–80) |
| Female | n (%) | 371 (51.9) | 22 (38.6) | 81 (59.6) | 27 (49.1) | 1194 (50.4) | 26 (50.0) | 32 (52.5) | 1753 (50.9) |
| Number of medicines | Median (IQR) | 5 (2–8) | 6 (2–8) | 6 (3–10) | 5 (3–8) | 6 (2–8) | 6 (3–10) | 6 (3–9) | 5 (2–8) |
| Hospital stay | Median (IQR) | 4 (2–8) | 3 (1.5–8) | 3 (2–6) | 4.5 (2–13) | 4.5 (2–8) | 13 (5–36) | 4.5 (2–10) | 4 (2–8) |
| Time of discharge summary arrival | Median (IQR) | 2 (2–8) | 2 (2–4) | 1 (0–2) | 2 (1–2.5) | 2 (1–3) | 2 (2–4) | 2 (1–3) | 2 (1–3) |
| Type of discharge summary | |||||||||
| Electronic discharge summaries | n (%) | 110 (15.4) | 29 (50.9) | 126 (92.6) | 25 (45.5) | 2211 (93.4) | 30 (57.7) | 39 (63.9) | 2570 (74.6) |
| Type of admission | |||||||||
| Unplanned admission | n (%) | 433 (60.6) | 28 (49.1) | 20 (14.7) | 41 (74.5) | 1591 (67.2) | 30 (57.7) | 25 (41.0) | 2168 (63.0) |
| Unspecified type of admission | n (%) | 106 (14.8) | 10 (17.5) | 92 (67.6) | – | 128 (5.4) | 14 (26.9) | 15 (26.6) | 365 (10.6) |
| Ward specialities | |||||||||
| Medicine for Elderly | n (%) | 73 (10.2) | 3 (5.3) | 21 (15.4) | 1 (1.8) | 454 (19.2) | 7 (13.5) | 5 (8.2) | 564 (16.4) |
| Urology | n (%) | 76 (10.6) | 4 (7.0) | 25 (18.4) | 2 (3.6) | 292 (12.3) | 2 (3.8) | 2 (3.3) | 403 (11.7) |
| General surgery | n (%) | 54 (7.6) | 8 (14.0) | 1 (0.7) | 10 (18.2) | 244 (10.3) | 3 (5.8) | 1 (1.6) | 321 (9.3) |
| Thoracic | n (%) | 27 (3.8) | 1 (1.8) | 5 (3.7) | – | 210 (8.9) | – | – | 243 (7.1) |
| Cardiology | n (%) | 24 (3.4) | 4 (7.0) | 5 (3.7) | 3 (5.5) | 195 (8.2) | 1 (1.9) | 3 (4.9) | 235 (6.8) |
| Orthopaedic | n (%) | 62 (8.7) | 4 (7.0) | 3 (2.2) | 7 (12.7) | 137 (5.8) | 3 (5.8) | 7 (11.5) | 223 (6.5) |
| Paediatrics | n (%) | 63 (8.8) | 2 (3.5) | 6 (4.4) | – | 131 (5.5) | 1 (1.9) | – | 203 (5.9) |
| General medicine | n (%) | 70 (9.8) | 1 (1.8) | 40 (29.4) | 9 (16.4) | 65 (2.7) | 2 (3.8) | 2 (3.8) | 189 (5.5) |
| Gynaecology | n (%) | 21 (2.9) | 4 (7.0) | 13 (9.6) | 2 (3.6) | 105 (4.4) | – | 4 (6.6) | 149 (4.3) |
| Oncology | n (%) | 10 (1.4) | 6 (10.5) | 1 (0.7) | – | 121 (5.1) | 2 (3.8) | 1 (1.6) | 141 (4.1) |
| Gastroenterology | n (%) | 26 (3.6) | 2 (3.5) | 2 (1.5) | 4 (7.3) | 90 (3.8) | – | 8 (13.1) | 132 (3.8) |
| Others* | n (%) | 65 (9.1) | 15 (26.3) | 9 (6.6) | 15 (27.3) | 266 (11.2) | 9 (17.3) | 14 (23.0) | 393 (11.4) |
| Unspecified specialities | n (%) | 144 (20.1) | 3 (5.3) | 5 (3.7) | 2 (3.6) | 58 (2.4) | 22 (42.3) | 14 (23.0) | 248 (7.2) |
| Profession types | |||||||||
| Doctors | n (%) | 602 (84.2) | 40 (70.2) | 22 (16.2) | 33 (60.0) | 1728 (73.0) | 38 (73.1) | 41 (67.2) | 2504 (72.7%) |
| Pharmacists | n (%) | – | – | – | – | 36 (1.5) | – | – | 36 (10.5) |
| Specialist nurse practitioners | n (%) | 5 (0.7) | 2 (3.5) | – | – | 135 (5.7) | 1 (1.9) | 3 (4.9) | 146 (4.2) |
| Unspecified profession | n (%) | 108 (15.1) | 15 (26.3) | 114 (83.8) | 22 (40.0) | 469 (19.8) | 13 (25.0) | 17 (27.9) | 758 (22.0) |
e.g. Nephrology, Neurology, ENT, Endocrinology, Dermatology, Rheumatology, Ophthalmology, Maternity care and Neonatal.
Extent of adherence to total NPC minimum dataset
Mean (95% CI) discharge summary adherence to the total NPC minimum dataset was 71.7% (70.2, 73.2). Table 4 illustrates the range of discharge summary adherence with different procedural characteristics. The adherence rates of discharge summaries arising from planned and unplanned admissions were similar. Electronic discharge summaries, however, were associated with notably higher adherence than handwritten. Variation was found between hospitals with H3 demonstrating the greatest adherence whilst H1 and community hospitals demonstrated substantially lower adherence rates than other hospitals.
Table 4.
Discharge summary adherence to NPC minimum dataset
| Discharge summaries adherence [mean (95% CI)] | |||||
|---|---|---|---|---|---|
| n | Total NPC minimum Dataset | Patient, admission and discharge information | Medicine Information | Therapy change information | |
| Type of discharge summary | |||||
| Electronic | 2570 | 73.7% (73.3, 74.1) | 79.5% (79.1, 79.9) | 67.2% (66.3, 68.20) | 50.9% (49.4, 52.3) |
| Handwritten | 874 | 67.0% (65.2, 66.8) | 71.0% (70.2, 71.9) | 54.8% (53.4, 56.3) | 40.2% (36.9, 43.7) |
| Type of admission | |||||
| Planned | 911 | 71.3% (70.6, 72.1) | 77.2% (6.5, 78.0) | 63.9% (62.2, 65.6) | 46.3% (43.8, 48.9) |
| Unplanned admission | 2168 | 71.8% (71.3, 72.3) | 77.5% (77.1, 78.0) | 62.9% (61.9, 64.0) | 49.0% (47.3, 50.8) |
| Unspecified type of admission | 365 | 72.6% (71.2, 74.1) | 76.4% (75.0, 77.8) | 70.8% (68.5, 73.1) | 55.4% (51.2, 59.7) |
| Hospital | |||||
| H1 | 715 | 65.0% (64.1, 65.9) | 69.8% (68.9, 70.7) | 54.3% (52.9, 55.8) | 41.8% (37.8, 45.9) |
| H2 | 57 | 73.5% (70.6, 76.8) | 79.7% (76.2, 83.1) | 69.1% (62.5, 75.8) | 46.9% (34.7, 59.1) |
| H3 | 136 | 81.4% (79.7, 83.2) | 85.4% (83.9, 87.0) | 83.0% (80.0, 86.0) | 65.5% (60.0, 71.0) |
| H4 | 55 | 71.7% (68.3, 75.1) | 79.4% (76.7, 82.1) | 48.2% (40.2, 56.2) | 26.4% (14.6, 38.2) |
| H5 | 2368 | 73.5% (73.1, 74.0) | 79.3% (79.0, 79.7) | 66.4% (65.4, 67.4) | 50.6% (49.0, 52.1) |
| Community hospital | 52 | 62.4% (58.1, 66.9) | 68.6% (64.3, 72.9) | 58.5% (49.5, 67.5) | 27.7% (15.8, 39.6) |
| Others | 61 | 65.8% (62.5, 69.2) | 72.5% (69.2, 75.8) | 60.3% (54.2, 66.4) | 36.9% (26.1, 47.7) |
| Ward specialities | |||||
| Medicine for Elderly | 564 | 73.5% (72.6, 74.4) | 79.7% (78.8, 80.6) | 64.7% (62.8, 66.7) | 53.0% (49.7, 56.2) |
| Urology | 403 | 73.3% (72.2, 74.4) | 78.4% (77.1, 79.1) | 67.6% (65.3, 69.9) | 52.0% (48.3, 56.2) |
| General surgery | 321 | 71.1% (69.9, 72.4) | 78.1% (76.9, 79.3) | 58.8% (55.7, 61.9) | 42.3% (37.7, 46.9) |
| Thoracic | 243 | 73.3% (72.0, 74.6) | 78.7% (77.5, 80.0) | 67.2% (64.4, 69.7) | 51.5% (46.6, 56.4) |
| Cardiology | 239 | 73.0% (71.5, 74.5) | 78.9% (77.4, 80.4) | 65.2% (62.3, 68.1) | 50.7% (46.5, 54.9) |
| Orthopaedic | 217 | 68.6% (67.1, 70.2). | 75.0% (73.5, 76.5) | 63.5% (60.5, 66.6) | 34.9% (29.0, 40.7) |
| Paediatrics | 203 | 71.4% (69.7, 73.1) | 76.6% (74.9, 78.2) | 64.7% (61.0, 68.3) | 46.8% (40.8, 52.8) |
| General medicine | 187 | 72.0% (70.3, 73.7) | 75.8% (73.9, 77.5) | 64.8% (61.1, 68.6) | 58.3% (51.5, 64.9) |
| Gynaecology | 145 | 72.2% (70.1, 74.3) | 78.9% (77.1, 80.6) | 64.0% (59.4, 68.5) | 49.6% (.0, 56.9) |
| Oncology | 140 | 73.9% (72.1, 75.7) | 77.8% (76.2, 79.4) | 68.2% (64.4, 72.1) | 58.9% (52.6, 65.3) |
| Gastroenterology | 126 | 69.6% (67.7, 71.6) | 75.7% (73.7, 77.7) | 60.2% (56.1, 64.2) | 48.1% (41.0, 55.3) |
| Others* | 421 | 72.6% (71.5, 73.7) | 78.4% (77.3, 79.4) | 62.8% (59.9, 65.6) | 43.1% (39.0, 47.2) |
| Unspecified specialities | 235 | 64.4% (62.7, 66.1) | 68.8% (67.1, 70.5) | 60.2% (56.0, 62.5) | 49.0% (43.2, 54.9) |
| Profession types | |||||
| Doctors | 2504 | 71.0% (70.5, 71.5) | 76.6% (76.2, 77.1) | 62.8% (61.9, 63.8) | 48.1% (46.4, 49.7) |
| Pharmacists | 36 | 74.6% (71.7, 77.5) | 80.1% (77.6, 82.6) | 69.1% (61.2, 77.0) | 51.5% (38.4, 64.6) |
| Specialist nurse practitioners | 146 | 74.5% (72.5, 76.6) | 79.8% (78.1, 81.5) | 65.6% (61.0, 70.3) | 53.0% (46.8, 59.2) |
| Unspecified profession | 758 | 73.6% (72.6, 74.4) | 79.1% (78.3, 79.9) | 67.5% (65.7, 69.3) | 50.5% (47.8, 53.2) |
| Extent of adherence | 3444 | 71.7% (70.2, 73.2) | 77.3% (77.0, 77.7) | 67.2% (66.3, 68.2) | 48.9% (47.5, 50.3) |
e.g. Nephrology, Neurology, ENT, Endocrinology, Dermatology, Rheumatology, Ophthalmology, Maternity care and Neonatal.
Table 5 presents the content of the discharge summary templates used by the hospitals representing the majority of the audit sample. No two templates were identical and the extent of template adherence followed a similar pattern to discharge summary adherence to the NPC minimum dataset. The template of H3 exhibited greatest adherence to the NPC minimum dataset whilst the template of H1 and community hospitals demonstrated the lowest adherence.
Table 5.
Templates of the primary medium of discharge summary
| Information | Electronic templates | Handwritten template | ||||
|---|---|---|---|---|---|---|
| Template2 | Template 3 | Template 5 | Template 1 | Template 4 | Community hospital template | |
| Patient | ||||||
| Name | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Date of birth | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| NHS number | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Past medical history | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Allergy and hypersensitivities | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ |
| Admission and discharge | ||||||
| Admission date | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Discharge date | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Presenting diagnosis | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Procedures and investigation | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ |
| Medicine | ||||||
| Name | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Dose | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Frequency | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Route | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ |
| Formulation | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ |
| Duration | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ |
| Therapy change | ||||||
| Medication started | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ |
| Reason for medication started | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Medication stopped | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ |
| Reason for medication stopped | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Medication changes | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ |
| Reason for medication changed | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Ward details | ||||||
| Consultant name | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Ward name | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| % Template adherence to the NPC minimum dataset | 65.2% | 78.3% | 73.9% | 60.9% | 65.2% | 60.9% |
With respect to ward specialities and profession types, discharge summaries from orthopaedic wards and those prepared by doctors demonstrated the lowest adherence rates.
Adherence to NPC requirements relating to patient, admission and discharge information
Figure 1 illustrates adherence rates to the NPC minimum dataset for patient, admission and discharge information. Mean (95% CI) discharge summary adherence was 77.3% (77.0, 77.7) with allergy status, co-morbidities and medication history contributing to the most frequent omissions.
Figure 1.
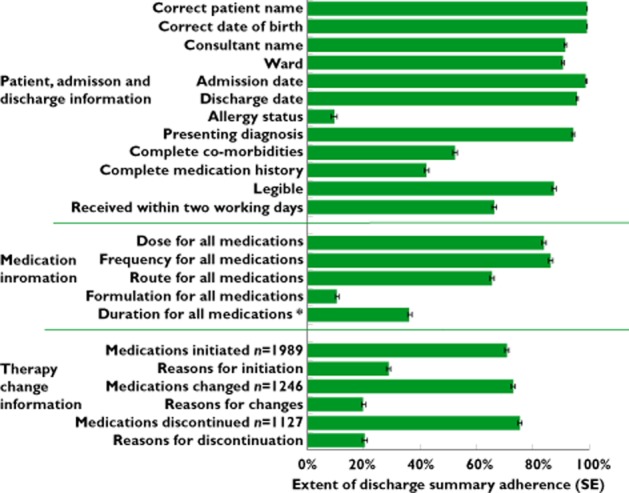
Magnitudes of discharge summaries adherence to NPC minimum dataset. *When medications were initated by hospital n = 1989
The majority of discharge summaries were electronic and thus legible. However, 374 (42.8%, 95% CI 39.5, 46.1) of the handwritten discharge summaries were considered partially illegible with the clinical message deemed unaffected, 33 (8.8%, 95% CI 6.9, 10.7) were considered mostly illegible with the meaning of the clinical message unclear and 13 (1.5%, 95% CI 0.69, 2.3) were deemed completely illegible.
Table 4 presents the extent of discharge summary adherence to the NPC requirement for patient, admission and discharge information. Electronic discharge summaries were more likely to provide comprehensive patient, admission and discharge information compared with handwritten discharge summaries. Planned and unplanned admissions, however, demonstrated similar adherence rates.
Variation can be seen between wards with respect to patient, admission and discharge information with orthopaedic wards demonstrating the lowest adherence. The most notable deviations were in the recording of co-morbidities and medication histories which were only fulfilled for 79 (41.8%) and 87 (39.0%) discharge summaries, respectively. Discharge summaries written by pharmacists and nurses demonstrated better adherence than those written by doctors. It was again in the recording of co-morbidities and medication histories that the main differences lay. Discharge summaries prepared by doctors reported full details of co-morbidities and medication histories for only 50.6% (1266) and 41.7% (1042) compared with 58.3% (21) and 50% (18) for pharmacists and 61.6% (90) and 43.8% (46) for nurses, respectively.
Adherence to NPC requirements relating to medication information
Mean (95% CI) discharge summary adherence to medication information reporting was 64.0% (63.2, 64.8). Figure 1 illustrates adherence rates for medication information with deviations manifested particularly with medicine formulation and duration.
Table 4 presents the extent of discharge summary adherence to medication information reporting. It can be seen that electronic discharge summaries demonstrated higher adherence than handwritten discharge summaries. Variation can be seen between wards with general surgery wards demonstrating the lowest adherence rate. No discernible differences were seen between planned and unplanned admissions or profession types.
Adherence to NPC requirements relating to therapy change information
Discharge summary reporting of therapy change information demonstrated the lowest adherence among the three categories of the NPC minimum dataset with a mean adherence of 48.9% (95% CI 47.5, 50.3). Figure 1 illustrates adherence rates for therapy change information. The rationale for medicines initiated, discontinued or changed was persistently omitted.
Table 4 presents the variation in discharge summary adherence to therapy change information reporting; electronic discharge summaries demonstrated better adherence than handwritten discharge summaries. Unplanned admissions were associated with a slightly higher adherence rate than planned admissions. Of the different types of ward, orthopaedic wards demonstrated the lowest adherence. Small variation can be seen between healthcare professions with discharge summaries prepared by doctors demonstrating lower adherence.
Predictors of adherence to NPC minimum dataset
Table 6 summarizes the regression models for factors influencing discharge summary adherence to the total NPC minimum dataset, patient, admission and discharge information, medication information and therapy change information.
Table 6.
Regression models* for factors predicting discharge summary adherence to the total NPC minimum dataset, patient, admission and discharge information, mediation information and therapy change information
| Adherence to total NPC minimum dataset | Adherence to patient, admission & discharge information | Adherence to medication information | Adherence to therapy change information | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | P | 95% CI for B | B | SE | P | 95% CI for B | B | SE | P | 95% CI for B | B | SE | P | 95% CI for B | |||||
| Lower limit | Upper limit | Lower limit | Upper limit | Lower limit | Upper limit | Lower limit | Upper limit | |||||||||||||
| Constant | 78.6 | 0.75 | <0.001 | 77.1 | 80.1 | 79.1 | 0.32 | <0.001 | 78.4 | 79.7 | 66.7 | 0.82 | <0.001 | 65.1 | 68.3 | 52.1 | 1.2 | <0.001 | 49.7 | 54.5 |
| Number of medications | −0.24 | 0.04 | <0.001 | −0.3 | −0.2 | 0.11 | 0.04 | .007 | 0.03 | 0.2 | −0.02 | 0.10 | 0.86 | −0.2 | 0.18 | −0.23 | 0.16 | 0.15 | −0.6 | 0.1 |
| Type of discharge summary | ||||||||||||||||||||
| Handwritten | −3.51 | 0.63 | <0.001 | −4.8 | −2.3 | −4.8 | 0.86 | <0.001 | −6.5 | 3.1 | −13.5 | 3.62 | <0.001 | −20.6 | −6.4 | −5.6 | 4.2 | 0.19 | −13.9 | 2.8 |
| Electronic | 0 | 0 | 0 | 0 | ||||||||||||||||
| Discharge summary template | ||||||||||||||||||||
| Template 1 | −5.83 | 0.68 | <0.001 | −7.2 | −4.5 | −8.5 | 1.00 | <0.001 | −10.5 | −6.5 | −6.1 | 2.3 | 0.01 | −10.6 | −1.7 | −5.6 | 4.2 | 0.19 | −13.9 | 2.8 |
| Template 2 | 1.66 | 1.50 | 0.27 | −1.3 | 4.6 | 3.9 | 1.90 | 0.04 | 0.1 | 7.7 | 7.1 | 4.4 | 0.11 | −1.5 | 15.8 | −3.3 | 7.5 | 0.66 | −17.9 | 11.3 |
| Template 3 | 8.14 | 0.97 | <0.001 | 6.2 | 10.1 | 6.3 | 0.96 | <0.001 | 4.5 | 8.2 | 18.2 | 2.1 | <0.001 | 14.2 | 22.3 | 17.9 | 3.6 | 0.01 | 10.8 | 24.9 |
| Template 4 | −0.13 | 1.53 | 0.93 | −3.1 | 2.9 | −0.58 | 2.1 | 0.78 | −4.7 | 3.5 | −6.2 | 4.6 | 0.18 | −15.2 | 2.8 | −12.1 | 6.8 | 0.08 | −25.5 | 1.3 |
| Template 5 | 0 | 0 | 0 | |||||||||||||||||
| Community hospital template | −9.47 | 1.56 | <0.001 | −12.5 | −6.4 | −9.5 | 1.9 | <0.001 | −13.2 | −5.7 | −4.9 | 4.3 | 0.25 | −13.5 | 3.5 | −19.2 | 8.1 | 0.02 | −35.1 | −3.3 |
Final stepwise elimination models.
With respect to adherence to the total NPC minimum dataset (r2 = 0.14, adjusted r2 = 0.14), template 1 and community hospital templates contributed significantly to lower adherence whilst template 3 contributed to higher adherence. Handwritten discharge summaries and an increased number of medicines contributed to lower adherence. The effect of ward speciality on discharge summary adherence to the NPC minimum dataset adjusting for type of discharge summary and number of medicines (r2 = 0.10, adjusted r2 = 0.11) identified that orthopaedic wards contributed to the lowest adherence; B (SE) = −3.7 (1.1), P < 0.001 followed by general surgery −2.36 (1.03), P = 0.02.
Investigating factors influencing the three categories of NPC minimum dataset identified similar predictors. For patient, admission and discharge information (r2 = 0.18, adjusted r2 = 0.16), the community hospital template was the strongest predictor of poor adherence. For medicine information (r2 = 0.13, adjusted r2 = 0.11), a handwritten discharge summary was the strongest predictor of poor adherence. For therapy change information (r2 =.11, adjusted r2 = 0.09), template 3 was the only predictor of good adherence, the remainder were very strong predictors of poor adherence.
Similarly, investigating the influence of ward specialty adjusting for discharge summary template, the number of medications and type of discharge summary, identified orthopaedic wards as the strongest predictor of poor adherence; B (95% CI −3.68 (−6.3, −1.06), P = 0.01 for patient, admission and discharge details (r2 = 0.14, adjusted r2 = 0.14) whilst general surgery wards were the strongest predictor of poor adherence for medicine information (r2 = 0.11, adjusted r2 = 0.09); −8.90 (2.7) (95% CI −14.27, −3.52), P = 0.001. For therapy change information, all wards demonstrated poor adherence with orthopaedic wards again being the strongest predictor of poor adherence (r2 = 0.11, adjusted r2 = 0.06); −22.4 (4.9) (95% CI −32.1, −12.7), P < 0.001.
Quality assurance of audit data
Ninety-five discharge summaries were re-audited and Kappa scores ranged between 0.61 and 1 with a mean (95% CI) of 0.83 (0.81, 0.85) indicating good to substantial agreement. The weighted kappa score (95% CI) for legibility assessment was 0.86 (0.59, 1) (P = 0.001) indicating substantial agreement.
Discussion
This study highlights that 3 years after the UK minimum dataset for discharge information transfer being stipulated, the requirements are not consistently met. The deviations identified reflect those of previous studies which have also cited allergy status, co-morbidities, medication history, details of medicines prescribed and rationale for therapy changes as common omissions 4–7,12,24–27.
Incomplete allergy status, omissions regarding medicines prescribed before admission and co-morbidities have been demonstrated to contribute to patient harm associated with unintended discontinuation or unsafe prescribing 28,29. Additionally, incomplete information regarding therapy changes and discharge medications might confuse primary care providers and contribute to time wastage while attempting to establish whether change was intentional.
The lack of progress with discharge information communication is of concern. This study has identified predictors of non-adherence plus characteristics associated with increased adherence to NPC requirements. Recommendations to enhance discharge information transfer have therefore been proposed.
Considerable variations were seen between hospitals. H3 demonstrated the greatest adherence. Notably, deviations between hospitals followed a similar pattern to the extent of discharge summary template adherence to the NPC minimum dataset. This is consistent with previous research outlining that the use of a standardized discharge summary form resulted in more comprehensive and accurate communication of discharge information 8,17. Similarly, this has been advocated by the Health Informatics Unit at the UK Royal College of Physicians since 2008 30.
Electronic discharge summaries demonstrated better adherence to all NPC requirements compared with handwritten discharge summaries. Similar findings have been reported in previous studies with electronic discharge summaries reducing hand transcription and allowing faster and uniform recording of discharge information 5,13. However, they have been associated with increased errors due to incorrect selection or user entry 10,31. This present study design did not allow for such errors in recording to be captured.
The inverse relationship between adherence to the NPC minimum dataset and the number of prescribed medicines is intuitive and consistent with previous reports 24,25. When a patient is prescribed a medication there is an increased opportunity for communication errors.
The poor performance of orthopaedic and general surgery wards is consistent with previous studies 3,7,32,33. Discharge summaries from these wards persistently recorded no rationale for therapy changes and provided incomplete information related to medicine and co-morbidity history. Patient short stay admissions for minor risk procedures within these care areas might contribute to a hospital team perception that the GP will decipher changes and continue patient care from the clinical history provided 34. However, without comprehensive notification about post-discharge treatment and full details of patient medicines, the GP might feel unable to continue patient care and maintain clinical responsibility 35. Additionally, inattention to secondary conditions could explain these frequent deficits. This has been also suggested in a recent report in 2012 highlighting that errors that occurred on discharge were more likely attributed to medicines unrelated to the primary diagnosis 36. Inattention to secondary conditions and consequently medicines which are unrelated to the primary diagnosis might be of significant implication to patient care and safety. A national review in the USA including over 11 million discharged patients from 2003–2004 highlighted that among patients who were readmitted within 30 days after a surgical discharge, 70.5% were readmitted for non-surgical condition 37. Thus, it is important to devote equal attention to all patient medicines and/or co-morbidities in these acute settings.
Further exploration of the factors contributing to variations in ward performance is warranted. This may be achieved through interviews with care providers at health transition points to enhance our understanding of the reasons underlying persistent deviations within individual wards and the contributors to good adherence within others. Such information might guide future intervention development and resource prioritization.
This study found no difference between profession types with respect to discharge summary adherence to the NPC minimum dataset or risk of discrepancy. This is, however, inconsistent with two large UK reports 15,38 and smaller studies in the USA and Europe 39,40 which have indicated that trainee doctors are a contributing factor to increased risk of admission error. The absence of effect of profession type in the present audit could reflect the high proportion of discharge summaries with an unspecified profession or training level resulting in a limited number of data points for this factor. Thus, no firm conclusion can be drawn on this regard warranting further work.
Our study is the first to report adherence levels to the NPC minimum dataset across an entire primary care trust. Whilst not generalizable to the whole of the UK, the audit has presented a large dataset representing various hospitals and specialities. This study is also the first to investigate a number of process, system and patient related factors predicting adherence to the NPC minimum dataset.
However, the sampling strategy could have resulted in more than one discharge summary being received from the same hospital doctor which could in turn lead to less discrimination within the study results. The methodological approach of data collection by multiple people whilst affording a large sample size, introduced the potential for variations in quality. The audit process required the whole discharge summary to be reviewed to identify changes in therapy and rationales. It is possible that the reasons for change and additional information included in the body of the discharge summary may have been missed due to human error. Additionally, discharge summary adherence in our study was not graded on a discrete scale and therefore variation in quality might not have been fully captured by the simplistic yes/no criteria. Nevertheless, the quality assurance process demonstrated good to substantial agreement thus providing confidence in the presented data.
This study has reported the magnitude of discharge summary adherence to the NPC minimum dataset but it is not possible to comment on the accuracy of information provided. Therefore, further work to capture the accuracy of information communication is necessary.
This study has identified clear predictors of good adherence and thus allows recommendations to be developed. However, the amount of variance explained by the regression model was small and thus a substantial proportion remains unexplained warranting further work to explore other predictors which might contribute to the quality of discharge communication.
The discharge summary template was identified as a significant predictor of the quality of discharge information. This valuable finding might help to promote the implementation of a standardized pro-forma across all NHS trusts. However, there were variations in the templates employed between wards within each hospital and the template representing the majority of discharge summaries generated from each hospital was audited. The lack of standardization and use of multiple templates may indicate variation in care standards and patient management between hospitals or wards. Therefore, it is impossible to determine from the present study design, the extent to which variation in template design affected discharge summary adherence. Future work capturing these other variables may therefore be beneficial.
Although the NPC is a government funded agency responsible for improving the quality of prescribing, there is no mandate for hospitals to adhere to this guidance and the extent to which the guidance is utilized is unknown. There might be a need to publicize widely and mandate the use of the NPC minimum dataset by hospitals and UK health institutions. Of note is that the NPC criterion for discharge summaries to be received within 2 days post discharge was fulfilled by 70% of discharge summaries. Recent recommendations, however, have placed greater emphasis on discharge summaries being sent within 24 h of the patient being discharged 41.
In conclusion, the completeness of discharge information communication in one primary care trust was found to be inadequate 3 years post-issue of national standards. Comprehensive electronic pro-forma incorporating all NPC minimum dataset requirements may improve the quality of discharge communication.
Adherence to the NPC minimum dataset varies across care areas and identifying wards demonstrating poor adherence as well as good adherence is necessary to guide future interventions. Patients prescribed higher numbers of medicines need greater care whilst completing their discharge summary and communicating information upon care transition. However, such recommendations might be difficult to implement in an environment of multiple competing demands. Thus it would be of value to identify the optimum method to implement and prioritize medicines reconciliation service provision to patients most likely to benefit.
Competing Interests
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare no support from any organization for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years and no other relationships or activities that could appear to have influenced the submitted work.
The authors would like to acknowledge the valuable contribution of Mr John Wood and Mr Ian Small to this work.
References
- World Health Organization. 2007. Patient safety: action on patient safety: high 5s. Available at http://www.who.int/patientsafety/implementation/solutions/high5s/en/index.html (last accessed 3 August 2014)
- Institute for Healthcare Improvement. Medication reconciliation to prevent adverse drug events. Available at http://www.ihi.org/explore/adesmedicationreconciliation/Pages/default.aspx (last accessed 3 August 2014)
- 2010. East & South East England specialist pharmacy services. Results of a Collaborative Audit of Pharmacy-Led Medicine Reconcilaition (MR) in 56 trusts across E&SE England. Available at http://www.acutemedicine.org.uk/wp-content/uploads/2014/04/Report_Collaborative_MR_Audit_Results_May_2010.pdf (last accessed 3 August 2014)
- Ellitt G, Engblom E, Aslani P, Westerlund T, Chen T. Drug related problems after discharge from an Australian teaching hospital. Pharm World Sci. 2010;32:622–630. doi: 10.1007/s11096-010-9406-9. [DOI] [PubMed] [Google Scholar]
- Grimes TC, Duggan CA, Delaney TP, Graham IM, Conlon KC, Deasy E, Jago-Byrne MC, Brien PO. Medication details documented on hospital discharge: cross sectional observational study of factors associated with medication non-reconciliation. Br J Clin Pharmacol. 2011;71:449–457. doi: 10.1111/j.1365-2125.2010.03834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witherington E, Pirzada O, Avery A. Communication gaps and readmissions to hospital for patients aged 75 years and older: observational study. Qual Saf Health Care. 2008;17:71–75. doi: 10.1136/qshc.2006.020842. [DOI] [PubMed] [Google Scholar]
- Unroe KT, Pfeiffenberger T, Riegelhaupt S, Jastrzembski J, Lokhnygina Y, Colón-Emeric C. Inpatient medication reconciliation at admission and discharge: a retrospective cohort study of age and other risk factors for medication discrepancies. Am J Geriatr Pharmacother. 2010;8:115–126. doi: 10.1016/j.amjopharm.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paterson JM, Allega RL. Improving communication between hospital and community physicians. Feasibility study of a handwritten, faxed hospital discharge summary. Discharge Summary Study Group. Can Fam Physician. 1999;45:2893–2899. [PMC free article] [PubMed] [Google Scholar]
- Scullard P, Iqbal N, White LA, Olla E, Thomson GA. Improved communication between hospital and general practice using online patient discharge summaries. J Telemed Telecare. 2007;13:56–58. [Google Scholar]
- Jansen JO, Grant IC. Communication with general practitioners after accident and emergency attendance: computer generated letters are often deficient. Emerg Med J. 2003;20:256–257. doi: 10.1136/emj.20.3.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Care Quality Commission. 2009. Managing patients' medicines after discharge from hospital. Available at http://www.npc.nhs.uk/ (last accessed 3 August 2014)
- Horwitz LI, Jenq GY, Brewster UC, Kanade S, Van Ness PH, Araujo KL, Ziaeian B, Moriarty JP, Fogerty RL, Krumholz HM. Comprehensive quality of discharge summaries at an academic medical center. J Hosp Med. 2013;8:436–443. doi: 10.1002/jhm.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297:831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 2011. East & South East England specialist pharmacy services. Which patient benefit most from the medicines reconcilaition? A collaborative evaluation of the outcomes of pharmacy-led medicine reconciliation in various care areas. Available at http://www.medicinesresources.nhs.uk/ (last accessed 3 August 2014)
- Dornan T, Ashcroft D, Heathfield H, Lewis P, Miles J, Taylor D, Tully M, Wass V. An in depth investigation into causes of prescribing errors by foundation trainees in relation to their medical education – EQUIP study. Available at http://www.gmc-uk.org/ (last accessed 3 August 2014)
- Tulloch AJ, Fowler GH, McMullan JJ, Spence JM. Hospital discharge reports: content and design. BMJ. 1975;4:443–446. doi: 10.1136/bmj.4.5994.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers K, Tierney M, Singh A, McLean W. Assessment of a seamless care prescription/discharge notes form. Can J Hosp Pharm. 2003;56:14–23. [Google Scholar]
- Pippins JR, Gandhi TK, Hamann C, Ndumele CD, Labonville SA, Diedrichsen EK, Carty MG, Karson AS, Bhan I, Coley CM, Liang CL, Turchin A, McCarthy PC, Schnipper JL. Classifying and predicting errors of inpatient medication reconciliation. J Gen Intern Med. 2008;23:1414–1422. doi: 10.1007/s11606-008-0687-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tulner LR, Kuper IM, Frankfort SV, van Campen JP, Koks CH, Brandjes DP, Beijnen JH. Discrepancies in reported drug use in geriatric outpatients: relevance to adverse events and drug-drug interactions. Am J Geriatr Pharmacother. 2009;7:93–104. doi: 10.1016/j.amjopharm.2009.04.006. [DOI] [PubMed] [Google Scholar]
- National Prescribing Centre. Medicines reconciliation: a guide to implementation. Available at http://www.npc.nhs.uk/improving_safety/medicines_reconciliation/implement.php (last accessed 3 August 2014)
- Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37:360–363. [PubMed] [Google Scholar]
- Jakobsson U, Westergren A. Statistical methods for assessing agreement for ordinal data. Scand J Caring Sci. 2005;19:427–431. doi: 10.1111/j.1471-6712.2005.00368.x. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Vera FJ, Marin Y, Sanchez A, Borrachero C, Pujol E. Illegible handwriting in medical records. J R Soc Med. 2002;95:545–546. doi: 10.1258/jrsm.95.11.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimes T, Delaney T, Duggan C, Kelly J, Graham I. Survey of medication documentation at hospital discharge: implications for patient safety and continuity of care. Ir Med J. 2008;177:93–97. doi: 10.1007/s11845-008-0142-2. [DOI] [PubMed] [Google Scholar]
- Perren A, Previsdomini M, Cerutti B, Donghi D, Marone C. Omitted and unjustified medications in the discharge summary. BMJ Qual Saf. 2009;18:205–208. doi: 10.1136/qshc.2007.024588. [DOI] [PubMed] [Google Scholar]
- Wilson S, Ruscoe W, Chapman M, Miller R. General practitioner–hospital communications: a review of discharge summaries. J Qual Clin Pract. 2001;21:104–108. doi: 10.1046/j.1440-1762.2001.00430.x. [DOI] [PubMed] [Google Scholar]
- Wong JD, Bajcar JM, Wong GG, Alibhai SMH, Huh JH, Cesta A, Pond GR, Fernandes OA. Medication reconciliation at hospital discharge: evaluating discrepancies. Ann Pharmacother. 2008;42:1373–1379. doi: 10.1345/aph.1L190. [DOI] [PubMed] [Google Scholar]
- Boockvar K, Fishman E, Kyriacou CK, Monias A, Gavi S, Cortes T. Adverse events due to discontinuations in drug use and dose changes in patients transferred between acute and long-term care facilities. Arch Intern Med. 2004;164:545–550. doi: 10.1001/archinte.164.5.545. [DOI] [PubMed] [Google Scholar]
- Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- Medical record content structure standards for hospital practice: admission, handover and discharge records. Health Informatics Unit, the UK Royal College of Physicians. Available at https://www.rcplondon.ac.uk (last accessed 3 August 2014)
- Pillai A, Thomas SS, Garg M. The electronic immediate discharge document: experience from the South West of Scotland. Inform Prim Care. 2004;12:67–73. doi: 10.14236/jhi.v12i2.110. [DOI] [PubMed] [Google Scholar]
- Bell CM, Rahimi Darabad P, Orner AI. Discontinuity of chronic medications in patients discharged from the intensive care unit. J Gen Intern Med. 2006;21:937–941. doi: 10.1111/j.1525-1497.2006.00499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner BK, Venarske J, Yu M, Mathis K. Towards the reduction of medication errors in orthopedics and spinal surgery: outcomes using a pharmacist-led approach. Spine. 2008;33:104–107. doi: 10.1097/BRS.0b013e31815e3a5d. [DOI] [PubMed] [Google Scholar]
- Tully MP, Cantrill JA. Insights into creation and use of prescribing documentation in the hospital medical record. J Eval Clin Pract. 2005;11:430–437. doi: 10.1111/j.1365-2753.2005.00553.x. [DOI] [PubMed] [Google Scholar]
- Sibbald B, Wilkie P, Raftery J, Anderson S, Freeling P. Prescribing at the hospital-general practice interface. II: impact of hospital outpatient dispensing policies in England on general practitioners and hospital consultants. BMJ. 1992;304:31–34. doi: 10.1136/bmj.304.6818.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziaeian B, Araujo KB, Ness P, Horwitz L. Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge. J Gen Intern Med. 2012;27:1513–1520. doi: 10.1007/s11606-012-2168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Abdel-Qader DH, Harper L, Cantrill JA, Tully MP. Pharmacists interventions in prescribing errors at hospital discharge: an observational study in the context of an electronic prescribing system in a UK teaching hospital. Drug Saf. 2010;33:1027–1044. doi: 10.2165/11538310-000000000-00000. [DOI] [PubMed] [Google Scholar]
- McMillan TE, Allan W, Black PN. Accuracy of information on medicines in hospital discharge summaries. Intern Med J. 2006;36:221–225. doi: 10.1111/j.1445-5994.2006.01028.x. [DOI] [PubMed] [Google Scholar]
- Midlöv P, Bergkvist A, Bondesson Å, Eriksson T, Höglund P. Medication errors when transferring elderly patients between primary health care and hospital care. Pharm World Sci. 2005;27:116–120. doi: 10.1007/s11096-004-3705-y. [DOI] [PubMed] [Google Scholar]
- Barr R, Chin KY, Yeong K. Improving transmission rates of electronic discharge summaries to GPs. BMJ Qual Improv Rep. 2013 doi: 10.1136/bmjquality.u756.w1013. doi: 10.1136/bmjquality.u756.w1013. [DOI] [PMC free article] [PubMed] [Google Scholar]


