Abstract
A functional corneal graft 34 years after penetrating keratoplasty (PKP) is rare and even rarer is its survival after wound dehiscence. We present a case of a 69-year-old man who had presented to the emergency services in January 2012 with corneal wound dehiscence OS extending to 8 o’clock following blunt trauma. His vision was perception of light. The best corrected visual acuity (BCVA) of the patient prior to graft dehiscence was 20/30. The patient had undergone optical penetrating keratoplasty for healed keratitis in OS in 1978 followed by phacoemulsification with intraocular lens implantation in 2009. Suturing of the graft was performed under topical anaesthesia. At 18 months follow-up, the BCVA was 20/60 with clear graft centrally and specular count was 865 cells/mm2. This case highlights that early and appropriate management of corneal graft dehiscence can achieve good functional outcome even 34 years following PKP.
Background
Graft dehiscence is a known complication after penetrating keratoplasty (PKP) due to the inherent weakness in the wound. Ours was a case of traumatic wound dehiscence 34 years after PKP and remained functional after repair. There are many unique findings in this case. The graft has remained clear for almost 31 years with specular count of 1138 cells/mm2, after which the patient underwent phacoemulsification with explained guarded prognosis. Following phacoemulsification, the patient maintained a clear graft with best corrected visual acuity (BCVA) 20/30. The patient sustained blunt trauma following a fall 3 years after phacoemulsification (34 years after PKP), which led to graft dehiscence that was immediately repaired as an emergency procedure. He maintained a clear graft with BCVA 20/60 at the last follow-up (2 years postoperatively). There are no cases published in the literature of a graft remaining functional for 34 years post PKP with good visual acuity despite resuturing. The longest reported case of wound dehiscence post PKP in the literature has been 33 years.
Case presentation
A 69-year-old man presented to the emergency services of Dr Rajendra Prasad Centre for Ophthalmic Sciences in January 2012 after having fallen a day earlier. He had sustained an eye injury resulting in redness, pain and diminution of vision. On examination, the patient was noted to have dehiscence of a PKP graft at 8 o’clock (extending from 4 o’clock to 11 o’clock) with flat anterior chamber and perception of light vision (figure 1). The patient had undergone optical PKP for healed keratitis in 1978 (34 years prior) followed by phacoemulsification with intraocular lens (IOL) implantation in 2009 (3 years prior) with BCVA of 20/30 postphacoemulsification. The patient was a known hypertensive on irregular treatment, with no other significant medical, social or family history.
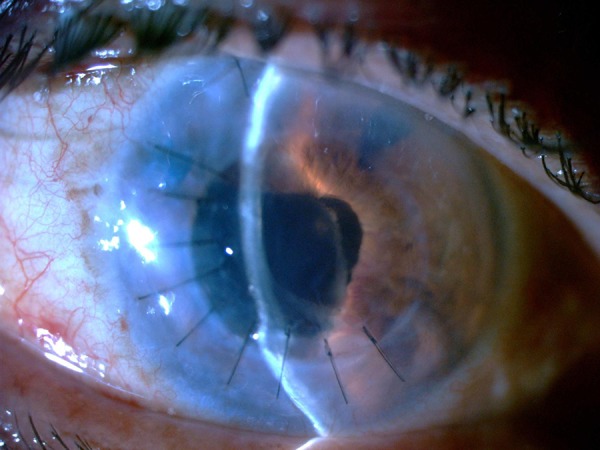
Figure 1.

Preoperative photograph of the eye (image captured by microscope before repair of the wound).
Treatment
Suturing of the graft was performed under topical anaesthesia using 0.5% proparacaine hydrochloride as an emergency procedure. Nine interrupted 10–0 monofilament nylon sutures were applied in the area of wound dehiscence. Intraoperatively subluxation of the IOL–capsular bag complex at 6 o’clock was noted with IOL in the visual axis. As the closure of the wound was of primary importance and the IOL appeared to be stable, the bag IOL subluxation was left untouched.
Outcome and follow-up
The patient had an episode of acute graft rejection 2 months following repair, which successfully resolved with intensive topical prednisolone therapy. Peripheral anterior synechiae (PAS) at 4 o’clock was noted in the area of wound repair (figure 2). Secondary glaucoma occurred in the postoperative period and was managed using topical antiglaucoma medications. Since the IOL was centred and stable, and the patient had a low endothelial cell count, no secondary intervention was performed for capsular bag fixation or PAS release (figure 3). All sutures were removed 18 months postrepair. Fundus examination revealed cup disc ratio of 0.6:1 with dull foveal reflex, no retinal tears or detachment. At 2 years postoperatively, the patient maintained a clear graft centrally with temporal graft haze with BCVA 6/18 and specular count of 865 cells/mm2 (figure 4).
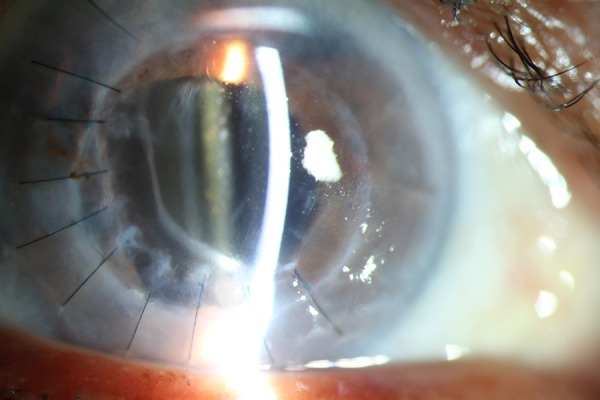
Figure 2.
Slit-lamp photograph on day 4 after wound repair showing intact sutures with well-formed anterior chamber centrally and peripheral anterior synechiae temporally. Inflammatory membrane can be noted over the intraocular lens.
Figure 3.
Decentration of capsular bag with well centred and stable intraocular lens optic.
Figure 4.
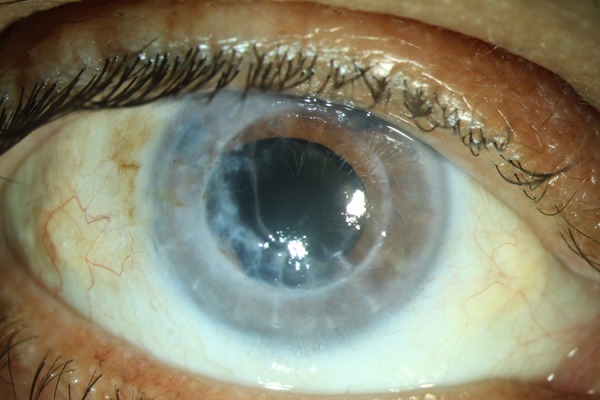
Slit-lamp photograph of the patient after suture removal at 2 years follow-up.
Discussion
Wound dehiscence after PKP is a known complication. It occurs due to an inherently weak graft host junction as compared to that in a normal cornea. Occurrence of dehiscence 34 years after PKP, as in this case, very well proves that because of the biomechanics, the wound after surgery never achieves normal tensile strength.
Nevertheless, having a clear corneal graft 34 years after PKP is very rare and even rarer is the good functional outcome after management of wound dehiscence and graft rejection. It is important to defer additional procedures during the primary repair of a wound dehiscence as the sole objective is to have a closed globe with a well formed anterior chamber. Further intraocular procedures should be contemplated depending on the visual acuity postoperatively and taking into account the endothelial cell count. Our patient developed acute graft rejection despite the use of topical 1% prednisolone acetate eye drops QID, which resolved with intensive topical steroid therapy.
Das et al1 have described 19 cases of post-traumatic wound dehiscence after PKP of which the longest time period is 33 years. Wound dehiscence has also been reported after deep anterior lamellar keratoplasty,2 cataract surgery,3 penetrating globe injury and radial keratotomy.4 Trauma is the most common cause for dehiscence followed by early suture removal2 and increased intraocular pressure. The functional outcome in most of these post traumatic cases depends on the extent of damage to the ocular structures, especially the lens and posterior segment. Steinberg et al5 in their review had noted that severely reduced visual acuity (<hand movement) and lens damage at the time of trauma were the most reliable predictors of final visual outcome. A permanent loss of visual acuity was related to the intraocular damage from vitreous loss, vitreous haemorrhage, retinal tears or detachment rather than the readapted graft.
Learning points.
This is the first reported case in the literature of dehiscence of a penetrating keratoplasty wound 34 years after surgery. It shows that a penetrating keratoplasty wound can never regain the strength of a virgin eye and that the risk of dehiscence exists even many years after surgery.
Timely repair of graft dehiscence can still save the graft and achieve good functional outcome.
Appropriate management of coexisting complications such as subluxated capsular bag, intraocular lens complex, graft rejection and secondary glaucoma.
Long-term immune privilege of the corneal grafts.
Footnotes
Contributors: SG involved in the surgery, patient follow-up and manuscript preparation. NS and JST were involved in the case discussion with supervision of management and manuscript editing.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Das S, Whiting M, Taylor HR. Corneal wound dehiscence after penetrating keratoplasty. Cornea 2007;26:526–9. [DOI] [PubMed] [Google Scholar]
- 2.Mannan R, Jhanji V, Sharma N et al. Spontaneous wound dehiscence after early suture removal after deep anterior lamellar keratoplasty. Eye Contact Lens 2011;37:109–11. [DOI] [PubMed] [Google Scholar]
- 3.Kloek CE, Andreoli MT, Andreoli CM. Characteristics of traumatic cataract wound dehiscence. Am J Ophthalmol 2011;152:229–33. [DOI] [PubMed] [Google Scholar]
- 4.Jammal HM, Dolat WM. Ruptured globe 20 years after radial and transverse keratotomy. Int Ophthalmol 2012;32:51–3. [DOI] [PubMed] [Google Scholar]
- 5.Steinberg J, Eddy MT, Katz T et al. Traumatic wound dehiscence after penetrating keratoplasty: case series and literature review. Eur J Ophthalmol 2012;22:335–41. [DOI] [PubMed] [Google Scholar]


