Abstract
The purpose of this study was to determine if third-year medical students participating in a mandatory 12-week simulation course perceived improvement in decision-making, communication, and teamwork skills. Students participated in or observed 24 acute emergency scenarios. At 4-week intervals, students completed 0-10 point Likert scale questionnaires evaluating the curriculum and role of team leader. Linear contrasts were used to examine changes in outcomes. P-values were Bonferroni-corrected for multiple pairwise comparisons. Student evaluations (n = 96) demonstrated increases from week 4 to 12 in educational value (p = 0.006), decision-making (p < 0.001), communication (p = 0.02), teamwork (p = 0.01), confidence in management (p < 0.001), and translation to clinical experience (p < 0.001). Regarding the team leader role, students reported a decrease in stress (p = 0.001) and increase in ability to facilitate team function (p < 0.001) and awareness of team building (p = <0.001). Ratings demonstrate a positive impact of simulation on both clinical management skills and team leadership skills. A simulation curriculum can enhance the ability to manage acute clinical problems and translates well to the clinical experience. These positive perceptions increase as the exposure to simulation increases.
Keywords: medical education, simulation, communication skills
Introduction
High-fidelity mannequin simulation provides medical students the opportunity for observation, evaluation, and feedback that may not occur in the clinical setting. A high-fidelity simulator, such as the Laerdal SimMan® 3G (Laerdal, Stavanger, Norway), is a mannequin paired with a patient monitor and laboratory results display that allows learners of all levels in health care to simulate the interactions with and treatment of a real patient. The mannequin can be programmed to carry out specific states that mimic illness and injury. A microphone in the mannequin’s mouth, connected to the control room, permits communication. These high-fidelity simulators allow learners to listen to breath sounds, heart sounds, check pupillary response to light, and have a built-in physiologic airway. Learners can perform advanced airway management, insert thoracostomy tubes, foley catheters, and palpate pulses whose strength corresponds to the blood pressure of the simulated patient. Treatment with medications or procedures leads to standardized physiologic responses in the patient’s clinical status that can be programmed for a specific illness. Such high-fidelity simulators are often utilized in the training of medical students.
In the clinical environment, medical students have few opportunities to be the primary provider for critically ill patients, to initiate difficult conversations with patients and families, or to lead a health care team in caring for a patient. However, the transition from student to intern is abrupt and places new demands on a junior physician, who may be expected to care for a critically ill patient independently. This challenge is not only stressful to the intern but also potentially unsafe for the patient [1-3]. Simulation provides a unique and safe environment for students to practice these important skills and for faculty to devote undivided attention to observation and feedback.
At Yale School of Medicine in 2006-07, the lead author of this study (LVE) designed and implemented a mandatory clinical simulation curriculum for third-year medical students during a 12-week Surgery/Emergency Medicine/Anesthesia clerkship. Now in its eighth year, more than 700 students have participated in this simulation course. Three of the co-authors (KLD, JWB, and AT) are core simulation faculty members whose primary academic responsibility has been participating in designing the clinical scenarios and running simulation sessions. RJG, a member of the Surgery faculty, has helped to design the scenarios and participates in the course as both a debriefer and a clinical expert. Each week there are three 1-hour sessions with two teams and eight students per session. The authors undertook this study to determine student perception of the educational value of this comprehensive simulation curriculum, integrated into a third-year clinical clerkship.
Our objectives were to determine if students perceived improvement in decision-making, communication, and teamwork skills over the duration of the course. In addition, we sought to determine the students’ degree of enhanced confidence in their acute clinical problem-solving and team-building skills as well as their perception as to the extent to which their simulation-based skills translate to clinical experiences in the hospital setting.
Methods
Study Design
This was a prospective study conducted at a U.S. medical school during the 2011-12 academic year. This study received a waiver of consent from our institutional review board. Third-year medical students who were enrolled in a mandatory 12-week simulation curriculum during which they managed and/or observed 24 acute emergency medicine or surgical scenarios were included in the study. Students received a 2-hour orientation prior to the start of the simulation curriculum. During this orientation, students signed confidentiality agreements, had the objectives of the course reviewed, and received a hands-on orientation to the Laerdal SimMan® 3G, the simulation room, and all of its capabilities and supplies. In addition, grading for the simulation part of the course was explained. Grading for simulation was based on participation and timeliness; the nature and quality of the clinical decision making did not affect a participant’s grade. All simulation sessions were conducted in Yale Emergency Medicine’s simulation center, which closely mimicked an emergency department patient room but was separated by a one-way mirror from a control room from which the simulator was controlled and the student teams observed. Equipment used for each scenario mirrors that which was used in the Adult Emergency Department. For example, all advanced airway equipment, code cart medications, and foley catheters were the same as students encountered in our hospital. All supplies needed for each case were readily available, and their locations were reviewed during orientation.
Scenario Generation
All scenarios were based on actual cases encountered by the authors in the Emergency Department. Students were exposed to the actual presentation of the patient, experiencing the true vital signs, laboratory values, physical exam findings, and family member interactions that mimicked those experienced by the primary provider for that patient when seen in the Emergency Department. This contributed to the realism of the case. Each case was anonymized and programmed so that student actions would yield physiologic responses seen in the actual patient.
Faculty Roles
Each simulation session included four faculty/resident participants: the coordinator, facilitator, expert, and debriefer. The coordinator was an emergency medicine faculty member with simulation expertise (LVE, KLD, JWB, AT) who operated the computer-based simulation from behind a one-way mirror and provided the patient’s “voice” by communicating through a speaker in the mannequin’s mouth. A senior level emergency medicine (EM) resident (ACC) functioned as the facilitator in the simulation laboratory and played the role of “nurse,” “family member,” and/or “emergency medical service provider.” The EM resident facilitated the flow of the scenario, provided requested laboratory data, electrocardiography, and relevant radiography, and prevented students from becoming sidetracked or misinformed by imperfections in the simulated environment. The faculty expert had clinical expertise in the topics being covered during the session. During each scenario, the assigned team leader requested a consultation from a specialist; the faculty expert received this consultation and responded as if a resident or fellow were requesting the consult, offering help or asking for additional information where appropriate. An additional faculty member functioned as the debriefer, focusing on observation, facilitating student self-reflection, and providing feedback regarding team leadership and communication with team members, patients, and the patient’s family.
Student Roles
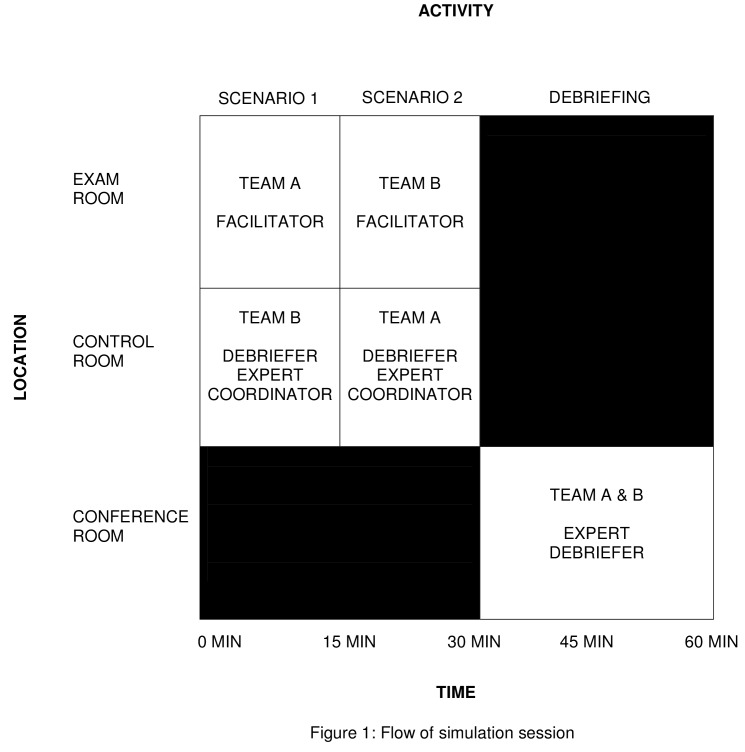
Students attended weekly 1-hour sessions for 12 weeks. Four students at a time, with one student acting as team leader, participated in one scenario, while a second group of students observed from behind a one-way mirror. Groups then switched roles (Figure 1). Each student functioned as a team leader three times over the course of the 12 weeks — once each during the first 4 weeks, the middle 4 weeks, and the final 4 weeks. Each team leader was responsible for calling an expert consultant during the scenario and discussing the patient’s diagnosis with the patient and/or a family member as well as answering questions from the patient regarding diagnosis and prognosis.
Figure 1.
Flow of Simulation Session. During each 60-minute simulation session, four students (Team A) participate in a 15-minute simulation while four students observe (Team B). Students then switch roles for a second 15-minute simulation scenario. All eight students then participate in a 30-minute debriefing session with a faculty expert and faculty debriefer.
Debriefing
At the conclusion of each week’s session, students participated in a debriefing session involving two faculty members; the faculty expert discussed critical actions related to clinical management, and one of the faculty debriefers (LVE, RJG, KLD, JWB, or AT) discussed team interactions as well as leadership and communication skills. In addressing communication, special emphasis was placed on the consultation with the faculty expert and the discussion with the simulated patient and family members. During the consultation, students learned the importance of introducing themselves, providing a diagnosis, conveying the stability of the patient, and stating the purpose of the call, all in the first sentence of the consult. In the discussion with the patient, emphasis was placed on keeping the patient well informed about their progress and the plan, using appropriate and easily understood language conveyed in a supportive and empathetic manner, and asking the patient if he/she had any additional questions.
Student Questionnaire
At the conclusion of the sessions at weeks 4, 8, and 12, each student completed an anonymous questionnaire with responses scored on a 0-10 point Likert scale. Student responses about the simulation curriculum included educational value of participating in the course, development of decision-making skills, development of communication skills, development of teamwork skills, enhanced confidence in managing acute medical problems, and translation to clinical experience in the hospital setting. Student responses to functioning as the team leader included the number of hours spent preparing for the scenario, the stress level as team leader, the ability to facilitate effective team function, and the awareness of team building skills.
Statistical Analysis
Statistical analysis was performed by one of the co-authors (JDD) using repeated measures mixed model analysis. Linear contrasts were used for pairwise comparison of outcomes at each timepoint. The models included a fixed effect for time and a random subject effect. P-values were Bonferroni-corrected for multiple pairwise comparisons. Data are expressed as least squares means and standard errors. All analyses were performed using SAS V 9.2 (Cary, NC).
Results
Over the course of the year, surveys were administered to each group at 4 week intervals (N = 95 for weeks 4 and 12, N = 71 for week 8). Students completed the survey prior to leaving the simulation center these weeks. The survey was not administered to one group during week 8 of one of the 12-week blocks of the study. During weeks 4 and 12, there was a 100 percent response rate, and during week 8, there was a 75 percent response rate.
Educational Value
Student evaluations of the course demonstrated a statistically significant increase in perceived educational value of 0.40 ± 0.14 from week 4 (8.48 ± 1.48) to week 12 (8.88 ± 1.34) (P < 0.01) (Table 1). In addition, student ratings from week 4 to week 12 increased in the following areas: clinical decision-making skills increased by 0.47 ± 0.13 (P < 0.001); teamwork skills increased by 0.41 ± 0.17 (P = 0.02); and translation to clinical experience in the hospital increased by 0.97 ± 0.19 (P < 0.001).
Table 1. Summary of student responses regarding clinical simulation curriculum.
| Mean±SD | Change from week 4 to week 12 (P value) | |
| Educational Value | ||
| Week 4 | 8.48 ± 0.14 | .40 ± 0.14 (<0.01) |
| Week 12 | 8.88 ± 0.14 | |
| Enhanced confidence in managing acute medical problems | ||
| Week 4 | 7.84 ± 0.15 | 0.87 ± 0.17 (<0.001) |
| Week 12 | 8.71 ± 0.15 | |
| Translation to clinical experience in the hospital | ||
| Week 4 | 7.33 ± 0.17 | 0.97 ± 0.19 (<0.001) |
| Week 12 | 8.31 ± 0.17 | |
| Development of decision-making skills | ||
| Week 4 | 8.49 ±0.13 | 0.47 ± 0.13 (<0.001) |
| Week 12 | 8.97 ± 0.13 | |
| Development of communication skills | ||
| Week 4 | 8.25 ± 0.14 | 0.41 ± 0.17 (0.02) |
| Week 12 | 8.66 ± 0.14 | |
| Development of teamwork skills | ||
| Week 4 | 8.43 ± 0.13 | 0.38 ± 0.15 (0.01) |
| Week 12 | 8.81 ± 0.13 | |
Mean values based on a 0-10 Likert scale
Team Leader
Over the 12-week course, student ratings of their ability to facilitate effective team function increased by 1.33 ± 0.21 (P < 0.001) (Table 2). They also reported an increased awareness of team building skills by 0.73 ± 0.18 (P < 0.001). The reported stress level of being team leader decreased by 1.03 ± 0.29 (P = 0.001). Time spent preparing for the team leader role averaged approximately 3 hours (3.16 ± 0.20 hours at week 4, 2.95 ± 0.20 hours at week 12) and did not change significantly between weeks four and 12 (P = 0.213).
Table 2. Summary of student responses regarding role of team leader.
| Mean±SD | Change from week 4 to week 12 (P value) | |
| Stress level as team leader | ||
| Week 4 | 6.04 ± 0.26 | 1.03 ± 0.29 (0.001) |
| Week 12 | 7.07 ± 0.25 | |
| Ability to facilitate effective team function | ||
| Week 4 | 6.79 ± 0.16 | 1.33 ± 0.21 (<0.001) |
| Week 12 | 8.13 ± 0.15 | |
| Increased awareness of team building skills | ||
| Week 4 | 7.52 ± 0.15 | 0.73 ± 0.18 (<0.001) |
| Week 12 | 8.25 ± 0.15 | |
Mean values based on a 0-10 Likert scale
Discussion
Simulation technology has gained widespread acceptance in the training of health care professionals and is felt to be an effective educational medium [4]. Research continues into the educational outcomes of simulation-based teaching as it becomes more commonly adopted by medical schools [1,5-7]. Several institutions have published descriptions of simulator-based curricula focused on the educational needs of medical students during their clinical years [5,8-10]. Simulation-based education has even been incorporated into first-year basic science courses [11].
Despite this, very little has been published regarding either the incorporation of high-fidelity mannequin simulation into undergraduate medical education or the students’ perception of this educational medium. The existing studies describe curricula with few simulation encounters or lack longtitudinal data [10,12,13]. There is no literature that examines student responses to the role of team leader in a simulated resuscitation.
Our longitudinal, 12-week simulation course has been a required part of our third-year medical school curriculum since 2006 and provides a unique opportunity to assess both feasibility and effectiveness of a contemporary and comprehensive experience in the simulation-based clinical education of medical students.
Based on the results of our study, a comprehensive simulation program of this size and duration is well received by third-year medical students. The reported educational value of the course increased with immersion over several months. This longitudinal feature is one that separates it from published descriptions of other medical school simulation programs. This type of program provides students with enhanced confidence in clinical management and translates well to their experience in the hospital. Students reported a tangible enhancement of their decision-making skills and felt that their ability to effectively manage a team improved significantly over the course. This is coupled with the fact that students also reported a decreasing amount of stress when faced with challenging, time-sensitive critical care decisions.
Increasingly, medical schools have recognized the educational value of longitudinal educational experiences for their students. Rather than provide isolated learning experiences in simulation, we have sought to create a longitudinal program with continued exposure to simulation over 3 months. This can pose a difficult scheduling challenge for educators during the clinical years. We have addressed this challenge in several ways, some of which may be generalizable to other medical schools.
First, the simulation course occurs at the same time weekly so that students, residents, and faculty are aware that students will be excused from their clinical responsibilities during 1 hour of one afternoon per week. We are able to accomplish this even though our clerkship includes emergency department shifts and operating room assignments — two clinical experiences with less scheduling flexibility than other clerkships. The students are never scheduled for emergency department shifts during their simulation time, and every surgical attending is made aware that students are to be excused from the OR at the specific time each week. The success and durability of the course has been dependent on the commitment of the faculty based on the time-efficient and unique teaching experience and the positive response of the students to this innovative approach to learning.
Second, the longitudinal experience provides an opportunity for meaningful growth and focused feedback. Such longitudinal experiences can be developed at other schools by creating courses that bridge different specialties and departments; at our institution, we accomplished this by having surgery and emergency medicine integrated into a 12-week clerkship block.
There are several limitations to this study. First is that it relies on medical student self-assessment, and thus may not reflect true clinical strengths and weaknesses. Whether the increase in self confidence that medical students report actually translates to improved performance in clinical medicine was beyond the scope of this study. Our study did not compare the students’ self-assessment to the assessment of students by the faculty. This would be an interesting follow-up study in further examining the validity of the student self-assessment. Another limitation of this study is that it included only a single institution and therefore may not be generalizable. In addition, student ratings related to the team leader role may have been affected by the proximity of the time they filled out the evaluation to the time that they last acted as team leader.
In summary, we developed a comprehensive simulation course with a particular focus on communication skills and team leadership as a mandatory part of a 12-week clinical clerkship and demonstrated that it is well-received by medical students. Students perceive both an educational and a clinical benefit from this simulation program, which is supported by their evaluations of the course. Future studies designed to determine if medical students perform better in the clinical setting after simulation training are needed to determine the ultimate value of this type of course.
Abbreviations
- EM
emergency medicine
Author contributions
Leigh V. Evans: study design, data acquisition, data interpretation and analysis, manuscript draft and revision, study supervision; Ashley C. Crimmins: data acquisition, data interpretation and analysis, manuscript draft and revision; James W. Bonz: study design, data acquisition, data interpretation and analysis, manuscript draft and revision; Richard J. Gusberg: study design, data acquisition, data interpretation and analysis, manuscript draft and revision; Alina Tsyrulnik: study design, data acquisition, data interpretation and analysis, manuscript draft and revision; James D. Dziura: statistical expertise, data interpretation, manuscript draft and revision; Kelly L. Dodge: study design, data acquisition, data interpretation and analysis, manuscript draft and revision.
References
- Laack T, Newman J, Goyal D, Torsher L. A 1-week simulated internship course helps prepare medical students for transition to residency. Simul Healthc. 2010;5(3):127–132. doi: 10.1097/SIH.0b013e3181cd0679. [DOI] [PubMed] [Google Scholar]
- Morgan R, Westmoreland C. Survey of junior hospital doctors’ attitudes to cardiopulmonary resuscitation. Postgrad Med J. 2002;78:413–415. doi: 10.1136/pmj.78.921.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes C, Rhee A, Detsky M, Leblanc V, Wax R. Residents feel unprepared and unsupervised as leaders of cardiac arrest teams in teaching hospitals: a survey of internal medicine residents. Crit Care Med. 2007;35:1668–1672. doi: 10.1097/01.CCM.0000268059.42429.39. [DOI] [PubMed] [Google Scholar]
- Ten Eyck R, Tews M, Ballaster J. Improved medical student satisfaction and test performance with a simulation-based emergency medicine curriculum: A Randomized Controlled Trial. Ann Emerg Med. 2009;54:684–691. doi: 10.1016/j.annemergmed.2009.03.025. [DOI] [PubMed] [Google Scholar]
- Gordon J, Shaffer D, Raemer D, Pawlowski J, Hurford W, Cooper J. A randomized controlled trial of simulation based teaching versus traditional instruction in medicine: a pilot study among clinical medical students. Adv Health Sci Educ Theory Pract. 2006;11:33–39. doi: 10.1007/s10459-004-7346-7. [DOI] [PubMed] [Google Scholar]
- Issenberg S, Petrusa E, McGaghie W. Effectiveness of a computer-based system to teach bedside cardiology. Acad Med. 1999;74:S93–S95. doi: 10.1097/00001888-199910000-00051. [DOI] [PubMed] [Google Scholar]
- Paskins Z, Kirkcaldy J, Allen M, Macdougall C, Fraser I, Peile E. Design, validation and dissemination of an undergraduate assessment tool using SimMan in medical emergencies. Med Teach. 2010;32(1):e12–e17. doi: 10.3109/01421590903199643. [DOI] [PubMed] [Google Scholar]
- McMahon G, Monaghan C, Falchuk K, Gordon J, Alexander E. A simulator-based curriculum to promote comparative and reflective analysis in an internal medicine clerkship. Acad Med. 2005;80:84–89. doi: 10.1097/00001888-200501000-00021. [DOI] [PubMed] [Google Scholar]
- Brim N, Venkatan S, Gordon J, Alexander E. Long-term educational impact of a simulator curriculum on medical student education in an internal medicine clerkship. Simul Healthc. 2010;5:75–81. doi: 10.1097/SIH.0b013e3181ca8edc. [DOI] [PubMed] [Google Scholar]
- Weller J. Simulation in undergraduate medical education: bridging the gap between theory and practice. Med Educ. 2004;38:32–38. doi: 10.1111/j.1365-2923.2004.01739.x. [DOI] [PubMed] [Google Scholar]
- Euliano T. Small group teaching: clinical correlation with a human patient simulator. Adv Physiol Educ. 2001;25(1-4):36–43. doi: 10.1152/advances.2001.25.1.36. [DOI] [PubMed] [Google Scholar]
- Gordon J, Wilkerson W, Shaffer D, Armstrong E. “Practicing” medicine without risk: Students’ and educators’ responses to high-fidelity patient simulation. Acad Med. 2001;76:469–472. doi: 10.1097/00001888-200105000-00019. [DOI] [PubMed] [Google Scholar]
- Takayesu J, Farrell S, Evans A, Sullivan J, Pawlowski J, Gordon J. How do clinical clerkship students experience simulator-based teaching? A qualitative analysis. Simul Healthc. 2006;1:215–219. doi: 10.1097/01.SIH.0000245787.40980.89. [DOI] [PubMed] [Google Scholar]