Abstract
Objective
African Americans are disproportionately burdened by asthma. We assessed the individual and joint contribution of socioeconomic status (SES) on asthma morbidity among African American youth.
Methods
We examined 686 African Americans (8–21 years) with asthma. To account for the joint effects of SES, a composite index was derived from maternal educational attainment, household income, and insurance status. Ordinal logistic regression was used to estimate the individual and joint effect of SES on asthma control. Models were adjusted for age, sex, controller medication use, in utero smoke exposure, family history of asthma, family history of rhinitis, breastfeeding, daycare attendance, and mold exposure.
Results
Participants were classified as Poorly Controlled Asthma (40.8%), Partially Controlled Asthma (29.7%), or Controlled Asthma (30.2%). Of the individual SES indicators, low income was the strongest predictor of poor asthma control. Children with low income had worse asthma control than those with higher income (OR 1.39; 95%CI 0.92–2.12). The SES index ranged from 4–9. SES was associated with 17% increased odds of poor asthma control with each decrease in the index (95%CI 1.05–1.32). The SES index was associated with asthma-related symptoms, nocturnal awakenings, limited activity, and missed school days.
Conclusions
The negative effects of SES were observed along the entire socioeconomic gradient, and the adverse asthma outcomes observed in African American youth were not limited to the very poor. We also found that the SES index may be a more consistent and useful predictor of poor asthma outcomes than each indicator alone.
Keywords: Health status disparities, youth, income, education, minority health
INTRODUCTION
African American children have among the highest asthma prevalence and mortality rates in the U.S. (1). Compared with white children, African Americans have higher rates of hospitalizations and emergency room visits (1), and are more likely to report missed school days due to their asthma (2). This discrepancy in asthma outcomes is multifactorial and greatly influenced by social adversities, such as poverty, that disproportionately affect African American populations (3). Socioeconomic status (SES) is often measured by educational level, annual household income, and insurance status (4–6). Individuals with low educational attainment are at high risk for poor health literacy (7), and low parental literacy is associated with moderate and severe persistent asthma as well as higher rescue medication use in children (8). Moreover, individuals with low educational attainment have reduced insurance coverage which can limit optimal access to healthcare (9, 10). Lastly, households in the lowest income levels are more likely to perceive financial burden in managing their child’s asthma, have higher rates of urgent care use, and experience missed school days due to asthma (11).
Despite the number of studies assessing the association of individual indicators of SES and asthma (8, 12–14), there is still insufficient knowledge regarding what the joint effect of these SES indicators have on asthma outcomes and the effect of these indicators along the entirety of the socioeconomic gradient. Effective interventions are dependent on understanding the full impact of SES on asthma as well as the specific aspects of SES that contribute to poor asthma outcomes. Previously, we demonstrated that a composite score of socioeconomic status was a better a predictor of asthma susceptibility in minority populations than each socioeconomic indicator alone (15). We aim to examine both the individual and joint contribution of maternal educational attainment, annual household income, and insurance status on asthma control among African American youth living in the San Francisco Bay Area. Some of the results of this study have been previously reported in the form of an abstract (16).
METHODS
Study Population
Study of African Americans, Asthma, Genes & Environments (SAGE II) is an on-going case control study of African American youth with asthma in the San Francisco Bay Area initiated in 2008, designed to examine the complex genetic and socio-environmental contributors to asthma prevalence, control, and severity among minority children and adolescents. Participants are aged 8–21 years and recruited through a combination of community and clinic-based recruitment at urban-based health maintenance organizations or community health centers. The parents and all four grandparents of the participants must self-identify as African Americans to be eligible for the study. Asthma is defined as physician diagnosis, report of symptoms, and asthma controller or rescue medication use within the last 2 years. Participants are excluded if they reported any of the following: 1) 10 or more pack-years of smoking; 2) any smoking within 1 year of recruitment date; 3) history of lung diseases other than asthma (cases) or chronic illness (cases and controls); or 4) pregnancy in the third trimester. All local institutional review boards approved the study and all parents/participants provided appropriate written consent/assent.
SAGE II has enrolled 1,556 participants (920 cases and 636 controls) from 2008 to August 2013. The analyses presented here were limited to children with asthma. Participants were excluded from the analysis if there was no self-reported maternal educational level (n = 8), annual household income (n = 152), or insurance status history (n = 3) or had missing demographic or covariate information (n = 71). The final analytical sample size was 686.
Scale and Measurements
Trained interviewers administered comprehensive questionnaires to the parents/caretakers of the participants or to the participants themselves, if aged 18 years or older, to collect basic socio-demographic information, medical histories, and environmental exposure-related information. The primary exposures (i.e. SES indicators) for this analysis were maternal educational attainment, annual household income, and insurance type. For this study, education was considered a stable measure of SES (17), income was indicative of current access to resources (5, 18), and insurance status was a marker of access to healthcare services (6). We derived a composite socioeconomic index (SES index)(15, 19–21) for each participant by summing the ordinal rank scores as follows: Maternal educational level was categorized into low (less than high school graduate, score=1), medium (high school graduate, score=2), and high (some college or higher, score=3). Reported annual income was divided into tertiles based on the study population distribution as seen in Table 1, with the lowest income level receiving a score of 1 and the highest income level a score of 3. Participants were asked whether they had no health insurance; government subsidized insurance (i.e., Medicaid) with care through community-based clinics; government subsidized insurance through a closed health network such as Kaiser Permanente, who provides a government subsidized insurance option through California’s Medicaid program; privately owned closed health network insurance (i.e., Kaiser Permanente); or other private insurance including preferred provider organizations. Medical insurance was then scored as follows: no health insurance (score=1), government subsidized insurance with care through community-based clinics (score=2), and government subsidized insurance through a closed health network or privately owned closed health network insurance or other private insurance (score=3). Thus, the SES index varied between 3 and 9, with each unit weighted equally and higher values indicating higher SES. After collapsing extreme low scores to limit the effect of outliers, the SES index used for our analyses ranged from 4 to 9.
Table 1.
Selected characteristics of SAGE II participants with asthma
| Controlled | Partially Controlled |
Poorly Controlled |
p-value | |
|---|---|---|---|---|
| N | 207 | 204 | 275 | |
| Age, median (IQR) | 13.4 (10.5, 16.3) | 13.5 (10.9, 16.1) | 13.5 (10.7, 16.8) | 0.86 |
| Sex, n (%) | 0.44 | |||
| Male | 100 (48.3) | 105 (51.5) | 149 (54.2) | |
| Maternal Education*, n (%) | 0.03 | |||
| Low | 19 (9.2) | 27 (13.2) | 50 (18.2) | |
| Medium | 52 (25.1) | 51 (25.0) | 77 (28.0) | |
| High | 136 (65.7) | 126 (61.8) | 148 (53.8) | |
| Annual Household Income, n (%) | <0.001 | |||
| < 25 K | 53 (25.6) | 83 (40.7) | 139 (50.5) | |
| 25–100 K | 124 (59.9) | 97 (47.5) | 117 (42.5) | |
| > 100 K | 30 (14.5) | 24 (11.8) | 19 (6.9) | |
| Insurance Status†, n(%) | <0.001 | |||
| No Insurance | 2 (1.0) | 2 (1.0) | 6 (2.2) | |
| Public | 59 (28.5) | 83 (40.7) | 136 (49.5) | |
| Public-Closed HN | 31 (15.0) | 22 (10.8) | 36 (13.1) | |
| Closed HN | 98 (47.3) | 87 (42.6) | 84 (30.5) | |
| Private | 17 (8.2) | 10 (4.9) | 13 (4.7) | |
| SES Index‡, median (IQR) | 8 (6,8) | 7 (6,8) | 6 (5,8) | <0.001 |
| In Utero Smoke Exposure, n(%) | 0.02 | |||
| Yes | 31 (15.0) | 45 (22.1) | 71 (25.8) | |
| Indoor Exposure to Mold, n(%) | ||||
| Yes | 57 (27.5) | 59 (28.9) | 97 (35.3) | 0.14 |
| NO2 exposure(ppb)§, Median (IQR) | 10.6 (8.1, 15.5) | 10.9 (8.4, 15.6) | 11.6 (8.6, 15.5) | 0.60 |
| Missing, n(%) | 30 (18.4) | 42 (20.6) | 41 (14.9) | |
| BMI Percentile, Median (IQR) | 85 (66.0, 97.0) | 86.5 (59.8, 97.0) | 88 (60.0, 97.0) | 0.92 |
| Missing, n(%) | 16 (7.7) | 12 (5.6) | 12 (4.4) | |
| Global African Ancestry‖, Median (IQR) | 0.83 (0.75, 0.87) | 0.82 (0.75, 0.86) | 0.83 (0.75, 0.86) | 0.69 |
| Missing, n(%) | 26 (12.6) | 19 (9.3) | 38 (13.8) | |
| Family History of Atopy, n(%) | ||||
| Asthma | 156 (75.4) | 155 (76.0) | 229 (83.3) | 0.06 |
| Eczema | 101 (48.8) | 111 (54.4) | 152 (55.3) | 0.33 |
| Allergic Rhinitis | 145 (70.0) | 122 (59.8) | 163 (59.3) | 0.03 |
| History of Breastfeeding, n(%) | 0.005 | |||
| Yes | 136 (65.7) | 114 (55.9) | 140 (50.9) | |
| Early Daycare Attendance, n(%) | 0.007 | |||
| Yes | 167 (80.7) | 155 (76.0) | 188 (68.4) | |
| Medication Use**, n(%) | <0.001 | |||
| No Medications | 33 (15.9) | 13 (6.4) | 10 (3.6) | |
| Rescue Inhalers | 55 (26.6) | 50 (24.5) | 50 (16.2) | |
| Controller Monotherapy | 93 (44.9) | 104 (51.0) | 134 (48.7) | |
| Combination Therapy | 26 (12.6) | 37 (18.1) | 81 (29.5) | |
| Oral Corticosteroids, n(%) | <0.001 | |||
| Yes | 12 (5.9) | 47 (23.3) | 83 (30.3) | |
| Unknown | 2 (1.0) | 1 (0.5) | 3 (1.1) | |
Maternal education categorized into low (less than high school graduate), medium (high school graduate), and high (some college or higher)
Public: government subsidized insurance with care through community-based clinics; Public-Closed HN: government subsidized insurance with care through closed health network; Closed HN = closed health network
Composite Socioeconomic Index: derived from reported maternal education attainment level, annual household income, and insurance status
Nitrogen Dioxide exposure, ppb= parts per billion, represents average 24hr-NO2 exposure for the 30 days prior to recruitment
Ancestry proportions derived from genome wide data
Rescue Inhaler indicates the use of short acting Beta-Agonist as only medication, monotherapy indicates the use of inhaled corticosteroids, leukotriene receptor antagonist, or theophylline to control asthma, combination therapy indicates the concomitant use of two or more controller medications with or without long-acting beta agonists, and oral corticosteroids indicates any participant requiring oral corticosteroids in the 12 months prior to recruitment
To account for the asthma controller medications participants might have been using, we asked the participants and their primary caretaker to identify and list their asthma prescriptions. Responses were grouped into five different treatment categories: 1) no medications, 2) rescue inhalers/short-acting beta agonists only, 3) controller monotherapy, 4) combination therapy, and 5) oral corticosteroids. Monotherapy included participants who were using an inhaled corticosteroid, leukotriene receptor antagonist, or theophylline to control their asthma. The combination therapy group described participants with the concomitant use of two or more controller medications with or without long-acting beta agonists, and participants using oral corticosteroids were classified into a separate category.
Outcome Measurements
The National Heart, Lung, and Blood Institute’s (NHLBI) definition of asthma control is a composite score and the accepted standard to measure control (22). Asthma control was derived from information collected through a modified version of the 1978 American Thoracic Society–Division of Lung Diseases Epidemiology Questionnaire (23) on symptoms, nighttime awakening, interferences with normal activities, and rescue medication use during the week prior to participant recruitment and interview and lung function measurements. Specifically, participants with a Forced Expiratory Volume in One Second (FEV1) or FEV1/Forced Vital Capacity Ratio of less than 80% were classified as having worse control. Using a modification of the NHLBI guidelines to fit our questionnaire data, asthma control was defined as controlled, partially controlled, or poorly controlled (Table 2) (24). Secondary outcomes included presence of daytime/nocturnal symptoms in the week prior to recruitment, asthma-related activity limitations in the week prior to recruitment, report of missed school days due to asthma in the previous 12 months, report of oral corticosteroids in the previous 12 months, and FEV1 <80% of predicted by Hankinson et al. spirometric reference equations for African Americans (25).
Table 2.
Criteria for determining asthma control*
| Participants with asthma were considered to have their asthma under control if they met all of the following: |
|---|
| 1. Daytime symptoms no more than twice per week |
| 2. No limitation of activities caused by asthma |
| 3. No nocturnal symptoms |
| 4. Use of rescue medication no more than twice per week |
| 5. FEV1 or FEV1/FVC ratio ≥80% |
| Asthma control for participants not meeting at least 1 of these criteria was classified as partially controlled, and participants with at least 3 measures present were classified as having uncontrolled asthma. |
NHLBI Third Expert Panel on the Management of Asthma. Guidelines for the diagnosis and management of asthma: full report 2007
Selection of Covariates
Consistent with previous studies, age (1, 13), sex (26), and in utero smoke exposure (27) (i.e., maternal smoking during pregnancy) were considered potential confounders and included in the analyses. Additional covariates were considered as confounders and included in the final model if they were associated with asthma control (P<0.2). We identified the following covariates: use of asthma controller medications, history of breastfeeding, daycare attendance, family history of asthma, family history of allergic rhinitis, and report of mold exposure in the home. History of breastfeeding was a positive response to the question “Was the child ever breastfed?”; daycare attendance was report of the participant ever being in a daycare setting with at least 5 other unrelated children; and a family history of asthma was the report of asthma in at least one of the participant’s siblings, parents, and/or grandparents. Covariates considered, but not selected, included secondhand smoke exposure, global African Ancestry estimates from genome-wide data, and elevated total serum IgE (>100 IU/mL). We also considered the role of obesity, as there is a strong link between obesity and SES (28); however, obesity was not observed to affect the relationship between SES and asthma control in our population, even when we stratified the results by sex (29). Lastly, we considered exposure to air pollution as a confounder of the association between SES and asthma control. We used the 30-day average of 24-hour maximum nitrogen dioxide (NO2) exposure as a marker of traffic related air pollution. Despite several studies demonstrating an increased risk of asthma (30), a reduction in pulmonary function (31), and an increase report of asthma-related symptoms with NO2 exposure (31), we did not find an association between NO2 and asthma control in our population. Moreover, NO2 exposure was not associated with our SES index; thus it was not included as a covariate in our final model.
Statistical Analysis
Baseline study characteristics of participants with controlled, partially controlled, and poorly controlled asthma were compared using Student t-test for continuous variables with normal distribution, Kruskal-Wallis test for variables with non-parametric distribution, and chi square tests. Ordinal logistic regression was used to estimate the association of the SES predictor of interest with one level of asthma control (controlled asthma, partially controlled asthma, and uncontrolled asthma) and a worse level of asthma before and after controlling for selected covariates. This model assumes parallel regression lines for the three categories of asthma control. Because the two lines have the same parameter estimates, there is only one odds ratio for each predictor variable in the model (i.e., a single odds ratio (OR) is reported to compare controlled versus partially/poorly controlled asthma or controlled/partially controlled versus poorly controlled asthma) (32). After verifying the proportional odds assumption, we used ordinal logistic regression to calculate unadjusted and adjusted odds ratios and 95% CIs. Lastly, we estimated what proportion of the observed SES effect was explained by reported mold exposure by using the Imai, Keele, Tingley and Yanonoto bootstrapping method (33). All analyses were conducted with R 2.15.1 (34).
RESULTS
We excluded 234 individuals due to missing socioeconomic data or covariate information. Non-response to survey items regarding individual or household income is a common problem that plagues health disparities research. It is estimated that non-response can range from 20–50% (35) and our study falls within this range with approximately 20% of non-response to our income question. When we compared included participants versus excluded participants in the study, we observed that included participants were significantly younger (13.3 vs. 14.5, p=0.02) and were less likely to have mothers who had completed some college or greater (56.1 vs. 64.1%, p=0.03). Exclusion of these participants may have resulted in an over-estimation of the association between education and asthma control; however, there was no association made between education and asthma control in the adjusted models so its unlikely that exclusion of this sub-population would have biased our results.
Characteristics of the children and adolescents with asthma are displayed in Table 1. Greater than two-thirds of SAGE II participants had either poorly controlled asthma (40.1%) or partially controlled asthma (29.7%), with 30.2% of participants classified as controlled asthma. Participants with poorly controlled asthma were more likely to have mothers with lower levels of educational attainment, to be poorer, and to have less insurance coverage compared with those with controlled asthma. The overall median SES index was lower for individuals with poorly controlled asthma compared than those with partially controlled or controlled asthma (6 vs. 7 and 8, p<0.001). Participants with poorly controlled asthma were also more likely to report history of in utero smoke exposure and less likely to have been breastfed or have attended a daycare compared with those with controlled asthma.
Asthma Control
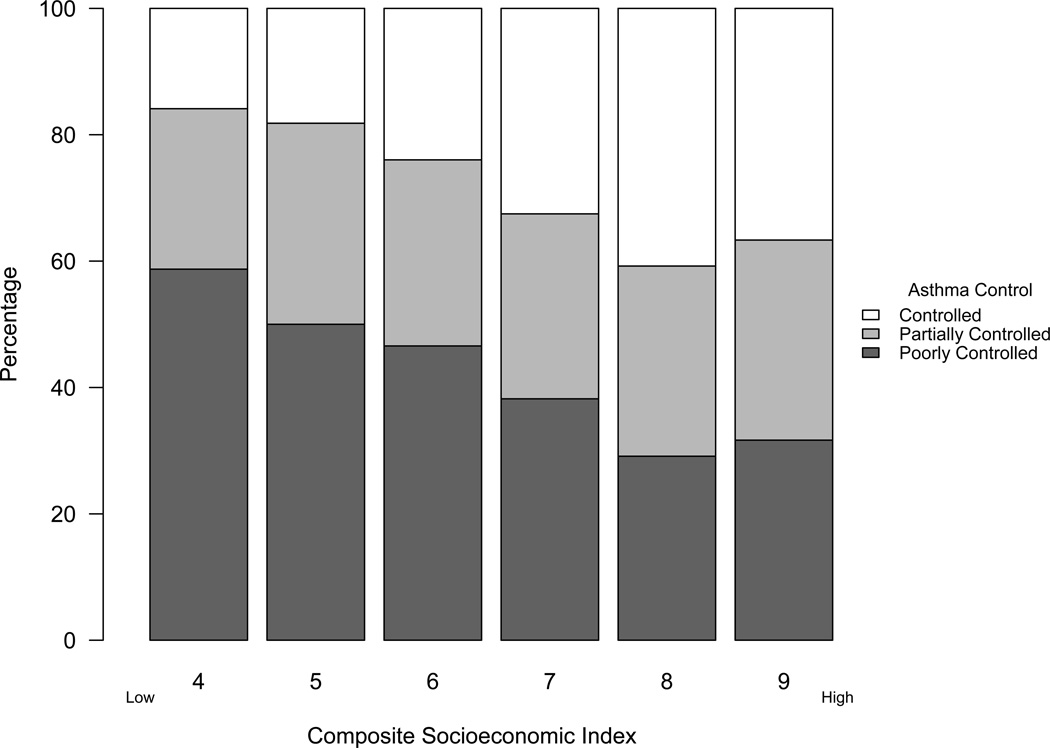
Poorly controlled asthma was associated with low maternal educational attainment, low income and government-subsidized insurance with care through community-based clinics in unadjusted analyses (Table 3). However, in the adjusted model, none of the independent SES predictors remained significant. While we did not find significant evidence of an independent association going from the highest income bracket to the lowest with poor asthma control (OR 1.39), the association (95% CI 0.92–2.12) suggests that low income was associated with worse asthma control (p = 0.12). The joint contribution of the indicators, captured by the SES index, was significantly associated with poor asthma control in the adjusted analysis. The adjusted analysis included reported mold exposure, which was independently associated with poor asthma control in the adjusted model (OR 1.49; 95%CI 1.08–2.05). In a mediation analysis, reported mold exposure accounted for less than 5% of the observed SES effect on asthma control (2.1%; 95%CI 1.2–2.2%, p<0.001). Children with poor asthma control were more likely to be lower on the socioeconomic gradient (OR 1.17 for each unit decrease, 95%CI 1.05–1.32, Table 3), and with the lower socioeconomic gradient there is a greater percentage of children with worse asthma control (Figure 1).
Table 3.
Independent and joint effect of indicators of socioeconomic status on asthma control
| Socioeconomic Indicator | Unadjusted OR (95% CI) | Adjusted OR* (95% CI) |
|---|---|---|
| Maternal Education‡ | ||
| Low | 1.94 (1.28 – 2.97) | 0.94 (0.56 – 1.56) |
| Medium | 1.28 (0.93 – 1.77) | 0.90 (0.63 – 1.30) |
| High | Referent | -- |
| Low Income§ | 2.07 (1.48 – 2.91) | 1.39 (0.92 – 2.12) |
| Insurance Status‖, n(%) | ||
| No Insurance | 3.34 (0.88 – 14.43) | 2.42 (0.57 – 11.30) |
| Public | 2.34 (1.25 – 4.41) | 1.72 (0.86 – 3.46) |
| Public-Closed HN | 1.44 (0.71 – 2.92) | 1.45 (0.69 – 3.07) |
| Closed HN | 1.12 (0.60 – 2.11) | 1.54 (0.79 – 3.00) |
| Private | Referent | -- |
| SES Index† | 1.33 (1.20 – 1.46) | 1.17 (1.05 – 1.32) |
Adjusted for age, sex, in utero smoke exposure, history of breastfeeding, daycare attendance, family history of asthma, family history of allergic rhinitis, reported mold exposure, and asthma control medication use
Maternal education categorized into low (less than high school graduate), medium (high school graduate), and high (some college or higher)
Low Income: Odds ratio displayed represents the odds of going from a high income to a low income
Public: government subsidized insurance with care through community-based clinics; Public-Closed HN: government subsidized insurance with care through closed health network; Closed HN = closed health network
Composite Socioeconomic Index: derived from reported maternal education attainment level, annual household income, and insurance status. Odds Ratio reported is for each unit decrease in the index.
Figure 1.
Proportion of children with Controlled, Partially Controlled, and Poorly Controlled asthma along the composite socioeconomic index (P for trend = 0.005)
Secondary Outcomes
Of the individual socioeconomic indicators, reported household income was most predictive of reporting asthma-related symptoms and was associated with report of activities limited by asthma (OR 1.82; 95%CI 1.08–3.14), missed school days (OR 1.84; 95%CI 1.10–3.10), and, while not statistically significant, with nocturnal symptoms (OR 1.52; 95%CI 0.90–2.63) (Table 4). Participants with no health insurance had increased odds of reporting nocturnal symptoms (OR 5.41; 95% CI 1.14–31.1) and activities limited by asthma (OR 7.05; 95%CI 1.46–41.8) compared with those with private insurance. Similarly, participants with government subsided health insurance with care through community-based clinics had increased odds of reporting activities limited by asthma (OR 2.92; 95%CI 1.27–7.21) than those with private insurance. The SES index was consistently more predictive of asthma-related symptoms compared to examining each indicator separately. We found that there were increased odds of reporting all symptoms (Table 4) with each unit decrease in the SES index. Despite the consistent finding with symptoms, pulmonary function, as measured by a FEV1 <80% of predicted, was not associated with the SES index.
Table 4.
Odds ratio^ for the association between secondary outcomes and socioeconomic status indicators and covariates
| Symptoms | Nocturnal | Activities | Missed School |
Oral Steroids^^ | FEV1<80% | |
|---|---|---|---|---|---|---|
| SES Index‡ | 1.20 (1.05–1.37) | 1.26 (1.11–1.44) | 1.32 (1.51–1.16) | 1.89 (1.14–3.21) | 1.07 (0.92–1.24) | 0.89 (0.71–1.12) |
| Maternal Education* | ||||||
| Low | 0.91 (0.49–1.69) | 0.87 (0.49–1.56) | 0.75 (0.42–1.35) | 0.86 (0.46–1.60) | 0.82 (0.43–1.52) | 0.97 (0.35–2.52) |
| Medium | 1.02 (0.67–1.55) | 0.89 (0.58–1.36) | 0.66 (0.43–1.01) | 0.97 (0.62–1.51) | 0.78 (0.47–1.27) | 1.20 (0.58–2.40) |
| High | Reference | -- | -- | -- | -- | -- |
| Low Income§ | 1.05 (0.66–1.68) | 1.52 (0.90–2.63) | 1.82 (1.08–3.14) | 1.84 (1.10–3.10) | 1.22 (0.66–2.36) | 0.72 (0.33–1.66) |
| Insurance Status† | ||||||
| No Insurance | 5.36 (0.79–108.3) | 5.41 (1.14–31.1) | 7.05 (1.46–41.8) | 0.86 (0.10–5.56) | 0.59 (0.03–4.76) | 0.53 (0.02–4.80) |
| Public | 1.34 (0.61–2.91) | 1.55 (0.70–3.61) | 2.92 (1.27–7.21) | 0.70 (0.29–1.73) | 1.46 (0.59–4.02) | 0.48 (0.14–1.89) |
| Public-Closed HN | 0.89 (0.39–2.03) | 0.78 (0.32–1.95) | 1.93 (0.79–5.00) | 0.78 (0.30–2.01) | 1.58 (0.59–4.57) | 0.75 (0.20–3.14) |
| Closed HN | 1.01 (0.48–2.10) | 1.03 (0.48–2.34) | 1.53 (0.68–3.70) | 0.72 (0.31–1.68) | 0.99 (0.41–2.70) | 0.76 (0.25–2.86) |
| Private | Reference | -- | -- | -- | -- | -- |
| Covariates | ||||||
| Sex, Male | 0.96 (0.69–1.34) | 1.10 (0.78–1.55) | 0.95 (0.68–1.34) | 1.34 (0.94–1.92) | 1.15 (0.78–1.71) | 0.98 (0.54–1.78) |
| Age | 1.08 (1.03–1.13) | 1.03 (0.98–1.09) | 1.05 (1.00–1.10) | 0.90 (0.85–0.95) | 0.95 (0.90–1.01) | 1.05 (0.97–1.14) |
| Family History of Asthma, Yes | 1.36 (0.90–2.05) | 1.50 (0.96–2.37) | 1.73 (1.11–2.74) | 1.24 (0.79–1.94) | 1.54 (0.91–2.69) | 0.96 (0.48–2.08) |
| Family History of Allergic Rhinitis, Yes | 0.97 (0.68–1.40) | 0.82 (0.57–1.19) | 1.17 (0.81–1.69) | 1.04 (0.71–1.52) | 0.91 (0.60–1.40) | 1.09 (0.58–2.10) |
| Mold Exposure, Yes | 1.19 (0.82–1.71) | 1.27 (0.88–1.84) | 1.42 (0.99–2.04) | 1.29 (0.88–1.90) | 1.29 (0.84–1.96) | 1.34 (0.71–2.47) |
| In Utero Smoke Exposure, Yes | 1.34 (0.86–2.12) | 0.86 (0.55–1.32) | 1.22 (0.79–1.85) | 0.61 (0.38–0.98) | 0.85 (0.52–1.39) | 1.48 (0.74–2.86) |
| History of breastfeeding, Yes | 0.94 (0.66–1.35) | 0.89 (0.62–1.28) | 0.89 (0.62–1.27) | 0.73 (0.50–1.07) | 0.84 (0.55–1.27) | 0.46 (0.24–0.86) |
| Early daycare attendance, Yes | 1.00 (0.67–1.47) | 0.77 (0.52–1.14) | 1.05 (0.71–1.56) | 0.65 (0.43–0.98) | 0.85 (0.54–1.33) | 0.65 (0.35–1.23) |
Symptoms, wheeze or shortness of breath in past week; nocturnal, woken by asthma in past week; activities, activities limited by asthma in past week; missed school, missed school days due to asthma in last year; Oral Steroids, reported oral corticosteroids in the previous 12 months
ORs represent multivariable associations between a given characteristic and secondary outcomes adjusted for the other covariates in the table, as well as for asthma controller medication use.
Composite Socioeconomic Index: derived from reported maternal education attainment level, annual household income, and insurance status. Odds Ratio reported is for each unit decrease in the index.
Maternal education categorized into low (less than high school graduate), medium (high school graduate), and high (some college or higher)
Low Income: Odds ratio displayed represents the odds of going from a high income to a low income
Public: government subsidized insurance with care through community-based clinics; Public-Closed HN: government subsidized insurance with care through closed health network; Closed HN = closed health network
Model also adjusted for asthma control in addition to the covariates listed in table.
DISCUSSION
With this study, we identified that specific health disparities exist among African American youth with asthma along the entirety of the socioeconomic gradient. African American children and adolescents not only have increased odds of poor asthma control but also of increased asthma-related symptoms and missed school days with each step down the socioeconomic gradient. These associations were independent of the use of an asthma controller medication, including inhaled corticosteroids, in utero smoke exposure, history of breastfeeding, history of daycare attendance, and report of mold exposure. Compared with the examination of the individual SES indicators, the SES index was shown to be a more accurate and consistent predictor of poor asthma outcomes.
Previously, it has been suggested that the finding of poor asthma outcomes associated with SES may be related to increased exposure to indoor and outdoor air pollutants (14, 36–39). Individuals with low SES are more likely to live in areas with high levels of air pollution exposure and live in substandard housing conditions (40), which increases the exposure to cockroach and mold antigen (41). In our study, we included the self-report of mold exposure as a marker of substandard housing in our final model. In addition, mold exposure was an independent predictor of poor asthma control in our population, yet did not explain the observed effect of SES on asthma control. We also considered the role of air pollution, as measured by nitrogen dioxide (a common marker of traffic related air pollution) as a mediator, but found no significant association between air pollution and the SES index or with asthma control. The models presented were robust to the inclusion of environmental exposure measures; this suggests that the effects of SES are imparted through mechanisms that are not limited to environmental exposures.
Individual SES indicators not only represent what that indicator is measuring but also account for the unmeasured variables associated with the particular indicator. For example, a low household income will affect where an individual lives and the ability to pay for medications(42) while the highest level of education completed by the child’s parent will impact their health literacy (7). Lastly, insurance status will determine if the child will have access to preventative services and chronic disease management (43). The joint effect of these indicators is captured in the composite socioeconomic index. Knowing the joint effect of SES on asthma is important, as it will allow us to identify a particularly high-risk population for individualized interventions that target social determinants in order to improve outcomes (44–47). Moreover, the delivery of effective asthma management must consider and address stressors in the context of concurrent, multiple, adverse living conditions in all patients that may have not been targeted in more traditional asthma intervention programs (40). For example, The Moving to Opportunity Study allowed families from high poverty areas and public housing to move to apartments in better neighborhoods. Families who moved rated their children’s asthma to be less severe after the move (48). The Neighborhood Asthma Coalition and the Asthma Coach programs demonstrated that addressing topics that may appear to be unrelated to asthma, such as problems with landlords, domestic disputes, or community violence, led to reduced acute care visits and increased confidence in asthma management (45). The Medical Legal Partnership, which integrates legal assistance into patient care to remove barriers that impede health, was shown to reduce emergency room visits and hospitalizations and lessen asthma severity in inner-city adults with asthma (46).
Adversities and stress related to socioeconomic status negatively impact asthma by reducing access to quality asthma management and preventive medications. These stressors also increase the risk of asthma exacerbations (14, 40, 49, 50). The physiological response to environmental, social, and personal stressors is referred to as allostatic load, which is the body’s adaption response to psychosocial stress (51). As allostatic load increases, the ability to effectively respond to stress deteriorates and results in poor health outcomes. Thus it is possible that allostatic load may play a role among children with lower SES to affect asthma outcomes. In addition, individuals with low SES have little control over changing their personal environment to reduce exposure to important risk factors for asthma (52, 53). This is particularly relevant to our patient population in the San Francisco Bay Area, which is composed of a high minority, urban population with vast income disparities and exposure to violence.
The limitations of this study relate to the cross-sectional nature of the study, the variability of SES indicators, and generalization of results. The temporal relationship between SES indicators and asthma is not well defined since information on SES and asthma was collected at the same time. Secondly, while education tends to be stable over time, income and insurance coverage/type may fluctuate, and using them as indicators of SES may provide different results at different points in time. Longitudinal studies are needed to confirm the temporal sequence of the results and to better elucidate the impact of SES on the course of asthma. Our assessment of asthma control was also limited to the one week prior to recruitment, which may have over or under-estimated the true asthma control participants. This would have resulted in nondifferential misclassification and biased the results towards the null. A more in-depth assessment into neighborhood effects would provide a more holistic understanding of the different factors that influence asthma status and outcomes. Finally, participants were recruited as part of a clinic-based case-control study of African American youth. Therefore, the prevalence of asthma control in our study should not be interpreted as population prevalence nor are the results generalizable to non-urban, non-African American pediatric population.
CONCLUSIONS
The findings from our study provide additional support that low socioeconomic status is associated with poor asthma-related outcomes. We have also shown that this effect is observed along the entire socioeconomic gradient and adverse asthma outcomes are not limited to the very poor.
Supplementary Material
Footnotes
Author Contributors:
N.T. was responsible for analyzing the data with supervision and input from L.N.B., K.B-D., L.A.R., S.S.O., S.S. and E.G.B. N.T. wrote the first version and all subsequent revisions of the manuscript. M.M. wrote components of the first version of the manuscript. E.C. assisted with subsequent drafts included in the manuscript. H.J.F, L.N.B., E.B-B., A.D., M.A.L., S.T., and E.G.B. planned and supervised the collection of data from the various recruitment regions in the initial cohort. N.T. and E.G.B. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to interpretation of results, and provided revisions and approval of the final manuscript.
REFERENCES
- 1.Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, et al. Trends in asthma prevalence, health care use, mortality in the United States, 2001–2010. NCHS Data Brief. 2012;(94):1–8. Epub 2012/05/24. [PubMed] [Google Scholar]
- 2.Lieu TA, Lozano P, Finkelstein JA, Chi FW, Jensvold NG, Capra AM, et al. Racial/ethnic variation in asthma status and management practices among children in managed medicaid. Pediatrics. 2002;109(5):857–865. doi: 10.1542/peds.109.5.857. Epub 2002/05/03. [DOI] [PubMed] [Google Scholar]
- 3.Elmelech Y, Lu H-H. Race, ethnicity, and the gender poverty gap. Social Science Research. 2004;33(1):158–182. [Google Scholar]
- 4.Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annual review of sociology. 1995:349–386. [Google Scholar]
- 5.McDonough P, Duncan GJ, Williams D, House J. Income dynamics and adult mortality in the United States, 1972 through 1989. Am J Public Health. 1997;87(9):1476–1483. doi: 10.2105/ajph.87.9.1476. Epub 1997/10/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Devoe JE, Tillotson CJ, Wallace LS, Lesko SE, Angier H. The effects of health insurance and a usual source of care on a child's receipt of health care. J Pediatr Health Care. 2012;26(5):e25–e35. doi: 10.1016/j.pedhc.2011.01.003. Epub 2012/08/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baker DW, Parker RM, Williams MV, Clark WS, Nurss J. The relationship of patient reading ability to self-reported health and use of health services. American journal of public health. 1997;87(6):1027–1030. doi: 10.2105/ajph.87.6.1027. Epub 1997/06/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeWalt DA, Dilling MH, Rosenthal MS, Pignone MP. Low parental literacy is associated with worse asthma care measures in children. Ambul Pediatr. 2007;7(1):25–31. doi: 10.1016/j.ambp.2006.10.001. Epub 2007/01/31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Callahan ST, Cooper WO. Gender and uninsurance among young adults in the United States. Pediatrics. 2004;113(2):291–297. doi: 10.1542/peds.113.2.291. Epub 2004/02/03. [DOI] [PubMed] [Google Scholar]
- 10.Holt EW, Theall KP, Rabito FA. Individual, Housing, and Neighborhood Correlates of Asthma among Young Urban Children. J Urban Health. 2012 doi: 10.1007/s11524-012-9709-3. Epub 2012/06/13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel MR, Brown RW, Clark NM. Perceived Parent Financial Burden and Asthma Outcomes in Low-Income, Urban Children. J Urban Health. 2012 doi: 10.1007/s11524-012-9774-7. Epub 2012/11/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holt EW, Theall KP, Rabito FA. Individual, housing, and neighborhood correlates of asthma among young urban children. Journal of urban health : bulletin of the New York Academy of Medicine. 2013;90(1):116–129. doi: 10.1007/s11524-012-9709-3. Epub 2012/06/13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basagana X, Sunyer J, Kogevinas M, Zock JP, Duran-Tauleria E, Jarvis D, et al. Socioeconomic status and asthma prevalence in young adults: the European Community Respiratory Health Survey. Am J Epidemiol. 2004;160(2):178–188. doi: 10.1093/aje/kwh186. Epub 2004/07/06. [DOI] [PubMed] [Google Scholar]
- 14.Northridge J, Ramirez OF, Stingone JA, Claudio L. The role of housing type and housing quality in urban children with asthma. J Urban Health. 2010;87(2):211–224. doi: 10.1007/s11524-009-9404-1. Epub 2010/01/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thakur N, Oh SS, Nguyen EA, Martin M, Roth LA, Galanter J, et al. Socioeconomic Status and Childhood Asthma in Urban Minority Youths. The GALA II and SAGE II Studies. American journal of respiratory and critical care medicine. 2013;188(10):1202–1209. doi: 10.1164/rccm.201306-1016OC. Epub 2013/09/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neeta T, Sam SO, Lindsey R, Celeste E, Emerita B-B, Adam D, et al. C94 UNDERSTANDING AND OVERCOMING THE EFFECTS OF HEALTH DISPARITIES ON RESPIRATORY DISEASE MANAGEMENT. American Thoracic Society; 2013. The Impact Of Socioeconomic Status On Asthma Outcomes Among Black Youths; p. A4955-A. [Google Scholar]
- 17.Williams DR, Collins C. Us Socioeconomic and Racial-Differences in Health - Patterns and Explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]
- 18.Larson K, Halfon N. Family income gradients in the health and health care access of US children. Matern Child Health J. 2010;14(3):332–342. doi: 10.1007/s10995-009-0477-y. Epub 2009/06/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu WH, Yang L, Peng FH, Yao J, Zou LL, Liu D, et al. Lower socioeconomic status is associated with worse outcomes in pulmonary arterial hypertension. American journal of respiratory and critical care medicine. 2013;187(3):303–310. doi: 10.1164/rccm.201207-1290OC. Epub 2012/12/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Niu S, Zhao D, Zhu J, Liu J, Liu Q, Liu J, et al. The association between socioeconomic status of high-risk patients with coronary heart disease and the treatment rates of evidence-based medicine for coronary heart disease secondary prevention in China: Results from the Bridging the Gap on CHD Secondary Prevention in China (BRIG) Project. Am Heart J. 2009;157(4):709–715. e1. doi: 10.1016/j.ahj.2008.12.009. Epub 2009/04/01. [DOI] [PubMed] [Google Scholar]
- 21.Ezeamama AE, Viali S, Tuitele J, McGarvey ST. The influence of socioeconomic factors on cardiovascular disease risk factors in the context of economic development in the Samoan archipelago. Soc Sci Med. 2006;63(10):2533–2545. doi: 10.1016/j.socscimed.2006.06.023. Epub 2006/08/01. [DOI] [PubMed] [Google Scholar]
- 22.Health NIo. National Asthma Education and Prevention Program. Full Report of the Expert Panel: Guidelines for the diagnosis and management of asthma (EPR-3) 2007. 2011 [Google Scholar]
- 23.Ferris BG. Epidemiology Standardization Project (American Thoracic Society) The American review of respiratory disease. 1978;118(6 Pt 2):1–120. Epub 1978/12/01. [PubMed] [Google Scholar]
- 24.National Asthma Education and Prevention Program (National Heart Lung and Blood Institute) Guidelines for the diagnosis and management of asthma: Full report 2007. Bethesda, DC: US Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute; 2010. Third Expert Panel on the Management of Asthma. [Google Scholar]
- 25.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. American journal of respiratory and critical care medicine. 1999;159(1):179–187. doi: 10.1164/ajrccm.159.1.9712108. Epub 1999/01/05. [DOI] [PubMed] [Google Scholar]
- 26.Almqvist C, Worm M, Leynaert B. Impact of gender on asthma in childhood and adolescence: a GA2LEN review. Allergy. 2008;63(1):47–57. doi: 10.1111/j.1398-9995.2007.01524.x. Epub 2007/09/08. [DOI] [PubMed] [Google Scholar]
- 27.Oh SS, Tcheurekdjian H, Roth LA, Nguyen EA, Sen S, Galanter JM, et al. Effect of secondhand smoke on asthma control among black and Latino children. J Allergy Clin Immunol. 2012;129(6):1478–1483. e7. doi: 10.1016/j.jaci.2012.03.017. Epub 2012/05/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and socioeconomic status in children and adolescents: United States, 2005–2008. NCHS data brief. 2010;(51):1–8. Epub 2011/01/08. [PubMed] [Google Scholar]
- 29.Borrell LN, Nguyen EA, Roth LA, Oh SS, Tcheurekdjian H, Sen S, et al. Childhood obesity and asthma control in the GALA II and SAGE II studies. American journal of respiratory and critical care medicine. 2013;187(7):697–702. doi: 10.1164/rccm.201211-2116OC. Epub 2013/02/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nishimura KK, Galanter JM, Roth LA, Oh SS, Thakur N, Nguyen EA, et al. Early Life Air Pollution and Asthma Risk in Minority Children: The GALA II & SAGE II Studies. American journal of respiratory and critical care medicine. 2013 doi: 10.1164/rccm.201302-0264OC. Epub 2013/06/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dick S, Doust E, Cowie H, Ayres JG, Turner S. Associations between environmental exposures and asthma control and exacerbations in young children: a systematic review. BMJ open. 2014;4(2):e003827. doi: 10.1136/bmjopen-2013-003827. Epub 2014/02/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Afifi A, Clark VA, May S. Computer-Aided Multivariate Analysis. 4th ed. Boca Raton, FL: Chapman & Hall; 2004. [Google Scholar]
- 33.Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods. 2010;15(4):309–334. doi: 10.1037/a0020761. Epub 2010/10/20. [DOI] [PubMed] [Google Scholar]
- 34.R Core Team. R Foundation for Statistical Computing. Vienna, Austria: 2012. [accessed 2012 July 30]. R: A language and environment for statistical computing. ISBN 3-900051-07-0 Available from http://www.R-project.org/. [Google Scholar]
- 35.Moore JC, Stinson LL, Welniak EJ. Income measurement error in surveys: A review. JOURNAL OF OFFICIAL STATISTICS-STOCKHOLM- 2000;16(4):331–362. [Google Scholar]
- 36.Singh GK, Siahpush M, Kogan MD. Disparities in children's exposure to environmental tobacco smoke in the United States, 2007. Pediatrics. 2010;126(1):4–13. doi: 10.1542/peds.2009-2744. Epub 2010/07/01. [DOI] [PubMed] [Google Scholar]
- 37.Stevenson LA, Gergen PJ, Hoover DR, Rosenstreich D, Mannino DM, Matte TD. Sociodemographic correlates of indoor allergen sensitivity among United States children. J Allergy Clin Immunol. 2001;108(5):747–752. doi: 10.1067/mai.2001.119410. Epub 2001/11/03. [DOI] [PubMed] [Google Scholar]
- 38.Neidell MJ. Air pollution, health, and socio-economic status: the effect of outdoor air quality on childhood asthma. Journal of health economics. 2004;23(6):1209–1236. doi: 10.1016/j.jhealeco.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 39.Bornehag CG, Blomquist G, Gyntelberg F, Jarvholm B, Malmberg P, Nordvall L, et al. Dampness in buildings and health. Nordic interdisciplinary review of the scientific evidence on associations between exposure to "dampness" in buildings and health effects (NORDDAMP) Indoor air. 2001;11(2):72–86. doi: 10.1034/j.1600-0668.2001.110202.x. Epub 2001/06/08. [DOI] [PubMed] [Google Scholar]
- 40.Williams DR, Sternthal M, Wright RJ. Social determinants: taking the social context of asthma seriously. Pediatrics. 2009;123(Suppl 3):S174–S184. doi: 10.1542/peds.2008-2233H. Epub 2009/04/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sporik R, Holgate ST, Platts-Mills TA, Cogswell JJ. Exposure to house-dust mite allergen (Der p I) and the development of asthma in childhood: a prospective study. New England Journal of Medicine. 1990;323(8):502–507. doi: 10.1056/NEJM199008233230802. [DOI] [PubMed] [Google Scholar]
- 42.Cesaroni G, Farchi S, Davoli M, Forastiere F, Perucci CA. Individual and area-based indicators of socioeconomic status and childhood asthma. The European respiratory journal. 2003;22(4):619–624. doi: 10.1183/09031936.03.00091202. Epub 2003/10/30. [DOI] [PubMed] [Google Scholar]
- 43.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) 2002;21(2):60–76. doi: 10.1377/hlthaff.21.2.60. Epub 2002/03/20. [DOI] [PubMed] [Google Scholar]
- 44.Cook JT, Frank DA, Berkowitz C, Black MM, Casey PH, Cutts DB, et al. Welfare reform and the health of young children: a sentinel survey in 6 US cities. Archives of pediatrics & adolescent medicine. 2002;156(7):678–684. doi: 10.1001/archpedi.156.7.678. Epub 2002/07/02. [DOI] [PubMed] [Google Scholar]
- 45.Fisher EB, Strunk RC, Sussman LK, Sykes RK, Walker MS. Community organization to reduce the need for acute care for asthma among African American children in low-income neighborhoods: the Neighborhood Asthma Coalition. Pediatrics. 2004;114(1):116–123. doi: 10.1542/peds.114.1.116. Epub 2004/07/03. [DOI] [PubMed] [Google Scholar]
- 46.O'Sullivan MM, Brandfield J, Hoskote SS, Segal SN, Chug L, Modrykamien A, et al. Environmental improvements brought by the legal interventions in the homes of poorly controlled inner-city adult asthmatic patients: a proof-of-concept study. The Journal of asthma : official journal of the Association for the Care of Asthma. 2012;49(9):911–917. doi: 10.3109/02770903.2012.724131. Epub 2012/10/02. [DOI] [PubMed] [Google Scholar]
- 47.Thyne SM, Rising JP, Legion V, Love MB. The Yes We Can Urban Asthma Partnership: a medical/social model for childhood asthma management. The Journal of asthma : official journal of the Association for the Care of Asthma. 2006;43(9):667–673. doi: 10.1080/02770900600925288. Epub 2006/11/10. [DOI] [PubMed] [Google Scholar]
- 48.Katz LF, Kling JR, Liebman JB. Moving to opportunity in Boston: Early results of a randomized mobility experiment. The Quarterly Journal of Economics. 2001;116(2):607–654. [Google Scholar]
- 49.Akinbami LJ, Sullivan SD, Campbell JD, Grundmeier RW, Hartert TV, Lee TA, et al. Asthma outcomes: healthcare utilization and costs. J Allergy Clin Immunol. 2012;129(3 Suppl):S49–S64. doi: 10.1016/j.jaci.2011.12.984. Epub 2012/03/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bair-Merritt MH, Johnson SB, Okelo S, Page G. Intimate partner violence exposure, salivary cortisol, and childhood asthma. Child abuse & neglect. 2012;36(7–8):596–601. doi: 10.1016/j.chiabu.2011.12.002. Epub 2012/08/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. Epub 1998/01/15. [DOI] [PubMed] [Google Scholar]
- 52.Isaacs SL, Schroeder SA. Class - the ignored determinant of the nation's health. The New England journal of medicine. 2004;351(11):1137–1142. doi: 10.1056/NEJMsb040329. Epub 2004/09/10. [DOI] [PubMed] [Google Scholar]
- 53.Adler NE, Snibbe AC. The role of psychosocial processes in explaining the gradient between socioeconomic status and health. Current Directions in Psychological Science. 2003;12(4):119–123. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.