Abstract
Background
The World Health Organization has identified the primary referral hospital as its priority site for improving surgical care in low- and middle-income countries. Little is known about the relative burden surgical patients place on health care facilities at this level. This research estimates the fraction of admissions due to surgical conditions at three hospitals in rural Mozambique.
Methods
Prospective data were collected on all inpatients at three primary referral hospitals in Mozambique during a 12-day period. We compared the number of surgical patients and their length of stay (LOS) to the patients admitted to the medicine, pediatric, and maternity wards. These findings were validated using retrospective data collected from one hospital from January to May 2012.
Results
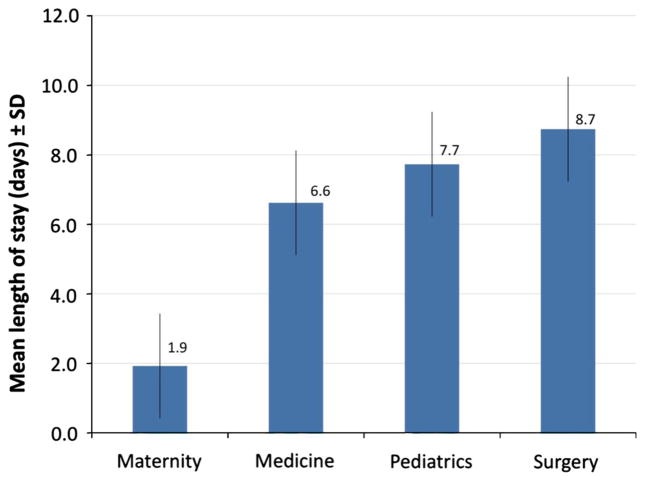
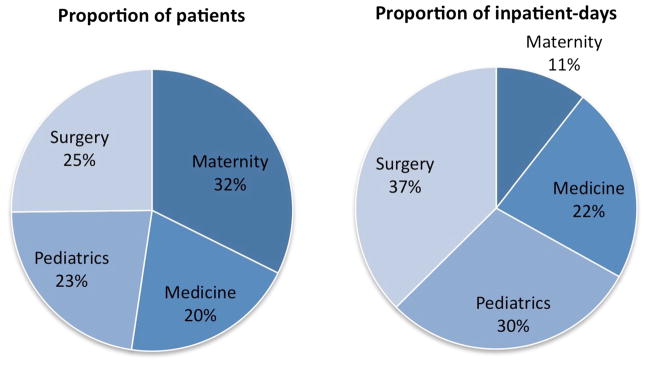
Patients with surgical conditions (i.e., patients admitted to the surgical or maternity ward) accounted for 57.5 % of admissions and 48.0 % of patient-days. The majority of patients were admitted to the maternity ward (32.3 %). The other admissions were evenly distributed to the pediatric (22.5 %), medical (20.0 %), and surgical (25.2 %) wards. Compared to patients from the three other wards, surgical patients had longer average LOS (8.7 vs. 1.9–7.7 days) and a higher number of total patient-days (891 vs. 252–703 days). The most prevalent procedures were cesarean section (33.3 %) and laceration repair/wound care (11.8 %).
Conclusions
Surgical conditions are the most common reason for admissions at three primary referral hospitals in rural Mozambique. These data suggest that surgical care is a major component of health care delivered at primary referral hospitals in Mozambique and likely other sub-Saharan African countries.
Introduction
Surgical conditions have been a largely neglected public health issue in low- and middle-income countries (LMICs). Globally, surgical disease has been estimated as among the top 15 causes of disability [1, 2]. It has been estimated that there is approximately one operation performed for every 25 people—double the annual world volume of childbirth [3]. An estimated 11 % of the global burden of disease can be treated by surgery, which includes injuries (38 %), malignancies (19 %), congenital anomalies (9 %), complications of pregnancy (6 %), cataracts (5 %), and perinatal conditions (4 %) [1, 4]. Surgical conditions have also been estimated to account for up to 15 % of total disability-adjusted life years (DALYs) lost worldwide, estimated at 38 DALYs lost per 1,000 people [1, 5]. Untreated surgical conditions contribute to an estimated 10 % of all deaths and 20 % of deaths in young adults [6].
This article examines the relative burden of surgical diseases at three primary referral hospitals in rural Mozambique. This information could be useful when planning surgical services for population living in rural areas of LMICs.
Methods
Data were collected from three primary referral hospitals (Chókwè, Nhamatanda, Ribaue) in the southern, central, and northeastern regions of Mozambique, respectively (Fig. 1; Table 1). Mozambique is a country of approximately 24 million people located in southeastern Africa. It ranks 184 of 187 countries in the world on the United Nations Development Programme (UNDP) Human Development Index [7]. The average life expectancy is 50 years, and nearly half (43.9 %) of its population is aged <15 years [8].
Fig. 1.
Map of Mozambique shows the location of the three primary referral hospitals
Table 1.
Study sites
| Parameter | Chókwè hospital | Nhamatanda hospital | Ribaue hospital |
|---|---|---|---|
| Catchment population | 259,000 | 281,000 | 228,000 |
| No. of beds | 125 | 128 | 57 |
| No. of doctors | 2 | 3 | 4 |
| No. of high-level nurses | 9 | 3 | 1 |
| No. of mid- and basic-level nurses | 64 | 110 | 89 |
| Distance to referral center (km) | 125 | 110 | 150 |
Less than half of Mozambique’s population lives within 5 km of a public health facility. There is an estimated one physician for every 23,000 people [9, 10]. Each hospital serves a catchment area of roughly 230,000–280,000 people and is located approximately 110–150 km from the nearest referral center. Chókwè and Nhamatanda Rural Hospitals have 125 and 128 beds, respectively. Ribaue Rural Hospital is somewhat smaller with 57 beds. Each hospital employs two to four doctors and has a total of 75–116 medical staff. Each hospital is equipped with an emergency room, an operating room, and an ambulance.
Prospective data were collected from all inpatients at Chókwè Rural Hospital from June 18–29, 2012, from Nhamatanda Rural Hospital from June 23–29, 2012, and from Ribaue Rural Hospital from July 5–12, 2012. Data included demographics, diagnosis, dates of admission and discharge, type of operation performed (if applicable), and human immunodeficiency virus (HIV) status (if available). To identify the proportion of surgical disease within these hospitals, the proportion of patients, patient-days, and average length of stay (LOS) of surgical patients were compared to those of the three other hospital wards: medicine, pediatrics, and maternity.
Selection bias from the limited period of prospective data collection was accounted for by reviewing retrospective data from all inpatients at Chókwè Rural Hospital from January 2012 to May 2012. These data included the number of patients in each ward, total patient-days (number of patients multiplied by their LOS), summary statistics of diagnoses and operations performed, and deaths. Although retrospective data offered a larger sample size and time period that was not possible during the prospective data collection, the prospective data allowed for a more detailed analysis.
Surgical conditions were defined as a disease state requiring the expertise of a surgically trained provider [11]. Thus, surgical patients were defined as those admitted to the surgical ward and any patient admitted to the maternity ward who underwent an operation. Not all patients admitted to the surgical ward had an operation. For example, some patients may have had nonoperative management of burns, wounds, lacerations, or fractures, but these patients were still cared for by the surgical team.
Statistical analysis was performed using STATA 64-bit Special Edition, version 11.2 (Stata Corp., College Station, TX, USA). The National Bioethics Committee of Mozambique and the Human Research Protection program at University of California, San Diego approved this study.
Results
The number of patients in each ward was not equally distributed among the hospitals (Table 2). At Chókwè, the surgical ward had the highest proportion of patients (30.6 %), whereas pediatrics had the highest proportion of patients at Nhamatanda (34.2 %) and maternity had the highest proportion at Ribaue (50.6 %). Total patient-days had similar distributions, except surgical patients had more patient-days in Ribaue than maternity patients (147 vs. 86 days). Women made up a majority of patients in all wards except pediatrics at Chókwè (22.2 %) and medicine at Nhamatanda (34.6 %). The surgical ward had the most patients per available beds, exceeding 100 % at Nhamatanda (128.6 %) and Ribaue (111.3 %). The average LOS was longest for surgical patients at all hospitals (6–10 days, p <0.001). Overall, the maternity wards had the highest number of patients, but the surgical wards had the most total patient-days (Fig. 2). Combined, surgical patients had a longer average LOS (p <0.001) (Fig. 3).
Table 2.
Summary statistics of all inpatients, prospective study period
| Parameter | Chókwè (n = 173)
|
Nhamatanda (n = 153)
|
Ribaue (n = 79)
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Maternity | Medicine | Pediatrics | Surgery | Maternity | Medicine | Pediatrics | Surgery | Maternity | Medicine | Pediatrics | Surgery | |
| No. of patients | 48 (27.8 %) | 45 (26.0 %) | 27 (15.6 %) | 53 (30.6 %) | 43 (27.7 %) | 26 (18.1 %) | 53 (34.2 %) | 31 (20.0 %) | 40 (50.6 %) | 10 (12.7 %) | 11 (13.9 %) | 18 (22.8 %) |
| Total patient-days | 107 | 245 | 211 | 422 | 59 | 228 | 450 | 322 | 86 | 63 | 42 | 147 |
| Female (%) | 100 % | 57.8 % | 22.2 % | 67.9 % | 100 % | 34.6 % | 54.7 % | 51.6 % | 100.0 % | 60.0 % | 54.5 % | 55.6 % |
| Age (years)a | 25 (16–39) | 35 (23–63) | 2 (0–7) | 29 (1–70) | 22 (16–32) | 35.5 (20–60) | 2 (0–7) | 21 (7–64) | 23 (15–38.5) | 32 (17–70) | 1 (0–12) | 23 (4–62) |
| LOSa | 1 (0–8) | 5 (1–10) | 4 (2–21) | 6 (1–28) | 1 (0–2) | 6.5 (1–22) | 5 (1–1) | 10 (1–26) | 2 (0–5) | 5 (3–16) | 5 (1–8) | 7 (2–26) |
| Average capacityb | 20.0 % | 64.4 % | 45.8 % | 72.6 % | 43.7 % | 51.3 % | 100.0 % | 128.6 % | 51.9 % | 29.4 % | 45.0 % | 111.3 % |
LOS length of hospital stay
Median (95 % CI). Bartlett’s test for equal variance p <0.001 between wards for each hospital, respectively
Median (95 % CI). Calculated by (total number of patient days)/(beds × days in study period)
Fig. 2.
Proportion of the total number of patients and total inpatient days by hospital ward. Data shown represent combined patients from all three hospitals
Fig. 3.
Average length of stay by hospital ward (number of days, mean ± SD). Data shown represent combined patients from all three hospitals
Table 3 summarizes the surgical patients during the prospective study period at all hospitals. Cesarean sections made up the highest proportion of surgeries (49.3 %), followed by inguinal herniorrhaphies (15.9 %). Among patients who underwent a procedure, the median age was highest in patients with inguinal herniorrhaphies (50 years) and lowest in patients with cesarean sections (19.5 years). Average LOS was longest both preoperatively and postoperatively for patients with amputations (5.0 and 11.7 days, respectively). Patients who underwent a cesarean section or other obstetric and gynecologic surgeries had the shortest average preoperative LOS (0.5 and 0.4 days, respectively). Among patients who did not have an operation, lacerations/wounds made up the largest proportion of all surgical conditions (36.4 %). The average LOS was highest among burn patients (14.6 days).
Table 3.
Summary of surgery patients, prospective study period
| Parameter | No. of patients | % Female | Age (years)a | Average LOS, preoperatively (days) | Average LOS, postoperatively (days) | Overall LOS, average (days) |
|---|---|---|---|---|---|---|
| Procedure performed | ||||||
| Cesarean section | 34 | 100 | 19.5 ± 2.0 | 0.5 | 8.1 | 8.5 |
| Other obstetric/gynecologic surgery | 5 | 100 | 30.0 ± 17.3 | 0.4 | 3.4 | 6.4 |
| Amputation | 3 | 0 | 24.0 ± 13.9 | 5.0 | 11.7 | 16.7 |
| Inguinal herniorrhaphy | 11 | 9.0 | 50.0 ± 5.7 | 1.1 | 7.5 | 8.5 |
| Epigastric herniorrhaphy | 3 | 100 | 26.0 ± 15.0 | 1.3 | 6.0 | 7.3 |
| Hydrocele | 5 | 0.0 | 26.0 ± 25.4 | 1.2 | 6.0 | 7.2 |
| Other | 8 | 37.5 | 28.5 ± 5.1 | 2.4 | 10.4 | 12.8 |
| Total | 69 | 66.7 | 24.0 ± 18.0 | 1.0 | 54.5 | 61.5 |
| No procedure performed | ||||||
| Fracture | 5 | 25.0 | 29.0 ± 16.6 | N/A | N/A | 7.4 |
| Burn | 5 | 40.0 | 7.0 ± 5.6 | 14.6 | ||
| Laceration/wound | 12 | 58.3 | 34.5 ± 14.6 | 5.8 | ||
| Other | 11 | 45.5 | 32.0 ± 17.0 | 11.0 | ||
| Total | 33 | 45.5 | 29.0 ± 16.7 | 9.1 | ||
Data shown represent combined patients from all three hospitals
Median ± SD
Table 4 summarizes diagnoses and mortality by inpatient ward at the Chókwè Rural Hospital retrospectively from January to May 2012. Cesarean section and nonoperative surgical patients comprised the largest proportion of patients in the surgical ward (39.7 and 31.1 %, respectively). Among pediatric cases, malaria and malnutrition contributed to a majority of disease (23.9 and 23.1 %, respectively), whereas most deaths were a result of malnutrition (13.3 %). Among medical cases, HIV/acquired immunodeficiency disease (AIDS) made up the largest proportion of all diseases and cerebrovascular accidents had the highest mortality rate (39.4 and 43.8 %, respectively).
Table 4.
Diagnoses and mortality by hospital ward at Chókwè Rural Hospital, January to May 2012
| Diagnosis | No. of patients | No. of deaths | Mortality rate (%) |
|---|---|---|---|
| Pediatrics | |||
| Diarrhea | 21 (5.8 %) | 2 | 9.5 |
| Tuberculosis | 13 (3.6 %) | 1 | 7.7 |
| Malaria | 86 (23.9 %) | 2 | 2.3 |
| Anemia | 36 (10.0 %) | 5 | 13.9 |
| Pneumonia | 67 (18.6 %) | 0 | 0.0 |
| HIV/AIDS | 6 (1.7 %) | 3 | 50.0 |
| Meningitis | 5 (1.4 %) | 1 | 0.0 |
| Malnutrition | 83 (23.1 %) | 11 | 13.3 |
| Other | 43 (11.9 %) | 1 | 2.3 |
| Total | 360 (100 %) | 26 | 7.2 |
| Medicine | |||
| Diarrhea | 7 (1.7 %) | 0 | 0.0 |
| Tuberculosis | 17 (4.1 %) | 2 | 11.8 |
| Malaria | 16 (3.9 %) | 0 | 0.0 |
| Anemia | 20 (4.9 %) | 5 | 25.0 |
| Pneumonia | 18 (4.4 %) | 5 | 27.8 |
| HIV/AIDS | 162 (39.4 %) | 43 | 26.5 |
| Meningitis | 11 (2.7 %) | 4 | 36.4 |
| CVA (stroke) | 16 (3.9 %) | 7 | 43.8 |
| Hypertension | 44 (10.7 %) | 14 | 31.8 |
| Psychosis | 21 (5.1 %) | 0 | 0.0 |
| Diabetes | 9 (2.2 %) | 1 | 11.1 |
| Cardiac | 4 (1.0 %) | 0 | 0.0 |
| Asthma | 0 | 0 | 0.0 |
| Other | 66 (16.1 %) | 11 | 0.0 |
| Total | 411 (100 %) | 92 | 22.4 |
| Surgery | |||
| Herniorrhaphy | |||
| Elective | 21 (5.5 %) | 0 | 0.0 |
| Urgent | 9 (2.3 %) | 0 | 0.0 |
| Laparotomy | 33 (8.6 %) | 1 | 3.0 |
| Cesarean section | 152 (39.7 %) | ||
| Hysterectomy | 2 (0.5 %) | 0 | 0.0 |
| Other surgery | 47 (12.2 %) | 0 | 0.0 |
| Nonoperative | 119 (31.1 %) | 6 | 5.0 |
| Total | 383 (100 %) | 7 | 1.8 |
| Maternity | |||
| Births (not including cesarean sections) | 1,045 | ||
| Maternal deaths | 2 | ||
| Live births | 1,100 | – | |
| Low birth weight | 50 | – | |
| Stillbirths | – | 47 | |
| Other | 136 | 0 | |
| Total | 1,333 | 2 | 0.2 |
HIV human immunodeficiency virus, AIDS acquired immunodeficiency disease syndrome, CVA cerebrovascular accident
Table 5 summarizes retrospective data from Chókwè Rural Hospital from January to May 2012. Most patients were admitted to the maternity ward (53.6 %), which also had the highest percentage of occupied beds (30.0 %). The medical ward had the highest mortality rate (22.4 %), and the maternity and surgical wards had the lowest mortality rates (0.2 and 1.8 %, respectively).
Table 5.
Total patients, days of occupied beds, and mortality by hospital ward at Chókwè Rural Hospital, January to May 2012
| Department | No. of patients | Inpatient days of occupied beds | No. of deaths | Mortality rate (%) |
|---|---|---|---|---|
| Pediatrics | 360 (14.5 %) | 1,866 (19.4 %) | 26 | 7.2 |
| Medicine | 411 (16.5 %) | 2,649 (27.5 %) | 92 | 22.4 |
| Surgery | 383 (15.4 %) | 2,224 (23.1 %) | 7 | 1.8 |
| Maternity | 1,333 (53.6 %) | 2,894 (30.0 %) | 2 | 0.2 |
| Total | 2,487 (100 %) | 9,633 (100 %) | 127 | 5.1 |
Discussion
Surgical conditions represent a significant proportion of admissions to three primary referral hospitals in rural Mozambique. Although maternity patients made up the largest proportion of patients overall (32.3 % compared to 25.2 % of surgical patients), surgical patients accounted for the largest proportion of total patient-days (37.4 %) and had the longest average LOS (8.7 days). Together, patients with surgical conditions (i.e., patients admitted to the surgical and maternity wards) accounted for 57.5 % of admissions and 48.0 % of patient-days. Examining retrospective data over a five-month period at one hospital, the number of surgical patients was about equal to the number of medical and pediatric patients, whereas maternity patients made up the majority of the patient population (53.6 %). Mortality was lowest among the surgical and maternity patients (1.8 and 0.2 %, respectively)—far below the mortality rates for the medical and pediatric patients (22.4 and 7.2 %, respectively).
This study suggests that the provision of surgical services plays a key role, rather than a peripheral one, in delivering health care at the district level. In settings where medical management is unavailable or fails, resources for adequate surgical management are of even greater importance. For example, in the absence of appropriate antibiotics, higher rates of serious infections may lead to more amputations. In settings of already limited medical resources, surgical care offers a vital last resort when medical management fails.
Other studies suggest that surgical care at the district level has not adequately met patients’ needs. At hospitals in Tanzania, Uganda, and Mozambique, a majority of nonobstetric surgery was emergent rather than elective, suggesting a lack of access to surgical care for common conditions such as hernias [12, 13]. In a survey of 132 facilities in eight countries, most facilities reported the capacity to perform minor procedures, such as incision and drainage of abscesses, wound suturing, and management of acute burns. The capacity to perform more complex procedures, however, such as appendectomies, hernia repairs, and laparotomies, ranged from 6 to 92 % [10]. Only 44 % of facilities were able to offer cesarean sections [14].
Increased attention to improve surgical capacity in LMICs is also necessary as these countries have a disproportionate lack of access to surgical care. Countries with per-capita health expenditures of less than $100 account for one-third (34.5 %) of the world’s population but only undertake 3.5 % of the world’s surgical procedures [3]. Outcomes in these settings are also worse. Surgical mortality is estimated to be 5–10 % in LMICs, compared to <1 % in high-income countries [3]. Furthermore, in many LMICs, surgical care is disproportionately available to patients who can afford services and live in urban areas [5].
It is estimated that surgical conditions will contribute to an even larger proportion of morbidity and mortality in the future, further increasing demand for adequate surgical care at the district hospital. Mathers and Loncar estimated that road-traffic accidents will move from being the tenth leading cause of death in 2002 to being the eighth leading cause of death globally in 2030 [2]. Changing public health priorities, such as promoting circumcisions in an effort to reduce HIV transmission, may further increase demand for minor procedures in LMICs [15].
Surgical care has been shown to be cost-effective when delivered at the district hospital level. In such settings, the cost per surgical DALY averted is estimated at US$19–102 compared to immunizations (US$10/DALY averted), malaria prevention and treatment (US$2–24/DALY averted), oral rehydration therapy (US$1062/DALY averted), and antiretroviral therapy for HIV in sub-Saharan Africa (US$350–1494/DALY averted) [1, 16, 17]. The cost-effectiveness of providing surgical care is yet another reason to increase its availability at the district level.
This study has several limitations. The analysis assumes that data collected over the relatively short time period from these three hospitals is representative of diseases treated throughout the year. Our analysis was performed during winter, when burns are more prevalent and other diseases such as malaria are less prevalent. Birthing patterns also vary throughout the year.
These data should not be interpreted as a measure of the burden of disease in the community, as they include only patients admitted to the hospital [11]. The study also underestimated the number of surgical procedures performed, as it only counted major procedures performed in the operating room. It did not include minor procedures performed with local anesthesia, such as circumcisions or abscess drainage, which can represent a large proportion of all procedures performed. In addition, these results may not be representative of other LMICs. For example, the HIV/AIDS rate in Mozambique was estimated to be 11.5 % in 2009, which may contribute to different disease distribution and health care services than are seen in other countries [18].
Conclusions
These data show that surgical patients accounted for the majority of admissions and inpatient days at three primary referral hospitals in rural Mozambique. Together, patients with surgical conditions (i.e., patients admitted to the surgical and maternity wards) accounted for 57.5 % of admissions and 48.0 % of patient-days. Future research is needed to quantify the ability of the health care system to meet the total surgical needs of the community and to identify interventions that could close this gap.
Acknowledgments
The research was supported by Grant No. R24TW 008910 from the Fogarty International Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Fogarty International Center or the National Institutes of Health. The NIH Common Fund supports the first award.
Footnotes
Conflict of interest None.
Contributor Information
Jamie E. Anderson, Email: jaa002@ucsd.edu, Department of Surgery, University of California, San Diego, 200 W. Arbor Drive, San Diego, CA 92103, USA
Anne Erickson, Stanford University School of Medicine, Palo Alto, CA, USA.
Carlos Funzamo, Univsersidade Eduardo Mondlane, Maputo, Mozambique.
Peter Bendix, Department of Surgery, Dartmouth-Hitchcock Memorial Hospital, Lebanon, NH, USA.
Americo Assane, Univsersidade Eduardo Mondlane, Maputo, Mozambique.
John Rose, Department of Surgery, University of California, San Diego, 200 W. Arbor Drive, San Diego, CA 92103, USA.
Fernando Vaz, Univsersidade Eduardo Mondlane, Maputo, Mozambique.
Emilia Virginia Noormahomed, Department of Surgery, University of California, San Diego, 200 W. Arbor Drive, San Diego, CA 92103, USA. Univsersidade Eduardo Mondlane, Maputo, Mozambique. Department of Medicine, University of California, San Diego, CA, USA.
Stephen W. Bickler, Department of Surgery, University of California, San Diego, 200 W. Arbor Drive, San Diego, CA 92103, USA
References
- 1.Debas HT, Gosselin R, McCord C, et al. Surgery. In: Jamison DT, Breman JG, Measham AR, et al., editors. Disease control priorities in developing countries. 2. The International Bank for Reconstruction and Development/The World Bank Group; Washington: 2006. [PubMed] [Google Scholar]
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008;372:139–144. doi: 10.1016/S0140-6736(08)60878-8. [DOI] [PubMed] [Google Scholar]
- 4.Ozgediz D, Jamison D, Cherian M, et al. The burden of surgical conditions and access to surgical care in low- and middle-income countries. Bull World Health Organ. 2008;86:646–647. doi: 10.2471/BLT.07.050435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farmer PE, Kim JY. Surgery and global health: a view from beyond the OR. World J Surg. 2008;32:533–536. doi: 10.1007/s00268-008-9525-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atiyeh BS, Gunn SW, Hayek SN. Provision of essential surgery in remote and rural areas of developed as well as low and middle income countries. Int J Surg. 2010;8:581–585. doi: 10.1016/j.ijsu.2010.07.291. [DOI] [PubMed] [Google Scholar]
- 7.UNDP. Human development report 2011: sustainability and equity—a better future for all. Palgrave Macmillan; New York: 2011. [Google Scholar]
- 8.The World Bank. World development indicators. The World Bank; Washington: 2011. [Google Scholar]
- 9.USAID. [Accessed 1 May 2013];Health sector (SO8) overview: briefing book. 2006 http://transition.usaid.gov/mz/doc/misc/health%20overview_nov2006.pdf.
- 10.Lindelow M. [Accessed 1 May 2013];Health care demand in rural Mozambique: evidence from the 1996/97 household survey. 2002 http://www.ifpri.org/publication/health-care-demand-rural-mozambique-0.
- 11.Bickler S, Ozgediz D, Gosselin R, et al. Key concepts for estimating the burden of surgical conditions and the unmet need for surgical care. World J Surg. 2010;34:374–380. doi: 10.1007/s00268-009-0261-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galukande M, von Schreeb J, Wladis A, et al. Essential surgery at the district hospital: a retrospective descriptive analysis in three African countries. PLoS Med. 2010;7:e1000243. doi: 10.1371/journal.pmed.1000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Notrica MR, Evans FM, Knowlton LM, et al. Rwandan surgical and anesthesia infrastructure: a survey of district hospitals. World J Surg. 2011;35:1770–1780. doi: 10.1007/s00268-011-1125-4. [DOI] [PubMed] [Google Scholar]
- 14.Kushner AL, Cherian MN, Noel L, et al. Addressing the millennium development goals from a surgical perspective: essential surgery and anesthesia in 8 low- and middle-income countries. Arch Surg. 2010;145:154–159. doi: 10.1001/archsurg.2009.263. [DOI] [PubMed] [Google Scholar]
- 15.Williams BG, Lloyd-Smith JO, Gouws E, et al. The potential impact of male circumcision on HIV in sub-Saharan Africa. PLoS Med. 2006;3:e262. doi: 10.1371/journal.pmed.0030262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Laxminarayan R, Chow J, Shahid-Salles SA. Intervention cost-effectiveness: overview of main messages. In: Jamison DT, Breman JG, Measham AR, editors. Disease control priorities in developing countries. 2. The International Bank for Reconstruction and Development/The World Bank Group; Washington: 2006. [PubMed] [Google Scholar]
- 17.Luboga S, Macfarlane SB, von Schreeb J, et al. Increasing access to surgical services in sub-saharan Africa: priorities for national and international agencies recommended by the Bellagio Essential Surgery Group. PLoS Med. 2009;6:e1000200. doi: 10.1371/journal.pmed.1000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.UNAIDS. [Accessed 1 May 2013];Global report: UNAIDS report on the global AIDS epidemic. 2012 http://www.unaids.org/globalreport/global_report.htm.