Abstract
Objectives
Teach HIV-negative men who have sex with men (MSM) symptoms of acute HIV infection (AHI) and direct them to nucleic acid amplification testing (NAAT) though Public Health—Seattle & King County (PHSKC).
Design
Cross-sectional surveys, retrospective database analysis and chart review.
Methods
Beginning in June 2009, the ru2hot? campaign described AHI symptoms and NAAT. Two preintervention and two postintervention surveys assessed campaign visibility, symptom knowledge, and healthcare-seeking behaviour. Regression analyses evaluated secular trends in case-finding.
Results
366 MSM completed surveys. In survey 4, 23% of 100 men reported seeing the campaign, and 25% knew ‘ru2hot?’ referred to AHI. From survey 1 to survey 4, the proportion of subjects who knew ≥2 symptoms or that AHI was a ‘flu-like’ illness was unchanged (61% vs 57%, p=0.6). However, in survey 4, 13 (72%) of 18 subjects who saw the campaign named fever as a symptom of AHI compared with 19 (35%) of 55 subjects who had not seen the campaign (p=0.005). From 9/2003 to 12/2010, 622 (2.2%) of 27 661 MSM tested HIV-positive, and 111 (18%) were identified by the Public Health—Seattle & King County NAAT programme. In terms of the impact of the campaign on case-finding, diagnosis of EIA-negative/NAAT-positive and OraQuick-negative/EIA-positive cases increased from six in 2004 to 20 in 2010 (p=0.01), but postcampaign numbers were unchanged. 23 (51%) of 45 cases identified before and 8 (44%) of 18 cases identified after the campaign reported symptoms at initial testing (p=0.6).
Conclusions
Although a quarter of MSM surveyed saw the campaign and knowledge of fever (the symptom of emphasis) was high, case-finding was unchanged. Increasing campaign visibility could have had greater impact.
INTRODUCTION
Acute HIV infection (AHI) refers to the events from acquisition of HIV up to seroconversion. Approximately 50–90% of people develop nonspecific symptoms 2–4 weeks after HIV acquisition.1 However, AHI is infrequently diagnosed because symptoms may not be recognised by patients or providers.1 Even when individuals do seek care, AHI may not be diagnosed if only antibody testing is ordered.2
In 2003, Public Health—Seattle & King County (PHSKC) began a pooled HIV nucleic acid amplification testing (NAAT) programme for men who have sex with men (MSM).3–5 Individuals with AHI are highly infectious,6 and recognition of AHI may reduce transmission by decreasing risky behaviours7,8 and through partner services9 and anti-retroviral treatment.10 However, despite successful implementation of the programme, fewer than 10% of the estimated 300–325 persons infected with HIV each year in King County, Washington, USA are diagnosed during AHI.
We previously reported results of a survey designed to assess knowledge of symptoms consistent with the acute retroviral syndrome.11 Between April 2004 and March 2005, 91 (61%) of 150 HIV-negative MSM identified two or more symptoms of AHI or knew the acute retroviral syndrome was a ‘flu-like illness.’ There was no association between knowledge of symptoms and intent to seek care for symptoms.
In 2009, we developed a public health education campaign (figure 1) designed to teach HIV-negative MSM the symptoms of AHI and increase the proportion of HIV-infected individuals who are diagnosed by PHSKC during AHI. This manuscript describes evaluation of the campaign.
Figure 1.

Billboard image used in ru2hot?, an acute HIV infection public health education campaign targeting men who have sex with men in Seattle, Washington, USA. This figure is only reproduced in colour in the online version.
METHODS
The campaign
The ru2hot? campaign was developed in conjunction with the PHSKC HIV/sexually transmitted disease (STD) Programme and several Seattle community-based organisations. Focus groups and individual interviews of HIV-negative MSM informed the campaign name, messages and imagery. The campaign focused on fever recognition because fever is reported in over 90% of persons with symptoms associated with AHI.1 Primary campaign messages were ‘know the symptoms’ and ‘get an RNA test.’ Secondary messages listed other symptoms, described NAAT and the ‘window period’ and provided testing locations and rationale for testing and early treatment.
The campaign was designed primarily to reach MSM already motivated to seek HIV testing. Beginning in June 2009, wallet cards were distributed after HIV testing at the PHSKC STD Clinic and Seattle bathhouses, in gay bars and in safe sex packets at Gay Pride. Print media advertisements coincided with the 2009 Pride weekend. We used Google Analytics to track traffic to the website (ru2hot.org). In October 2010, after results from the first preplanned assessment showed limited impact, we augmented the campaign through two 14′×28′ billboards in Capitol Hill, the Seattle neighbourhood with greatest concentration of gay bars and businesses (figure 1). At the same time, we placed banner ads and an outreach profile on Manhunt.net. The total campaign cost, including staff time, was $19 038 over 3 years.
Campaign evaluation
Knowledge of AHI and intent to seek care
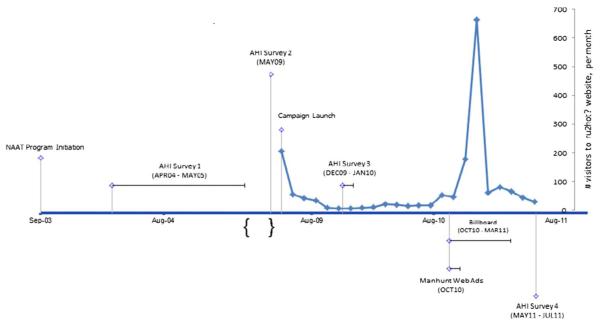
To assess symptom knowledge, convenience samples of MSM were surveyed at four time points: (1) April 2004–May 2005; (2) May 2009, prior to the campaign release; (3) December 2009–January 2010, 6 months after the initial release; and (4) May 2011–July 2011, approximately 6 months following the augmented campaign (figure 2). We approached men in the PHSKC STD Clinic waiting room during hours when there was a clinic room and research staff available for this activity. Subjects were eligible to participate if they were male or transgendered, reported sex with a man in the past year, had never been told they were HIV-infected, and were able to read and write in English.
Figure 2.
ru2hot? Timeline with Google Analytics. AHI: acute HIV infection; MSM: men who have sex with men; NAAT: nucleic acid amplification testing; PHSKC: Public Health—Seattle & King County. In 2003 the PHSKC pooled NAAT programme began testing serum samples from MSM to identify persons with AHI. AHI Survey 1 was conducted to assess knowledge of AHI symptoms among MSM prior to development of the campaign, which was initially launched in June 2009 and augmented in October 2010 with billboards and banner ads on Manhunt.net. From June 2009 to June 2011, 1164 unique individuals made 1753 visits to ru2hot.org, with the peak number of visitors occurring in December 2010, 2 months after the augmentation of the campaign. Access the article online to view this figure in colour.
The anonymous, written, self-administered surveys included a combination of true-false, multiple choice and open-ended questions. Questions about campaign visibility and recognition asked ‘Have you heard or seen or received information about HIV that included the phrase “ru2hot?”’, ‘When people get HIV infected, they go through different stages from the time of infection, through asymptomatic HIV, to AIDS. What part of HIV infection did the “ru2hot?” campaign talk about?’, and ‘What do you think the phrase “ru2hot?” means?’ Questions focused on knowledge of primary HIV infection and healthcare-seeking behaviour for symptoms compatible with AHI or other STDs. Because the surveys were administered anonymously, results were not linked to subjects’ HIV test results.
The University of Washington Institutional Review Board determined that this research activity was exempt from federal regulations governing human subjects research. All subjects gave verbal consent for study procedures and received a study-specific information statement and $5 for participation.
The primary outcome of this component of the evaluation was a change in proportion of subjects who, in an open-ended question, were able to list either two or more symptoms associated with AHI or who wrote that AHI is associated with a ‘flu-like’ illness. We evaluated the relationship between knowledge of and intent to seek attention for symptoms consistent with AHI by χ2 tests, Fisher’s exact tests and other analyses, as appropriate.
Case identification and healthcare-seeking behaviour
Since September 2003, the PHSKC pooled HIV NAAT programme has been targeted to all antibody-negative MSM tested through the PHSKC STD Clinic.3–5 This programme expanded over time to include bathhouses, Gay City Health Project (a community-based organisation), and private providers. The primary objective of the campaign was to increase the number of HIV-infected individuals diagnosed during AHI through PHSKC and in King County. This assessment included: number of MSM identified through the NAAT programme, referrals to the University of Washington Primary Infection Clinic (UW PIC), and number of MSM reporting concern for primary HIV infection during evaluation at the PHSKC STD Clinic or Gay City Health Project.
Specimens underwent antibody testing and NAAT as previously described4 with the following changes: after January 2010, antibody screening used the Genetic Systems HIV-1/2 Plus O enzyme immunoassay (EIA) (Bio-Rad, Redmond, Washington, USA), and NAAT was performed using the Abbott RealTime HIV-1 assay (Abbott Molecular, Des Plaines, Illinois, USA) on 27-specimen master pools created with a 3×3×3 matrix.12 For men screened by rapid testing, we continue to use an EIA to test specimens prior to pooling in order to reduce time and costs.4 The NAAT programme began as a quality control activity. Medical record review was approved by the University of Washington Institutional Review Board.
The UW PIC is a research clinic that has enrolled over 325 persons with acute and early infection into a variety of studies since 1992. Subjects are referred from local primary care providers and emergency departments when AHI is suspected. All subjects give written consent. Temporal trends in PHSKC case finding and PIC referrals were evaluated by multivariable regression analysis using case-finding as dependent and calendar year as an independent variable. The precampaign and postcampaign comparison included this as a dichotomised variable in the model.
Beginning in 2006 and 2008 respectively, patients seeking evaluation at the PHSKC STD Clinic and Gay City Health Project were asked whether they had concern about primary HIV infection. Frequency of this report and test results in these persons are presented as descriptive analyses.
RESULTS
From June 2009 to June 2011, 1164 unique individuals made 1753 visits to ru2hot.org (figure 2). First-time visitors spent a mean 2.5 min on the site viewing a mean 7.7 web pages. A mean 5.8 pages were viewed in 589 repeat visits. Nearly half (48%) of first-time visitors accessed the website directly, meaning that they typed the website address into the URL bar. Another 29% of first-time visitors were referred from Manhunt. net, 16% visited via search engines (eg, http://www.google.com) and 7% were referred from other websites (ie, http://www.facebook.com, http://www.seafukits.org, http://www.washington.edu, etc). Of the 1164 individuals, 1083 were from the USA, 844 (78%) of whom were from Washington State. The remaining 81 visitors came from 30 other countries.
Surveys of knowledge of AHI and intent to seek care
A total of 366 subjects participated in four cross-sectional surveys, including 150 subjects in the initial survey (survey 1),11 50 subjects immediately prior to the campaign release (survey 2), 87 subjects surveyed 6 months after the campaign began (survey 3) and 79 subjects surveyed 6 months after the augmented campaign (survey 4) (table 1). Nine (10%) of 87 subjects surveyed in survey 3 and 18 (23%) of 79 subjects surveyed in survey 4 reported seeing the campaign phrase ‘ru2hot?’ (p=0.005 for test of trend). There was a similar increase in the proportion of respondents who knew that the ru2hot? campaign was associated with AHI (p=0.0003). In survey 4, subjects who had seen the campaign were more likely to know that the ru2hot? campaign was associated with AHI compared with those who had not seen the campaign (10 (56%) of 18 and 9 (16%) of 55, p=0.001). In survey 4, 25 subjects wrote that the meaning of the phrase ‘ru2hot?’ had something to do with fever (n=14), HIV RNA levels and infectiousness (n=4), or AHI specifically (n=11); however, many subjects who had not seen the campaign interpreted the tagline to be about appearance (eg, ‘Are you too attractive to have HIV?’).
Table 1.
Survey responses
| Prior to campaign |
Initial campaign December 2009–January 2010 Survey 3 (n=87) |
Augmented campaign May 2011–July 2011 Survey 4 (n=79) |
|||
|---|---|---|---|---|---|
| April 2004–May 2005 Survey 1 (n=150) |
May 2009 Survey 2 (n=50) |
p value | |||
| Saw campaign phrase (ru2hot?) | n/a | 3 (6%) | 9 (10%) | 18 (23%) | 0.005 |
| Knew ru2hot? associated with AHI | n/a | 2 (4%) | 8 (9%) | 20 (25%) | 0.0003 |
| Median (IQR) symptoms named | 1 (0–3) | 2 (0–4) | 1 (0–3) | 1 (0–3) | NS |
| Named fever as AHI symptom | 47 (31%) | 21 (42%) | 33 (38%) | 35 (44%) | NS |
| Named ≥2 symptoms or ‘flu-like illness’ | 91 (61%) | 29 (58%) | 53 (61%) | 45 (57%) | NS |
| Ever had RNA test due to symptoms | n/a | 20 (40%) | 25 (29%) | 12 (15%) | 0.0015 |
AHI, acute HIV infection; n/a: not asked; NS: not significant.
When asked to name symptoms associated with primary HIV infection, fever was the most commonly named symptom, increasing from 47 (31%) subjects in survey 1 to 21 (42%) subjects in survey 2 prior to the campaign’s release. Following the campaign release, 33 (38%) subjects in survey 3 and 35 (44%) subjects in survey 4 named fever as a symptom of AHI. In survey 4, 13 (72%) of 18 subjects who saw the campaign named fever as a symptom of AHI compared with 19 (35%) of 55 subjects who had not seen the campaign (p=0.005). Other symptoms reported in survey 4 included fatigue (23%), sore throat (15%) and rash (14%). ‘Flu-like symptoms’ was written by 18% of subjects. From survey 1 to survey 4, the proportion of subjects who could name either two or more symptoms associated with AHI or wrote that AHI is associated with a ‘flu-like’ illness did not change (61% vs 57%, p=0.6), and there was not a significant difference in this measure among subjects in survey 4 who had seen the campaign versus those who had not (67% vs 53%, p=0.3).
Subjects were asked whether they would be likely to seek attention for a variety of symptoms lasting for 5 days that occurred after unprotected intercourse with an anonymous partner. In survey 4, the symptoms having the highest percentage of subjects reporting that they would be very or somewhat likely to seek attention were painless and painful genital ulcers (both at 93%), followed by oral ulcer (79%), night sweats (77%), rash in their partner (74%), lymphadenopathy (64%), rash (57%), flu-like illness (53%), fever and sore throat (51%), and cough and rhinorrhoea (24%). In survey 4, there were no associations between the identification of fever or sore throat as a symptom of AHI and the likelihood of seeking attention for fever and sore throat (p=1.0) naming AHI as a flu-like illness and the likelihood of seeking attention if a participant thought that he had influenza (p=0.4) or identifying rash as a symptom of AHI and the likelihood of seeking attention for a non-pruritic rash on the chest and back (p=0.2).
Case identification and healthcare-seeking behaviour
Between September 2003 and December 2010, PHSKC tested 27 661 specimens from MSM and 622 (2.2%) MSM were HIV-infected. The number of specimens tested increased from 2468 in 2004 to 4463 in 2010 (p=0.008 for linear trend), but there was not an additional change following the campaign (p=0.4) (figure 3). Of the 16 049 MSM screened initially by the OraQuick ADVANCE Rapid HIV-1/2 Antibody Test (performed on either oral fluids or fingerstick whole blood specimens), 314 (2.0%) had antibodies detected by this method. However, we identified 40 (0.2%) additional MSM who had antibodies detected by the standard EIA and 52 (0.3%) MSM who were EIA-negative/NAAT-positive. OraQuick therefore identified only 77% of the 406 HIV-infected persons screened initially by rapid testing. EIA identified 551 (89%) of the 622 HIV-infected persons, and HIV NAAT had an additional case-finding yield of 12.9% in our population. Numbers of EIA-negative/NAAT-positive and OraQuick-negative/EIA-positive cases diagnosed per year increased from six in 2004 to 20 in 2010 (p=0.06 for linear trend), but there was no change following the initiation of the campaign (p=0.6). From 2004 to 2010, there were 104 persons enrolled at the UW PIC, but referrals did not change over time (p=0.7) (figure 3).
Figure 3.
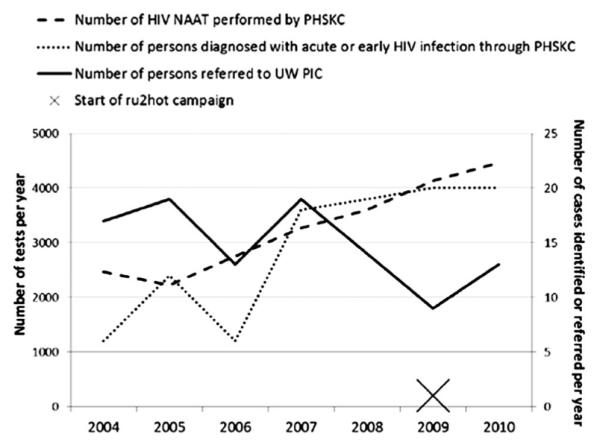
PHSKC NAAT programme case identification and UW PIC referral, 2004–2010. NAAT: nucleic acid amplification testing; PHSKC: Public Health—Seattle & King County; UW PIC: University of Washington Primary Infection Clinic. Between 2004 and 2010, there was an increase in the number of specimens tested by the PHSKC HIV NAAT programme (p=0.008) and cases of persons with acute and early HIV infection (p=0.06) over time, but there was no change following the campaign initiation in 2009. During this timeframe, there were 104 persons enrolled at the UW PIC, but referrals did not change following the campaign (note: enrolment was temporarily discontinued in 2009 due to funding issues).
Of 63 antibody-negative/NAAT-positive MSM diagnosed through the NAAT programme who had medical records available for review at PHSKC-funded sites, 31 (49%) reported symptoms or concern for AHI at the time of the initial visit. These 31 persons included 23 (51%) of the 45 cases identified before and eight (44%) of the 18 cases identified after the campaign started (p=0.6). In follow-up visits, an additional 10 (16%) men retrospectively reported that they had experienced symptoms consistent with AHI.
Since 2006, 732 MSM reported concern for primary HIV infection at the time of testing at the PHSKC STD Clinic or Gay City Health Project. Twelve (1.6%) of these persons had AHI, and 52 (7%) had detectable antibodies. The numbers reporting concern and the numbers and proportions testing HIV-positive decreased non-significantly over time (data not shown).
DISCUSSION
In this manuscript we describe results of a public health education campaign designed to teach HIV-negative MSM in King County, Washington the signs and symptoms associated with AHI and increase the proportion of HIV-infected MSM diagnosed during AHI. Although our campaign was successful in reaching some of the target population and most men surveyed knew the symptoms associated with AHI, our campaign had no impact on case-finding.
There are few examples of similar campaigns. Most recently published was ‘First Call NYU’, a small-scale education campaign in New York City designed to educate MSM and other at-risk communities about symptoms of AHI and encourage testing for research recruitment.13 Over 4 years and $84 187 (excluding costs of NAAT), this campaign tested 497 persons with rapid tests and individual NAAT and identified 14 (2.8%) persons with acute and early HIV infection. Other education campaigns such as ‘Are You Sure It’s the Flu?’ in San Diego, California, USA and ‘It’s Hottest at the Start’ in Vancouver, British Columbia, Canada, have been launched, but none to our knowledge were evaluated from a public health perspective.14
Greater emphasis must be placed on evaluation of HIV testing campaigns in order to compare effectiveness to other programming. A review by Noar15 outlined the ideal components of campaigns: (1) audience segmentation and formative research (eg, focus groups), (2) goals that include behaviour change in addition to education, (3) use of behavioural theory, (4) use of multiple media outlets to maximise exposure, (5) study designs that enable strong evaluations, and (6) behavioural outcomes.15 In our estimation, campaigns should ideally include biological outcomes such as case-finding and population-level markers such as incidence. Unfortunately, a Cochrane review of social marketing interventions to increase HIV testing among MSM identified only three campaigns that were adequately studied, all of which had weak study designs.16
Our campaign may have been partially successful in that there was increasing recognition of the campaign, and qualitative interviews conducted with survey 4 (data not shown) suggest that we successfully created ‘brand recognition’.17 The campaign slogans ‘ru2hot?’ and ‘maybe it’s not just a fever?’ aimed to link fever as a symptom of HIV acquisition. Although we did not observe an increase in our predetermined metric of knowledge, subjects in survey 4 who had seen the campaign were more likely to name fever as a symptom of AHI.
Despite this limited success, the campaign had no apparent impact on the number of HIV-infected MSM diagnosed during AHI, and this knowledge about AHI of MSM seeking care at the STD Clinic might not represent knowledge of all MSM. It is theoretically possible that we failed to see an increase in case-finding because men were diagnosed with AHI by community providers who did not refer to the PIC; we are currently using PHSKC surveillance data to determine the number of cases identified during AHI. It is more likely that the campaign was ineffective in translating knowledge to changes in healthcare-seeking behaviour. Given the small size of the campaign, additional funding could have had significant impact. For comparisons, ‘Check-It-Out’, a campaign promoting HIV testing among Australian MSM, cost $A130 230 and had no clear impact.18 ‘It’s Never Just HIV,’ a New York City campaign describing long-term complications of HIV infection, was reported to cost $726 000.19 ‘Plenty of Syph,’ a syphilis awareness campaign in Alberta, Canada, that parodied the online dating site Plenty of Fish, was reported to cost $2 million.20
Strategies are still needed to identify persons as soon as possible after HIV acquisition, particularly highly infectious persons with AHI6 who contribute to a significant proportion of ongoing transmission.21,22 This could be achieved through greater symptom recognition, as was attempted with this campaign, or by increasing the frequency of highly-sensitive HIV testing. Some persons already seek attention in healthcare settings with symptoms of AHI but are infrequently diagnosed1,23,24 because symptoms are non-specific and persons may not be asked or identify risk for HIV acquisition. Modelling suggests that individual NAAT may be cost-effective for MSM who present with fever or influenza-like illnesses in outpatient clinical settings.25,26 Routine HIV screening of persons in healthcare settings27 and greater frequency of testing among high-risk populations could also increase AHI case-finding if testing algorithms include pooled NAAT or fourth-generation antigen-antibody combination assays. In Seattle, laboratory-based antibody testing fails to identify about one-tenth of HIV-infected MSM, and rapid antibody testing fails in nearly a quarter of cases. Antigen-antibody assays may be a reasonable alternative to NAAT, as studies of high risk populations suggest that only 6–20% of AHI cases would be missed if combination assays were used instead of EIA plus NAAT.4,28,29
In summary, although the ru2hot? campaign was not successful in achieving its primary goals, a multifaceted approach to testing could identify greater numbers of persons with AHI. The components of such an approach would include: HIV testing using the most sensitive tests, frequent testing among populations at risk, education to those populations to direct them to seek testing for symptoms consistent with AHI and providing education to increase testing. Ultimately, there must be more rigorous evaluation of interventions that promote HIV testing in order to prove their relative effectiveness compared with other prevention programming.
Supplementary Material
Supplementary appendix 1: Self-administered Survey 1, March 2005.
Supplementary appendix 2: Self-administered Survey 2, March 2009.
Supplementary appendix 3: Self-administered Survey 3, December 2009.
Supplementary appendix 4: Self-administered Survey 4, April 2011.
Key messages.
▶ Diagnosis of persons with acute HIV infection (AHI) is an important but challenging problem.
▶ Although this modest education campaign had some success, it did not increase case-finding of persons with AHI.
▶ Public health programmes should use highly sensitive HIV tests, promote frequent testing, and educate at-risk populations and healthcare providers in order to diagnose acute infection.
Acknowledgements
We thank the clients and providers at the Gay City Health Project Wellness Center, PHSKC STD Clinic, and other PHSKC testing sites, as well as PHSKC for database management and data support.
Funding This project was funded by NIH K23 AI-65243 ( JS).
Footnotes
Contributors JS, ML and MG designed the campaign and study design. JS, HB, and DK collected, analysed and interpreted study data. All authors gave final approval of the manuscript to be published.
Competing interests None.
Patient consent Obtained.
Ethics approval University of Washington Human Subjects Division.
Provenance and peer review Not commissioned; externally peer reviewed.
An additional supplementary materials are published online only. To view this file please visit the journal online (http://dx.doi.org/10.1136/sextrans-2012-050730).
REFERENCES
- 1.Schacker T, Collier AC, Hughes J, et al. Clinical and epidemiologic features of primary HIV infection. Ann Intern Med. 1996;125:257–64. doi: 10.7326/0003-4819-125-4-199608150-00001. [DOI] [PubMed] [Google Scholar]
- 2.Fiebig EW, Wright DJ, Rawal BD, et al. Dynamics of HIV viremia and antibody seroconversion in plasma donors: implications for diagnosis and staging of primary HIV infection. AIDS. 2003;17:1871–9. doi: 10.1097/00002030-200309050-00005. [DOI] [PubMed] [Google Scholar]
- 3.Stekler J, Swenson PD, Wood RW, et al. Targeted screening for primary HIV infection through pooled HIV-RNA testing in men who have sex with men. AIDS. 2005;19:1323–5. doi: 10.1097/01.aids.0000180105.73264.81. [DOI] [PubMed] [Google Scholar]
- 4.Stekler JD, Swenson PD, Coombs RW, et al. HIV testing in a high-incidence population: is antibody testing alone good enough? Clin Infect Dis. 2009;49:444–53. doi: 10.1086/600043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stekler J, Maenza J, Stevens CE, et al. Screening for acute HIV infection: lessons learned. Clin Infect Dis. 2007;44:459–61. doi: 10.1086/510747. [DOI] [PubMed] [Google Scholar]
- 6.Wawer MJ, Gray RH, Sewankambo NK, et al. Rates of HIV-1 transmission per coital act, by stage of HIV-1 infection, in Rakai, Uganda. J Infect Dis. 2005;191:1403–9. doi: 10.1086/429411. [DOI] [PubMed] [Google Scholar]
- 7.Colfax GN, Buchbinder SP, Cornelisse PG, et al. Sexual risk behaviors and implications for secondary HIV transmission during and after HIV seroconversion. AIDS. 2002;16:1529–35. doi: 10.1097/00002030-200207260-00010. [DOI] [PubMed] [Google Scholar]
- 8.Marks G, Crepaz N, Senterfitt JW, et al. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States— implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39:446–53. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- 9.Moore ZS, McCoy S, Kuruc J, et al. Number of named partners and number of partners newly diagnosed with HIV infection identified by persons with acute versus established HIV infection. J Acquir Immune Defic Syndr. 2009;52:509–13. doi: 10.1097/QAI.0b013e3181ac12bf. [DOI] [PubMed] [Google Scholar]
- 10.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stekler J, Collier AC, Holmes KK, et al. Primary HIV infection education: knowledge and attitudes of HIV-negative men who have sex with men attending a public health sexually transmitted disease clinic. J Acquir Immune Defic Syndr. 2006;42:123–6. doi: 10.1097/01.qai.0000218357.82970.67. [DOI] [PubMed] [Google Scholar]
- 12.Goldsmith J, Faruki H, Smith R, et al. High throughput donor plasma NAT screening assay applied to acute HIV detection in a public health setting. 2007 HIV Diagnostic Conference.2007. [Google Scholar]
- 13.Silvera R, Stein D, Hutt R, et al. The Development and Implementation of an Outreach Program to Identify Acute and Recent HIV Infections in New York City. Open AIDS J. 2010;4:76–83. doi: 10.2174/1874613601004010076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kerndt PR, Dubrow R, Aynalem G, et al. Strategies used in the detection of acute/early HIV infections. The NIMH Multisite Acute HIV Infection Study: I. AIDS Behav. 2009;13:1037–45. doi: 10.1007/s10461-009-9580-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Noar SM, Palmgreen P, Chabot M, et al. A 10-year systematic review of HIV/AIDS mass communication campaigns: Have we made progress? J Health Commun. 2009;14:15–42. doi: 10.1080/10810730802592239. [DOI] [PubMed] [Google Scholar]
- 16.Wei C, Herrick A, Raymond HF, et al. Social marketing interventions to increase HIV/STI testing uptake among men who have sex with men and male-to-female transgender women. Cochrane Database Syst Rev. 2011;(9):CD009337. doi: 10.1002/14651858.CD009337. [DOI] [PubMed] [Google Scholar]
- 17.Wood M. Applying commercial marketing theory to social marketing: a tale of 4Ps (and a B) Soc Mar Q. 2008;14:76–85. [Google Scholar]
- 18.Guy R, Goller J, Leslie D, et al. No increase in HIV or sexually transmissible infection testing following a social marketing campaign among men who have sex with men. J Epidemiol Community Health. 2009;63:391–6. doi: 10.1136/jech.2008.077099. [DOI] [PubMed] [Google Scholar]
- 19. [accessed 26 Nov 2012]; http://www.nyc.gov/html/doh/downloads/pdf/condoms/ap-article2007.pdf.
- 20. [accessed 26 Nov 2012]; http://alberta.ca/acn/201105/305132284A9C5-C79C-E04F-894F907FF9E586BF.h.
- 21.Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20:1447–50. doi: 10.1097/01.aids.0000233579.79714.8d. [DOI] [PubMed] [Google Scholar]
- 22.Hollingsworth TD, Anderson RM, Fraser C. HIV-1 transmission, by stage of infection. J Infect Dis. 2008;198:687–93. doi: 10.1086/590501. [DOI] [PubMed] [Google Scholar]
- 23.Rosenberg ES, Caliendo AM, Walker BD. Acute HIV infection among patients tested for mononucleosis. N Engl J Med. 1999;340:969. doi: 10.1056/nejm199903253401217. [DOI] [PubMed] [Google Scholar]
- 24.Coco A, Kleinhans E. Prevalence of primary HIV infection in symptomatic ambulatory patients. Ann Fam Med. 2005;3:400–4. doi: 10.1370/afm.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coco A. The cost-effectiveness of expanded testing for primary HIV infection. Ann Fam Med. 2005;3:391–9. doi: 10.1370/afm.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Juusola JL, Brandeau ML, Long EF, et al. The cost-effectiveness of symptom-based testing and routine screening for acute HIV infection in men who have sex with men in the USA. AIDS. 2011;25:1779–87. doi: 10.1097/QAD.0b013e328349f067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Branson BM, Handsfield HH, Lampe MA, et al. Practice guideline. Centers for Disease Control and Prevention; Sep 22, 2006. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. Report No.: 1545-8601 (Electronic) 1057-5987 (Linking) Contract No.: RR-14. [PubMed] [Google Scholar]
- 28.Pandori MW, Hackett J, Jr, Louie B, et al. Assessment of the ability of a fourth-generation immunoassay for human immunodeficiency virus (HIV) antibody and p24 antigen to detect both acute and recent HIV infections in a high-risk setting. J Clin Microbiol. 2009;47:2639–42. doi: 10.1128/JCM.00119-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patel P, Mackellar D, Simmons P, et al. Detecting acute human immunodeficiency virus infection using 3 different screening immunoassays and nucleic acid amplification testing for human immunodeficiency virus RNA, 2006–2008. Arch Intern Med. 2010;170:66–74. doi: 10.1001/archinternmed.2009.445. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary appendix 1: Self-administered Survey 1, March 2005.
Supplementary appendix 2: Self-administered Survey 2, March 2009.
Supplementary appendix 3: Self-administered Survey 3, December 2009.
Supplementary appendix 4: Self-administered Survey 4, April 2011.