Abstract
Background
Although depression screening occurs annually in Department of Veterans Affairs (VA) primary care, many Veterans may not be receiving guideline-concordant depression treatment.
Objectives
To determine whether Veterans’ illness perceptions of depression may be serving as barriers to guideline-concordant treatment.
Research Design
We used a prospective, observational design involving a mailed questionnaire and chart review data collection to assess depression treatment utilization and concordance with Healthcare Effectiveness Data and Information Set guidelines adopted by the VA. The Self-Regulation Model of Illness Behavior guided the study.
Subjects
Veterans who screened positive for a new episode of depression at three VA primary care clinics in the U.S. Northeast.
Measures
The Illness Perceptions Questionnaire-Revised, measuring patients’ perceptions of their symptoms, cause, timeline, consequences, cure or controllability and coherence of depression and its symptoms, was our primary measure to calculate Veterans’ illness perceptions. Treatment utilization was assessed three months after the positive depression screen through chart review. HEDIS guideline-concordant treatment was determined according to a checklist created for the study.
Results
839 Veterans screened positive for a new episode of depression from May 2009–June 2011; 275 (32.8%) completed the survey. 92 (33.9%) received HEDIS guideline-concordant depression treatment. Veterans’ illness perceptions of their symptoms, cause, timeline, and controllability of depression predicted receiving guideline-concordant treatment.
Conclusions
Many Veterans are not receiving guideline-concordant treatment for depression. HEDIS guideline measures may not be assessing all aspects of quality depression care. Conversations about Veterans’ illness perceptions and their specific needs are encouraged to ensure that appropriate treatment is achieved.
Keywords: Mental health, mixed methods, illness perceptions, Veterans, primary care, treatment-seeking
INTRODUCTION
The Department of Veterans Affairs (VA), following national guidelines1, mandates annual screening for depression for all Veterans receiving primary care. Between 4% and 9% of Veterans are newly diagnosed with depression each year2, yet not all Veterans with depression are receiving treatment. One study of VA primary care patients found that 44% of those with depression symptomatology were neither diagnosed nor treated3. In primary care, the availability of new medications, such as selective serotonin reuptake inhibitors, make it easier for primary care physicians to treat depression4, and combining medication with cognitive behavioral therapy has shown to be more efficacious in treating depression than one treatment alone5. However, previous research has determined that many patient-centered barriers and beliefs are the most significant barriers to receiving depression care6,7.
Healthcare Effectiveness Data and Information Set (HEDIS) measures are one way in which health care systems determine whether or not patients are receiving appropriate care, including for depression. The VA adopted two HEDIS measures to assess for appropriate depression treatment: 1) optimal practitioner contact, defined as at least three outpatient mental health follow-up encounters within the 84 day acute phase period from diagnosis ; and 2) effective medication coverage, defined as continuity of antidepressant medication treatment during 84 of the 114 days from the index diagnosis date or index prescription date8. We aimed to examine Veterans’ illness perceptions of depression and its treatment at the beginning of a new depression episode, as required to meet HEDIS guideline-concordant treatment, to determine whether or not “illness perceptions” predict treatment utilization.
We used the Self-Regulation Model of Illness Behavior (SRM)9 as a potential conceptual framework for understanding how patients’ perceptions of depressive symptomatology may determine their receipt of treatment10–12. The SRM posits that seven commonsense perceptions of an illness (identity, cause, consequences, timeline, cure/control and coherence beliefs, and emotional responses to symptoms) shape the selection and performance of coping procedures, including the decision to obtain or not obtain medical treatment. Because the SRM was developed as a conceptual model based on self-regulation theory, the Illness Perceptions Questionnaire-Revised (IPQ-R) was developed to assess and quantify these SRM aspects of illness perceptions13. These components of illness perceptions mapping on to the SRM inform whether a person perceives depression as a health threat. A diagnosis stage is not included in the model, as the model is specifically about patients’ illness beliefs.
Our hypothesis was that Veterans who perceive depression as a health threat would be more likely to receive guideline-concordant depression treatment, as measured by two HEDIS depression measures adopted by the VA,8 three months after a positive screen than Veterans who do not perceive depression as a health threat. As only patients’ perceptions of illness are examined through this quantitative measure of illness perceptions, we also collected chart review data of providers’ notes regarding patients’ understanding of depression and treatment decisions, as well as objective treatment utilization data. We synergistically connected a quantitative survey of illness perceptions with qualitative information collected using a content analysis method from providers’ notes in electronic medical records to form a greater awareness of how Veterans’ illness perceptions and provider’ views of patients’ perceptions impact depression treatment utilization14.
METHODS
Study Setting
Veterans from three VA primary care settings in the U.S. Northeast with a primary care mental health integrative clinic in place to enhance Veterans’ access to behavioral services and treatment, including depression15, formed our sample. All study procedures were approved by each facility’s institutional review board. A Certificate of Confidentiality from the National Institutes of Health was obtained to protect Veterans’ health information.
Study Eligibility Screening
As an initial screen for study eligibility, we extracted information weekly from May 2009 through June 2011 from the local electronic database at each of the participating sites in order to identify Veterans’ who had positive screens for depression and for whom this was a new episode of depression. A positive depression screen was based on the annually mandated Patient Health Questionnaire-2 (PHQ-2)16 or Patient Health Questionnaire-9 (PHQ-9)17, if no PHQ-2 score was available, administered in the clinic. Severity scores range from 0–6 on the PHQ-2 and 0–27 on the PHQ-9. Veterans with scores of 3 or higher on the PHQ-2 or 10 or higher on the PHQ-9 were potentially eligible for our study, subject to further criteria as noted below. A waiver of HIPAA authorization allowed a study staff member to access the previous week’s PHQ-2 and PHQ-9 (if available) scores from primary care clinics in order to identify Veterans with positive screens. Two members of the study team then reviewed those Veterans’ electronic medical records to determine whether the Veteran had 1) previously screened positive for depression in the past 12 months or 2) been prescribed any antidepressant in the previous 12 months. If neither of these exclusion criteria were present, indicating that this was a new episode of depression, the Veteran was eligible for the study.
Survey Procedure
Eligible Veterans were sent an invitational letter signed by the site’s clinical investigator to inform them of the study and to invite them to participate. We received a waiver of documentation of written informed consent for completing the questionnaire. If the Veteran did not wish to participate, he or she was instructed to mail back the pre-paid, opt-out postcard. If this postcard was not returned within 10 days, a questionnaire with an enclosed, stamped addressed enveloped was mailed to the Veteran. A reminder letter was sent if the questionnaire was not received after 10 days. After another 10 days, study staff began telephoning Veterans at home to remind them to return the survey18. Up to three telephone messages were left for each Veteran called. Once a questionnaire was received, the Veteran was enrolled in the study.
Questionnaire Items: Illness Perception Questionnaire-Revised
The IPQ-R13 is a widely used, 90-item quantitative measure to assess the seven SRM components. Each item is measured on a five-point Likert type scale with dimensions of strongly disagree, disagree, neither agree nor disagree, agree and strongly agree. IPQ-R questions specific to depression were used in this study10. High scores represent a “health threat”, consisting of strongly held beliefs about the number of symptoms attributed to depression (identity), causal beliefs (cause), the chronicity of depression (timeline), the negative consequences of depression (consequences), positive beliefs about the controllability of depression (cure/control) a personal understanding of depression (coherence) and greater emotional response such as worry, anger or fear (emotional response). Identity questions examine the label of an illness and the symptoms that the patient views as being part of the disease, such as questions asking if the respondent is “feeling sad, blue or down in the dumps”. Cause questions ascertain personal ideas about etiology which may include simple single causes or more complex causal models. An example IPQ-R question is inquires “the loss of a significant relationship caused my symptoms”. Timeline questions explore how long the patient believes the illness will last, such as “the symptoms of my illness change a great deal from day to day”. How one recovers from, or controls, an illness is the focus of the Cure/Control questions, an example being “there is very little that can be done to improve my symptoms”. Consequence questions are about the expected effects and outcomes of an illness. One IPQ-R item states “my symptoms cause difficulties for those who are close to me”. Asking respondents who well they understand an illness or symptoms form the Coherence questions. One example involves asking respondents to indicate their strength of agreement or disagreement with “I don’t understand my symptoms”. Emotional Response questions assess the emotions generated by the illness and symptoms, such as “my symptoms do not worry me”.
In many studies which have used the IPQ-R, factor analyses have determined that scale questions assessing specific SRM components become further divided into subscales, such as three subscales of personal control, treatment control and external control for questions used to assess the SRM Cure/Control component.13 Thus, factor analysis to determine subscales from these 90 questions was undertaken in this study (see Analysis section).
Questionnaire Items: Demographics
Participants’ age, gender, race/ethnicity, education, employment status, and treatment for depression in the past five years were assessed in the mailed questionnaire.19 For patients who did not complete the questionnaire, we collected gender and race/ethnicity data from chart reviews, if available. Research has shown that past treatment behavior often predicts future behavior.20 As we were not able to determine objective treatment data beyond the past 12 months according to chart review, we asked Veterans to complete a self-reported yes/no question about whether or not they received any treatment for depression from a VA or a non-VA provider in the past five years before the 12 month inclusion period.
Treatment Utilization
Treatment for depression, which corresponds to receipt of treatment in the SRM, was measured using the two HEDIS measures adopted by the VA, as described earlier. We recorded whether depression treatment received was guideline-concordant or not for each Veteran patient, according to both optimal practitioner contact and effective medication coverage measures. For those who did not receive guideline-concordant treatment, we tracked the amount and what kind of treatment they did receive, if any at all (Table 2).
Table 2.
Characteristics of Study Sample
|
Study sample N=271 |
% | |||
|---|---|---|---|---|
| Agea | ||||
| 20–50 | 65 | 24.2 | ||
| 51–60 | 74 | 27.5 | ||
| 61–70 | 70 | 26.0 | ||
| 71+ | 60 | 22.3 | ||
| Gendera | ||||
| Male | 251 | 93.3 | ||
| Female | 18 | 6.7 | ||
| Racea | ||||
| White | 244 | 92.8 | ||
| Other | 19 | 7.2 | ||
| Educationa | ||||
| Less than 12th Grade | 16 | 5.9 | ||
| 12th Grade or Equivalent | 65 | 24.2 | ||
| Trade/Tech/Vocational | 32 | 11.9 | ||
| Some College | 83 | 30.9 | ||
| Associate/Bachelor Degree | 55 | 20.5 | ||
| Post-Graduate/Professional | 18 | 6.7 | ||
| Marital Statusa | ||||
| Married/With Partner | 135 | 50.0 | ||
| Divorced | 42 | 15.6 | ||
| Never Married | 40 | 14.8 | ||
| Widowed | 31 | 11.5 | ||
| Separated | 22 | 8.2 | ||
| Respondents by VA Facility | ||||
| Site 1, Surburan | 93 | 34.3 | ||
| Site 2, Urban | 74 | 27.3 | ||
| Site 3, Urban | 104 | 38.4 | ||
| Treatment for Depression | ||||
| VHA & Non-VHA (Past 5 Years)a | 103 | 38.4 | ||
| Depression Treatment Within HEDIS Guidelinesb | 92 | 34.0 | ||
| Depression Treatment Not Within HEDIS Guidelinesb | 51 | 18.8 | ||
| Mental Health Treatment (Not For Depression) | 10 | 3.7 | ||
| No Treatment | 118 | 43.5 | ||
Note:
To account for missing data among the overall sample, n = 263 for race, n = 269 for age, gender, and education, and n = 270 for marital status.
HEDIS guidelines include optimal practitioner contact, defined as three or more outpatient mental health follow-up encounters with a mental health or non-mental health practitioner within the 84 day acute treatment phase of depression; and 2) effective medication coverage, defined as continuity of antidepressant medication treatment during 84 of the 114 days following the index anti-depressant prescription date.
Treatment utilization was determined from providers’ notes and diagnosis codes in medical records and extracted using a checklist which was piloted by one clinician and one non-clinician investigator (Table 1). After pilot testing, one investigator reviewed each Veteran’s electronic medical record to answer the eight checklist questions. Two investigators allocated Veterans to one of the two treatment groups (guideline-concordant or not) for each of the HEDIS measures based on answers to these checklist questions. A third, clinical investigator reviewed the treatment categorization decisions by the first two investigators. If changes were determined based on this third review, they were reached through consensus and discussion. Providers’ notes about Veterans who did not receive any treatment were collected in a Microsoft Access database for further qualitative analysis to examine providers’ reasons about why Veterans may not have received any depression treatment.
Table 1.
Checklist Questions to Determine HEDIS Treatment Concordance
| Table 1: Checklist Questions | Eligibility | Guideline Concordant Treatment |
|---|---|---|
| 1. Does the patient have a depression diagnosis? | Yes: only if a result of the most recent positive depression screen (index screen) | Either optimal practitioner contact or effective medication coverage |
| 2. When was the depression diagnosis given? | Yes: if given at index screen or in 84 days after index screen | Either optimal practitioner contact or effective medication coverage |
| 3. Did the provider refer the patient to mental health services? | Yes: if referred at index screen or in 84 days after index screen | Optimal practitioner contact |
| 4. Was depression discussed with the patient? | Yes: only if discussed at index screen or 84 days after index screen | Optimal practitioner contact |
| 5. If there is no evidence of depression being discussed, do words such as mood, sad, down or suicide appear in a free text search and do these suggest evidence of discussion with provider about depression or treatment? | Yes: only if discussed at index screen or in 84 days after screen | Optimal practitioner contact |
| 6. Did the patient have any follow-up appointments with a provider about depression? | Yes: if in 84 days after index screen | Optimal practitioner contact |
| 7. Was the patient prescribed antidepressant medication? | Yes: if in 84 out of 114 days after index screen | Effective medication coverage |
| 8. If the patient was prescribed antidepressant medication, did he/she refill the medication? | Yes: if in 84 out of 114 days after index screen | Effective medication coverage |
Data Analysis: Quantitative
We carried out our quantitative analyses in two phases. First, rather than use individual 90 IPQ-R scale items as predictor variables in our models, we conducted factor analyses to form subscales of collections of items. Each subscale was assessed for reliability using Cronbach’s alpha23. Once subscales were formed, we fit a logistic regression analysis to model predictors of receiving HEDIS guideline-concordant treatment, with the IPQ-R subscales, age, gender, self-reported past depression treatment and PHQ-2 scores as a proxy for depression severity, as predictors, along with VA primary care site-specific random effects. In five cases where only a PHQ-9 score was available, we imputed the mean average of the PHQ-2 and used that score (4.4) in the logistic regression models. To check for multicollinearity, we computed variance inflation factors (VIF) for each predictor in the model24 and checked whether any were greater than 10, a conventional threshold above which collinearity is considered problematic. All analyses were conducted using the SAS statistical package; the factor analyses were performed using PROC FACTOR, and the random effects logistic regressions were implemented in PROC GLIMMIX. Intra-class correlations (ICC) were computed through an approximation method to determine whether variations in receipt of guideline-concordant treatment varied by VA site25.
Data Analysis of Chart Narratives from “No Treatment” Group
Two analysts used conventional content analysis to examine providers’ notes from Veterans’ electronic medical records, to determine documented reasons a Veteran may not have received treatment. In conventional content analysis, coding categories are derived directly from text data to describe a phenomenon.26 Providers’ notes about “no treatment” Veterans were read and examined independently and then categories were created through a discussion process. Where possible, these emergent categories were mapped onto the IPQ-R domains.
RESULTS
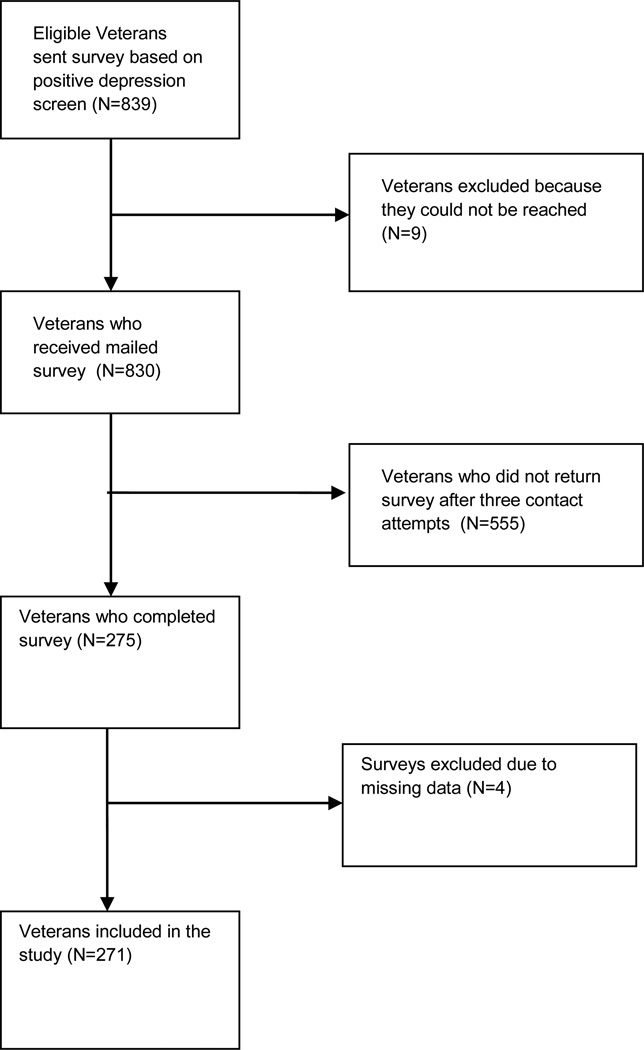
Weekly reviews of electronic medical record data across the three VA sites resulted in identification of 839 positive depression screens for new episodes of depression (Figure 1). Of the 271 Veterans who completed a questionnaire, 92 (34%) received HEDIS guideline-concordant depression treatment, 51 (18.8%) received depression treatment that was not guideline-concordant, 10 (3.7%) received mental health treatment that was not specifically for depression and 118 (43.5%) did not receive any treatment in the three months following a positive depression screen (Table 2). Conducting additional chart reviews to six months post-positive depression screen did not alter these proportions significantly. Veterans who did not complete the questionnaire (n=555) were mostly White and male. Women accounted for 16 of these Veterans, three were Latino, three were African American, 2 were of other race/ethnicity, and 28 did not have their race or ethnicity recorded in the medical record.
Figure 1.
Flow Chart Diagram of Veteran Participant Population
Table 3 lists the individual subscale means, standard deviations and percent missing data by treatment groups and Cronbach alpha scores for each of the 21 IPQ-R subscales representing seven SRM domains resulting from the factor analysis of the 90 items measuring illness perceptions of depression. The main IPQ-R components of identity, cause, timeline and cure/control were further subdivided into subscales, while the main components of consequence, coherence and emotional response remained single scales. Most scales were internally consistent with Cronbach’s alphas substantially above 0.70. Missing data was low.
Table 3.
IPQ-R Subscale α’s and Mean Scores among Treatment Groups on IPQ-R Subscales across 3 VA Sites
| IPQ-R main components and subscale information |
Missing | Alpha | HEDIS Guideline- Concordant Depression Treatment vs. Others |
|||
|---|---|---|---|---|---|---|
| N (%) | α | Yes (n=92) | No (n=179) | |||
| M | SD | M | SD | |||
| Identity (5 subscales) | ||||||
| Lethargy (8 items) | 0 | 0.84 | 2.14 | 0.54 | 2.40 | 0.63 |
| Depressed mood (5 items) | 0 | 0.84 | 2.30 | 0.63 | 2.71 | 0.63 |
| Anxiety symptoms (5 items) | 0 | 0.78 | 3.26 | 0.65 | 3.28 | 0.56 |
| GI/Somatic (4 items) | 0 | 0.69 | 2.84 | 0.63 | 2.86 | 0.63 |
| Sexual (1 item) | 9 (3.3) | N/A | 2.27 | 1.12 | 2.56 | 1.15 |
| Cause (7 subscales) | ||||||
| Stress (6 items) | 3 (1.1) | 0.81 | 2.62 | 0.79 | 2.85 | 0.84 |
| Family (5 items) | 2 (0.7) | 0.73 | 3.49 | 0.76 | 3.51 | 0.78 |
| Poor health (4 items) | 2 (0.7) | 0.74 | 3.45 | 0.99 | 3.38 | 0.94 |
| Environment (4 items) | 2 (0.7) | 0.75 | 4.10 | 0.69 | 3.82 | 0.83 |
| Risky behavior (4 items) | 3 (1.1) | 0.66 | 4.00 | 0.73 | 3.96 | 0.75 |
| Grief/loss (2 items) | 2 (0.7) | 0.71 | 3.55 | 1.13 | 3.45 | 1.14 |
| Overworked (1 item) | 7 (2.6) | N/A | 3.70 | 1.04 | 3.73 | 1.11 |
| Timeline (3 subscales) | ||||||
| Acute (3 items) | 3 (1.1) | 0.65 | 2.33 | 0.48 | 2.48 | 0.55 |
| Chronic (3 items) | 3 (1.1) | 0.84 | 2.33 | 0.98 | 2.53 | 0.96 |
| Cyclical (3 items) | 4 (1.5) | 0.82 | 2.44 | 0.86 | 2.71 | 0.88 |
| Cure/Control (3 subscales) | ||||||
| Personal control (7 items) | 4 (1.5) | 0.85 | 2.75 | 0.71 | 2.88 | 0.65 |
| Treatment control (3 items) | 4 (1.5) | 0.84 | 2.60 | 0.69 | 2.87 | 0.73 |
| External control (4 items) | 4 (1.5) | 0.45 | 3.03 | 0.57 | 2.94 | 0.55 |
| Consequence (1 scale, 5 items) | 3 (1.1) | 0.88 | 2.15 | 0.80 | 2.50 | 0.86 |
| Coherence (1 scale, 5 items) | 5 (1.8) | 0.62 | 2.83 | 0.92 | 2.99 | 1.04 |
| Emotional Response (1 scale, 5 items) | 3 (1.1) | 0.51 | 2.14 | 0.69 | 2.43 | 0.76 |
Table 4 presents the random effects logistic regression model predicting HEDIS guideline-concordant depression treatment by IPQ-R subscale, age, gender, self-reported past treatment and PHQ-2 score. Veterans who perceived that their symptoms were unrelated to depressed mood, who believed that they personally could control their depressive symptoms (personal control), who perceived their symptoms as coming and going (cyclical timeline), and who attributed the cause of their depressive symptoms to family problems were less likely to receive guideline-concordant treatment three months after a positive depression screen. However, Veterans who felt that control of their symptoms was not up to them (external control) were more likely to receive guideline-concordant depression treatment three months later. These results were upheld even with the significance of covariates such as self-reported past depression treatment in the past five years. The intra-class correlation (ICC) of 12.4% indicated that variation in the three VA sites accounted for a moderate amount of variation in depression treatment outcomes (Table 4).
Table 4.
Random Effects Logistic Regression Predicting Likelihood of HEDIS Guideline-Concordant Treatment within 3 Months Following a Positive Depression Screen across 3 VA Sites
| IPQ-R subscale (main component) |
HEDIS Guideline-Concordant Depression Treatment (n=81) vs. Others (n=161) ICC=12.4% |
||
|---|---|---|---|
| Beta | SE | 95% CI | |
| Depressed mood (Identity) | −1.28** | 0.45 | −2.16, −0.40 |
| Cyclical timeline (Timeline) | −0.50* | 0.25 | −0.98, −0.01 |
| Personal control (Cure/Control) | −0.86* | 0.42 | −1.69, −0.03 |
| External control (Cure/Control) | 1.10** | 0.39 | 0.33, 1.87 |
| Poor health (Cause) | 0.21 | 0.24 | −0.27, 0.68 |
| Family (Cause) | −0.68* | 0.31 | −1.29, −0.07 |
| Risky behavior (Cause) | 0.46 | 0.30 | −0.13, 1.05 |
| Consequence | −0.70 | 0.37 | −1.43, 0.03 |
| Race (White) | 0.35 | 0.66 | −0.94, 1.64 |
| Gender (Male) | −0.72 | 0.67 | −2.04, 0.61 |
| Ages 20–50 | 0.65 | 0.66 | −0.96, 2.25 |
| Ages 51–60 | 0.81 | 0.60 | −0.66, 2.28 |
| Ages 61–70 | 0.42 | 0.60 | −1.05, 1.89 |
| Depression Treatment (Past 5 Years) | 1.37*** | 0.38 | 0.63, 2.11 |
| Total PHQ-2 score | 0.005 | 0.15 | −0.30, 0.30 |
Note:
p<.05.
p<.01.
p<.001.
N=242 in final model to account for missing data.
SE=Standard Error, CI=Confidence Interval, Bold indicates statistical significance at any level from p<.05. IPQ-R Illness Perception Questionnaire-Revised. IPQ-R variables that were not significant are not included in the table.
Qualitative Results from Chart Narratives among Veterans who did not Receive Treatment
Six categories of providers’ documented reasons were derived from the content analysis to examine providers’ viewpoints on why 118 Veterans did not receive any treatment in this study: 1) Veteran refused treatment (n=44, 37%); 2) No treatment referral was made (n=32, 27%); 3) Provider did not mention positive depression screen to Veteran (n=20, 17%); 4) Veteran cancelled or was a no show to treatment session (n=13, 11%); 5) Veteran denied having depression (n=5, 4%) and 6) No follow-up occurred with Veteran following discussion of treatment (n=4, 3%).
A Veteran was classified as having refused treatment when a note such as the following was documented in the electronic medical record:
“states due to life changes, has started to feel depressed; states has financial stressors as well. Feels bored, loss of job and goal in life has also caused depression. Pt [sic] refuses treatment at this time”.
These reasons for refusing treatment may be related to the patient’s perception of the cause of depression, one of the SRM components. To indicate that a provider did not refer a patient for further treatment, a note stated that “patient not clinically depressed” or “patient does not require further Tx [sic] at this time”, suggesting that a conversation about the positive depression screen had taken place and that the provider and patient had decided that further treatment was not warranted.
Evidence that no follow-up occurred after the positive screen is when a discussion about depression is noted, but no further information on the Veteran’s treatment for depression appears in any part of the electronic medical record. If a patient denied his or her depression, a provider note stated, as an example:
“he has been fatigued, excess sleep, anhedonia; lives with his son here. His foot pain is mild and not contributing to lack of interest in doing things. He does not think he has depression”.
These notes suggest that during the patient-provider conversation about depression, the patient was attributing symptoms of depression to other factors such as fatigue and pain. This aspect of labeling depressive symptoms as indicative of physical pain or functioning is part of the SRM component of identity and is measured by several subscales in the IPQ-R. When a patient cancelled or was a no show at referral appointments, an example provider note was as follows:
“Patient screened in [Primary Care Behavioral Health] upon referral from PCP [sic] to talk to someone about stress. Pt [sic] wasn’t interested in setting up any more appointments, despite staff contacting him over phone twice”.
The mention of stress again may be related to the SRM components of cause and identity, which, according to this provider’s note, were part of the dialogue between provider and patient.
DISCUSSION
This study found that some illness perceptions of depression are predictive of Veterans’ receiving HEDIS guideline-concordant depression treatment in the three months following a positive depression screen, and that providers’ notes about Veterans who did not receive treatment often reflected these same illness perceptions. These results provide empirical evidence for our hypothesis, that Veterans who perceive depression as a health threat would be more likely to receive guideline-concordant treatment three months after a positive screen than Veterans who do not perceive depression as a health threat.
How Providers Can Benefit from Understanding Patients’ Perceptions of Depression
These results provide high validity of the SRM as a logic model for helping clinicians and organizational leaders conceptualize how Veterans understand depression and its treatment and the types of constructs that should be part of patient-provider discussions in order to fully involve Veterans in decisions about depression care. Specific IPQ-R scales of depressed mood, cyclical timeline, personal and external control, and family as the cause of depression predicted Veterans’ receipt of guideline-concordant depression treatment. When Veterans did not think that their symptoms were indicative of depressed mood but rather gave some other label to their symptoms, they were less likely to receive guideline-concordant treatment. Discussing aspects of depressed mood (such as irritability, bowel pain) may help patients correctly identify their symptoms as depression. For patients whose depressive symptoms are cyclical in nature, they may believe that relief is anticipated, which may be one reason why seeking treatment for depression is perceived as unnecessary. Increasing patients’ understanding of the timeline of depressive symptoms may help them make informed decisions about seeking depression treatment.
When patients’ perceived that they have personal control over their symptoms, they were less likely to seek or receive guideline-concordant depression treatment. It is possible that these patients believed that they have the ability to conquer depression on their own. Conversely, patients who believed that something else—an external source—controls depression, they were more likely to receive guideline-concordant depression. Patients who perceived this may have tried treating depression on their own (personal control) and did not succeed. This is not known from the current study, but is a potential avenue for future research, to explore this mechanism of action. Patients who reported that their family issues caused their depression were less likely to receive guideline-concordant treatment. In these situations, it is possible that patients felt that if they achieved relief in their personal life, they would be rid of these depressive symptoms. Provider notes also indicated this. It is true that not all positive depression screens will result in a diagnosis of depression;16 however, it is important for patients and providers to discuss what true causes of depression might be and what other causes may be aggravating symptoms, so that patients can have a fuller understanding of depression etiology.
Our findings can inform different ways of thinking about the types of interventions needed to encourage Veterans’ greater uptake of depression treatment. Identifying how to tailor information to patients based on their specific illness perceptions of depression will be important for providers when trying to encourage greater uptake of treatment. Additionally, these tailored discussions may provide insight into patients’ readiness to seek treatment, a concept not assessed in our study but is likely related to illness perceptions, contextual barriers such as unemployment and access, and decisions to seek treatment30.
A limitation of our study is the use of HEDIS measures to determine quality depression treatment. Researchers have shown that using HEDIS depression indicators to predict clinical improvement in depression outcomes is a difficult accomplishment.31 Another limitation of this study is that it involves Veterans only from the U.S. Northeast, and therefore it is possible that other illness perceptions may play a role in Veterans’ treatment utilization in other parts of the country. However, our study highlights the importance of acknowledging and discussing Veterans’ illness perceptions about the severity and cause of symptoms, its controllability, and beliefs about how long depression and its symptoms as one way to facilitate uptake of treatment.
Acknowledgments
This study was funded by the Department of Veterans Affairs, Health Services Research and Development Service, Grant IAC 07-087, to A.R. Elwy.
Dr. Elwy is also an investigator with the Implementation Research Institute (IRI), at the George Warren Brown School of Social Work, Washington University in St. Louis, through an award from the National Institute of Mental Health (R25 MH080916-01A2) and the Department of Veterans Affairs, Health Services Research and Development Service, Quality Enhancement Research Initiative.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
REFERENCES
- 1.O’Connor EA, Whitlock EP, Beil TL, et al. Screening for depression in adult patients in primary care settings: a systematic evidence review. Ann Intern Med. 2009;151:793–803. doi: 10.7326/0003-4819-151-11-200912010-00007. [DOI] [PubMed] [Google Scholar]
- 2.Desai MM, Rosenheck RA, Craig TJ. Case-finding for depression among medical outpatients in the Veterans Health Administration. Med Care. 2006;44:175–181. doi: 10.1097/01.mlr.0000196962.97345.21. [DOI] [PubMed] [Google Scholar]
- 3.Liu CF, Campbell DG, Chaney EF, et al. Depression diagnosis and antidepressant treatment among depressed VA primary care patients. Admin Pol Ment Health Ment Health Serv Res. 2006;33:331–341. doi: 10.1007/s10488-006-0043-5. [DOI] [PubMed] [Google Scholar]
- 4.Druss BG. The changing face of U. S. mental health care. Am J Psychiatry. 2010;167:1419–1421. doi: 10.1176/appi.ajp.2010.10091258. [DOI] [PubMed] [Google Scholar]
- 5.Thase ME, Friedman ES, Biggs MM, et al. Cognitive therapy versus medication in augmentation and switch strategies as second-step treatments: a STAR*D report. Am J Psychiatry. 2007;164:739–752. doi: 10.1176/ajp.2007.164.5.739. [DOI] [PubMed] [Google Scholar]
- 6.Edlund MJ, Fortney JC, Reaves CM, et al. Beliefs about depression and depression treatment among depressed veterans. Med Care. 2008;46:581–589. doi: 10.1097/MLR.0b013e3181648e46. [DOI] [PubMed] [Google Scholar]
- 7.Nutting PA, Rost K, Dickinson M, et al. Barriers to initiating depression treatment in primary care practice. J Gen Intern Med. 2002;17:103–111. doi: 10.1046/j.1525-1497.2002.10128.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chermack ST, Zivin K, Valenstein M, et al. The prevalence and predictors of mental health treatment services in a national sample of depressed veterans. Med Care. 2008;46:813–820. doi: 10.1097/MLR.0b013e318178eb08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leventhal H, Leventhal EA, Contrada RJ. Self-regulation, health and behavior: a perceptual-cognitive approach. Psych Health. 1998;13:717–733. [Google Scholar]
- 10.Brown C, Battista DR, Sereika SM, et al. Primary care patients’ personal illness models for depression: relationship to coping behavior and functional disability. Gen Hosp Psychiatry. 2007;29:492–500. doi: 10.1016/j.genhosppsych.2007.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ward EC, Clark LO, Heidrich S. African American women’s beliefs, coping behaviors and barriers to seeking mental health services. Qual Health Res. 2009;19:1589–1601. doi: 10.1177/1049732309350686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elwy AR, Yeh J, Worcester J, et al. An illness perception model of help seeking for depression. Qual Health Res. 2011;21:1495–1507. doi: 10.1177/1049732311413781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moss-Morris R, Weinman JA, Petrie KJ, et al. The Revised Illness Perception Questionnaire (IPQ-R) Psych Health. 2002;17:1–16. [Google Scholar]
- 14.Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. 2nd ed. Thousand Oaks, CA: Sage; 2011. [Google Scholar]
- 15.Pomerantz A, Cole BH, Watts BV, et al. Improving efficiency and access to mental health care: combining integrated care and advanced access. Gen Hosp Psychiatry. 2008;30:546–551. doi: 10.1016/j.genhosppsych.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 16.Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: Validity of a 2 item depression screener. Med Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 17.Spitzer RL, Kroenke K, Williams JBW the Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 18.Dillman DA. Why choice of survey mode makes a difference. Pub Health Rep. 2006;121:11–13. doi: 10.1177/003335490612100106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eisen SV, Normand SL, Belanger AJ, et al. The Revised Behavior and Symptom Identification Sale (BASIS-R): reliability and validity. Med Care. 2004;42:1230–1241. doi: 10.1097/00005650-200412000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Sutton S. Predicting and explaining intentions and behavior: how well are we doing? J Appl Soc Psych. 1998;28:1317–1338. [Google Scholar]
- 21.Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 2nd ed. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- 22.Charmaz K. Constructing Grounded Theory. Thousand Oaks, CA: Sage; 2006. [Google Scholar]
- 23.Cronbach L. Coefficient alpha and the internal dtructure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 24.Kutner MH, Nachtsheim C, Neter J. Applied Linear Regression Models. 4th ed. McGraw-Hill Irwin: 2004. [Google Scholar]
- 25.Hedeker D. A mixed-effects multinomial logistic regression model. Statistics in Medicine. 2003;22:1433–1446. doi: 10.1002/sim.1522. [DOI] [PubMed] [Google Scholar]
- 26.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 27.Miles MB, Huberman AM. Qualitative Data Analysis. 2nd ed. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 28.Qualitative Solutions and Research. NUD*IST Vivo (Nvivo) Melbourne, Australia: Pty. Ltd; 1999. [Google Scholar]
- 29.AUTHORS. A mixed methods examination of the impact of stigma on veteran treatment seeking for depression. Under review [Google Scholar]
- 30.Wells A, Lagomasino IT, Palinkas LA, et al. Barriers to depression treatment among low-income, Latino emergency department patients. Comm Ment Health J. 2012 doi: 10.1007/s10597-012-9547-5. Published online September 30. [DOI] [PubMed] [Google Scholar]
- 31.Rost K, LM Dickinson, Fortney J, Westfall J, Hermann RC. Clinical improvement associated with conformance to HEDIS-based depression care. Ment Health Serv Res. 2005;7:103–112. doi: 10.1007/s11020-005-3781-1. [DOI] [PMC free article] [PubMed] [Google Scholar]