Abstract
Background
Adolescent substance use treatment outcome research generally shows small to moderate effects in reducing substance use, with no specific “brand” of treatment emerging as clearly superior to any other, and treatment gains that fade over time. The relatively weak and temporary effects of treatment call for improving the potency and durability of intervention effects. In response to this call, this critical narrative review summarizes research on mechanisms of change for both adults and adolescents in substance use treatment, with a particular focus on reviewing what is known regarding “how” adolescent substance use treatment works.
Methods
A comprehensive review of the adolescent (ages 11–18) substance use treatment literature was conducted to identify empirical studies that examined mediators of intervention effects. Relevant databases (e.g., PsychINFO, Medline) were searched using key words (e.g., “mediator”), and relevant articles from reference sections of identified studies and review papers were considered.
Results
Studies of mechanisms of psychotherapy change are rare in the adult, and particularly adolescent, substance use treatment outcome literature. The four adolescent studies that examined substance use treatment mechanisms found that positive social support, motivation to abstain, and positive parenting behaviors mediated treatment effects. To date, research has not supported therapy-specific mechanisms of change, finding instead that “common” processes of change largely account for improvements in outcome across distinct “brands” of treatment.
Conclusions
The lack of empirical support for treatment-specific mechanisms of change may be due to the need for greater precision in defining and measuring treatment-specific causal chains. Future directions include neuroscience approaches to examining changes in brain functioning that are associated with treatment response and recovery and examining mechanisms in adaptive treatment designs, which can accommodate individual differences in targets for intervention and response to treatment.
Keywords: adolescent, substance use treatment, mechanisms of change, treatment outcome
INTRODUCTION
A recent national survey indicated that less than one out of five (<20%) youth identified as needing substance use treatment received intervention1, despite significant health, social, and financial costs associated with youth substance use2. Given the importance of early and effective intervention, this review focuses on treatment for adolescent substance use, including what is known regarding youth treatment outcomes, and mechanisms underlying reductions in substance use. Due to the limited literature on mechanisms of change (MOC) for adolescent substance use treatment, findings from adult studies will be reviewed as a starting point for recommendations regarding MOC research with adolescent substance users. This review focuses on theorized MOC for Motivational Interviewing/Enhancement Treatment (MI/MET) and Cognitive Behavioral Therapy (CBT) because these interventions have the greatest cumulative evidence for efficacy3, 4, 5. This review concludes by discussing future directions for studying MOC in adolescent substance use treatment.
REVIEW
Historical Background and Effectiveness of Adolescent Substance Use Treatment
Adolescent substance use treatment has historically been based on programs developed for adults, often with little to no modification despite developmental differences in type of substances commonly used by youth (e.g., alcohol and marijuana), adolescents’ lower readiness to change due to external pressure for treatment, shorter histories of use, adolescent-specific negative consequences of use (e.g., poor academic performance), and developing cognitive abilities6, 7. For example, community-based treatment for adolescent substance use commonly relies on an approach developed for adults, which has the Minnesota Model and its adherence to the 12-steps of Alcoholics and Narcotics Anonymous at its core, with supplemental training in relapse prevention8. However, based on the relatively recent recognition of the special needs and developmental context of adolescent substance use, adaptations of CBT, MI/MET, and family-based interventions have been developed to address adolescent substance use (e.g., Cannabis Youth Study treatment manuals). The National Registry of Evidence-based Programs and Practices catalogs effective treatment options for adolescents and adults (http://nrepp.samhsa.gov/).
Adolescent treatment outcome research has shown some promising results in terms of reductions in substance use following treatment4, 9, 10. Reductions in substance use are most robust at treatment completion4. Similar to the adult treatment outcome literature11, 12, many youth return to substance use after treatment4,13. Importantly, individuals differ in response to treatment, as evidenced by multiple post-treatment trajectories of substance use, including patterns of continuing heavy use, gradual reductions in use, an increase from low levels of use during treatment, and steady low levels of substance use14–16. Predictors of worse adolescent treatment outcome include greater severity and chronicity of use; co-occurring psychopathology, particularly conduct problems; and early treatment drop-out13, 16. In brief, treatment gains occur, but tend to fade over time, and there is heterogeneity in response to treatment that is associated with certain client characteristics.
A landmark clinical trial for adolescent substance use, the Cannabis Youth Treatment study CYT17, 18, compared the effectiveness of five evidence-based treatments: CBT, Multidimensional Family Therapy (MDFT), Family Support Network, Adolescent Community Reinforcement Approach, and MET. These interventions were selected, in part, because they are well-defined and relatively distinct in terms of theoretical basis and prescribed techniques17. CYT results indicated that no single intervention emerged as more effective than another18. These CYT “null” results regarding differential effectiveness of specific therapies are similar to other clinical trials that compared specific “brands” of therapy among adolescent substance users 4, adult substance users11, 19, and treatment research involving adults with other psychiatric conditions20. Overall, clinical trials comparing distinct types of treatment in adolescent and adult substance users have found small to moderate effects in reducing substance use, with no specific “brand” of treatment emerging as superior to another4, 11.
Shift from Treatment Outcome Research to Studying MOC
The small to moderate effects of adolescent substance use treatment on outcomes and fading treatment gains over time, underscore the need for more potent interventions with more durable effects4, 10. To address this need, the research paradigm has shifted from documenting treatment outcomes to examining how treatment works21. Identifying mechanisms of behavior change, or factors that explain “how” treatment works (e.g., “active ingredients”), has important implications for increasing treatment effectiveness. For example, by identifying “active ingredients,” treatment could focus on the delivery of these “active ingredients” in an optimal dosing range and in specific combinations according to individual needs to boost effectiveness22, 23. Treatment components that are shown to be ineffective or counterproductive (e.g., confrontational therapist style) could be reduced or eliminated24. MOC research also may inform the development of novel interventions that amplify the effect of “active ingredients”22. Finally, increased understanding of how behavioral change occurs, specifically in a therapeutic context, could help to refine the theoretical basis for distinct forms of treatment and more broadly, could reveal cross-cutting or “common” processes across therapies, such as therapeutic alliance, goal-setting, and monitoring progress that lead to positive outcomes25, 26.
Hypothesized Treatment-specific MOC: CBT and MI
Distinct forms of treatment (e.g., CBT, MI/MET) are thought to exert their effects through unique theory-based MOC (e.g., treatment-specific techniques and processes), which can be distinguished from other active treatments and placebo27. A particular “brand” of therapy could involve many active ingredients and multiple MOC. Further, MOC may operate as part of a larger causal chain of sequenced and interacting processes that lead to specific outcomes28. Although distinct therapies might be equally effective18, 19, the active ingredients used and MOC through which each treatment operates might differ29.
CBT treatment strategies, which include relapse prevention techniques8, are based in large part on social learning theory30. CBT is based on the hypothesis that substance using individuals may have deficits in the ability to cope with general life stressors and high-risk situations for substance use27, 31. CBT active ingredients include, for example, instruction in coping skills, role play, behavioral rehearsal, and positive reinforcement to improve general and substance-specific coping skills and to enhance self-efficacy to resist substance use32. Skill acquisition in CBT has been proposed to involve strengthening cognitive control over behavior, and improved ability to regulate emotion in response to stressors33. A primary goal of CBT is to enhance an individual’s cognitive and behavioral coping skills and self-efficacy in handling stressors as mechanisms that lead to reduction in substance use.
Whereas CBT assumes that an individual is ready to change and only needs to acquire the skills and confidence to do so, MI/MET aims to enhance motivation to change substance use by exploring an individual’s ambivalence to change in the context of an empathic, directive discussion34. MI principles are based on decision-making and cognitive dissonance theories35, 36. MI active ingredients include therapist style (non-confrontational, directive, client-centered: “MI spirit”) and specific techniques (e.g., decisional balance, providing normative feedback) used to elicit “change talk” or a commitment to positive behavior change34. Hypothesized MI mechanisms include client behaviors such as experiencing discrepancy between current and desired behavior, and amount of client “change talk” generated24, 37. Among proposed active ingredients, “change talk” has received the most consistent support in analyses of mechanisms underlying MI effects on outcome38.
Methods to Identify Mechanisms that Explain “How” Treatment Works
Study design for treatment outcome research, which relies on pre- and post-treatment assessment, is not optimal for investigating “how” treatment works. Ideally, a study of treatment mechanisms would include: fine-grained (e.g., session by session) longitudinal assessment that begins prior to the first treatment session to establish a “baseline”39, evaluation of the therapist-client relationship across sessions40, 41, assessment of extra-treatment factors related to outcome (e.g., family and peer environment), and follow-up assessments to examine durability of effects. In addition, methods such as Ecological Momentary Assessment (EMA), which collect fine-grained data, have been used to identify proximal relapse precipitants42. Fine-grained, longitudinal assessment can identify individual trajectories of change during treatment43, as well as better capture discontinuities and non-linear patterns of change that predict relapse44, 45. Intensive assessment, however, increases participant burden, and assessment reactivity needs to be considered46.
In addition to study design issues, conceptual guidelines and statistical methods used to identify MOC have received attention22, 29, 47. Seven suggested requirements for testing MOC in psychotherapy research include: (1) strong association between active ingredient (e.g., coping skills training) and outcome (e.g., reduced alcohol use); (2) specificity of the association between active ingredient, proposed mechanism (e.g., assertive drink refusal behavior) and outcome; (3) dose-response relationship (i.e., greater effects with greater treatment dose); (4) manipulation of the proposed active ingredient results in a change in outcome; (5) temporal precedence of the mechanism in relation to outcome; (6) replicability of results; and (7) plausibility and coherence, that is, the explanation of how the active ingredient works makes sense in the context of theory and the existing literature22, 47. Although all guidelines are unlikely to be met, meeting more guidelines provides stronger support for the proposed MOC22.
Statistically, MOC are most commonly examined by testing a mediator or an intervening variable through which treatment is proposed to have an effect on outcome48, 49. A mediator is a variable that is used to represent a mechanism of change50. However, a mediator may not necessarily be the mechanism of change. Instead, a mediator might point to or be associated with a MOC. For example, increased self-efficacy as the measured mediator might point to the mechanism of cognitive restructuring in CBT, which may, in turn, be associated with increased self-efficacy. General analytic guidelines in testing mediation include demonstration of an association between: the intervention (e.g., coping skills training) and outcome (e.g., reduced alcohol use), although this is not necessary for testing mediation48, 49; intervention and mediator (e.g., improved drink refusal behavior); and mediator and outcome51.
The basic method to statistically test mediation has been extended to examine multiple mediators simultaneously, moderated mediation, mediated moderation, and conditional indirect effects49, 50. Importantly, a moderator can provide information on “for whom” treatment has greater or lesser effect. For example, gender might moderate the extent to which improved coping skills mediate the association between an active ingredient (e.g., teaching drink refusal skills) and outcome (e.g., binge drinking frequency). Identification of moderators can aid efforts to match client characteristics and needs to specific interventions in order to improve outcomes among certain subgroups. To date, however, evidence for client-treatment matching in adult samples using CBT has resulted in small and inconsistent effects50.
Research on MOC for CBT and MI/MET in Adults
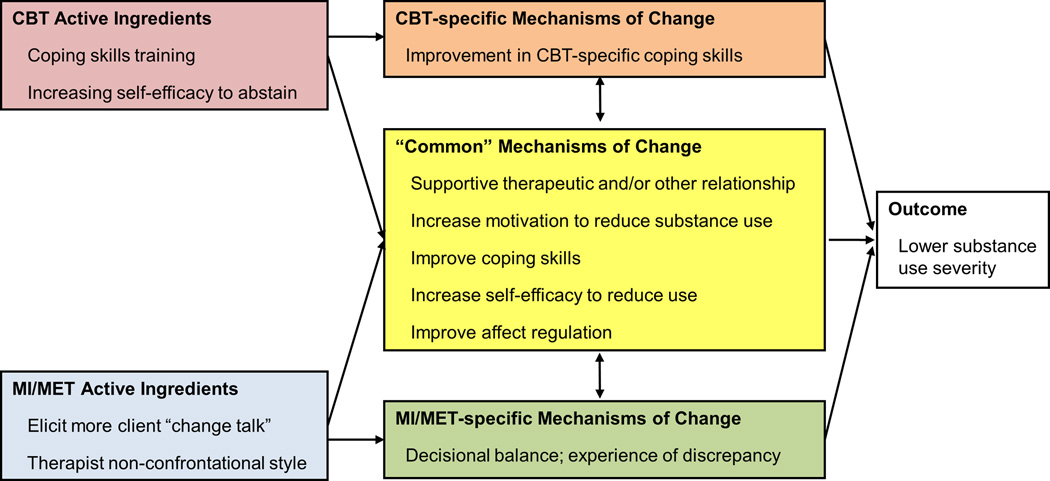
Findings from the adult literature on how substance treatment works may serve as a guide for future adolescent MOC research, as the extant adolescent work is limited. Overall, studies examining MOC for CBT and MI/MET in adult substance users generally have not shown that treatments work through the theorized treatment-specific mechanisms29, 31. For example, interventions such as MET and 12-step facilitation, which do not focus on teaching coping skills, tend to be just as effective as CBT in increasing substance-specific and general coping skills, as well as increasing self-efficacy to reduce use52, 53. Thus, some researchers have concluded that existing treatments, despite different theoretical foundations and prescribing distinct techniques, may not be sufficiently different in terms of MOC50. Specifically, distinct therapies might operate through “common” MOC, such as positive therapeutic alliance and social support (see Figure 1). Alternatively, greater elaboration of causal chains, focusing on therapy-specific micro-processes, may reveal subtle differences in the time course of intervention effects (i.e., rapidity of treatment response) or the pathways through which a particular sequence or combination of therapy-specific active ingredients may have an effect on outcome50,54. Emerging findings suggest that failure to confirm hypothesized treatment-specific causal chains may be due to imprecise definition and/or measurement of key constructs, the need to identify relevant parameters of change (e.g., rapidity and durability of effects), and the need for greater specificity of the causal chains to be tested31, 55.
FIGURE 1.
Proposed relationships between therapy-specific active ingredients, “common” and “therapy-specific” mechanisms of change, and treatment outcome.
Note. CBT=Cognitive Behavioral Therapy, MI/MET=Motivational Interviewing/Motivational Enhancement Intervention.
MOC in Adolescent Substance Use Treatment Research
Few studies have examined MOC in the youth treatment outcome literature22, which often lags behind research conducted with adults. To identify articles that examined MOC in adolescent substance use treatment, PsychINFO, Medline, and Global Health databases were searched using key words such as mediator, indirect effect, substance use (including separate terms for alcohol, cannabis, polysubstance use), treatment, intervention, and adolescent. Further, potentially relevant articles from the reference section of identified studies, and reviews of adolescent substance use treatment were extracted for consideration. Criteria for inclusion in the review were: (1) empirical results from an intervention for youth substance use; (2) participants ages 11–18; (3) test of mediation. Studies involving college students were excluded since they are considered “emerging adults”. The search yielded seven adolescent studies that could be considered as potentially examining mediators of treatment effects (see Table 1). Two studies reported results from the same parent study56, 57. One study did not test mediation due to the lack of a significant relationship between treatment condition and outcomes over follow-up58. Another study, which focused on aftercare (and is thus not reviewed in detail), found that adherence to continuing care and social/environmental risk mediated the association between Assertive Aftercare and substance use outcomes59. Among the remaining four studies, two studies involved youth in community-based treatment60, 61, and two studies were randomized trials56, 57, 62.
TABLE 1.
Adolescent Substance Use Treatment Studies That Proposed Tests Of Mediation
| Study | N | Treatment | Mean Age | % Male | Mediators Testeda | Follow-up length | Results/comments |
|---|---|---|---|---|---|---|---|
| Chi et al. 200960 | 117 | 12-step affiliation | 16.1 | 66 | Social Support, Religious Service Attendance | 6-months | Mediator and outcome both measured at 6-mo. |
| Garner et al. 200759 | 183 | Assertive Aftercare | 16.2 | 71 | Adherence to Continuing Care, Social/ Environmental Risk | 3- and 6-months | Tested an aftercare protocol |
| Henderson et al. 200962 | 83 | MDFT vs. Group CBT | 13.7 | 74 | Parental Monitoring | 3- and 6-months | |
| Kelly et al. 200061 | 99 | 12-Step affiliation | 16 | 40 | Motivation for Abstinence, Coping, Self-Efficacy to abstain | 3- and 6-months | |
| Stanger et al. 200958 | 69 | CM + Parent Training vs. CM + Parent Psychoeducation | 16 | 83 | Not able to test mediation | Treatment type not associated with outcome | |
| Winters et al. 201256 | 315 | BI with Teen Only; BI with Parent Session; Assessment Only | 16.3 | 52 | Motivation to Change; Parenting Practices; Problem Solving Skills; Other service utilization | 6-weeks | Mediator and outcome both measured at same time |
| Winters et al. in press57 | 284 | BI with Teen Only; BI with Parent Session; Assessment Only | 16.1 | 50 | Motivation to Change; Parenting Practices; Problem Solving Skills; Other service utilization | 1-year | Same sample as Winters et al., 2012 |
Note. a: Bold indicates significant mediator. BI=Brief Intervention, MDFT=Multidimensional Family Therapy, CBT=Cognitive Behavioral Therapy, CM=Contingency Management.
In the two community-based treatment studies60, 61 both examined 12-step affiliation as the “intervention” of interest but tested different mediators. Social support was found to mediate the association between 12-step affiliation and abstinence from substance use at 3-year follow-up60. The strength of evidence for mediation in the study, however, is limited because certain variables were assessed at the same time, making temporal ordering of the variables indeterminate. In the other study, only motivation for abstinence was identified as a mediator of 12-step attendance (during the first 3-months post-treatment) and number of abstinent days at 4-to-6-months post-treatment, although coping and self-efficacy also were tested as mediators61. In addition to testing different mediators, the two studies differed in treatment setting, timing of assessments, and length of follow-up, which limits comparability of results across these two studies.
The two adolescent clinical trials that tested mediation examined different types of treatment. One clinical trial, which compared MDFT and group-based CBT among youth with behavioral and substance-related problems (N=83), found that youth report of improved parenting practices from pre- to post-treatment marginally mediated the relationship between treatment condition (MDFT>CBT) and abstinence at 12-month follow-up62. The other clinical trial (i.e., two reports from the same project) compared Brief Intervention with the adolescent (BI-A) against Brief Intervention with the adolescent combined with a parent session (BI-AP) among school-referred substance-using youth (N=315)56, 57. Analysis of 6-month outcomes indicated that problem solving and use of additional community services mediated the association between both interventions (BI-AP>BI-A) and substance use outcomes56. A limitation of the 6-month mediation analyses in that study is that the mediator and outcome were both assessed at 6-months. At 12-month follow-up, motivation to change assessed at 6-months mediated BI-A and BI-AP effects on outcome, and use of additional services and parenting practices (both assessed at 6-months) mediated the association between BI-AP and 12-month outcomes57. Although these two clinical trials examined different interventions (i.e., MDFT, BI-A/BI-AP), both found some support for parenting practices as a mediator of treatment effects based on 12-month outcomes. The convergence on improved parenting behavior as a mechanism of change points to the potential importance of “common” mechanisms, although further research is needed to confirm and elaborate these effects.
In sum, the adolescent substance abuse treatment mechanism studies reviewed differed in treatment setting, type of intervention, mediators examined, and length of follow-up. Mediators of the association between community-based treatment and outcome differed in two studies, but suggest possible roles of motivation to abstain and social support in the pathway to better outcome. Improvement in parenting behaviors was supported as a mediator in two studies57, 62, which used different interventions involving parents, suggesting the operation of “common” rather than “treatment-specific” MOC. These preliminary findings suggest that social support, including parent involvement in treatment, is an important “common” mechanism of change in adolescent treatment outcome.
Broader Perspective on MOC: Cross-cutting Behavior Change Processes
In the adult and adolescent substance use treatment literature, there is little evidence that treatment-specific factors are more important than “common” mechanisms of change (e.g., improved coping, improved parenting behaviors, positive social support) in determining outcome. Because therapy-specific active ingredients may work through “common” processes of change, there has been a call for research on “empirically supported treatment processes” instead of “empirically supported treatments”26. General behavioral principles, such as reinforcement and punishment, cut across specific theories of cognitive and behavioral change, and different “brands” of therapy26, 63. The idea of cross-cutting principles of therapeutic change is in line with a recent proposed framework, Research Domain Criteria (RDoC)64, which is an alternative to psychiatric diagnosis. In the RDoC framework, interventions would not target specific “disorders,” but would target more narrowly defined domains of functioning, such as improving affect regulation through empirically-supported treatment processes65.
In the absence of evidence to support treatment-specific mechanisms of change, treatment-specific mechanisms might be operating but may involve therapy-specific “micro-processes,” pathways, or parameters of treatment response (e.g., rapidity, durability) that have not yet received much attention. The study of therapy-specific mechanisms of change seems to require greater elaboration of a treatment-specific causal chain, which would ultimately need to be distinguished from, but also related to, “common” mechanisms of change. The ability to distinguish “therapy-specific” and “common” processes of change may depend on fine-grained analysis of detailed causal chains. Just as various drugs of abuse might activate a “common final pathway” involving the mesolimbic dopamine system66, therapy-specific active ingredients may impact therapy-specific “micro-targets” through pathways that converge on, for example, increased self-efficacy as a “common” mechanism of change.
MOC from a Developmental Neuroscience Perspective
Understanding how psychotherapy works at the level of brain functioning could help to identify mechanisms of behavior change67, 68, as well as client neurocognitive characteristics (e.g., on-going brain development in adolescence) that might affect treatment response7. For example, a neuroscience approach could reveal how newer approaches, such as mindfulness-based interventions69, 70, work at the level of brain functioning to reduce risk for relapse71. Although neuroimaging could provide novel insights into brain-based mechanisms of change72, 73, the approach requires a high degree of precision in definition and measurement of the “active ingredient” and “mechanism” to be tested. In this regard, Feldstein-Ewing and colleagues74 proposed a neurobiological model of mechanisms underlying MI, focusing on brain-based response to “change talk” as the mechanism underlying reductions in substance use. Functional neuroimaging results with adolescent substance users suggested that “change talk” inhibited activation in brain regions that respond to alcohol cues75 or among cannabis users, increased activation in brain areas involved in introspection, which was in turn associated with reductions in cannabis use over 1-month follow-up76. The narrow focus on a single mechanism of change (e.g., change talk) suggests the potential utility of a micro-intervention approach to studying MOC, which can provide greater precision by targeting smaller units of cause and effect77, albeit with a trade-off in external validity.
Recommendations and Future Directions
Research to date has not clearly identified therapy-specific mechanisms of change. However, the lack of empirical evidence might be due to limitations involving the need for detailed delineation of micro-processes embedded within causal chains. Specifically, greater precision is needed in defining and measuring proposed therapy-specific “active ingredients,” their respective “targets,” and mechanisms of action at a micro-process level (e.g., within session, session-by-session), in order to reveal treatment-specific pathways of intervention effects 77. Greater attention needs to be given to the interaction between therapy-specific and “common” (e.g., therapeutic alliance) factors in generating treatment outcomes27, as well as factors that operate outside of treatment (e.g., family environment) that influence outcome26. The dynamic nature of the therapist-client relationship also has only begun to be explored in terms of therapist behavior and skill and client responses as predictors of treatment outcome24, 25, 78. Few studies have addressed all of the seven guidelines for identifying MOC22, although newer methods of real-time data collection (e.g., ecological momentary assessment) and statistical analysis (e.g., dynamic systems modeling,79, 80) provide opportunities to better assess and model the dynamic process of change.
In addition, there is movement toward discovering “what will work best for me” rather than “which treatment works best”81. In this regard, differences in client response to treatment suggests the utility of adaptive interventions23. Adaptive interventions may involve clients choosing from a menu of intervention options82, provision of interventions based on a comprehensive assessment of client needs and capacities83 or other types of treatment algorithms based on decision rules that specify when and how to alter interventions provided based on client response84, 85.
CONCLUSIONS
Substance use treatment research has shifted from examining treatment outcome to determining “how” treatment works and “for whom” it may work best. Studies that test MOC, however, are still rare in the adult, and especially adolescent, treatment literature. Further, MOC research has generally not supported the identification of treatment-specific MOC, despite the distinctiveness of the treatments examined. Identification of treatment-specific mechanisms appear to require greater precision in defining and measuring causal chains, possibly using a micro-intervention approach, more fine-grained assessment (e.g., within session, session-by-session), and novel analytic methods (e.g., dynamic systems analysis). Future directions in studying MOC include neuroscience approaches to examining cognitive processes and affect regulation that are associated with relapse and successful recovery and using adaptive treatment designs to better accommodate individual differences in response to treatment.
Acknowledgments
FUNDING
This work was supported by NIAAA T32 AA07453, R01 AA014357, K02 AA018195. The funding agency was not involved in the preparation of this review.
Footnotes
AUTHOR CONTRIBUTIONS
Dr. Chung and Black contributed to the conception and design, analysis and interpretation, and writing and revision of the manuscript. Dr. Black performed the majority of the literature search.
REFERENCES
- 1.SAMHSA. Substance Abuse and Mental Health Services Administration, Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 2.PIRE. Underage drinking costs. [Accessed Nov 27, 2013];2013 http://www.udetc.org/UnderageDrinkingCosts.asp. [Google Scholar]
- 3.Miller WR, Wilbourne PL. Mesa Grande: a methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction. 2002;97:265–277. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- 4.Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. J Clin Child Adolesc. 2008;37:238–261. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- 5.Jensen CD, Cushing CC, Aylward BS, Craig JT, Sorell DM, Steele RG. Effectiveness of motivational interviewing interventions for adolescent substance use behavior change: a meta-analytic review. J Consult Clin Psychol. 2011;79:433–440. doi: 10.1037/a0023992. [DOI] [PubMed] [Google Scholar]
- 6.Deas D, Thomas SE. An overview of controlled studies of adolescent substance abuse treatment. Am J Addiction. 2001;10:178–189. doi: 10.1080/105504901750227822. [DOI] [PubMed] [Google Scholar]
- 7.Wetherill R, Tapert SF. Adolescent brain development, substance use, and psychotherapeutic change. Psychol Addict Behav. 2012 Jun 27;Vol 27:393–402. doi: 10.1037/a0029111. ed2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marlatt A, Gordon J. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. New York, NY: Guilford Press; 1985. [Google Scholar]
- 9.Becker SJ, Curry JF. Outpatient interventions for adolescent substance abuse: a quality of evidence review. J Consult Clin Psychol. 2008;76:531–543. doi: 10.1037/0022-006X.76.4.531. [DOI] [PubMed] [Google Scholar]
- 10.Williams R, Chang S. A Comprehensive and Comparative Review of Adolescent Substance Abuse Treatment Outcome. Clin Psychol-Sci Pr. 2000;7:138–166. [Google Scholar]
- 11.Magill M, Ray LA. Cognitive-behavioral treatment with adult alcohol and illicit drug users: a meta-analysis of randomized controlled trials. J Stud Alcohol Drugs. 2009;70:516–527. doi: 10.15288/jsad.2009.70.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller WR, Walters ST, Bennett ME. How effective is alcoholism treatment in the United States? J Stud Alcohol Drugs. 2001;62:211–220. doi: 10.15288/jsa.2001.62.211. [DOI] [PubMed] [Google Scholar]
- 13.Chung T, Maisto SA. Relapse to alcohol and other drug use in treated adolescents: review and reconsideration of relapse as a change point in clinical course. Clin Psychol Rev. 2006;26:149–161. doi: 10.1016/j.cpr.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Chung T, Maisto SA, Cornelius JR, Martin CS, Jackson KM. Joint trajectory analysis of treated adolescents' alcohol use and symptoms over 1 year. Addict Behav. 2005;30:1690–1701. doi: 10.1016/j.addbeh.2005.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chung T, Martin CS, Clark DB. Concurrent change in alcohol and drug problems among treated adolescents over three years. J Stud Alcohol Drugs. 2008;69:420–429. doi: 10.15288/jsad.2008.69.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anderson KG, Ramo DE, Cummins KM, Brown SA. Alcohol and drug involvement after adolescent treatment and functioning during emerging adulthood. Drug Alcohol Depend. 2010;107:171–181. doi: 10.1016/j.drugalcdep.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dennis M, Titus JC, Diamond G, et al. The Cannabis Youth Treatment (CYT) experiment: rationale, study design and analysis plans. Addiction. 2002;97(Suppl 1):16–34. doi: 10.1046/j.1360-0443.97.s01.2.x. [DOI] [PubMed] [Google Scholar]
- 18.Dennis M, Godley SH, Diamond G, et al. The Cannabis Youth Treatment (CYT) Study: main findings from two randomized trials. J Subst Abuse Treat. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 19.Imel ZE, Wampold BE, Miller SD, Fleming RR. Distinctions without a difference: direct comparisons of psychotherapies for alcohol use disorders. Psychol Addict Behav. 2008;22:533–543. doi: 10.1037/a0013171. [DOI] [PubMed] [Google Scholar]
- 20.Wampold BE. The great psychotherapy debate: Models, methods, and findings. Hillsdale, NJ: Erlbaum; 2001. [Google Scholar]
- 21.Huebner RB, Tonigan JS. The search for mechanisms of behavior change in evidencebased behavioral treatments for alcohol use disorders: overview. Alcohol Clin Exp Res. 2007;31:1s–3s. doi: 10.1111/j.1530-0277.2007.00487.x. [DOI] [PubMed] [Google Scholar]
- 22.Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. J Child Psychol Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- 23.Murphy SA, Lynch KG, Oslin D, McKay JR, TenHave T. Developing adaptive treatment strategies in substance abuse research. Drug Alcohol Depend. 2007;88(Suppl 2):S24–S30. doi: 10.1016/j.drugalcdep.2006.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moyers TB, Martin T, Christopher PJ, Houck JM, Tonigan JS, Amrhein PC. Client language as a mediator of motivational interviewing efficacy: where is the evidence? Alcohol Clin Exp Res. 2007;31:40s–47s. doi: 10.1111/j.1530-0277.2007.00492.x. [DOI] [PubMed] [Google Scholar]
- 25.Castonquay LG, Beutler LE. Common and unique principles of therapeutic change. In: Castonquay LG, Beutler LE, editors. Principles of therapeutic change that work. New York: Oxford; 2006. pp. 353–369. [Google Scholar]
- 26.Moos RH. Theory-based active ingredients of effective treatments for substance use disorders. Drug Alcohol Depend. 2007;88:109–121. doi: 10.1016/j.drugalcdep.2006.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morgenstern J, McKay JR. Rethinking the paradigms that inform behavioral treatment research for substance use disorders. Addiction. 2007;102:1377–1389. doi: 10.1111/j.1360-0443.2007.01882.x. [DOI] [PubMed] [Google Scholar]
- 28.Longabaugh R, Wirtz PW, editors. Project MATCH Hypotheses: Results and causal chain analyses. Bethesda, MD: National Institute on Alcohol Abuse and Aloholism; 2001. Project MATCH Monograph series; No. 8. [Google Scholar]
- 29.Morgenstern J. Perspectives and future directions. Alcohol Clin Exp Res. 2007;31:87s–90s. doi: 10.1111/j.1530-0277.2007.00502.x. [DOI] [PubMed] [Google Scholar]
- 30.Bandura A. Social foundations of thought and action. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 31.Morgenstern J, Longabaugh R. Cognitive-behavioral treatment for alcohol dependence: a review of evidence for its hypothesized mechanisms of action. Addiction. 2000;95:1475–1490. doi: 10.1046/j.1360-0443.2000.951014753.x. [DOI] [PubMed] [Google Scholar]
- 32.Kadden RM, Carroll KM, Donovan D, et al., editors. Cognitive-Behavioral Coping Skills Therapy Manual. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- 33.Morgenstern J, Naqvi NH, Debellis R, Breiter HC. The contributions of cognitive neuroscience and neuroimaging to understanding mechanisms of behavior change in addiction. Psychol Addict Behav. 2013;27:336–350. doi: 10.1037/a0032435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York: Guilford Press; 2002. [Google Scholar]
- 35.Janis IL, Mann L. Decision making: a psychological analysis of conflict, choice, and commitment. New York, NY: Free Press; 1977. [Google Scholar]
- 36.Orford J. Excessive appetites: A psychological view of addiction. 1st ed. Chichester, England: Wiley Press; 1985. [Google Scholar]
- 37.Amrhein PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. J Consult Clin Psychol. 2003;71:862–878. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- 38.Apodaca TR, Longabaugh R. Mechanisms of change in motivational interviewing: a review and preliminary evaluation of the evidence. Addiction. 2009;104:705–715. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hayes A, Hope DA, Hayes S. Towards an Understanding of the Process and Mechanisms of Change in Cognitive Behavioral Therapy: Linking Innovative Methodology with Fundamental Questions. Clin Psychol Rev. 2007;27:679–681. doi: 10.1016/j.cpr.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barber JP, Connolly MB, Crits-Christoph P, Gladis L, Siqueland L. Alliance predicts patients' outcome beyond in-treatment change in symptoms. J Consult Clin Psychol. 2000;68:1027–1032. doi: 10.1037//0022-006x.68.6.1027. [DOI] [PubMed] [Google Scholar]
- 41.Karno MP, Longabaugh R. Less directiveness by therapists improves drinking outcomes of reactant clients in alcoholism treatment. J Consult Clin Psychol. 2005;73:262–267. doi: 10.1037/0022-006X.73.2.262. [DOI] [PubMed] [Google Scholar]
- 42.Holt LJ, Litt MD, Cooney NL. Prospective analysis of early lapse to drinking and smoking among individuals in concurrent alcohol and tobacco treatment. Psychol Addict Behav. 2012;26:561–572. doi: 10.1037/a0026039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Renzelli C, Maisto SA, Sealy L, Chung T. Tracking adolescents’ session-to-session change in motivation to abstain from alcohol and marijuana in community-based treatment. Paper presented at: Research Society on Alcoholism; San Franciso, CA. 2012. [Google Scholar]
- 44.Hayes AM, Laurenceau JP, Feldman G, Strauss JL, Cardaciotto L. Change is not always linear: the study of nonlinear and discontinuous patterns of change in psychotherapy. Clin Psychol Rev. 2007;27:715–723. doi: 10.1016/j.cpr.2007.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Witkiewitz K, van der Maas HL, Hufford MR, Marlatt GA. Nonnormality and divergence in posttreatment alcohol use: reexamining the Project MATCH data "another way". J Abnorm Psychol. 2007;116:378–394. doi: 10.1037/0021-843X.116.2.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Clifford PR, Maisto SA. Subject reactivity effects and alcohol treatment outcome research. J Stud Alcohol Drugs. 2000;61:787–793. doi: 10.15288/jsa.2000.61.787. [DOI] [PubMed] [Google Scholar]
- 47.Kazdin AE. Understanding how and why psychotherapy leads to change. Psychother Res. 2009;19:418–428. doi: 10.1080/10503300802448899. [DOI] [PubMed] [Google Scholar]
- 48.MacKinnon D. Introduction to statistical mediation analysis. New York, NY: Lawrence Erlbaum; 2008. [Google Scholar]
- 49.Preacher KJ. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Press; 2013. [Google Scholar]
- 50.Longabaugh R, Magill M. Recent advances in behavioral addiction treatments: focusing on mechanisms of change. Curr Psychiatry Rep. 2011;13:382–389. doi: 10.1007/s11920-011-0220-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psychol. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- 52.Litt MD, Kadden RM, Cooney NL, Kabela E. Coping skills and treatment outcomes in cognitive-behavioral and interactional group therapy for alcoholism. J Consult Clin Psychol. 2003;71:118–128. doi: 10.1037//0022-006x.71.1.118. [DOI] [PubMed] [Google Scholar]
- 53.Litt MD, Kadden RM, Stephens RS. Coping and self-efficacy in marijuana treatment: results from the marijuana treatment project. J Consult Clin Psychol. 2005;73:1015–1025. doi: 10.1037/0022-006X.73.6.1015. [DOI] [PubMed] [Google Scholar]
- 54.Morgenstern J, Kuerbis A, Amrhein P, Hail L, Lynch K, McKay JR. Motivational interviewing: a pilot test of active ingredients and mechanisms of change. Psychol Addict Behav. 2012;26:859–869. doi: 10.1037/a0029674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bertholet N, Palfai T, Gaume J, Daeppen J-B, Saitz R. Do brief alcohol motivational interventions work like we think they do? Alcohol Clin Exp Res. doi: 10.1111/acer.12274. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Winters KC, Fahnhorst T, Botzet A, Lee S, Lalone B. Brief intervention for drug-abusing adolescents in a school setting: outcomes and mediating factors. J Subst Abuse Treat. 2012;42:279–288. doi: 10.1016/j.jsat.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Winters KC, Lee S, Botzet A, Fahnhorst T, Nicholson A . One-year outcomes and mediators of a brief intervention for drug abusing adolescents. Psychology of Addictive Behaviors. doi: 10.1037/a0035041. in-press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stanger C, Budney AJ, Kamon JL, Thostensen J. A randomized trial of contingency management for adolescent marijuana abuse and dependence. Drug and Alcohol Dependence. 2009;105:240–247. doi: 10.1016/j.drugalcdep.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Garner BR, Godley MD, Funk RR, Dennis ML, Godley SH. The impact of continuing care adherence on environmental risks, substance use, and substance-related problems following adolescent residential treatment. Psychol Addict Behav. 2007;21:488–497. doi: 10.1037/0893-164X.21.4.488. [DOI] [PubMed] [Google Scholar]
- 60.Chi FW, Kaskutas LA, Sterling S, Campbell CI, Weisner C. Twelve-Step affiliation and 3-year substance use outcomes among adolescents: social support and religious service attendance as potential mediators. Addiction. 2009;104:927–939. doi: 10.1111/j.1360-0443.2009.02524.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kelly JF, Myers MG, Brown SA. A multivariate process model of adolescent 12-step attendance and substance use outcome following inpatient treatment. Psychol Addict Behav. 2000;14:376–389. [PMC free article] [PubMed] [Google Scholar]
- 62.Henderson CE, Rowe CL, Dakof GA, Hawes SW, Liddle HA. Parenting Practices as Mediators of Treatment Effects in an Early-Intervention Trial of Multidimensional Family Therapy. Am J Drug Alcohol Ab. 2009;35:220–226. doi: 10.1080/00952990903005890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Webb TL, Sniehotta FF, Michie S. Using theories of behaviour change to inform interventions for addictive behaviours. Addiction. 2010;105:1879–1892. doi: 10.1111/j.1360-0443.2010.03028.x. [DOI] [PubMed] [Google Scholar]
- 64.Insel T, Cuthbert B, Garvey M, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiat. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 65.Barlow DH, Farchione TJ, Fairholme CP, et al. Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: Therapist Guide. New York, NY: Oxford University Press; 2011. [Google Scholar]
- 66.Baler RD, Volkow ND. Drug addiction: the neurobiology of disrupted self-control. Trends Mol Med. 2006;12:559–566. doi: 10.1016/j.molmed.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 67.Feldstein Ewing SW, Chung T. Neuroimaging Mechanisms of Change in Psychotherapy for Addictive Behaviors: Emerging Translational Approaches That Bridge Biology and Behavior. Psychol Addict Behav. 2013;27:329–335. doi: 10.1037/a0031491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Potenza MN, Sofuoglu M, Carroll KM, Rounsaville BJ. Neuroscience of behavioral and pharmacological treatments for addictions. Neuron. 2011;69:695–712. doi: 10.1016/j.neuron.2011.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Witkiewitz K, Lustyk MK, Bowen S. Retraining the addicted brain: a review of hypothesized neurobiological mechanisms of mindfulness-based relapse prevention. Psychol Addict Behav. 2013;27:351–365. doi: 10.1037/a0029258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Brewer JA, Elwafi HM, Davis JH. Craving to quit: psychological models and neurobiological mechanisms of mindfulness training as treatment for addictions. Psychol Addict Behav. 2013;27:366–379. doi: 10.1037/a0028490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Holzel BK, Lazar S, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspect Psychol Sci. 2011;6:537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- 72.DeVito EE, Worhunsky PD, Carroll KM, Rounsaville BJ, Kober H, Potenza MN. A preliminary study of the neural effects of behavioral therapy for substance use disorders. Drug Alcohol Depend. 2012;122:228–235. doi: 10.1016/j.drugalcdep.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kober H, Kross EF, Mischel W, Hart CL, Ochsner KN. Regulation of craving by cognitive strategies in cigarette smokers. Drug Alcohol Depend. 2010;106:52–55. doi: 10.1016/j.drugalcdep.2009.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Feldstein Ewing SW, Filbey FM, Hendershot CS, McEachern AD, Hutchison KE. Proposed model of the neurobiological mechanisms underlying psychosocial alcohol interventions: the example of motivational interviewing. J Stud Alcohol Drugs. 2011;72:903–916. doi: 10.15288/jsad.2011.72.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Feldstein Ewing SW, Filbey FM, Sabbineni A, Chandler LD, Hutchison KE. How psychosocial alcohol interventions work: a preliminary look at what FMRI can tell us. Alcohol Clin Exp Res. 2011;35:643–651. doi: 10.1111/j.1530-0277.2010.01382.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Feldstein Ewing SW, McEachern AD, Yezhuvath U, Bryan AD, Hutchison KE, Filbey FM. Integrating brain and behavior: evaluating adolescents' response to a cannabis intervention. Psychol Addict Behav. 2013;27:510–525. doi: 10.1037/a0029767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Strauman TJ, Goetz EL, Detloff AM, Macduffie KE, Zaunmuller L, Lutz W. Self- Regulation and Mechanisms of Action in Psychotherapy: A Theory-Based Translational Perspective. J Pers. 2012;81:542–553. doi: 10.1111/jopy.12012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Moyers TB, Miller WR, Hendrickson SM. How does motivational interviewing work? Therapist interpersonal skill predicts client involvement within motivational interviewing sessions. J Consult Clin Psychol. 2005;73:590–598. doi: 10.1037/0022-006X.73.4.590. [DOI] [PubMed] [Google Scholar]
- 79.Pachankis JE, Goldfried MR. On the next generation of process research. Clin Psychol Rev. 2007;27:760–768. doi: 10.1016/j.cpr.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 80.Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med. 2011;1:53–71. doi: 10.1007/s13142-011-0021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Witkiewitz K, Marlatt A. Behavioral therapy across the spectrum. Alcohol Res Health. 2011;33:313–319. [PMC free article] [PubMed] [Google Scholar]
- 82.Longabaugh R, Zweben A, Locastro JS, Miller WR. Origins, issues and options in the development of the combined behavioral intervention. J Stud Alcohol. 2005:179–187. doi: 10.15288/jsas.2005.s15.179. discussion 168-179. [DOI] [PubMed] [Google Scholar]
- 83.Gulliver SB, Longabaugh R, Davidson D, Swift R. The development of a broad spectrum treatment for patients with alcohol dependence in early recovery. Cogn Behav Pract. 2005;12:53–63. [Google Scholar]
- 84.Lei H, Nahum-Shani I, Lynch K, Oslin D, Murphy SA. A "SMART" design for building individualized treatment sequences. Annu Rev Clin Psychol. 2012;8:21–48. doi: 10.1146/annurev-clinpsy-032511-143152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lagoa C, Bekiroglu K, Lanza S, Murphy S. Designing adaptive interventions using methods from engineering. J Consult Clin Psychol. doi: 10.1037/a0037736. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]