Abstract
In 2011, the FIGO classification system (PALM-COEIN) was published to standardize terminology, diagnostic and investigations of causes of abnormal uterine bleeding (AUB). According to FIGO new classification, in the absence of structural etiology, the formerly called “dysfunctional uterine bleeding” should be avoided and clinicians should state if AUB are caused by coagulation disorders (AUB-C), ovulation disorder (AUB-O), or endometrial primary dysfunction (AUB-E). Since this publication, some societies have released or revised their guidelines for the diagnosis and the management of the formerly called “dysfunctional uterine bleeding” according new FIGO classification. In this review, we summarize the most relevant new guidelines for the diagnosis and the management of AUB-C, AUB-O, and AUB-E.
Keywords: Abnormal uterine bleeding, Dysovulation, Menorrhagia
Abnormal uterine bleeding (AUB) has negative impact on women’s health and well-being inducing anemia, impacting their quality of life by impairing sexuality, and leads to absenteeism and social embarrassment. Non-structural abnormal uterine bleeding, or the formerly called dysfunctional menometrorrhagia, is a frequent cause of AUB.
Until recently, there was confusion in clinical management and in the interpretations of clinical trials due to a great heterogeneity in terminology and definitions of AUB and their etiologies.
In 2011, the FIGO classification system (PALM-COEIN) for causes of AUB in non-gravid women of reproductive age was published in order to standardize terminology, diagnostic and investigations [1]. AUB was defined as “bleeding from the uterine corpus that is abnormal in volume, regularity, and/or timing, and has been present for the majority of the past 6 months.”
The classification system based on AUB etiologies includes nine categories, organized under the acronym “PALM-COEIN”. PALM group includes five entities with structural etiologies of AUB that can be diagnosed with imaging techniques and/or histopathology (polyp; adenomyosis; leiomyoma; malignancy, and hyperplasia). COEIN group includes non-structural entities that are not diagnosed by imaging or histopathology: coagulopathy; ovulatory dysfunction; endometrial; iatrogenic; and not yet classified.
The term “dysfunctional uterine bleeding” (in opposition to organic uterine bleeding), which was previously used when there was no structural cause for AUB, has been discarded. Women who fit this description should, actually, be distinguished according to FIGO classification, in one or in a combination of the following three etiologies: coagulopathy (AUB-C), disorder of ovulation (AUB-O), or primary endometrial disorder (AUB-E) [1].
Different societies have subsequently published new guidelines for the diagnostic and the management of the formerly called dysfunctional uterine bleeding after reviewing the literature data according to the new FIGO classification.
Materials and Methods
To review the implications of the new FIGO PALM-COEIN on the diagnosis and the management of dysfunctional uterine bleeding, we searched for all guidelines and recommendations of scientific societies which have interested AUB and matched the following inclusion criteria:
Released after the publication of the new terminology recommended by FIGO [1].
Concerning the diagnosis and management of formerly called dysfunctional AUB.
In which authors adopted, for their analysis and conclusions the new terminology recommended by FIGO [1].
For this purpose, we performed a research of reviews on “Pubmed” limited to publications after 2011 using the following terms “Abnormal uterine bleeding” and “guidelines” or and «recommendations” or and “Practice Bulletin.”
We obtained 50 results corresponding to these terms. After reviewing abstracts and applying inclusion criteria, we included:
-
(i)
Two practice bulletins of the American College of Obstetricians and Gynecologists (ACOG): one about “the diagnosis of AUB [2] and the second about “the management of AUB related to dysovulation” [3].
-
(ii)
A clinical practice guideline of the Society of Obstetricians and Gynecologists of Canada (SOGC) “Abnormal Uterine Bleeding in Pre-Menopausal Women” [4].
-
(iii)
A review and recommendations of the Gynecologic Surgeons Systematic Review Group about “Nonsurgical Management of Heavy Menstrual Bleeding” [5].
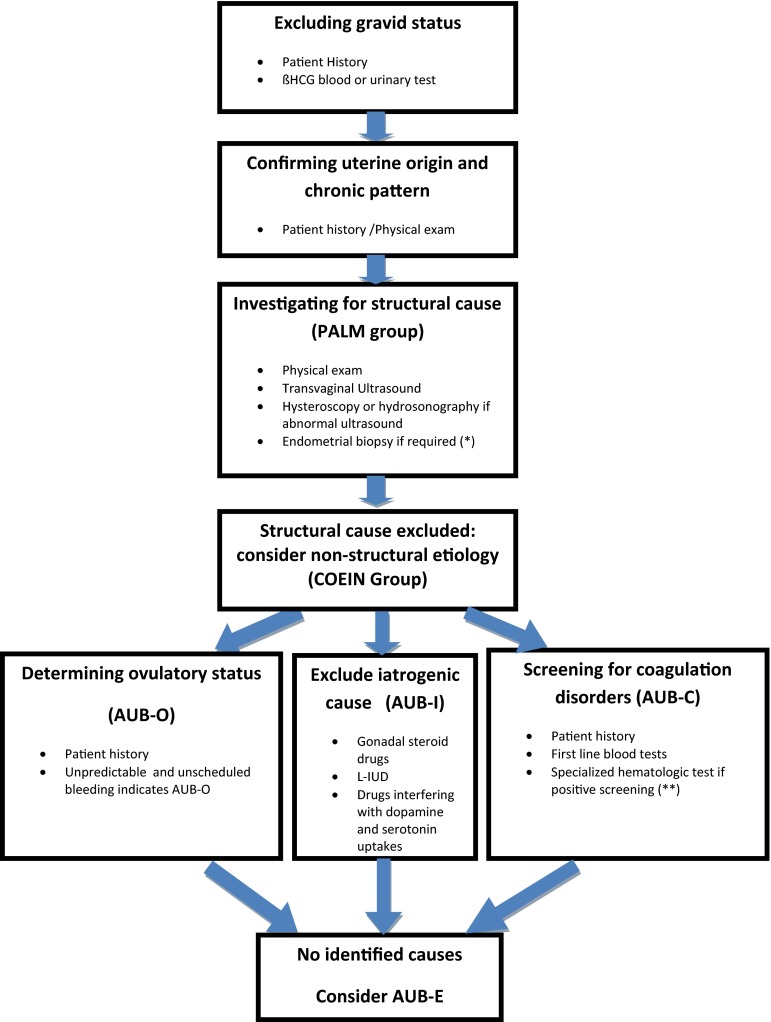
Diagnosis and Investigation Strategy (Figs. 1, 2)
Fig. 1.
A summary of a global strategy for the diagnosis of causes of non-structural abnormal uterine bleeding. L-IUD levonorgestrel Intrauterine device; AUB-C abnormal uterine bleeding related to Coagulopathy; AUB-O abnormal uterine bleeding related to Ovulatory dysfunction; AUB-E abnormal uterine bleeding related to Endometrial dysfunction; AUB-I abnormal uterine bleeding related to iatrogenic causes. (*) Patients over 45 years (40 years for Canadian society), and those at higher risk of endometrial cancer: Nulliparous, high BMI > 30 kg/m2, PCOS, diabetic, history of family cases of hereditary non-polyposis colorectal cancer syndrome and when treatment failed to stop AUB. (**) Refer to Diagnosis and investigation strategy section AUB-C
Fig. 2.
Summary of first-line laboratory exams for the diagnosis of abnormal uterine bleeding
Before starting investigations, clinicians should, first, exclude a gravid context by patient history and urine/serum assay for the presence of the β-subunit of human chorionic gonadotropin [1, 4].
The uterine origin of bleeding but also the chronic feature should also been confirmed by physical exam. Indeed, AUB has been defined by FIGO as “bleeding from the uterine corpus that is abnormal in volume, regularity, and/or timing, and has been present for the majority of the past 6 months”. Therefore, the clinical evaluation should not “in the opinion of the clinician, require immediate intervention” [1].
The second step is to exclude a structural (or organic) etiology (belonging to the PALM group of PALM-COEIN classification). Organic causes may include Polyps, Adenomyosis, Leiomyoma, and malignancy (or pre-malignancy conditions such as hyperplasia). For this purpose, uterine assessment should be performed using a transvaginal ultrasound. In case of intrauterine abnormalities, further exams such as hysteroscopy or saline hydrosonography should be performed [1]. An office endometrial biopsy should be planned for patients over 45 years (40 years for Canadian society), and those at higher risk of endometrial cancer: Nulliparous, high BMI > 30 kg/m2, PCOS, diabetic, history of family cases of hereditary non-polyposis colorectal cancer syndrome and when treatment failed to stop AUB [1, 2, 4].
After all these steps have been completed, the dysfunctional origin of AUB is suspected, and clinicians have to classify patients of this group in one or a combination of the following etiologies: coagulopathy (AUB-C), primary endometrial disorder (AUB-E), or disorder of ovulation (AUB-O).
The COEIN group includes two other entities: AUB-I which encompasses iatrogenic causes of bleeding, generally due to intrauterine contraceptive device, sex steroid hormones, or drugs interfering with dopamine or serotonin metabolism [1] and AUB-N referring to all entities that have not been yet identified as a confirmed cause of AUB. Both AUB-I and AUB-N are not itself dysfunctional disorders, so they will not be included in this review.
AUB-C and AUB-O can, in most cases, be suspected by patient history. AUB-C has to be confirmed by hematologic tests if screening is positive (Fig. 1). AUB-E is an exclusion diagnosis when no other causes are identified [1].
Abnormal uterine bleeding related to coagulopathy (AUB-C) includes a spectrum of systemic disorders of hemostasis. In a study we conducted in collaboration with the hematology department, we showed that 33 % of women had inherited bleeding disorder reports, AUB [6]. Inversely, it is estimated that 13 % of women with AUB are diagnosed with Von Willebrand disease [7] which is one of the most common disorders [6]. Specialized tests (Willebrand factor, ristocetin cofactor) should be reserved for patients who are positive to screening for hemostatic disorders. The screening is based on patient history. It is considered positive if it comprises any of the following: heavy menstrual bleeding since menarche, postpartum hemorrhage, surgery-related bleeding, bleeding associated with dental work; or two or more of the following symptoms: bruising one to two times per month, epistaxis one to two times per month, frequent gum bleeding, and Family history of bleeding symptoms [1, 8]. The FIGO experts stated that hemostasis disorder induced by pharmacologic agent is also classified as AUB-C [1].
Abnormal uterine bleeding due to ovulation disorders (AUB-O) occurs in the absence of ovulation and formation of corpus luteum. In this situation, there is a lack of Progesterone and the unopposed secretion of estrogens leading to a continual endometrial proliferation without progesterone-withdrawal-induced shedding. The endometrium is fragile, vascular, and lacking sufficient stromal support. The clinical manifestation is an unpredictable bleeding which may result in heavy menstrual bleeding or acute episode of hemorrhage [3]. Therefore, when bleeding is unpredictable and sometimes interspersed with episodes of amenorrhea, this should be considered as AUB-O [1].
There are different situations causing dysovulation, such as Polycystic Ovarian Syndrome (POS), prolactin and thyroid disorders, or premature ovarian failure. However, dysovulation may also occur physiologically especially during adolescence (due to immaturity of the hypothalamic–hypophysis axis) or during perimenopause when ovulation disorders precede menopause [3]. For etiology investigation of ovulations disorders, the following first-line blood tests are recommended: prolactin, thyroid-stimulating hormone ultrasensitive (TSH-US)m and for some cases, Progesterone during luteal phase.
Abnormal uterine bleeding related to endometrial dysfunction (AUB-E) is considered after exclusion of structural causes, ovulatory or coagulation dysfunctions. Typically, bleeding is predicable indicating cycling normal ovulation, but heavy or prolonged. This disorder may also be caused by an infection or inflammation [1, 2].
In this situation, it is postulated that a primary endometrial dysfunction is causing AUB. The primary disorder may be related to deficiencies in local production of vasoconstrictors (endothelin-1 and prostaglandin F2α), accelerated lysis of endometrial clot (excessive production of plasminogen activator) [9], or increased local production of prostaglandin E2 and prostacyclin (I2) [10]. AUB-E may also be caused by infection or inflammation of endometrium [1].
According to FIGO consensus, there are no tests to perform in this situation. AUB-E remains “determined by exclusion of other identifiable abnormalities in women of reproductive age who seem to have normal ovulatory function” [1].
Management
In case of AUB-C, AUB-O, or AUB-E, medical treatment is the first-line therapy in order to decrease blood loss. It includes hormonal therapy regimes such as oral contraceptive pills (OCP), progestin given during luteal phase or in an extended regimen, Levonorgestrel intra-uterine device (L-IUD), and Gn-RH agonist. There are also non-hormonal medical therapies: NSAIDs and tranexamic acid.
Endometrial ablation and hysterectomy are the two surgical options for AUB.
SOGC recommends considering medical treatment as the first-line therapy once malignancy and significant pelvic pathology have been ruled out, which includes AUB-O, AUB-C, and AUB-E [4].
AUB-C
According to SOCG, women with AUB-C are best managed in a multidisciplinary approach including Gynecologist and Hematologist. In a patient with AUB related to coagulation disorders, the same medical agents used among women with normal coagulation can effectively be administrated with the exception of non-steroidal anti-inflammatory drugs [4]. This may include OCP and L-IUD.
If the first-line medical treatment failed, “specific treatment including desmopressin or factor replacement can be considered” with the assistance of an hematologist [4].
Surgical treatments (hysterectomy or endometrium ablation) are possible, but “should be planned carefully along with a hematologist, for measures to normalize coagulation factors preoperatively, intraoperatively, and postoperatively” [4].
AUB-O
The ACOG stated that as “AUB-O is an endocrinologic abnormality; the underlying disorder should be treated medically rather than surgically” [3].
The SOGC claimed that “Irregular or prolonged bleeding is most effectively treated with hormonal options that regulate cycles, decreasing the likelihood of unscheduled and potentially heavy bleeding episodes” [4]. However, data concerning treatment of patients, women with AUB presumed secondary to ovulatory dysfunction (AUB-O), are limited [5]. There are no randomized trials that evaluated the use of hormonal therapy specifically for the treatment of AUB-O [11]. ACOG is, to our knowledge, the unique society that released specific recommendations for the management of AUB-O [3]. Despite lack of data, ACOG recommends in this situation the use of hormonal therapy: progestin combined with hormonal contraception and Leovonorgestrel Intrauterine device (L-IUD). In girls aged from 13 to 18 years, the ACOG recommends the use of OCP to diminish blood loss and regulate cycles. In 18–39-year-old patients, it recommends one of the following therapies: low-dose combined with hormonal contraceptive therapy, progestin therapy, or levonorgestrel IUD. In women from 40 to menopause: cyclic progestin therapy, low-dose OCP, and the levonorgestrel IUD, according to ACOG, may be prescribed [3].
The underlying cause of dysovulation has to be treated (example: weight loss and insulin sensitizers for PCOS patients, treating thyroid or Prolactin disorders) [3].
In case of AUB-O, the surgical treatment should be reserved for patients with concomitant significant intracavitary lesions and for medical therapy failures, contraindication, or intolerance. Failure of medical management requires further investigation, including imaging or hysteroscopy [9]. As chronic anovulation is associated with increased risk of endometrial cancer compared with women who are treated with medical therapy, the ACOG does not recommend endometrial ablation as the first-line therapy for AUB-O [3].
In conclusion, there are few data concerning AUB-O management. In this situation, ACOG recommends to treat the underlying disorder, when possible and to consider hormonal treatment as the first choice.
AUB-E
In this situation, the SOGC recommends the use of treatments under both hormonal and non-hormonal therapy [4].
In 2013, the Society of Gynecologic Surgeons Systematic Review Group published a review of 22 studies comparing non-surgical therapy for the treatment of AUB presumed due to endometrial dysfunction (AUB-E) [5]. The authors concluded that in regard to reduction of menstrual bleeding, L-IUD (71–95 %reduction), combined OCPs (35–69 % reduction), extended cycle oral progestins (87 % reduction), tranexamic acid (26–54 % reduction), and NSAIDs (10–52 % reduction) were all effective treatments. The L-IUD, combined OCPs, and antifibrinolytics were all superior to luteal-phase progestins. The L-IUD was the best treatment, and it has been shown that it is superior to combined OCPs and NSAIDs. Antifibrinolytics were superior to NSAIDs. The authors have also underlined the lack of data about the impact of such treatment on the quality of life. Once again, according to American and Canadian guidelines, surgical treatments (hysterectomy and endometrial ablation) should be restricted to the failure of medical therapy, inability to utilize medical therapies, significant anemia, impact on quality of life, and concomitant uterine pathology.
In summary, AUB-E can be managed both by hormonal and non-hormonal treatments. L-IUD seems to be the most effective choice.
Regardless of the type of abnormal bleeding, SOGC recommends a patient-centered approach for the selection of a specific medical therapy. The choice of the best therapy has to take into consideration not only patient tolerance to drugs, her desire of fertility or to preserve fertility potential, associated complaints (dysmenorrhea), medical contraindications, but also the cost and the availability of treatments [4].
In conclusion, it is no longer recommended to diagnose non-structural AUB as being dysfunctional. Clinicians have to specify (after excluding AUB-I): whether AUB is related to endometrial dysfunction (AUB-E) or to ovulation disorder (AUB-O). Indeed, management is different according to the situation. In the first one, both hormonal and non-hormonal treatments are effective, and L-IUD seems to be the best choice. If AUB-O is diagnosed, treatment should be based on restoring ovulation (when possible) and on hormonal treatment. Non-hormonal drugs are not recommended in this situation.
Acknowledgments
Compliance with ethical requirements and Conflict of interest
This article does not contain any studies with human or animal subjects. Mohamed Khrouf and Khaled Terras declare that they have no conflict of interest.
Mohamed Khrouf,
after his residency training in obstetrics and gynecology in the Faculty of Medicine of Tunis, Mohamed Khrouf completed 2-years of residency in Paris. He sub-specialized in Reproductive Medicine and obtained diplomas on Assisted Reproductive Technologies and hysteroscopic surgery. In 2010, he returned to Tunis and worked as Assistant Professor in Aziza Othmana IVF Center (Faculté de Médecine de Tunis) teaching Infertility care and management in the Faculty of Medicine of Tunis. His major areas of interest are assisted reproduction, intrauterine adhesions, ovarian hyperstimulation syndrome, and PCOS.
Contributor Information
Mohamed Khrouf, Phone: +216 20 221 445, Email: medkhrouf@yahoo.fr.
Khaled Terras, Phone: +216 70860600, Email: khaledterras@voila.fr.
References
- 1.Munro MG, Critchley HO, Broder MS, et al. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynaecol Obstet. 2011;113(1):3–13. doi: 10.1016/j.ijgo.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 2.Diagnosis of abnormal uterine bleeding in reproductive aged women. Practice Bulletin No. 128. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2012; 120(1):197–206. [DOI] [PubMed]
- 3.Management of abnormal uterine bleeding associated with ovulatory dysfunction. Practice Bulletin No. 136. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2013;122(1):176–85. [DOI] [PubMed]
- 4.Singh S, Best C, Dunn S, et al. Abnormal uterine bleeding in pre-menopausal women. J Obstet Gynaecol Can. 2013;35(5):473–479. doi: 10.1016/S1701-2163(15)30939-7. [DOI] [PubMed] [Google Scholar]
- 5.Matteson KA, Rahn DD, Wheeler TL, 2nd, et al. Nonsurgical management of heavy menstrual bleeding: a systematic review. Obstet Gynecol. 2013;121(3):632–643. doi: 10.1097/AOG.0b013e3182839e0e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fadhlaoui A, Khrouf M, Chelbi A, et al. Quality of life during menstruation in women with an inherited bleeding disorder: report of 31 cases. Tunis Med. 2012;90(12):856–861. [PubMed] [Google Scholar]
- 7.Shankar M, Lee CA, Sabin CA, et al. von Willebrand disease in women with menorrhagia: a systematic review. BJOG. 2004;111(7):734–740. doi: 10.1111/j.1471-0528.2004.00176.x. [DOI] [PubMed] [Google Scholar]
- 8.Kouides PA, Conard J, Peyvandi F, et al. Hemostasis and menstruation: appropriate investigation for underlying disorders of hemostasis in women with excessive menstrual bleeding. Fertil Steril. 2005;84(5):1345–1351. doi: 10.1016/j.fertnstert.2005.05.035. [DOI] [PubMed] [Google Scholar]
- 9.Gleeson NC. Cyclic changes in endometrial tissue plasminogen activator and plasminogen activator inhibitor type 1 in women with normal menstruation and essential menorrhagia. Am J Obstet Gynecol. 1994;171(1):178–183. doi: 10.1016/0002-9378(94)90466-9. [DOI] [PubMed] [Google Scholar]
- 10.Smith SK, Abel MH, Kelly RW, et al. A role for prostacyclin (PGi2) in excessive menstrual bleeding. Lancet. 1981;1(8219):522–524. doi: 10.1016/S0140-6736(81)92862-2. [DOI] [PubMed] [Google Scholar]
- 11.Hickey M, Higham JM, Fraser I, et al. Progestogens with or without oestrogen for irregular uterine bleeding associated with anovulation. Cochrane Database Syst Rev. 2012;9:CD001895. doi: 10.1002/14651858.CD001895.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]