Introduction
Deep aggressive angiomyxoma (DAA) is a rare benign tumor with about 250 cases being reported worldwide. It was first reported as a distinct variant of myxoid neoplasm in female pelvis by Steeper and Rosai in 1983. It is a locally aggressive tumor of unknown histogenesis having high potential for local infiltration into adjacent skeletal muscles and adipose tissue. It is commonly seen in females during reproductive age group with peak incidence in the fourth decade. DAA is most often found in pelvic, perineum, genital, or inguinal region. Its exact etiology is not known, but in some cases, chromosomal aberrations have been reported. Most of these tumors are slow growing, presenting as pelvic masses with or without pressure symptoms on surrounding structures. These lesions are soft unencapsulated tumors with fingerlike projections into surrounding structures. Wide surgical excision is the mainstay of managing these tumors since tumor projections increase chances of recurrence. Immunohistochemical evaluations of these tumors show positivity to estrogen and progesterone receptors. Hence, GnRH therapy may be helpful in difficult cases [1, 2].
Case Report
A 45-year-old female presented with mass per abdomen and pain in abdomen without other significant medical history, since the past 1 month. Ultrasonography (USG) study shows a large solid left ovarian mass measuring 19 × 14 cm with heterogeneous echo texture, extending into abdomen. Intraoperatively mass was adherent to posterior wall of uterus and upper part of vagina. There was minimal ascites. Hence, hysterectomy with bilateral salpingo-oophorectomy was performed along with excision of tumor mass and sent for histopathological study.
Histopathological Study
Grossly excised tumor mass measures 26 × 18 × 11 cm. External surface of tumor is smooth and bosselated with breached capsule at places. Cut surface of tumor has solid and gelatinous appearance with microcysts filled with myxoid material (Fig. 1). Microscopically, tumor is paucicellular, consisting of small, uniform spindle and stellate cells with indistinct cell border. These cells have bland vesicular nuclei. Stroma shows abundant myxoid matrix with variable number of medium and large blood vessels with perivascular hyalinization and vascular hypertrophy (Fig. 2). At capsular breach site, tumor is infiltrated into adjacent skeletal muscle bundles. No necrosis or mitosis was seen in extensively sampled tissue. No significant pathology is noted in the hysterectomy with bilateral salpingo-oophorectomy specimen except submucosal leiomyoma.
Fig. 1.

Tumor cut surface showing solid gelatinous appearance with microcysts
Fig. 2.
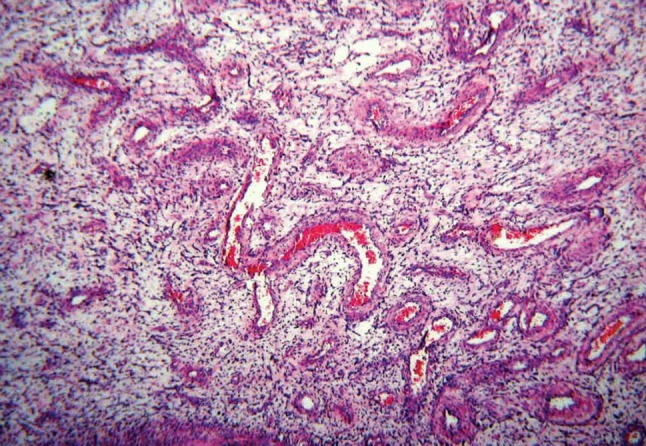
Tumor showing vessels of varying calibers of perivascular hyalinization and vascular hypertrophy. (H&E 10×)
Discussion
Diagnosis of DAA is clinically difficult and often missed as its incidence is low and its presentation mimics a lot of other pelvic and perineal lesions such as lipoma, abscess, vaginal cyst, bartholin cyst, pelvic and perineal soft tissue tumors, perineal hernia, etc. In the present case, based on USG, the clinical diagnosis of ovarian tumor was made. Histological differential diagnosis for DAA ranges from benign myxoid tumors, such as myxolipoma, myxoid neurofibroma, angiomyofibroblastoma, to low grade myxosarcoma. Histological hallmark of DAA is that vessels of varying calibers arranged haphazardly throughout the tumor. This distinctive vascular component helped in the present case to rule out most of the above mentioned tumors [1, 2].
Prognosis in DAA is very good with only two reported cases with metastatic disease followed by death having been reported. Although slow growing, these tumors have a local recurrence rate in the range of 9–72 %. Late recurrence may develop after several years; hence, long-term follow up is important. The major problem posed by this tumor is the need for mutilating surgery to avoid the recurrence, and that the DAA which are located in close proximity to vital organs such as bladder and rectum may cause difficulty in excision or may cause morbidity. Hence, multidisciplinary approach consisting of surgeons, gynecologists, and urologists is always resorted to [2, 3].
Conclusion
Deep aggressive angiomyxoma is a rare locally aggressive neoplasm, which can be mistaken clinically and histologically for several benign and low-grade malignant myxoid tumors. Hence, one should consider this entity for differential diagnosis of asymptomatic pelvic mass. Long-term follow up is necessary due to high rate of local recurrence. Complete margin-free excision is the must to avoid local recurrence.
Acknowledgments
The authors are grateful to the Department of Obstetrics and Gynecology and thankful to the Head, Department of Pathology, BLDEU’s Sri B M Patil Medical College and Hospital, Bijapur for their support and guidance in completion of this article.
References
- 1.Sutton BJ, Laudadio J. Aggressive angiomyxoma. Arch Pathol Lab Med. 2012;136(2):217–221. doi: 10.5858/arpa.2011-0056-RS. [DOI] [PubMed] [Google Scholar]
- 2.Blandamura S, Cruz J, Faure VL, et al. Aggressive angioomyxoma: a second case of metastasis with patients death. Hum Pathol. 2003;34:1072–1074. doi: 10.1053/S0046-8177(03)00419-2. [DOI] [PubMed] [Google Scholar]
- 3.Micci F, Brindal P. Soft tissue tumors: aggressive angiomyxoma. Atlas Genet Cytogenet Oncol Haematol. 2007;11(4):340–343. [Google Scholar]


