Abstract
A careful examination of the multigenerational relationship between immigrant status and mental disorders can provide important information about the robustness and nature of the immigrant-mental health link. We examine immigrant status as a protective factor against mental illness, assess intergenerational effects, examine differences across race/ethnicity, and report the prevalence of mood, anxiety, and personality disorders of immigrants across major world regions. We employ data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) and compare first (n = 5,363) and second-generation (n = 4826) immigrants from Asia, Africa, Europe, and Latin America to native-born Americans (n = 24,461) with respect to mental disorders. First-generation immigrants are significantly less likely than native-born Americans to be diagnosed with a mood, anxiety, or personality disorder, though the prevalence of mental health diagnoses increases among second generation immigrants. Similar results were observed for immigrants from major world regions as the prevalence of psychiatric morbidity was lower among immigrants from Africa, Latin America, Europe, and Asia compared to native-born Americans. Findings provide evidence in support of the notion that the immigrant paradox may be extended to include mood, anxiety, and personality disorders in the United States.
Keywords: immigrant, mental health, immigration, mood disorders, anxiety disorders, personality disorders, immigrant paradox
1. Introduction
In recent years, a growing number of studies have examined the relationship between immigrant status and mental disorders (Shrout et al., 1992; Vega et al., 1998; Grant et al., 2004; Cantor-Graae and Selten, 2005; Breslau et al., 2007; Takeuchi et al., 2007; Alegría et al., 2008; Breslau et al., 2009; Bourque et al., 2011; Cantor-Graae and Petersen, 2013). This body of work points to a multifaceted relationship in which the nature of the association between immigrant status and mental disorders varies according to both the particular characteristics of the immigrant and the nature of the disorder in question. For instance, prior research suggests that immigrants to the United States are a heterogeneous population (Salas-Wright et al., 2014a) and that factors such as immigrant generation (i.e., first-generation, second-generation), age of immigration, and duration as an immigrant in the receiving nation have important implications for the relationship between immigrant status and mental disorders (Vega et al., 1998; Breslau et al., 2007, 2009; Cantor-Graae and Petersen, 2013). Mental health is also a heterogeneous construct and the various types of mental disorders appear to be differentially related to immigrant status in both United States and European samples. Indeed, while meta-analytic reviews have now demonstrated quite convincingly that the prevalence and incidence of psychotic disorders tends to be greater among immigrants than among the native-born (Cantor-Graae and Selten, 2005; Bourque, Van der Ven, and Malla, 2011), research also points to immigrant status as a protective factor for most mood and anxiety disorders (Vega et al., 1998; Grant et al., 2004; Breslau et al., 2007; Takeuchi et al., 2007; Alegría et al., 2008; Breslau et al., 2009; Cantor-Graae and Petersen, 2013).
Despite the manifold advances made by previous studies, several important facets of the immigrant-mental disorder link have yet to be fully explored. To begin, while numerous studies have examined mood and anxiety disorders among particular immigrant groups in the United States (i.e. Hispanics, Asian/Pacific Islanders), few studies have systematically examined the multigenerational relationships between immigrant status and an extensive array of mood, anxiety, and personality disorders among immigrants in general. That is, additional research is needed with respect to the prevalence of particular mood (i.e., bipolar disorder, major depression, dysthymia), anxiety (i.e., generalized anxiety disorder, panic disorder, social phobia, specific phobia, and posttraumatic stress disorder ), and personality (i.e., antisocial, avoidant, borderline, narcissistic, obsessive-compulsive, paranoid, schizoid, schizotypal) disorders among first and second-generation immigrants in contrast with native-born Americans. Second, few studies have examined the stability of the relationship between immigrant status and mental disorders among racial/ethnic minority and non-minority immigrants. In light of research suggesting a link between experiences of discrimination and mental health (Pascoe and Richman, 2009), further research into the potentially segmented nature of the relationship between immigrant status and mental disorders is warranted. In all, while much has been learned in recent years, a careful examination of the multigenerational links between immigrant status and mood, anxiety, and personality disorders can provide important information about the robustness and nature of the immigrant-mental health link.
1.1. Research Context
Each phase in the migration process presents unique migration-related stressors. The pre-flight phase—the period preceding the actual migration event—is especially dire for individuals coerced into undertaking this relocation. Mental illness risk factors experienced in this phase include prolonged civil conflicts and wars (Goodman, 2004), sexual and physical abuse (Crisp, 2000), separation from family (Paardekooper et al., 1999), and prolonged stays in refugee and other transitionary camps (Steel et al., 2006). Individuals who have endured these experiences report mental health and behavioral disorders, including depression, anxiety, psychosis, anger, violence, and posttraumatic stress disorder (Paardekooper et al., 1999; Steel et al., 2002; Fazel et al., 2005; Pumariega et al., 2005; Steel et al., 2006; Liddell et al., 2013; Salas-Wright and Vaughn, 2014). In the resettlement phase, immigrants often have to contend with and acclimatize to a new socio-cultural and economic environment. Factors such as a drop in socio-economic status (Aycan and Berry, 1996; Porter and Haslam, 2005), changing family and gender roles and expectations (Potocky-Tripodi, 2002), cultural dissonance, and cultural bereavement (Choi et al., 2008) are cited as post-migration mental illness triggers.
In addition to migration-related stressors, immigrant populations face barriers to mental health services both before and after relocation. Inadequately structured and financed mental health systems across many developing economies means that a significant number of individuals migrating from these regions have had limited contact with mental health professionals (World Health Organization, 2009). They are less likely to have had access to preventive or curative mental health services and are more likely to experience undiagnosed mental disorders, and have minimal knowledge regarding the primacy of mental health in overall health and well-being (Derose et al., 2009). After migration, low rates of health insurance access (Derose et al., 2009), and other socio-cultural impediments including stigma (Nadeem et al., 2007), linguistic challenges (Sentell et al., 2007; Kim et al., 2011), and lack of ethnically-matched providers (Sue et al., 1991) account for obstacles faced in mental health services utilization.
It is therefore of interest to note that, despite the manifold mental illness triggers associated with immigration, a number of studies have found that immigrant populations tend to report lower rates of most mood and anxiety disorders as compared to their native-born peers (Shrout et al., 1992; Vega et al., 1998; Alegría et al., 2008; Grant et al., 2004; Breslau et al., 2007; Takeuchi et al., 2007; Breslau et al., 2009; Cantor-Graae and Petersen, 2013). Several protective factors are postulated to explain these counter-intuitive results, including: social support, cultural beliefs and practices, extended family support networks, and lower rates of substance misuse (Escobar, 1998; Escovar et al., 2000; Schwartz et al., 2010; Marks et al., 2013; Salas-Wright et al., 2014b; Salas-Wright and Vaughn, 2014; Suárez-Orozco et al., 2014). In addition, the healthy immigrant effect—the selective process whereby only those in relatively good health elect to migrate—is also postulated to explain these health dissimilarities ( Jasso et al., 2004; Akresh and Frank, 2008). This effect may be particularly applicable for immigrants to the United States due to geography (greater distance and cost necessary to travel from major population centers) and post-migration experiences (employment and educational opportunities). However, the mental health advantage enjoyed by first-generation immigrants may not hold fast for second and even third-generation immigrants. First-generation immigrants report better mood/anxiety disorder outcomes compared to subsequent immigrant generations (Harker, 2001; Alegríaet al., 2007; Takeuchi et al., 2007; Williams et al., 2007) whose mental health outcomes mirror those of native-born individuals. Furthermore, even among first-generation immigrants, additional time spent in the diaspora is also associated with declining mental health (Alegría et al., 2007).
It should also be noted that the nature of the relationship between immigrant status and mental health may be distinct among individuals from different racial/ethnic groups and, potentially, among immigrants from various regions of the world. For instance, in light of research on the relationship between discrimination and mental health (Pascoe and Richman, 2009), scholars have increasingly begun to highlight the importance of considering the degree to which factors such as racism, discrimination, and social marginalization may differentially impact racial/ethnic minority and non-minority immigrants (Viruell-Fuentes, 2007; Chung et al., 2008). Moreover, numerous studies have examined how the disruption of family networks and social support may contribute to increased mental distress among immigrants, particularly immigrants from collectivist cultures (Garcia Coll et al., 1996; Oppedal et al., 2004; Alegria et al., 2007). As such, it may be that the links between immigrant status and mental health are distinct among immigrants from global regions with a greater collectivist orientation (i.e., Africa, Asia, Latin America) than among those from regions that tend to be less collectivist in nature (i.e., Europe). Recent studies of immigrant well-being have pointed to regional differences among immigrants across various global regions (Vaughn et al., 2014a, 2014b).
1.2. The present study
This paper explores the immigrant paradox argument by examining the similarities and differences in mental health diagnoses between immigrants to the United States and their native-born peers. Using Wave I and Wave II of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), we examine the prevalence of mood, anxiety, and personality disorders across immigrant groups and compare these rates with the native-born population in the United States. In particular, we explore the following questions. First, is immigrant status protective for mood, anxiety, and personality disorders? Second, do the effects of immigrant status hold across immigrant generations and among both racial/ethnic minority and non-minority populations? Finally, what is the prevalence of mood/anxiety and personality disorders of immigrants representing major regions of the world?
2. Method
2.1. Participants
Study findings are based on data from Wave I (2001–2002) and Wave II (2004–2005) of the NESARC. The NESARC is a nationally representative sample of non-institutionalized U.S. residents aged 18 years and older. The design and methods are presented in a summarized form; however, a detailed description of the NESARC procedures is available elsewhere (Grant et al., 2003). The NESARC utilized a multistage cluster sampling design, oversampling young adults, Hispanics, and African-Americans in the interest of obtaining reliable statistical estimation in these subpopulations and ensuring appropriate representation of racial/ethnic subgroups.
2.2. Diagnostic assessment
Data were collected through face-to-face structured psychiatric interviews conducted by U.S. Census workers trained by the National Institute on Alcohol Abuse and Alcoholism and U.S. Census Bureau. Interviewers administered the Alcohol Use Disorder and Associated Disabilities Interview Schedule – DSM-IV version (AUDADIS-IV), which provides diagnoses for mood, anxiety, personality, and substance use disorders. The AUDADIS-IV has shown to have good-to-excellent reliability in assessing mental disorders in the general population (Grant et al., 1995; Hasin et al., 1997). Participants had the option of completing the NESARC interview in English, Spanish, or one of four Asian languages (Mandarin, Cantonese, Korean and Vietnamese).
2.3 Measures
2.3.1. Immigrant status
Respondents were asked whether they and their parents were born in the United States of America. Three mutually exclusive categories were created: Respondents who reported having been born outside the United States (n = 5363, 13.86%) were classified as first-generation immigrants. Respondents who reported that they had been born in the United States but at least one parent had been born outside the United States (n = 4826, 15.02%) were classified as second-generation immigrants. Respondents who reported that they and their parents were born in the United States were considered native-born Americans (n = 24,461). It should be noted that both “native-born” and “second-generation” respondents were born in the United States and therefore these terms are slightly imprecise. Nevertheless, we elected to use these terms are they are consistent with the work of scholars in prior research on immigration and health (e.g., Escobar et al., 2000; Glaesmer et al., 2011).
2.3.2. Mental health
Using the AUDADIS-IV, we examined lifetime DSM-IV mood (i.e., bipolar disorder, major depression, dysthymia), anxiety (i.e., generalized anxiety disorder, panic disorder, social phobia, specific phobia, and posttraumatic stress disorder) and personality disorders (i.e., antisocial, avoidant, borderline, narcissistic, obsessive-compulsive, paranoid, schizoid, and schizotypal). To ensure model stability, we limited our analyses to mental disorders with a prevalence of at least 2% in the general population. For each of these disorders, respondents who were identified as having met diagnostic criteria during their lifetime were coded as 1 and all other individuals coded as 0.
2.3.3. Sociodemographic and behavioral controls
The following sociodemographic variables were included as controls: age, gender, race/ethnicity, household income, education level, marital status, region of the United States, and urbanicity. Additionally, in examining the associations between immigration status and mental health disorders, we controlled for diagnoses of lifetime alcohol use disorders (abuse/dependence) as well as lifetime drug use disorders (abuse/dependence on heroin, hallucinogens, cocaine/crack, marijuana, stimulants, painkillers, tranquilizers, or sedatives). Prevalence estimates for substance use disorders among native-born Americans and immigrants are not reported in this study, but are available elsewhere (Salas-Wright and Vaughn, 2014).
2.4. Statistical analysis
Logistic regression analyses were conducted that compared non-immigrants with first- and second-generation immigrants to the United States in terms of mood, anxiety, and personality disorders. Adjusted odds ratios (AORs) were considered to be statistically significant if the associated confidence intervals did not cross the 1.0 threshold when controlling for sociodemographic factors and lifetime alcohol and illicit drug use disorders. For all statistical analyses, weighted prevalence estimates and standard errors were computed using Stata 13.1 SE software (StataCorp, 2013). This system implements a Taylor series linearization to adjust standard errors of estimates for complex survey sampling design effects including clustered data. Additional information about the sampling weights used in the NESARC is described in greater detail elsewhere (Grant et al., 2003).
3. Results
3.1. Sociodemographic characteristics of first- and second-generation immigrants
Table 1 displays the sociodemographic characteristics of native-born and first-generation immigrant adults ages 18 and older in the United States. No significant differences were observed for age or gender. However, first-generation immigrants to the United States were significantly more likely to be a racial/ethnic minority, to reside in households earning less than $70,000 per year, and to not have completed high school (AOR = 1.29, 95% CI = 1.20–1.39). Compared to native-born Americans, first-generation immigrants were significantly less likely to report a marital status other than married/ cohabitating.
Table 1.
Sociodemographic characteristics of native-born and first-generation immigrant adults in the United States
| Immigrated to the United States | Unadjusted | Adjusted | ||||||
|---|---|---|---|---|---|---|---|---|
| No (n = 24,461; 84.10%) |
Yes (n = 5363; 15.90%) |
|||||||
| % | 95% CI | % | 95% CI | OR | (95% CI) | OR | (95% CI) | |
| Sociodemographic | ||||||||
| Factors | ||||||||
| Age | ||||||||
| 18–34 years | 24.43 | (23.9–24.9) | 29.38 | (28.9–29.9) | 1.00 | 1.00 | ||
| 35–49 years | 31.66 | (31.2–32.1) | 34.92 | (34.4–35.4) | 0.92 | (0.88–0.95) | 1.00 | (0.95–1.05) |
| 50–64 years | 25.45 | (25.0–25.9) | 22.26 | (21.9–22.6) | 0.73 | (0.70–0.76) | 0.98 | (0.92–1.04) |
| 65+ | 18.46 | (18.1–18.8) | 13.44 | (13.1–13.8) | 0.60 | (0.58–0.63) | 0.98 | (0.90–1.07) |
| Gender | ||||||||
| Female | 52.33 | (51.9–52.7) | 50.48 | (50.0–51.0) | 1.00 | 1.00 | ||
| Male | 47.67 | (47.3–48.1) | 49.52 | (49.0–50.0) | 1.08 | (1.05–1.10) | 0.99 | (0.96–1.03) |
| Race/Ethnicity | ||||||||
| Non-Hispanic White | 80.97 | (80.3–81.6) | 22.21 | (21.8–22.8) | 1.00 | 1.00 | ||
| Non-Hispanic Black | 12.40 | (11.9–12.9) | 7.78 | (7.5–8.0) | 2.28 | (2.13–2.43) | 2.39 | (2.24–2.55) |
| Hispanic | 3.42 | (3.3–3.6) | 46.18 | (45.6–46.9) | 48.95 | (46.2–51.8) | 45.53 | (43.0–48.2) |
| Other | 3.21 | (2.9–3.5) | 23.74 | (23.2–24.3) | 26.86 | (24.3–29.6) | 26.09 | (23.6–28.8) |
| Household Income | ||||||||
| < $20,000 | 18.77 | (18.4–19.1) | 22.65 | (22.2–23.1) | 1.58 | (1.51–1.64) | 1.12 | (1.02–1.22) |
| $20,000–$34,999 | 18.03 | (17.7–18.4) | 22.23 | (21.8–22.7) | 1.61 | (1.55–1.67) | 1.21 | (1.14–1.29) |
| $35,000–69,999 | 32.89 | (32.5–33.3) | 31.91 | (31.4–32.4) | 1.27 | (1.23–1.31) | 1.10 | (1.05–1.16) |
| > $70,000 | 30.30 | (29.9–30.6) | 23.20 | (22.8–23.6) | 1.00 | 1.00 | ||
| Education Level | ||||||||
| Less than H.S. | 11.16 | (10.8–11.5) | 29.25 | (28.7–29.8) | 2.86 | (2.73–3.00) | 1.29 | (1.20–1.39) |
| H.S. Graduate | 28.89 | (28.4–29.4) | 20.95 | (20.6–21.3) | 0.79 | (0.76–0.82) | 0.60 | (0.57–0.64) |
| Some College | 22.57 | (22.2–22.9) | 15.61 | (15.4–15.9) | 0.75 | (0.73–0.78) | 0.59 | (0.56–0.63) |
| Completed AA, BA, or Technical Degree | 37.37 | (36.9–37.8) | 34.20 | (33.5–34.8) | 1.00 | 1.00 | ||
| Marital Status | ||||||||
| Married/ Cohabitating | 63.57 | (63.1–64.0) | 629.74 | (69.4–70.1) | 1.00 | 1.00 | ||
| Separated/Divorced | 12.46 | (12.2–12.7) | 8.79 | (8.5–9.1) | 0.64 | (0.61–0.67) | 0.60 | (0.56–0.65) |
| Widowed | 6.90 | (6.7–7.1) | 5.33 | (5.2–5.5) | 0.70 | (0.67–0.74) | 0.82 | (0.75–0.90) |
| Never Married | 17.08 | (16.7–17.5) | 16.13 | (15.8–16.4) | 0.86 | (0.83–0.89) | 0.76 | (0.72–0.80) |
| Region of U.S.A. | ||||||||
| Northeast | 18.67 | (18.2–19.2) | 15.15 | (14.7–15.6) | 0.79 | (0.75–0.83) | 0.85 | (0.78–0.93) |
| Midwest | 17.65 | (17.3–18.0) | 22.31 | (21.7–22.9) | 1.23 | (1.18–1.28) | 1.09 | (1.03–1.16) |
| South | 38.76 | (38.2–39.3) | 36.96 | (36.5–37.4) | 0.93 | (0.90–0.96) | 0.91 | (0.86–0.96) |
| West | 24.93 | (24.5–25.4) | 25.57 | (25.1–26.1) | 1.00 | 1.00 | ||
| Urbanicity | ||||||||
| Urban | 67.50 | (66.9–68.1) | 66.71 | (66.1–67.3) | 1.04 | (1.00–1.07) | 1.05 | (0.99–1.11) |
| Rural | 32.50 | (31.9–33.1) | 33.29 | (32.6–33.9) | 1.00 | 1.00 | ||
Note: Adjusted odds ratios adjusted for age, gender, race/ethnicity, household income, education level, marital status, region of the United States, and urbanicity. Odds ratios in bold are significant at p < .05 or lower
We also examined the sociodemographic characteristics of native-born and second-generation immigrant adults ages 18 and older in the United States (not shown). Compared to native-born Americans, second-generation immigrants were significantly more likely to be 65 years or older (AOR = 2.33, 95% CI = 2.17–2.50), and significantly less likely to be between the ages of 35 and 49 (AOR = 0.83, 95% CI = 0.78–0.88) or 50 and 64 (AOR = 0.92, 95% CI = 0.85–0.98). Second-generation immigrants were significantly more likely to be Hispanic (AOR = 0.72, 95% CI = 8.31–9.39) or other race (AOR = 2.65, 95% CI = 2.35–3.00) and significantly less likely to be non-Hispanic black (AOR = 0.72, 95% CI = 0.67–0.77). Second-generation immigrants were also significantly less likely to reside in households earning less than $70,000 per year and to have completed less than a post-high school degree program. Compared to native-born Americans, second-generation immigrants were significantly more likely to be divorced or widowed (AOR = 1.25, 95% CI = 1.16–1.35) or to never have been married (AOR = 1.41, 95% CI = 1.33–1.50). Second-generation immigrants were significantly less likely to reside in either the Northeastern (AOR = 0.82, 95% CI = 0.77–0.88) or Southern United States (AOR = 0.93, 95% CI = 0.87–0.98). No significant differences were identified in contrasting second-generation immigrants and native-born Americans in terms of gender or urbanicity.
3.2. Mental disorders among first- and second-generation immigrants
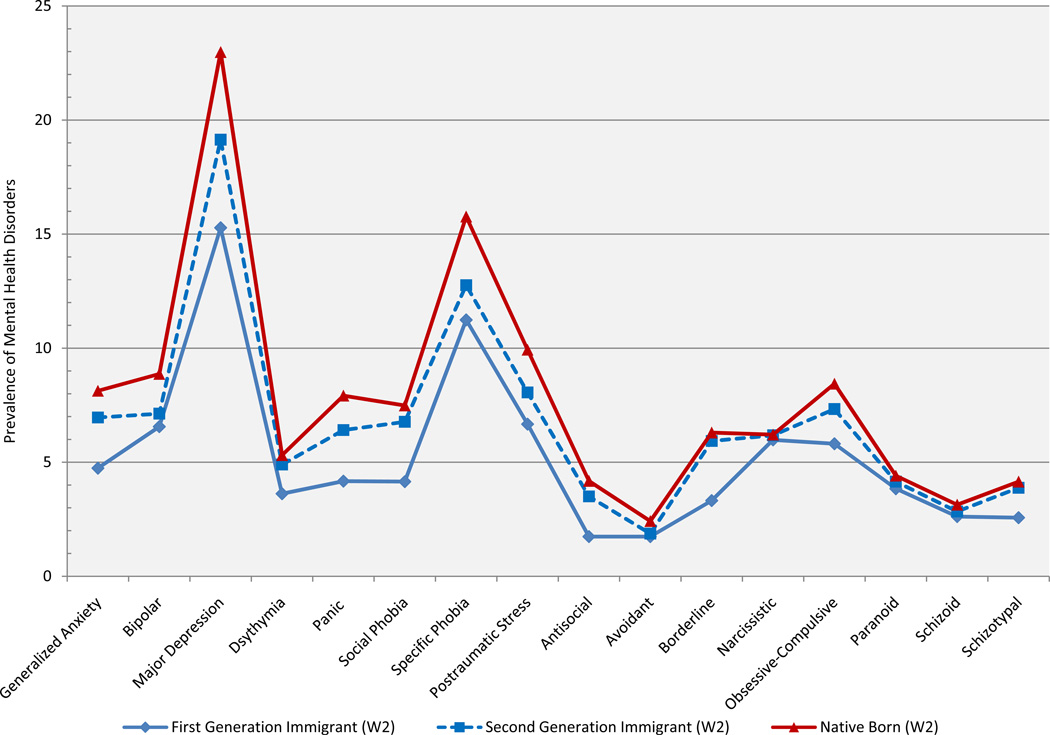
Figure 1 displays the prevalence of lifetime mood, anxiety, and personality disorders among native-born Americans and first- and second-generation immigrant adults ages 18 and older in the United States. For all disorders examined in this study, the prevalence of morbidity was lowest among first-generation immigrants followed by second-generation immigrants, and, finally, native-born Americans. For instance, a steady increase in the prevalence of major depressive disorder can be identified in comparing first-generation immigrants (15.28%), second-generation immigrants (19.14%), and native-born Americans (22.98%). Similarly, the prevalence of borderline personality disorder is lowest among first-generation immigrants (3.32%) as compared to second-generation immigrants (5.93%) and native-born Americans (6.30%).
Figure 1.
Prevalence of lifetime mood/anxiety and personality disorders among native-born and first- and second-generation immigrant adults in the United States
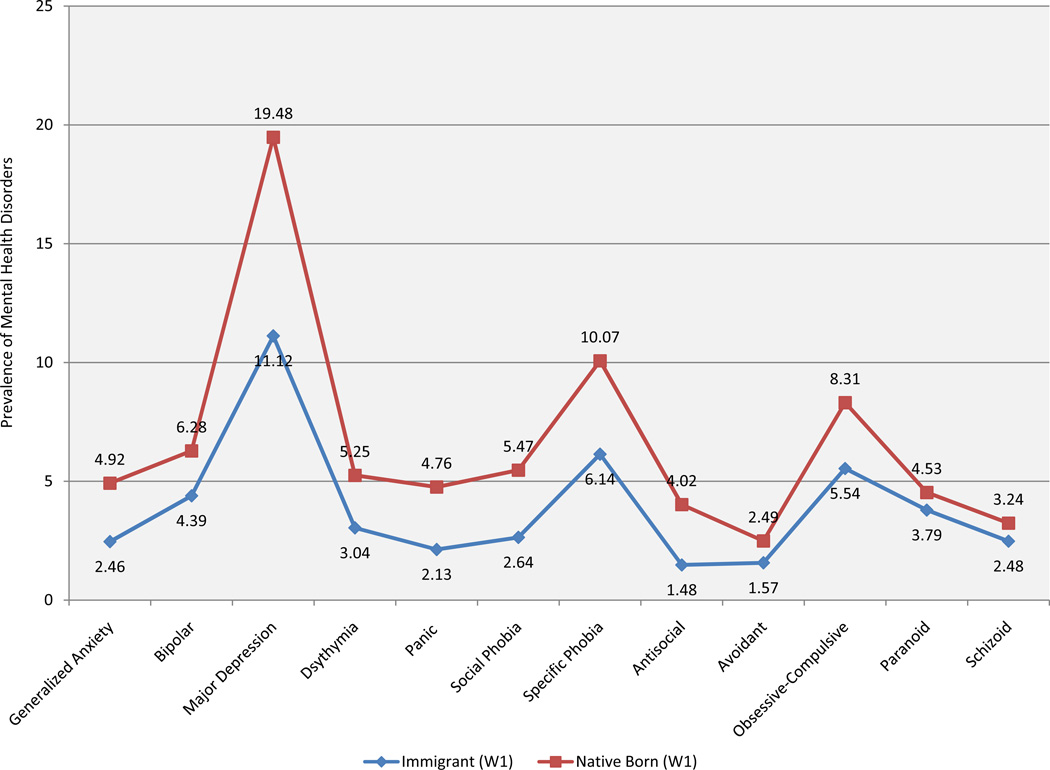
Results presented above are for Wave II data; however, we assessed the stability of the results using Wave I data collected three years prior. Although the prevalence of mental disorders was slightly lower at Wave I than at Wave II and several disorders examined in Wave II were not included in the Wave I data collection (see Figure 2), results of logistic regression analyses for Wave I largely mirrored the overall pattern found for Wave II. Namely, controlling for the same list of sociodemographic factors utilized in the present study, immigrants were found to be significantly less likely to meet diagnostic criteria for nearly all mood, anxiety, and personality disorders examined in the study. Sensitivity analysis could not be conducted for second-generation immigrants as this information was not available in the Wave I data.
Figure 2.
Sensitivity analysis of the prevalence of lifetime mood/anxiety and personality among native-born and immigrant adults (Wave I).
Table 2 compares the prevalence of mood, anxiety, and personality disorders among native-born Americans and first-and second-generation immigrants to the United States. Controlling for sociodemographic factors as well as lifetime diagnoses of alcohol and illicit drug use disorders, first-generation immigrants were significantly less likely to have met criteria for one or more mood/anxiety disorders (AOR = 0.70, 95% CI = 0.67–0.73). In terms of particular disorders, first-generation immigrants were significantly less likely to have met criteria for most mood disorders (i.e., major depression, bipolar disorder), all anxiety disorders (i.e., generalized anxiety, panic disorder, social phobia, specific phobia, posttraumatic stress disorder) and the majority of personality disorders (i.e., antisocial, avoidance, borderline, paranoid, and schizotypal) examined in this study. Significant associations were not observed for dysthymia and narcissistic, obsessive-compulsive, paranoid, and schizoid personality disorders. However, with the exception of narcissistic personality disorder, all of the personality disorders that were found to be not significantly associated with immigration status when controlling for sociodemographic and substance use factors, were significantly associated with first-generation immigration status at the bivariate level.
Table 2.
Odds ratios for psychiatric disorders among first- and second-generation immigrant adults in the U.S.A.
| Immigrated to the United States | Second Generation Immigrant | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | (95% CI) | AOR | (95% CI) | OR | (95% CI) | AOR | (95% CI) | |
| Mood/Anxiety Disorders | ||||||||
| Any Mood/Anxiety Disorder | 0.60 | (0.58–0.62) | 0.70 | (0.67–0.73) | 0.82 | (0.79–0.85) | 0.92 | (0.88–0.96) |
| Generalized Anxiety | 0.55 | (0.52–0.57) | 0.74 | (0.70–0.79) | 0.83 | (0.78–0.88) | 1.00 | (0.93–1.06) |
| Bipolar Disorder | 0.69 | (0.66–0.73) | 0.83 | (0.77–0.89) | 0.76 | (0.73–0.80) | 0.86 | (0.81–0.90) |
| Major Depression | 0.58 | (0.55–0.61) | 0.73 | (0.68–0.77) | 0.77 | (0.73–0.80) | 0.86 | (0.82–0.90) |
| Dysthymia | 0.66 | (0.61–0.71) | 0.87 | (0.76–1.00) | 0.91 | (0.85–0.97) | 1.07 | (0.99–1.16) |
| Panic disorder | 0.49 | (0.46–0.51) | 0.62 | (0.58–0.67) | 0.77 | (0.73–0.82) | 0.88 | (0.83–0.93) |
| Social phobia | 0.53 | (0.47–0.58) | 0.69 | (0.60–0.80) | 0.89 | (0.82–0.96) | 1.04 | (0.96–1.13) |
| Specific Phobia | 0.65 | (0.62–0.68) | 0.73 | (0.69–0.78) | 0.75 | (0.72–0.79) | 0.84 | (0.80–0.88) |
| Posttraumatic Stress | 0.62 | (0.60–0.65) | 0.66 | (0.62–0.71) | 0.77 | (0.72–0.82) | 0.84 | (0.79–0.91) |
| Personality Disorders | ||||||||
| Any Personality Disorder | 0.75 | (0.73–0.77) | 0.78 | (0.74–0.82) | 0.90 | (0.87–0.94) | 0.97 | (0.92–1.01) |
| Antisocial | 0.39 | (0.32–0.48) | 0.51 | (0.37–0.71) | 0.81 | (0.74–0.89) | 0.86 | (0.77–0.96) |
| Avoidant | 0.68 | (0.62–0.75) | 0.74 | (0.59–0.91) | 0.75 | (0.66–0.84) | 0.82 | (0.71–0.95) |
| Borderline | 0.50 | (0.48–0.53) | 0.64 | (0.58–0.71) | 0.93 | (0.87–0.99) | 1.11 | (1.03–1.20) |
| Narcissistic | 0.96 | (0.90–1.02) | 1.00 | (0.92–1.08) | 0.99 | (0.93–1.06) | 1.06 | (0.99–1.14) |
| Obsessive-Compulsive | 0.65 | (0.61–0.69) | 0.92 | (0.82–1.03) | 0.84 | (0.79–0.89) | 0.96 | (0.89–1.02) |
| Paranoid | 0.86 | (0.77–0.95) | 0.88 | (0.73–1.06) | 0.94 | (0.85–1.03) | 1.01 | (0.90–1.13) |
| Schizoid | 0.82 | (0.76–0.88) | 0.90 | (0.80–1.01) | 0.90 | (0.81–1.00) | 0.99 | (0.89–1.12) |
| Schizotypal | 0.60 | (0.56–0.64) | 0.69 | (0.62–0.76) | 0.93 | (0.84–1.02) | 1.10 | (1.00–1.21) |
Note: Adjusted odds ratios adjusted for age, gender, race/ethnicity, household income, education level, marital status, region of the United States, urbanicity, and lifetime diagnosis of alcohol and any drug abuse or dependence. Odds ratios in bold are significant at p < .05 or lower.
Table 2 also compares the prevalence of mood, anxiety, and personality disorders among native-born Americans and second-generation immigrants to the United States. Controlling for the same list of sociodemographic and substance use factors, second-generation immigrants were significantly less likely to have met criteria for one or more mood/anxiety disorder (AOR = 0.92, 95% CI = 0.88–0.96). In terms of particular disorders, second-generation immigrants were also significantly less likely to have met criteria for the majority of mood and anxiety disorders examined in this study (i.e., bipolar disorder, major depression, panic disorder, specific phobia, and posttraumatic stress disorder). However, in contrast to first-generation immigrants, no significant associations were identified in terms of generalized anxiety disorder, dysthymia, or social phobia. Moreover, as evidenced by non-overlapping confidence intervals, the strength of the association between second-generation immigrant status and major depressive disorder (AOR = 0.86, 95% CI = 0.82–0.90), panic disorder (AOR = 0.88, 95% CI = 0.83–0.93), specific phobia (AOR = 0.84, 95% CI = 0.80–0.88) and posttraumatic stress disorder (AOR = 0.84, 95% CI = 0.79–0.91) was significantly weaker among second-generation immigrants as compared to first generation immigrants.
In terms of personality disorders, compared to native-born Americans, second-generation immigrants were significantly less likely to meet criteria for antisocial (AOR = 0.86, 95% CI = 0.77–0.96) and avoidant personality disorder (AOR = 0.82, 95% CI = 0.71–0.95). With respect to antisocial personality disorder, the strength of the association between immigrant status and morbidity was significantly weaker among second-generation immigrants as compared to first-generation immigrants. Finally, with respect to borderline personality disorder (AOR = 1.11, 95% CI = 1.03–1.20), second-generation immigrants were found to be significantly more likely to meet criteria for this disorder as compared to native-born Americans when controlling for sociodemographic and substance use factors.
3.3. Mental disorders among first and second-generation immigrants by racial/ethnic minority versus non-minority status
To assess the impact of racism/discrimination on the mental health of immigrants, we conducted supplementary analyses examining the lifetime prevalence of mood/anxiety and personality disorders among native-born, first-generation, and second-generation respondents while stratifying by racial/ethnic minority (i.e., Black, non-Hispanic; Hispanic; other race/ethnicity) and non-minority (i.e., non-Hispanic white) status. Controlling for sociodemographic and behavioral confounds, first-generation immigrants from both racial/ethnic minority (AOR = 0.64, 95% CI = 0.60–0.67) and non-minority (AOR = 0.82, 95% CI = 0.77–0.88) groups were significantly less likely to meet criteria for a mood/anxiety disorder. Notably, as evidenced by nonoverlapping confidence intervals, effects were significantly greater for racial/ethnic minority immigrants than for non-minority immigrants. Among second-generation immigrants, the link between immigrant status and mood/anxiety disorders was significant for racial/ethnic minority immigrants (AOR = 0.84, 95% CI = 0.78–0.89) but no significant relationship was observed for second-generation non-minority immigrants. Similarly, first (AOR = 0.70, 95% CI = 0.65–0.75) and second-generation (AOR = 0.79, 95% CI = 0.73–0.86) racial/ethnic minority immigrants were significantly less likely to meet criteria for a personality disorder, but no relationship was identified for non-minority immigrants.
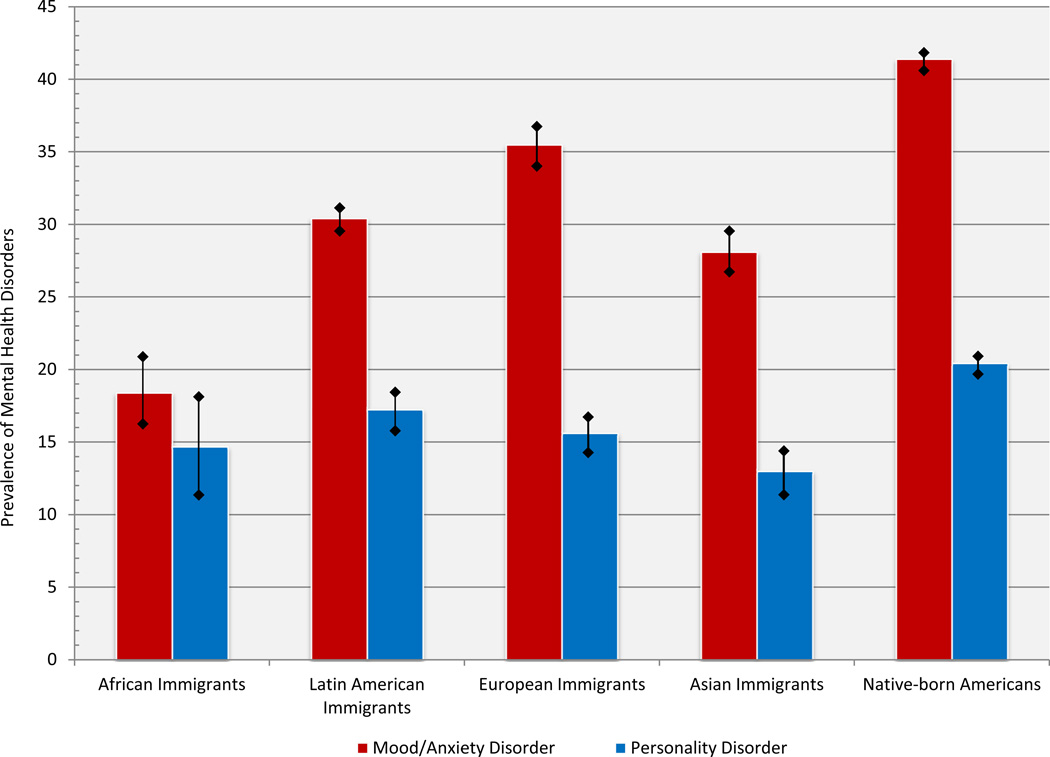
3.4. Mental disorders among immigrants from major global regions
Figure 2 presents the prevalence of mood, anxiety, and personality disorders among immigrants from four major global regions as well as that of native-born Americans. The prevalence of mood/anxiety and personality disorders of native-born Americans was greater than the prevalence identified among immigrants from Africa, Latin America, Europe, and Asia. European immigrants were identified as having the highest prevalence of mood/anxiety disorders (35.48%, 95% CI = 34.30–36.68) followed by Latin American (30.41%, 95% CI = 29.78–31.05) and Asian (28.09%, 95% CI = 26.94–29.26) immigrants. The lowest prevalence of mood/anxiety disorders was identified among African immigrants (18.39%, 95% CI = 16.01–21.04). With respect to personality disorders, less variability was observed as the prevalence of personality disorders among immigrants from Africa (14.67%, 95% CI = 11.90–70.94), Europe (15.61%, 95% CI = 14.61–16.65), and Latin America (17.24%, 95% CI = 16.90–17.58) was found to be roughly 15%. The prevalence of personality disorders among Asian immigrants was slightly lower than that of immigrants from other regions of the world (12.98%, 95% CI = 12.32–13.66).
4. Discussion
Present study results indicate that the prevalence of mood, anxiety, and personality disorders among first-generation immigrants is significantly less than that of native-born Americans. This is noteworthy given that immigrants were found to report lower income and education levels, both of which have been identified as risk factors for psychiatric morbidity among individuals in the general population (Lorant et al., 2003). We also found that, independent of what region of the world they came from, immigrants were less likely to be diagnosed with a mood/anxiety or personality disorder than native-born Americans. The disparities in prevalence between immigrants from these major regions of the world and native-born Americans were more pronounced for mood/anxiety disorders than for personality disorders. Asian immigrants were the least likely to be diagnosed with a personality disorder while African immigrants were least likely to be diagnosed with a mood or anxiety disorder.
With respect to second-generation immigrants, who also tend to be disproportionately disadvantaged in terms of income and education, the protective effect of immigrant status was somewhat attenuated. While second-generation immigrants were still less likely to be diagnosed with a mood/anxiety disorder, the effect wanes for general anxiety, dysthymia, and social phobia. With the exception of antisocial and avoidant personality disorders, the effect is also less pronounced for personality disorders. In fact, second-generation immigrants were more likely to be diagnosed with borderline personality disorder than native-born Americans. While the effects were small, this finding is noteworthy given the role of adverse life events in the etiology of borderline personality disorder in the general population (Leichsenring et al., 2011). This finding also raises questions as to intergenerational changes in exposure to childhood adversity and trauma among immigrant families.
This study examines several protective factors and, of these, immigrant status seems to be the constant determinant of mental health differences between first and second-generation immigrants and native-born respondents. It is of interest to note, however, that the effects of immigrant status seem to diminish over time. As such, present study results align with previous investigations that indicate a similar pattern and suggest a link between exposure to U.S. society and mental illness (e.g., Harker, 2001; Alegría et al., 2007; Takeuchi et al., 2007; Williams et al., 2007). It should also be noted that the relationship between immigrant status and mental health appears to be distinct among racial/ethnic minorities and non-minorities. Specifically, we found that, while both racial/ethnic minority and nonminority first-generation immigrants were found to be less likely to have a mood/anxiety disorder, the magnitude of this relationship was greater among minority immigrants than among non-minorities (i.e., non-Hispanic whites). Along the same lines, immigrant status was protective for mood/anxiety disorders among minority second-generation immigrants, but no relationship was observed among non-minority second-generation immigrants. Moreover, the relationship between immigrant status and personality disorders held for minority first and second-generation immigrants, but no link was observed among non-minority first or second-generation immigrants.
That there are generational and racial/ethnic differences provides a clear indication that post-migration factors do matter. Notwithstanding well-documented pre-migration stressors, the resettlement process seems to play a bigger role in informing mental health outcomes. Studies that have examined the resettlement phase point to adjustment stressors as potential triggers for mental illness (Aycan and Berry, 1996; Porter and Haslam, 2005). The loss of lifelong relationships, altered family roles, and economic incongruencies prior to and after migration are posited to adversely affect mental well-being. Additionally, the differential findings among minority and non-minority immigrants raise questions about segmented assimilation (Portes and Zhou, 1993) and the possible impact of racism and discrimination on the health of immigrants (Viruell-Fuentes, 2007; Chung et al., 2008; Pascoe and Richman, 2009). These findings also may be interpreted in the context of research examining the disruption of family and social support networks, particularly studies pointing to the importance of these factors among immigrants from non-western collectivist cultures (Garcia Coll et al., 1996; Oppedal et al., 2004; Alegria et al., 2007). A more robust body of research that examines the dynamics of resettlement in relation to mental health is needed to disentangle the etiology of generational and discriminatory factors.
4.1. Study limitations
The current study results should be interpreted within the context of several limitations. One limitation is that the data are less than ideal with respect to temporal ordering. Although we have follow-up data, the NESARC is not a true longitudinal investigation. We rely on retrospective lifetime measures and are unable to clarify the causal mechanisms that are associated with mental health among immigrants. Further, we do not know what the longer-term prevalence of mental disorders will be. This will require life-course study designs. Although the NESARC is a nationally representative sample, it is uncertain how the association between immigrant status and mental health would be similar or different if correctional or clinical samples were sampled. It seems likely that this would bias study findings and the difference between immigrants and native-born Americans would be magnified. We also don’t know if findings from the present investigation would replicate for immigrants to other nations. An additional limitation is that the NESARC did not include information on schizophrenia or other psychotic disorders. This omission is noteworthy given that such disorders have been found to be positively related to first- and second-generation immigrant status in previous research (Cantor-Graae and Selten, 2005; Bourque et al., 2011). The NESARC also is lacking variables tapping the reasons why individuals elected to immigrate to the United States (e.g., economic scarcity, professional re-location). This is noteworthy as, for example, the mental health of someone who immigrated to the United States due to economic scarcity may be different than someone who was recruited for a high-paying professional position. Finally, although respondents had the option of completing the NESARC in one of several different languages, it is possible that potential respondents who did not speak one of these languages were excluded. It is possible that these “linguistically isolated” individuals may be at greater risk of mental problems and thus the results may underestimate the true prevalence of morbidity among immigrants. Future studies on immigration and mental health will benefit from addressing these study features.
4.2. Conclusions
Findings of the present study provide evidence in support of a multigenerational immigrant paradox for mood, anxiety, and personality disorders. First-generation immigrants and, to a lesser extent, second-generation immigrants were found to be significantly less likely to be diagnosed with a mood, anxiety, or personality disorder compared to native-born Americans. Notably, however, these effects were distinct among racial/ethnic minority and non-minority immigrants. These effects held for immigrants from major regions across the globe, including Africa, Asia, Europe, and Latin America. In all, while caution should be exercised in interpreting study findings due to the potential effects of selection and treatment bias, results suggest that immigrant status and generation are important factors related to mental health and wellbeing among first and second-generation immigrants in the United States.
Figure 3.
Prevalence of lifetime mood/anxiety and personality disorders among native-born and immigrant adults by immigrant region of origin
Highlights.
First-generation immigrants at lower risk for mood, anxiety, or personality disorders
Similar results observed for first-generation immigrants from major world regions
Protective effects for morbidity more robust among racial/ethnic minority immigrants
Protective effect of immigrant status was somewhat attenuated by second-generation
Acknowledgments
This research was supported in part by a grant from the National Institute on Drug Abuse at the National Institutes of Health (R25 DA026401-PI: Valdez).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Akresh IR, Frank R. Health selection among new immigrants. American Journal of Public Health. 2008;98(4):1–7. doi: 10.2105/AJPH.2006.100974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, Torres M, Chen CN, Meng XL. Prevalence of mental illness in immigrant and non-immigrant US Latino groups. The American Journal of Psychiatry. 2008;165(3):359. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. American Journal of Public Health. 2007;97(1):68–75. doi: 10.2105/AJPH.2006.087205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Shrout PE, Woo M, Guarnaccia P, Sribney W, Vila D, Canino G. Understanding differences in past year psychiatric disorders for Latinos living in the US. Social Science & Medicine. 2007;65(2):214–230. doi: 10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aycan Z, Berry JW. Impact of employment-related experiences on immigrants' psychological well-being and adaptation to Canada. Canadian Journal of Behavioural Science. 1996;28(3):240. [Google Scholar]
- Breslau J, Aguilar-Gaxiola S, Borges G, Kendler KS, Su M, Kessler RC. Risk for psychiatric disorder among immigrants and their US-born descendants: Evidence from the National Comorbidity Survey-Replication. The Journal of Nervous and Mental Disease. 2007;195(3):189. doi: 10.1097/01.nmd.0000243779.35541.c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Borges G, Hagar Y, Tancredi D, Gilman S. Immigration to the USA and risk for mood and anxiety disorders: variation by origin and age at immigration. Psychological Medicine. 2009;39(07):1117–1127. doi: 10.1017/S0033291708004698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourque F, Van der Ven E, Malla A. A meta-analysis of the risk for psychotic disorders among first-and second-generation immigrants. Psychological Medicine. 2011;41(5):897. doi: 10.1017/S0033291710001406. [DOI] [PubMed] [Google Scholar]
- Cantor-Graae E, Selten JP. Schizophrenia and migration: A meta-analysis and review. American Journal of Psychiatry. 2005;162(1):12–24. doi: 10.1176/appi.ajp.162.1.12. [DOI] [PubMed] [Google Scholar]
- Choi Y, He M, Harachi TW. Intergenerational cultural dissonance, parent-child conflict and bonding, and youth problem behaviors among Vietnamese and Cambodian immigrant families. Journal of Youth and Adolescence. 2008;37(1):85–96. doi: 10.1007/s10964-007-9217-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung RCY, Bemak F, Ortiz DP, Sandoval-Perez PA. Promoting the mental health of immigrants: A multicultural/social justice perspective. Journal of Counseling & Development. 2008;86(3):310–317. [Google Scholar]
- Crisp J. A state of insecurity: The political economy of violence in kenya's refugee camps. African Affairs. 2000;99(397):601–632. [Google Scholar]
- Derose KP, Bahney BW, Lurie N, Escarce JJ. Review: immigrants and health care access, quality, and cost. Medical Care Research and Review. 2009;66(4):355–408. doi: 10.1177/1077558708330425. [DOI] [PubMed] [Google Scholar]
- Escobar JI. Immigration and mental health: Why are immigrants better off? Archives of General Psychiatry. 1998;55(9):781–782. doi: 10.1001/archpsyc.55.9.781. [DOI] [PubMed] [Google Scholar]
- Escobar JI, Nervi CH, Gara MA. Immigration and mental health: Mexican Americans in the United States. Harvard Review of Psychiatry. 2000;8(2):64–72. [PubMed] [Google Scholar]
- Farley T, Galves A, Dickinson LM, Perez MdJD. Stress, coping, and health: a comparison of Mexican immigrants, Mexican-Americans, and non-Hispanic whites. Journal of Immigrant Health. 2005;7(3):213–220. doi: 10.1007/s10903-005-3678-5. [DOI] [PubMed] [Google Scholar]
- Fazel M, Reed RV, Panter-Brick C, Stein A. Mental health of displaced and refugee children resettled in high-income countries: risk and protective factors. The Lancet. 2012;379(9812):266–282. doi: 10.1016/S0140-6736(11)60051-2. [DOI] [PubMed] [Google Scholar]
- Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. The Lancet. 2005;365(9467):1309–1314. doi: 10.1016/S0140-6736(05)61027-6. [DOI] [PubMed] [Google Scholar]
- Garcia Coll CG, Lamberty J, McAdoo HP, Crnic K, Wasik J, Garcia VH. An integrative model for the study of developmental competencies in minority children. Child Development. 1996;67(5):1891–1914. [PubMed] [Google Scholar]
- Glaesmer H, Wittig U, Braehler E, Martin A, Mewes R, Rief W. Health care utilization among first and second generation immigrants and native-born Germans: a population-based study in Germany. International Journal of Public Health. 2011;56(5):541–548. doi: 10.1007/s00038-010-0205-9. [DOI] [PubMed] [Google Scholar]
- Goodman JH. Coping with trauma and hardship among unaccompanied refugee youths from Sudan. Qualitative Health Research. 2004;14(9):1177–1196. doi: 10.1177/1049732304265923. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan KD, Shepard J, Moore T. Source and accuracy statement for Wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- Grant BF, Hartford T, Dawson DA, Chou PS, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): Reliability of alcohol and drug modules in the general population sample. Drug and Alcohol Dependence. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61(12):1226. doi: 10.1001/archpsyc.61.12.1226. [DOI] [PubMed] [Google Scholar]
- Harker K. Immigrant generation, assimilation, and adolescent psychological well-being. Social Forces. 2001;79(3):969–1004. [Google Scholar]
- Hasin D, Carpenter KM, McCloud S, Grant BF. The alcohol use disorders and associated disabilities interview schedule (AUDADIS): Reliability of alcohol and drug modules in a clinical sample. Drug and Alcohol Dependence. 1997;44:133–141. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- Jasso G, Massey DS, Rosenzweig MR, Smith JP. Immigrant health: selectivity and acculturation. Critical Perspectives on Racial and ethnic Differences in Health in Late Life. 2004:227–266. [Google Scholar]
- Kim G, Aguado Loi CX, Chiriboga DA, Jang Y, Parmelee P, Allen RS. Limited English proficiency as a barrier to mental health service use: A study of Latino and Asian immigrants with psychiatric disorders. Journal of Psychiatric Research. 2011;45(1):104–110. doi: 10.1016/j.jpsychires.2010.04.031. doi: http://dx.doi.org/10.1016/j.jpsychires.2010.04.031. [DOI] [PubMed] [Google Scholar]
- Leichsenring F, Leibing E, Kruse J, New AS, Leweke F. Borderline personality disorder. The Lancet. 2011;377(9759):74–84. doi: 10.1016/S0140-6736(10)61422-5. [DOI] [PubMed] [Google Scholar]
- Liddell BJ, Chey T, Silove D, Phan TT, Giao NM, Steel Z. Patterns of risk for anxiety-depression amongst Vietnamese-immigrants: a comparison with source and host populations. BMC Psychiatry. 2013;13(1):329. doi: 10.1186/1471-244X-13-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorant V, Deliège D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. American Journal of Epidemiology. 2003;157(2):98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Lustig SL, Kia-Keating M, Knight WG, Geltman P, Ellis H, Kinzie JD, Keane T, Saxe GN. Review of child and adolescent refugee mental health. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(1):24–36. doi: 10.1097/00004583-200401000-00012. [DOI] [PubMed] [Google Scholar]
- Marks AK, Ejesi K, García Coll C. Understanding the US Immigrant Paradox in Childhood and Adolescence. Child Development Perspectives. 2014;8(2):59–64. [Google Scholar]
- Nadeem E, Lange J, Edge D, Fongwa M, Belin T, Miranda J. Does stigma keep poor young immigrant and US-born black and Latina women from seeking mental health care? Psychiatric Services. 2007;58(12):1547–1554. doi: 10.1176/ps.2007.58.12.1547. [DOI] [PubMed] [Google Scholar]
- Oppedal B, Røysamb E, Sam DL. The effect of acculturation and social support on change in mental health among young immigrants. International Journal of Behavioral Development. 2004;28(6):481–494. [Google Scholar]
- Paardekooper B, De Jong J, Hermanns J. The psychological impact of war and the refugee situation on South Sudanese children in refugee camps in Northern Uganda: an exploratory study. Journal of child Psychology and Psychiatry. 1999;40(4):529–536. [PubMed] [Google Scholar]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychological Bulletin. 2009;135(4):531. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter M, Haslam N. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons. JAMA: The Journal of the American Medical Association. 2005;294(5):602–612. doi: 10.1001/jama.294.5.602. [DOI] [PubMed] [Google Scholar]
- Portes A, Zhou M. The new second generation: Segmented assimilation and its variants. The Annals of the American Academy of Political and social Science. 1993;530(1):74–96. [Google Scholar]
- Potocky-Tripodi M. Best practices for social work with refugees and immigrants. Columbia University Press; 2002. [Google Scholar]
- Pumariega AJ, Rothe E, Pumariega JB. Mental health of immigrants and refugees. Community Mental Health Journal. 2005;41(5):581–597. doi: 10.1007/s10597-005-6363-1. [DOI] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG. A refugee paradox for substance use disorders? Drug and Alcohol Dependence. 2014 doi: 10.1016/j.drugalcdep.2014.06.008. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright CP, Clark TT, Vaughn MG, Córdova D. Profiles of acculturation among Hispanics in the United States: links with discrimination and substance use. Social Psychiatry and Psychiatric Epidemiology. 2014a doi: 10.1007/s00127-014-0889-x. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG, Clark TT, Terzis L, Córdova D. Substance use disorders among first and second-generation immigrants in the USA: Evidence of an immigrant paradox? Journal of Studies on Alcohol and Drugs. 2014b doi: 10.15288/jsad.2014.75.958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: implications for theory and research. American Psychologist. 2010;65(4):237. doi: 10.1037/a0019330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sentell T, Shumway M, Snowden L. Access to mental health treatment by English language proficiency and race/ethnicity. Journal of General Internal Medicine. 2007;22(Suppl. 2):289–293. doi: 10.1007/s11606-007-0345-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Canino GJ, Bird HR, Rubio-Stipec M, Bravo M, Burnam MA. Mental health status among Puerto Ricans, Mexican Americans, and non-Hispanic whites. American Journal of Community Psychology. 1992;20(6):729–752. [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 13. StataCorp LP: College Station, TX; 2013. [Google Scholar]
- Steel Z, Silove D, Brooks R, Momartin S, Alzuhairi B, Susljik I. Impact of immigration detention and temporary protection on the mental health of refugees. The British Journal of Psychiatry. 2006;188(1):58–64. doi: 10.1192/bjp.bp.104.007864. [DOI] [PubMed] [Google Scholar]
- Steel Z, Silove D, Phan T, Bauman A. Long-term effect of psychological trauma on the mental health of Vietnamese refugees resettled in Australia: a population-based study. The Lancet. 2002;360(9339):1056–1062. doi: 10.1016/S0140-6736(02)11142-1. [DOI] [PubMed] [Google Scholar]
- Suárez-Orozco MM, Suárez-Orozco C, Qin-Hilliard D. Theoretical Perspectives: Interdisciplinary Perspectives on the New Immigration. New York, NY: Routledge; 2014. [Google Scholar]
- Sue S, Fujino DC, Hu L-t, Takeuchi DT, Zane NWS. Community mental health services for ethnic minority groups: A test of the cultural responsiveness hypothesis. Journal of Consulting and Clinical Psychology. 1991;59(4):533–540. doi: 10.1037//0022-006x.59.4.533. [DOI] [PubMed] [Google Scholar]
- Takeuchi DT, Zane N, Hong S, Chae DH, Gong F, Gee GC, Walton E, Sue S, Alegría M. Immigration-related factors and mental disorders among Asian Americans. American Journal Of Public Health. 2007;97(1):84–90. doi: 10.2105/AJPH.2006.088401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinghög P, Hemmingsson T, Lundberg I. To what extent may the association between immigrant status and mental illness be explained by socioeconomic factors? Social Psychiatry and Psychiatric Epidemiology. 2007;42(12):990–996. doi: 10.1007/s00127-007-0253-5. [DOI] [PubMed] [Google Scholar]
- Vaughn MG, Salas-Wright CP, Cooper-Sadlo S, Maynard BR, Larson MJ. Are immigrants more likely than native-born Americans to perpetrate intimate partner violence? Journal of Interpersonal Violence. 2014a doi: 10.1177/0886260514549053. [DOI] [PubMed] [Google Scholar]
- Vaughn MG, Salas-Wright CP, DeLisi M, Maynard BR. The immigrant paradox: Immigrants are less antisocial than native-born Americans. Social Psychiatry and Psychiatric Epidemiology. 2014b;49(7):1129–1137. doi: 10.1007/s00127-013-0799-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega WA, Kolody B, Aguilar-Gaxiola S, Alderete E, Catalano R, Caraveo-Anduaga J. Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Archives of General Psychiatry. 1998;55(9):771–778. doi: 10.1001/archpsyc.55.9.771. [DOI] [PubMed] [Google Scholar]
- Viruell-Fuentes EA. Beyond acculturation: immigration, discrimination, and health research among Mexicans in the United States. Social Science and Medicine. 2007;65(7):1524–1535. doi: 10.1016/j.socscimed.2007.05.010. [DOI] [PubMed] [Google Scholar]
- WHO. Investing in mental health: Evidence for action. Geneva: Switzerland; 2013. [Google Scholar]
- Williams DR, Haile R, González HM, Neighbors H, Baser R, Jackson JS. The mental health of Black Caribbean immigrants: Results from the National Survey of American Life. American Journal of Public Health. 2007;97(1):52–59. doi: 10.2105/AJPH.2006.088211. [DOI] [PMC free article] [PubMed] [Google Scholar]