Abstract
Objectives
To investigate whether levels of blood pressure and fasting glucose differ among Chinese children of three different ethnicities (i.e., Uyghurs, Kazakhs and Hans) and whether the differences are explained by childhood obesity.
Methods
A school-based cross-sectional study was conducted in a large three ethnic pediatric population (n=6,633), whose ages ranged from 7–18 years. Anthropometrics and blood pressure were measured using standard protocols. Fasting glucose was measured in a subset of children (n=2,295) who were randomly selected based on ethnicity and age. The age-sex stratified Chinese national cutoffs were used to define obesity and high blood pressure (HBP). The prevalence of HBP, impaired fasting glucose (IFG), mean levels of blood pressure and glucose were compared among three ethnic groups.
Results
2,142 Uyghurs, 2,078 Han and 1,997 Kazakhs were analyzed. After adjusting for age and body mass index (BMI), the mean blood pressure for Uyghurs was on average, 2–4 mmHg lower than those for Hans and Kazakhs. Kazakhs had the lowest mean fasting glucose compared with Hans and Uyghurs (4.5 vs 5.0 vs. 4.8mmol/L, respectively). The differences in blood pressure and fasting glucose persisted even after adjusting for age and BMI, and the differences among ethnic groups in blood pressure levels and fasting glucose levels were observed as early as 7 to 9 years of age.
Conclusions
The prevalence of HBP and IFG differed significantly among Uyghurs, Hans and Kazakhs, and the ethnic differences observed in childhood were consistent with those observed in adults from the same region. While childhood obesity is a significant risk factor for hypertension and elevated glucose, the differences among ethnic groups were not explained by obesity alone.
Keywords: children and adolescents, hypertension, obesity, ethnic difference, diabetes
Introduction
Childhood hypertension and diabetes have become global public health problems, especially in developing countries, and childhood obesity is one of the leading causes (Freedman et al. 1999; Sorof et al. 2002; Rosner et al. 2000). Previous studies have shown that the prevalence of obesity and of metabolic syndrome components differ in Chinese Uyghur, Hans and Kazakhs, and the differences are observed in children (Yan et al. 2006) as well as in adults (Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: a working group report from the National High Blood Pressure Education Program. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents 1996; Yan et al. 2005). For example, at the same level of BMI, Kazakh adults have a higher risk of having hypertension than Uyghur adults; on the other hand, Uyghur adults have a higher risk of having type 2 diabetes than Kazakh adults (Yan et al. 2005). A recent Chinese national survey showed that the mean systolic blood pressure (SBP) for seven year old Kazakh children was significantly higher than that for Uyghur children (100.5 mmHg vs. 81.0 mm Hg, respectively), and this pattern persisted to 18 years of age (118.4 mmHg vs. 107.2 mmHg) (Work Group of Physical Fitness and Health Surveillance of Chinese School Students. Report on the Physical Fitness and Health Surveillance of Chinese School Students. 2007). To date, studies have not examined how obesity and related traits influence risks of high blood pressure and type 2 diabetes in three ethnic groups who are living within one geographical area, Xinjiang, China. In the present paper, we examined whether: (1) the risks of hypertension and type 2 diabetes differ by ethnicity in a Chinese pediatric population; and (2) childhood overweight/obesity contribute significantly to high blood pressure and impaired glucose regulation.
Methods
Study population
A school-based cross-sectional study was conducted across several schools in Xinjiang Uyghur Autonomous Region of China. Schools with high enrollment of ethnic Uyghur, Han and Kazakh school-aged children were selected. All students from the participating schools whose ages ranged between 7 and 18 years were eligible to enroll in the study. The three major ethnic groups in Xinjiang Uyghur Autonomous Region -- Uyghurs, Hans and Kazakhs,-- comprised 45.9%, 39.6% and 7.0%, respectively, of the total population according to the 5th National Census of China. Children of Hans and Uyghur ethnicity were recruited from six state-run primary schools (grades 1–6) and six middle schools (grades 7 to 12) schools located in Urumqi city. Because only a small number of Kazakhs live in Urumqi city, Kazakhs were recruited from urban and suburban areas: two schools were located in Urumqi (15%) and four schools were in Altay city and surrounding suburban areas (85%).
Demographics, anthropometrics and overweight
A questionnaire was used to obtain demographic information. Self-reported ethnicity was obtained, and inter-ethnic marriages were rare due to differences in religion and traditional customs. Body weight and height were measured by standardized protocols according to the Physical Fitness and Health Surveillance of Chinese School Students (Work Group of Physical Fitness and Health Surveillance of Chinese School Students. Report on the Physical Fitness and Health Surveillance of Chinese School Students. 2007). To define overweight and obesity, we adopted the current Chinese national cutoff points as proposed by Ji and colleagues(supplement Table 1) (Ji 2005). Briefly, Ji and colleagues used the 2000 Chinese National Survey on Students Constitution and Health data that included 216,620 students with ages ranging from 7 to 18. The best fitting sex-age-specific curves were generated. This standard curves better fit the growth characteristics of Chinese children. As suggested, children with BMI between 85th and 95th percentile for their age and sex were considered overweight and those with BMI of 95th percentile and higher were considered obese. For example, 12-year old Chinese boys with a BMI of 21.0 were considered overweight and those with a BMI of 24.7 were considered obese. For 12-year old Chinese girls, the cut points were 21.9 and 24.5, respectively. The oldest subjects, 18 year olds, were treated as adults, and the adult cut points of BMI of 24 and 28 were applied for overweight and obese. For logistic regression modeling, we transformed BMI values into age and sex adjusted BMI percentiles, and then grouped them into tertile, representing high, medium and low BMI groups.
High Blood Pressure (HBP)
We adhered to the standard protocols of blood pressure measurement as proposed by the Fourth report of on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents (The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents 2004). Briefly, SBP (K1) and DBP (K5) were measured on right arm in a sitting position, using standard mercury sphygmomanometers that had been calibrated prior to the start of each fieldwork. Appropriate cuffs based on the circumference of upper arm were used. For each participant, two measures of SBP and DBP were obtained with a minimum of 5-minute rest between the two measures. All anthropometric and blood pressure measurements were obtained from the same visit, and all measurements were performed in school between 5:30–8:30pm. We classified children as having high blood pressure (HBP), if their SBP, DBP or both exceeded the age-sex specific 90th percentile cut points based on the national cutoffs (Mi et al. 2010). These cut points include prehypertension and hypertension.
Impaired Fasting Glucose (IFG)
Fasting blood glucose was obtained in a subset of children (n=765 Uyghurs; n=634 Hans; and n=896 Kazakhs) to follow up on our earlier report, which showed much lower prevalence of IFG in Kazakh adults than in other ethnic groups (Yan et al. 2005). For this assay, students were asked to fast over 12 hours. Fasting blood glucose was measured by one-touch glucose autoanalyzer (ACCU-Chek Advantage II Test Strips; Roche Diagnostics, Mannheim, Germany) between 8:30 a.m. and 9:30 a.m in school. The second drop of blood was used for testing after cleaning the finger by ethyl alcohol cotton swab and removing the first drop of blood. IFG was defined as fasting glucose ≥6.1 mmol/L.
Statistical analyses
For discrete traits, Pearson's chi-square test was applied, and Fisher's exact test was used when the number of subjects within a cell was five or under. For continuous traits, we first checked to see whether the traits satisfied the assumption of normality, and found all traits to conform to normality. Subsequently, we used ANOVA to compare trait values across three ethnic groups.
For multivariate modeling of continuous traits, we applied generalized linear modeling (GLM). To compare three ethnic groups, we used indicator variables for ethnicity, setting Hans as the reference group. To examine levels of blood pressure among ethnic groups, we first performed GLM models using all subjects, adjusting for age, BMI and height. However, when we studied fasting glucose, we applied the same model as above but did not include height as a covariate. We further compared the mean levels of blood pressure and glucose among ethnic groups after stratifying by four age groups (7–9, 9–12, 12–15 and 15–18 years old) to see how early the ethnic differences started. Subsequently, multivariate logistic regression was used to evaluate ethnic differences in HBP or IFG risks and the role of overweight. For this model, age, sex and height were also included in the model. All statistical analyses were carried out by STATA/SE software (Stata SE 11.0 for Windows, StataCorp LP, College Station, TX, USA). P-values less than 0.05 were considered statistical significant.
Oral assent by students and written consents from parents or guardians were obtained before data collection. This study protocols and all related assent and consent forms were reviewed and approved by the Institutional Review Board from Xinjiang Medical University.
Results
Table 1 presents the demographic and clinical data of the study population. Of 6,633 eligible subjects, 6,217 subjects (93.7%) completed the survey and provided full data for analysis, including 2,142 Uyghurs (34.5%), 2,078 Hans (33.4%) and 1,997 Kazakhs (32.1%). Forty-seven percent of the study participants were boys, and the mean age was 12.9 years (ranged 7–18 years).
Table 1.
Demographic and Clinical Characteristics of the Study Participants
| P | |||||
|---|---|---|---|---|---|
| Characteristics | Overall | Uyghurs | Kazakhs | Hans | value 3 |
| Total number of subjects (N) | 6217 | 2142 (34.5) | 1997 (32.1) | 2078 (33.4) | — |
| Sex | |||||
| Male | 2917 | 965 (45.1) | 918 (46.0) | 1034 (49.8) | 0.006 |
| Female | 3300 | 1177 (54.9) | 1079 (54.0) | 1044 (50.2) | |
| Age (year) Anthropometries (percentile) | 12.9±3.6 | 12.6±3.3 | 13.3±3.1 | 12.6±3.3 | <0.001 |
| BMI (kg/m2) | 18.2 ± 8.7 | 18.4±6.7 | 20.4±7.9 | 19.5±3.7 | <0.001 |
| Height (cm) | 150.3±16.7* | 146.7±16.9 | 152.4±17.0 | 152.0±15.7 | <0.001 |
| Obesity (n, %) | 1353(21.8) | 152(7.1) | 848(40.8) | 353(17.7 | <0.001 |
| Blood pressure1 | |||||
| SBP (mmHg) | 105 ±15 | 104±10 | 107±10 | 108±10 | <0.001 |
| DBP (mmHg) | 67 ±12 | 66±9 | 67±8 | 70±10 | <0.001 |
| HBP (n, %) | 1422(22.9) | 359(16.8) | 443(21.3) | 620(31.1) | <0.001 |
| Fasting | |||||
| Glucose2(mmol/L) | 4.7±0.6 | 4.8±0.6 | 4.5±0.5 | 5.0±0.6 | <0.001 |
| IFG (n, %) | 59(2.6) | 25(3.3) | 5(0.6) | 29(4.6) | <0.001 |
Blood pressure based on arm cuff measurement was measured twice and an average of the 2 measurements was used.
Fasting blood glucose (FBG) was measured on a randomly selected subset of 2,295 subjects (765 Uyghurs, 896 Kazakhs, and 634 Hans)
Univariate comparisons are presented.
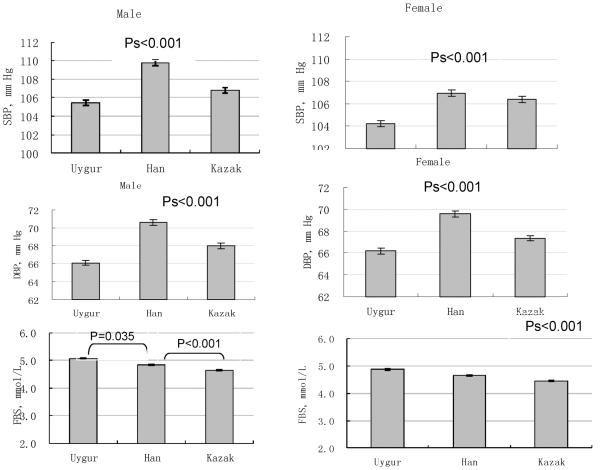
As shown in Table 1, Kazakh children were slightly older than Uyghur and Han children (13.3 vs. 12.6 vs. 12.6 years, respectively), and had the highest mean BMI and height, followed by Han and Uyghur children (Ps<0.001). Uyghurs had the lowest mean blood pressure (P<0.001) and Hans had the lowest mean fasting glucose (P<0.001). The prevalence of obesity, HBP and IFG significantly differed by ethnicity. Kazakhs children had the highest proportion of obesity and Han children had the highest proportion of IFG than the other two ethnicities (obesity: 40.8% vs 17.7% and 7.1 % for Kazakhs, Han, and Uyghurs; IFG: 4.6%, 3.3% and 0.6% for, Han, Uyghur and Kazakhs), however, the highest prevalence of HBP was seen in Hans, followed by Kazakhs and Uyghurs (31.1% vs. 21.3% vs. 16.8%). Compared with Uyghurs, Kazakhs had more obese (40.8% vs 7.1%), more HBP (21.3% vs 16.8%) and less IFG (0.6% vs 3.3%), differences were significant (Ps<0.001). Further analyses by gender showed that (data not shown), among boys, approximately one-third of Hans had HBP followed by Kazakhs and Uyghurs (31.0% vs. 19.7% vs. 15.4%, respectively). For IFG, Hans had the highest prevalence closely followed by Uyghurs and by Kazakhs (5.1% vs 5.0% vs 0.5%, Ps<0.001for overall and between-ethnic differences), the same pattern was observed for girls (4.0% vs. 1.9% vs. 0.7%, respectively). Kazakh children had the highest prevalence of overweight (38.7% for males and 47.6% for females) and yet they had the lowest prevalence of IFG among three ethnic groups. Figure 1 presents the differences in mean levels of SBP, DBP and fasting glucose among the three ethnic groups by sex after adjusting age, height (for blood pressure only) and BMI. Among three ethnic groups, Han boys and girls had the highest SBP and DBP levels, followed by Kazakh boys and Uyghurs boys. On the other hand, Kazakh children had the lowest fasting glucose levels (P values<0.001 for the two comparisons against Hans). For fasting glucose levels, Uyghur children had the highest fasting glucose levels, followed by Han children, and then by Kazakh children. At the same time, the Uyghur children had the lowest SBP and DBP levels. These differences were significant.
Figure 1. The mean SBP, DBP and fasting glucose of Han, Uyghur and Kazakh boys and girls after adjustment for age, BMI and height (for blood pressure only).
Figure 1 presents the adjusted means and standard errors (SE) of systolic blood pressure (SBP), diastolic blood pressure (DBP) and fasting glucose levels among three ethnic groups (i.e., Uyghurs, Hans and Kazakhs) separately for boys and girls. The mean values of SBP and DBP were adjusted for age, height and BMI. For fasting glucose, age and BMI were adjusted. Pair-wise ethnic comparisons were made using Han children as the reference group. All pair-wise comparisons between two ethnic groups were significant at p<0.05. When both pair-wise comparisons (Uyghurs vs. Hans and Kazakhs vs. Hans) were significant at p<0.001, only one P value of 0.001 was presented above each graph.
One possible explanation for the Uyghurs children to have a low prevalence of HBP and a high prevalence of IFG may be that they have a low prevalence of obesity but they may have a low threshold for physiological effect of obesity. This may be relevant as earlier reports have shown that certain Asian populations may require low cutpoints for obesity (Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies 2004). Our analysis supports this possibility. We observed that the role of BMI on blood pressure differ by ethnicity (P-values ranges from <0.001 to 0.011). We note that, while the effect of BMI on blood pressure differed by ethnicity; however, it is not the true for fasting glucose levels (for BMI, P=0.304 for males and P=0.135 for females; for weight status, P=0.677 for males and P=0.766 for females).
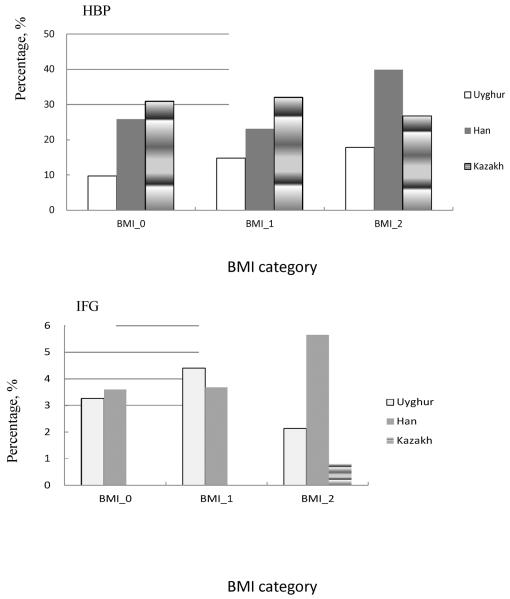
To evaluate further whether excessive body weight explains the ethnic difference in the prevalence of HBP and IFG in this pediatric population, we compared the prevalence of HBP and IFG among ethnic groups after stratifying by BMI tertile (Figure 2). For HBP, Kazakh children had the highest prevalence of HBP in the low and middle BMI groups, but not in the high BMI group. For all three BMI groups, Uyghurs had the lowest prevalence of HBP. For IFG, Kazakh children had the lowest prevalence. Specifically, none of the Kazakh children in the low and medium BMI groups had IFG, and only those in the high BMI group had a low prevalence. As shown in Figure 2, both Uyghur and Han children had a similarly high prevalence of IFG compared with Kazakh children, However, in the highest BMI category, Uyghurs children were one-half as likely as Han children to have IFG. Interestingly, in the highest BMI group, Han children had the highest rate of both HBP and IFG, suggesting that Han children may be less tolerant of obesity compared with Uyghur and Kazakh children.
Figure 2. Prevalence of high blood pressure (HBP) and impaired fasting glucose (IFG) by BMI categories.
Figure 2 presents the ethnic difference in the prevalence of high blood pressure (HBP) and impaired fasting glucose (IFG) by three BMI categories. BMI_0 represents the low level BMI including BMI of 0 to the 33th percentile; BMI_1 represents the mid level BMI including BMI percentile between the 33rd and 66th percentiles, and BMI_2 represents the high level BMI including BMI ≥66th percentile. P<0.05 was deemed significant. All comparisons were made after adjusting for age and sex, and Bonferroni correction was applied to correct for multiple testing that α=0.015 was used.
To determine how early ethnic differences in levels of blood pressure and fasting glucose may have started, we compared mean levels of blood pressure and fasting glucose by ethnicity, age and sex (Table 2). Ethnic differences in levels of SBP in girls (Kazakhs vs. Hans, p=0.001) and DBP (Uyghurs vs. Hans, P=0.012 for boys and P=0.003 for girls) started as early as 7–9 years of age, and BMI has a significant modifying effect. For certain age groups, namely age groups 10–12 and 16–18 among girls, levels of SBP did not differ between Kazakh and Han children. Similarly, ethnic differences in fasting glucose levels may have started as early as 10–12 years of age (Kazakhs vs. Hans both in both genders) and the observed differences were particularly pronounced for Kazakh vs. Han children. For these comparisons of IFG, BMI was not a significant modifier of ethnic differences.
Table 2.
Ethnic differences in SBP, DBP and fasting glucose by age group
| Variables | Age | Boys |
Girls |
||
|---|---|---|---|---|---|
| group | Uyghurs vs. Hans | Kazakhs vs. Hans | Uyghurs vs. Hans | Kazakhs vs. Hans | |
| SBP | 7–9 1,2 | 0.168 | 0.207 | 0.032 | 0.001 |
| 10–121,2 | 0.020 | 0.001 | 0.041 | 0.899 | |
| 13–151,2 | <0.001 | <0.001 | <0.001 | <0.001 | |
| 16–181 | <0.001 | <0.001 | 0.816 | 0.757 | |
| DBP | 7–9 2 | 0.012 | 0.967 | 0.003 | 0.627 |
| 10–12 | <0.001 | <0.001 | <0.001 | 0.001 | |
| 13–152 | <0.001 | 0.013 | <0.001 | 0.155 | |
| 16–181 | 0.090 | <0.001 | 0.001 | <0.001 | |
| Fasting | 7–9 | 0.739 | <0.001 | 0.886 | <0.001 |
| glucose | 10–12 | 0.827 | <0.001 | 0.750 | <0.001 |
| 13–151 | 0.672 | <0.001 | 0.361 | <0.001 | |
| 16–182 | 0.063 | <0.001 | <0.001 | <0.001 | |
Notes:
P-values are presented. P<0.05 was deemed significant difference.
Indicator variable was used for ethnicity with Han being the reference group
BMI was a significant covariate in the model for boys
BMI was a significant covariate in the model for drls
Discussion
The current study of multi-ethnic Chinese population (Hans, Uyghurs and Kazakhs) reports that Uyghur children had the lowest prevalence of HBP and mean levels of SBP and DBP, while Kazakh children had the lowest prevalence of IFG, and levels of fasting glucose, independent of BMI. In the highest BMI group, however, Han children had the highest HBP and IFG, suggesting that Han children may have low tolerance for obesity. The observed ethnic differences in SBP, DBP and FBG among children may have started as early as 7–9 years of age, and the observed differential patterns for HBP and IFG by ethnicity and the role of obesity remained consistent with the patterns observed in the adult population from the same geographic region (Yan et al. 2005).
Racial or ethnic differences in obesity, hypertension and diabetes have been widely reported by a number of studies in adults as well as in pediatric populations (McBean et al. 2004; Whincup et al.; Harding et al. 2008; Cruickshank et al. 2005). In China, differences in the prevalence of hypertension, as well as in diabetes, have been found between Uyghur, Kazakh and Han adult populations (The Chinese Task Force of National Survey of Hypertension. The prevalence, awareness, treatment and control of hypertension in China: The report of national sampling survey of hypertension. 1999; Yan et al. 2005). However, it is unclear as to whether the differences are present in pediatric populations or not; or if such differences exist, it has not been quantified as to how early the observed differences start. This is the first study to provide evidence that the ethnic differences in levels of blood pressure and glucose vary in children as young as 7–9 years of age. The trends of ethnic differences in HBP and IFG between Kazakh and Uyghur children observed in this study are similar to the earlier findings in adults by Yan and colleagues (Yan et al. 2005). The authors showed that ethnic differences in HBP and IFG levels among Uyghur and Kazakh adults from the same region were profound. In that study, Uyghur adults were more likely to have higher diabetes risk (IFG rate) but were less likely to have hypertension, even after adjusting for BMI, age and sex. In contrast, Kazakhs had a higher prevalence of hypertension, but had a lower prevalence of diabetes. Taken together, the differences in HBP and IFG risks in children of different ethnic groups cannot be explained by obesity alone.
Are the racial/ethnic differences in the prevalence of diabetes or hypertension in adults or in children associated with differences in obesity? Multiple studies illustrate the complexity involving the relations among obesity, HBP and IFG in different ethnic groups. A cross-sectional study by Rosner, Bernard and colleagues (Rosner et al. 2000) found that at lower levels of BMI, African Americans were more likely to have high blood pressure and hypertension compared with European Americans. However, at the highest levels of BMI, European Americans had a higher prevalence of hypertension than African Americans did (Rosner et al. 2000). In a subsequent study, they found that the ethnic difference in SBP and DBP levels could not be completely explained by obesity (Rosner et al. 2009), and they suggested that the differences in disease risks were explained by the differences in body size. Similarly, in our study, the ethnic differences in risk for HBP and IFG risk were independent of obesity (i.e., BMI percentile). O'Brien and colleagues found a higher prevalence of diabetes in African American adults than in European American adults, and this observed difference was not explained by differences in obesity prevalence (O'Brien et al. 1989). The CHASE study found that the emergence of ethnic differences in precursors of diabetes (including fasting glucose) between children of South Asian ancestry and European white ancestry were not explained by differences in relative adiposity (Whincup et al. 2010). In the US, where the prevalence of high BMI has not changed substantially in the past decade, several studies showed that the increasing trend of hypertension has been controlled, whereas the prevalence of type 2 diabetes has not declined or plateaued (Ogden, Carroll, and Flegal 2008; Ogden et al.; Lee, Brancati, and Yeh; Din-Dzietham et al. 2007). Taken together, these findings suggest that, obesity may play a more significant role in hypertension than in type 2 diabetes.
The current study has some limitations. First, this cross-sectional study does not allow us to evaluate the temporal relations among obesity and the two outcomes: hypertension and impaired fasting glucose. Second, our measures of the risk for diabetes were limited to fasting glucose levels and the classification of impaired fasting glucose, and have not performed further oral glucose tolerance tests or insulin resistance indices. Third, blood pressure measurements (average of twice measurement at the same visit) based on one school visit, and it was not possible to evaluate within-individual variations across multiple readings. Thus the estimation of HBP prevalence in the three ethnic groups is only appropriate for ethnic comparisons within the current study, and caution is warranted when comparing against other published studies that may have used different protocols for blood pressure measures.
The current study calls to attention early monitoring of obesity and related complications, particularly hypertension and diabetes indicators. Moreover, tolerance for obesity differs by ethnicity and these differences have clinical consequences related to elevated risks for diabetes and hypertension. Thus, early management of obesity and other known disease-related environmental factors in high risk pediatric population may lead to reduction in disease risks in children, and may provide further benefits when they reach adulthood.
Supplementary Material
Acknowledgments
This research was supported in part by the National Science Foundation of China [Grant number NSFC 30960329 to W. Yan]. The authors thank Jun Cui and colleagues at the Student Health Care Center of Urumqi; Y. Zhao, L. Dai, and J. Dai from Xinjiang Medical University and nurse candidates from the Nursing School of Altay for their assistance with the fieldwork and data entry. J. H. Lee was partly supported by NIH R01 MH084995.
Sources of financial support: This research was supported by the National Science Foundation of China [grant number NSFC 30960329], Children's Hospital of Fudan University, and Xinjiang Medical University.
Abbreviations
- SBP
systolic blood pressure
- DBP
diastolic blood pressure
- HBP
high blood pressure
- IFG
impaired fasting glucose
- SD
standard deviation
- SE
standard error.
Footnotes
The authors declare no conflicts of interest.
Contributors W.L. Yan designed and conducted the study, supervised statistical analysis, drafted and edited the manuscript.
X.S. Li participated the field work, contributed to data analysis, and edited the manuscript.
Q Wangb, Y. D. Huangb, W. G. Zhangb, X. H. Zhaib, and C. C. Wangb participated in data acquisition and field work, and reviewed and edited the manuscript.
J. H. Lee contributed to statistical analysis, editing and the final language reviewing of the manuscript.
REFERENCES
- Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies Lancet. 2004;363(9403):157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- The Chinese Task Force of National Survey of Hypertension. The prevalence, awareness, treatment and control of hypertension in China: The report of national sampling survey of hypertension Chin J Hypertens. 1999;(3 (suppl)):14–18. [Google Scholar]
- Cruickshank JK, Mzayek F, Liu L, Kieltyka L, Sherwin R, Webber LS, Srinavasan SR, Berenson GS. Origins of the “black/white” difference in blood pressure: roles of birth weight, postnatal growth, early blood pressure, and adolescent body size: the Bogalusa heart study. Circulation. 2005;111(15):1932–7. doi: 10.1161/01.CIR.0000161960.78745.33. [DOI] [PubMed] [Google Scholar]
- Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116(13):1488–96. doi: 10.1161/CIRCULATIONAHA.106.683243. [DOI] [PubMed] [Google Scholar]
- Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103(6 Pt 1):1175–82. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- Harding S, Teyhan A, Maynard MJ, Cruickshank JK. Ethnic differences in overweight and obesity in early adolescence in the MRC DASH study: the role of adolescent and parental lifestyle. Int J Epidemiol. 2008;37(1):162–72. doi: 10.1093/ije/dym252. [DOI] [PubMed] [Google Scholar]
- Ji CY. Report on childhood obesity in China (1)--body mass index reference for screening overweight and obesity in Chinese school-age children. Biomed Environ Sci. 2005;18(6):390–400. [PubMed] [Google Scholar]
- Lee JW, Brancati FL, Yeh HC. Trends in the prevalence of type 2 diabetes in Asians versus whites: results from the United States National Health Interview Survey, 1997–2008. Diabetes Care. 34(2):353–7. doi: 10.2337/dc10-0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBean AM, Li S, Gilbertson DT, Collins AJ. Differences in diabetes prevalence, incidence, and mortality among the elderly of four racial/ethnic groups: whites, blacks, hispanics, and asians. Diabetes Care. 2004;27(10):2317–24. doi: 10.2337/diacare.27.10.2317. [DOI] [PubMed] [Google Scholar]
- Mi J, Wang TY, Meng LH, Zhu GJ, Han SM, Zhong Y, Liu GS, Wan YP, Xiong F, Shi JP, Yan WL, Zhou PM. Development of blood pressure reference standards for Chinese children and adolescents. Chin J Evid Based Pediatr. 2010;5(1):4–14. [Google Scholar]
- O'Brien TR, Flanders WD, Decoufle P, Boyle CA, DeStefano F, Teutsch S. Are racial differences in the prevalence of diabetes in adults explained by differences in obesity? Jama. 1989;262(11):1485–8. [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. Jama. 303(3):242–9. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. Jama. 2008;299(20):2401–5. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- Rosner B, Cook N, Portman R, Daniels S, Falkner B. Blood pressure differences by ethnic group among United States children and adolescents. Hypertension. 2009;54(3):502–8. doi: 10.1161/HYPERTENSIONAHA.109.134049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosner B, Prineas R, Daniels SR, Loggie J. Blood pressure differences between blacks and whites in relation to body size among US children and adolescents. Am J Epidemiol. 2000;151(10):1007–19. doi: 10.1093/oxfordjournals.aje.a010129. [DOI] [PubMed] [Google Scholar]
- Sorof JM, Poffenbarger T, Franco K, Bernard L, Portman RJ. Isolated systolic hypertension, obesity, and hyperkinetic hemodynamic states in children. J Pediatr. 2002;140(6):660–6. doi: 10.1067/mpd.2002.125228. [DOI] [PubMed] [Google Scholar]
- Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: a working group report from the National High Blood Pressure Education Program. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents Pediatrics. 1996;98(4 Pt 1):649–58. [PubMed] [Google Scholar]
- Whincup PH, Nightingale CM, Owen CG, Rudnicka AR, Gibb I, McKay CM, Donin AS, Sattar N, Alberti KG, Cook DG. Early emergence of ethnic differences in type 2 diabetes precursors in the UK: the Child Heart and Health Study in England (CHASE Study) PLoS Med. 7(4):e1000263. doi: 10.1371/journal.pmed.1000263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whincup PH, Nightingale CM, Owen CG, Rudnicka AR, Gibb I, McKay CM, Donin AS, Sattar N, Alberti KG, Cook DG. Early emergence of ethnic differences in type 2 diabetes precursors in the UK: the Child Heart and Health Study in England (CHASE Study) PLoS Med. 2010;7(4):e1000263. doi: 10.1371/journal.pmed.1000263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Work Group of Physical Fitness and Health Surveillance of Chinese School Students . Report on the Physical Fitness and Health Surveillance of Chinese School Students. Beijing: 2007. [Google Scholar]
- Yan WL, Zheng YJ, Wu J, Chen SF, Ti XK, Li L, Liu XR. Ethnic differences in body mass index and prevalence of obesity in school children of Urumqi City, Xinjiang, China. Biomed Environ Sci. 2006;19(6):469–73. [PubMed] [Google Scholar]
- Yan W, Yang X, Zheng Y, Ge D, Zhang Y, Shan Z, Simu H, Sukerobai M, Wang R. The metabolic syndrome in Uygur and Kazak populations. Diabetes Care. 2005;28(10):2554–5. doi: 10.2337/diacare.28.10.2554. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.