Abstract
Background
Although the presence of an electronic health record (EHR) alone does not ensure high quality, efficient care, few studies have focused on the work of those charged with optimizing use of existing EHR functionality.
Objective
To examine the approaches used and challenges perceived by analysts supporting the optimization of primary care teams’ EHR use at a large U.S. academic healthcare system.
Methods
A qualitative study was conducted. Optimization analysts and their supervisor were interviewed and data was analyzed for themes.
Results
Analysts needed to reconcile the tension created by organizational mandates focused on the standardization of EHR processes with the primary care teams’ demand for EHR customization. They gained an understanding of health information technology (HIT) leadership’s and primary care team’s goals through attending meetings, reading meeting minutes, and visiting with clinical teams. Within what was organizationally possible, EHR education could then be tailored to fit team needs. Major challenges were related to organizational attempts to standardize EHR use despite varied clinic contexts, personnel readiness, and technical issues with the EHR platform. Forcing standardization upon clinical needs that current EHR functionality could not satisfy was difficult.
Conclusions
Dedicated optimization analysts can add value to health systems through playing a mediating role between HIT leadership and care teams. Our findings imply that EHR optimization should be performed with an in-depth understanding of the workflow, cognitive, and interactional activities in primary care.
Keywords: primary care, electronic health records/utilization, computerized medical record systems, EHR optimization, EHR acceptance
INTRODUCTION
In the United States, there is increasing recognition that the presence of an electronic health record (EHR) does not assure high quality, efficient care.1–4 Understanding how EHRs are used within the clinical context is critical to achieving improvements in care.5,6 The 2009 American Reinvestment and Recovery Act contained significant incentives for EHRs in its Health Information Technology for Economic and Clinical Health provisions.7 These incentives require clinicians and hospitals to demonstrate the use of certified EHR technology in ways that require significant changes in care processes. Additionally, in the past five years, there has been an emphasis on the appropriate use of information technology as a key component of practices becoming certified patient-centered medical homes.8 Medical homes are a term in the United States used to describe a model for primary care where care is coordinated and patients receive comprehensive, understandable care when and where they need it.9,10 In response to these forces, health information technology (HIT) adoption has increased in the past few years.11,12 A growing literature is providing in-depth insights into the role of the EHR in improving the quality of health care13–15 and barriers to its adoption.16–24 These research findings help decision-makers understand how EHRs can transform health care services and how organizations can best support EHR adoption and use among clinicians and staff. Studies also document wide variation in practices’ use of EHR functionality (e.g., electronic prescribing, patient problem lists)21 and significant physician time costs in learning effective ways to use an EHR.22
Few studies to date, however, are focused on improving the use of existing functionality within an EHR (i.e., EHR optimization) after implementation. In particular, study of this support in the ambulatory care setting is limited.25 One comparative study found that sites that used the EHR most successfully spent time on optimization, which was defined as dedicating ongoing resources for improving use of EHR functionality beyond the period when the EHR was implemented.20 Increased understanding of how organizations can support and improve EHR usage after implementation is a critical step towards achieving the EHR’s potential as a tool for facilitating high quality, efficient care.
The objective of this exploratory study was to examine the approaches to primary care EHR optimization used by optimization analysts working for a large academic health care system in the Midwestern United States. We also describe the perceived goals and challenges for optimization with the aim of assisting other organizations to design and implement EHR optimization programs for primary care teams.
METHODS
Organizational Context
This study was conducted as part of a formal evaluation of a primary care team building and quality improvement initiative based on the Dartmouth Macro-Meso-Microsystem approach.26–34 Training primary care teams to make full use of technology is one of the organizational goals for this initiative. Two optimization analysts were funded to work (1.8 full-time equivalent) with participating primary care teams in order to increase their competency in using the EHR. Twenty-seven primary care teams had participated in this initiative at the time of data collection.
Primary care teams consisted of physicians, medical assistants, nurses, receptionists, and occasionally nurse-practitioners, physician assistants, radiology, pharmacy, and laboratory staff. The health system uses Epic Systems’ EpicCare™ (locally called Health Link) as its EHR. This EHR was implemented in stages across primary care from 2004 to 2012.
Analysts focused on optimization activities that supported mastery of EHR functionality that was currently available rather than developing new functionality.
Participants and Procedures
First, a joint in-person interview was conducted with these two primary care optimization analysts. These individuals have over ten years of experience with EHR implementation and training, and one had a prior clinical background. A semi-structured interview guide was used to focus the discussion, and conversation between the participants was evoked. Next, a separate in-person interview was conducted with the analysts’ supervisor, an organizational HIT leadership team member. Two researchers conducted each session, one serving as the moderator to ensure that the session progressed smoothly and the other taking field notes and ensuring coverage of all topics. Sessions were recorded, transcribed verbatim, and imported into NVivo 935 for open coding and text retrieval.36
Analysis
Guided by an immersion/crystallization technique,36 three researchers first independently immersed themselves in the data by examining and coding each transcript in. The researchers then met to discuss this coding and developed a codebook, which facilitated the identification of future meaningful transcript segments. The researchers then independently used the codebook to revisit the transcripts and develop categories that described bigger concepts. They then jointly discussed these larger codes to identify patterns in the data, and validated these patterns against the original transcripts. Multiple iterations of this process continued until the team members reached consensus upon the themes that emerged.
Procedures to Establish Validity
The researchers involved in data analysis were from family medicine (NP), education (WY), and liberal arts (ZK) backgrounds, thereby allowing for multidisciplinary perspectives through discussion and minimizing disciplinary bias in data interpretation. The lead author also periodically presented the ongoing data analysis to a larger multidisciplinary qualitative research group for further discussion and feedback.
RESULTS
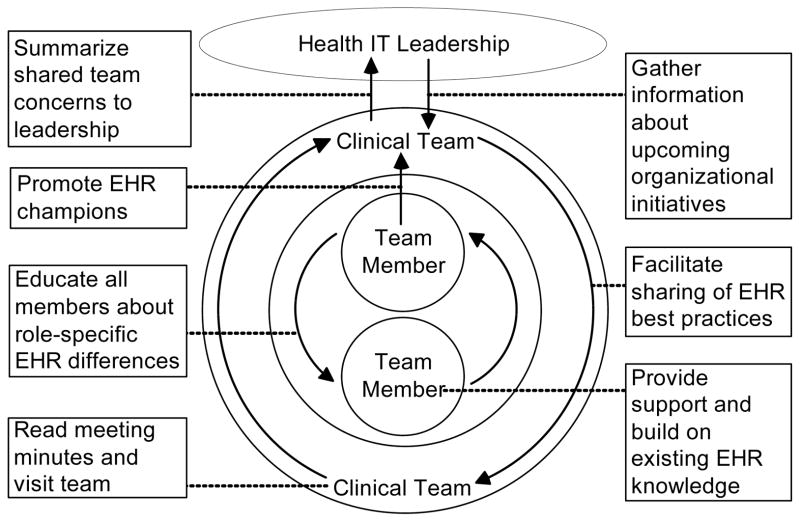
Overall, as shown in Figure 1, optimization analysts served as mediators between HIT leadership and primary care teams and performed various activities to bridge these organizational levels.
Figure 1. Analyst Bridging Activities Between and Within Organizational Levels to Achieve Optimization.
Dashed lines indicate the level at which activities occur
Lines capped with an arrow indicate the directionality of these activities, when applicable
Goals and Approaches when Working with HIT Leadership
Table 1 summarizes the analysts’ goals and approaches when working with HIT leadership.
Table 1.
Optimization Analysts’ Goals and EHR Optimization Approaches When Working With HIT Leadership
| Goals | Approaches with HIT Leadership |
|---|---|
| Develop a thorough understanding of planned system-wide EHR initiatives |
|
| Align team’s EHR use with current or planned organizational operations |
|
| Facilitate organizational efficiency when deciding upon changes to the EHR |
|
Analysts tried to understand upcoming system-wide initiatives by attending strategic leadership meetings. They augmented this understanding with informal conversations. They also met regularly with their supervisor to develop a strategy when a team’s EHR use directly conflicted with current or planned operations. This supervisor involved operational leadership and clinic managers in the troubleshooting process if additional assistance was needed:
We have to talk to different people and [primary care] teams and initiatives to make sure that our teams are doing the correct work and to make sure that they’re not wasting time coming up with a process that is only going to be undone or not organizationally supported.
For consistency, the organization changes the EHR only for an entire specialty at once, rather than by individual request. Therefore, analysts let leadership know about shared technology challenges that clinical teams faced so that solutions could be considered and applied across the group.
Goals and Approaches when Working with Primary Care Teams
Table 2 summarizes the analysts’ goals and approaches with primary care teams.
Table 2.
Optimization Analysts’ Goals and EHR Optimization Approaches When Working With Primary Care Teams
| Goals | Approaches with Primary Care Teams |
|---|---|
| Target EHR optimization to meet teams’ needs |
|
| Align EHR requests with current or planned organizational operations |
|
| Improve understanding of existing EHR functionality |
|
| Develop shared understanding among team members |
|
| Spread best practices that align with organizational standards |
|
Analysts received diverse requests for assistance due to variations in each clinical team’s situation. They obtained a further understanding of teams’ needs by reading weekly team meeting minutes, and visiting teams to observe EHR use. Analysts perceived that their efforts were better received if they introduced new concepts of how the EHR could be utilized to facilitate the team’s daily work:
We’ve been working with [the team’s] project[s] and their gaps and their work. Their world. We understand what they’re trying to do and we really help them with their questions and not [just] give them a general Health Link optimization.
To achieve the goal of aligning teams’ EHR usage with organizational standards, analysts helped teams understand the rationale for why certain changes could or could not be made. Then, a frequently used strategy involved redirection towards developing a process that would be organizationally supported and could achieve the same goal. The analysts also tried to customize the way they presented upcoming organizational EHR initiatives to primary care teams to demonstrate how these changes reflected specific EHR functionality needs that a team had expressed in the past.
Primary care teams were generally unaware of the full functionality of the EHR, and this often led to inefficient usage. Therefore, another goal was to optimize use of current EHR functionality by increasing awareness of existing features. For example, when a team thought it needed to create a new flow sheet, analysts directed them to an existing EHR tool that would also improve workflow:
It seemed like a lot of time we were going, “So you know you can do that, this is where it is.”
Analysts tried to train each team member to have a similar EHR knowledge base. Realistically, however, analysts worked more closely with certain team members who were willing or had the time to learn in the hope that they would become champions who would promote the optimal use of the EHR across the team.
Analysts perceived that the team members found it difficult to devote time to EHR optimization due to the busy nature of primary care. Therefore, they provided EHR optimization training activities in multiple ways. They answered questions virtually using e-mail in conjunction with EHR screen shots. However, they preferred providing in-person support because they perceived it led to better recall afterwards. They also provided group learning opportunities, such as lunch-and-learn demonstrations focused on a specific functionality within the EHR, and overall refresher courses for team members needing additional support. One specific optimization activity that was performed in person was developing a shared understanding of how team members had different screen views within the EHR because of their professional role:
And having them understand what an [medical assistant] sees is different from reception. So it’s facilitating that communication. A lot of it was, “Okay, if you type it in here, reception is going to see it here.”
Lastly, as the individuals that were able to see what all the teams were doing, optimization analysts found themselves as a conduit for information sharing between primary care teams.
Whereas, we’re the people that read everybody’s minutes, so we go, “Oh, someone else was talking about this....why don’t you contact them and look at their work?”
Challenges Experienced When Attempting Optimization
Analysts experienced multiple challenges when trying to optimize primary care teams EHR usage as described below.
Standardization versus Customization Challenge
A major responsibility was to help teams use the EHR in a consistent way. However, analysts perceived tension between EHR decisions being made by top HIT leadership and changes in grassroots team empowerment to improve clinical care processes. The analysts perceived an unintended consequence of empowering team members through the Microsystems approach was that it allowed teams to refuse organizational requests to test processes that were being considered for dissemination across the organization.
They’ve [the teams] got power to do what they want. The Microsystems [program] gave them that power, and as long as they keep meeting they can still have the power. We’re kind of running into this where top-down, we want them to test things and pilot, but they say, “No thanks, we don’t want to.”
A particular challenge was when teams wanted to use an EHR tool to improve clinical care before HIT leadership at the organization felt ready to dedicate the appropriate resources to support this work. For example, teams were very excited develop new ways to use My Chart, a portal that allows patients direct access to portions of their own EHR and provides a means of electronic communication with the primary care office. In one instance, a team wanted to put the form used to collect a medical history from the patient into My Chart instead of handing it to patients when they came into the office. However, the organization wanted to make sure that anything that was placed into My Chart would be applicable across all patients. It also didn’t want to spend resources on building a form that the EHR vendor might be providing in a future update. So the analysts were put in the position of explaining why this couldn’t be done.
So everyone is diving towards My Chart, going “We want this history form to be done this way, wouldn’t that be cool? Why do we have to give to them [the patients]?” And it’s like, well, we can do that soon, but there is so much build and development to get that right....Knowing that we’re not going to put a lot of work into a form that we know very possibly by the end of next year could be available on My Chart [through the EHR vendor].
Challenge from Varied Physical and Cultural Contexts of Clinics
Each clinic has a unique culture, with differences across patient populations, staffing needs, and governing regulations. The primary care clinics are owned and managed by three separate entities that have different legal, financial, and governance structures. Therefore, an organizationally mandated standard process might not necessarily benefit a specific clinic in gaining time efficiencies or in facilitating their workflow.
Let’s think of [Clinic A] or [Clinic B]. They’re really small town and they know their patients and it’s hard for them to understand why would we be doing a learning assessment? We’ve known this patient for years, as opposed to [Clinic C], which is a big clinic, and they may have a lot of transient patients who come in and don’t have that same patient base where they really don’t know their patients quite as well.
[Certain] clinics have to run under [Joint Commission on Accreditation of Healthcare Organizations (JCAHO)] regulations. Our other clinics don’t. So some standards have been put into place, like pain scale and learning assessment for [these] clinics because that is a JCAHO regulation that they are required to document on each visit.
Challenges from Operational Issues
Analysts described the challenge of the teams’ lack of compensated time for EHR optimization within the clinic day.
If they don’t have time allowed — if it’s being put on top of their work, if they don’t have the time to be able to do the stuff that they do outside their meeting, you’re not going to get engagement.
They were constrained by a limited organizational budget for more personnel.
We have a schedule of how we will hit each clinic so we have to go clinic by clinic, so it is somewhat of a slow process. But, we only have so much budget, also. So, obviously, it would always be nice to go faster if we could get more people.
Finally, there was a perceived lack of clarity in the analysts’ initial job definition, making its scope unclear.
That was challenging because it was hard for [Optimization Analyst 1] and [Optimization Analyst 2] because they really weren’t sure what they were supposed to do. Were they supposed to sit at the team meeting?
Challenges of Personnel Readiness
Analysts perceived a challenge with teaching team members to do something differently, saying, “It’s a lot of work. It’s a lot of old habits we’re trying to break.” They thought this challenge was more present with physicians’ and nurses’ reluctance to admit knowledge gaps as opposed to medical assistants and receptionists.
Now when we’re looking at standardization across all of the organization, the providers will need to start entering their own orders. That’s definitely an area where we are going to have complaints. They are not liking the standardization because we are requiring them to do something that they didn’t have to do previously, maybe don’t want to do.
Analysts perceived nurses, in particular, to be the most challenging group to optimize due to a lack of related technological knowledge:
A lot of the time the RNs just don’t pick up. When we first trained them they were the worst part of the group because they are clinical, they are not typists. They didn’t understand the concept, all they wanted to do was nursing. So they were the hardest, many times, to get using the functionality, just because it was so foreign to them.
They’ll tell you, “I’m a nurse, I’m not a computer person.”
Challenges from EHR Technical Issues
Inconsistency and inefficiency within the EHR software frustrated team members:
“Epic software isn’t always consistent. In one place, it might say “close” and it is a blue square and in the next set of functionality it might say exit and it is a red triangle or something. So there’s no consistency in that. Providers have complained about that.”
“One of the big things is providers hate how many clicks it takes to do something – they don’t want to hit six buttons to do something.”
Future Optimization Plans
The organization is piloting the combination of clinical education and EHR optimization training as part of an initiative that is developing a standardized workflow for clinics.
Previously in the past, a new staff member came in, they had clinical education – you know, how you take a blood pressure, how do you use the scales correctly, things like that – that was all separate and then they would have separate days of how to use the EHR. So we never, we really didn’t work together.
It’s not always just how to enter it or where to enter it, but how to get the best information – the most accurate – and get it in the system.
More optimization analysts are being hired as part of this initiative. These analysts’ expected duties include observing and analyzing teams’ current workflow, identifying training needed before a standardized workflow can be implemented, and providing on-site assistance and training to teams. Over time, this process is expected to be expanded across all primary care clinics and into specialty care clinics.
DISCUSSION
Principal Findings
We found that analysts played a mediating role between HIT leadership and primary care teams and were constantly dealing with issues arising at the interface between these groups. They worked within the organizational goals for EHR optimization, and tailored their approaches on primary care teams’ needs. The analysts needed to reconcile the tension created by organizational mandates focused on standardization with the primary care teams’ demand for EHR use customization. They did this by trying to stay abreast of and realign teams’ EHR use with upcoming organizational initiatives and alerting HIT leadership of concerns shared across primary care teams. They also customized EHR training by explaining existing options that met team member’s needs, and thereby deflected requests for new functionality. Other challenges to optimization were related to the varied physical and cultural contexts in which clinics existed, operational issues (e.g., time and budget), personnel readiness for technology adoption, and technical issues with the EHR software.
Implications of the Findings
It is critical to understand how organizations can support and improve EHR use after implementation in order for the EHR to achieve its potential as a tool for facilitating high quality care.5,37 This study poses the question about how to organize EHR optimization activities. The analysts in charge of EHR optimization clearly experience a range of conflicting demands with regard to training and education (e.g., providing in-person support versus responding to requests via email), and organizational expectations versus requests and expectations from primary care teams. The analyst’s position is, therefore, subject to role conflict, a well-known stressor.38 It is important to ensure that individuals in this position have the organizational support, tools, and resources necessary to accomplish their goals effectively and efficiently.
We discovered a tension between standardization and customization that was embedded within the EHR optimization process. For the organization, standardization is perceived as efficient, and leading towards the goal of improving the quality of care. For primary care teams, however, standardization might result in unnecessary documentation for their clinical context. Teams desired customized functionality to improve the efficiency of care. This conflict raises a debate on whether standardization truly should be weighted more than customization in terms of efficiency, and whether it can lead to meaningful optimization without buy-in or direction from the end user primary care teams. Existing research indicates a key to successful EHR implementation involves organizational support for an interactive, flexible process of planning.39,40 Therefore, one possible solution to this tension is to have organizational support for customization in certain dimensions. By extension, it may be also critical to involve all stakeholders in planning EHR optimization in order to understand how EHR usage can best fit in with or improve the existing organizational structure and culture.
The analysts’ recognition of the conflict between organizational standardization and desired team customization is based on some real and quite fundamental issues with EHR use in primary care. In the initial optimization process it appeared that the analysts organized, as perhaps they must, their training around the question of “How do we get the users to use the EHR properly?” rather than starting with the larger question of “How can we utilize the EHR to improve the quality and efficiency of care?” Thus, the data collected from the analysts in this study raises other broader (and generally unaddressed) questions about implementation as well. The implementation of EHRs has generally been done in the absence of an in-depth understanding of the workflow, cognitive, and interactional activities in primary care,5 much less the support needed to accomplish these tasks.41 The tasks in primary care have been enumerated,42 but have not been incorporated into EHR design.6 Training may be able to make up for poor design or implementation goals, but only to a point. Forcing EHR standardization upon clinical needs that EHR functionality cannot satisfy is counterproductive. An understanding of the contexts of use and having the EHR implementation be responsive to these contexts along with end users’ needs and values appears to be crucial for successful EHR optimization.
Comparison with the Literature
Prior literature is focused on barriers to EHR implementation.18–20,22,43–45 and documents wide variation in the use of existing EHR functionality.21 This study adds to the existing literature by identifying approaches and challenges to EHR optimization encountered by analysts who are embedded within a large institution that is undergoing large-scale primary care transformation. Other organizations that are considering designing a program for EHR optimization may wish to use this information as anticipatory guidance regarding potential challenges. In particular, the lack of time for teams to engage in EHR optimization may be reflective of the multiple competing demands, high workloads, and time pressures reported by primary care clinicians,46,47 that necessitates creative solutions.
Limitations of the Method
Our findings are subject to several limitations. First, the number of participants involved in this exploratory study was small because only three individuals in this organization were involved in this mediating role with primary care teams. In order to explore their unique role, our interviews were limited to these three individuals. Secondly, our findings may have limited generalizability to other settings. In particular, the comments about nurses being the most challenging group to optimize may not be generalizable to other healthcare settings as our study involved only primary care teams. However, the nature of qualitative research is to provide thick description of the case rather than universally applicable findings. Despite these limitations, we hope that our findings can be instructive regarding needed support for EHR optimization.
Call for Further Research
Further research exploring EHR optimization is critical for improving the EHR’s use as a tool to improve the quality and efficiency of care. This research should use more participants and then propose and test best practices to determine how the EHR can be used to meet multiple stakeholder needs. In particular, future research needs to further address the potential conflicting goals and expectations of primary care team members versus HIT leaders regarding EHR use. It will be useful for future studies also to consider how an emphasis on fully using EHR functionality can produce unintended consequences, such as team workflow disruption48 and the loss of important interpersonal communication, which appears to be important in the quality of care.49 The poignant comment that “I’m a nurse, I’m not a computer person” raises the question of what valuable interactional or other qualities might be lost through implementing some of the EHR functionality. It is possible, although not proven, that some of the “old habits we’re trying to break” have value or add efficiency.
Conclusions
We discovered that analysts played an important role as mediators at the interface between clinical primary care teams and HIT leadership when performing EHR optimization. These individuals did not merely convey the organizational HIT goals to primary care teams but instead, developed an understanding of both organizational and clinical teams’ goals. They used this context to tailor their training to team needs and to express shared team concerns to leadership. We also discovered several challenges to EHR optimization including tension between standardization and customization, operational, personnel readiness, and technical software issues.
Box.
What is known about the topic
Successful primary care HIT adoption has been impacted by wide variation in EHR functionality between practice sites and time costs in learning effective ways to use the EHR.
Ongoing support beyond the implementation period targeting improved use of existing functionality within the EHR is positively associated with organizations that are effective in maximizing physician EHR adoption and use.
What this paper adds
This study identifies in detail the approaches used by optimization analysts to bridge different goals of HIT leadership and primary care teams at a large organization undergoing primary care transformation.
The study highlights challenges inherent in EHR optimization and can inform other organizations who are interested in developing optimization training.
The study underscores the need to involve all stakeholders in planning EHR optimization in order to understand how EHR use can be integrated within the existing organizational structure and culture.
Acknowledgments
This project was supported by the Health Innovation Program, the UW School of Medicine and Public Health from The Wisconsin Partnership Program, and the Community-Academic Partnerships core of the University of Wisconsin Institute for Clinical and Translational Research (UW ICTR) through the National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. In addition, Nancy Pandhi is supported by a National Institute on Aging Mentored Clinical Scientist Research Career Development Award, grant number l K08 AG029527.
Footnotes
No financial disclosures were reported by the authors of this paper.
A portion of this data was previously presented at the 2012 World Conference on E-Learning in Corporate, Government, Healthcare, and Higher Education, October 9-12, Montréal, Quebec, Canada.
Contributor Information
Nancy Pandhi, Email: nancy.pandhi@fammed.wisc.edu.
Wan-Lin Yang, Email: wlyang9@mail.ncku.edu.tw.
Zaher Karp, Email: zaher.karp@fammed.wisc.edu.
Alexander Young, Email: alexander.young@uwmf.wisc.edu.
John W. Beasley, Email: john.beasley@fammed.wisc.edu.
Sally Kraft, Email: sakraft@wisc.edu.
Pascale Carayon, Email: carayon@ie.engr.wisc.edu.
References
- 1.Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Annals of Internal Medicine. 2006;144(10):742–52. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 2.Furukawa MF. Electronic medical records and efficiency and productivity during office visits. American Journal of Managed Care. 2011;17(4):296–303. [PubMed] [Google Scholar]
- 3.Karsh BT. Clinical practice improvement and redesign: how change in workflow can be supported by clinical decision support. Rockville, Maryland: Agency for Healthcare Research and Quality; 2009. [Google Scholar]
- 4.Romano MJ, Stafford RS. Electronic Health Records and Clinical Decision Support Systems: Impact on National Ambulatory Care Quality. Archives of Internal Medicine. 2011;171(10):897–903. doi: 10.1001/archinternmed.2010.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beasley JW, Holden RJ, Sullivan F. Electronic health records: research into design and implementation. British Journal of General Practice. 2011;61(591):604–5. doi: 10.3399/bjgp11X601244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karsh BT, Weinger MB, Abbott PA, Wears RL. Health information technology: fallacies and sober realities. Journal of the American Medical Informatics Association. 2010;17(6):617–23. doi: 10.1136/jamia.2010.005637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Health Information Technology for Economic and Clinical Health (HITECH) Act, Title XIII of Division A and Title IV of Division B of the American Recovery and Reinvestment Act of 2009 (ARRA), Pub. L. No. 111-5 (Feb 17, 2009), codified at 42 U.S.C. §§300jj et seq.; §§17901 et seq., 111th Congress.
- 8.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. Joint Principles of the Patient-Centered Medical Home. 2007 March. [Google Scholar]
- 9.AHRQ. Defining the PCMH. Rockville, MD: Agency for Healthcare Research and Quality; [cited]; Available from. [Google Scholar]
- 10.NCQA. Standards and Guidelines for Physician Practice Connections®—Patient-Centered Medical Home (PPC-PCMH™) Washington, D.C: National Committee for Quality Assurance; 2008. [Google Scholar]
- 11.Edsall R, Adler K. The 2012 EHR User Satisfaction Survey: Responses From 3,088 Family Physicians. Family Practice Management. 2012;19(6) [PubMed] [Google Scholar]
- 12.Hsiao CJ, Hing E, Socey TC, Cai B. Electronic health record systems and intent to apply for meaningful use incentives among office-based physician practices: United States, 2001–2011. NCHS Data Brief. 2011;(79):1–8. [PubMed] [Google Scholar]
- 13.Harrison JP, Palacio C. The role of clinical information systems in health care quality improvement. Health Care Manag (Frederick) 2006;25(3):206–12. doi: 10.1097/00126450-200607000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Taylor R, Bower A, Girosi F, Bigelow J, Fonkych K, Hillestad R. Promoting health information technology: is there a case for more-aggressive government action? Health Affairs (Project Hope) 2005;24(5):1234–45. doi: 10.1377/hlthaff.24.5.1234. [DOI] [PubMed] [Google Scholar]
- 15.Zhou L, Soran CS, Jenter CA, Volk LA, Orav EJ, Bates DW, et al. The relationship between electronic health record use and quality of care over time. Journal of the American Medical Informatics Association. 2009;16(4):457–64. doi: 10.1197/jamia.M3128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simon SR, Kaushal R, Cleary PD, Jenter CA, Volk LA, Poon EG, et al. Correlates of electronic health record adoption in office practices: a statewide survey. Journal of the American Medical Informatics Association. 2007;14(1):110–7. doi: 10.1197/jamia.M2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reid RJ, Fishman PA, Yu O, Ross TR, Tufano JT, Soman MP, et al. Patient-centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manag Care. 2009;15(9):e71–87. [PubMed] [Google Scholar]
- 18.Stream GR. Trends in adoption of electronic health records by family physicians in Washington State. Inform Prim Care. 2009;17(3):145–52. doi: 10.14236/jhi.v17i3.729. [DOI] [PubMed] [Google Scholar]
- 19.Yoon-Flannery K, Zandieh SO, Kuperman GJ, Langsam DJ, Hyman D, Kaushal R. A qualitative analysis of an electronic health record (EHR) implementation in an academic ambulatory setting. Inform Prim Care. 2008;16(4):277–84. doi: 10.14236/jhi.v16i4.703. [DOI] [PubMed] [Google Scholar]
- 20.McAlearney AS, Song PH, Robbins J, Hirsch A, Jorina M, Kowalczyk N, et al. Moving from good to great in ambulatory electronic health record implementation. Journal for Healthcare Quality. 2010;32(5):41–50. doi: 10.1111/j.1945-1474.2010.00107.x. [DOI] [PubMed] [Google Scholar]
- 21.Rao SR, Desroches CM, Donelan K, Campbell EG, Miralles PD, Jha AK. Electronic health records in small physician practices: availability, use, and perceived benefits. Journal of the American Medical Informatics Association. 2011;18(3):271–5. doi: 10.1136/amiajnl-2010-000010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miller RH, Sim I. Physicians’ use of electronic medical records: barriers and solutions. Health Aff (Millwood) 2004;23(2):116–26. doi: 10.1377/hlthaff.23.2.116. [DOI] [PubMed] [Google Scholar]
- 23.Godfrey MM, Melin CN, Muething SE, Batalden PB, Nelson EC. Clinical microsystems, Part 3. Transformation of two hospitals using microsystem, mesosystem, and macrosystem strategies. Joint Commission Journal on Quality and Patient Safety. 2008;34(10):591–603. doi: 10.1016/s1553-7250(08)34074-4. [DOI] [PubMed] [Google Scholar]
- 24.Ajami S, Arab-Chadegani R. Barriers to implement Electronic Health Records (EHRs) Mater Sociomed. 2013;25(3):213–5. doi: 10.5455/msm.2013.25.213-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shachak A, Barnsley J, Montgomery C, Tu K, Jadad AR, Lemieux-Charles L. End-user support for a primary care electronic medical record: a qualitative case study of a vendor’s perspective. Inform Prim Care. 2012;20(3):185–95. doi: 10.14236/jhi.v20i3.24. [DOI] [PubMed] [Google Scholar]
- 26.Nelson EC, Batalden PB, Huber TP, Mohr JJ, Godfrey MM, Headrick LA, et al. Microsystems in health care: Part 1. Learning from high-performing front-line clinical units. Jt Comm J Qual Improv. 2002;28(9):472–93. doi: 10.1016/s1070-3241(02)28051-7. [DOI] [PubMed] [Google Scholar]
- 27.Nelson EC, Batalden PB, Homa K, Godfrey MM, Campbell C, Headrick LA, et al. Microsystems in health care: Part 2. Creating a rich information environment. Jt Comm J Qual Saf. 2003;29(1):5–15. doi: 10.1016/s1549-3741(03)29002-x. [DOI] [PubMed] [Google Scholar]
- 28.Godfrey MM, Nelson EC, Wasson JH, Mohr JJ, Batalden PB. Microsystems in health care: Part 3. Planning patient-centered services. Jt Comm J Qual Saf. 2003;29(4):159–70. doi: 10.1016/s1549-3741(03)29020-1. [DOI] [PubMed] [Google Scholar]
- 29.Wasson JH, Godfrey MM, Nelson EC, Mohr JJ, Batalden PB. Microsystems in health care: Part 4. Planning patient-centered care. Jt Comm J Qual Saf. 2003;29(5):227–37. doi: 10.1016/s1549-3741(03)29027-4. [DOI] [PubMed] [Google Scholar]
- 30.Batalden PB, Nelson EC, Mohr JJ, Godfrey MM, Huber TP, Kosnik L, et al. Microsystems in health care: Part 5. How leaders are leading. Jt Comm J Qual Saf. 2003;29(6):297–308. doi: 10.1016/s1549-3741(03)29034-1. [DOI] [PubMed] [Google Scholar]
- 31.Mohr JJ, Barach P, Cravero JP, Blike GT, Godfrey MM, Batalden PB, et al. Microsystems in health care: Part 6. Designing patient safety into the microsystem. Jt Comm J Qual Saf. 2003;29(8):401–8. doi: 10.1016/s1549-3741(03)29048-1. [DOI] [PubMed] [Google Scholar]
- 32.Kosnik LK, Espinosa JA. Microsystems in health care: Part 7. The microsystem as a platform for merging strategic planning and operations. Jt Comm J Qual Saf. 2003;29(9):452–9. doi: 10.1016/s1549-3741(03)29054-7. [DOI] [PubMed] [Google Scholar]
- 33.Huber TP, Godfrey MM, Nelson EC, Mohr JJ, Campbell C, Batalden PB. Microsystems in health care: Part 8. Developing people and improving work life: what front-line staff told us. Jt Comm J Qual Saf. 2003;29(10):512–22. doi: 10.1016/s1549-3741(03)29061-4. [DOI] [PubMed] [Google Scholar]
- 34.Batalden PB, Nelson EC, Edwards WH, Godfrey MM, Mohr JJ. Microsystems in health care: Part 9. Developing small clinical units to attain peak performance. Jt Comm J Qual Saf. 2003;29(11):575–85. doi: 10.1016/s1549-3741(03)29068-7. [DOI] [PubMed] [Google Scholar]
- 35.QSR International. NVivo 9. Cambridge, MA: 2010. [Google Scholar]
- 36.Crabtree B, Miller W, editors. Doing Qualititative Research. 2. Thousand Oaks, CA: Sage Publications, Inc; 1999. [Google Scholar]
- 37.Walker JM, Carayon P. From tasks to processes: the case for changing health information technology to improve health care. Health Affairs (Project Hope) 2009;28(2):467–77. doi: 10.1377/hlthaff.28.2.467. [DOI] [PubMed] [Google Scholar]
- 38.Rizzo JR, House RJ, Lirtzman SI. Role Conflict and Ambiguity in Complex Organizations. Administrative Science Quarterly. 1970;15(2):150–63. [Google Scholar]
- 39.Gagnon MP, Desmartis M, Labrecque M, Legare F, Lamothe L, Fortin JP, et al. Implementation of an electronic medical record in family practice: a case study. Inform Prim Care. 2010;18(1):31–40. doi: 10.14236/jhi.v18i1.751. [DOI] [PubMed] [Google Scholar]
- 40.Cresswell K, Sheikh A. The NHS Care Record Service (NHS CRS): recommendations from the literature on successful implementation and adoption. Inform Prim Care. 2009;17(3):153–60. doi: 10.14236/jhi.v17i3.730. [DOI] [PubMed] [Google Scholar]
- 41.Beasley JW, Wetterneck TB, Temte J, Lapin JA, Smith P, Rivera-Rodriguez AJ, et al. Information chaos in primary care: implications for physician performance and patient safety. Journal of the American Board of Family Medicine. 2011;24(6):745–51. doi: 10.3122/jabfm.2011.06.100255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wetterneck TB, Lapin JA, Krueger DJ, Holman GT, Beasley JW, Karsh BT. Development of a primary care physician task list to evaluate clinic visit workflow. BMJ Qual Saf. 2012;21(1):47–53. doi: 10.1136/bmjqs-2011-000067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kaushal R, Bates DW, Jenter CA, Mills SA, Volk LA, Burdick E, et al. Imminent adopters of electronic health records in ambulatory care. Inform Prim Care. 2009;17(1):7–15. doi: 10.14236/jhi.v17i1.709. [DOI] [PubMed] [Google Scholar]
- 44.Menachemi N, Perkins RM, van Durme DJ, Brooks RG. Examining the adoption of electronic health records and personal digital assistants by family physicians in Florida. Inform Prim Care. 2006;14(1):1–9. doi: 10.14236/jhi.v14i1.609. [DOI] [PubMed] [Google Scholar]
- 45.Menachemi N. Barriers to ambulatory EHR: who are ‘imminent adopters’ and how do they differ from other physicians? Inform Prim Care. 2006;14(2):101–8. doi: 10.14236/jhi.v14i2.620. [DOI] [PubMed] [Google Scholar]
- 46.Linzer M, Gerrity M, Douglas JA, McMurray JE, Williams ES, Konrad TR. Physician stress: results from the physician worklife study. Stress and Health. 2002;18(1):37–42. [Google Scholar]
- 47.Lawler EE., III . High Involvement Management: Participative Strategies for Improving Organizational Performance. San Francisco: Jossey-Bass; 1986. [Google Scholar]
- 48.Zheng K, Haftel HM, Hirschl RB, O’Reilly M, Hanauer DA. Quantifying the impact of health IT implementations on clinical workflow: a new methodological perspective. Journal of the American Medical Informatics Association. 2010;17(4):454–61. doi: 10.1136/jamia.2010.004440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hess DR, Tokarczyk A, O’Malley M, Gavaghan S, Sullivan J, Schmidt U. The value of adding a verbal report to written handoffs on early readmission following prolonged respiratory failure. Chest. 2010;138(6):1475–9. doi: 10.1378/chest.09-2140. [DOI] [PubMed] [Google Scholar]