Abstract
Social support and social relationships have been repeatedly identified as essential to nursing home resident quality of life. However, little is known about ways residents develop relationships with peers or staff.
Objective
This study was conducted to explore the ways resident develop relationships with peers and staff in nursing homes.
Design & methods
Fifteen cognitively intact nursing home residents from two facilities were interviewed for this grounded theory study. Sampling, interviewing, and analysis occurred in a cyclical process with results at each stage of the study informing decisions about data collection and analysis in the next. Unstructured interviews and field observations were conducted. Data were analyzed with open, axial, and selective coding.
Results
Residents developed relationships with peers and staff largely as an unintended consequence of trying to have a life in the nursing home. Having a life was a two-step process. First, life motivations (Being Self and Creating a Positive Atmosphere) influenced resident preferences for daily activities and interaction goals and subsequently their strategies for achieving and establishing both. Second, the strategies residents used for achieving their required daily activities (Passing Time and Getting Needs Met) and interaction goals then influenced the nature of interaction and the subsequent peer or staff response to these interactions. Residents defined relationships as friendly or unfriendly depending on whether peers or staff responded positively or negatively. There was considerable overlap in the ways peer and staff relationships developed and the results highlight the role of peer and staff responsiveness in relationship development.
Implications
The results provide possible explanations for the success of interventions in the literature designed to improve staff responsiveness to residents. The results suggest that adapting these kinds of interventions for use with peers may also be successful. The conceptual model also presents a number of opportunities for developing interventions for residents.
Keywords: Grounded Theory, Interpersonal Relations, Nursing Homes, Aged
Introduction
Social relationships have been repeatedly identified as essential to nursing home resident quality of life (Bergland and Kirkevold, 2005, Bowers et al., 2001, Cooney et al., 2009, Custers et al., 2012, Tseng and Wang, 2001), life meaning and satisfaction (Bitzan and Kruzich, 1990, Haugan, 2013, Huss et al., 1988, Nussbaum, 1983, Takkinen and Ruoppila, 2001), and psychological well-being (Carpenter, 2002). Residents who are socially engaged are at lower risk for depression, loneliness, other negative health outcomes (Drageset, 2004) and have lower mortality (Kiely and Flacker, 2003). The centrality of relationships to resident quality of life has been acknowledged globally with philosophical and practical shifts in nursing home care delivery. Over 50% of U.S. nursing homes are committed to, or engaged in, ‘culture change’ (Doty et al., 2008), a care approach founded on the principle that relationships should be central to care delivery (Koren, 2010, Pioneer Network, 2012). My Home Life, which supports practice change in care homes across the U.K., emphasizes the need for community in care homes, focusing on relationships residents, family, and staff have with each other in the facility and within the larger community as central to resident quality of life (My Home Life, 2012). The Australian Government (2012) also promotes relationships in the care of older people as a mechanism for delivering person-centered care.
Research on resident relationships in nursing homes has often focused on predictors of relationships (Cook et al., 2006, Mor et al., 1995, Resnick et al., 1997, Schroll et al., 1997, Tsai et al., 2009), outcomes or significance of relationships (as noted above), and the ‘dose’ of relationships as measured by frequency of contact with others (Blackman et al., 1976, Chen et al., 2000, Quattrochi-Tubin and Jason, 1980) or levels of activity participation (Achterberg et al., 2003, Kiely and Flacker, 2003, Mor et al., 1995, Resnick et al., 1997, Schroll et al., 1997). However, studies of this nature do little to inform practitioners, policy makers, or researchers about the process by which residents develop relationships.
There is a growing body of research exploring the process of resident relationship development. However, the majority of studies have focused on the relationships residents develop with staff (Cook and Brown Wilson, 2010, Heliker and Nguyen, 2010, McGilton and Boscart, 2007, McGilton et al., 2003, McGilton et al., 2012, Medvene et al., 2006, Nakrem et al., 2011, Palacios-Ceña et al., 2013) rather than other residents (see exceptions (Bergland and Kirkevold, 2008, Hubbard et al., 2003, Powers, 1991)), and very few have explored the process by which residents develop relationships with both staff and other residents in a single study (see exception (Brown Wilson et al., 2009)). As relationships with both peers and staff are important to residents, exploring relationship development with both in a single study is needed to more clearly understand any important differences or similarities.
Further limiting our understanding of resident relationship development is the largely one-sided focus of current research. In particular, most studies have been conducted to inform the efforts staff need to make to improve resident relationships, specifically focusing on staff responsiveness to residents, by either enhancing personal knowledge of residents (Cook and Clarke, 2010, Heliker and Nguyen, 2010, Medvene et al., 2006), personal aptitude and skill in empathetic or relational caring (Brown Wilson, 2009, Cook and Clarke, 2010, McGilton et al., 2003, McGilton et al., 2012), or both (Brown Wilson et al., 2013). Little research has been conducted from the resident perspective for the sake of understanding what residents do to develop relationships and how their processes can be directly supported. Therefore, expanding current understandings of relationship development to include more information from the perspective of the resident is needed.
Articulating the views of residents and the work residents engage in to develop relationships with both peers and staff is necessary to facilitate identification of opportunities for targeted interventions that promote, support, and sustain relationships in practice. The purpose of this grounded theory study was to develop a conceptual model that explains how residents develop relationships with peers and staff in nursing homes. Specifically the following questions were addressed;
How are relationships defined by residents? Specifically, how do residents think about, experience, and engage in relationships?
- What is the process by which residents develop relationships?
- What are strategies residents use to develop relationships?
- What are the conditions under which relationships develop?
Methods
A grounded theory design was used to explore the ways residents developed relationships with peers and staff in this study. Sampling, data collection, and analysis occurred in a cyclical process (Corbin and Strauss, 2008). In other words, the goals of ongoing analysis guided decisions about theoretical sampling, interview questions, field observations, and coding. Data were progressively abstracted into a conceptual model as the study progressed (Corbin and Strauss, 2008).
Participants & Setting
Nursing home residents in two nursing homes who spoke fluent English, could carry on a conversation, and understand the consent process as judged by a facility designee, who had knowledge of the residents and their histories, were included. Nursing home residents who had a legal guardian or an activated health care power of attorney due to mental incapacity were excluded. A total of 15 residents were interviewed in this study. Consistent with general U.S. nursing home demographics, the majority of participants were Caucasian, widowed, females. The mean resident age was 78.23 years (range 55–97) and the average length of stay was 1.75 years (range 3 weeks – 9 years).
Facility 1 was a 90 bed, for-profit, national chain facility. The facility experienced high administrator turnover during the period of data collection. However, many nursing staff members had been working in the facility for several years, had come from the local community, and were generally assigned to work on the same units (although they did not explicitly use consistent assignment). Most residents shared rooms in this facility.
Facility 2 was a 108 bed, non-profit facility. The building had been renovated into neighborhoods of approximately 10–12 residents each and staff were consistently assigned to residents. However, at the time of data collection, residents described the facility as experiencing some turnover so staff assignments were not always consistent. Most rooms in this facility were private with the exception of some semi-private rooms.
Data Collection & Analysis
A combination of convenience sampling and theoretical sampling was used to obtain the final sample size of 15 residents. Convenience sampling was used at the outset of the study. As concepts were developed from the data, theoretical sampling was used, with researchers asking to speak to individuals who might have had specific experiences that would further the conceptual model (Corbin and Strauss, 2008, Glaser and Strauss, 1967). For example, researchers asked to speak to residents who did not leave their rooms on a regular basis as their access to others for developing relationships would be limited and their experience potentially different. In addition, interview questions were altered to inquire about experiences that were theoretically relevant as data collection progressed. Sampling continued until saturation, or the point at which no new conceptual information was obtained in the data.
Unstructured one-on-one, resident-directed interviews with open-ended questions were conducted. Interview questions started out general, allowing residents to define important relationship concepts, and became more focused as the study progressed. For example, all residents were asked to begin the interview with, “Please tell me what it has been like for you to stay in the nursing home” which was followed with additional broad questions to address issues grounded in the participant’s response. Residents often responded by saying they had many friends in the facility. They were subsequently asked, “Can you say more about the friends you have here?” Interviews lasted between 18 and 116 minutes (average = 47 minutes) and were audio recorded, transcribed and transferred to NVIVO 9.0 software(QSR International Pty Ltd, 2010) for data storage and management. Each resident was interviewed only one time. Field observations of residents interacting with others in public spaces were conducted before and after interviews and used to supplement interview responses and prompt new interview questions. For example, in field observations it was noted that residents participating in a structured activity did not interact with one another and that there was little opportunity for relationship work. This knowledge was used to probe residents who spent considerable time attending structured activities about their relationships to determine if their relationships were different than those of residents had who attended fewer activities.
Data were analyzed using open, axial, and selective coding. Open coding involved breaking down sentences into concepts. “Codes” were assigned to concepts which were organized into categories based on relationships described by participants. Axial coding involved specifying the context of categories such as the dimensions and properties (e.g. when, how, or under what conditions a phenomenon may occur) and identifying how categories were related. Selective coding was used to articulate the core category and finalize the theory.
Team analysis, memoing, and member checking were used to ensure study rigor (Strauss and Corbin, 1998). Team analysis was done on a regular basis with a multi-perspective research group to ensure assumptions and biases were revealed and kept in check. The team was comprised of health science professionals with various levels of knowledge in the care and research of older adults and nursing homes. Memoing was used extensively throughout the study to inform sampling, data collection, and data analysis and record analytic decisions. Memoing included activities such as identifying important theoretical sampling pursuits, determining appropriate changes to interview questions as the study progressed, raising comparative and theoretical questions about the data, and drawing and expanding maps of concepts and their linkages after interviews. Member checking with residents was conducted at several points throughout the study by asking residents specific questions about emerging concepts and their linkages, with the explicit purpose of ensuring the researchers had a thorough understanding of resident experiences. Resident responses at each of these points were used to expand the researchers’ understandings of the definitions and variations in the concepts and were incorporated, by the researchers, into the final conceptual diagram.
Ethical Considerations
Ethical approval of the study was granted by the minimal risk committee of the local university Institutional Review Board and informed written consent was obtained from each resident who volunteered for the study. To ensure confidentiality, interviews were conducted in private spaces. Residents were given opportunities to refuse questions and withdraw from the interview at any time. Observations were only conducted in public spaces.
Results
Residents spontaneously addressed relationships in their responses to questions, often in the first moments of the interview. In these responses, residents defined relationships in a number of ways, judging them by their positive or negative qualities as well as their contribution to residents’ experiences in the facility or residents’ quality of life. When probed in more depth about their various relationships, residents revealed an elaborate process by which relationships with peers and staff formed, not by deliberate efforts to develop them, but rather as unintended consequences of resident efforts to have a life in the nursing home.
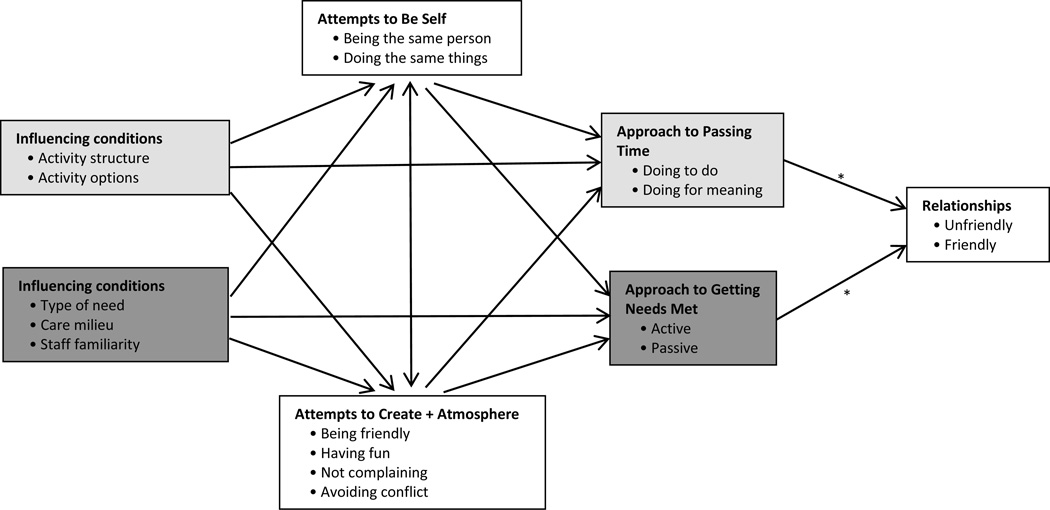
The process of having a life was comprised of two important dimensions, higher level life motivations (Being Self and Creating a Positive Atmosphere) and required daily activities (Passing Time and Getting Needs Met). Attending to these dimensions had important consequences for relationship development and can be thought of as two steps of a process. First, life motivations influenced resident preferences for daily activities and interaction goals and subsequently their strategies for achieving and establishing both. Second, the strategies residents used for achieving their required daily activities and interaction goals influenced the nature of the relationships residents developed with peers and staff. This process was sufficiently complicated and nuanced and varied depending on several situational conditions. The factors of this process and their interrelationships are depicted in Figure 1.
Figure 1. Conceptual model of factors of ‘Having a Life’ that influence peer and staff relationship development.
Note. Residents engage in a complicated process to have a life in the nursing home, determining the appropriate timing and use of a variety of strategies under various conditions. The decisions they make about which strategies to use to have a life influence the nature of their interaction with peers and staff. Residents define a relationship as friendly or unfriendly based on peer or staff responses during interaction. The * symbol denotes the usual place where peer and staff responses occur. White boxes highlight factors common to both peer and staff relationship development. Light gray boxes highlight factors that are more common to peer relationship development. Dark gray boxes highlight factors more common to staff relationship development. + = Positive.
Relationships as Defined by Residents
Residents defined relationships according to the ways peers and staff reciprocated or responded to the strategies they used to have a life. Positively reciprocated interactions were common, and residents labeled these relationships as friendly. Negatively reciprocated interactions were less common, but when they existed, residents left the relationship unlabeled and discussed it as somewhat of an enigma, as they often seemed unaware of what had led to the relationship being unfriendly. Judgment about a relationship was often quick and residents described a number of situations in which they determined the type of relationship after a single interaction. Responses indicated residents largely, but not exclusively, judged what it meant to live in a nursing home in terms of the types and qualities of the interactions and relationships they had with others, including peers and staff. Furthermore, residents also revealed the significance of relationships in their lives by discussing some peer or staff relationships with great emotion and as capable of influencing their quality of life, either improving or worsening it, depending on the nature of the relationships.
Residents in this study described more relationships, both friendly and unfriendly, with peers than staff, but generally did not differentiate a peer or staff relationship in any significant way or talk about relationships differently based on these roles. In particular, the first step of having a life – life motivations influencing activity preferences and interaction goals – was consistent whether a resident interacted with peers or staff. Residents however, did report interacting with peers and staff for very different reasons, making the context surrounding the development of peer or staff relationships different. The second step of having a life – strategies for activities and interactions influencing relationships directly – therefore varied and the case of peer or staff relationships are reported separately below to illustrate how the second step operationalizes differently for each.
Life Motivations Influence Daily Activity Preferences & Interaction Goals
Residents in this study discussed two fundamental motivations for having a life in the nursing home that influenced indirectly the relationships they developed with peers and staff. These motivations were Being Self and Creating a Positive Atmosphere. Because these motivations were fundamental, higher order goals, they tended to influence both peer and staff relationships.
Being Self
Being Self was the propensity for residents to continue being the person they always were. Resident interview responses suggested Being Self was a process that was fundamental to life and influenced preferences for their daily needs and activities. Residents put considerable effort into remaining themselves, attempting to craft a life that would allow them to do so even when their actions were not understood or perceived undesirable by others. Being Self consisted of two interlinked strategies; a) continuing to ‘be’ the same person and b) continuing to ‘do’ the same things. See Table 1 for definitions and examples of strategies. Being Self influenced relationships because it motivated residents to make certain decisions about their strategies for having a life to be consistent with past practices and preferences and these choices could ultimately influence the type of relationships residents developed with peers and staff. For example, a resident who was often reluctant to ask for assistance with care, was getting inconsistent care. The inconsistency had resulted in verbal discipline of staff that subsequently seemed to cause friction and unfriendly relationships between the resident and the staff. However, not asking for assistance allowed the resident to get care more consistent with his past practices.
… they’ve been having a little trouble getting [me] washed up at night … Interviewer asks: Do you ask them or tell them that you’re ready? Resident responds: No I don’t ever really ask them … I never was too good for grooming and cleaning up all the time anyway. Just so you kept cleaned up and new clothes on ya. R5F1.
Table 1.
Strategies residents use to ‘Have a Life’ and their influence on relationship development.
| Strategy | Definition | Purpose | Connection to Relationship Development |
Study Examples |
|---|---|---|---|---|
| Being Self | ||||
| Continuing to Be the Same Person |
Maintaining lifelong traits, demeanor, or other characteristics & preferences |
Continue behaving/engaging in life in ways consistent with lifelong patterns |
1. Influence daily activity preferences below |
History of avoiding gossip influences resident decision not to engage with peers when they gossip. |
| 2. Support or impede friendly relationships |
Friendly resident reaches out to peers. Solitary resident unable to make friends. |
|||
| Continuing to Do the Same Things |
Partaking in, or talking about, same routines, hobbies, commitments, rituals, or traditions of past |
Continue behaving/engaging in life in ways consistent with lifelong patterns |
Influence daily activity preferences below |
Resident with a lifelong hobby of cross-stitching prefers to do for meaning which keeps her in her room & inhibits opportunities to develop friendly relationships with others. |
| Creating a Positive Atmosphere | ||||
| Being Friendly |
Acting friendly and/or neighborly to persons in the facility |
Deal with living & existing with strangers |
1. Interaction goal: Test how peers &/or staff will respond to interaction & relationship advances |
Resident acts friendly and waits for staff/peer response. Judges relationship based on response. |
| 2. Support ongoing friendly peer &/or staff relationships |
Taking candy to a familiar resident whose room is nearby. |
|||
| Having Fun | Joking, assigning nicknames, teasing, & using humor |
Deal with negative aspects of living in a facility, asking for care, & receiving care |
1. Interaction goal: Make interactions more comfortable |
Singing songs or being silly with staff in the bathroom during toileting. |
| 2. Support ongoing friendly peer &/or staff relationships |
Nickname assigned after a shared experience and used regularly to make the person feel special. |
|||
| Not Complaining |
Not voicing disdain for infractions in expectations |
Demonstrate respect for others |
1. Interaction goal: Prevent negative interactions |
Not speaking up because it would create friction and not change the situation. |
| 2. Support ongoing friendly &/or prevent unfriendly peer &/or staff relationships |
Feeling staff work hard; do not complain when needs delayed. Treated with respect in return. |
|||
| Avoiding Conflict |
‘Staying away’ from individuals 1. one experienced or expected to experience conflict with 2. who would not reciprocate attempts to make atmosphere positive |
1. Prevent threats to a positive environment 2. Prevent sustained negative interactions with others |
1. Interaction goal: Prevent uncomfortable interactions where possible 2. Prevent unfriendly relationships with peers &/or staff |
Staying away from another resident who has dementia, or cannot hear/see/speak clearly, does not follow conversation or keep up in a conversation making the experience of interaction difficult. Ignoring a roommate that one does not get along with. |
| Passing Time | ||||
| Doing for the Sake of Doing |
Engaging in activities that do not have inherent value |
1. Make days go by; fill time 2. Have something to look forward to |
1. Impede friendly peer relationships |
Attending structured activities that leave little time for socialization. |
| 2. Support friendly peer relationships |
Talking with peers between activities. |
|||
| Doing for Meaning |
Engaging in activities that have meaning |
Continue activities consistent with past practices that were personally important |
1. Support friendly peer relationships |
Playing favorite games with another peer. |
| 2. Impede friendly peer relationships |
Preferring solitary activities. | |||
| 3. Support unfriendly peer relationships |
Preferring an activity disliked by a roommate. |
|||
| Getting Needs Met | ||||
| Active Approaches |
Explicit strategies used to make needs known and get them met |
1. Make a need known 2. Specific requests to make care consistent with preferences |
1. Impede friendly staff relationships |
Transactional exchange of care with little opportunity for talking or getting to know one another. |
| 2. Support unfriendly staff relationships |
Staff respond poorly to care requests. |
|||
| Passive Approaches |
Assumption that needs will be known and met without direction |
1. Allow staff to direct care 2. No need to use active approaches because staff are already aware of needs & can address them without direction |
1. Support friendly staff relationships |
Staff appreciate passive approaches & respond positively to residents when delivering care. |
| 2. Support unfriendly staff relationships |
Care not accomplished; resident & staff get upset with each other. |
|||
Another resident who was having difficulty developing friendly relationships with peers described how her peers often choose to engage with each other in ways she historically disliked. She subsequently spent considerable time in her room.
They [peers she spent time with] have the same things in mind. Flowers and grass and … Well, a lot of times it’s gossip. And I don’t like that. Not very much. I like to know what’s going on but I don’t like to, I don’t like the gossip part of it. I never did. I never went to uh, the neighbors with coffee klatches. Uh uh. I never did … I go out, I go out of my room, but then I come back again. R7F1.
Creating a Positive Atmosphere
Creating a Positive Atmosphere was a motivation residents had in order to neutralize threats to well-being associated with the unpredictability and constraints in the environment they encountered in their daily lives (see Table 2 for examples). Creating a Positive Atmosphere involved a deliberate process of engaging others in positive ways to improve the environment. There were four ways residents did this; a) being friendly, b) having fun, c) not complaining, and d) avoiding conflict or distressing situations. See Table 1 for definitions and examples of these strategies. Creating a Positive Atmosphere was a pervasive motivation that affected interaction goals. However, the strategy did not necessarily have a specific purpose or exist for accomplishing a daily need or activity. Creating a Positive Atmosphere involved inherent risk because it often entailed interaction with unfamiliar people. Therefore, residents had little knowledge about the potential response they would receive. The following resident provides an example of test interactions for Creating a Positive Atmosphere which could eventually lead to friendly relationships.
… they just had a change of shift and gave some of us different places to sit and eat. And when you, when you first come in, it’s kinda quiet. But then afterwards somebody will talk about the food, whether it’s good, whether you like it or don’t like it. R12F2.
Table 2.
Lists of examples for selected categories.
| Factor | Dimension | Subdimension | Example |
|---|---|---|---|
|
Creating a Positive Atmosphere |
Unpredictability | Changes in surroundings or people |
New roommate |
| New dining seating arrangement | |||
| Rotation or turnover of aides | |||
| In care delivery | Delays due to emergencies | ||
| Changes in health status |
Fluctuations in physical well-being | ||
| Constraints | In freedoms | Leaving the building without notifying staff |
|
| In ability to Manipulate environment |
Inability to get away from serious or sustained conflict with roommate |
||
|
Getting Needs Met |
Type of need | Obtaining items for everyday living |
Hygiene products |
| Incontinence products | |||
| Completing activities of daily living |
Dressing | ||
| Toileting | |||
| Treatment of Physical conditions by Appropriately trained individuals |
Physical therapy for broken hip | ||
| Intravenous antibiotics for infection | |||
| Equipment or major medical supplies |
Specialty mattress for wound care | ||
| Higher order needs |
Booting computer to interface with family |
||
| Accommodations to address changes in needs |
Having meals in room when acutely ill |
||
| Active approaches |
Making oneself available for care |
Being in room when expected | |
| Going to a nurse for a blood sugar check |
|||
| Assisting staff to get need met |
Holding bedrail to assist in turning | ||
| Making requests | Asking for polident | ||
| Direct care | Telling staff how to turn the resident to best accomplish care |
||
| Doing it one’s self | Putting self to bed | ||
| Going outside facility |
Going to beauty shop for a haircut |
Note. Selected factors of having a life are presented here because they include long lists of conceptually relevant and distinct examples that would be difficult to follow in text.
Creating a Positive Atmosphere was often successful for developing friendly relationships as residents described a number of others, both peers and staff who were responsive to their efforts to create a positive atmosphere. However, there were a number of failed attempts. In particular, residents described how residents with dementia were unable to reciprocate in efforts to create a positive atmosphere and residents did not often discuss having friendly relationships with them. For example, the following resident lived in a household in which the majority of residents had dementia.
This place has sort of these little households here… Interviewer asks: So is it hard to find people to be friends with? Resident responds: Yeah, [people with dementia] can’t converse about anything, R10F2.
Residents also found it difficult to have friendly relationships with staff who did not reciprocate efforts to create a positive atmosphere. For example, the following resident did not have a friendly relationship with a night nurse.
There’s an older [nurse] and she comes at night and all I can think of is the description of her was an army nurse. All business. R6F1.
There were some residents who described general discomfort with the risk of interacting with others for the sake of Creating a Positive Atmosphere and were reluctant to do so. While these residents could therefore limit the potential for unfriendly relationships, they could also limit their potential for friendly relationships. Some residents also described a process in which they learned to tolerate the risk over time to deal with potential loneliness and how this helped them form relationships.
There was a time when … it took me a while to loosen up… If you don’t open up you might as well sit in the corner … you have to put yourself forward a little or nobody will even respond to you … And you learn that kind of fast, at least I did … Here you have to get used to all kinds of people. R12F2.
Daily Activities & Interaction Goals Influence Peer Relationship Development
Passing Time was a daily activity that specifically influenced interaction with and development of relationships with peers. Passing Time could be accomplished by doing for the sake of doing or by doing for meaning. See Table 1 for definitions and examples of these strategies. Passing Time influenced peer relationship development because the decisions residents made about which strategy they used to pass time influenced their opportunities for interaction. In some cases, the choices residents made limited their opportunities to interact or form relationships at all. For example, in structured, formal events (e.g. those on the activities calendar), in which there was staff effort to get residents to and from the activity and staff direction of the activity, there was often little time for interaction.
… sometimes you’re just in a big audience then you don’t have time to look somebody up because they’re in one place and you’re in another. R12F2.
However, doing things for meaning could also limit opportunities for interaction. For example, one resident choose to stay in her room to cross-stitch rather than come out to engage in facility activities.
I tell everybody, my stitching is my therapy. That’s all I need. I love it so much that I just spend time doing it… It makes me happy. That’s what I try and tell the activities director here and she’s finally come to the conclusion that leave me alone because that’s what I want… She’d come in and try to get me to come out and do things. R10F2.
In other cases, resident choices for Passing Time provided opportunities for interaction. Residents often passed time more informally with activities which were unplanned, unannounced, not facility-wide, and typically resident-initiated. Residents were often able to spend considerable time interacting and forming friendly relationships in these kinds of activities.
… [my friend and I] sit at that round table [in the lobby] together … A lot of us gather around there and talk. And sometimes we have games that they play on that table too. R1F1.
Residents also did things for meaning that allowed opportunity for interaction or intentionally involved other people to do them.
I enjoy playing cribbage … for me that’s a really nice outside activity. And to get somebody that enjoys it with me makes the, makes the day. R14F2.
Generally, residents gave few examples of unfriendly interactions and relationships that resulted from their preferences and choices for Passing Time. However, there were examples of unfriendly roommates, particularly when the pair had discordant preferences for Passing Time.
And we never made it off. She came. They brought her. And she came and I had the TV on and she said “shut that damn thing off.” Oh my, I’m not shutting that off. I said “that’s my tv” ya know. R1F1.
While many of the examples residents provided about passing time suggested they made some choices about how they did so, their choices were constrained by certain conditions. In particular, the opportunities for certain types of activities (e.g. those a resident might prefer vs. not prefer) and the structure of the activity (e.g. large group, highly structured vs. small group, unstructured) were not always in their control and restricted choices to those options available.
Daily Activities & Interaction Goals Influence Staff Relationship Development
Getting Needs Met (see Table 2 for a list of needs) was the second daily activity that influenced interaction with and development of relationships with staff. Getting Needs Met consisted of two strategies; a) active approaches and b) passive approaches. See Table 1 for definitions and examples of strategies and Table 2 for a list of active approaches. Getting Needs Met could influence relationships with staff. Residents often described carefully choosing which strategy to use to best avoid negative interactions with staff. While residents had many examples of receiving care, despite their approach, from positive and friendly staff, that was not always the case. Active approaches could draw resistance from staff.
I’m really used to directing my own care … And that doesn’t always go over real well with people in a place like this because I’m used to telling people what to do and having it done when I tell them to do it. If they don’t know how to do it I should probably be able to explain to them how to do it. Um, that can step on some toes. R9F1.
Passive approaches were also related to unfriendly relationships with staff. However, residents did not have a sense for whether passive approaches influenced development of unfriendly relationships or vice versa. For example, the following resident described not getting along well with some staff.
I had [grumpy CNA] last night. I fell asleep. I went in my recliner early. She never got me ready for bed. And that kind of ticks me off… Interviewer asks: Is that because you don’t get along with each other? Participant responds: Mm hmm. R2F1.
Residents subsequently learned to determine the right amount and timing of active and passive approaches that would best support friendly relationships. Residents changed their approaches depending on a number of conditions such as who was working (i.e. how familiar the assigned staff were of the resident’s needs and preferences), how the day was going (e.g. how many interruptions to workflow staff were experiencing), and how important staff might feel the need is (e.g. need to use the toilet vs. the need for help in getting a computer turned on and booted up). The balancing of active and passive approaches could be exhausting and had to be individualized for different staff idiosyncrasies.
Discussion
The conceptual framework developed in this study highlights the multilayered influences on resident interactions and development of relationships with peers and staff. The strategies residents decide to use in the various aspects of ‘having a life’ are the key components that link and operationalize various parts of the process and ultimately drive the type of relationships that develop. Life motivations influence preferences for how, when, and with whom residents want to spend their day and receive their care. Resident choices about which strategies to choose to act on these preferences, given situational factors, lead to interactions that can be positively or negatively reciprocated by peers or staff. The response determines whether residents report a relationship as friendly or unfriendly. The process was generally the same whether a resident was developing a relationship with a peer or staff; however, the reason for interacting was usually different.
The residents in this study highlighted the role of human responsiveness in the process of relationship development. This finding provides support for past research that has focused on human responsiveness interventions, particularly with staff, as a key mechanism for improving relationship outcomes for residents. Moreover, despite varied approaches and theoretical underpinnings, human responsiveness interventions with staff have generally been demonstrated to be successful in improving relationship outcomes (Brown Wilson et al., 2013, McGilton, 2002, McGilton et al., 2003, Medvene et al., 2006). By soliciting the resident perspective in the current study, the results provide a potential explanation for the universal success of these approaches. From the resident perspective, it is clear that a positive response by staff is key to a positive and friendly relationship. However, it is important to note the residents in this study reported negative staff responsiveness as a rarity. The results of this study suggest staff responsiveness interventions should be continued and supported; but there may be limited potential to make major changes to resident relationship development particularly if residents are already engaged with generally responsive staff.
By taking a broad view of relationships in this study, it was possible to make general comparisons of peer and staff relationships and their development. The findings of this study suggest that there was considerable overlap in the ways residents experienced, defined, and developed relationships with peers or staff. In particular, human responsiveness to interaction was a common finding across peer and staff relationship development. This finding raises questions about whether and how interventions that have been developed for, and tested with, staff might be adapted for use with peers. Future research should be conducted to determine how peer interventions could be developed, with whom they can be conducted (e.g. persons with dementia), and whether there is any relative benefit from using them. Given that residents in this study identified more concerns with developing relationships with peers than staff, there may also be great potential for making improvements in relationship development if peers are targeted for intervention. The overlap in the role of higher life motivations, specifically Being Self and Creating a Positive Atmosphere, in both peer and staff relationship development, also suggests that developing and targeting resident-level interventions that will improve or enhance the ability for residents to use strategies to operationalize these motivations might improve relationship with peers and staff simultaneously.
By exploring the resident perspective in this study, it is possible to see that residents are very active participants in relationship development, making calculated decisions about how to behave and interact with peers and staff in ways that produce or support specific types of relationships. Some of these strategies have been reported in prior research; in particular, avoiding conflict (Palacios-Ceña et al., 2013), not complaining (Palacios-Ceña et al., 2013), and using passive approaches to getting needs met (Fiveash, 1998) have been noted as important ways to manage relationships with staff. Consistent with ‘having fun’ in this study, using humor, jokes, and teasing has been found to support peer relationship development even among persons with dementia (Hubbard et al., 2003). Future research could focus on development of simple resident-level interventions that make explicit, and teach, successful strategies for developing relationships. However, the complexity of relationship development presented by residents in this study raises questions about the ability of persons with dementia to execute some of the complex thinking to engage appropriately in these strategies. Future research should consider exploring the process of having a life for persons with varying levels of dementia and determining whether and where there might be potential for intervention with this group.
The findings of this study and the resultant conceptual model also provide new insights into future avenues for research and practice inquiry. For example, residents were quick to designate a relationship as friendly or unfriendly. However, it was clear from responses that there were nuances in these relationships and they were not simply, one or the other. In addition, past research has demonstrated consistently that residents have different relationship preferences and needs (Bergland and Kirkevold, 2008, Bowers et al., 2001, Powers, 1991). Determining how life strategies reported in this study lead to more nuanced relationships and do, or do not, support relationship preferences and needs is vital. It was also outside the scope of this study to determine whether there was any harm or benefit associated with any particular relationship or net harm or benefit from various relationships comprised in a network. Future research examining the effect of the entire relationship network on resident well-being is needed to better understand how to identify and intervene for residents at particular risk from the detrimental effects of poor relationships. Finally, more research is needed to articulate other practical conditions (e.g. activity options) that influence relationship development and how they might be amenable to intervention at a system or organizational level.
Limitations
The conceptual model developed in this study was highly grounded in the experiences of cognitively intact residents who were generally positive people, had positive feelings about their experiences in the nursing home, and were successful at developing friendly relationships with others. However, each resident had some cases and experiences from which they could draw examples of negative interactions with others, both peers and staff. One resident who was known to have many negative relationships with others refused to participate. Further research conducted with persons who have been less successful socially integrating in the nursing home may prove useful for expanding the framework. Furthermore, results may not be generalizable to persons with dementia.
Constructions of relationship development in this study relied on the perceptions of one member of relationship only. While the resident perception of relationship development is informative, and residents did provide the role of peers and staff in relationship development from their perspective, it may also be important to conduct future research exploring dyadic understandings of relationship development. Furthermore, observations were only conducted in public spaces, where residents were often interacting with one another or with staff in large groups, greatly limiting the opportunity for observations of more intimate and ongoing dyadic relationship interactions between residents and staff and residents and roommates. Observations in public spaces also limited strategic and theoretically driven observations in some cases. More extensive observation is warranted to better inform the nuances of dyadic interactions and expand the framework.
Due to these limitations, the information presented here is not regarded as the only explanation, or the complete explanation, of relationships development in nursing homes. However, the findings may have theoretical and clinical relevance regarding the complexities by which resident develop relationships.
Conclusions
The ways residents define and develop relationships with peers and staff is considerably complex. The conceptual framework developed in this study provides new insight into these processes and the strategies residents use throughout them. The framework provides some explanation for the success of past interventions used with nursing home staff to improve resident-staff relationships and raises new questions about potential ways to expand these interventions for peers The results also suggest resident-level interventions that teach strategic application of life strategies might be valuable. Future research to expand the framework is warranted, particularly to better understand the consequences of certain levels and combinations of relationships for residents as well as how the framework is relevant for persons with dementia.
Research Highlights.
What is already known on this topic?
Relationships are essential to nursing home resident quality of life.
Considerable knowledge exists regarding the predictors, outcomes, and dose of resident relationships.
Little is known regarding the process by which nursing home residents develop relationships.
What this paper adds
Residents define relationships as friendly or unfriendly based on peer or staff responses to interaction.
Nursing home residents develop relationships unintentionally while simply trying to have a life in the facility. The timing and type of strategies used to have a life depend on resident life motivations and goals and greatly influence peer and staff relationship development.
Residents develop relationships with peers and staff in largely similar ways raising questions about whether relationship interventions designed for use with staff could also be applied and transferred for use with peers.
Residents are very active participants in relationship development. However, some residents may be less successful in developing friendly relationships.
Acknowledgements
TR acknowledges training support from the John A. Hartford foundation BAGNC Scholar’s program during the conduct of this study and postdoctoral training support from the William S. Middleton Veterans Affairs Hospital in Madison, WI during the writing of the manuscript. GRECC manuscript XXXX-XX. BB acknowledges partial support from the Clinical and Translational Science Award (CTSA) program, through the National Institutes of Health National Center for Advancing Translational Sciences (NCATS) [UL1TR000427]. The views and content expressed in this article is solely the responsibility of the authors and does not necessarily reflect the position, policy, or official views of the Department of Veteran Affairs, U.S. government, or National Institutes of Health.
References
- Achterberg W, Pot A, Kerkstra A, Ooms M, Muller M, Ribbe M. The effect of depression on social engagement in newly admitted Dutch nursing home residents. The Gerontologist. 2003;43(2):213–218. doi: 10.1093/geront/43.2.213. [DOI] [PubMed] [Google Scholar]
- Bergland A, Kirkevold M. Resident-caregiver relationships and thriving among nursing home residents. Research in Nursing and Health. 2005;28(5):365–375. doi: 10.1002/nur.20097. [DOI] [PubMed] [Google Scholar]
- Bergland Å, Kirkevold M. The significance of peer relationships to thriving in nursing homes. Journal of Clinical Nursing. 2008;17(10):1295–1302. doi: 10.1111/j.1365-2702.2007.02069.x. [DOI] [PubMed] [Google Scholar]
- Bitzan JE, Kruzich JM. Interpersonal relationships of nursing home residents. The Gerontologist. 1990;30(3):385–390. doi: 10.1093/geront/30.3.385. [DOI] [PubMed] [Google Scholar]
- Blackman D, Howe M, Pinkston E. Increasing participation in social interaction of the institutionalized elderly. The Gerontologist. 1976;16(1 Part 1):69–76. doi: 10.1093/geront/16.1_part_1.69. [DOI] [PubMed] [Google Scholar]
- Bowers BJ, Fibich B, Jacobson N. Care-as-service, care-as-relating, care-as-comfort. The Gerontologist. 2001;41(4):539–545. doi: 10.1093/geront/41.4.539. [DOI] [PubMed] [Google Scholar]
- Brown Wilson C. Developing community in care homes through a relationship-centred approach. Health & Social Care in the Community. 2009;17(2):177–186. doi: 10.1111/j.1365-2524.2008.00815.x. [DOI] [PubMed] [Google Scholar]
- Brown Wilson C, Davies S, Nolan M. Developing personal relationships in care homes: Realising the contributions of staff, residents and family members. Ageing and Society. 2009;29(7):1041–1063. [Google Scholar]
- Brown Wilson C, Swarbrick C, Pilling M, Keady J. The senses in practice: Enhancing the quality of care for residents with dementia in care homes. Journal of Advanced Nursing. 2013;69(1):77–90. doi: 10.1111/j.1365-2648.2012.05992.x. [DOI] [PubMed] [Google Scholar]
- Carpenter B. Family, peer, and staff social support in nursing home patients: Contributions to psychological well-being. Journal of Applied Gerontology. 2002;21(3):275–293. [Google Scholar]
- Chen Y, Ryden M, Feldt K, Savik K. The relationship between social interaction and characteristics of aggressive, cognitively impaired nursing home residents. American Journal of Alzheimer’s Disease and Other Dementias. 2000;15(1):10–17. [Google Scholar]
- Cook G, Brown Wilson C. Care home residents’ experiences of social relationships with staff. Nursing Older People. 2010;22(1):24–29. doi: 10.7748/nop2010.02.22.1.24.c7492. [DOI] [PubMed] [Google Scholar]
- Cook G, Brown Wilson C, Forte D. The impact of sensory impairment on social interaction between residents in care homes. International Journal of Older People Nursing. 2006;1(4):216–224. doi: 10.1111/j.1748-3743.2006.00034.x. [DOI] [PubMed] [Google Scholar]
- Cook G, Clarke C. A framework to support social interaction in care homes. Nursing Older People. 2010;22(3):16–21. doi: 10.7748/nop2010.04.22.3.16.c7631. [DOI] [PubMed] [Google Scholar]
- Cooney A, Murphy K, O’Shea E. Resident perspectives of the determinants of quality of life in residential care in Ireland. Journal of Advanced Nursing. 2009;65(5):1029–1038. doi: 10.1111/j.1365-2648.2008.04960.x. [DOI] [PubMed] [Google Scholar]
- Corbin J, Strauss A. Basics of qualitative research: Techniques and procedures for developing grounded theory. Thousand Oaks: Sage Publications, Inc.; 2008. [Google Scholar]
- Custers AFJ, Westerhof GJ, Kuin Y, Gerritsen DL, Riksen-Walraven JM. Relatedness, autonomy, and competence in the caring relationship: The perspective of nursing home residents. Journal of Aging Studies. 2012;26(3):319–326. [Google Scholar]
- Doty M, Koren M, Sturla E. Culture change in nursing homes: How far have we come? Findings from the Commonwealth Fund 2007 national survey of nursing homes. New York, NY: Commonwealth Fund; 2008. [Google Scholar]
- Drageset J. The importance of activities of daily living and social contact for loneliness: A survey among residents in nursing homes. Scandinavian Journal of Caring Sciences. 2004;18(1):65–71. doi: 10.1111/j.0283-9318.2003.00251.x. [DOI] [PubMed] [Google Scholar]
- Fiveash B. The experience of nursing home life. International Journal of Nursing Practice. 1998;4(3):166–174. doi: 10.1046/j.1440-172x.1998.00062.x. [DOI] [PubMed] [Google Scholar]
- Glaser B, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. New York: Sociology Press; 1967. [Google Scholar]
- Haugan G. The relationship between nurse-patient interaction and meaning-in-life in cognitively intact nursing home patients. Journal of Advanced Nursing. 2013;70(1):107–120. doi: 10.1111/jan.12173. [DOI] [PubMed] [Google Scholar]
- Heliker D, Nguyen HT. Story sharing: Enhancing nurse aide-resident relationships in long-term care. Research in Gerontological Nursing. 2010;3(4):240–252. doi: 10.3928/19404921-20100303-01. [DOI] [PubMed] [Google Scholar]
- Hubbard G, Tester S, Downs M. Meaningful social interactions between older people in institutional care settings. Ageing and society. 2003;23(1):99–114. [Google Scholar]
- Huss M, Buckwalter K, Stolley J. Nursing’s impact on life satisfaction. Journal of Gerontological Nursing. 1988;14(5):31–36. doi: 10.3928/0098-9134-19880501-09. [DOI] [PubMed] [Google Scholar]
- Kiely D, Flacker J. The protective effect of social engagement on 1-year mortality in a long-stay nursing home population. Journal of Clinical Epidemiology. 2003;56(5):472–478. doi: 10.1016/s0895-4356(03)00030-1. [DOI] [PubMed] [Google Scholar]
- Koren MJ. Person-centered care for nursing home residents: the culture change movement. Health Affairs. 2010;29(2):312–317. doi: 10.1377/hlthaff.2009.0966. [DOI] [PubMed] [Google Scholar]
- McGilton K. Enhancing relationships between care providers and residents in long-term care. Designing a model of care. Journal of Gerontological Nursing. 2002;28(12):13–21. doi: 10.3928/0098-9134-20021201-05. [DOI] [PubMed] [Google Scholar]
- McGilton K, Boscart V. Close care provider-resident relationships in long-term care environments. Journal of Clinical Nursing. 2007;16(11):2149–2157. doi: 10.1111/j.1365-2702.2006.01636.x. [DOI] [PubMed] [Google Scholar]
- McGilton K, O’Brien-Pallas L, Darlington G, Evans M, Wynn F, Pringle D. Effects of a relationship-enhancing program of care on outcomes. Journal of Nursing Scholarship. 2003;35(2):151–156. doi: 10.1111/j.1547-5069.2003.00151.x. [DOI] [PubMed] [Google Scholar]
- McGilton KS, Sidani S, Boscart VM, Guruge S, Brown M. The relationship between care providers’ relational behaviors and residents mood and behavior in long-term care settings. Aging & Mental Health. 2012;16(4):507–515. doi: 10.1080/13607863.2011.628980. [DOI] [PubMed] [Google Scholar]
- Medvene L, Grosch K, Swink N. Interpersonal complexity: A cognitive component of person-centered care. The Gerontologist. 2006;46(2):220–226. doi: 10.1093/geront/46.2.220. [DOI] [PubMed] [Google Scholar]
- Mor V, Branco K, Fleishman J, Hawes C, Phillips C, Morris J, Fries B. The structure of social engagement among nursing home residents. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 1995;50(1):P1–P8. doi: 10.1093/geronb/50b.1.p1. [DOI] [PubMed] [Google Scholar]
- My Home Life. Eight Themes. 2012 Jul 8; http://myhomelife.org.uk/research/8-key-themes/ 2012.
- Nakrem S, Vinsnes AG, Seim A. Residents’ experiences of interpersonal factors in nursing home care: A qualitative study. International Journal of Nursing Studies. 2011;48(11):1357–1366. doi: 10.1016/j.ijnurstu.2011.05.012. [DOI] [PubMed] [Google Scholar]
- Nussbaum JF. Relational closeness of elderly interaction: Implications for life satisfaction. Western Journal of Communication. 1983;47(3):229–243. [Google Scholar]
- Palacios-Ceña D, Losa-Iglesias ME, Gómez-Calero C, Cachón-Pérez JM, Brea-Rivero M, Fernández-de-las-Peñas C. A qualitative study of the relationships between residents and nursing homes nurses. Journal of Clinical Nursing. 2013;23(3–4):550–559. doi: 10.1111/jocn.12202. [DOI] [PubMed] [Google Scholar]
- Pioneer Network. Mission, Vision and Values. 2012 Jul 8; http://www.pioneernetwork.net/ 2012.
- Powers BA. The meaning of nursing home friendships. Advances in Nursing Science. 1991;14(2):42–58. doi: 10.1097/00012272-199112000-00006. [DOI] [PubMed] [Google Scholar]
- QSR International Pty Ltd. NVIVO qualitative data analysis software Version 9. 2010. [Google Scholar]
- Quattrochi-Tubin S, Jason LA. Enhancing social interactions and activity among the elderly through stimulus control. Journal of Applied Behavior Analysis. 1980;13(1):159–163. doi: 10.1901/jaba.1980.13-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick HE, Fries BE, Verbrugge LM. Windows to their world: the effect of sensory impairments on social engagement and activity time in nursing home residents. Journals of Gerontology. Series B: Psychological Sciences and Social Sciences. 1997;52(3):S135–144. doi: 10.1093/geronb/52b.3.s135. [DOI] [PubMed] [Google Scholar]
- Schroll M, Jonsson P, Berg K, Sherwood S. An international study of social engagement among nursing home residents. Age and Ageing. 1997;26(Supplement 2):55–59. doi: 10.1093/ageing/26.suppl_2.55. [DOI] [PubMed] [Google Scholar]
- State Government of Victoria Australia. Best care for older people everywhere: Person-centred practice. 2012 Jul 8; http://www.health.vic.gov.au/older/toolkit/02PersonCentredPractice/index.htm 2012.
- Strauss AL, Corbin JM. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Newbury Park: Sage Publications, Inc.; 1998. [Google Scholar]
- Takkinen S, Ruoppila I. Meaning in life in three samples of elderly persons with high cognitive functioning. International Journal of Aging and Human Development. 2001;53(1):51–74. doi: 10.2190/WBUG-NRKM-XJ7A-5QWP. [DOI] [PubMed] [Google Scholar]
- Tsai CF, Ouyang WC, Chen LK, Lan CF, Hwang SJ, Yang CH, Su TP. Depression is the strongest independent risk factor for poor social engagement among Chinese elderly veteran assisted-living residents. Journal of the Chinese Medical Association. 2009;72(9):478–483. doi: 10.1016/S1726-4901(09)70411-3. [DOI] [PubMed] [Google Scholar]
- Tseng S, Wang R. Quality of life and related factors among elderly nursing home residents in Southern Taiwan. Public Health Nursing. 2001;18(5):304–311. doi: 10.1046/j.1525-1446.2001.00304.x. [DOI] [PubMed] [Google Scholar]