Abstract
The cyanobacterial lectin scytovirin (SVN) binds with high affinity to mannose-rich oligosaccharides on the envelope glycoprotein (GP) of a number of viruses, blocking entry into target cells. In this study, we assessed the ability of SVN to bind to the envelope GP of Zaire Ebola virus (ZEBOV) and inhibit its replication. SVN interacted specifically with the protein’s mucin-rich domain. In cell culture, it inhibited ZEBOV replication with a 50% virus-inhibitory concentration (EC50) of 50 nM, and was also active against the Angola strain of the related Marburg virus (MARV), with a similar EC50. Injected subcutaneously in mice, SVN reached a peak plasma level of 100 nm in 45 minutes, but was cleared within 4 hours. When ZEBOV-infected mice were given 30 mg/kg/day of SVN by subcutaneous injection every 6 hours, beginning the day before virus challenge, 9 of 10 animals survived the infection, while all infected, untreated mice died. When treatment was begun one hour or one day after challenge, 70-90% of mice survived. Quantitation of infectious virus and viral RNA in samples of serum, liver and spleen collected on days 2 and 5 postinfection showed a trend toward lower titers in treated than control mice, with a significant decrease in liver titers on day 2. Our findings provide further evidence of the potential of natural lectins as therapeutic agents for viral infections.
Introduction
A number of cyanobacterial lectins bind with high affinity to high-mannose oligosaccharides on viral envelope glycoproteins, preventing virus attachment and entry into target cells (Boyd et al. 1997; Bokesch et al. 2003; Mori et al. 2005). These natural products might therefore be utilized to prevent or treat human viral diseases. One potential target for lectin therapy is the Zaire Ebola virus (ZEBOV), the causative agent of the current epidemic in West Africa. The surface of the EBOV virion bears multiple copies of a heavily glycosylated envelope glycoprotein (GP), which is cleaved by furin into two sub-units, GP1 and GP2, covalently linked by a disulfide bond. GP1 is a ~110 kDa protein that contains complex, hybrid and oligomannose oligosaccharides and a terminal mucin-rich region (Lee et al. 2008). It is responsible both for initiating viral attachment and entry and for evading immune response elements in the host (Takada et al. 1997; Lee, and Saphire 2009).
In an earlier proof-of-concept study, we found that the lectin cyanovirin (CVN), which is highly active against the human immunodeficiency virus (HIV), also inhibits the replication of ZEBOV (Boyd et al. 1997; Barrientos et al. 2003). Mice inoculated with ZEBOV and treated with repeated subcutaneous (s.c.) injections of CVN showed a significant prolongation of the course of illness, compared to untreated animals, but none survived the infection. Those findings suggested that additional lectins should be screened, to identify those with an enhanced ability to inhibit ZEBOV replication.
In the present study, we characterized the anti-ZEBOV activity of the lectin scytovirin (SVN), a 9.7 kDa monomeric protein isolated from the cyanobacterium Scytonema varium (Bokesch et al. 2003). SVN is known to bind with high affinity to the envelope GP of HIV and of the hepatitis C virus (HCV) (Bokesch et al. 2003; Takebe et al. 2013), but its activity against a highly pathogenic virus such as ZEBOV had not been assessed. We found that SVN was more active against ZEBOV than CVN, as it had a lower 50% virus-inhibitory concentration (EC50) in tissue culture and prevented the death of most ZEBOV-infected mice, when treatment was initiated the day before, the day of or the day after virus challenge, while all infected, untreated mice died. As discussed below, our findings suggest that researchers should continue to test other cyanobacterial lectins, to identify those with even greater activity against highly virulent pathogens.
Materials and Methods
SVN production
Scytovirin (SVN) was produced in E. coli and purified as previously described (Xiong et al. 2006). All protein samples were diluted to a final concentration of 1 mg/ml in PBS, as determined by amino acid analysis, and sterile-filtered before use.
Virus and cells
Studies utilizing live ZEBOV and Marburg virus (MARV) were performed in Biosafety Level 4 (BSL-4) facilities at the U. S. Army Medical Research Institute of Infectious Diseases (USAMRIID); personnel wore positive-pressure protective suits fitted with HEPA filters and umbilical-fed air. USAMRIID is registered with the Centers for Disease Control and Prevention (CDC) Select Agent Program for the possession and use of biological select agents and toxins and has implemented a biological surety program in accordance with U. S. Army Regulation AR 50-1 “Biological Surety”. The construction of recombinant ZEBOV encoding green fluorescent protein (ZEBOV-eGFP) has been described (Towner et al. 2005). The virus was provided by John Towner at CDC and amplified in Vero E6 cells. Mouse-adapted ZEBOV has been described (Bray et al. 1998). The Angola strain of MARV was obtained from the USAMRIID collection. Vero E6 cells (ATCC: CRL-1586) were maintained in Eagle’s minimum essential medium (EMEM) supplemented with 10% fetal bovine serum.
In vitro assays for inhibition of ZEBOV-eGFP and MARV replication
For each assay, serial dilutions of SVN were added at a 4× concentration to 96-well plates of Vero E6 cells, which were then transferred to BSL-4 containment. ZEBOV-eGFP or MARV was added at a multiplicity of infection of 0.01. For ZEBOV, the plates were incubated for 48 hr and then read on a spectrofluorometer (Molecular Devices, Sunnyvale CA) at an excitation wavelength of 485 nm. For assays of MARV inhibition, the plates were incubated for 48 hours, then assayed for viral antigen by an immunofluorescence method using the 9G4 monoclonal antibody, as previously described (Radoshitzky et al. 2011). To confirm that decreases in fluorescence did not reflect cellular toxicity, uninfected cells were treated with the same concentrations of SVN and incubated for 48 hr, and their viability was assessed by an ATP-based method (Cell Titer-Glo, Promega, Madison, WI).
ELISA of scytovirin binding to EBOV-infected cell lysates or recombinant GP1
Recombinant ZEBOV GP1 (rGP1) and the protein lacking the mucin region (rGP1ΔMuc) were provided by Dr. Erica Ollman Saphire, Scripps Research Institute. Wells of a 96-well protein binding plate (Nunc Immunosorp, Thermo Scientific, Waltham, MA) were inoculated with 100 ng of a EBOV-infected cell lysate, rGP1 or rGP1ΔMuc and allowed to incubate for 2 hr. The plate was then washed with PBS-0.5% Tween 20 and blocked overnight at 4° C with Superblock Buffer in PBS-Tween 20 (Pierce, Rockford, IL). The plate was washed three times and SVN was then added to triplicate wells at concentrations of 0.001-10 pmol/well and allowed to incubate for 2 hrs. After washing, the plate was incubated with a 1:1000 dilution of rabbit polyclonal anti-SVN IgG for 1hr, followed by washing, incubation with a 1:5000 dilution of goat-anti-rabbit secondary antibodies ligated to horseradish peroxidase (HRP) (Immunopure, Thermo Scientific, Waltham, MA), washing and addition of HRP substrate (Kirkegaard & Perry Laboratories, Gaithersburg, MD). The reaction was stopped by the addition of H2SO4 and absorbance was measured at 450 nm. All tests were performed in triplicate.
Western blots of ZEBOV-infected cell lysates and rGP1
Infected cell lysates and purified GP1 were electrophoresed by SDS-PAGE into a Tris-glycine 8 to 16% acrylamide gel (Invitrogen, Carlsbad, CA) under reducing conditions. Gels were stained with SimplyBlue SafeStain (Invitrogen, Carlsbad, CA) or blotted onto polyvinylidene difluoride (PVDF) membranes at a constant voltage of 25 volts for 2 hr. Membranes were blocked overnight at 4°C with Superblock Buffer in PBS containing 0.05% Tween 20. After washing, the membranes were incubated with buffered solutions of SVN (0.1 μg/ml) for 1 hr at room temperature, washed and incubated with polyclonal rabbit anti-SVN antibodies for 1 hr, washed, then incubated with goat anti-rabbit-HRP antibodies for 1 hr and washed again. Binding was detected with electrochemiluminescent reagents (Amersham, Buckinghamshire, UK).
Bioavailability of injected SVN in mice
Four-8-week old BALB/c mice were obtained from the National Cancer Institute, Frederick, MD and housed under specific pathogen-free conditions. For bioavailability studies, 33 mice were injected s.c. with 10 mg/kg of SVN or with PBS; 3 mice were then sacrificed at each of 11 time points from 15 min to 48 hrs after injection, their blood was collected and the plasma separated. The concentration of SVN in the plasma of treated mice was determined using an adaptation of a method previously published for use with CVN (McFeeters et al. 2007). Briefly, wells of a 96-well plate were incubated with 100 ng/well of recombinant HIV-1 GP120 (Intracel, Columbia MD); after 2 hr, the wells were washed and then blocked overnight with 2% BSA in PBS. Subsequently, 50 μl of mouse plasma from varying time points was added to triplicate wells. After 2 hr incubation and repeat washing, binding of SVN was visualized by the antibody-bound HRP method described above. Samples with known concentrations of SVN in mouse plasma were tested on the same plate to provide a calibration curve for quantitation of the SVN in test samples.
Drug efficacy studies in EBOV-infected mice
Virus challenge of BALB/c mice was performed by inoculating each animal intraperitoneally (i.p.) with 1000 plaque-forming units (pfu) of mouse-adapted ZEBOV (Bray et al. 1998). Treated mice were inoculated s.c. with 10, 20 or 30 mg/kg of SVN per day, divided into four equal doses given approximately every 6 hours; control mice received PBS in the same manner. One group was treated beginning 24 hours before virus challenge, with doses at −18, −12 and −6 hours, then one hour after infection and continuing every 6 hours. A second group was treated beginning 1 hr after virus challenge and a third beginning 24 hr after challenge. All groups were treated for a total of 10 days, and were monitored daily through day 28 for weight loss and survival. To assess adaptive immunity, the surviving mice and a naive control group were challenged with mouse-adapted EBOV at day 28 and monitored daily for additional 28 days.
Quantitation of infectious virus by plaque assay and of viral RNA by qRT/PCR
Two experiments in mice were performed to determine titers of viral RNA and infectious virus in plasma and tissues. They were performed in the same manner as the efficacy studies just described, except that, instead of following the entire cohort for survival, some animals were sacrificed at various time points for plasma and tissue collection. As above, treated mice received 30mg/kg of SVN per day, divided into 4 s.c. doses, and control mice received PBS. In the first experiment, 3 mice were sacrificed on days 2, 5, 8 and 10; in the second, 5 mice were sacrificed on days 0, 0.5, 1, 2, 5, 6, 8, and 10. Titers of infectious virus in plasma and homogenized tissue were determined by the plaque assay method (Moe et al. 1981), in which 6-well plates of Vero E6 cells were infected with serial dilutions of samples in EMEM, followed by an agarose overlay and neutral red staining on day 7. Copy numbers of viral RNA in plasma and homogenized tissue were determined, based on detection of a viral nucleoprotein (NP) sequence by qRT-PCR. Samples were inactivated by the addition of Trizol LS (Invitrogen, Carlsbad, CA); extraction of viral RNA was obtained by mixing the inactivated sample with chloroform and incubating, then isolation of the aqueous phase through ethanol precipitation and centrifugation. This method was first described by Weidmann et al (2004).
Histologic and immunohistologic studies
Liver, spleen, lungs and other tissues were collected at necropsy and preserved in 10% phosphate buffered formalin. Paraffin-embedded sections were stained by hematoxylin and eosin (H & E) and examined by light microscopy. Immunohistochemical staining using a polyclonal rabbit anti-EBOV antibody (R1645), kindly provided by Cindy Rossi at USAMRIID, was performed using standard methods (Raymond et al. 2011).
Statistical analysis
For animal experiments involving the measurement of weight loss over time, we used two-way ANOVA to assess differences in weight loss between treated and control groups, with stepdown Bonferroni adjustment for pairwise comparisons.. We used Fisher’s exact test to compare survival rates among groups, and a t-test to evaluate differences in geometric mean virus titers (GMT) in tissue and serum samples. Significance was set with a confidence interval of 95% and a p value < 0.05. All analyses were performed using GraphPad Prism® (GraphPad, La Jolla, CA).
Results
SVN inhibits ZEBOV and MARV replication in vitro
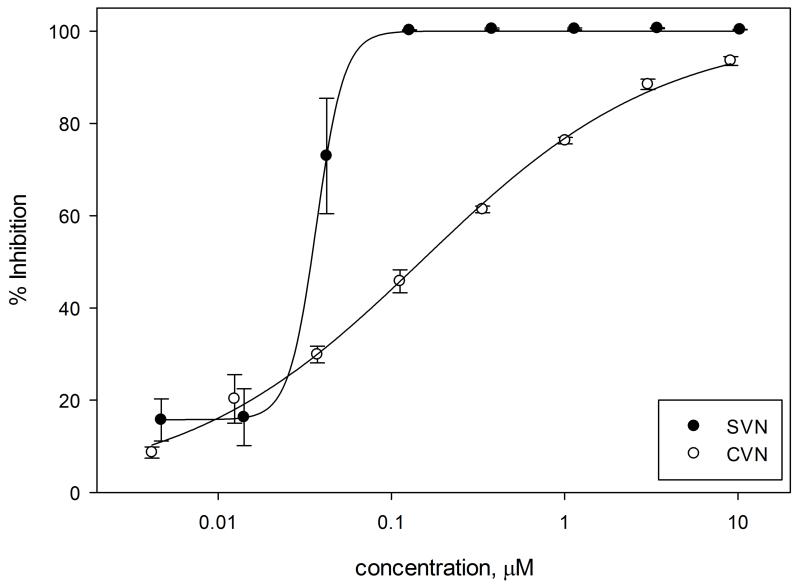
SVN inhibited the replication of EBOV-eGFP in Vero E6 cells with an EC50 of 41 nM, which was lower than the level for CV-N tested simultaneously (EC50 = 154 nM) (Figure 1). SVN also inhibited the replication of MARV, with an EC50 similar to that for ZEBOV (Figure S1). Testing of cellular viability by an ATP-based assay failed to detect cytotoxicity at the more than 200-fold higher SVN concentration of 10.3 μM (Figure S2). Similarly, when other researchers tested SVN in Huh 7.5.1 cells, it showed no toxicity at concentrations up to 2 μM (Takebe et al, 2013). These results differed significantly from CV-N, which was cytotoxic at levels as low as 4 μM (Barrientos et al. 2003).
Figure 1. SVN and CV-N inhibit ZEBOV replication in vitro.
SVN (red circles) and CV-N (black squares) were tested for inhibitory activity against ZEBOV in Vero E6 cells, using a recombinant GFP-encoding virus. SVN exhibited an EC50 of 41 nM, while CV-N was found to have an EC50 = 154 nM. The data shown are the average of triplicate experiments; error bars indicate standard deviations.
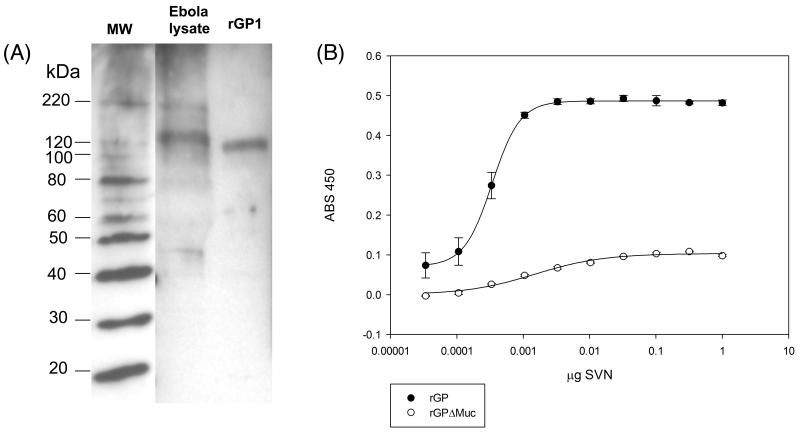
SVN binds to ZEBOV GP1
Western blotting showed that SVN bound specifically to a 120 kDA target in the ZEBOV-infected cell lysate, which migrated in parallel with rGP1 (Figure 2A). By ELISA, SVN showed increasing concentration-specific binding to rGP1 however, rGP1 lacking the mucin domain (rGP1ΔMuc) showed significantly reduced SVN binding indicating that the mucin domain is an important target for SVN (Figure 2B).
Figure 2. SVN binds to the mucin-rich region of ZEBOV GP1.
A. Western blot analysis showed that SVN bound predominantly to a single ~120 kDa protein in a EBOV-infected cell lysate, corresponding to GP1 (Lane 2), and to recombinant GP1 (Lane 3). Molecular weight markers (MW) are from a Coomassie stain of the corresponding SDS-PAGE gel. B. ELISA showing binding of SVN to rGP1 and rGP1ΔMuc. The data shown are the average of triplicate experiments; error bars indicate standard deviations.
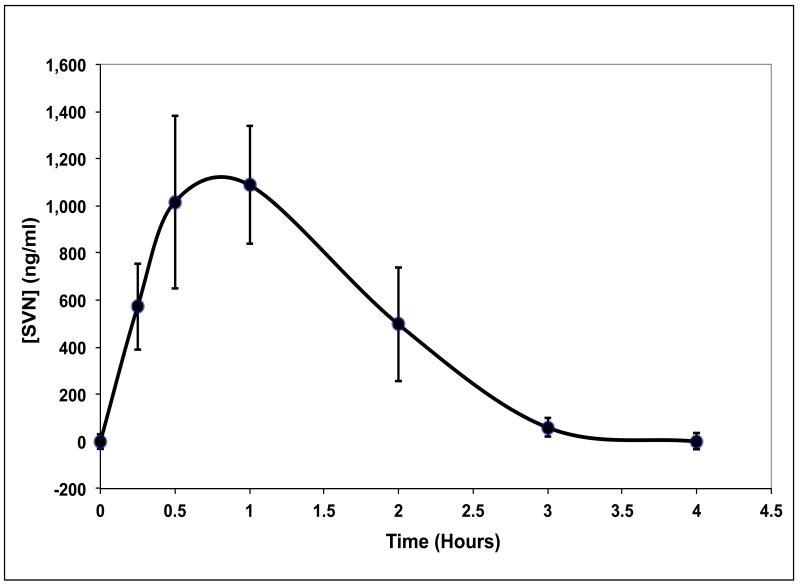
Injected SVN is bioavailable
The serum concentration of SVN peaked approximately 45 min after s.c. injection at a level of 1.1 μg/ml (113 nM) and decreased to baseline levels by 4 hr (Figure 3). The peak serum level was thus approximately twice the EC50 of SVN in cell culture.
Figure 3. SVN persists in the serum in mice for up to 4 hours.
Mice (n = 3 per time point, 33 total) were injected SC with 10 mg/kg SVN and 3 were euthanized at each indicated time point. The level of SVN in plasma was measured by HIV-1 gp120 capture ELISA. Each time point is the average of triplicate experiments; error bars indicate standard deviations.
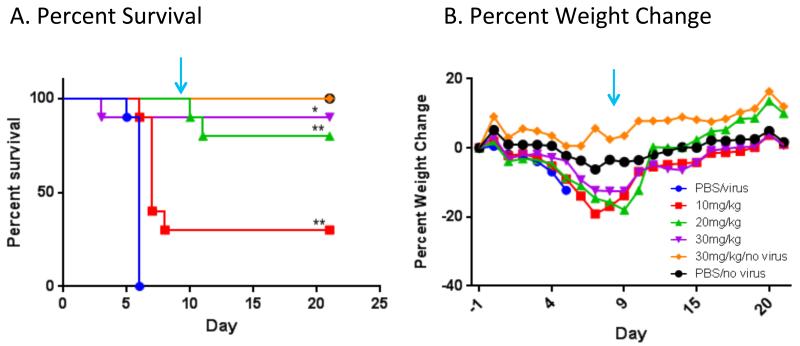
Treatment with SVN protects mice against lethal ZEBOV challenge
Treatment initiated on the day before virus inoculation was highly effective in preventing death from ZEBOV infection (Figure 4A). All mice given PBS succumbed to infection by day 6, while 90% of the mice that received 30 mg/kg/day of SVN beginning on day −1 survived. Those treated with 20 or 10 mg/kg/day showed 80% and 30% survival rates respectively. Infected, treated mice lost weight beginning on day 4-5, but started to regain weight on days 9-10 (Figure 4B). Uninfected control mice that received 30 mg/kg/day of SVN showed no weight loss or other signs of drug toxicity. Treated mice that survived infection were challenged a second time approximately 3 months later with ZEBOV and all survived; however, mice that were in a simultaneously infected control group (previously treated with 30 mg SVN but not challenged with ZEBOV) died (data not shown).
Figure 4. SVN treatment protects mice when begun before virus challenge.
Groups of 10 mice were injected s.c. every 6 hours, beginning 24 hr before virus challenge, to give a total daily dose of 10 (red square), 20 (green triangle) or 30 (purple triangle) mg/kg. The initial doses were given at −24, −18, −12 and −6 hr, then 1 hr after i.p. virus challenge, and continuing every 6 hr through day 9 (arrow). Control groups were infected and treated with PBS (blue circle), or were left uninfected (black circle) and given a total daily dose of 30 mg/kg of SVN (orange diamond). A. Percent survival. A log-rank test was performed to compare survival of treated and untreated, infected mice; (*) denotes statistical significance with a 95% CI and p = 0.0006, while (**) denotes p < 0.0001. B. Percent weight change relative to mean group weight on day −1. A two-way ANOVA was performed and no significant difference was found in the weight changes between treatment groups and the uninfected, PBS-treated control group.
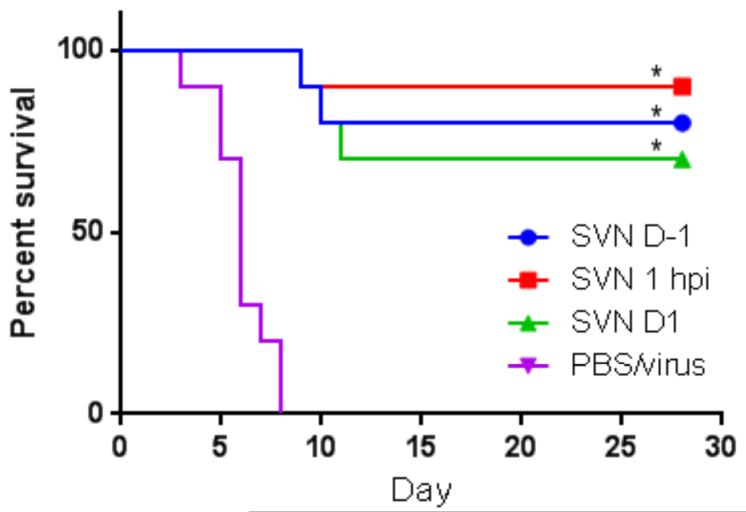
In a second experiment, SVN treatment was initiated 1 hr or 1 day after virus challenge, with the same regimens used in the first study. All control mice succumbed to infection by day 10, while 80% of the mice treated at day-1, 90% of those treated at +1 hr and 70% of those treated at day +1 survived infection (Figure 5).
Figure 5. SVN treatment protects mice when begun before or after virus challenge.
Groups of 10 mice were injected every 6 hours with a total daily dose of 30 mg/kg, beginning 24 hr before (see description in previous figure) (blue circle), 1 hr after (red square) or 24 hours after (green triangle) ZEBOV challenge, continuing through day 9 (arrow). A control group (purple inverse triangle) received PBS beginning 1 hr after challenge. A log-rank test was performed, comparing treated and untreated groups; (*) denotes statistical significance, with a 95% CI and p < 0.0001.
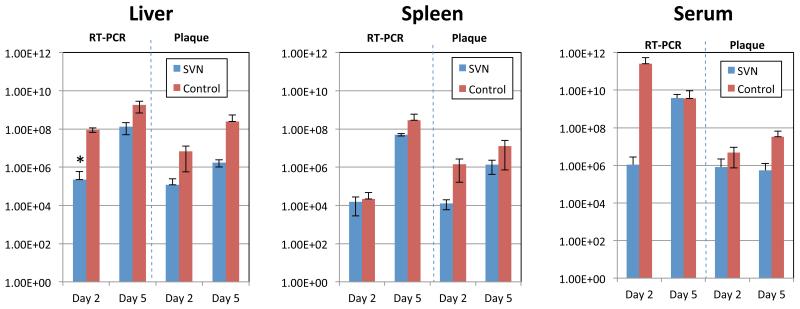
SVN therapy reduces ZEBOV titers in serum and tissues
Levels of infectious virus and viral RNA in serum, liver and spleen on days 2 and 5 post-infection were determined for mice treated with 30 mg/kg/day of SVN or with PBS, beginning the day before virus challenge (Figure 6). Titers of infectious virus were consistently lower in samples from treated than untreated animals, with decreases ranging from roughly 10-fold to more than 100-fold. As expected, copy numbers of viral RNA tended to be higher than titers of infectious virus in the same samples. Except for approximately equal titers in serum on day 5, SVN-treated mice had lower viral RNA levels than controls, but the extent of the decrease was more variable than for infectious virus. A repeat experiment gave similar results (data not shown).
Figure 6. SVN treatment reduces titers of infectious virus and viral RNA in serum and tissues.
Mice (n = 3) either untreated or treated beginning 1 hr after ZEBOV challenge with 30 mg/kg/day of SVN were sacrificed on days 2 and 5 postinfection. Samples of serum, spleen and liver were collected and assayed for infectious virus by plaque formation on Vero E6 cells and for levels of viral RNA by RT-PCR. SVN-treated samples are represented by blue bars and PBS controls by red bars. Error bars indicate standard deviation for three independent samples from three mice. There was a consistent trend toward lower mean viral titers in treated than untreated mice, but compariso by t-test found a statistically significant difference in only one sample set (*), with a 95% CI and p = 0.0221.
SVN therapy reduces tissue injury in ZEBOV-infected mice
The principal histologic abnormality in infected, untreated mice was extensive hepatic inflammation and necrosis, which corresponded with the presence of large amounts of viral antigen in hepatocytes and Kupffer cells (Supplemental Figure 3, A and B). Only minimal changes were seen in the livers of SVN-treated mice (C and D). Significant differences were also seen in the lungs, which showed mild inflammatory changes in treated mice (E), but moderate to severe pneumonia in control animals (F). Splenic lymphocytolysis and myocarditis were observed in less than half of untreated, infected mice, but were absent in SVN-treated animals (not shown).
Discussion
The current epidemic of Ebola virus disease in West Africa has made it clear that safe and effective countermeasures are urgently needed against this devastating infection. Several approaches, including various small molecules and monoclonal antibodies, have proven beneficial for pre- and postexposure prophylaxis in ZEBOV-infected nonhuman primates, but none is yet approved for human use (Wong et al. 2014). Although cyanobacterial lectins are still in an early stage of development, we believe they hold promise as broad-spectrum antiviral agents, because their affinity for oligosaccharides commonly found on viral surface glycoproteins would allow them to inhibit many different pathogens.
In an earlier paper, we reported that treatment with the lectin CVN slowed the progression of illness in ZEBOV-infected mice, but did not prevent death (Barrientos et al. 2003). The present study has shown that SVN is a more potent inhibitor of ZEBOV replication than CVN. Its antiviral activity appears to result from specific binding to the mucin region of the enveloped GP, which is rich in N-linked high-mannose oligosaccharides (Lee and Saphire 2009) (Ritchie et al. 2010). A dose of 30 mg/kg/day of SVN produced no signs of toxicity, was protective in the majority of the mice when started the day before challenge, and prevented the death of nearly all mice when begun the day before or the day after challenge, suggesting that this lectin might be used in either a prophylactic or a therapeutic role for human ZEBOV infections. The fact that SVN was equally potent when begun the day before or the day after virus challenge indicates that its effects extend beyond the first round of infection. Since treated animals become ill and lose weight, it is apparent that SVN slows the progress of ZEBOV infection, rather than blocking it completely.
An interesting observation from our study is that only partial suppression of ZEBOV replication was needed to bring about survival. Under experimental conditions in which nearly all treated mice survived, but all control mice died, there was a general trend for titers of infectious virus in the serum, liver and spleen of treated mice on days 2 and 5 postinfection to be roughly 10- to 100-fold lower than in control animals (Figure 6). Levels of viral RNA, as measured by RT-PCR, appeared to be more variable, but were generally lower in treated mice at both time points; however, a statistically significant difference was only observed in liver tissue on day 2. The occurrence of considerable viral replication in mice that survived infection resembles that seen in some earlier evaluations of experimental ZEBOV therapy, such as an assessment of the small-molecule inhibitor FGI-103, which found that virus titers in the serum and tissues of treated mice differed by less than 100-fold at days 4 and 6 post-infection from those of controls (Warren et al. 2010). It is also consistent with some studies in macaques, such as treatment with the anticoagulant rNAPc2, in which animals that survived infection developed peak serum virus titers approaching 104 pfu/mL, while mean titers were approximately10-fold higher in treated macaques that showed a delay in death and 100-fold higher in fatally infected controls (Geisbert et al. 2003). However, more effective reduction in circulating virus in ZEBOV-infected macaques has recently been achieved by monoclonal antibody therapy, which resulted in complete suppression of viremia (Pettitt et al. 2013).
Although SVN was highly protective in ZEBOV-infected mice, its short serum persistence required dosing every 6 hours, a significant burden for researchers in Biosafety Level 4 containment and a disadvantage for any potential human therapy. A lectin that possesses SVN’s strong antiviral activity, but a longer serum half-life, would therefore be highly desirable. We have recently shown that griffithsin, a red algal lectin that binds high-mannose oligosaccharides in a manner similar to CVN and SVN, has a remarkably long serum persistence in mice, and could still be detected two weeks after a single high-dose inoculation (Barton et al. 2014). Griffithsin is now being evaluated for its protective efficacy against EBOV. Given the inherent stability of lectins and their potential for large-scale production (O’Keefe et al. 2009), we believe that these proteins have promise as therapeutic agents against ZEBOV and other highly pathogenic filoviruses.
Supplementary Material
Supplemental Figure 1. SVN shows no toxicity for Vero E6 cells. Concentrations of SVN up to 10.3 μM in EMEM were added to cultured Vero E6 cells and the cells were incubated for 48 hrs prior to assessment of viability by Cell TiterGlo assay. The assay was performed in duplicate (red squares and blue diamonds) with the average at each dose shown as a green bar.
Supplemental Figure 2. SVN displays in vitro inhibitory activity against MARV. SVN was tested for the ability to inhibit the replication of the Angola strain of MARV in Vero E6 cells, as measured by an ELISA assay for MARV antigen. SVN exhibited an EC50 of 260 nM. The data shown are the average of duplicate experiments.
Supplemental Figure 3. ZEBOV-infected mice treated with SVN have minimal tissue injury. (A). H & E-stained sections of liver from untreated mice show extensive coagulative necrosis (star). (B) Immunohistochemical staining for viral VP40 reveals large amounts of antigen in hepatocytes and Kupffer cells (arrow). Corresponding samples from treated mice show normal hepatocellular architecture (C, arrow) and lack of viral antigen (D). Lung sections show a mild degree of interstitial pneumonitis in treated mice (E), but moderate to severe pneumonia with abundant neutrophilic infiltrates in untreated controls (F).
Garrison et al. 2014 highlights revised.
The cyanobacterial lectin scytovirin inhibits the replication of Zaire ebolavirus and marburgvirus in vitro.
Scytovirin binds to the mucin domain of the ebolavirus glycoprotein.
The compound caused no detectable toxicity in cell culture assays or in mice.
Treatment of mice beginning the day before, the day of or the day after ZEBOV challenge resulted in 70-90% survival.
The short persistence of scytovirin in the serum necessitated s.c. dosing every 6 hours.
Acknowledgements
This research was supported by the Intramural Research Program of the NIH, National Cancer Institute, Center for Cancer Research and the NIAID Trans-NIH/FDA Biodefense Grant Program. This project has been funded in whole or in part with federal funds from the Frederick National Laboratory for Cancer Research, National Institutes of Health, under contract HHSN261200800001E. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. Opinions, interpretations, conclusions, and recommendations are those of the author and are not necessarily endorsed by the U.S. Army.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Ethics statement
Animal research was conducted under an IACUC approved protocol at USAMRIID (USDA Registration Number 51-F-0021/728 & OLAW Assurance number A3473-01) in compliance with the Animal Welfare Act and other federal statutes and regulations relating to animals and experiments involving animals. The facility where this research was conducted is fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care, International and adheres to principles stated in the Guide for the Care and Use of Laboratory Animals, National Research Council, 2011.
References
- Barrientos LG, O’Keefe BR, et al. Cyanovirin-N binds to the viral surface glycoprotein, GP1,2 and inhibits infectivity of Ebola virus. Antiviral Res. 2003;58(1):47–56. doi: 10.1016/s0166-3542(02)00183-3. [DOI] [PubMed] [Google Scholar]
- Barton C, Kouokam JC, et al. Activity of and effect of subcutaneous treatment with the broad-spectrum antiviral lectin griffithsin in two laboratory rodent models. Antimicrob Agents Chemother. 2014;58(1):120–127. doi: 10.1128/AAC.01407-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bokesch HR, O’Keefe BR, et al. A potent novel anti-HIV protein from the cultured cyanobacterium Scytonema varium. Biochemistry. 2003;42(9):2578–2584. doi: 10.1021/bi0205698. [DOI] [PubMed] [Google Scholar]
- Boyd MR, Gustafson KR, et al. Discovery of cyanovirin-N, a novel human immunodeficiency virus-inactivating protein that binds viral surface envelope glycoprotein gp120: potential applications to microbicide development. Antimicrob Agents Chemother. 1997;41(7):1521–1530. doi: 10.1128/aac.41.7.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray M, Davis K, et al. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis. 1998;178(3):651–661. doi: 10.1086/515386. [DOI] [PubMed] [Google Scholar]
- Dias JM, Kuehne AI, et al. A shared structural solution for neutralizing ebola viruses. Nat Struct Mol Biol. 2011;18(12):1424–7. doi: 10.1038/nsmb.2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisbert TW, Hensley LE, et al. Treatment of Ebola virus infection with a recombinant inhibitor of factor VIIa/tissue factor: a study in rhesus monkeys. Lancet. 2003;362(9400):1953–1958. doi: 10.1016/S0140-6736(03)15012-X. [DOI] [PubMed] [Google Scholar]
- Lee JE, Fusco ML, et al. Structure of the Ebola virus glycoprotein bound to an antibody from a human survivor. Nature. 2008;454(7201):177–82. doi: 10.1038/nature07082. 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JE, Saphire EO. Ebola virus glycoprotein structure and mechanism of entry. Future Virol. 2009;4(6):621–635. doi: 10.2217/fvl.09.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFeeters RL, Xiong C, et al. The novel fold of scytovirin reveals a new twist for antiviral entry inhibitors. J Mol Biol. 2007;369(2):451–461. doi: 10.1016/j.jmb.2007.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moe JB, Lambert RD, et al. Plaque assay for Ebola virus. J Clin Microbiol. 1981;13(4):791–793. doi: 10.1128/jcm.13.4.791-793.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mori T, O’Keefe BR, et al. Isolation and characterization of griffithsin, a novel HIV-inactivating protein, from the red alga Griffithsia sp. J Biol Chem. 2005;280(10):9345–53. doi: 10.1074/jbc.M411122200. [DOI] [PubMed] [Google Scholar]
- O’Keefe BR, Vojdani F, et al. Scaleable manufacture of HIV-1 entry inhibitor griffithsin and validation of its safety and efficacy as a topical microbicide component. Proc Natl Acad Sci U S A. 2009;106(15):6099–104. doi: 10.1073/pnas.0901506106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettitt J, Zeitlin L, et al. Therapeutic intervention of Ebola virus infection in rhesus macaques with the MB-003 monoclonal antibody cocktail. Sci Transl Med. 2013;5(199):199ra113. doi: 10.1126/scitranslmed.3006608. [DOI] [PubMed] [Google Scholar]
- Radoshitzky SR, Warfield KL, et al. Ebola virus delta-peptide immunoadhesins inhibit marburg virus and ebola virus cell entry. J Virol. 2011;85(17):8502–13. doi: 10.1128/JVI.02600-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymond J, Bradfute S, et al. Filovirus infection of STAT-1 knockout mice. J Infect Dis. 2011;204(Suppl 3):S986–990. doi: 10.1093/infdis/jir335. [DOI] [PubMed] [Google Scholar]
- Ritchie G, Harvey DJ, et al. Identification of N-glycans from Ebola virus glycoproteins by matrix-assisted laser desorption/ionisation time-of-flight and negative ion electrospray tandem mass spectrometry. Rapid Commun Mass Spectrom. 2010;24(5):571–585. doi: 10.1002/rcm.4410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada A, Robison C, et al. A system for functional analysis of Ebola virus glycoprotein. Proc Natl Acad Sci U S A. 1997;94(26):14764–9. doi: 10.1073/pnas.94.26.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takebe Y, Saucedo CJ, et al. Antiviral lectins from red and blue-green algae show potent in vitro and in vivo activity against hepatitis C virus. PLoS One. 2013;8(5):e64449. doi: 10.1371/journal.pone.0064449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towner JS, Paragas J, et al. Generation of eGFP expressing recombinant Zaire ebola virus for analysis of early pathogenesis events and high-throughput antiviral drug screening. Virology. 2005;332(1):20–27. doi: 10.1016/j.virol.2004.10.048. [DOI] [PubMed] [Google Scholar]
- Warren TK, Warfield KL, et al. Antiviral activity of a small-molecule inhibitor of filovirus infection. Antimicrob Agents Chemother. 2010;54(5):2152–2159. doi: 10.1128/AAC.01315-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weidmann M, Muhlberger E, et al. Rapid detection protocol for filoviruses. J Clin Virol. 2004;30(1):94–99. doi: 10.1016/j.jcv.2003.09.004. [DOI] [PubMed] [Google Scholar]
- Wong G, Qiu W, et al. Post-exposure therapy of filovirus infections. Trends Microbiol. 2014;22(8):456–463. doi: 10.1016/j.tim.2014.04.002. [DOI] [PubMed] [Google Scholar]
- Xiong C, O’Keefe BR, et al. Overexpression and purification of scytovirin, a potent, novel anti-HIV protein from the cultured cyanobacterium Scytonema varium. Protein Expr Purif. 2006;46(2):233–239. doi: 10.1016/j.pep.2005.09.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. SVN shows no toxicity for Vero E6 cells. Concentrations of SVN up to 10.3 μM in EMEM were added to cultured Vero E6 cells and the cells were incubated for 48 hrs prior to assessment of viability by Cell TiterGlo assay. The assay was performed in duplicate (red squares and blue diamonds) with the average at each dose shown as a green bar.
Supplemental Figure 2. SVN displays in vitro inhibitory activity against MARV. SVN was tested for the ability to inhibit the replication of the Angola strain of MARV in Vero E6 cells, as measured by an ELISA assay for MARV antigen. SVN exhibited an EC50 of 260 nM. The data shown are the average of duplicate experiments.
Supplemental Figure 3. ZEBOV-infected mice treated with SVN have minimal tissue injury. (A). H & E-stained sections of liver from untreated mice show extensive coagulative necrosis (star). (B) Immunohistochemical staining for viral VP40 reveals large amounts of antigen in hepatocytes and Kupffer cells (arrow). Corresponding samples from treated mice show normal hepatocellular architecture (C, arrow) and lack of viral antigen (D). Lung sections show a mild degree of interstitial pneumonitis in treated mice (E), but moderate to severe pneumonia with abundant neutrophilic infiltrates in untreated controls (F).