Abstract
Objective
To assess the time-trends in utilization, clinical characteristics and outcomes of patients undergoing total ankle arthroplasty (TAA) in the U.S.
Methods
We used the Nationwide Inpatient Sample (NIS) data from 1998 to 2010 to examine time-trends in the utilization rates of TAA. We used the Cochran Armitage test for trend to assess time-trends across the years and the analysis of variance (ANOVA), Wilcoxon test or chi-squared test (as appropriate) to compare the first (1998–2000) and the last time periods (2009–10).
Results
TAA utilization rate increased significant from 1998 to 2010: 0.13 to 0.84 per 100,000 overall, 0.14 to 0.88 per 100,000 in females and from 0.11 to 0.81 per 100,000 in males (p<0.0001 for each comparison for time-trends). Compared to the 1998–2000, those undergoing TAA in 2009–10: were older (41% fewer patients <50 years, p<0.0001); less likely to have RA as the underlying diagnosis (55% fewer patients, p=0.0001); more likely to have Deyo-Charlson index of two or more (197% more, p=0.0010); and had a shorter length of stay at 2.5 days (17% reduction, p<0.0001). Mortality was rare, ranging 0 to 0.6% and discharge to inpatient facility ranged 12.6–14.1%; we noted no significant time-trends in either (p>0.05).
Conclusions
The utilization rate of TAA increased rapidly in the U.S. from 1998 to 2010, but post-arthroplasty mortality rate was stable. Underlying diagnosis and medical comorbidity changed over time and both can impact outcomes after TAA. Further studies should examine how the outcomes and complications of TAA have evolved over time.
Keywords: Ankle arthroplasty, time-trends, utilization, sex, outcomes
Introduction
Total ankle arthroplasty (TAA) is a surgical treatment for end-stage ankle joint disease (1, 2), an alternative to ankle arthrodesis (3). The introduction of the new generation of ankle prostheses and associated improved outcomes (4–7), has likely led to a rapid increase in its popularity. Recent studies reported an improved 5-year survival of TAA implant at 83–86% in two arthroplasty registers (8, 9). Rates of ankle surgery (combined arthrodesis and TAA) in California peaked in the mid-1990s (10), but declined in the recent years from mid 1990s. Compared to 1983–1987, the relative risk of ankle surgery was 21% higher in 1993–1997 but 39% lower in 2003–2007 (10). This recent decline is ankle surgery rate (that included TAA) is in contrast to rapidly increasing rates of knee, hip and shoulder joint arthroplasty in the recent years (11–13). It is unclear why TAA rates should be declining, while the rates of all other arthroplasties are increasing.
To our knowledge, there are no published studies of time-trends in TAA using nationally representative data. A recent 10-year study using the national inpatient sample compared characteristics and outcomes TAA and ankle arthroplasty (14). The study examined time-trend in TAA volume and patient age from 2000–2010, but did not examine any time-trends in other patient characteristics or outcomes post-TAA and did not examine time-trends by age group or sex. Our objective was to assess the time-trends in patient characteristics and outcomes after TAA for the last 13-years in the U.S. using the Nationwide Inpatient Sample (NIS). We hypothesized that over the last 13-years (a) the utilization rates of TAA have increased, (b) the patient characteristics have changed, and (3) that the outcomes, i.e., length of hospital stay, proportion discharged to home and post-arthroplasty mortality, have improved.
Methods
Data Source
We used the data from the NIS from 1998 to 2010. The NIS is the largest all-payer inpatient care database that is publicly available in the United States, containing data from 5 to 8 million hospital stays and discharges from >1,000 hospitals sampled to approximate a 20-percent stratified sample of U.S. community hospitals; 45 states provide data in the NIS database that comprise over 96 percent of the U.S. population (15). The NIS provides data on hospital inpatient stays on all patients regardless of the payer and includes patients covered by Medicare, Medicaid, private insurance and the uninsured. It has been used to analyze national trends in health care utilization, and study quality of care and outcomes of various conditions during the inpatient stay (16–19). For each hospital admission, the International Classification of Diseases, ninth revision common modification (ICD-9-CM) diagnostic and procedure information are available. The NIS can be weighted to produce national estimates. The data are publically available for analyses. The Institutional Review Board (IRB) at University of Alabama at Birmingham approved the study.
Study Cohort and Covariates
For each Calender year starting from 1998, we identified patients in the NIS dataset with the ICD-9-CM procedure code of 81.56 for Total ankle arthroplasty (TAA). We abstracted patient demographic and clinical characteristics including age (<50, 50–64, 65–79 and ≥80 years), sex, underlying diagnosis (osteoarthritis (OA), rheumatoid arthritis (RA), avascular necrosis of the bone (AVN), fracture, traumatic arthroplasty and other conditions). Comorbidity was assessed using the Deyo-Charlson index, a validated measure of comorbidity, consisting of 17 comorbidities, based on the presence of ICD-9-CM codes at the index admission preoperatively (20). Hospital length of stay was calculated as the number of days from admission to discharge for the index TAA admission (the length of stay variable). Mortality was assessed using the mortality variable, which combines death either in the hospital, medical facility, home or place unknown related to the index admission.
Patient’s discharge status was categorized as discharge to: (1) an inpatient facility that included the short term hospital, skilled nursing facility, intermediate care facility or another type of inpatient facility; or (2) to home with or without home health care. Patients who died in the hospital or left the hospital against medical advice were set to missing. We categorized the annual hospital volumes for TAA as <5, 5–9, 10–14, 15–24 and ≥25 procedures, based on a review of overall frequency distribution. We divided the calendar years a priori into roughly equal intervals as follows: 1998 – 2000, 2001 – 2002, 2003 – 2004, 2005 – 2006, 2007 – 2008 and 2009 – 2010.
Statistical Analyses
The utilization rates for TAA per 100,000 population for each year were calculated by dividing the estimates by the total population in the respective category, for overall and age-stratified utilization rates. The 95% confidence interval was calculated based on binomial proportions. We used the Cochran Armitage test for trend to assess time-trends across the years and the analysis of variance (ANOVA), Wilcoxon or chi-squared test (as appropriate) to compare the first and the last time periods. The tables show the crude (unweighted) estimates. Data weights were applied to obtain weighted estimates (http://www.hcup-us.ahrq.gov/reports/methods/2003_2.jsp#as) as recommended, presented in figures. Total U.S. population obtained from the U.S. census site (http://www.census.gov/compendia/statab/cats/population.html) was used to calculate TAA utilization rates and arthrodesis rates for the U.S. population, for the respective year. Mortality, length of stay and discharge disposition were compared by each time-period.
Results
Overall clinical and demographic characteristics
3,187 patients in the NIS sample underwent TAA between 1998 and 2010. The mean age of patients undergoing TAA was 61 year and 54% were female (Table 1). The underlying diagnosis was OA in 62%, RA in 7%, avascular necrosis in 1%, traumatic arthropathy in 18% and unspecified arthropathy/other in 12% (Table 1).
Table 1.
Characteristics of patients undergoing primary total ankle arthroplasty
| All patients | Study time-periods | Comparison of 2009–10 (last) to 1998–00 (first) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| 1998–2010 | 1998–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 | 2009–2010 | Last – first period (% difference) | p-value | |
|
|
|||||||||
| Total | 3,187 | 390 | 545 | 524 | 346 | 538 | 844 | -- | -- |
| Mean Age | 61 (12.7) | 58 (14.0) | 59 (13.2) | 60 (12.4) | 62 (12.6) | 63 (11.6) | 62 (12.2) | 6.9% | <0.0001 |
| % female | 53.9 | 49.7 | 55.8 | 57.8 | 53.8 | 54.8 | 51.7 | 3.9% | 0.49 |
| Age group | |||||||||
| <50 | 18.1 | 24.9 | 23.8 | 19.7 | 15.3 | 13.2 | 14.6 | −41.4% | <0.0001 |
| 50–64 | 38.7 | 35.6 | 38.3 | 42.7 | 39.0 | 36.2 | 39.1 | 9.7% | 0.24 |
| 65–79 | 38.6 | 36.4 | 35.6 | 31.3 | 40.5 | 46.1 | 40.5 | 11.3% | 0.16 |
| ≥80 | 4.3 | 3.1 | 2.2 | 5.1 | 4.6 | 4.1 | 5.7 | 84.7% | 0.047 |
| Hospital volume | |||||||||
| <5 | 34.6 | 37.2 | 29.0 | 35.7 | 44.5 | 39.2 | 29.4 | −21.0% | 0.006 |
| 5–9 | 23.9 | 17.7 | 21.3 | 19.7 | 32.4 | 28.6 | 24.8 | 40.0% | 0.006 |
| 10–14 | 10.7 | 9.0 | 4.0 | 12.4 | 0 | 10.2 | 19.3 | 115.3% | <0.0001 |
| 15–24 | 14.0 | 13.8 | 17.3 | 20.0 | 15.3 | 8.0 | 13.0 | −5.9% | 0.69 |
| ≥25 | 16.4 | 22.3 | 28.4 | 12.2 | 7.8 | 13.9 | 13.5 | −39.4% | <0.0001 |
| Underlying diagnosis | |||||||||
| Osteoarthritis | 61.9 | 56.7 | 56.5 | 60.3 | 72.8 | 67.8 | 60.7 | 7.0% | 0.18 |
| Rheumatoid arthritis | 6.7 | 10.8 | 8.8 | 7.6 | 3.8 | 5.8 | 4.9 | −54.9% | 0.0001 |
| Fracture | 0.1 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0% | - |
| Avascular necrosis | 0.7 | 0.5 | 0.9 | 1.1 | 0.3 | 0.7 | 0.5 | −7.8% | - |
| Traumatic arthropathy | 18.3 | 21.0 | 24.2 | 17.1 | 11.8 | 11.9 | 20.5 | −2.2% | 0.83 |
| Other | 12.3 | 11.0 | 9.0 | 13.7 | 11.3 | 13.7 | 13.5 | 22.5% | 0.22 |
| Deyo-Charlson score | |||||||||
| 0 | 71.3 | 73.6 | 73.2 | 75.2 | 73.4 | 66.9 | 68.4 | −7.1% | 0.06 |
| 1 | 23.6 | 24.1 | 24.9 | 21.2 | 21.7 | 23.6 | 24.8 | 2.7% | 0.82 |
| ≥2 | 5.1 | 2.3 | 1.8 | 3.6 | 4.9 | 9.5 | 6.9 | 197.4% | 0.001 |
-, small numbers did not allow for a comparison
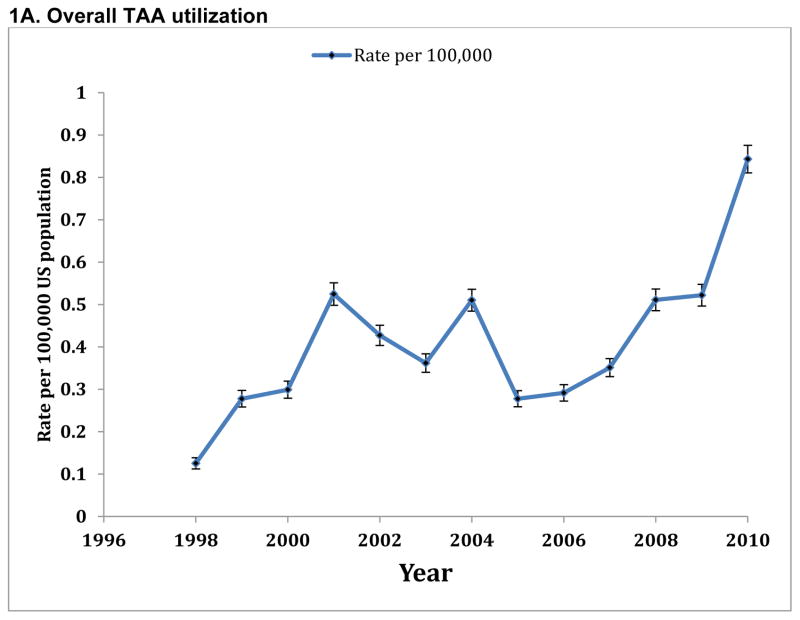
Time trends in utilization rates
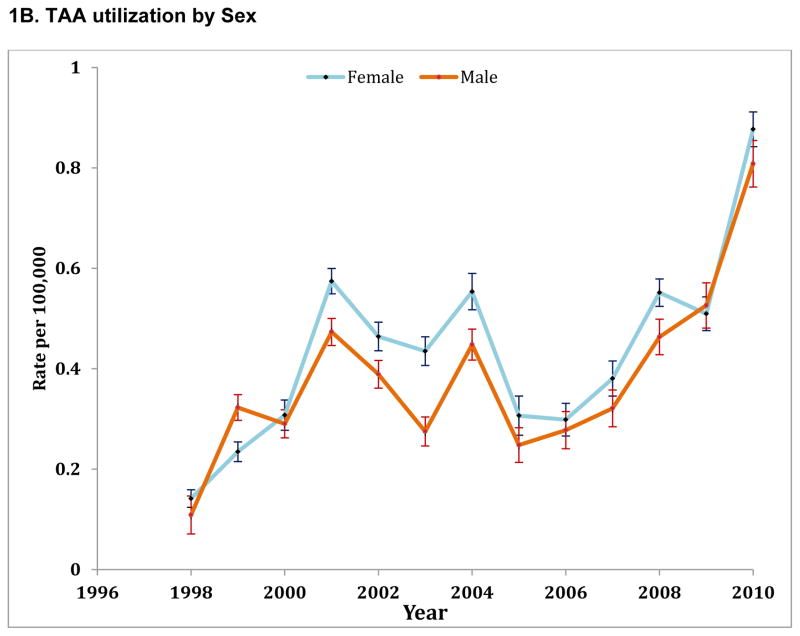
346 patients underwent TAA in 1998 in the U.S. and 2,608 in 2010 (Table 2). The overall TAA utilization rate increased 7-fold from 0.12 per 100,000 in 1998 to 0.84 per 100,000 in 2010 (Table 2 and Figure 1A). In females, the TAA utilization rate increased 7.1 times from 0.14 per 100,000 in 1998 to 0.88 per 100,000 in 2010 (Figure 1B and Appendix 1). In males, TAA utilization rate increased 7.4 times from 0.11 per 100,000 in 1998 to 0.81 per 100,000 in 2010 (Figure 1B and Appendix 1).
Table 2.
Utilization rates for TAA per 100,000 US populations based on NIS estimates
| Year | Number of patients who underwent TAA | Rate per 100,000 US population |
|---|---|---|
| 1998 | 346 | 0.13 |
| 1999 | 775 | 0.28 |
| 2000 | 844 | 0.30 |
| 2001 | 1,495 | 0.52 |
| 2002 | 1,229 | 0.43 |
| 2003 | 1,050 | 0.36 |
| 2004 | 1,494 | 0.51 |
| 2005 | 821 | 0.28 |
| 2006 | 870 | 0.29 |
| 2007 | 1,058 | 0.35 |
| 2008 | 1,554 | 0.51 |
| 2009 | 1,601 | 0.52 |
| 2010 | 2,608 | 0.84 |
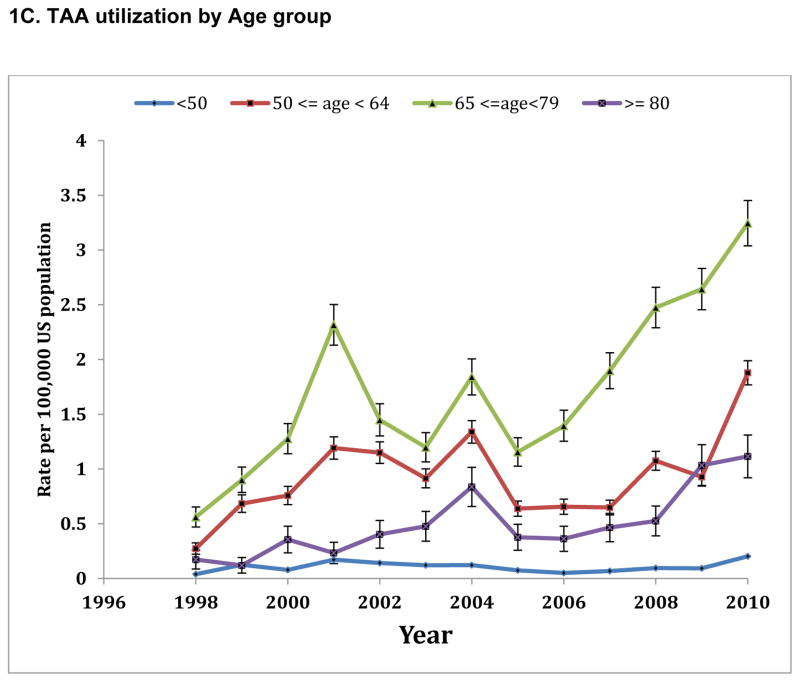
Figure 1.
Time trends in Utilization rates of Total Ankle Arthroplasty (TAA) per 100,000 population (weighted), overall (1A), by sex (1B) and age group (1C)
Whiskers represent 95% error bars
We also analyzed age-specific TAA utilization rates. TAA utilization rates increased in three higher age categories over time, with relatively lesser increase for those <50 years over the study period (Figure 1C, Appendix 2).
Time trends in patient demographics and comorbidity
Over the 13-year period, the mean age of patients undergoing TAA increased by 1 year, from 61 years in 1998–00 to 62 years in 2009–10 (p<0.0001; Table 1). The proportion of female patients did not increase over the study period (p=0.49). Compared to the 1998–00, significantly fewer proportion of patients <50 years (41% fewer; p<0.0001) and more patients ≥80 years (85% higher; p=0.047) underwent TAA in 2009–10. RA was less frequently the underlying diagnosis in 2009–10 compared to the earlier periods (55% reduction compared to 1998–00; p=0.0001).
Over the study period, comorbidity increased. In particular, the proportion of patients with Deyo-Charlson index of two or more increased by 197% from 2.3% to 6.9% (p=0.001; Table 1). We noted a significant increase in the proportion of patients with certain Deyo-Charlson comorbidities including diabetes (5.9% to 11.4%; p=0.0024) and moderate or severe renal disease (0.3% to 2.4%; p=0.0073).
Time trends in TAA outcomes
The length of index hospital stay decreased significantly over the study period from 3 to 2.5 days (17% reduction; p<0.0001, Table 3). The proportion of patients being discharged to an inpatient facility increased non-significantly by 12% over the study period from 12.6% in 1998–00 to 14.1% in 2009–10 (p=0.47, Table 3). Mortality was rare after TAA (range, 0–0.6%) and the numbers were too small to perform time-trends comparison.
Table 3.
Temporal trends in length of stay, discharge to home and mortality after primary total ankle arthroplasty (TAA)
| All patients | Study Time-periods | Comparison of 2009–10 to 1998–00 | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| 1998–2010 | 1998–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 | 2009–2010 | Last - first period (% Difference) | p-value | |
|
|
|||||||||
| Length of stay mean (SD), days | 2.7 (2.1) | 3 (1.8) | 2.7 (2) | 2.9 (2.7) | 2.7 (3.0) | 2.4 (1.3) | 2.5 (1.8) | −16.7% | <0.0001 |
| Discharge, n (%)a | 0.47 | ||||||||
| Home | 2,767 (87.0) | 340 (87.2) | 490 (89.9) | 463 (88.4) | 300 (86.7) | 450 (83.6) | 724 (85.8) | −1.6% | |
| Inpatient facility | 412 (12.9) | 49 (12.6) | 55 (10.1) | 59 (11.3) | 44 (12.7) | 86 (16.0) | 119 (14.1) | 12.3% | |
| Mortality, n (%) | 4 (0.1) | 0 | 0 | 1 (0.2) | 2 (0.6) | 0 | 1 (0.1) | n/a | n/a |
Information missing for 8 patients
n/a, not applicable, since the event rate was zero in the first and low in the last time-period
Discussion
To our knowledge, this is the first detailed study to assess time-trends in TAA utilization rates, patient characteristics and outcomes, in the U.S. population. A previous study of 10-years of NIS data found findings similar to our study with an increasing volume of TAA from 2000–10 and increasing patient age (14). Our study has several important observations that merit further discussion. A key observation in this study is the impressive 670% (or 6.7 times) increase in TAA utilization rate over a 13-year period, especially the increase since 2007. This may be related to better implants and surgical techniques, although the availability of more surgeons with training to perform TAA might also contribute. The previous study reporting a 39% decrease in the rate of ankle surgery (arthrodesis or TAA) from 1993–1997 to 2003–2007 combined the two surgeries and analyzed data up to 2007 only (10). Therefore, our results focused only on TAA using contemporary data are more likely valid for patients undergoing TAA.
Thus, the increase in TAA utilization rate in the 13-year period far exceeded that noted for knee (3-times) and hip arthroplasty (50%) previously in a similar period (21). This is likely due to the recent evolution of this procedure compared to THA and TKA, surgeries that are well established. This recently rapidly increasing TAA rate also implies that studies are needed for future projections of TAA to assess its future burden and to see if the projected increase is similar to or greater than that projected for primary THA and TKA (174% and 673% respectively, from 2005 and 2030) (12). The increase in utilization rate was similar for females and males.
We also noted a significantly lower proportion of TAA recipients were younger than 50 years in recent years and the mean age of patients undergoing TAA increased by one year over the 13-year study period. Specifically, TAA utilization rates in age groups 50–64, 65–80 and 80 or more increased by 7–10 fold over the study period. This indicates that the increase in TAA utilization is largely attributable to a higher number of older patients receiving this procedure in the recent years.
Increasing comorbidity and increasing age of patients undergoing TAA over time is an important observation. This indicates an increasing complexity of patients, which might lead to worse outcomes over time. This needs to be factored in the interpretation of studies that examine TAA outcomes over time or compare study results to more historical older cohorts. Our finding of increasing age of patients undergoing TAA in the U.S. confirms a similar finding from a recently published study that used NIS data from 2000–10 (14).
There was a 55% reduction in the proportion of patients with RA as the underlying diagnosis for TAA from 1998 to 2010, an impressive decline over a short time-period. This may also be responsible for fewer patients younger then 50 years in the more recent years compared to previously (50% reduction), since RA is a more common reason for TAA in younger patients, as opposed to OA in older patients. For example, in our study 12% of patients under age 50 vs. 5.6% over age 50 had RA as the underlying diagnosis.
Mortality was rare after TAA, ranging 0–0.6%. The length of hospital stay decreased by 17% from 1998–00 to 2009–10. It is reassuring that discharge to inpatient facility was still <15% in recent years, implying that most patients are still being discharged to home. This is an important and impressive finding, given the increase in patient age and comorbidity over the same time. Shorter hospital stays and more discharges to non-home care setting over time have been noted in studies of knee/hip arthroplasty (13, 22).
Our study extends these findings to TAA cohorts. Our study has several limitations. NIS does not include federal facilities, which may miss a small number of patients receiving TAA at these health care facilities. Another limitation is that NIS treats each hospital admission as an event; we would theoretically miss if a patient underwent simultaneous bilateral TAA. This selection bias is likely small, given that bilateral TAA is rare. We used the entire US population and not the population at risk for the denominator for calculating the rates, but this method has been used in other studies from NIS (23, 24). Comorbidity and underlying diagnosis were captured using the ICD-9 codes in the NIS, and given the method of diagnosis ascertainment, it is liable to misdiagnosis and underreporting.
This study has several strengths as well. The NIS is a nationally representative dataset and studies using NIS data for knee, shoulder and hip arthroplasty have been published (11, 12, 21, 25). We used ICD-9-CM codes for identifying TAA, similar to codes used in other arthroplasty studies, which were reasonably accurate (26). Confirmation of increasing age and increasing annual volume of TAA with time (27) in our study supports the robustness of this finding, now that two independent groups have reported the same finding with slight differences in methods and time-period.
In summary, in this first detailed study of time-trends in patient characteristics and outcomes of TAA in the U.S., a rapidly increasing TAA utilization rate over a 13-year period was noted. The increase in annual TAA volume was seen in both females and males. Patients with age 50 or older were the fastest growing age group for TAA. In the more recent years, more patients with higher comorbidity and older age received TAA than previously. This is an important observation, since increasing patient complexity over time can impact outcomes. More research is needed to understand the impact of increasing comorbidity and age over time on complications following TAA.
Supplementary Material
Acknowledgments
Grant Support: JAS is supported by grants from the Agency for Health Quality and Research Center for Education and Research on Therapeutics (AHRQ CERTs) U19 HS021110, National Institute of Arthritis, Musculoskeletal and Skin Diseases (NIAMS) P50 AR060772 and U34 AR062891, National Institute of Aging (NIA) U01 AG018947, and National Cancer Institute (NCI) U10 CA149950, and research contract CE-1304-6631 from Patient Centered Outcomes Research Institute (PCORI). JAS is also supported by the resources and the use of facilities at the VA Medical Center at Birmingham, Alabama, USA.
Footnotes
Financial Conflict: There are no financial conflicts related directly to this study. JAS has received research and travel grants from Takeda and Savient; and consultant fees from Savient, Takeda, Ardea and Regeneron. RR has no conflicts.
IRB approval: the Institutional Review Board (IRB) at the University of Alabama at Birmingham approved the study.
References
- 1.Maffulli N. Recent advances in foot and ankle surgery: editorial comment. Clin Orthop Relat Res. 2010;468(4):921. doi: 10.1007/s11999-009-1044-y. Epub 2009/08/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Park JS, Mroczek KJ. Total ankle arthroplasty. Bull NYU Hosp Jt Dis. 2011;69(1):27–35. Epub 2011/02/22. [PubMed] [Google Scholar]
- 3.Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am. 2001;83-A(2):219–28. doi: 10.2106/00004623-200102000-00009. Epub 2001/02/24. [DOI] [PubMed] [Google Scholar]
- 4.Anderson T, Montgomery F, Carlsson A. Uncemented STAR total ankle prostheses. Three to eight-year follow-up of fifty-one consecutive ankles. J Bone Joint Surg Am. 2003;85-A(7):1321–9. Epub 2003/07/10. [PubMed] [Google Scholar]
- 5.Knecht SI, Estin M, Callaghan JJ, Zimmerman MB, Alliman KJ, Alvine FG, et al. The Agility total ankle arthroplasty. Seven to sixteen-year follow-up. J Bone Joint Surg Am. 2004;86-A(6):1161–71. Epub 2004/06/03. [PubMed] [Google Scholar]
- 6.Bai LB, Lee KB, Song EK, Yoon TR, Seon JK. Total ankle arthroplasty outcome comparison for post-traumatic and primary osteoarthritis. Foot Ankle Int. 2010;31(12):1048–56. doi: 10.3113/FAI.2010.1048. Epub 2010/12/30. [DOI] [PubMed] [Google Scholar]
- 7.Conti SF, Wong YS. Complications of total ankle replacement. Clin Orthop Relat Res. 2001;(391):105–14. doi: 10.1097/00003086-200110000-00011. Epub 2001/10/18. [DOI] [PubMed] [Google Scholar]
- 8.Skytta ET, Koivu H, Eskelinen A, Ikavalko M, Paavolainen P, Remes V. Total ankle replacement: a population-based study of 515 cases from the Finnish Arthroplasty Register. Acta Orthop. 2010;81(1):114–8. doi: 10.3109/17453671003685459. Epub 2010/02/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hosman AH, Mason RB, Hobbs T, Rothwell AG. A New Zealand national joint registry review of 202 total ankle replacements followed for up to 6 years. Acta Orthop. 2007;78(5):584–91. doi: 10.1080/17453670710014266. Epub 2007/10/30. [DOI] [PubMed] [Google Scholar]
- 10.Louie GH, Ward MM. Changes in the rates of joint surgery among patients with rheumatoid arthritis in California, 1983–2007. Ann Rheum Dis. 2010;69(5):868–71. doi: 10.1136/ard.2009.112474. Epub 2009/07/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am. 2011;93(24):2249–54. doi: 10.2106/JBJS.J.01994. Epub 2012/01/20. [DOI] [PubMed] [Google Scholar]
- 12.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–5. doi: 10.2106/JBJS.F.00222. Epub 2007/04/04. [DOI] [PubMed] [Google Scholar]
- 13.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012;308(12):1227–36. doi: 10.1001/2012.jama.11153. Epub 2012/09/27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raikin SM, Rasouli MR, Espandar R, Maltenfort MG. Trends in treatment of advanced ankle arthropathy by total ankle replacement or ankle fusion. Foot Ankle Int. 2014;35(3):216–24. doi: 10.1177/1071100713517101. Epub 2013/12/21. [DOI] [PubMed] [Google Scholar]
- 15.Healthcare Cost and Utilization Project. Overview of the Nationwide Inpatient Sample (NIS) Rockville, MD: AHRQ; 2012. http://www.hcup-us.ahrq.gov/nisoverview.jsp Last updated 2/19/13. [6/14/13] [Google Scholar]
- 16.Masoomi H, Mills S, Dolich MO, Ketana N, Carmichael JC, Nguyen NT, et al. Comparison of outcomes of laparoscopic versus open appendectomy in children: data from the Nationwide Inpatient Sample (NIS), 2006–2008. World J Surg. 2012;36(3):573–8. doi: 10.1007/s00268-011-1417-8. Epub 2012/01/25. [DOI] [PubMed] [Google Scholar]
- 17.Shivaraju A, Patel V, Fonarow GC, Xie H, Shroff AR, Vidovich MI. Temporal trends in gastrointestinal bleeding associated with percutaneous coronary intervention: analysis of the 1998–2006 Nationwide Inpatient Sample (NIS) database. Am Heart J. 2011;162(6):1062–8. e5. doi: 10.1016/j.ahj.2011.09.009. Epub 2011/12/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vassileva CM, Shabosky J, Boley T, Markwell S, Hazelrigg S. Tricuspid valve surgery: the past 10 years from the Nationwide Inpatient Sample (NIS) database. J Thorac Cardiovasc Surg. 2012;143(5):1043–9. doi: 10.1016/j.jtcvs.2011.07.004. Epub 2011/08/30. [DOI] [PubMed] [Google Scholar]
- 19.Masoomi H, Mills S, Dolich MO, Ketana N, Carmichael JC, Nguyen NT, et al. Comparison of outcomes of laparoscopic versus open appendectomy in adults: data from the Nationwide Inpatient Sample (NIS), 2006–2008. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2011;15(12):2226–31. doi: 10.1007/s11605-011-1613-8. Epub 2011/07/05. [DOI] [PubMed] [Google Scholar]
- 20.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9. doi: 10.1016/0895-4356(92)90133-8. Epub 1992/06/01. [DOI] [PubMed] [Google Scholar]
- 21.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87(7):1487–97. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 22.Cram P, Lu X, Kaboli PJ, Vaughan-Sarrazin MS, Cai X, Wolf BR, et al. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991–2008. JAMA. 2011;305(15):1560–7. doi: 10.1001/jama.2011.478. Epub 2011/04/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jain NB, Higgins LD, Guller U, Pietrobon R, Katz JN. Trends in the epidemiology of total shoulder arthroplasty in the United States from 1990–2000. Arthritis Rheum. 2006;55(4):591–7. doi: 10.1002/art.22102. Epub 2006/07/29. [DOI] [PubMed] [Google Scholar]
- 24.Jain NB, Higgins LD, Ozumba D, Guller U, Cronin M, Pietrobon R, et al. Trends in epidemiology of knee arthroplasty in the United States, 1990–2000. Arthritis Rheum. 2005;52(12):3928–33. doi: 10.1002/art.21420. Epub 2005/12/02. [DOI] [PubMed] [Google Scholar]
- 25.Jain N, Pietrobon R, Hocker S, Guller U, Shankar A, Higgins LD. The relationship between surgeon and hospital volume and outcomes for shoulder arthroplasty. J Bone Joint Surg Am. 2004;86-A(3):496–505. doi: 10.2106/00004623-200403000-00006. Epub 2004/03/05. [DOI] [PubMed] [Google Scholar]
- 26.Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, et al. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2001;83-A(11):1622–9. doi: 10.2106/00004623-200111000-00002. Epub 2001/11/10. [DOI] [PubMed] [Google Scholar]
- 27.Singh JA, Wells GA, Christensen R, Tanjong Ghogomu E, Maxwell L, Macdonald JK, et al. Adverse effects of biologics: a network meta-analysis and Cochrane overview. Cochrane Database Syst Rev. 2011;2:CD008794. doi: 10.1002/14651858.CD008794.pub2. Epub 2011/02/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.