Abstract
Objective
1) To test the association among depression symptoms, distressed personality-type, and preoperative beta-blocker non-adherence. 2) To estimate the prevalence of untreated major depression in this population.
Design
Prospective Observational Study
Setting
A Veterans hospital
Patients
120 subjects on outpatient beta-blocker therapy presenting for surgery.
Interventions
The Patient Health Questionnaire (PHQ)-9, the D-Scale-14 (DS14), and Modified Morisky Scale (MMS) questionnaires.
Measurements and Main Results
Of 99 participants who presented for surgery, the incidence of preoperative non-adherence was 14.1% (95% CI 7–21%), consistent with prior research. Non-adherence was 9.5% among those with no depression, 27.8% among those with mild depression, and 28.6% among those with moderate to severe depression (Cochrane-Armitage test for trend p=0.03). Distressed personality-type was found in 35% of the cohort (95% CI 26–45%) and was not associated with beta-blocker non-adherence (Fisher’s exact p=0.24). Among participants with symptoms of Major Depressive Disorder (N=25, 25.3%), over half (N=14, 56%) had no indication of depression listed at their most recent primary care visit.
Conclusions
Patients with symptoms of depression on chronic beta-blocker therapy are prone to medication non-adherence on the day of surgery. The majority of surgical patients with symptoms of major depression lack a diagnosis of depression. Preoperative depression screening may thus 1) identify a population at increased risk of beta-blocker withdrawal and 2) identify patients who may benefit from anesthesiologist-initiated referral for this treatable condition.
Keywords: beta-Adrenergic Blockers, Depression, Preoperative Care, Medication Adherence, Preventive Medicine
INTRODUCTION
Preoperative beta-blocker non-adherence is a common and potentially modifiable behavior that may predispose patients to adverse perioperative cardiovascular events.1–10 Preoperative beta-blocker withdrawal has previously been shown to occur in 9–31% of surgical patients prescribed chronic outpatient beta-blockers.11 Discontinuous use of perioperative beta-blockade has been associated with increased perioperative mortality.10 It is therefore important to understand patient characteristics that may increase the likelihood of medication non-adherence, particularly in those patients who present for surgery from home and who therefore may not benefit from in-hospital electronic decision-support initiatives.
In the non-surgical outpatient population, depression is one patient factor that has previously been identified to increase risk for medication non-adherence to cardio-protective medications.12–15 Within the surgical context, depression has been linked to delirium and post-operative cognitive dysfunction,16,17 but its potential association with preoperative medication non-adherence has remained unexplored. Similarly, the distressed personality-type known as “Type D personality” – a well-validated personality-type characterized by negative affectivity and social inhibition18 - has been associated with poor medication adherence and unhealthy lifestyle choices outside of the perioperative milieu among patients with ischemic heart disease. Again, however, the association of Type-D personality and medication non-adherence has not been examined in perioperative patients.19–21 The connections among emotional distress, social inhibition, depression, and cardiovascular health continue to be intensively studied in the cardiology literature,22–28 and such literature may carry particular relevance within the perioperative period – a timeframe that is frequently experienced as highly stressful for patients and their families and that is known to be associated with acute increases in the incidence of major adverse cardiac events.
If depressive symptoms or the distressed personality-type are shown to be associated with increased rates of preoperative beta-blocker non-adherence, then screening for these conditions would assume added importance within the preoperative testing environment. Moreover, if significant numbers of patients with previously undetected depression symptoms or emotional distress could be identified during preoperative evaluations, then the preadmission testing clinic could present a valuable opportunity for care coordination between perioperative physicians and primary care doctors for longitudinal treatment of depression - a disease that is common, treatable, and associated with significant morbidity. Similar anesthesiologist-initiated care coordination efforts have been encouraged to promote smoking cessation29–31 and to improve treatment of hypertension32,33 among surgical patients. Each of these care coordination initiatives that target long-term improvement in health outcomes among surgical patients may provide a further justification for the anesthesiologist’s central role in the relatively nascent concept of the Perioperative Surgical Home.33–36
Accordingly, the purpose of this prospective, observational study was 1) To test the association of preoperative depression symptom severity and Type-D personality, with day-of-surgery beta-blocker non-adherence in patients on chronic beta-blocker therapy, and 2) to measure the prevalence of untreated major depression symptoms among this population. Secondary aims were to test 1) the association between depression symptom severity and self-reported knowledge and motivation about beta-blocker usage, and 2) the association between perioperative beta-blocker non-adherence and day of surgery vital signs.
METHODS
This study was approved by the appropriate Institutional Review Boards of the study institutions. Patients with an active prescription for outpatient beta-blocker therapy who presented to the preadmission testing clinic at a tertiary care VA medical center between May 2011 and August 2012 were eligible for inclusion. Potential subjects proceeded through their standard preoperative testing visit. As part of each visit, patients received both verbal and written instructions to continue taking their beta-blocker medication as directed, up to and including the day of surgery (or the evening prior to surgery in the case of once-daily evening dosing). At the conclusion of their preadmission testing visit, eligible patients were approached about study participation.
After obtaining written informed consent, study participants were asked to complete a brief psychometric battery that included the Patient Health Questionnaire-9 (PHQ-9),37 a validated 9-item self-report scale that has been used as a brief instrument to assist primary care physicians in diagnosing, monitoring, and tracking the severity of depression symptoms. The PHQ-9 has been shown to have superior discriminative power versus other comparable instruments.38 It has been extensively validated in multiple populations against trained interviewers using the Diagnostic and Statistical Manual of Mental Disorders IV-Text Revision (DSM–IV-TR),39 with a cutoff score of 10 or higher demonstrating both a sensitivity and specificity of 88% for Major Depressive Disorder (MDD).37 Patients were also asked to complete the D Scale-14 (DS-14),18 a validated 14-item self-report scale used to assess for the presence of Type-D personality, a distressed personality-type characterized by negative affectivity and social inhibition, and that has been associated with poor cardiovascular outcomes independent from depression.40–49 Patients were also asked to complete the Modified Morisky Scale (MMS),50 an expanded 6-question version of the Morisky Medication Adherence scale,51 a self-report instrument designed to measure medication adherence.. The MMS questionnaire contains 6 yes/no items, 3 addressing knowledge about a medication and 3 addressing motivation for taking a medication. Each set of 3 items is scored separately, with scores of 0–1 indicating low knowledge/motivation and scores of 2–3 indicating high knowledge/motivation, respectively.
On the day of surgery, participants were asked if they took their most recent beta-blocker dose, and their blood pressure and heart rate were recorded by their treating clinician. Additional perioperative blood pressures and heart rates, comorbidities, and the presence or absence of a prior diagnosis of depression were recorded based on manual chart reviews conducted by the study investigators. Blood pressure and heart rate measurements were obtained for the following four time points: 1) from the most recent primary care visit, 2) upon arrival to the hospital prior to entering the preoperative holding area, 3) on entrance to the operating room, and 4) maximal blood pressures and heart rates in the operating room. Preoperative blood pressures were measured by a non-invasive automated oscillometric blood pressure cuff. Intraoperative blood pressure measurements were done at the discretion of the anesthesia provider. Maximal intraoperative values were determined by review of the manually recorded intraoperative anesthesia records. Participants were coded as having depression if a provider had listed depression in the past medical history or problem list, or if the participant was prescribed an antidepressant medication in the absence of an indication for such medication other than depression.
The primary aims were to test the association of PHQ-9-assessed depression symptom severity and Type-D personality with preoperative beta-blocker non-adherence and to measure the prevalence of untreated major depression symptoms among this population. Secondary aims were to test 1) the association between depression symptom severity and self-reported knowledge and motivation about beta-blocker usage, and 2) the association between perioperative beta-blocker non-adherence and day of surgery vital signs.
Statistics
Following the Veterans Affairs/Department of Defense (VA/DoD) clinical practice guidelines for interpreting the PHQ-9 questionnaire,52 PHQ-9 scores are typically classified into a 4-level ordinal variable of depression symptom severity as follows: Scores of 0–9 are classified as “no depression or remission,” scores of 10–14 are classified as “mild depression symptoms,” scores of 15–19 are classified as “moderate depression symptoms,” and scores of 20–27 are classified as “severe depression symptoms”52 Due to a paucity of scores above 20, we chose to combine moderate and severe depressive symptoms into a single category. Type-D or distressed personality-type was determined as present or absent based on DS-14 scores as previously described,18 with scores for both negative affectivity and social inhibition greater than 9 required for the finding of the presence of Type-D personality. Preoperative beta-blocker adherence was determined as yes or no based on participant self-report on the day of surgery regarding the most recently scheduled dose. The Cochrane-Armitage test for trend was used to measure the possible association between the ordinal PHQ-9 depression severity variable and likelihood of beta-blocker non-adherence. The Fisher’s Exact Test was used to test the association between beta-blocker non-adherence and Type-D personality.
Descriptive statistics are reported as N (percent) or mean (SD). Hypothesis tests for significant associations or differences among groups are based on the Cochrane-Armitage test for trend, Fisher’s Exact Test, or the Mann-Whitney U Test as indicated. All p-values are reported for two-tailed tests with p<0.05 considered the threshold of statistical significance without correction for multiple comparisons.
RESULTS
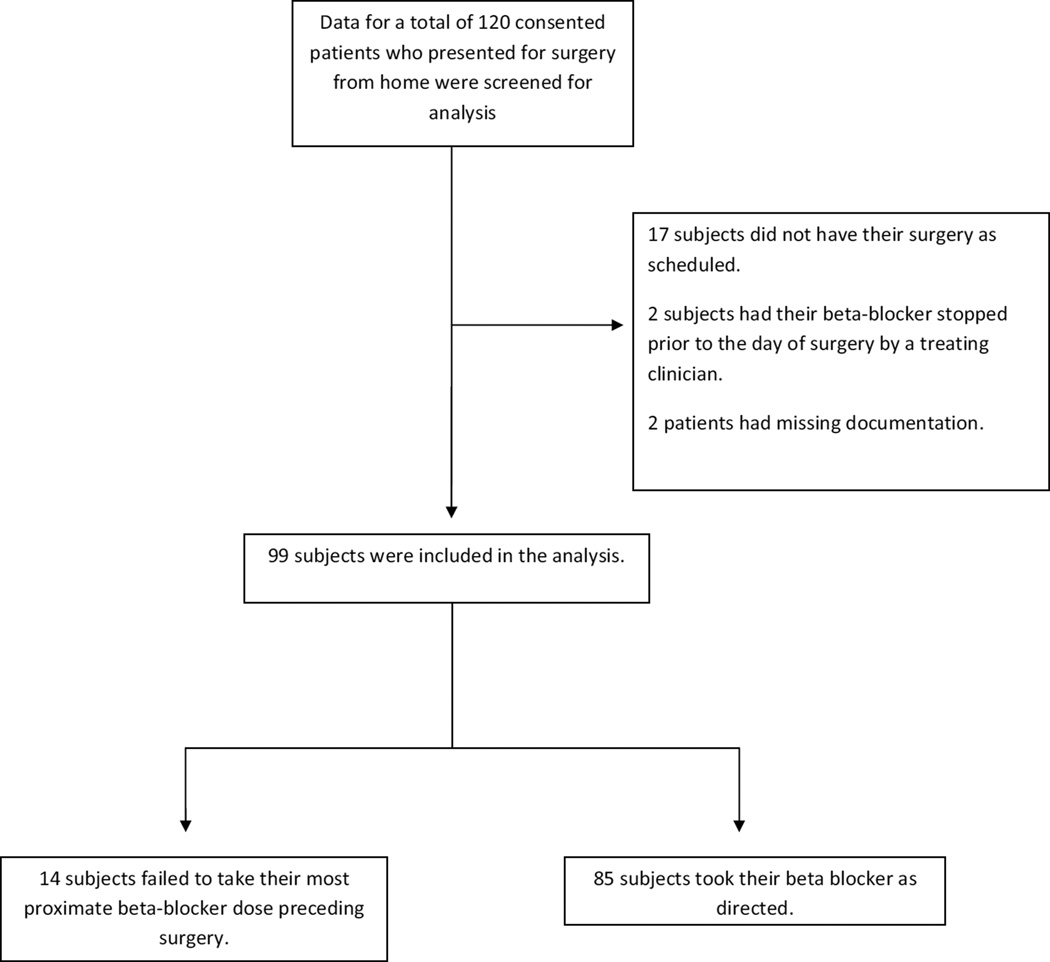
Of 120 patients consented into the study, day of surgery data were available for 99. Of the 21 excluded participants, 17 did not have surgery as scheduled, 2 had their beta-blocker stopped by a treating clinician prior to the day of surgery, and 2 had missing data (see Consort Diagram, Figure 1).
Figure 1.
Flow diagram of patient screening and analysis.
The mean age of the sample was 69.3 (±10.5) years and ranged from 33 years to 89 years, 96 (97.0%) were male, and 15 (15.1%) were scheduled for cardiac or vascular surgery (Table 1). The most commonly prescribed beta-blocker types were metoprolol (N=59, 59.6%), followed by atenolol (N=29, 29.3%), with the remaining participants prescribed either carvedilol (N=6, 6.1%) or propranolol (N=5, 5.1%). Table 1 provides a descriptive summary of the study cohort stratified by beta-blocker adherence. Adherent and non-adherent participants demonstrated similar demographic and comorbid characteristics across all baseline variables with the exception that significantly more in the non-adherent group carried the diagnosis of coronary artery disease (85.7% vs. 52.9%, p = 0.04).
Table 1.
Descriptive Characteristics of Cohort
| Variable | Full Cohort | Adherent | Non- Adherent |
|
|---|---|---|---|---|
| (N=99) | (N=85) | (N=14) | ||
| Mean(SD) or N(%) |
Mean(SD) or N(%) |
Mean(SD) or N(%) |
||
| Age | 69.3 (10.5) | 68.8 (10.5) | 72.0 (10.1) | |
| Male Gender | 96 (97.0%) | 82 (96.5%) | 14 (100%) | |
| Type of Beta Blocker | ||||
| Atenolol | 29 (29.3%) | 24 (28.2%) | 5 (35.7%) | |
| Metoprolol | 59 (59.6%) | 52 (61.2%) | 7 (50.0%) | |
| Other | 11 (11.1%) | 9 (10.6%) | 2 (14.3%) | |
| Cardiac or Vascular Surgery | 15 (15.1%) | 11 (12.9%) | 4 (28.6%) | |
| Comorbidities | ||||
| Hypertension | 89 (89.9%) | 77 (90.6%) | 12 (85.7%) | |
| Congestive Heart Failure | 10 (10.1%) | 8 (9.4%) | 2 (14.3%) | |
| Coronary Artery Disease | 57 (57.6%) | 45 (52.9%) | 12 (85.7%) | |
| Chronic Renal Insufficiency | 4 (4.0%) | 4 (4.7%) | 0 (0%) | |
| Diabetes | 45 (45.5%) | 38 (44.7%) | 7 (50.0%) | |
| Psychiatric Diagnoses | ||||
| Depression | 25 (25.3%) | 21 (24.7%) | 4 (28.6%) | |
| Anxiety | 12 (12.1%) | 10 (11.8%) | 2 (14.3%) | |
| Post Traumatic Stress Disorder | 12 (12.1%) | 10 (11.8%) | 2 (14.3%) | |
| Psychosis | 3 (3.0%) | 3 (3.5%) | 0 (0%) |
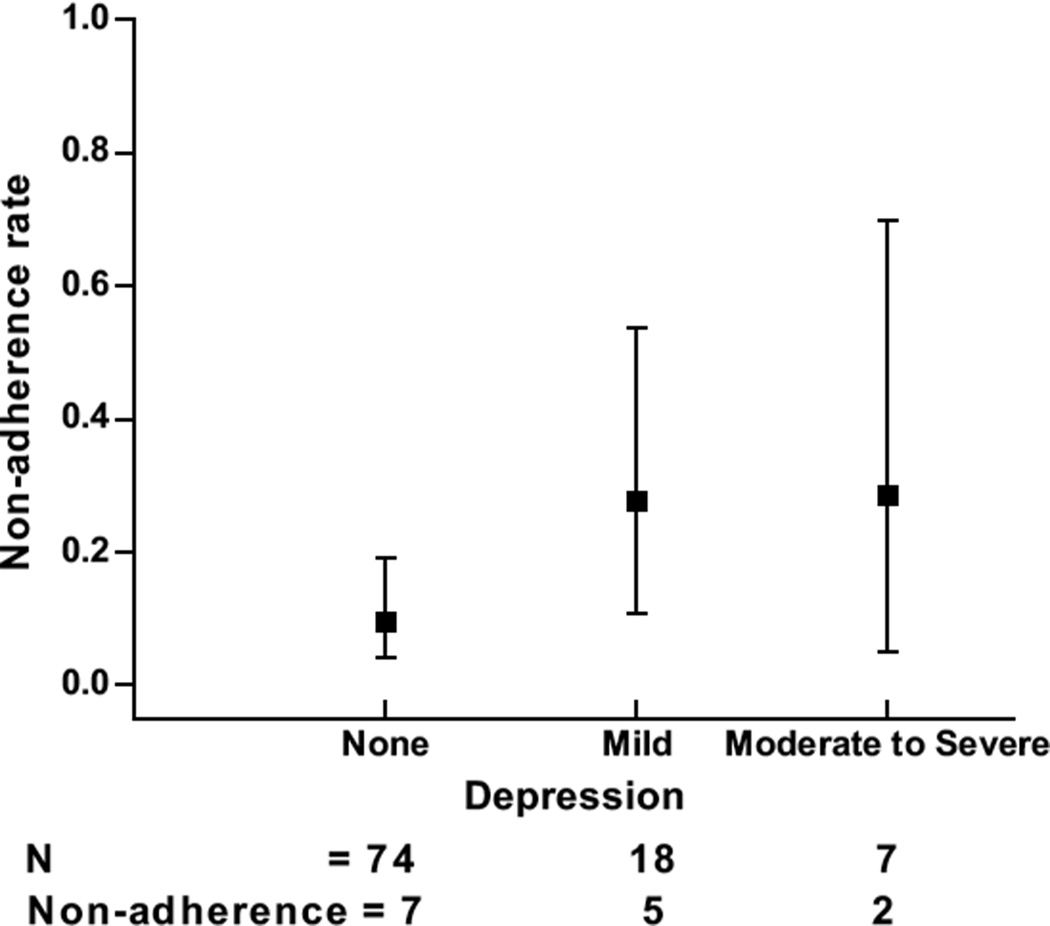
Based on PHQ-9 scores, 74 (74.7%) participants scored as “no depression or remission” versus 25 (25.3%) with scores of 10 or higher, indicating depression symptom severity in the MDD range. When stratified in accordance with VA/DoD depression severity categories, 18 (18.2%) endorsed “mild depression” and 7 (7.1%) endorsed “moderate or severe depression.”
Primary outcomes analysis
The overall incidence of preoperative beta-blocker non-adherence in the study population was 14.1% (95% CI 7–21%), which is consistent with prior research.11 The incidence of beta-blocker non-adherence was 9.5% (95% CI 4.2–19.1%) among participants with no depression/remission, increasing to 27.8% (95% CI 10.7–53.6%) among participants with mild depression symptoms, and 28.6% (95% CI 5.1–69.7%) among participants with moderate/severe depression symptoms. The trend increase of non-adherence with increasing depression symptom severity demonstrated statistical significance (the Cochrane-Armitage test for trend p=0.03, see Figure 2). The statistical significance of this association persisted in alternative analyses when treating depression symptom severity either as a dichotomous variable or as a 4-level ordinal variable.
Figure 2.
The relationship between the rate of beta-blocker non-adherence and preoperative depression symptom severity. Error bars indicate 95% Confidence Intervals. P for trend = 0.03.
DS-14 scores demonstrated a prevalence of Type-D personality of 35% (95% CI 26–45%) which is consistent with other populations. Although a higher proportion of participants who were non-adherent to their beta-blocker therapy were positive for Type-D personality as compared to the adherent group (50% vs. 33%), the association did not reach statistical significance (Fisher’s exact test p=0.24).
Regarding the prevalence of undiagnosed major depression, of the 25 participants who scored positive for symptoms consistent with Major Depressive Disorder, the majority (n=14; 56%) had no indication of depression listed at their most recent primary care visit.
Secondary Outcomes
Modified Morisky Scale: Of the overall sample, 22 (22.2%) reported low motivation to take their beta-blockers, while 98 (99.0%) reported a high degree of knowledge about their beta-blockers. There was a significant, inverse correlation between depression symptom severity and motivation toward beta-blocker adherence. Specifically, 14.9% of participants with no depression/remission, 38.9% with symptoms of mild depression, and 57.1% with moderate to severe depression symptoms reported low motivation toward beta-blocker adherence (Cochrane-Armitage test for trend p=0.001).
Vital Signs
There was no significant association of self-reported beta-blocker adherence with either preoperative, initial operating room, or maximal intraoperative blood pressure or heart rate. This may have been due to the fact that hemodynamic management was left to the discretion of individual anesthesia providers who provided intravenous beta-blockade to greater than 90% of participants reporting beta blocker non-adherence. In a post hoc finding, when the most recent preoperative primary care heart rate was incorporated into the analysis (N=95), the difference between the most recent primary care visit heart rate and maximum operating room heart rate was higher for those reporting non-adherence than for those reporting adherence (+15.8 bpm in the non-adherent group vs. +2.5 bpm in the adherent group; p=0.01). See Table 2 for summary of vital signs data.
Table 2.
Vital Signs Data
| Vital Sign | Adherent Mean (SD) |
Non- Adherent Mean (SD) |
P for difference Mann Whitney U Test |
|---|---|---|---|
| PRIMARY CARE VITAL SIGNS | N=95 | N=95 | |
| Heart Rate | 73.4(15.1) | 67.1(13.3) | 0.14 |
| Systolic Blood Pressure | 128.1(16.7) | 128.9(24.3) | 0.83 |
| Diastolic Blood Pressure | 71.7(13.2) | 69.8(12.0) | 0.55 |
| INITIAL DAY OF SURGERY VITAL SIGNS | N=99 | N=99 | |
| Heart Rate | 69.4(12.4) | 68.3(13.9) | 0.56 |
| Systolic Blood Pressure | 132.8(27.2) | 129.1(23.5) | 0.61 |
| Diastolic Blood Pressure | 72.8(15.1) | 69.9(13.5) | 0.42 |
| FIRST VITAL SIGNS OR | N=99 | N=99 | |
| Heart Rate | 67.8(10.9) | 67.4(8.1) | 0.94 |
| Systolic Blood Pressure | 140.1(28.2) | 147.4(19.1) | 0.36 |
| Diastolic Blood Pressure | 79.0(16.8) | 75.3(12.4) | 0.34 |
| MAXIMAL VITAL SIGNS OR | N=99 | N=99 | |
| Heart Rate | 76.2(11.4) | 80.6(16.8) | 0.53 |
| Systolic Blood Pressure | 144.6(24.0) | 151.2(24.2) | 0.35 |
| Diastolic Blood Pressure | 78.5(13.3) | 75.1(15.2) | 0.44 |
| DIFFERENCE IN DIFFERENCE ANALYSIS | N=95 | N=95 | |
| Maximal OR-Primary Care Heart Rate | +2.5(14.7) | +15.8(17.4) | <0.01 |
DISCUSSION
We observed a clinically significant dose-response relationship between the severity of preoperative depression symptoms and the likelihood of preoperative beta-blocker non-adherence among surgical patients. There was no statistically significant association between the Type-D personality-type and beta-blocker adherence. Overall rates of preoperative beta-blocker non-adherence in the present study were consistent with prior research,11 demonstrating the reproducibility of estimates of the incidence of this phenomenon and supporting the notion that there is a need for more research focusing on medication non-adherence in the surgical context. In a post hoc analysis, among participants reporting beta-blocker non-adherence, the mean increase in maximal intraoperative heart rate was +15.8 beats per minute versus +2.5 beats per minute among adherent participants, suggesting the potential clinical significance of beta-blocker adherence among high-risk populations.2 Tight heart rate control among high risk patients may prevent major adverse cardiac events, and if clinicians wrongly assume that their patients are taking beta-blockers as directed, they may be less vigilant about the potential for rebound tachycardia associated with beta-blocker withdrawal.7,8 Moreover, the finding that almost 1 in 7 participants did not follow this single preoperative instruction suggests that further research regarding adherence to other preoperative instructions and the accompanying effects on perioperative safety and efficiency may be warranted.
Regarding the issue of screening for undiagnosed Major Depressive Disorder in the preoperative environment, we found that among participants who scored positive for symptoms consistent with Major Depressive Disorder (N=25, 25.3%), more than half (N=14, 56%) had no indication of a depression diagnosis listed at their most recent primary care visit. This finding may carry implications for the role of anesthesiologists as important members of the longitudinal healthcare team who can impact patient health beyond the immediate perioperative period. Echoing our prior findings of a significant incidence of undiagnosed hypertension among surgical patients,33 our present findings again suggest that the preoperative visit provides a unique opportunity for anesthesiologists to intervene in the longitudinal well-being of surgical patients by communicating important findings of possible undiagnosed chronic diseases back to primary care providers. It should be noted, however, that high PHQ-9 scores in the present study represented a cross-sectional measurement of depression symptom severity that did not conclusively indicate the presence of major depressive disorder. While the PHQ-9 is a well-validated metric that has good discriminative properties for the diagnosis of major depressive disorder, a high PHQ-9 score in itself is neither necessary nor sufficient to confer the diagnosis of major depressive disorder. Further studies are needed to measure the effects of anesthesiologist-initiated primary care referrals, but analogous care coordination interventions have been shown to improve chronic disease outcomes in several other healthcare contexts.30,53–60
Finally, we found a very high rate of knowledge about beta-blockers among our cohort in contrast to significant numbers of participants with low motivation for beta-blocker adherence, perhaps suggesting a fruitful direction for future interventions to increase pre-surgical beta-blocker adherence. Patients who present for surgery with significant depressive symptoms and lack of motivation may benefit from established and highly effective methods to improve motivation for following preoperative instructions, rather than efforts to simply make these instructions easier to understand. Similar suggestions have emerged from a recent qualitative study that looked at perspectives on non-adherence between heart failure patients and their treating physicians in which patients perceived themselves as “understanding what to do but needing help with how to carry out [instructions]” whereas doctors perceived patients as “not understanding… and therefore needing more repetition of knowledge-based instructions.”61 The present study offers some support to the generalizability of such findings to the preoperative physician-patient encounter.
Left open is the question of whether improving pre-operative beta-blocker adherence will improve patient outcomes. Our secondary analyses did not convincingly demonstrate that self-reported non-adherence had a clinically meaningful effect on vital signs. Although the maximal operating room heart rate was only marginally higher than a recent primary care measurement among adherent participants, it was substantially higher for non-adherent participants. In a recent study of a large cohort of United States Veterans, London, et al. noted an approximate doubling of mortality risk among Veterans who were withdrawing from beta blockers during the perioperative period.62 The extent to which beta-blocker withdrawal may be associated with potentially harmful increases in intraoperative heart rates is a controversy that the present study was not designed to answer. Interestingly, there was no association found between beta-blocker adherence and any of the other vital signs measurements that were examined (Table 2). It should be emphasized however, that day of surgery hemodynamic management was left to the discretion of individual providers, and our vital signs comparisons may have been confounded by our post hoc observation that 93% of participants who reported non-adherence in the present study received intravenous beta-blockade from their anesthesia provider at some point during the day of surgery. Perhaps then, the most generalizable finding from the present data is that patients presenting for surgery are often depressed and untreated for it. Regardless of whether a patient is taking a beta-blocker, referral for untreated depression symptoms is likely to be a low-risk intervention with potentially important rewards in the lives of surgical patients.
The present study has several limitations that deserve highlighting. Most obviously, the modest sample size and 17.5% rate of drop out leave our observational findings prone to selection bias that may have distorted the results either toward or away from the association between depression symptom severity, Type-D personality, and beta-blocker non-adherence. In addition, the decision not to correct for multiple comparisons, while common in exploratory studies of this type, leaves our findings prone to inflated Type-1 error. The study results reported herein should therefore be viewed as suggestive findings within a limited cohort of surgical patients rather than definitively established and broadly generalizable conclusions. If our findings are confirmed, however, they may carry important implications for the preoperative care of surgical patients and for the role of anesthesiologists within the perioperative surgical home.
Also, our assessment of beta-blocker adherence was limited to the most proximate scheduled dose prior to surgery. It would have been useful to obtain a more longitudinal measure of beta-blocker non-adherence in these patients, as it is quite possible that many non-adherent subjects were regularly not taking their medications. For this group, day-of-surgery adherence would have represented acute initiation of beta blockade rather than acute withdrawal as we assumed. Moreover, an expanded analysis of reasons for non-adherence such as assessments of specific side-effects due to beta-blockade would offer more nuanced guidance for future interventions aimed at improving rates of perioperative beta-blocker adherence. In addition, it would be of interest in future studies to stratify subjects by severity of surgery and to attempt to determine whether some depressed feelings may have been due to the acute surgical condition in the absence of a longitudinal depressive syndrome.
A further limitation is that our study population included only United States military veterans who represent a unique and predominantly male population which may impact the generalizability of these results to surgical populations outside of the VA system.63 In addition to their male predominance, US Veterans also exhibit higher rates of post-traumatic stress disorder (PTSD), depression, and other mental health diagnoses as compared to the general US population. PTSD and depression may also interact to affect behavior among combat veterans in ways that are not frequently seen in non-Veterans. Despite this limitation, it bears pointing out that the VA population included approximately 8.6 million enrollees as of 2011,64 so that even in the extreme case that our findings were entirely limited in their relevance to the VA population, they would still be applicable to patients within the largest single healthcare system in the United States.
In conclusion, among surgical patients on chronic beta-blocker therapy presenting to a preadmission testing center, the severity of depression symptoms significantly correlated with the likelihood of pre-surgical beta-blocker non-adherence. Moreover, many patients who endorsed a level of depressive symptom severity consistent with Major Depressive Disorder lacked a diagnosis or treatment for depression from their primary care providers. Future research is needed to determine whether anesthesiologist-initiated depression screening and subsequent communication with primary care providers may confer health benefits to surgical patients both by means of improved perioperative cardiovascular protection and improved mental health treatment long after the surgical encounter has passed.
Acknowledgments
Financial Support: This research was funded in part by the following National Institutes of Health grants: T32 GM086287-01 (Niklason) from NIGMS and CTSA Grant UL1 RR024139 from NCRR and NCATS. This research was also supported in part by the Department of Veterans Affairs. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the National Institutes of Health, or the United States government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Robert B. Schonberger, Yale University School of Medicine, Department of Anesthesiology..
Jessica Feinleib, Yale University School of Medicine and VA Connecticut Healthcare System, Department of Anesthesiology..
Natalie Holt, Yale University School of Medicine and VA Connecticut Healthcare System, Department of Anesthesiology..
Feng Dai, Yale School of Public Health, Yale Center for Analytical Sciences..
Cynthia Brandt, Yale University School of Medicine and VA Connecticut Healthcare System, Departments of Anesthesiology and Emergency Medicine..
Matthew M. Burg, Yale University School of Medicine, VA Connecticut Healthcare System, and Columbia University College of Physicians and Surgeons; Department of Internal Medicine..
REFERENCES
- 1.Beattie WS, Wijeysundera DN, Karkouti K, McCluskey S, Tait G. Does tight heart rate control improve beta blocker efficacy? An updated analysis of the noncardiac surgical randomized trials. Anesthesia & Analgesia. 2008;106:1039–1048. doi: 10.1213/ane.0b013e318163f6a9. [DOI] [PubMed] [Google Scholar]
- 2.Feringa HH, Bax JJ, Boersma E, et al. High dose beta blockers and tight heart rate control reduce myocardial ischemia and troponin T release in vascular surgery patients. Circulation. 2006;114:I344–I349. doi: 10.1161/CIRCULATIONAHA.105.000463. [DOI] [PubMed] [Google Scholar]
- 3.Fleisher LA, Beckman JA, Brown KA, et al. 2009 ACCF/AHA focused update on perioperative beta blockade incorporated into the ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American college of cardiology foundation/American heart association task force on practice guidelines. Circulation. 2009;120:e169–e276. doi: 10.1161/CIRCULATIONAHA.109.192690. [DOI] [PubMed] [Google Scholar]
- 4.Hoeks SE, Scholte Op Reimer WJM, van Urk H, et al. Increase of 1 year mortality after perioperative beta blocker withdrawal in endovascular and vascular surgery patients. European Journal of Vascular & Endovascular Surgery. 2007;33:13–19. doi: 10.1016/j.ejvs.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 5.Lederballe Pedersen O, Mikkelsen E, Lanng Nielsen J, Christensen NJ. Abrupt withdrawal of beta blocking agents in patients with arterial hypertension. Effect on blood pressure, heart rate and plasma catecholamines and prolactin. European Journal of Clinical Pharmacology. 1979;15:215–217. doi: 10.1007/BF00563108. [DOI] [PubMed] [Google Scholar]
- 6.London MJ. Perioperative beta blockade, discontinuation, and complications: do you really know it when you see it? Anesthesiology. 2009;111:690–694. doi: 10.1097/ALN.0b013e3181b6a79f. [DOI] [PubMed] [Google Scholar]
- 7.Miller D. Letter: Non compliance and propranolol withdrawal. New England Journal of Medicine. 1975;293:830. doi: 10.1056/NEJM197510162931617. [DOI] [PubMed] [Google Scholar]
- 8.Miller RR, Olson HG, Amsterdam EA, Mason DT. Propranolol withdrawal rebound phenomenon. Exacerbation of coronary events after abrupt cessation of antianginal therapy. New England Journal of Medicine. 1975;293:416–418. doi: 10.1056/NEJM197508282930902. [DOI] [PubMed] [Google Scholar]
- 9.Shand DG. Editorial: Propranolol withdrawal. New England Journal of Medicine. 1975;293:449–450. doi: 10.1056/NEJM197508282930910. [DOI] [PubMed] [Google Scholar]
- 10.Wallace AW, Au S, Cason BA. Association of the Pattern of Use of Perioperative B Blockade and Postoperative Mortality. Anesthesiology. 2010;113:794–805. doi: 10.1097/ALN.0b013e3181f1c061. [DOI] [PubMed] [Google Scholar]
- 11.Schonberger RB, Feinleib J, Lukens CL, Turkoglu OD, Haspel K, Burg M. Beta blocker withdrawal among patients presenting for surgery from home. Journal of Cardiothoracic & Vascular Anesthesia. 2012 doi: 10.1053/j.jvca.2012.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Addolorato G, De Lorenzi G, Abenavoli L, Leggio L, Capristo E, Gasbarrini G. Psychological support counselling improves gluten free diet compliance in coeliac patients with affective disorders. Aliment Pharmacol Ther. 2004;20:777–782. doi: 10.1111/j.1365-2036.2004.02193.x. [DOI] [PubMed] [Google Scholar]
- 13.Herlitz J, Toth PP, Naesdal J. Low dose aspirin therapy for cardiovascular prevention: quantification and consequences of poor compliance or discontinuation. Am J Cardiovasc Drugs. 2010;10:125–141. doi: 10.2165/11318440-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 14.Louis ED, Huey ED, Gerbin M, Viner AS. Depressive traits in essential tremor: impact on disability, quality of life, and medication adherence. Eur J Neurol. 2012;19:1349–1354. doi: 10.1111/j.1468-1331.2012.03774.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mumby PB, Hurley C, Samsi M, Thilges S, Parthasarathy M, Stiff PJ. Predictors of non compliance in autologous hematopoietic SCT patients undergoing out patient transplants. Bone Marrow Transplant. 2012;47:556–561. doi: 10.1038/bmt.2011.129. [DOI] [PubMed] [Google Scholar]
- 16.Kadoi Y, Kawauchi C, Ide M, et al. Preoperative depression is a risk factor for postoperative short term and long term cognitive dysfunction in patients with diabetes mellitus. Journal of Anesthesia. 2011;25:10–17. doi: 10.1007/s00540-010-1072-5. [DOI] [PubMed] [Google Scholar]
- 17.Leung JM, Sands LP, Mullen EA, Wang Y, Vaurio L. Are preoperative depressive symptoms associated with postoperative delirium in geriatric surgical patients? J Gerontol A Biol Sci Med Sci. 2005;60:1563–1568. doi: 10.1093/gerona/60.12.1563. [DOI] [PubMed] [Google Scholar]
- 18.Denollet J. DS14: standard assessment of negative affectivity, social inhibition, and Type D personality. Psychosomatic Medicine. 2005;67:89–97. doi: 10.1097/01.psy.0000149256.81953.49. [DOI] [PubMed] [Google Scholar]
- 19.Molloy GJ, Randall G, Wikman A, Perkins Porras L, Messerli Burgy N, Steptoe A. Type D personality, self efficacy, and medication adherence following an acute coronary syndrome. Psychosomatic Medicine. 2012;74:100–106. doi: 10.1097/PSY.0b013e31823a5b2f. [DOI] [PubMed] [Google Scholar]
- 20.Svansdottir E, Denollet J, Thorsson B, et al. Association of type D personality with unhealthy lifestyle, and estimated risk of coronary events in the general Icelandic population. Eur J Prev Cardiolog. 2013;20:322–330. doi: 10.1177/2047487312441723. [DOI] [PubMed] [Google Scholar]
- 21.Williams L, O'Connor RC, Grubb N, O'Carroll R. Type D personality predicts poor medication adherence in myocardial infarction patients. Psychol Health. 2011;26:703–712. doi: 10.1080/08870446.2010.488265. [DOI] [PubMed] [Google Scholar]
- 22.Blumenthal JA, Babyak MA, Carney RM, et al. Exercise, depression, and mortality after myocardial infarction in the ENRICHD trial. Medicine & Science in Sports & Exercise. 2004;36:746–755. doi: 10.1249/01.mss.0000125997.63493.13. [DOI] [PubMed] [Google Scholar]
- 23.Blumenthal JA, Babyak MA, Ironson G, et al. Spirituality, religion, and clinical outcomes in patients recovering from an acute myocardial infarction. Psychosomatic Medicine. 2007;69:501–508. doi: 10.1097/PSY.0b013e3180cab76c. [Erratum appears in Psychosom Med. 2007 Nov;69(8):826]. [DOI] [PubMed] [Google Scholar]
- 24.Burg MM, Graeber B, Vashist A, et al. Noninvasive detection of risk for emotion provoked myocardial ischemia. Psychosomatic Medicine. 2009;71:14–20. doi: 10.1097/PSY.0b013e318187c035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Denollet J, Pedersen SS, Daemen J, de Jaegere P, Serruys PW, van Domburg RT. Reduced positive affect (anhedonia) predicts major clinical events following implantation of coronary artery stents. J Intern Med. 2008;263:203–211. doi: 10.1111/j.1365-2796.2007.01870.x. [DOI] [PubMed] [Google Scholar]
- 26.Lampert R, Joska T, Burg MM, Batsford WP, McPherson CA, Jain D. Emotional and physical precipitants of ventricular arrhythmia. Circulation. 2002;106:1800–1805. doi: 10.1161/01.cir.0000031733.51374.c1. [DOI] [PubMed] [Google Scholar]
- 27.Lampert R, Shusterman V, Burg M, et al. Anger induced T wave alternans predicts future ventricular arrhythmias in patients with implantable cardioverter defibrillators. Journal of the American College of Cardiology. 2009;53:774–748. doi: 10.1016/j.jacc.2008.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lett HS, Blumenthal JA, Babyak MA, et al. Social support and prognosis in patients at increased psychosocial risk recovering from myocardial infarction. Health Psychology. 2007;26:418–427. doi: 10.1037/0278-6133.26.4.418. [DOI] [PubMed] [Google Scholar]
- 29.Warner DO. American Society of Anesthesiologists Smoking Cessation Initiative Task F. Feasibility of tobacco interventions in anesthesiology practices: a pilot study. Anesthesiology. 2009;110:1223–1228. doi: 10.1097/ALN.0b013e3181a5d03e. [DOI] [PubMed] [Google Scholar]
- 30.Warner DO, Klesges RC, Dale LC, et al. Clinician delivered Intervention to Facilitate Tobacco Quitline Use by Surgical Patients. Anesthesiology. 2011:114. doi: 10.1097/ALN.0b013e31820d868d. [DOI] [PubMed] [Google Scholar]
- 31.Warner DO, Klesges RC, Dale LC, et al. Telephone quitlines to help surgical patients quit smoking patient and provider attitudes. American Journal of Preventive Medicine. 2008;35:S486–S493. doi: 10.1016/j.amepre.2008.08.032. [DOI] [PubMed] [Google Scholar]
- 32.Schonberger RB. Ideal Blood Pressure Management and our Specialty: RE: Drummond, et al. "An Observational Study of the Influence of "White coat Hypertension" on Day of Surgery Blood Pressure Determinations. J Neurosurg Anesthesiol. 2014 doi: 10.1097/ANA.0b013e31827a0151. In Press. [DOI] [PubMed] [Google Scholar]
- 33.Schonberger RB, Burg MM, Holt NF, Lukens CL, Dai F, Brandt C. The relationship between day of surgery and primary care blood pressure among Veterans presenting from home for surgery. Is there evidence for anesthesiologist initiated blood pressure referral? Anesthesia & Analgesia. 2012;114:205–214. doi: 10.1213/ANE.0b013e318239c4c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Committee on Standards and Practice Parameters (Apfelbaum JL, et al.) Practice advisory for preanesthesia evaluation: an updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology. 2012;116:522–538. doi: 10.1097/ALN.0b013e31823c1067. [DOI] [PubMed] [Google Scholar]
- 35.Holt NF, Silverman DG, Prasad R, Dziura J, Ruskin KJ. Preanesthesia clinics, information management, and operating room delays: results of a survey of practicing anesthesiologists. Anesthesia & Analgesia. 2007;104:615–618. doi: 10.1213/01.ane.0000255253.62668.3a. [DOI] [PubMed] [Google Scholar]
- 36.Hooper VD. Who staffs the perioperative surgical home? Anesthesia & Analgesia. 2013;116:754–755. doi: 10.1213/ANE.0b013e3182834728. [DOI] [PubMed] [Google Scholar]
- 37.Kroenke K, Spitzer RL, Williams JB. The PHQ 9: validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lowe B, Grafe K, Zipfel S, Witte S, Loerch B, Herzog W. Diagnosing ICD 10 depressive episodes: superior criterion validity of the Patient Health Questionnaire. Psychother Psychosom. 2004;73:386–390. doi: 10.1159/000080393. [DOI] [PubMed] [Google Scholar]
- 39.Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 40.Denollet J, Brutsaert DL. Personality, disease severity, and the risk of long term cardiac events in patients with a decreased ejection fraction after myocardial infarction. Circulation. 1998;97:167–173. doi: 10.1161/01.cir.97.2.167. [DOI] [PubMed] [Google Scholar]
- 41.Denollet J, Conraads VM. Type D personality and vulnerability to adverse outcomes in heart disease. Cleve Clin J Med. 2011;78(Suppl 1):S13–S19. doi: 10.3949/ccjm.78.s1.02. [DOI] [PubMed] [Google Scholar]
- 42.Denollet J, Holmes RVF, Vrints CJ, Conraads VM. Unfavorable outcome of heart transplantation in recipients with type D personality. J Heart Lung Transplant. 2007;26:152–158. doi: 10.1016/j.healun.2006.11.600. [DOI] [PubMed] [Google Scholar]
- 43.Denollet J, Pedersen SS. Prognostic value of Type D personality compared with depressive symptoms. Archives of Internal Medicine. 2008;168:431–432. doi: 10.1001/archinternmed.2007.120. [DOI] [PubMed] [Google Scholar]
- 44.Denollet J, Pedersen SS, Vrints CJ, Conraads VM. Usefulness of type D personality in predicting five year cardiac events above and beyond concurrent symptoms of stress in patients with coronary heart disease. American Journal of Cardiology. 2006;97:970–973. doi: 10.1016/j.amjcard.2005.10.035. [DOI] [PubMed] [Google Scholar]
- 45.Denollet J, Schiffer AA, Spek V. A general propensity to psychological distress affects cardiovascular outcomes: evidence from research on the type D (distressed) personality profile. Circulation Cardiovascular Quality & Outcomes. 2010;3:546–557. doi: 10.1161/CIRCOUTCOMES.109.934406. [DOI] [PubMed] [Google Scholar]
- 46.Denollet J, Sys SU, Brutsaert DL. Personality and mortality after myocardial infarction. Psychosomatic Medicine. 1995;57:582–591. doi: 10.1097/00006842-199511000-00011. [DOI] [PubMed] [Google Scholar]
- 47.Denollet J, Sys SU, Stroobant N, Rombouts H, Gillebert TC, Brutsaert DL. Personality as independent predictor of long term mortality in patients with coronary heart disease. Lancet. 1996;347:417–421. doi: 10.1016/s0140-6736(96)90007-0. [DOI] [PubMed] [Google Scholar]
- 48.Martens EJ, Mols F, Burg MM, Denollet J. Type D personality predicts clinical events after myocardial infarction, above and beyond disease severity and depression. J Clin Psychiatry. 2010;71:778–783. doi: 10.4088/JCP.08m04765blu. [DOI] [PubMed] [Google Scholar]
- 49.Mols F, Martens EJ, Denollet J. Type D personality and depressive symptoms are independent predictors of impaired health status following acute myocardial infarction. Heart. 2010;96:30–35. doi: 10.1136/hrt.2009.170357. [DOI] [PubMed] [Google Scholar]
- 50. [Accessed February 13, 2014];Case Management Adherence Guidelines version 2.0: Guidelines from the Case Management Society of America for improving patient adherence to medication therapies. Case Management Society of America. 2006 at http://www.cmsa.org/portals/0/pdf/cmag2.pdf.
- 51.Morisky DE, Ang A, Krousel Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. Journal of Clinical Hypertension. 2008;10:348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 52.The Management of MDD Working Group. [Accessed June 12, 2013];VA/DoD Clinical Practice Guideline For Management of Major Depressive Disorder. Department of Veterans Affairs and Department of Defense. 2009 et al., at http://www.healthquality.va.gov/MDD_FULL_3c.pdf.
- 53.Baren JM, Shofer FS, Ivey B, et al. A randomized, controlled trial of a simple emergency department intervention to improve the rate of primary care follow up for patients with acute asthma exacerbations. Annals of Emergency Medicine. 2001;38:115–122. doi: 10.1067/mem.2001.116593. [DOI] [PubMed] [Google Scholar]
- 54.Clark CE, Smith LFP, Taylor RS, Campbell JL. Nurse led interventions to improve control of blood pressure in people with hypertension: systematic review and meta analysis. BMJ. 2010;341:c3995. doi: 10.1136/bmj.c3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Horwitz SM, Busch SH, Balestracci KMB, Ellingson KD, Rawlings J. Intensive intervention improves primary care follow up for uninsured emergency department patients. Academic Emergency Medicine. 2005;12:647–652. doi: 10.1197/j.aem.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 56.Kinikini D, Sarfati MR, Mueller MT, Kraiss LW. American Heart A, American College of C. Meeting AHA/ACC secondary prevention goals in a vascular surgery practice: an opportunity we cannot afford to miss. Journal of Vascular Surgery. 2006;43:781–787. doi: 10.1016/j.jvs.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 57.Svarstad BL, Kotchen JM, Shireman TI, et al. The Team Education and Adherence Monitoring (TEAM) trial: pharmacy interventions to improve hypertension control in blacks. Circulation Cardiovascular Quality & Outcomes. 2009;2:264–271. doi: 10.1161/CIRCOUTCOMES.109.849992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tanabe P, Persell SD, Adams JG, McCormick JC, Martinovich Z, Baker DW. Increased blood pressure in the emergency department: pain, anxiety, or undiagnosed hypertension? Annals of Emergency Medicine. 2008;51:221–229. doi: 10.1016/j.annemergmed.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 59.Thomsen T, Tonnesen H, Okholm M, et al. Brief smoking cessation intervention in relation to breast cancer surgery: a randomized controlled trial. Nicotine & Tobacco Research. 2010;12:1118–1124. doi: 10.1093/ntr/ntq158. [DOI] [PubMed] [Google Scholar]
- 60.Weber CA, Ernst ME, Sezate GS, Zheng S, Carter BL. Pharmacist physician comanagement of hypertension and reduction in 24 hour ambulatory blood pressures. Archives of Internal Medicine. 2011;170:1634–1639. doi: 10.1001/archinternmed.2010.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Oertle M, Bal R. Understanding non adherence in chronic heart failure: a mixed method case study. Qual Saf Health Care. 2010;19:e37. doi: 10.1136/qshc.2009.033563. [DOI] [PubMed] [Google Scholar]
- 62.London MJ, Hur K, Schwartz GG, Henderson WG. Association of perioperative beta blockade with mortality and cardiovascular morbidity following major noncardiac surgery. JAMA. 309:1704–1713. doi: 10.1001/jama.2013.4135. [DOI] [PubMed] [Google Scholar]
- 63.Morgan RO, Teal CR, Reddy SG, Ford ME, Ashton CM. Measurement in Veterans Affairs Health Services Research: veterans as a special population. Health Services Research. 2005;40:1573–1583. doi: 10.1111/j.1475-6773.2005.00448.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. [Accessed February 14, 2014];Selected Veterans Health Administration Characteristics FY 2003 to FY 2011. et al. at http://www.va.gov/vetdata/Utilization.asp.