Abstract
The pathogenic bacterium Staphylococcus aureus actively evades many aspects of human innate immunity by expressing a series of small inhibitory proteins. A number of these proteins inhibit the complement system, which labels bacteria for phagocytosis and generates inflammatory chemoattractants. While the majority of staphylococcal complement inhibitors act on the alternative pathway (AP) to block the amplification loop, only a few proteins act on the initial recognition cascades that constitute the classical (CP) and lectin (LP) pathways. We screened a collection of recombinant, secreted staphylococcal proteins to determine if S. aureus produces other molecules that inhibit either the CP and/or LP. Using this approach, we identified the extracellular adherence protein (Eap) as a potent, specific inhibitor of both the CP and LP. We found that Eap blocked CP/LP-dependent activation of C3, but not C4, and that Eap likewise inhibited deposition of C3b on the surface of S. aureus cells. In turn, this significantly diminished the extent of S. aureus opsonophagocytosis and killing by neutrophils. This combination of functional properties suggested that Eap acts specifically at the level of the CP/LP C3 convertase (C4b2a). Indeed, we demonstrated a direct, nanomolar-affinity interaction of Eap with C4b. Eap binding to C4b inhibited binding of both full-length C2 and its C2b fragment, which indicated that Eap disrupts formation of the CP/LP C3 pro-convertase (C4b2). As a whole, our results demonstrate that S. aureus inhibits the two initiation routes of complement by expression of the Eap protein, and thereby define a novel mechanism of immune evasion.
Keywords: Staphylococcus aureus, Complement Inhibitor, Convertase
Introduction
The complement system serves as a critical hub in the human innate immune and inflammatory system, and fulfills numerous roles in homeostasis, defense, repair, and disease (1). Despite its diverse list of functions, complement remains best known for its ability to opsonize and eliminate invading microorganisms. To achieve this most efficiently, the microbial surface must first be recognized by one of a series of pattern-recognition proteins (1). These ligand-bound ‘sensors’ can then trigger one of three canonical activation routes, (the classical (CP), lectin (LP), and alternative (AP) pathways), which all result in cleavage of the abundant plasma protein C3 into its bioactive C3a (chemoattractant) and C3b (covalent opsonin) fragments. Although such activation of C3 may occur at a low level spontaneously, this central process is catalyzed at the bacterial surface through the function of two transiently-stable, multi-subunit proteolytic complexes known as C3 convertases. In the case of the CP or LP, the initiating complexes of surface Ig-bound C1 or carbohydrate-bound MBL/MASPs trigger proteolytic activation of C4 to produce C4b. Surface-bound C4b then binds C2 to form the CP/LP C3 pro-convertase which, when proteolytically-activated by the same initiation complexes named above, gives rise to the fully-active CP/LP C3 convertase, C4b2a. C4b2a converts native C3 into C3b, and ultimately gives rise to the AP C3 convertase (C3bBb). In this scenario surface deposed C3b, along with the pro-enzyme factor B (FB) and factor D (FD), cooperate to generate the C3bBb complex. It is this surface-bound AP C3 convertase that activates massive amounts of C3 into C3b, thereby being responsible for the self-amplifying nature of the complement response, and which stimulates efficient opsonization of bacteria and production of powerful inflammatory mediators like C3a and C5a (2). Furthermore, deposited C3b molecules also activate the terminal pathway of complement that results in the formation of the membrane attack complex (C5b-9) that can directly kill Gram-negative bacteria.
The pathogenic bacterium Staphylococcus aureus has evolved a diverse and multifaceted approach to successfully evade the human innate immune response (3-5). Central to this global strategy is its ability to manipulate the human complement system to a greater extent than perhaps any other pathogen studied thus far (3, 4, 6). While studies from the last decade have revealed much on the diverse nature of S. aureus complement evasion, the large number of C3 convertase inhibitors that act on the AP suggests that conceptually similar mechanism(s) that affect the CP and/or LP might be manifested by a component of the S. aureus immune evasion arsenal. In this regard, the fact that CP and LP share the same C3 convertase, C4b2a, raises the intriguing possibility that a single inhibitor might effectively block C3b deposition and downstream anaphylatoxin production via both of these pathways simultaneously. While staphylococcal complement inhibitor (SCIN) proteins have been reported to inhibit the CP and LP at the level of C3b deposition, their activities against these pathways are only partial and are substantially weaker than they are against the AP (7, 8). Thus, we hypothesized that S. aureus might express and secrete an as yet unidentified inhibitor of CP and LP C3 convertase formation and/or activity.
To this end, we screened a collection of recombinant secreted S. aureus proteins to examine whether any of these molecules had inhibitory activities on the CP/LP. In doing so, we identified the staphylococcal extracellular adherence protein (Eap) as a potent, specific inhibitor of both the CP and LP. We found that Eap, but not its structural homologs EapH1 and EapH2 (9), inhibits the CP/LP in a dose-dependent manner by forming a nanomolar affinity complex with C4b. This C4b/Eap complex inhibits binding of C2 to C4b, and therefore impedes formation of the CP/LP C3 pro-convertase. From a broader perspective, the studies we present here suggest that the effects of Eap on the CP/LP in many respects mirror those of the staphylococcal complement inhibitor Efb-C, which inhibits AP C3 pro-convertase formation by binding C3b (10). In sum, this work provides new insight into staphylococcal immune evasion, and also describes an entirely novel mechanism of CP/LP regulation that may hold significant implications for future design of therapeutic CP/LP inhibitors.
Materials and Methods
Preparation of Native and Recombinant Proteins
Human serum proteins C3, C3b, C4, C4b, C1s, C4b-binding protein (C4BP), and factor I (FI) were obtained in purified form from Complement Technologies (Tyler, TX). Recombinant forms of C2 and C2b were expressed and purified from the conditioned culture medium of transiently transfected human embryonic kidney (HEK)-293 cells according to the general methods described previously (11). All recombinant S. aureus proteins were overexpressed and purified according to the general methods described previously (12), with the exception that recombinant, full-length Eap was prepared according to the published protocol of Xie et al. (13).
Human Derived Materials
Blood was drawn from healthy adult volunteers after obtaining informed consent and approval of the protocol by the medical-ethical committee of the University Medical Center Utrecht (Utrecht, The Netherlands). Normal human serum (NHS) was isolated as described before (14) and frozen at −80 °C until needed for further use. For neutrophil preparation, heparinized vacutainers (Becton Dickinson) were used and neutrophils were isolated over a ficol/histopaque gradient as described previously (15).
Complement Pathway Activity on an Artificial Surface
Functional activity of the CP, LP and AP was determined essentially as described (16). In short, Nunc-Maxisorb ELISA plates were coated overnight to specifically activate the CP (coated with 3 μg/ml human IgM (Calbiochem)), LP (coated with 20 μg/ml Saccharomyces cerevisiae mannan (Sigma)), or AP (coated with 20 μg/ml Salmonella enteriditis LPS (Sigma)). Plates were blocked with 1% (w/v) BSA in PBS with 0.05% (v/v) Tween 20 (Merck). The indicated percentages of NHS or mouse serum (Innovative Research) were incubated with 1 μM of recombinant S. aureus proteins in the appropriate assay buffers for a maximum of 5 min at 25 °C (veronal-buffered saline (VBS) at pH 7.5 with 0.1% (w/v) gelatin, 500 μM CaCl2, and 250 μM MgCl2 for CP and LP; VBS at pH 7.5 with 0.1% (w/v) gelatin, 5 mM MgCl2, and 10 mM EGTA for AP). Deposited C3b, C4b, and C5b-9 were detected with specific antibodies (0.1 μg/ml α-human C3c WM-1 clone digoxigenin (DIG) labeled or 1 μg/ml rat-α-mouse C3 (Hycult, HM1078), American Type Culture Collection; 1 μg/ml αC4d, Quidel; 1 μg/ml αC5b-9 aE11, Santa Cruz respectively). Secondary, HRP-labeled antibodies were detected with 100 μg/ml tetramethylbenzidine and 60 μg/ml ureum peroxide in 100 mM sodium acetate buffer at pH 6.0. The reaction was stopped by adding an equal volume of 2 M H2SO4, and the absorbance at 450 nm was measured using a BioRad microplate reader.
Complement Deposition on S. aureus
S. aureus Newman WT or Δeap (MR1811) (17) were grown on a blood-agar plate overnight at 37 °C. Bacteria were resuspended in assay buffer (20 mM HEPES (pH 7.4) with 140 mM NaCl, 0.5 mM CaCl2, 0.25 mM MgCl2, and 0.1% (w/v) BSA). Eap (1 μM) was added to the indicated concentrations of NHS and this mixture was added directly to the bacteria (8 × 106 CFU) in a total volume of 100 μl and incubated at 37 °C with shaking for 10 min. Unbound components were washed away with assay buffer and deposited C3b was quantified by flow cytometry (FACS Verse, BD) by using the specific FITC-conjugated goat F(ab')2 anti-human-C3 (Protos Immunoresearch, Burlingame, CA).
Phagocytosis Assays
S. aureus Newman WT or Δeap transformed with pCM29 (18), a vector inducing constitutive expression of superfolded GFP (sGFP) under the sarA promotor, was grown in Todd-Hewitt broth (THB) until an OD600 of 0.5. Bacteria were washed with RPMI-1640 (Invitrogen) supplemented with 0.05% (w/v) human serum albumin (HSA; Sanquin), aliquoted, and stored at −80 °C until use. Eap, EapH1 or EapH2 (1 μM) was added to the indicated concentrations of NHS in RPMI/HSA and directly added to the thawed bacteria (2.5 × 106 CFU) Then, 2.5 × 105 isolated neutrophils were added to obtain a total volume of 250 μl and incubated at 37 °C with shaking at 600 rpm for 15 min. The reaction was stopped by adding 100 μl ice-cold 2% (v/v) paraformaldehyde. Phagocytosis was assessed by flow cytometry (FACS Verse, BD). Graphs show the percentage of GFP-positive neutrophils. The fluorescent signal exclusively originated from intracellular bacteria, as verified by confocal microscopy.
Neutrophil-mediated Killing
S. aureus Newman WT or Δeap were grown in THB to OD660 of 0.5 (corresponding to 2 × 108 CFU/ml). Eap was added in 1 μM and 10 % NHS was added for 15 min at 25 °C in RPMI/HSA to allow for opsonization. Opsonized bacteria (5 × 104 CFU) were incubated with 9 × 104 neutrophils in 100 μl RPMI/HSA. The reaction was stopped at the indicated time points with 900 μl ice-cold 0.1% saponin (w/v). After 15 min. the samples were resuspended via a 25-Gauge needle, to assure lysis of the neutrophils (19). Surviving bacteria were enumerated by plating serial dilutions on Luria broth-agar plates.
Eap Affinity Isolation of Human Serum Proteins
A recombinant form of Eap that harbored a single, N-terminal cysteine was expressed and purified from E. coli similarly to wild-type Eap (13). Eap produced in this manner was site-specifically biotinylated using EZ-link Maleimide-PEG2-Biotin reagent according to manufacturer's suggestions (ThermoFisher, Inc.). Following derivatization, 2 μg of Eap-biotin were added to samples containing either 20 μl EDTA serum or C4-depleted serum (Complement Technologies), and an appropriate quantity of PBS to give a final volume of 100 μl. The samples were incubated for 1 h at room temperature, after which time 30 μl of 50% (v/v) slurry of magnetic streptavidin-coated Dynabeads were added (Invitrogen, Inc.). Following an additional 15 min incubation, the beads were isolated via a magnet, washed three times with 100 μl of PBS, and all remaining liquid was removed by aspiration. 15 μl of non-reducing Laemmli buffer were added to each sample, and 5 μl of each sample were analyzed by SDS-PAGE followed by staining with Coomassie Brilliant Blue.
Stoichiometry and Molecular Weight Estimations
The apparent molecular weight and stoichiometry of the C4b/Eap complex was determined by a combination of size-exclusion chromatography and sedimentation equilibrium analytical ultracentrifugation. For chromatographic analysis, samples consisting of either C4b or C4b/Eap (20 μM final concentration) were prepared and 100 μl were injected at 0.75 ml/min onto a Superdex S200 Increase 10/30 column that had been previously equilibrated at 4 °C in a buffer of PBS. The contents of peak fractions were analyzed by Coomassie-stained SDS-PAGE of samples that had been prepared under non-reducing conditions. For sedimentation equilibrium analysis, all experiments were performed using a Beckman XL-I ultracentrifuge with a four-position analytical, titanium (AN-Ti) rotor. Protein solutions (1.6 μM C4b or C4b/Eap complex in PBS; 110 μl) and dialysate buffer (PBS; 120 μl) were placed in the double-sector centrifuge cells. The samples were equilibrated at 4 °C at 6,000 rpm and the approach to equilibrium was monitored by repetitive absorption scans at 280 nm every 6 h. The apparent equilibrium was reached after ~ 60 h. After the final data collection, the rotor was accelerated to 42,000 rpm for ~ 2 h and the cells were scanned to obtain the baseline absorption value. Data were analyzed with the software supplied with the instrument (Beckman-Coulter, Inc.). Both the protein partial specific volume and buffer density were calculated using Sednterp software (http://bitcwiki.sr.unh.edu/index.php/Main_Page).
Biotinylation of C4b
Biotinylated C4b was prepared by overnight, room-temperature incubation of native C4 (1 mg/ml final concentration) with C1s (5 μg/ml final concentration) in the presence of EZ-link Maleimide-PEG2-Biotin reagent according to manufacturer's suggestions (ThermoFisher, Inc.). The reaction mixture (250 μl in PBS (pH 7.0)) was buffer exchanged into 20 mM tris (pH 8.0), applied to a 1 ml Resource Q anion exchange column (GE LifeSciences), and the bound proteins eluted with a gradient to 1 M NaCl over 10 column volumes. Fractions containing biotinylated-C4b were identified and characterized by a combination of SDS-PAGE and Western blotting using streptavidin-conjugated HRP (ThermoFisher, Inc.). Purified C4b-biotin was pooled, quantified spectrophotometry, and stored at 4 °C in the existing buffer until further use.
AlphaScreen Binding Assays
An AlphaScreen equilibrium competition assay was used to derive both positional information and apparent dissociation constants for C4b binding to various complement components and staphylococcal inhibitors. This assay system is based upon modification of a previously published protocol (20) and is established via the following principle: a luminescence signal is generated by laser excitation of a streptavidin-coated donor bead, which recognizes C4b-biotin that binds directly to a second target protein (in this case myc-Eap), which itself can be adsorbed to an acceptor bead coated with anti-c-myc monoclonal IgG. C4b/Eap competition binding assays were carried out in a total volume of 25 μl by adding each assay component to the following final concentrations: 50 nM myc-Eap, 5 nM C4b-biotin, 20 μg/μl anti-c-myc AlphaScreen acceptor beads, and 20 μg/μl AlphaScreen donor beads. A dilution series was prepared for each unlabeled competitor protein of interest. Reactions were performed over 2.5 h and were begun by incubating the C4b-biotin, myc-Eap, and a given concentration of each competitor protein for 1 h. Following this, the acceptor beads were added, incubated for an hour, then the donor beads were added and incubated for an additional 0.5 h. At that point, the donor beads were excited at 680 nm and the evolving AlphaScreen signal (photon counts/s at 630 nm) for each data point was measured using an EnSpire multimode plate reader (Perkin Elmer Life Sciences). Data analysis and curve fitting was carried out as previously described (20).
Surface Plasmon Resonance Experiments
Interactions between C4b-biotin and the S. aureus proteins Eap, EapH1, and EapH2 were measured by surface plasmon resonance (SPR) using either a BiaCore X or BiaCore 3000 instrument (GE Life Sciences) at room temperature. PBS-T (i.e. PBS (pH 7.0) with 0.005% (v/v) Tween-20) was used as the running buffer throughout the entire set of experiments. C4b-biotin was captured on a streptavidin sensor chip (GE Life Sciences) to a density of approximately 5,000 resonance units (RU). Ligands were diluted to their working concentrations in PBS-T. For comparison of EAP-domain proteins’ binding to C4b, samples were prepared at 1 and 10 μM and injected for 1 min at a flow rate of 20 μl/min, followed by a dissociation phase of 2 min. Signals were normalized to the molecular weight of each respective analyte to allow for a ranking of Eap, EapH1, and EapH2 relative affinities for C4b. Surface regeneration was achieved by injecting a solution of 1 M NaCl. Data analyses were carried out using the BiaEvaluation software suite (GE Life Sciences).
An SPR assay was also used to assess the competition between Eap and C2 for binding to C4b (21). Briefly, a C4b-biotin surface was prepared as described above and a room temperature running buffer of HBS-CMT (20 mM HEPES (pH 7.4), 150 mM NaCl, 5 mM CaCl2, 5 mM MgCl2, and 0.005% (v/v) Tween-20) with a flow rate of 20 μl/min was used for all injections. C2 was injected in triplicate at a concentration of 200 nM to establish a basal level of C2 binding. This concentration was held constant for the competition experiments, which were carried out by varying either the Eap or Eap34 concentration over six points from 5000 nM to 8 nM. To calculate residual C2 binding, the sensorgram of the corresponding Eap/Eap34 injection alone was subtracted from the Eap/Eap34+C2 injection series. The averaged response for the 5 s preceding the injection stop was plotted against the concentration of Eap/Eap34 and fit to a dose-response inhibition curve by non-linear regression as previously described (20). Regeneration of the surface was carried out with 2 M NaCl for 2 min followed by 0.2 M sodium citrate for 2 min.
FI Proteolysis Assay
Sequential FI-dependent proteolysis of C4b to iC4b and C4c was monitored by an SDS-PAGE based method. A sample of C4b (0.4 μg/μl in PBS) was incubated with purified FI (0.01 μg/μl) either in the presence or absence of C4BP (0.09 μg/μl), and/or various concentrations of Eap (0, 0.01, 0.06, and 0.6 μg/μl, respectively). Aliquots reflecting the time-course of proteolysis were withdrawn at 0, 2, 5, 10, and 20 min, and the reaction was quenched by addition of Laemmli sample buffer with β-mercaptoethanol to reduce disulfide bonds. Samples were separated on a 10% (w/v) tris-tricine polyacrylamide gel and stained with Coomassie blue. Excised gel bands were reduced, alkylated and subjected to in-gel trypsin digestion by standard methods, and extracted peptides were analyzed by tandem MS as described previously (22). Identification of activated C4 fragments was accomplished using Mascot 2.4 (Matrix Science, Ltd.) with semi-trypsin specificity. Individual band staining intensities and ratios were quantified by ImageJ (23).
Statistics
All analyses were performed in GraphPad Prism 6.0.
Results
Identification of Eap as an inhibitor of the CP and LP of Complement
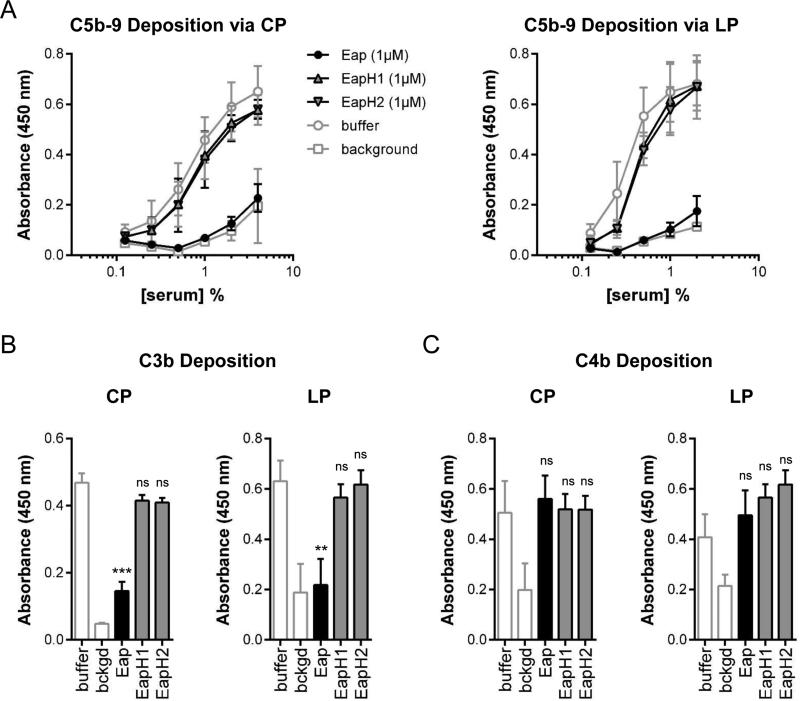
We screened a library of approximately 30 secreted staphylococcal proteins to test if any of these molecules were capable of inhibiting the CP and LP on the surface of pathway-specific activator/acceptor coated ELISA plates (16). In doing so, we discovered that a recombinant form of Eap inhibited both pathways at the level of terminal complement complex (C5b-9) deposition (Fig. 1A). This effect was specific for the CP and LP, since Eap did not block the AP (Data Not Shown). A gene encoding Eap is found in 98% of all clinical isolates of S. aureus (24). Although there is some variability in the molecular weight of Eap protein produced by different strains, characterization of Eap from S. aureus strain Mu50 (~50 kDa) and Newman (~63 kDa) in various assays suggests that these two isoforms retain similar functions (13, 17). Consistent with this, Eap proteins from both S. aureus Mu50 and Newman are equally potent in their ability to inhibit the CP and LP (Data Not Shown). Eap from S. aureus strain Mu50 is comprised of four tandem repeats of an ~100 residue motif known as the EAP domain (9). These repeats share between 40-80% identity with one another, and approximately 25-50% identity to the structurally related S. aureus proteins, EapH1 and EapH2, which themselves consist of little more than a single EAP domain (9). While Eap potently inhibited the CP and LP at the level of C5b-9, neither EapH1 nor EapH2 had any significant impact on either pathway. Thus, the inhibitory effect on the CP and LP is specific to Eap, and not a general feature of EAP domain-containing proteins. To determine the specific steps in the CP and LP that are inhibited by Eap, we investigated whether Eap could block C4b or C3b deposition. We found that Eap inhibited C3b deposition by the CP and LP both in human and mouse serum (Fig. 1B, Supplemental Fig. 1A), but Eap failed to block C4b deposition (Fig. 1C). Together, these results indicate that Eap blocks activation of C3, but not C4, via both the CP and LP of complement.
Figure 1. Eap Inhibits Complement Activation via the Classical and Lectin Pathways.
The effect of Eap on distinct routes of complement activation was assessed via ELISA-based methods. (a) The effect of 1 μM Eap, EapH1, or EapH2 on CP (left) and LP-mediated (right) complement activation was measured across a dilution series of NHS. Activation was detected as C5b-9 deposition on an ELISA plate surface. Legend is inset. (b) The effect of 1 μM Eap, EapH1, or EapH2 on CP and LP-mediated complement activation in 1% (v/v) NHS was measured. Activation was detected as C3b deposition on an ELISA plate surface. (c) The same experiment as in panel b, except that activation was detected as C4b deposition on an ELISA plate surface. Error bars represent the mean ± standard deviation of three independent experiments. Measures of statistical significance in panels b and c were determined by an unpaired t-test of each experimental series versus buffer control. **, p≤0.01; ***, p≤0.001; ns, not significant.
Eap Inhibits Deposition of C3b at the S. aureus Surface and Blocks Phagocytosis and Killing
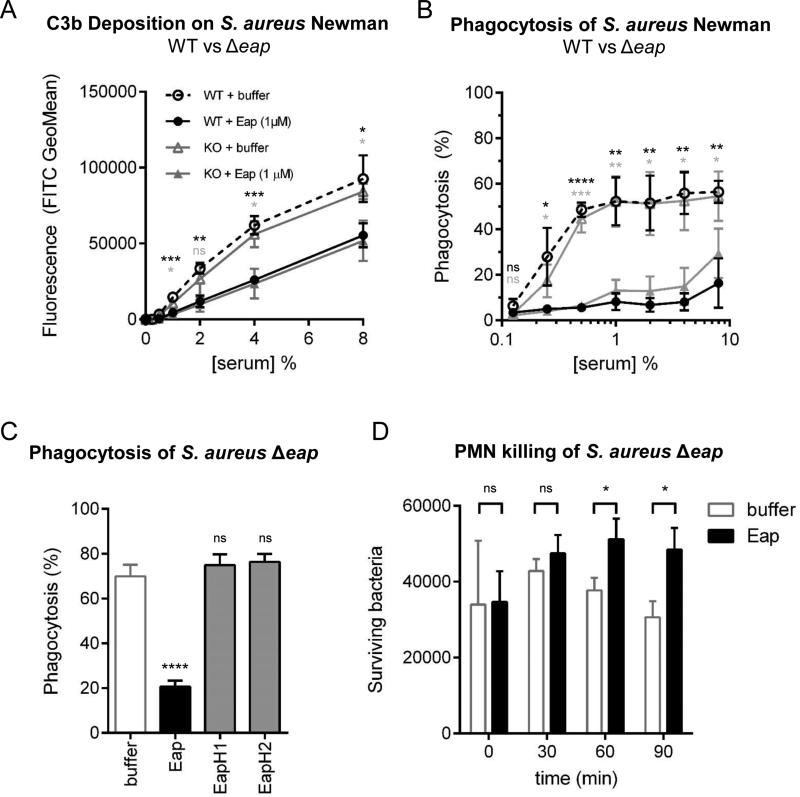
The results described above revealed that Eap specifically inhibits C3 activation via the CP and LP. Nevertheless, one limitation of these experiments is that they employed artificial activator and acceptor surfaces to study the complement response. To test whether Eap could impact an experimental system that more closely reflects the situation found in vivo, we examined the effect of Eap on C3b opsonization of the S. aureus cell surface. Although Eap is a secreted protein, approximately 30% of Eap rebinds the bacterial surface after secretion (25). To address the role of surface-bound Eap in complement inhibition, we analyzed C3b deposition and subsequent phagocytosis for both the S. aureus Newman WT strain and an isogenic eap-mutant strain (Δeap) in parallel (17) (Supplemental Fig. 1B). Neither assay revealed any difference in the level of C3b deposition or phagocytosis between the WT and mutant strain in the absence of exogenous Eap, suggesting that surface-retained Eap does not contribute significantly to S. aureus complement evasion (Fig. 2A, B). However, exogenously added Eap (1 μM) blocked deposition of C3b on both strains by nearly 50% across four different serum concentrations that ranged from 1% to 8% (v/v) (Fig. 2A). As expected, this diminished level of C3b opsonization in the presence of Eap significantly inhibited the efficiency with which neutrophils phagocytosed both strains (Fig. 2B).
Figure 2. Eap Inhibits Opsonization, Phagocytosis, and Killing of Staphylococcus aureus.
The impact of recombinant Eap on complement deposition and phagocytosis of S. aureus Newman strains was assessed using flow cytometry. (a) C3b deposition on the surface of S. aureus Newman WT or Δeap in the presence of 1 μM Eap or a buffer control. Legend is inset. (b) Phagocytosis of S. aureus Newman WT or Δeap in the presence of 1 μM Eap or a buffer control. Legend is inset in the adjacent panel. (c) Extent of phagocytosis of S. aureus Newman Δeap using 1% (v/v) NHS in the presence of 1 μM Eap, EapH1, or EapH2, or a buffer control. (d) Neutrophil-mediated killing of S. aureus Newman Δeap opsonized in the presence of 1 μM Eap or a buffer control. Error bars represent the mean ± standard deviation of three independent experiments and at least two different donors. Legend is inset. Measures of statistical significance were determined by an unpaired t-test of each experimental series versus the corresponding buffer control for each strain and serum concentration as appropriate. *, p≤0.05; **, p≤0.01; ***, p≤0.001; ****, p≤0.0001; ns, not significant.
We then used the Δeap strain to conduct several additional experiments aimed at assessing the significance of Eap's effects on phagocytosis and its impact on bacterial survival. To begin, we found that inhibition of phagocytosis by increasing concentrations of Eap was both dose-dependent and saturable (Supplemental Fig. 1C). Importantly, the concentration of Eap found in stationary liquid cultures of S. aureus (up to 10 μg/ml, or ~ 200 nM (26)) resulted in greater than 50% inhibition of phagocytosis by human neutrophils. While the concentration of Eap secreted into the human body during S. aureus infections remains uncertain, these data suggest that Eap-dependent inhibition of the CP/LP, and subsequently of phagocytosis, is likely physiologically relevant. Along these lines, and in concordance with the ELISA data presented above, this anti-phagocytic effect was not observed when either control protein EapH1 or EapH2 was added at the same exogenous concentration that resulted in potent inhibition of phagocytosis by Eap (Fig. 2C). Finally, we observed that diminished levels of phagocytosis likewise resulted in significantly diminished killing of S. aureus by human neutrophils (Fig. 2D). Together, these results indicate that secreted Eap specifically blocks CP/LP-mediated opsonization of S. aureus with C3b and subsequent phagocytosis and killing of S. aureus by neutrophils.
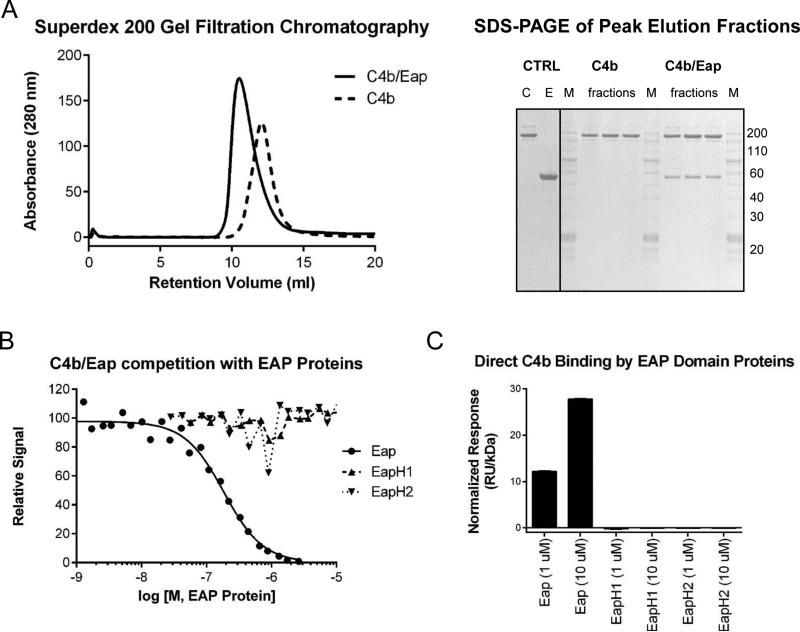
Eap Binds with Nanomolar Affinity to Complement Component C4b
We observed that Eap bound an approximately 200 kDa protein present in EDTA-treated human serum but not in C4-depleted serum (Supplemental Fig. 2A). While this result provided evidence that Eap binds to native C4, the functional studies presented above indicated that Eap inhibits an event within the CP and LP that mediates activation of C3 but leaves C4 activation intact. We therefore predicted that Eap must act on either the fully assembled CP/LP C3 convertase (C4b2a) or an isolated component thereof. As a first test of this hypothesis, we examined the behavior of purified C4b and a mixture of C4b and Eap by analytical size-exclusion chromatography (Fig. 3A, left panel). Inclusion of equimolar amounts of Eap in the C4b sample resulted in a pronounced shift of the peak to a larger apparent molecular weight that eluted as a single species. Indeed, bands corresponding to both Eap and C4b were present when the peak fractions were analyzed by Coomassie-stained SDS-PAGE (Fig. 3A, right panel). Due to potential inaccuracy of molecular weight estimates obtained from size-exclusion chromatography, we also used analytical ultracentrifugation to provide further characterization of the C4b/Eap complex. Sedimentation equilibrium data for both C4b/Eap and C4b alone were obtained at one concentration and were well-described by a single particle model (Supplemental Fig. 2C). Whereas the molecular weight for C4b itself was estimated at 268 kDa, the apparent molecular weight C4b/Eap was estimated at 308 kDa. Since previous sedimentation equilibrium studies of Eap yielded an apparent molecular weight of 51 kDa for this protein (27), these data strongly suggest that Eap forms a 1:1 complex with C4b.
Figure 3. Eap Forms a Nanomolar Affinity Complex with Complement Component C4b.
(a) Analysis of the C4b/Eap complex by analytical gel-filtration chromatography. Chromatograms for C4b and C4b/Eap are shown in the left panel, while Coomassie-stained SDS-PAGE analysis of the peak fractions from each injection is shown in the right panel. Control lanes are designated as: C, C4b; E, Eap; and M, molecular weight marker. (b) The ability of untagged Eap, EapH1, and EapH2 to compete the AlphaScreen signal generated by myc-Eap and C4b-biotin was assessed over a logarithmic dilution series. While three independent trials were carried out, the data presented here are from single representative titrations. The smooth line indicates the outcome of fitting all points to a dose-response curve when competition was observed. Legend is inset. (c) Binding of Eap, EapH1, and EapH2 to an oriented C4b-biosensor surface. The peak signals achieved following injection stop for samples at 1 and 10 μM, done in triplicate, were normalized to the molecular weight of their respective analyte proteins. Note that error bars are shown, but represent comparatively small variations due to the high precision of the assay system.
We next utilized a bead-based AlphaScreen assay to explore both the affinity and specificity of the C4b/Eap interaction in greater detail (20, 28). Whereas untagged Eap itself could diminish the luminescence signal generated by interaction between myc-tagged Eap and C4b-biotin in a dose-dependent manner, neither EapH1 nor EapH2 had any competitive effect even at the highest concentrations tested (Fig. 3B). Non-linear curve fitting of the C4b/Eap competition data revealed an apparent Kd of 185 ± 14 nM for this complex. Saturable binding of similar affinity was also observed when either native C4 or C4c was used as the competitor, and fit to apparent Kd values of 45 ± 2 and 138 ± 16 nM, respectively (Supplemental Fig. 2B). To study the C4b/Eap interaction through an independent approach, we constructed an SPR biosensor wherein C4b-biotin was uniformly immobilized on a streptavidin-coated surface similarly to what we have previously reported for C3b-biotin (10, 20, 21, 28). Significantly, neither EapH1 nor EapH2 bound the C4b surface even at concentrations 10-fold higher than those which showed clear evidence of C4b binding by Eap (Fig. 3C). Thus, the ability of Eap to bind C4b and the lack of C4b binding by EapH1 and EapH2 is in agreement with the inhibition of CP/LP function by Eap and the lack thereof by its homologues.
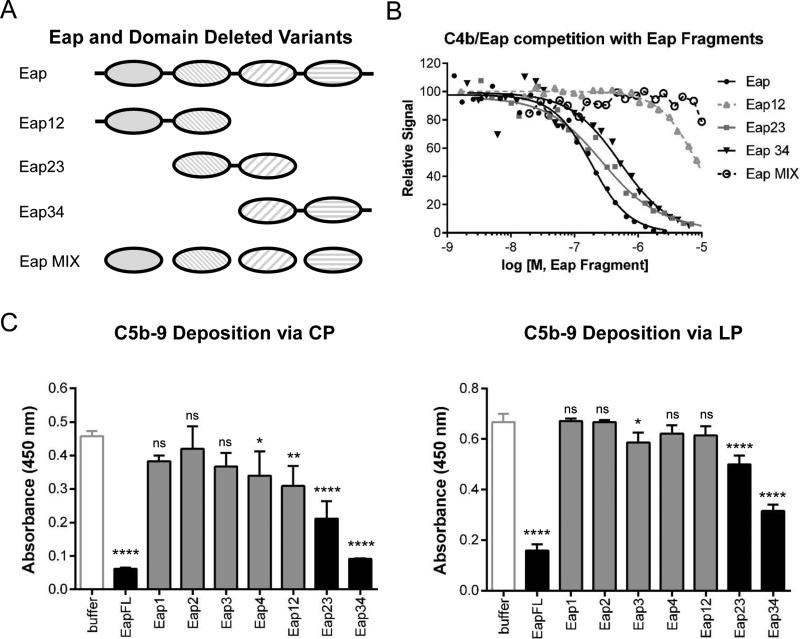
Eap Binding to C4b and Subsequent Inhibition of the CP/LP Requires the Third Domain of Eap
The modular architecture of the Eap protein raised questions as to whether a discrete combination of these domains is responsible for binding to C4b and, furthermore, whether that domain drives inhibition of CP/LP activity. To address these issues simultaneously, we overexpressed and purified a series of Eap fragments consisting of adjacent pairs of domains (i.e. Eap12, Eap23, and Eap34) as well as the individual Eap repeats themselves (i.e. Eap1, Eap2, Eap3, and Eap4) (Fig. 4A). Like EapH1 and EapH2, an equimolar mixture of the individual Eap repeats did not compete the luminescence signal generated by myc-Eap binding to C4b-biotin at concentrations up to 10 μM (Fig. 4B). Similarly, competition by Eap12 was detected only at the highest concentrations examined. By contrast, saturable binding of nearly equivalent affinity to Eap was observed in the same assay system for both Eap23 (Kd = 293 ± 38 nM) and Eap34 (Kd = 525 ± 65 nM) (Fig. 4B). Consistent with this, Eap23 and Eap34 both inhibited C5b-9 deposition via the CP and LP, though Eap34 did so at levels closer to Eap in both assays (Fig. 4C). In summary, the facts that (i) none of the individual Eap domains manifested clear C4b-binding or inhibitory properties against either the CP or LP, (ii) Eap12 bound C4b nearly 100-fold more weakly than Eap itself and failed to inhibit both the CP and LP on its own, and (iii) Eap23 and Eap34 both bind C4b and inhibit the CP and LP indicate that domain Eap3 is necessary, but not sufficient for Eap binding to C4b and inhibition of the CP and LP.
Figure 4. The Third Domain of Eap is Necessary for C4b Binding and Inhibition of the CP/LP.
(a) Diagram of full-length and domain-deleted forms of Eap used to map functional sites within the Eap protein. (b) The ability of untagged Eap, Eap12, Eap23, Eap34, and an equimolar mixture of individual Eap domains (Eap MIX) to compete the AlphaScreen signal generated by myc-Eap and C4b-biotin was assessed over a logarithmic dilution series. While three independent trials were carried out, the data presented here are from a single representative titrations. The smooth line indicates the outcome of fitting all points to a dose-response curve when competition was observed. Legend is inset. (c) The effect of including 1 μM Eap, or various truncations thereof, on C5b-9 deposition on ELISA plates coated with either CP- (left panel) or LP-specific (right panel) activators. 1% (v/v) NHS was used as a source of complement components. Error bars represent the mean ± standard deviation of three independent experiments. Measures of statistical significance were determined by one-way ANOVA for the various Eap truncations versus buffer control alone. *, p≤0.05; **, p≤0.01; ****, p≤0.0001; ns, not significant.
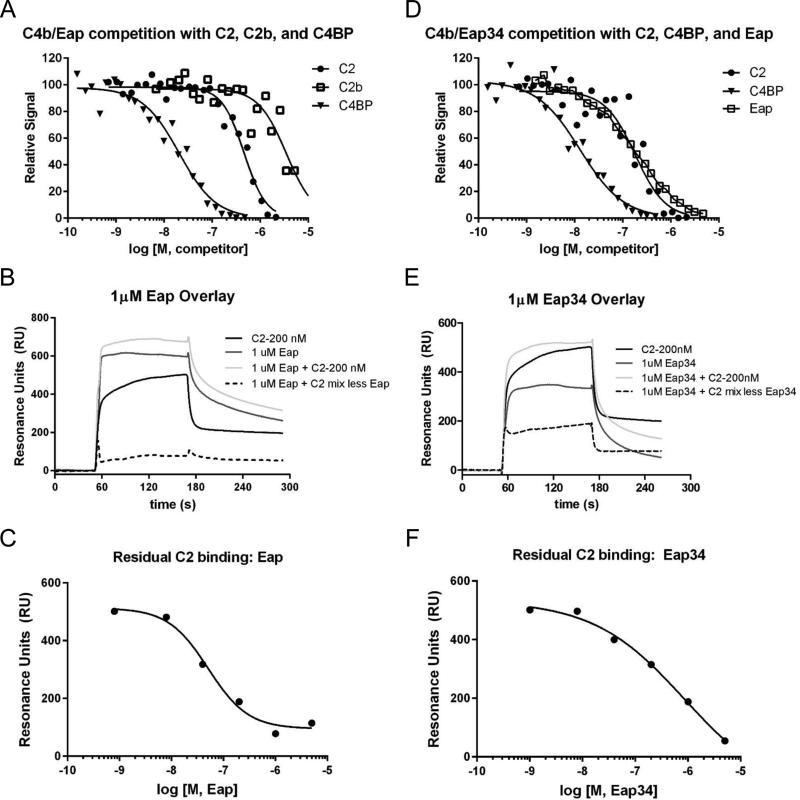
Eap Blocks Binding of C2 to C4b by Interfering with the Initial C4b2 Interaction
Formation of the CP/LP C3 convertase is a stepwise process that starts with the deposition of surface-bound C4b. Though C4b has no enzymatic activity of its own, it serves as a molecular platform first for binding of C2 to yield the C4b2 pro-convertase and then for C1s/MASP-dependent cleavage of C2 to generate a fully-active C4b2a convertase (1). We examined whether Eap binding to C4b would inhibit binding of C2 to C4b, and thus disrupt formation of the C4b2 pro-convertase. Indeed, C2 efficiently diminished the luminescence signal in the AlphaScreen assay generated by myc-Eap and C4b-biotin with an apparent IC50 of 460 ± 32 nM (Fig. 5A). The C2 pro-protease is comprised of two functionally discrete regions. Whereas the larger C2a region houses its serine protease module, the smaller C2b fragment provides the molecular basis for its initial interaction with C4b (29, 30). We therefore tested whether Eap inhibition of C2 binding to C4b might arise from disrupting the C4b2b interaction using the same AlphaScreen assay system described above. Although C2b bound to C4b with approximately 7.6-fold lower affinity than full-length C2 (IC50 = 3.5 ± 0.6 μM), it still effectively competed with Eap for C4b binding (Fig. 5A). Together, these data show that Eap shares a common binding site on C4b with C2 and, further, that this C4b site is also important for forming the initial interaction that gives rise to the CP/LP C3 pro-convertase, C4b2.
Figure 5. Eap Binding Inhibits the Interaction of Complement Component C2 with C4b.
(a) The ability of recombinant human C2, C2b, and C4BP to compete the AlphaScreen signal generated by myc-Eap and C4b-biotin was assessed over a logarithmic dilution series. While three independent trials were carried out, the data presented here are from a single representative titration. The smooth line indicates the outcome of fitting all points to a dose-response curve. (b) Representative data from an SPR competition experiment where the effect of 1 μM Eap on the interaction of 200 nM C2 with a C4b-biotin surface was examined. A legend showing the identity of each sensorgram is inset. The residual C2 binding in the presence of Eap is shown as a dashed line, while the sensorgram for the same concentration of C2 in the absence of any Eap is shown as the darkest black line. (c) Residual C2 binding in the presence of various concentrations of Eap fit to a dose-response curve (IC50 = 50 nM). (d) Identical experiment to panel a, with the exception that the ability of recombinant human C2, C4BP, and Eap to compete the AlphaScreen signal generated by myc-Eap34 and C4b-biotin was assessed. (e) Identical experiment to panel b, with the exception that Eap34 was used as the competitor instead of Eap. The residual C2 binding in the presence of Eap34 is shown as a dashed line, while the sensorgram for the same concentration of C2 is shown as the darkest black line. (f) Residual C2 binding in the presence of various concentrations of Eap34 fit to a dose-response curve (IC50 = 870 nM).
To test this inhibitory mechanism through an alternative approach, we devised an SPR strategy to investigate the outcome of increasing Eap concentrations on the ability of a C4b-biotin surface to bind C2 (Fig. 5B). In this experiment, if C4b were capable of binding Eap and C2 independently of one another, then the sensorgrams characteristic of the specific concentrations for each analyte alone would be strictly additive. Injection of 200 nM C2 in the presence of Eap resulted in a diminished response from what would be expected from two independent analytes, however. When the residual C2 contribution to the SPR signal from six different observations was fit to a dose-response curve as a function of Eap concentration, we obtained an IC50 value of approximately 50 nM (Fig. 5C). Since this figure is in reasonably good agreement with the Kd of the C4b/Eap interaction (185 nM, as determined by AlphaScreen (Fig. 3B)), the outcome of this set of experiments provided an independent confirmation of the results presented in Fig. 5A above.
The requirement of Eap3 for both C4b binding (Fig. 4B) and inhibition of CP/LP activity (Fig. 4C) suggested that the ability to inhibit C4b2 binding should also be intrinsic to a minimal functional region of the Eap protein. To test this hypothesis, we established another AlphaScreen assay system where the ability of various ligands to inhibit the luminescence signal generated by myc-Eap34 binding to C4b-biotin could be assessed quantitatively. Using this approach, we determined that full-length C2 likewise competed with Eap34 for a binding site on C4b with an apparent IC50 of 180 ± 31 nM (Fig. 5D). While this apparent IC50 represents somewhat tighter binding than was observed for C2 competing the myc-Eap C4b-biotin pair (460 ± 32 nM), the higher noise level inherent to this latter assay may have affected the accuracy of fitting these data. Nevertheless, a repeat of the SPR competition assay, this time using Eap34 instead of full-length Eap, yielded similar results to those obtained previously (Fig. 5E). When the residual C2 contribution to the SPR signal from six different observations was fit to a dose-response curve as a function of Eap34 concentration, we obtained an IC50 value of approximately 870 nM (Fig. 5F). Again, this value is in good agreement with the Kd of the C4b/Eap34 interaction (525 nM, as determined by AlphaScreen (Fig. 4B)). Thus, the observation that Eap34 on its own competes with C2 for C4b binding demonstrates that disruption of the initial pro-convertase assembly event is necessary for Eap-mediated inhibition of the CP/LP.
The Eap Binding Site on C4b Represents a Functional Hotspot within the CP/LP
The CP/LP C3 convertase is only transiently stable when formed and decays with a half-life of approximately 60 s at 37 °C (31). This rate of spontaneous decay is greatly enhanced in the presence C4BP, which irreversibly dissociates C2a from its C4b scaffold and in addition serves as a cofactor for FI-mediated degradation of C4b to iC4b and C4c. Since the results presented here demonstrated that Eap effectively inhibits C4b2 binding, we examined whether Eap might also disrupt the interaction of C4BP with C4b. Through use of the AlphaScreen assay, we found that C4BP also competed with Eap for binding to C4b (Fig. 5A). Non-linear curve fitting of the competition data revealed an apparent IC50 of 21 ± 3 nM for the C4b/C4BP interaction, which represents approximately 9-fold tighter binding when compared to the C4b/Eap interaction (Fig. 3B). This suggests that Eap would not disrupt the inhibitory function of C4BP when both are present in equimolar concentrations. We obtained a similar result when C4BP was used to compete the luminescence signal generated by myc-Eap34 binding C4b-biotin (Fig. 5B), where non-linear curve fitting revealed an apparent IC50 of 13 ± 2 nM. It has to be noted, however, that this IC50 value reflects only the apparent affinity, and does not represent that of the individual C4b binding sites present within the polyvalent C4BP assembly (32).
Since Eap binds C4b at a similar site as C4BP, we tested whether Eap itself might display intrinsic cofactor activity to stimulate FI-mediated proteolysis of C4b. When purified C4b was incubated with both C4BP and FI, we were able to show rapid degradation of C4b into iC4b and then C4c, as judged by SDS-PAGE and LC-MS/MS of tryptic peptides derived from various bands on gel (Supplemental Fig. 3A, top panel, left). However, substitution of Eap for C4BP in an otherwise identical assay provided no evidence for proteolysis of C4b by FI (Supplemental Fig. 3A, top panel, right). Thus, while Eap has no intrinsic FI co-factor activity, it shares a C4b binding site with multiple factors critical to the function and regulation of the CP/LP. We therefore propose that the Eap binding site on C4b represents a functional hotspot within the CP/LP, and that this hotspot is analogous to what we previously described for the binding site of the SCIN family of AP inhibitors on C3b (6, 20, 21, 33).
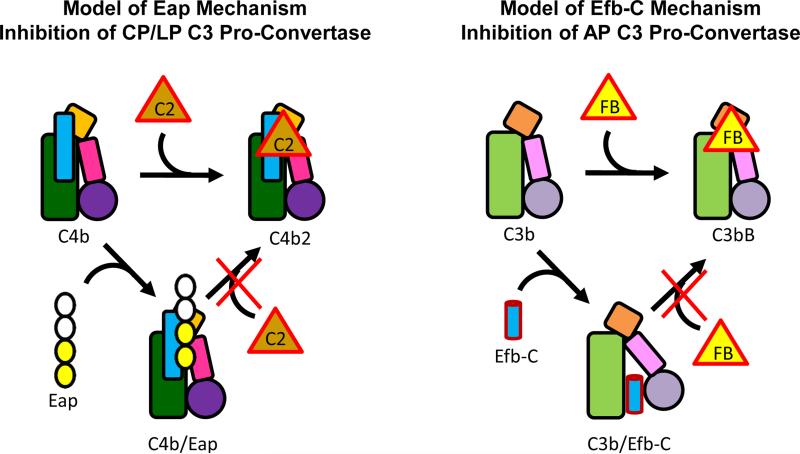
Discussion
Although a number of recent studies have described unique mechanisms deployed by S. aureus to disrupt and evade human immunity, a large majority of these have focused on strategies that specifically target components within the complement AP (e.g. C3b). In this study, however, we used a biochemical screening strategy to identify S. aureus Eap as an inhibitor of both the CP and LP. Inhibition of the CP/LP is specific to Eap, since this activity is not found in either of its closest structural homologs, EapH1 and EapH2, that also adopt the β-grasp fold characteristic of EAP domains (9, 34). Eap-mediated inhibition of the CP and LP occurs directly, since it arises from Eap forming a nanomolar affinity complex with a shared component of both pathways, C4b. Thus, instead of expressing specific inhibitors for the CP and LP separately, our results show that S. aureus simultaneously disrupts the two most potent complement initiation routes via a single protein, Eap. On this basis, we believe that Eap defines both a novel mechanism of staphylococcal immune evasion and a new class of complement regulatory proteins.
A number of other significant bacterial and fungal pathogens have also been shown to subvert the activity of CP and LP (Reviewed in (3, 35)). However, nearly all of these organisms evade the CP and LP via adsorption of the naturally occurring CP/LP regulator, C4BP, to their surface via expression of specific C4BP binding proteins. This is conceptually similar to evasion of the AP through cell-surface adsorption of FH via FH-binding proteins, which is very likely the single most widely distributed complement evasion strategy among pathogens (3, 35). Interestingly, the fact that Eap functions not by binding to a naturally occurring regulator (i.e. C4BP), but through the altogether distinct mechanism of blocking initial stages of CP/LP C3 pro-convertase assembly mirrors what we have previously described for S. aureus evasion of the AP (Reviewed in (6)). Here, expression and secretion of factors such as SCIN-A, SCIN-B/-C, Efb, and Ehp/Ecb has been demonstrated to interfere with one or more of the molecular events required to assemble and/or regulate the fully active AP C3 convertase, C3bBb. For whatever reason, it seems that S. aureus has taken a unique evolutionary path that has led it to produce multiple inhibitors that act by binding directly to either C3b or C4b, which themselves serve as essential scaffolds for assembly of all C3 and C5 convertases. Although the possibility that S. aureus also absorbs native host regulators FH (36) and C4BP (37) cannot be discounted, an overwhelming amount of structural, biochemical, functional, and immunological evidence in the literature strongly suggests that direct inhibition of convertase assembly, dynamics, and function, rather than indirect disruption via adsorption of fluid-phase regulators, is of paramount importance to S. aureus pathogenesis.
Our functional data demonstrate that Eap blocks both the CP and LP at the level of C3 activation. This inhibition arises from impaired formation of the CP/LP C3 pro-convertase, C4b2, which would subsequently reduce formation of the active CP/LP C3 convertase, C4b2a. The mechanistic basis of CP/LP inhibition by Eap therefore appears very similar to AP inhibition by Efb-C, which itself binds to C3b and reduces formation of the AP C3 pro-convertase, C3bB, by nearly 80% (10) (Fig. 6). An important distinction between Eap and Efb-C, however, is that the latter has been shown to act in an allosteric manner (10). Our observation of direct competition for C4b binding between Eap and both C2 and C2b seems to favor a purely steric mechanism for Eap inhibition of CP/LP C3 convertase formation, although the possibility of Eap-dependent ‘action-at-a-distance’ type effects on C4b cannot be dismissed without significantly more structural insights into these interactions. Still, the fact that Eap also blocks the C4b/C4BP interaction strongly suggests that the Eap binding site on C4b constitutes a functional ‘hotspot’ for CP/LP C3 convertase formation, dynamics, and function. This raises some attractive conceptual analogies between Eap and the SCIN family of C3b-binding AP C3 convertase inhibitors (6, 20, 21). Furthermore, it also suggests that effective targeting of these functional ‘hotspots’ that exist in various host response pathways might be a central theme behind pathogen-specific evolution of innate immune evasion mechanisms.
Figure 6. Proposed Mechanism for Eap-mediated Inhibition of the CP/LP C3 and Its Similarities to the S. aureus AP Inhibitor, Efb-C.
The overall structural similarities between C4b and C3b are represented by the similar shapes of their cartoon representations. The shaded green rectangle represents the macroglobulin-like core, the orange square the C345C domain, the small pink rectangle the CUB domain, and filled circle the thioester-containing domain (i.e. C4d and C3d). The thin blue rectangle represents the γ-chain unique to C4/b. The inhibitor Eap is shown in the left panel with two domains filled in yellow to represent the domains 3 and 4 ‘active site’, as described in Figs. 4 and 5. The inhibitor Efb-C is shown as a blue cylinder in the right panel. Efb-C binding to the C3d domain (45) and stabilization of an open, inactive conformation of C3b that is unable to bind FB (10) is depicted by reorientation of the CUB-TED region relative to the macroglobulin-like core of C3b.
Given its potent effects on the CP and LP, it is perhaps not surprising that Eap has been shown to promote staphylococcal virulence in rodent models of both acute peritonitis (38), as well as chronic arthritis, osteomyelitis, and abscess formation (39). Though the precise contributions of the CP and LP remain to be fully evaluated in each of these experimental systems, the consistent requirement of Eap for maximal levels of staphylococcal virulence in such studies is difficult to ignore. Moreover, the discovery that patients with demonstrated S. aureus infections present with high titers of anti-Eap antibodies (40), and that their titers of anti-Eap IgG correlate with the severity of infection (40), strongly suggests that Eap inhibition of the CP/LP is relevant to human disease as well. Along these lines, we have recently made the unexpected observation that all staphylococcal EAP domain-containing proteins (i.e. Eap, EapH1, and EapH2) are capable of high-affinity, non-covalent inhibition the innate immune serine proteases neutrophil elastase, cathepsin G, and proteinase-3 (17). These so-called ‘neutrophil serine proteases’ (NSPs), which are stored in azurophilic granules and released upon neutrophil activation, serve a number of crucial roles in both neutrophil effector functions and in the innate cellular response against invading microorganisms such as S. aureus (41). The fact that complement activity is based upon a series of site-specific proteolyses seems to suggest that EAP domain-mediated inhibition of NSPs must share basic molecular-level features with inhibition of the CP/LP by Eap. However, our observations that (i) CP/LP inhibition is specific to Eap, and not intrinsic to all EAP domains (Figs. 1 and 2), (ii) this inhibition is based upon the unique ability of Eap to bind C4b (Figs. 3 and 4), and (iii) Eap blocks, rather than promotes recruitment of the C2 pro-protease to C4b (Fig. 5), as might otherwise be expected for a high-affinity protease inhibitor (17), argue that the structural basis for Eap's effects on the CP/LP must be altogether distinct from EAP domain inhibition of NSPs. Understanding the nature of these distinctions at the structural level should therefore prove to be a very informative endeavor.
Though much remains to be learned in that regard, it is already abundantly clear that a number of debilitating and potentially lethal human diseases have been linked to either acute or chronic overactivation of the complement CP and/or LP (42-44). Among these are ischemia/reperfusion injuries, rheumatoid arthritis, systemic lupus erythematosus, multiple sclerosis, and even Alzheimer's disease. Since many of these diseases are only poorly managed by current therapeutic regimens, our discovery of Eap as a potent CP/LP inhibitor raises the possibility that improved treatment of these conditions might come through further detailed study of Eap, its molecular interactions, and its ability to specifically attenuate CP/LP activity in vivo. Since high levels of anti-Eap antibodies are found in even healthy persons (40), direct use of Eap as a therapeutic is unlikely, due to greatly increased risk of immune complex disease. Thus, future work aimed at discovering either non-immunogenic peptides, peptidomimetics, or even small molecules that retain Eap-like inhibitory activities on the CP/LP will be necessary to exploit Eap's promise within these areas.
Supplementary Material
Acknowledgements
We thank Dr. Edimara S. Reis, Dr. Apostolia Tzekou and Ms. Antigonia Ulndreaj for their assistance in the functional analysis of Eap. We also thank Prof. Matthias Herrmann and Dr. Markus Bischoff for providing samples of Eap from S. aureus strain Newman.
This work was supported by U.S. National Institutes of Health grants AI071028 and AI113552 to B.V.G., and AI068730, AI030040, and AI097805 to J.D.L, and by a Vidi grant from the Netherlands Organization for Scientific Research (NWO-Vidi, #91711379) to S.H.M.R.
References
- 1.Ricklin D, Hajishengallis G, Yang K, Lambris JD. Complement: a Key System for Immune Surveillance and Homeostasis. Nat. Immunol. 2010;11:785–797. doi: 10.1038/ni.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harboe M, Ulvund G, Vien L, Fung M, Mollnes TE. The Quantitative Role of Alternative Pathway Amplification in Classical Pathway Induced Terminal Complement Activation. Clin. Exp. Immunol. 2004;138:439–446. doi: 10.1111/j.1365-2249.2004.02627.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lambris JD, Ricklin D, Geisbrecht BV. Complement Evasion by Human Pathogens. Nat. Rev. Microbiol. 2008;6:132–142. doi: 10.1038/nrmicro1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laarman A, Milder F, van Strijp J, Rooijakkers S. Complement Inhibition by Gram-Positive Pathogens: Molecular Mechanisms and Therapeutic Implications. J. Mol. Med. (Berl) 2010;88:115–120. doi: 10.1007/s00109-009-0572-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zecconi A, Scali F. Staphylococcus aureus Virulence Factors in Evasion from Innate Immune Defenses in Human and Animal Diseases. Immunol. Lett. 2013;150:12–22. doi: 10.1016/j.imlet.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Garcia BL, Ramyar KX, Ricklin D, Lambris JD, Geisbrecht BV. Advances in Understanding the Structure, Function, and Mechanism of the SCIN and Efb Families of Staphylococcal Immune Evasion Proteins. Adv. Exp. Med. Biol. 2012;946:113–133. doi: 10.1007/978-1-4614-0106-3_7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rooijakkers SH, Ruyken M, Roos A, Daha MR, Presanis JS, Sim RB, van Wamel WJ, van Kessel KP, van Strijp JA. Immune Evasion by a Staphylococcal Complement Inhibitor that Acts on C3 Convertases. Nat. Immunol. 2005;6:920–927. doi: 10.1038/ni1235. [DOI] [PubMed] [Google Scholar]
- 8.Jongerius I, Köhl J, Pandey MK, Ruyken M, van Kessel KP, van Strijp JA, Rooijakkers SH. Staphylococcal Complement Evasion by Various Convertase-blocking Molecules. J. Exp. Med. 2007;204:2461–2471. doi: 10.1084/jem.20070818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geisbrecht BV, Hamaoka BY, Perman B, Zemla A, Leahy DJ. The Crystal Structures of EAP Domains from Staphylococcus aureus Reveal an Unexpected Homology to Bacterial Superantigens. J. Biol. Chem. 2005;280:17243–17250. doi: 10.1074/jbc.M412311200. [DOI] [PubMed] [Google Scholar]
- 10.Chen H, Ricklin D, Hammel M, Garcia BL, McWhorter WJ, Sfyroera G, Wu YQ, Tzekou A, Li S, Geisbrecht BV, Woods VL, Jr., Lambris JD. Allosteric Inhibition of Complement Function by a Staphylococcal Immune Evasion Protein. Proc. Natl. Acad. Sci. U.S.A. 2010;107:17621–17626. doi: 10.1073/pnas.1003750107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bouyain S, Watkins DJ. The Protein Tyrosine Phosphatases PTPRZ and PTPRG Bind to Distinct Members of the Contactin Family of Neural Recognition Molecules. Proc. Natl. Acad. Sci. U.S.A. 2010;107:2443–2448. doi: 10.1073/pnas.0911235107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geisbrecht BV, Bouyain S, Pop M. An Optimized System for the Expression and Purification of Secreted Bacterial Proteins. Prot. Expr. Purif. 2006;46:23–32. doi: 10.1016/j.pep.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Xie C, Alcaide P, Geisbrecht BV, Schneider D, Herrmann M, Preissner KT, Luscinskas FW, Chavakis T. Suppression of Experimental Autoimmune Encephalomyelitis by Extracellular Adherence Protein of Staphylococcus aureus. J. Exp. Med. 2006;203:985–994. doi: 10.1084/jem.20051681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berends ET, Dekkers JF, Nijland R, Kuipers A, Soppe JA, van Strijp JA, Rooijakkers SH. Distinct Localization of the Complement C5b-9 Complex on Gram-positive Bacteria. Cell Microbiol. 2013;15:1955–1968. doi: 10.1111/cmi.12170. [DOI] [PubMed] [Google Scholar]
- 15.Prat C, Bestebroer J, de Haas CJ, van Strijp JA, van Kessel KP. A New Staphylococcal Anti-Inflammatory Protein That Antagonizes the Formyl Peptide Receptor-Like 1. J. Immunol. 2006;177:8017–8026. doi: 10.4049/jimmunol.177.11.8017. [DOI] [PubMed] [Google Scholar]
- 16.Roos A, Bouwman LH, Munoz J, Zuiverloon T, Faber-Krol MC, Fallaux-van den Houten FC, Klar-Mohamad N, Hack CE, Tilanus MG, Daha MR. Functional Characterization of the Lectin Pathway of Complement in Human Serum. Mol. Immunol. 2003;39:655–668. doi: 10.1016/s0161-5890(02)00254-7. [DOI] [PubMed] [Google Scholar]
- 17.Stapels DAC, Ramyar KX, Bischoff M, von Koeckritz-Blickwede M, Milder FJ, Ruyken M, Eisenbeis J, McWhorter WJ, Herrmann M, van Kessel KP, Geisbrecht BV, Rooijakkers SHM. Staphylococcus aureus Secretes a Novel Class of Neutrophil-Serine-Protease Inhibitors that Promote Bacterial Infection. Proc. Natl. Acad. Sci. U.S.A. 2014;111:13187–13192. doi: 10.1073/pnas.1407616111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pang YY, Schwartz J, Thoendel M, Ackermann LW, Horswill AR, Nauseef WM. agr-Dependent Interactions of Staphylococcus aureus USA300 with Human Polymorphonuclear Neutrophils. J. Innate Immun. 2010;2:546–559. doi: 10.1159/000319855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu T, Porter AR, Kennedy AD, Kobayashi SD, Deleo FR. Phagocytosis and Killing of Staphylococcus aureus by Human Neutrophils. J. Innate Immun. 2014;6:639–649. doi: 10.1159/000360478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garcia BL, Summers BJ, Zhuoer L, Ramyar KX, Ricklin D, Fu Z-Q, Lambris JD, Geisbrecht BV. Diversity in the C3b Contact Residues and Tertiary Structures of the Staphylococcal Complement Inhibitor (SCIN) Protein Family. J. Biol. Chem. 2012;287:628–640. doi: 10.1074/jbc.M111.298984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ricklin D, Tzekou A, Garcia BL, Hammel M, McWhorter WJ, Sfyroera G, Wu Y-Q, Holers VM, Herbert AP, Barlow PN, Geisbrecht BV, Lambris JD. A Molecular Insight into Complement Evasion by the Staphylococcal Complement Inhibitor Protein Family. J. Immunol. 2009;183:2565–2574. doi: 10.4049/jimmunol.0901443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keightley JA, Shang L, Kinter M. Proteomic Analysis of Oxidative Stress-resistant Cells. Mol. Cell. Proteomics. 2004;3:167–175. doi: 10.1074/mcp.M300119-MCP200. [DOI] [PubMed] [Google Scholar]
- 23.Abramoff MD, Magalhaes PJ, Ram SJ. Image Processing with ImageJ. Biophotonics International. 2004;11:36–42. [Google Scholar]
- 24.Hussain M, Becker K, von Eiff C, Peters G, Herrmann M. Analogs of Eap protein Are Conserved and Prevalent in Clincal Staphylococcus aureus Isolates. Clin. Diag. Lab. Immunol. 2001;8:1271–1276. doi: 10.1128/CDLI.8.6.1271-1276.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flock M, Flock J-I. Rebinding of Extracellular Adherence Protein Eap to Staphylococcus aureus Can Occur through a Surface-Bound Neutral Phosphatase. J. Bacteriol. 2001;183:3999–4003. doi: 10.1128/JB.183.13.3999-4003.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Palma M, Haggar A, Flock J-I. Adherence of Staphylococcus aureus Is Enhanced by an Endogenous Secreted Protein with Broad Binding Activity. J. Bacteriol. 1999;181:2840–2845. doi: 10.1128/jb.181.9.2840-2845.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hammel M, Nemecek D, Keightley JA, Thomas GJ, Jr., Geisbrecht BV. The Staphylococcus aureus extracellular adherence protein (Eap) adopts an elongated but structured conformation in solution. Protein Sci. 2007;16:2605–2617. doi: 10.1110/ps.073170807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garcia BL, Summers BJ, Ramyar KX, Tzekou A, Lin Z, Ricklin D, Lambris JD, Laity JH, Geisbrecht BV. A Structurally Dynamic N-terminal Helix is a Key Functional Determinant in Staphylococcal Complement Inhibitor (SCIN) Proteins. J. Biol. Chem. 2013;288:2870–2881. doi: 10.1074/jbc.M112.426858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kerr MA, Parkes C. The Effects of Iodine and Thiol-blocking Reagents on Complement Component C2 and on the Assembly of the Classical-Pathway C3 Convertase. Biochem J. 1984;219:391–399. doi: 10.1042/bj2190391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Milder FJ, Raaijmakers HC, Vandeputte MD, Schouten A, Huizinga EG, Romijn RA, Hemrika W, Roos A, Daha MR, Gros P. Structure of Complement Component C2A: Implications for Convertase Formation and Substrate Binding. Structure. 2006;14:1587–1597. doi: 10.1016/j.str.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 31.Kerr MA. The Human Complement System: Assembly of the Classical Pathway C3 Convertase. Biochem J. 1980;189:173–181. doi: 10.1042/bj1890173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blom AM, Villoutreix BO, Dahlback B. Complement Inhibitor C4b-Binding Protein - Friend of Foe in the Innate Immune System? Mol. Immunol. 2004;40:1333–1346. doi: 10.1016/j.molimm.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 33.Garcia BL, Ramyar KX, Tzekou A, Ricklin D, McWhorter WJ, Lambris JD, Geisbrecht BV. Molecular Basis for Complement Recognition and Inhibition Determined by Crystallographic Studies of the Staphylococcal Complement Inhibitor (SCIN) Bound to C3c and C3b. J. Mol. Biol. 2010;402:17–29. doi: 10.1016/j.jmb.2010.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Papageorgiou AC, Acharya KR. Microbial superantigens: from structure to function. Trends Microbiol. 2000;369:369–375. doi: 10.1016/s0966-842x(00)01793-5. [DOI] [PubMed] [Google Scholar]
- 35.Blom AM, Hallstrom T, Riesbeck K. Complement Evasion Strategies of Pathogens - Acquisition of Inhibitors and Beyond. Mol. Immunol. 2009;46:2808–2817. doi: 10.1016/j.molimm.2009.04.025. [DOI] [PubMed] [Google Scholar]
- 36.Sharp JA, Cunnion KM. Disruption of the Alternative Pathway Convertase Occurs at the Staphylococcla Surface via the Acquisition of Factor H by Staphylococcus aureus. Mol. Immunol. 2011;48:683–690. doi: 10.1016/j.molimm.2010.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hair PS, Wagner SM, Friederich PT, Drake RR, Nyalwidhe JO, Cunnion KM. Complement Regulator C4BP Binds to Staphylococcus aureus and Decreases Opsonization. Mol. Immunol. 2012;50:253–261. doi: 10.1016/j.molimm.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 38.Chavakis T, Hussain M, Kanse SM, Peters GB, R.G., Flock J-I, Herrmann M, Preissner KT. Staphylococcus aureus extracellular adherence protein serves as anti-inflammatory factor by inhibiting the recruitment of host leukocytes. Nat. Med. 2002;8:687–693. doi: 10.1038/nm728. [DOI] [PubMed] [Google Scholar]
- 39.Lee LY, Miyamoto YJ, McIntyre BW, Hook M, McCrea KW, McDevitt D, Brown EL. The Staphylococcus aureus Map Protein is an Immunomodulator that Interferes with T Cell-Mediated Responses. J. Clin. Invest. 2002;110:1461–1471. doi: 10.1172/JCI16318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Joost I, Jacob S, Utermohlen O, Schubert U, Patti JM, Ong MF, Gross J, Justinger C, Renno JH, Preissner KT, Bischoff M, Herrmann M. Antibody Response to the Extracellular Adherence Protein (Eap) of Staphylococcus aureus in Healthy and Infected Individuals. FEMS Immunol. Med. Microbiol. 2011;62:23–31. doi: 10.1111/j.1574-695X.2011.00783.x. [DOI] [PubMed] [Google Scholar]
- 41.Amulic B, Cazalet C, Hayes GL, Metzler KD, Zychlinsky A. Neutrophil Function: From Mechanisms to Disease. Annu. Rev. Immunol. 2012;30:459–489. doi: 10.1146/annurev-immunol-020711-074942. [DOI] [PubMed] [Google Scholar]
- 42.Ricklin D, Lambris JD. Complement in Immune and Inflammatory Disorders: Therapeutic Interventions. J. Immunol. 2013;190:3839–3847. doi: 10.4049/jimmunol.1203200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ricklin D, Lambris JD. Compement in Immune and Inflammatory Disorders: Pathophysiological Mechanisms. J. Immunol. 2013;190:3831–3838. doi: 10.4049/jimmunol.1203487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ricklin D, Lambris JD. Progress and Trends in Complement Therapeutics. Adv. Exp. Med. Biol. 2013;734:1–22. doi: 10.1007/978-1-4614-4118-2_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hammel M, Sfyroera G, Ricklin D, Magotti P, Lambris JD, Geisbrecht BV. A Structural Basis for Complement Inhibition by Staphylococcus aureus. Nat. Immunol. 2007;8:430–437. doi: 10.1038/ni1450. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.