Abstract
Laparoscopic surgery has become well established in the management of both and malignant colorectal disease. The last decade has seen increasing numbers of surgeons trained to a high standard in minimally-invasive surgery. However there has not been the same enthusiasm for the use of laparoscopy in emergency colorectal surgery. There is a perception that emergent surgery is technically more difficult and may lead to worse outcomes. The present review aims to provide a comprehensive and critical appraisal of the available literature on the use of laparoscopic colorectal surgery (LCS) in the emergency setting. The literature is broadly divided by the underlying pathology; that is, inflammatory bowel disease, diverticulitis and malignant obstruction. There were no randomized trials and the majority of the studies were case-matched series or comparative studies. The overall trend was that LCS is associated with shorter hospital stay, par or fewer complications but an increased operating time.Emergency LCS can be safely undertaken for both benign and malignant disease providing there is appropriate patient selection, the surgeon is adequately experienced and there are sufficient resources to allow for a potentially more complex operation.
Keywords: Laparoscopic surgery, Colorectal disease, Colorectal cancer, Inflammatory bowel disease, Emergency surgery
Core tip: Laparoscopic surgery is increasingly used in the emergency setting. This has been perceived to be a challenging surgical approach for such cases. However with appropriate expertise and training, laparoscopy can be used for colorectal emergencies with good short- and medium term outcomes.
INTRODUCTION
Laparoscopic surgery has become a well-established part of elective gastrointestinal operative practice. The last decade has witnessed the evidence-based validation of laparoscopic colorectal surgery (LCS) for both benign and malignant disease, with indisputable advantages including shorter hospital stay, faster recovery, and less morbidity[1-3]. Increasingly, patients with uncomplicated colorectal disease are routinely offered laparoscopic surgery, and in many centres this is now the default position for elective cases, with national guidance recommending laparoscopic surgery performed by appropriately trained colorectal surgeons for patients with colorectal cancer[4].
Nonetheless, while LCS is universally regarded as appropriate in suitably selected elective cases, its role in emergent colorectal pathology remains uncertain[5]. Despite advances in technology and a more structured approach to training, which has allowed for a greater number of surgeons to become competent in laparoscopy, there is a perception that laparoscopic surgery should remain in the elective setting. At the present time, the most common use of laparoscopy in emergency surgery is for appendicectomy or the diagnosis of non-resolving, uncomplicated, right iliac fossa pain. Although some institutions routinely perform emergency laparoscopic cholecystectomies, repair of perforated peptic ulcers, and assessment of penetrating abdominal trauma by laparoscopic approaches, laparoscopy in colorectal emergencies is uncommonly performed.
In theory, emergency LCS is likely to be more challenging for several reasons. The procedures are technically more complex with significantly greater distortion to normal anatomy from infective or inflammatory processes. Indeed, the finding of dilated and vulnerable bowel in colonic obstruction was often considered a contraindication for minimally invasive surgery in the past[6]. Furthermore, the patient cohort is more likely to be physiologically compromised due to the presence of acute pathology. Laparoscopic colonic resections typically take more time, and in the setting of a high-risk patient profile, a swift open approach may lead to better outcomes. Yet the established advantages of elective laparoscopic colorectal surgery in reducing post-operative pain, the stress response to surgery, wound complications, respiratory complications, in-patient hospital stay, short term health-related quality of life, and health care costs[1,2,7-13], support the notion that emergency laparoscopic surgery may lead to similar benefits if performed by experienced laparoscopic surgeons in appropriately selected patients. For example, in a study comparing 42 patients undergoing emergency laparoscopic colonic resections vs 25 patients undergoing open emergency colon resections, observed benefits included a shorter hospital stay, less blood loss, reduced duration of ileus and intensive care unit stay, with equivalent mortality[14]. Ballian et al[15] evaluated the role of laparoscopy for emergent restorative colectomy using the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database and found that although less than 10% of patients that underwent emergency colon resection with primary anastomosis, they had at minimum comparable rates of morbidity and mortality but decreased total and post-operative length of stay.
These findings suggest that some of the documented advantages of laparoscopic surgery may be translatable to the emergency arena. Given the large volumes of patients who undergo emergency surgery for colorectal pathology, determining the precise role of LCS in this setting is of significant clinical importance. However a recent study comparing laparoscopic and open surgery for the emergency treatment of diverticulitis reported no decrease in morbidity or mortality and no overall benefit over open surgery[16]. As there is still some conflicting evidence, the present review aims to provide a comprehensive and critical appraisal of the available literature on the use of LCS in the emergency setting. We describe the role of laparoscopy in the emergency treatment of benign and malignant colorectal disease.
LITERATURE SEARCH
Identification of studies
An electronic search was carried out using MEDLINE (1965-2013), EMBASE (1980-2013), CINAHL (1982-2013) and the Cochrane library databases. The following medical subject heading (MeSH) terms and keywords were used: “emergency”; “laparoscopic”; and “colorectal”. The “related articles” function was used to broaden the search and all abstracts, studies, and citations retrieved were scanned for subject relevance. The latest date of this search was 1st June 2013. Complete articles of all potentially relevant manuscripts were retrieved and evaluated for inclusion. Additional references from the collective libraries of the senior authors were identified. Reference lists of all relevant publications were hand-searched for additional studies missed by this search strategy, and cross referencing continued until no further relevant publications were identified.
Study inclusion criteria and data extraction
Study methodology was carried out in accordance with the “Preferred Reporting for Systematic Reviews and Meta-Analyses” (PRISMA) recommendations for improving the standard of systematic reviews[17]. Studies that met the following pre-defined criteria were included in the review process: (1) language: English language publications were included; (2) patient population: Studies had to report outcomes on the use of LCS in the emergency setting. Adult patients over the age of 18 were included. Where multiple studies describing the same patient population were identified, the most recent publication was used unless additional information was imparted by earlier work. Case reports were excluded. Studies describing partial right colonic mobilization as part of an appendicectomy were excluded. Studies evaluating the use of Single Incision Laproscopic Surgery and robot-assisted surgery were excluded; and (3) outcome measures: Studies were only included if they reported outcome information including post-operative morbidity and mortality in addition to length of stay. Series describing the use of a technique alone in the absence of outcome data were excluded. The search strategy is shown in Figure 1.
Figure 1.
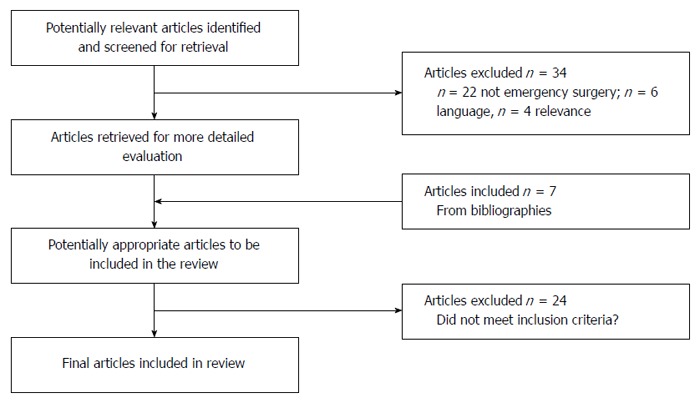
Flowchart of search strategy.
LITERATURE SEARCH AND DESCRIPTION OF STUDIES
The outlined search strategy identified 98 publications of potential relevance. Following screening of titles and abstracts, 34 studies were excluded (22 articles were not related to emergency surgery, 6 articles were not in English, 4 articles were not considered relevant to the scope of this article, 2 articles were not related to colorectal surgery) leaving 64 articles that were retrieved in full text. A further 7 articles were identified from a bibliographic search of these articles, providing a total of 71 articles for evaluation. Of these 24 did not meet the inclusion criteria, and were withdrawn from evaluation, leaving a total of 47 studies published between 1965 and 2013 that were entered into the review process. For ease of description, results are presented separately for benign and malignant pathology.
EMERGENCY LCS FOR BENIGN DISEASE
Inflammatory bowel disease
Laparoscopic surgery has been shown to be a safe alternative to open surgery in the elective surgical management for Ulcerative Colitis and Crohn’s disease of the colon. It is associated with faster recovery of bowel function, shorter time to oral intake and reduced hospital stay although may lead to increased operating times[18-23]. However in the emergency setting, the advantages are not so apparent and there is a paucity of data on long-term outcomes. 10 studies, of which 8 were comparative, reported on 286 cases of LCS in the emergency setting. The majority of reports undertaken are case-matched studies with fewer than 40 laparoscopic cases in the analyses[6,14,24-31]. Overall, the general trend is one of shorter hospital stay and increased operating time but morbidity which is either on par or better than open surgery. Table 1 shows the details of the studies and the main reported outcomes.
Table 1.
Table of studies involving emergent laparoscopic colorectal surgery and inflammatory bowel disease
| Ref. | Type of study | Number of LCS patients | Institution | Main outcome |
| Nash et al[27] | Comparative | 36 | Single | No difference in morbidity; |
| Longer operating time in LCS; | ||||
| Shorter hospital stay | ||||
| Stulberg et al[14] | Comparative | 42 | Single-centre | Less blood loss, shorter stay, less morbidity |
| Marceau et al[26] | Comparative | 40 | Single-centre | Similar operating time; |
| Hospital stay similar; | ||||
| Morbidity similar | ||||
| Fowkes et al[21] | Comparative | 22 | Single centre | Shorter hospital stay; |
| Similar morbidity | ||||
| Seshadri et al[28] | Comparative | 37 | Single-centre | Longer operating time in LCS; |
| No differences in complications; | ||||
| Less post-op morbidity; | ||||
| Shorter hospital stay | ||||
| Watanabe et al[29] | Comparative | 30 | Single-centre | Longer operating time in LCS; |
| Fewer post-op complications in LCS; | ||||
| Faster gut recovery in LCS | ||||
| Qazi et al[24] | Comparative | 17 | Single-centre | Increased complications in LCS; |
| Conversion rate of 32% | ||||
| Marcello et al[6] | Comparative | 16 | Single-centre | Early oral intake in LCS; |
| No difference in morbidity | ||||
| Ouaïssi et al[25] | Single cohort | 18 | Single-centre | Safe; feasible; |
| Morbidity 33% | ||||
| Bell and Seymour[31] | Single cohort | 18 | Single-centre | High morbidity; |
| Shorter hospital stay |
LCS: Laparoscopic colorectal surgery.
Nash et al[27] compared the peri-operative outcomes of 32 patients who underwent laparoscopic surgery with 36 patients that had open surgery for acute colitis. The majority of patients in the laparoscopic group had toxic colitis (n = 22) whereas in the open group there were more patients with obstruction and perforation, limiting direct comparisons. They found no difference in morbidity but longer operating times in the laparoscopic cases (mean difference of 59 min). Similar findings were also noted by Watanabe et al[29] in a comparison of 30 patients undergoing laparoscopic surgery and 30 patients having an open procedure. In addition, they reported a shortened recovery time for gut function (4.8 d in the laparoscopic group vs 5.9 d in the open group) - although in this series, the laparoscopic group comprised of a hand-assisted procedure. Earlier oral intake was a benefit also seen by Marcello et al[6] in their case-matched study of acute colitic patients.. Whilst most reports found complication rates and morbidity to be similar between open and laparoscopic surgery, Seshadri et al[28] found fewer peri-operative complications in the laparoscopic group (9 patients in LCS vs 24 in open group), in their series of 37 patients despite longer operating times (270 min vs 178 min). The perceived increased risk of peri-operative complications in patients that are often immunocompromised from steroids or immunosuppressants is similar in open surgery and only Qazi et al[24] and Bell et al[31] showed significant operation-related morbidity (up to 35%). However both these reports did not include a case-matched open group.
Acute diverticulitis
Acute diverticulitis poses a significant challenge even in open surgery due to the variable degrees of inflammation, and distortion of anatomical planes. However, the surgical management of diverticulitis has evolved in recent years and there has been a shift away from traditional Hartmann’s operation to percutaneous and laparoscopic drainage procedures[32]. There is accumulating evidence, albeit from case series and cohort observational studies, that laparoscopic lavage and drainage is not only a safe and efficient method of treating non-feculent complicated diverticulitis but does not always necessitate a future elective colonic resection[33-35].
All but one study had less than 40 patients - Table 2[36-42]. Complication rate/morbidity ranges from 0%-54% with mortality of < 3%. Only 3 studies had patients which required conversion to open operation[43-45]. The majority of patients included in these studies had advanced complicated disease as measured by the Hinchey classification (Hinchey Grade III or more)[46]. The rate of stoma formation was low; only Mutter et al[40] and Taylor et al[47] reported the need for stoma in 2 of 14 and 1 of 10 patients, respectively. The largest series was reported by Myers et al[38] of 100 patients. 92 patients underwent laparoscopic lavage with 8 requiring conversion to open Hartmann’s operation. 87 patients had complete resolution of acute disease however one patient also required a delayed Hartmann’s operation and a further patient undergoing percutaneous drainage under image guidance. There is 3% reported mortality in this series although this was not directly attributed to the surgical approach.
Table 2.
Studies involving the role of laparoscopic lavage in diverticular disease
| Ref. | No. of patients | LOS (d) | Morbidity | Mortality | Further resection |
| Lam et al[36] | 6 | 11 | 33% | 0% | 50% |
| O’Sullivan et al[45] | 8 | 10 | 25% | 0% | 0% |
| Myers et al[38] | 100 | 8 | 5% | 3% | 0% |
| Bretagnol et al[39] | 24 | 12 | 8% | 0% | 100% |
| Karoui et al[43] | 35 | 8 | 28% | 0% | 71% |
| White et al[44] | 35 | 14 | 12% | 0% | 64% |
| Da Rold et al[37] | 7 | 8 | 28% | 0% | 0% |
| Favuzza et al[42] | 7 | 6 | 14% | 0% | 57% |
| Mutter et al[40] | 10 | 9 | 0% | 0% | 67% |
| Franklin et al[41] | 40 | 3 | 20% | 0% | 60% |
LOS: Length of stay.
Although laparoscopic resection is routinely practiced with for patients requiring surgery due to previous episodes of recurrent diverticulitis in an elective setting[48-50], there is scarce data in the emergent setting. Five retrospective studies have reported on laparoscopic resection in acute diverticulitis including fewer complications, no deaths and more than 90% stoma reversal rates[51-55]. For example, Titu et al[54] included 66 patients who underwent emergency laparoscopic surgery for complicated diverticulitis. These authors reported only one conversion to laparotomy and a median operating time of 110 min. They performed a majority of anterior resections in patients who were mostly classified with Hinchey grade I or II (56 of 66 patients).
A large scale analysis by Rea et al[56] of network data in the US examined the emerging role of laparoscopic resections in acute diverticulitis using the National Inpatient Sample (NIS) database. Laparoscopic surgery was performed in 2664 patients in 4 years. There was no difference in mortality or morbidity although the conversion rate was 55%. Multivariate analysis showed laparoscopic approach to be a predictor of routine discharge - OR = 1.31; and a decreased length of stay - (-).78. However cost analysis revealed no overall savings in financial terms.
EMERGENCY LCS FOR MALIGNANT DISEASE
Emergency laparoscopic right colectomy
The highest quality studies in this section were comparative studies. In a small scale retrospective study, Ng et al[57] noted favourable short-term clinical outcomes and an acceptable lymph node yield when they studied seven consecutive patients. However these are retrospective results and a prospective randomized controlled trial will be needed to strengthen the evidence in favour of emergency laparoscopic surgery in obstructed patients. A further study by Ng et al[58] compared 43 consecutive patients with right-sided obstruction from colonic cancer and found less morbidity and faster recovery in the laparoscopic group in addition to the intra-operative benefit of reduced blood loss. Operating time was longer in the laparoscopic group. Li et al[59] compared emergency and elective laparoscopically-assisted right hemi-colectomy in 181 patients and found no difference in intra- and post-operative complications although procedure time was significantly longer in the 33 patients in the laparoscopic group.
Emergency laparoscopic surgery for left colonic obstruction
The traditional approach to left-sided colonic obstruction has been a Hartmann’s operation with the formation of an end-colostomy although in some cases primary anastomosis with or without a defunctioning stoma can be performed. However, the endo-laparoscopic approach consisting of endoscopic stenting followed by planned laparoscopic resection has become an important alternative to immediate open emergency surgery[60,61]. Endoluminal stenting can be a valuable “bridge” to elective surgery as a more definitive procedure. Stipa et al[60] investigated the effectiveness of colonic stenting to determine whether it could be used in advance of a single-stage operation. Of the 31 patients managed with stenting, 6 underwent subsequent laparoscopic resection and 16 had an open colectomy. The laparoscopic group had no associated morbidity and shorter hospital stay. In a further study, colonic stenting as a bridge to elective laparoscopic surgery has shown to be more cost-effective and reduces the need for a stoma by 83%[62]. The Colorectal Stent Trial (CReST) is a multi-centre phase III, randomized controlled trial, currently investigating the role of endoluminal stenting in the acute management of obstructing colorectal cancer[63]. The future results would be interesting regarding association with subsequent laparoscopic surgery.
Emergency colonic surgery in iatrogenic perforations during colonoscopy
In this group of patients, the lower peritoneal contamination as a consequence of bowel preparation can often result in less peritonitis and a conservative approach with antibiotics may be successful. For those who require surgery, less contamination not only provides a more suitable environment for laparoscopy but also generally results in a better outcome as the patient is less systemically unwell. The options include a laparoscopic lavage and insertion of drains with or without a defunctioning stoma, or a segmental resection with or without primary anastomosis. If a perforation occurs at a tumour site, the management options must be considered in light of the potential upstaging of disease to that of T4 status. In a study of 11 patients with iatrogenic perforation operated on laparoscopically compared to 7 patients operated by open surgery[64], results favoured the laparoscopic group in terms of less morbidity and less hospital stay. Further, none of the 11 patients who underwent laparoscopic treatment required colonic resection.
DISCUSSION
As laparoscopy has become a more accepted practice for colorectal surgeons, there has been a natural interest in the use of laparoscopy in emergency settings. The literature is broadly divided by the underlying pathology; that is, inflammatory bowel disease (IBD), diverticulitis and malignant obstruction. Interestingly, despite the technical difficulties that inflammation causes in terms of disruption of tissue planes, there are a greater number of reports regarding the role of laparoscopy in IBD rather than cancer.
There are no randomized trials in the IBD setting but the trend is that of shorter time to gut function which is important in nutritionally deplete patients. As many patients are on steroids, there are issues with wound healing and post-operative complications however the majority of studies have reported improved morbidity. A shorter hospital stay is associated with most laparoscopic operations and this is also the case with colitic patients. Operating times were increased but this may be expected with technically more challenging operations. As briefly mentioned, the inflammatory process makes the surgical anatomy more challenging and although laparoscopy gives enviable views at high magnification, there is not the same tactile feedback one gets during open surgery. This is most applicable in the cases of inflammation when the surgeon must be confident they are in the correct plane. This is a possible reason behind the increased operating time. Furthermore, whilst there are standard port positions due to the relatively consistent nature of cancer surgery, there may have to be more flexibility with IBD.
The reports on diverticulitis concentrate on lavage and drainage and no resection. However it is important to note that for many patients, this can be a definitive procedure. There is not sufficient medium or long-term data to know whether laparoscopic lavage will reduce the need for an elective resection in the future but in the short term the results do seem promising. There is a paucity of literature regarding emergent colonic resection for diverticular disease but those which have reported have shown equivocal results to open surgery whether this be primary anastomosis or Hartmann’s procedure. The contrast with IBD surgery is that there is no universal consensus on treatment for the surgical options in acute diverticulitis. A Hartmann’s procedure, primary anastomosis or lavage and drainage may all be suitable for specific cases and it is the judgment of the surgeon which is key.
Emergency cancer surgery is commonly associated with obstruction or perforation of the tumour. This has an impact on the oncological outcome of the disease whereby systemic control is important and surgery to the primary may only be part of the overall treatment. Most reports favour a combined approach with endoscopy for stenting but reports are emerging of resectional cases. Our single-centre study has analyzed short and long term outcomes for colonic cancer patients undergoing laparoscopy and open surgery. We found that laparoscopic resections of colon cancers presenting as emergency were not only feasible and safe, but also provided long- and short-term outcomes similar to open surgery[65].
With rapidly advancing technology and a greater number of trained surgeons, use of laparoscopy is emerging as the gold standard in the elective setting. More recently, surgeons are now attempting to take on the challenge of more complex interventions including emergency laparoscopic colorectal surgery. Selection of an appropriate case is important especially in the early part of the learning curve. In addition to increase technical ability of surgeon, improvement and availability of suitably trained theatre staff is also required to achieve better results. Barriers to adopting a minimally-invasive approach for colonic emergencies include surgeon-, patient- and resource-factors. The surgeon must be appropriately experienced and confident to recognize the potential pitfalls which may occur. Early conversion is preferable where technical problems are anticipated. In some cases, patients are not suitable to undergo pneumoperitoneum due to cardiopulmonary compromise or from previous procedures, although the latter is not an absolute contraindication. Finally, a significant proportion of the cases are undertaken outside normal working hours and there may not be adequate resources available - for example, some institutions lack sufficient time on their emergency theatre schedule to allow a potentially lengthy laparoscopic emergency operation.
LIMITATIONS
The present review is limited by the heterogeneity of the studies. This lack of universal definitions to key features of the study is the main limitation. The search strategy focused on studies either reporting on or comparing laparoscopic emergency surgery to open surgery. Laparoscopy or laparoscopic surgery is not defined in the all the studies included in the review. Some surgeons accept laparoscopically assisted or hand-assisted procedures to be included under the term laparoscopy, however this makes comparison difficult. The term “straight laparoscopy” is occasionally used to denote procedures in which only laparoscopic instruments were used and an open incision made to retrieve the specimen. A further term which was not universally defined was “conversion”. Other limitations included description of the surgeons’ experience and that of the institution. This has a bearing on the outcomes as we have mentioned the learning curve which is central to successful laparoscopic surgery.
CONCLUSION
There is comparatively little outcomes data for the medium and long-term to fully evaluate the role of laparoscopy in the emergency setting. Clearly, in selected patients there will be benefit and possibly cost-savings as well from shorter hospital stay and fewer complications. However, the heterogeneity of the studies causes difficulty in making direct comparison. There appears to be favourable short-term outcomes but sufficient equipoise to consider a randomized trial in the future.
Footnotes
P- Reviewer: Angriman I, Campos FG S- Editor: Ma YJ L- Editor: A E- Editor: Wang CH
References
- 1.Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224–2229. doi: 10.1016/S0140-6736(02)09290-5. [DOI] [PubMed] [Google Scholar]
- 2.Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718–1726. doi: 10.1016/S0140-6736(05)66545-2. [DOI] [PubMed] [Google Scholar]
- 3.Tjandra JJ, Chan MK. Systematic review on the short-term outcome of laparoscopic resection for colon and rectosigmoid cancer. Colorectal Dis. 2006;8:375–388. doi: 10.1111/j.1463-1318.2006.00974.x. [DOI] [PubMed] [Google Scholar]
- 4.Excellence NIfHaC. Laparoscopic surgery for colorectal cancer - TA105. London: National Institute for Health and Care Excellence; 2009. Available from: http://www.nice.org.uk/guidance/TA105. [Google Scholar]
- 5.Newman CM, Arnold SJ, Coull DB, Linn TY, Moran BJ, Gudgeon AM, Cecil TD. The majority of colorectal resections require an open approach, even in units with a special interest in laparoscopic surgery. Colorectal Dis. 2012;14:29–34; discussion 42-43. doi: 10.1111/j.1463-1318.2010.02504.x. [DOI] [PubMed] [Google Scholar]
- 6.Marcello PW, Milsom JW, Wong SK, Brady K, Goormastic M, Fazio VW. Laparoscopic total colectomy for acute colitis: a case-control study. Dis Colon Rectum. 2001;44:1441–1445. doi: 10.1007/BF02234595. [DOI] [PubMed] [Google Scholar]
- 7.Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, Gerhards MF, van Wagensveld BA, van der Zaag ES, van Geloven AA, et al. Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study) Ann Surg. 2011;254:868–875. doi: 10.1097/SLA.0b013e31821fd1ce. [DOI] [PubMed] [Google Scholar]
- 8.Li MZ, Xiao LB, Wu WH, Yang SB, Li SZ. Meta-analysis of laparoscopic versus open colorectal surgery within fast-track perioperative care. Dis Colon Rectum. 2012;55:821–827. doi: 10.1097/DCR.0b013e31824bd31e. [DOI] [PubMed] [Google Scholar]
- 9.Lourenco T, Murray A, Grant A, McKinley A, Krukowski Z, Vale L. Laparoscopic surgery for colorectal cancer: safe and effective? - A systematic review. Surg Endosc. 2008;22:1146–1160. doi: 10.1007/s00464-007-9686-x. [DOI] [PubMed] [Google Scholar]
- 10.Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, Krukowski Z, Vale L, Grant A. Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation. Health Technol Assess. 2006;10:1–141, iii-iv. doi: 10.3310/hta10450. [DOI] [PubMed] [Google Scholar]
- 11.Vaid S, Tucker J, Bell T, Grim R, Ahuja V. Cost analysis of laparoscopic versus open colectomy in patients with colon cancer: results from a large nationwide population database. Am Surg. 2012;78:635–641. [PubMed] [Google Scholar]
- 12.Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050–2059. doi: 10.1056/NEJMoa032651. [DOI] [PubMed] [Google Scholar]
- 13.COLOR Study Group. COLOR: a randomized clinical trial comparing laparoscopic and open resection for colon cancer. Dig Surg. 2000;17:617–622. doi: 10.1159/000051971. [DOI] [PubMed] [Google Scholar]
- 14.Stulberg JJ, Champagne BJ, Fan Z, Horan M, Obias V, Marderstein E, Reynolds H, Delaney CP. Emergency laparoscopic colectomy: does it measure up to open? Am J Surg. 2009;197:296–301. doi: 10.1016/j.amjsurg.2008.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ballian N, Weisensel N, Rajamanickam V, Foley EF, Heise CP, Harms BA, Kennedy GD. Comparable postoperative morbidity and mortality after laparoscopic and open emergent restorative colectomy: outcomes from the ACS NSQIP. World J Surg. 2012;36:2488–2496. doi: 10.1007/s00268-012-1694-x. [DOI] [PubMed] [Google Scholar]
- 16.Turley RS, Barbas AS, Lidsky ME, Mantyh CR, Migaly J, Scarborough JE. Laparoscopic versus open Hartmann procedure for the emergency treatment of diverticulitis: a propensity-matched analysis. Dis Colon Rectum. 2013;56:72–82. doi: 10.1097/DCR.0b013e3182749cf5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 18.Tan JJ, Tjandra JJ. Laparoscopic surgery for ulcerative colitis - a meta-analysis. Colorectal Dis. 2006;8:626–636. doi: 10.1111/j.1463-1318.2006.00971.x. [DOI] [PubMed] [Google Scholar]
- 19.Metcalf AM. Elective and emergent operative management of ulcerative colitis. Surg Clin North Am. 2007;87:633–641. doi: 10.1016/j.suc.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 20.Wu XJ, He XS, Zhou XY, Ke J, Lan P. The role of laparoscopic surgery for ulcerative colitis: systematic review with meta-analysis. Int J Colorectal Dis. 2010;25:949–957. doi: 10.1007/s00384-010-0898-5. [DOI] [PubMed] [Google Scholar]
- 21.Fowkes L, Krishna K, Menon A, Greenslade GL, Dixon AR. Laparoscopic emergency and elective surgery for ulcerative colitis. Colorectal Dis. 2008;10:373–378. doi: 10.1111/j.1463-1318.2007.01321.x. [DOI] [PubMed] [Google Scholar]
- 22.Stocchi L. Laparoscopic surgery for ulcerative colitis. Clin Colon Rectal Surg. 2010;23:248–258. doi: 10.1055/s-0030-1268251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maggiori L, Panis Y. Laparoscopic approach for inflammatory bowel disease surgical managment. Acta Chir Iugosl. 2012;59:75–79. doi: 10.2298/aci1202075m. [DOI] [PubMed] [Google Scholar]
- 24.Qazi SM, Skovdal J, Munck LK, Bisgaard T. High morbidity after laparoscopic emergency colectomy for inflammatory bowel disease. Dan Med Bull. 2011;58:A4326. [PubMed] [Google Scholar]
- 25.Ouaïssi M, Alves A, Bouhnik Y, Valleur P, Panis Y. Three-step ileal pouch-anal anastomosis under total laparoscopic approach for acute or severe colitis complicating inflammatory bowel disease. J Am Coll Surg. 2006;202:637–642. doi: 10.1016/j.jamcollsurg.2005.12.016. [DOI] [PubMed] [Google Scholar]
- 26.Marceau C, Alves A, Ouaissi M, Bouhnik Y, Valleur P, Panis Y. Laparoscopic subtotal colectomy for acute or severe colitis complicating inflammatory bowel disease: a case-matched study in 88 patients. Surgery. 2007;141:640–644. doi: 10.1016/j.surg.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 27.Nash GM, Bleier J, Milsom JW, Trencheva K, Sonoda T, Lee SW. Minimally invasive surgery is safe and effective for urgent and emergent colectomy. Colorectal Dis. 2010;12:480–484. doi: 10.1111/j.1463-1318.2009.01843.x. [DOI] [PubMed] [Google Scholar]
- 28.Seshadri PA, Poulin EC, Schlachta CM, Cadeddu MO, Mamazza J. Does a laparoscopic approach to total abdominal colectomy and proctocolectomy offer advantages? Surg Endosc. 2001;15:837–842. doi: 10.1007/s004640000356. [DOI] [PubMed] [Google Scholar]
- 29.Watanabe K, Funayama Y, Fukushima K, Shibata C, Takahashi K, Sasaki I. Hand-assisted laparoscopic vs. open subtotal colectomy for severe ulcerative colitis. Dis Colon Rectum. 2009;52:640–645. doi: 10.1007/DCR.0b013e31819d47b5. [DOI] [PubMed] [Google Scholar]
- 30.Dunker MS, Bemelman WA, Slors JF, van Hogezand RA, Ringers J, Gouma DJ. Laparoscopic-assisted vs open colectomy for severe acute colitis in patients with inflammatory bowel disease (IBD): a retrospective study in 42 patients. Surg Endosc. 2000;14:911–914. doi: 10.1007/s004640000262. [DOI] [PubMed] [Google Scholar]
- 31.Bell RL, Seymour NE. Laparoscopic treatment of fulminant ulcerative colitis. Surg Endosc. 2002;16:1778–1782. doi: 10.1007/s00464-001-8300-x. [DOI] [PubMed] [Google Scholar]
- 32.Gaertner WB, Kwaan MR, Madoff RD, Willis D, Belzer GE, Rothenberger DA, Melton GB. The evolving role of laparoscopy in colonic diverticular disease: a systematic review. World J Surg. 2013;37:629–638. doi: 10.1007/s00268-012-1872-x. [DOI] [PubMed] [Google Scholar]
- 33.Afshar S, Kurer MA. Laparoscopic peritoneal lavage for perforated sigmoid diverticulitis. Colorectal Dis. 2012;14:135–142. doi: 10.1111/j.1463-1318.2011.02606.x. [DOI] [PubMed] [Google Scholar]
- 34.Alamili M, Gögenur I, Rosenberg J. Acute complicated diverticulitis managed by laparoscopic lavage. Dis Colon Rectum. 2009;52:1345–1349. doi: 10.1007/DCR.0b013e3181a0da34. [DOI] [PubMed] [Google Scholar]
- 35.Toorenvliet BR, Swank H, Schoones JW, Hamming JF, Bemelman WA. Laparoscopic peritoneal lavage for perforated colonic diverticulitis: a systematic review. Colorectal Dis. 2010;12:862–867. doi: 10.1111/j.1463-1318.2009.02052.x. [DOI] [PubMed] [Google Scholar]
- 36.Lam HD, Tinton N, Cambier E, Navez B. Laparoscopic treatment in acute complicated diverticulitis: a review of 11 cases. Acta Chir Belg. 2009;109:56–60. doi: 10.1080/00015458.2009.11680372. [DOI] [PubMed] [Google Scholar]
- 37.Da Rold AR, Guerriero S, Fiamingo P, Pariset S, Veroux M, Pilon F, Tosato S, Ruffolo C, Tedeschi U. Laparoscopic colorrhaphy, irrigation and drainage in the treatment of complicated acute diverticulitis: initial experience. Chir Ital. 2004;56:95–98. [PubMed] [Google Scholar]
- 38.Myers E, Hurley M, O’Sullivan GC, Kavanagh D, Wilson I, Winter DC. Laparoscopic peritoneal lavage for generalized peritonitis due to perforated diverticulitis. Br J Surg. 2008;95:97–101. doi: 10.1002/bjs.6024. [DOI] [PubMed] [Google Scholar]
- 39.Bretagnol F, Pautrat K, Mor C, Benchellal Z, Huten N, de Calan L. Emergency laparoscopic management of perforated sigmoid diverticulitis: a promising alternative to more radical procedures. J Am Coll Surg. 2008;206:654–657. doi: 10.1016/j.jamcollsurg.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 40.Mutter D, Bouras G, Forgione A, Vix M, Leroy J, Marescaux J. Two-stage totally minimally invasive approach for acute complicated diverticulitis. Colorectal Dis. 2006;8:501–505. doi: 10.1111/j.1463-1318.2006.01011.x. [DOI] [PubMed] [Google Scholar]
- 41.Franklin ME, Portillo G, Treviño JM, Gonzalez JJ, Glass JL. Long-term experience with the laparoscopic approach to perforated diverticulitis plus generalized peritonitis. World J Surg. 2008;32:1507–1511. doi: 10.1007/s00268-007-9463-y. [DOI] [PubMed] [Google Scholar]
- 42.Favuzza J, Friel JC, Kelly JJ, Perugini R, Counihan TC. Benefits of laparoscopic peritoneal lavage for complicated sigmoid diverticulitis. Int J Colorectal Dis. 2009;24:797–801. doi: 10.1007/s00384-009-0641-2. [DOI] [PubMed] [Google Scholar]
- 43.Karoui M, Champault A, Pautrat K, Valleur P, Cherqui D, Champault G. Laparoscopic peritoneal lavage or primary anastomosis with defunctioning stoma for Hinchey 3 complicated diverticulitis: results of a comparative study. Dis Colon Rectum. 2009;52:609–615. doi: 10.1007/DCR.0b013e3181a0a674. [DOI] [PubMed] [Google Scholar]
- 44.White SI, Frenkiel B, Martin PJ. A ten-year audit of perforated sigmoid diverticulitis: highlighting the outcomes of laparoscopic lavage. Dis Colon Rectum. 2010;53:1537–1541. doi: 10.1007/DCR.0b013e3181f2ee2a. [DOI] [PubMed] [Google Scholar]
- 45.O’Sullivan GC, Murphy D, O’Brien MG, Ireland A. Laparoscopic management of generalized peritonitis due to perforated colonic diverticula. Am J Surg. 1996;171:432–434. doi: 10.1016/S0002-9610(97)89625-0. [DOI] [PubMed] [Google Scholar]
- 46.Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85–109. [PubMed] [Google Scholar]
- 47.Taylor CJ, Layani L, Ghusn MA, White SI. Perforated diverticulitis managed by laparoscopic lavage. ANZ J Surg. 2006;76:962–965. doi: 10.1111/j.1445-2197.2006.03908.x. [DOI] [PubMed] [Google Scholar]
- 48.Mbadiwe T, Obirieze AC, Cornwell EE, Turner P, Fullum TM. Surgical management of complicated diverticulitis: a comparison of the laparoscopic and open approaches. J Am Coll Surg. 2013;216:782–788; discussion 788-790. doi: 10.1016/j.jamcollsurg.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 49.Siddiqui MR, Sajid MS, Khatri K, Cheek E, Baig MK. Elective open versus laparoscopic sigmoid colectomy for diverticular disease: a meta-analysis with the Sigma trial. World J Surg. 2010;34:2883–2901. doi: 10.1007/s00268-010-0762-3. [DOI] [PubMed] [Google Scholar]
- 50.Siddiqui MR, Sajid MS, Qureshi S, Cheek E, Baig MK. Elective laparoscopic sigmoid resection for diverticular disease has fewer complications than conventional surgery: a meta-analysis. Am J Surg. 2010;200:144–161. doi: 10.1016/j.amjsurg.2009.08.021. [DOI] [PubMed] [Google Scholar]
- 51.Chouillard E, Maggiori L, Ata T, Jarbaoui S, Rivkine E, Benhaim L, Ghiles E, Etienne JC, Fingerhut A. Laparoscopic two-stage left colonic resection for patients with peritonitis caused by acute diverticulitis. Dis Colon Rectum. 2007;50:1157–1163. doi: 10.1007/s10350-006-0851-4. [DOI] [PubMed] [Google Scholar]
- 52.Agaba EA, Zaidi RM, Ramzy P, Aftab M, Rubach E, Gecelter G, Ravikumar TS, DeNoto G. Laparoscopic Hartmann’s procedure: a viable option for treatment of acutely perforated diverticultis. Surg Endosc. 2009;23:1483–1486. doi: 10.1007/s00464-009-0380-z. [DOI] [PubMed] [Google Scholar]
- 53.Fine AP. Laparoscopic surgery for inflammatory complications of acute sigmoid diverticulitis. JSLS. 2001;5:233–235. [PMC free article] [PubMed] [Google Scholar]
- 54.Titu LV, Zafar N, Phillips SM, Greenslade GL, Dixon AR. Emergency laparoscopic surgery for complicated diverticular disease. Colorectal Dis. 2009;11:401–404. doi: 10.1111/j.1463-1318.2008.01606.x. [DOI] [PubMed] [Google Scholar]
- 55.Zdichavsky M, Königsrainer A, Granderath FA. Laparoscopic rectosigmoid resection for acute sigmoid diverticulitis. J Gastrointest Surg. 2009;13:804–805. doi: 10.1007/s11605-008-0675-8. [DOI] [PubMed] [Google Scholar]
- 56.Rea JD, Herzig DO, Diggs BS, Cone MM, Lu KC. Use and outcomes of emergent laparoscopic resection for acute diverticulitis. Am J Surg. 2012;203:639–643. doi: 10.1016/j.amjsurg.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 57.Ng SS, Yiu RY, Li JC, Lee JF, Leung KL. Emergency laparoscopically assisted right hemicolectomy for obstructing right-sided colon carcinoma. J Laparoendosc Adv Surg Tech A. 2006;16:350–354. doi: 10.1089/lap.2006.16.350. [DOI] [PubMed] [Google Scholar]
- 58.Ng SS, Lee JF, Yiu RY, Li JC, Leung WW, Leung KL. Emergency laparoscopic-assisted versus open right hemicolectomy for obstructing right-sided colonic carcinoma: a comparative study of short-term clinical outcomes. World J Surg. 2008;32:454–458. doi: 10.1007/s00268-007-9400-0. [DOI] [PubMed] [Google Scholar]
- 59.Li JC, Hon SS, Ng SS, Lee JF, Leung WW, Leung KL. Emergency laparoscopic-assisted right hemicolectomy: can we achieve outcomes similar to elective operation? J Laparoendosc Adv Surg Tech A. 2011;21:701–704. doi: 10.1089/lap.2011.0039. [DOI] [PubMed] [Google Scholar]
- 60.Stipa F, Pigazzi A, Bascone B, Cimitan A, Villotti G, Burza A, Vitale A. Management of obstructive colorectal cancer with endoscopic stenting followed by single-stage surgery: open or laparoscopic resection? Surg Endosc. 2008;22:1477–1481. doi: 10.1007/s00464-007-9654-5. [DOI] [PubMed] [Google Scholar]
- 61.Iversen LH, Kratmann M, Bøje M, Laurberg S. Self-expanding metallic stents as bridge to surgery in obstructing colorectal cancer. Br J Surg. 2011;98:275–281. doi: 10.1002/bjs.7333. [DOI] [PubMed] [Google Scholar]
- 62.Targownik LE, Spiegel BM, Sack J, Hines OJ, Dulai GS, Gralnek IM, Farrell JJ. Colonic stent vs. emergency surgery for management of acute left-sided malignant colonic obstruction: a decision analysis. Gastrointest Endosc. 2004;60:865–874. doi: 10.1016/s0016-5107(04)02225-4. [DOI] [PubMed] [Google Scholar]
- 63.Group CCCS. The role of endoluminal stenting in the acute management of obstructing colorectal cancer. Available from: http://www.birmingham.ac.uk/Documents/college-mds/trials/bctu/crest/CReSTProtocolv2116072009.pdf 2009.
- 64.Bleier JI, Moon V, Feingold D, Whelan RL, Arnell T, Sonoda T, Milsom JW, Lee SW. Initial repair of iatrogenic colon perforation using laparoscopic methods. Surg Endosc. 2008;22:646–649. doi: 10.1007/s00464-007-9429-z. [DOI] [PubMed] [Google Scholar]
- 65.Odermatt M, Miskovic D, Siddiqi N, Khan J, Parvaiz A. Short- and long-term outcomes after laparoscopic versus open emergency resection for colon cancer: an observational propensity score-matched study. World J Surg. 2013;37:2458–2467. doi: 10.1007/s00268-013-2146-y. [DOI] [PubMed] [Google Scholar]


