Abstract
AIM: To report the incidence, clinical features and outcomes of gastrointestinal (GI) involvement in Behcet’s disease (BD).
METHODS: A total of 168 consecutive patients with BD were screened and upper and lower GI endoscopies were performed in 148 patients. Four hundred age- and sex-matched controls were enrolled for comparison.
RESULTS: Fifty-two (35.1%) patients had GI lesions. After a mean follow-up of 10 mo, ileocecal ulcers had been confirmed in 20 patients, including active ulcer(s) in 18 patients, but no ileocecal ulceration was found in controls. GI symptoms were present in 14 patients with active ulcer(s), while 4 patients with smaller ulcer were asymptomatic. Endoscopic features of ileocecal ulcer were: a single ulcer (50%), larger than 1 cm in diameter (72.2%), and round/oval or volcano-type in shape (83.3%). Compared with patients without GI involvement, less ocular lesions, lower levels of albumin, erythrocyte count and hemoglobin, and higher levels of C-reactive protein and erythrocyte sedimentation rate were confirmed in the intestinal BD group. Four patients had esophageal ulcers in the BD group but no case in controls. The other endoscopic findings were similar between the two groups. The prevalence of Helicobacter pylori infection was similar in both groups. Most patients received an immunomodulator and responded well.
CONCLUSION: GI lesions commonly occur in Chinese BD patients. The most frequently involved area is the ileocecal region. Esophageal ulcer might be a rare but unique lesion.
Keywords: Behcet’s disease, Gastrointestinal involvement, Ulcer, Endoscopy, Case-controlled
Core tip: This study reports the incidence and clinical features of gastrointestinal (GI) involvement in a total of 168 consecutive Chinese patients with Behcet’s disease (BD), of whom upper and lower GI endoscopies were performed in 148 patients. Controls were enrolled for comparison. Fifty-two (35.1%) patients had GI lesions. After a mean follow-up of 10 mo, ileocecal ulcers had been confirmed in 20 patients, but no ileocecal ulceration was found in controls. Four patients had esophageal ulcers in the BD group but no case in controls. The other endoscopic findings were similar between the two groups.
INTRODUCTION
Behcet’s disease (BD) is a rare, recurrent multisystem inflammatory disease that often presents with mucosal ulcerations and ocular lesions. It can also involve visceral organs such as the gastrointestinal (GI) tract, pulmonary, cardiovascular, musculoskeletal and neurological systems[1]. Its incidence is relatively higher in East Asia (13.5-20 patients per 100000 inhabitants) than in the United States and the United Kingdom (0.12-0.64 patients per 100000 inhabitants)[2-5]. The prognosis of BD varies from nuisance to fatality. The involvement of the central nervous system, large blood vessels, and GI tract often leads to a fatal prognosis[3].
Because GI involvement can result in severe morbidity and mortality[6], BD is designated ‘‘intestinal BD’’ or “entero-BD” if a typical oval-shaped large ulcer in the terminal ileum or ulcerations in the GI tract are objectively documented[6,7]. The prevalence of intestinal involvement in patients with BD has been reported to be 3%-25%, although it varies in different populations[2,8-10]. Symptomatic intestinal involvement is common in East Asian patients[6,8,11,12] but rare in Mediterranean patients[3,5,13,14]. Common clinical symptoms include abdominal pain, diarrhea, and bleeding, similar to those of inflammatory bowel disease. We had experiences in treating BD patients with acute manifestations of intestinal perforation or hemorrhage, but without chronic GI symptoms. Occasionally upper endoscopy might reveal esophageal ulcers without dysphagia, epigastric pain, or heartburn in BD patients. Several small-sample studies were conducted to investigate the prevalence of GI involvement in BD patients with GI symptoms[15-18]. However, the real frequency of GI involvement, including “silent” or asymptomatic ulcers, in BD is unknown. Accordingly, the aim of this study was to prospectively observe the frequency of GI involvement and assess the endoscopic features in BD patients by both esophagogastroduodenoscopy (EGD) and ileo-colonoscopy irrespective of GI symptoms at a single tertiary academic medical center in China.
MATERIALS AND METHODS
Ethics
This work was carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. The study protocol was approved by the institutional review board of Huadong hospital, and informed consent was obtained from all study participants.
Subjects and methods
We recruited 168 consecutive patients with BD presenting to the Division of Immunology and Rheumatology at the Fudan University Huadong Hospital, Shanghai, China, between July 2011 and June 2013. BD was diagnosed according to the revision of international study group criteria (ISG)[19] and BD Research Committee of Japan 1987[20]. The ISG criteria require recurrent oral ulcerations plus two of the following additional findings: (1) recurrent genital ulcerations; (2) eye lesions consisting of an iritis, posterior uveitis, renal vessel occlusion, and/or optic neuritis; (3) skin lesions consisting of folliculitis, erythema nodosum, an acne-like exanthema, or a migratory thrombophlebitis; or (4) a positive pathergy test, which is an inflammatory skin reaction to an intradermal injection of saline. The Japan criteria consist of four major (oral ulceration, skin lesions, eye lesions, and genital ulcers) and five minor symptoms (arthritis, intestinal ulcers, vascular disease, neuropsychiatric disorders, and epididymitis). Patients were classified into subset types: complete type (four major features), incomplete type (three major features, two major plus two minor, typical ocular symptom plus one major or two minor features), and suspected type (two major features, or one major plus two minor features). Additionally, patients were further categorized into two groups labeled as defined or probable for intestinal BD by diagnostic criteria based on two aspects: endoscopic findings and extra-intestinal manifestations[21]. The ulcerations were divided into “typical” and “atypical” ulcerations for intestinal BD on the basis of endoscopic findings. Patients with < 5 ulcers that were oval in shape, deep, with discrete borders, and were located in the ileocecal area were classified as having “typical” ulcers[22]. Ulcerations that did not fulfill all of the characteristics were regarded as atypical. The Japan criteria were applied to access the extra-intestinal manifestations. Patients with typical intestinal ulcerations in the ileo-colonoscopic examination who had extra-intestinal symptoms that could be classified as complete, incomplete, or suspected were allocated to the “definite” intestinal BD group. Whereas, those with atypical intestinal ulcerations presenting with extra-intestinal symptoms that could be classified as complete, incomplete, or suspected were allocated to the “probable” intestinal BD group. Four hundred age- and sex-matched control patients were enrolled for comparison of the prevalence of GI lesions (Figure 1).
Figure 1.
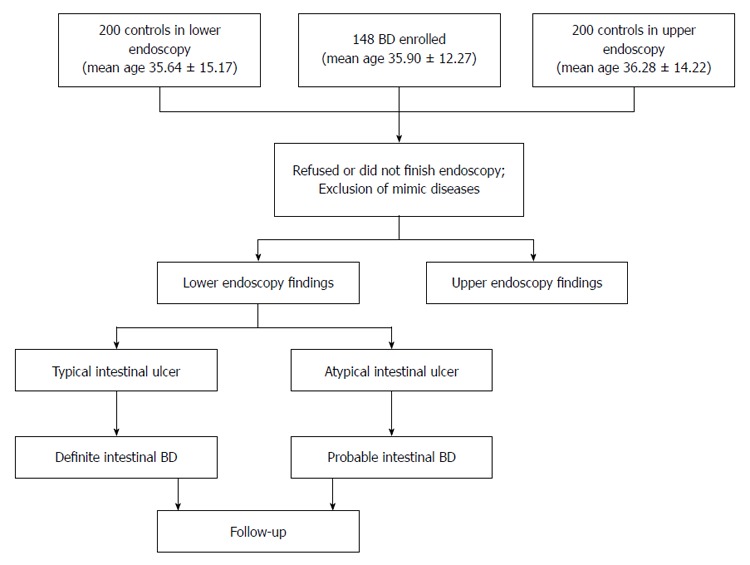
Study protocol and algorithm for the diagnosis of intestinal Behcet’s disease. Complete, incomplete, and suspected subtypes of systemic Behcet’s disease (BD) were classified according to the diagnostic criteria of the Research Committee of Japan 1987.
Exclusion criteria
Patients who refused GI endoscopic examination or did not have perfect bowel cleansing at ileo-colonoscopy were excluded. Differential diagnosis of particularly tuberculosis, lymphoma, carcinoma, Crohn’s disease, acid-related disease (peptic ulcer, stress ulcer or Zollinger-Ellison syndrome), drug-induced disease (corticosteroids and non-steroidal anti-inflammatory drugs), and ischemic colitis, during the initial evaluation and follow-up, was excluded based on clinical, endoscopic, blood, microbiologic, and/or histopathologic findings.
Endoscopy procedure
Endoscopic examination was performed by two gastroenterologists by using the Olympus GIF H260 and CF-H 260A1 in all subjects for upper and lower GI tract examinations. During endoscopy, two biopsies were taken from the antrum for rapid urease test and histological examination.
Clinical evaluation and laboratory findings
The presence of extra-GI symptoms (systemic symptoms), including genital ulcers, uveitis, dermatological lesions, neurological involvement, peripheral vasculitis, and joint involvement at the time of diagnosis, and GI symptoms such as dyspepsia, hunger pain, chest/abdominal pain, dysphagia, diarrhea, or bleeding, were recorded. Laboratory results including level of erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) level, peripheral blood count, and serum albumin were evaluated.
Statistical analysis
The software program SPSS (v. 19, Chicago, IL) was used for statistical analyses. Student’s t-test or Mann-Whitney U-test was used to compare numerical variables between groups. The χ2 or Fisher’s exact test was used to compare categorical variables. P values < 0.05 were considered statistically significant.
RESULTS
Recruitment
Among the total of 168 consecutive Chinese patients with BD, 20 either refused to undergo endoscopy, or did not complete an ileo-colonoscopy due to a non-perfect bowel cleansing. After excluding those patients, a total of 148 BD patients (mean age 35.9 ± 12.3 years, range: 13-65; mean duration of disease 95.8 ± 87.6 mo, range: 1-540) were enrolled in the study, including 68 female and 80 male patients. Eighty-seven (58.8%) patients fulfilled the ISG criteria and all met the Japan criteria: 9 (6.1%) patients classified as complete subtype, 87 (58.8%) as incomplete subtype, and 52 (35.1%) as suspected subtype.
There were 95 (64%) patients with newly diagnosed BD and taking no medication at endoscopy. Among the remaining 53 patients, 42 were using thalidomide, and 32 were using one or a combination of immunosuppressive drugs (cyclosporine, azathioprine, hydroxychloroquine, colchicine or steroid). Most of the immunosuppressive users had visceral organ involvement, with ocular, central nervous system, large blood vessel, GI tract or refractory skin lesions. None of our patients had a history of chronic or recent NSAID usage. Forty-four (30%) patients had GI symptoms at the time of the endoscopic study, most commonly epigastric pain (18%), heartburn (11%), abdominal pain (22%), diarrhea (11%), GI bleeding (3%), and constipation (8%).
Ileo-colonoscopy (macroscopic appearances)
GI lesions were noted in 52 (35.1%) patients in general. Initially, 21 patients with ileocolonic ulcers were identified. After a mean follow-up of 10.5 ± 6.3 mo (range: 2-26), a 50-year-old female with atypical colon ulceration was re-diagnosed with ischemic colitis involving the left-side colon and sigmoid by both endoscopic manifestation and histological findings. Eventually, ileocecal ulcer(s) were confirmed in 20 patients, including active lesions in 18 individuals (10 females and 8 males; sex ratio 1.25:1; Table 1) and ulcer scars in two. No ulceration was found in the control group. The extra-intestinal symptoms were: oral ulcers in 18 (100%) patients, genital ulcer in 17 (88.9%), ocular lesion in 0 (0%), skin lesion in 14 (77.8%), arthralgia in 3 (16.7%) and a positive pathergy result in 4 (40%). Fourteen (77.8%) patients fulfilled the ISG criteria. According to their extra-intestinal symptoms, 14 patients met incomplete subtype and 4 fulfilled suspected subtype. The ulcer locations were the terminal ileum in 11 patients (61.1%), the ileocecal valve in 3 (16.7%, Figure 2), the cecum in 4 (22.2%), and other segments of the colon in 3 (16.7%, Figure 3). Single ulcers were observed in 9 (50%) patients. Four (22.2%) patients had two to five localized ulcers. Multi-segmental and diffuse distribution of lesions was uncommon (27.8%). The size of ulcers ranged from 0.5 cm to 5 cm. Ulcer larger than 1 cm was recorded in 13 (72.2%) patients. Round/oval shape was the most common (55.6%), followed by volcano-type (27.7%) and irregular/geographic shape (16.7%). Based on the adopted criteria[21], 15 patients with typical ulcers were allocated to the definite group, whereas 3 patients with atypical ulcers were allocated to the probable group.
Table 1.
Clinical features of Behcet’s disease patients with gastrointestinal lesions (none had arthritis, vascular or neurological involvement)
| Case No. | Gender | Age | ISG | Japan | Abdominal pain | Other GI symptoms | Endoscopic findings | Distribution pattern | Size (cm) | Shape |
| 1 | Female | 26 | - | Incomplete | - | Constipation | Terminal ileum | Multiple | > 1, ≤ 3 | Round/oval |
| 2 | Male | 18 | - | Incomplete | + | EU, terminal ileum, CU | Multi-segmental | > 1, ≤ 3 | Geographic | |
| 3 | Male | 49 | + | Incomplete | + | Terminal ileum, GU | Multi-segmental | > 3, ≤ 5 | Volcano | |
| 4 | Female | 35 | - | Incomplete | - | Terminal ileum | Single | ≤ 1 | Round/oval | |
| 5 | Male | 23 | + | Incomplete | + | Terminal ileum | Single | > 1, ≤ 3 | Round/oval | |
| 6 | Female | 22 | + | Incomplete | + | Diarrhea | Terminal ileum, CU | Diffuse | > 1, ≤ 3 | Geographic |
| 7 | Female | 32 | + | Suspected | + | Ileocecal valve | Single | ≤ 1 | Round/oval | |
| 8 | Male | 19 | - | Suspected | + | Diarrhea | Ileocecal valve | Single | > 3, ≤ 5 | Volcano |
| 9 | Male | 56 | + | Incomplete | + | Bloody stool | Terminal ileum | Single | > 1, ≤ 3 | Round/oval |
| 10 | Female | 30 | + | Suspected | + | Terminal ileum | Single | > 1, ≤ 3 | Round/oval | |
| 11 | Female | 23 | + | Incomplete | - | Cecum | Multiple | ≤ 1 | Round/oval | |
| 12 | Female | 21 | + | Incomplete | - | Terminal ileum | Single | > 1, ≤ 3 | Round/oval | |
| 13 | Female | 28 | + | Incomplete | + | Diarrhea | Ileocecal valve | Single | > 5 | Round/oval |
| 14 | Male | 60 | + | Incomplete | + | Diarrhea | Cecum | Single | > 5 | Volcano |
| 15 | Female | 23 | + | Incomplete | - | Terminal ileum | Multiple | ≤ 1 | Round/oval | |
| 16 | Male | 50 | + | Incomplete | + | Diarrhea | EU, cecum | Multi-segmental | > 3, ≤ 5 | Volcano |
| 17 | Male | 40 | - | Suspected | + | Diarrhea | Terminal ileum | Multiple | > 1, ≤ 3 | Volcano |
| 18 | Female | 58 | + | Incomplete | + | Diarrhea | Cecum, CU | Multi-segmental | > 3, ≤ 5 | Geographic |
GI: Gastrointestinal; EU: Esophageal ulcer; GU: Gastric ulcer; CU: Colonic ulcer; ISG: International Study Group criteria; Japan: Criteria of the Research Committee of Japan 1987.
Figure 2.
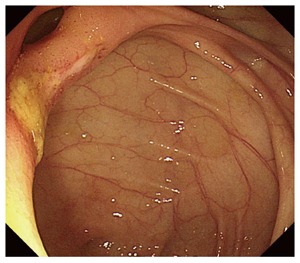
Ileocolonoscopic appearance of patient 10 with an ulcer in her ileocecal valve.
Figure 3.
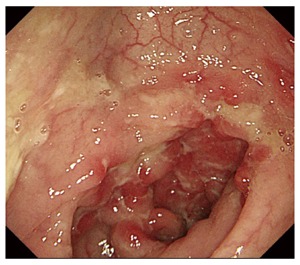
Colonoscopic appearance of patient 2 with ulcers in his transverse colon.
GI symptoms were present in 14 patients with active ulcer(s). GI symptoms included: abdominal pain in 13 (72.2%) patients, diarrhea in 7 (38.9%), GI bleeding in 1 (5.6%), and constipation in 1 (5.6%). Four patients with smaller ulcers (less than 1 cm in diameter in 3 patients) were asymptomatic at baseline.
The comparisons of extra-intestinal manifestations in BD patients with lower GI ulcer(s) and without GI lesion revealed that no ocular lesions, lower levels of albumin, erythrocyte count and hemoglobin, and higher levels of CRP and ESR were confirmed in the entero-BD group. No statistical difference was found between two groups in age, duration of BD, the presence of genital ulcer, uveitis, dermatological lesions, and joint pain, or pathergy test (Table 2).
Table 2.
Comparison of symptoms and laboratory findings in Behcet’s disease patients with lower gastrointestinal ulcer(s) and without gastrointestinal lesion n (%)
| BD with lower GI ulcer (n = 20) | BD without GI lesion (n = 96) | P value | |
| Age at diagnosis of intestinal BD (yr) | 34.65 ± 14.59 | 33.63 ± 11.50 | 0.77 |
| Male (%) | 8 (40) | 53 (55.2) | - |
| Duration (mo) | 104.30 ± 125.44 | 88.05 ± 70.13 | 0.58 |
| Systematic signs | |||
| Oral ulcer | 20 (100) | 96 (100) | 1.00 |
| Genital ulcer | 16 (80) | 69 (72) | 0.46 |
| Ocular lesion | 0 (0) | 27 (28) | < 0.01a |
| Skin lesion | 15 (75) | 62 (65) | 0.36 |
| Arthralgia | 3 (15) | 30 (31) | 0.10 |
| Epididymitis | 0 (0) | 1 (1) | 0.65 |
| Pathergy test | 4 (20) | 20 (21) | 0.95 |
| Vasculitis | 0 (0) | 2 (2) | 0.52 |
| Central nerve system | 0 (0) | 1 (1) | 0.65 |
| Laboratory findings at diagnosis | |||
| CRP (mg/L) | 30.34 ± 30.62 | 12.41 ± 9.18 | 0.02a |
| ESR (mm/h) | 36.75 ± 22.65 | 24.04 ± 23.50 | 0.03a |
| Albumin (g/L) | 38.70 ± 4.00 | 42.71 ± 6.12 | < 0.01a |
| WBC (109/L) | 7.00 ± 2.78 | 7.46 ± 2.69 | 0.49 |
| RBC (1012/L) | 4.13 ± 0.46 | 4.62 ± 0.64 | 0.02a |
| Hemoglobin (g/L) | 117.47 ± 15.11 | 137.81 ± 18.29 | < 0.01a |
| Platelets (109/L) | 249.65 ± 92.49 | 240.54 ± 73.60 | 0.63 |
P < 0.05 vs control. BD: Behcet’s disease; CRP: C-reactive protein; ESR: Erythrocyte sedimentation rate; WBC: White blood cell count; RBC: Red blood cell count; GI: Gastrointestinal.
One patient (patient 10, with a single ileocecal ulcer) presenting with sudden onset of a high-grade fever up to 39-40 °C and severe abdominal pain was diagnosed with BD associated with myelodysplastic syndrome (MDS), and chromosomal analysis revealed trisomy 8.
Upper gastrointestinal endoscopy (macroscopic appearances)
EGD revealed esophageal ulcers (Figure 4) in 4 patients in the BD group, but there was no patient with esophageal ulcer in the control group. The distribution pattern of lesions included: multiple localized type (2 patients) and multi-segments (2 patients, associated with ulcers in other parts of the gastrointestinal tract). Notably all the esophageal ulcers were small, superficial ulcers. The other upper endoscopic findings such as esophagitis (13.5% in the patients with BD and 15.5% in the control group, P > 0.05), gastric erosion (18.2% in the patients with BD and 8.7% in the control group, P > 0.05), gastric ulcer (6.8% in the patients with BD and 8.5% in the control group, P > 0.05), duodenal ulcer (5.7% in the patients with BD and 9.6% in the control group, P > 0.05), duodenitis (1.9% in the patients with BD and 1% in the control group, P > 0.05) were similar in both groups.
Figure 4.
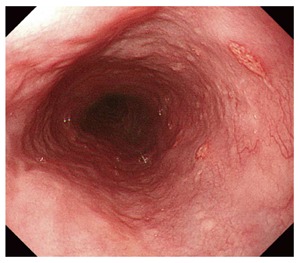
Endoscopic appearance of patient 2 with ulcers in his esophagus.
Helicobacter pylori infection and histology
Helicobacter pylori (H. pylori) infection was detectable in 13.2% of patients with BD, and 12.8% in controls by rapid urease test. No difference was found between the two groups.
The histological examinations of esophageal and ileocecal ulcerations revealed the lymphoplasmocytic and (or) polymorphonuclear infiltration and presence of granulation tissue and fibroblasts in all cases. There was crypt abscess in 2 patients. Two cases with typical ileocecal ulcer were reported with granulomas. Vasculitis was found in 2 cases (patients 12 and 18).
Treatments and prognosis
Treatments for 18 intestinal BD patients included steroids, 5-aminosalicylate, thalidomide, azathioprine and infliximab. Most patients received an immunomodulator and experienced a clinical response. Fourteen patients went into complete clinical remission. No patient experienced a deterioration and (or) severe complications which need surgical intervention.
DISCUSSION
We prospectively followed and assessed the incidence of GI involvement irrespective of GI symptoms and found that GI abnormalities were frequently present in Chinese BD patients. The typical GI lesion was ileocecal ulcer, featuring as a single or a few larger deep round/oval ulcer(s) with certain GI manifestations. Patients with small ulcer(s) were usually absent of GI symptoms. Esophageal ulcers were relative rare but unique manifestations.
Because BD lacks pathognomonic symptoms or laboratory findings, the diagnosis depends on clinical signs and symptoms. We employed the most commonly used criteria (the Japan criteria and ISG criteria) to assess the extra-intestinal manifestations.
The frequency of gastrointestinal involvement varies in different countries, for example, a lower frequency in Turkey[23], but a higher frequency in Japan[4,24,25]. The real incidence rate might be underestimated due to “silent” patients not included in most studies. By routine GI endoscopy we found the frequency of GI involvement in our series was 35.1%. Thus an underestimation might be eliminated in this situation.
Intestinal BD can be a difficult diagnosis to establish. Due to similarities in intestinal and extraintestinal manifestations and pathologic findings[2], clinicians could be confused by a differentiation between intestinal BD and other mimic diseases, particularly Crohn’s disease and intestinal tuberculosis. Hatemi et al[26] had proven that ISG criteria performed well in differentiating IBD from BD in a Turkish population. Although features commonly seen in BD such as oral ulcers and papulopustular lesions were widely present in IBD patients, there were only few patients who fulfilled the ISG criteria. In our study, all patients met the Japan criteria, and most of them (13/18) met the ISG criteria. The rest 5 patients did not meet the ISG criteria, however, all of them had typical ulcer(s): a single or a few large round/oval ileocecal ulcer(s). Compared with the ISG criteria, the Japan criteria include more clinical manifestations and have a gradual diagnostic system that can reflect a temporal change better than the ISG. Besides clinical manifestations, the endoscopic features including shape (round, irregular/geographic, or longitudinal) and distribution pattern (focal single/focal multiple, or segmental/diffuse) are helpful to distinguish intestinal BD from Crohn’s disease. In this study we adopted the algorithm proposed by Cheon et al[21] based on clinical manifestations and the type of ileocolonic ulcers and enrolled controls for comparison. It has been proven that after combining the definite, probable, and suspected groups, the sensitivity and specificity of this algorithm for diagnosing intestinal BD were 99% and 83%, respectively. Our study found that the algorithm was quite reliable. After short-term follow-up only one patient with atypical ulcer was re-diagnosed as ischemic colitis by endoscopic features and histological findings.
Our study found distribution pattern as single ulcer (50%), two to five localized (27.8%), multi-segmental and diffuse (22.2%), which is similar to the data reported in Japan and South Korea studies[6,22,27-30]. Typical ileocecal lesion is a single large ulcer, round or oval in shape, usually with a sharp outline. Larger typical ulcers were often accompanied by GI manifestations, including abdominal pain, diarrhea, bleeding, and constipation. The presence of GI symptoms is commonly considered an indication for endoscopic examination. In our series we found 4 cases with relatively smaller ileocecal ulcer(s) presenting with no GI symptom. Two patients with ulcer scar had no GI complaints. Intestinal BD usually was believed to be associated with GI symptom and worse prognosis[6,31]. However, we found that asymptomatic patients might experience a self-limited course and have a better outcome.
Esophageal ulceration in BD is believed to be rare according to previous studies[15,17,32,33], with frequencies ranging from 2% to 11% in different BD populations. Bektas et al[34] reported that esophageal motor abnormalities were found in one-third patients, although endoscopic abnormalities were observed in 16% patients. We found esophageal ulcer(s) in 4 BD patients, and esophageal erosion in 20 patients. In the control group, the rate of esophageal erosion was similar to that in the BD group, whereas, no esophageal ulcer had been found. There was no case of esophageal fistula; luminal strictures; pseudomembrane esophagitis; or “downhill” or classical esophageal varices associated with either superior vena cava obstruction or portal hypertension due to portal vein thrombosis in our study[35,36].
We have found no difference in the prevalence of esophagitis, gastric erosion, gastric ulcers, and duodenal ulcers between patients with BD and controls. Thus the above GI abnormalities might not be specific for BD. None of our patients with lesions had histories of NSAID usage. H. pylori infection rate in the BD group was similar to that of controls, while the rate of H. pylori infection is far lower than GI abnormality rate in either group, which suggests that except for H. pylori infection and BD, other factors account for the high rate of GI abnormality. Dieulafoy’s ulcer[37] and gastric non-Hodgkin’s lymphoma[38] associated with BD have not been revealed in this study.
Besides, one case with trisomy 8 was associated with MDS. This patient (patient 10) showed a significantly higher ESR level compared with patients without MDS (P < 0.05). Intestinal ulceration is a frequent characteristic in BD associated with bone marrow failure classified as conditions such as MDS or aplastic anemia[39-41]. Cytogenetic aberration, especially trisomy 8, may play an important role in the pathogenesis of intestinal BD.
Laboratory values including ESR, CRP, erythrocyte count, hemoglobin level, leukocyte count, platelet count and albumin were evaluated at baseline. The prevalence of anemia, hypoalbuminemia and increased parameters of inflammation (CRP, ESR) has been noticed in the ileocecal ulcer group. For a long time, anemia and hypoalbuminemia have been recognized as the key symptoms of inflammatory bowel disease[42,43]. In Crohn’s disease, serum levels of CRP correlate well with disease activity[44]. Our results confirmed that laboratory findings in intestinal BD were similar to those in inflammatory bowel disease.
The histological aspects of GI lesions in BD, involving acute or chronic nonspecific infiltrates and granulation tissue and fibroblasts, are typically seen at the base of the ulceration. The finding of vasculitis is an uncommon but strong indication of intestinal BD[45]. Although noncaseating epitheloid granuloma is one of the pathognomonic features of Crohn’s disease[46], occasionally granuloma can also present in patients with intestinal BD[47,48].
All patients in this report received various treatments for their GI lesions, and all but three patients responded well to treatments as evidenced by remission of symptoms. Although treatment strategies varied, all were given immunomodulators, which supports the importance of immunosuppressive therapy in BD.
There are certain limitations in the study. First, it was a single-center and hospital-based study with potential bias in its design. Second, the relatively short-term follow-up may be limiting factors towards the justification of accurate diagnosis. Hence, future long-term follow-up studies are needed to elucidate the natural history of GI tract involvement in BD. Third, because of poor tolerance or high cost of double-balloon enteroscopy or capsule endoscopy, the small intestine was not fully investigated in the study. Future studies should employ at least one method to investigate the small intestine.
In conclusion, GI abnormalities are frequently observed in Chinese BD patients. The typical lesion is ileocecal ulceration, featured by a single or few large ulcers, round or oval in shape, with a discrete margin. Small ulcers usually present without GI symptoms. Esophageal ulcer might be a rare but unique GI lesion in patients with BD.
COMMENTS
Background
Little is known about the incidence and features of Behcet’s disease (BD) with gastrointestinal (GI) lesions, especially in the Chinese population.
Research frontiers
A total of 168 consecutive patients with BD were screened and upper and lower GI endoscopies were performed in 148 patients. Four hundred age- and sex-matched controls were enrolled for comparison.
Innovations and breakthroughs
In the present study, the authors reported the incidence and clinical features of GI involvement in BD in China.
Applications
The study results suggest that GI lesions commonly occur in Chinese BD patients. The most frequently involved area is the ileocecal region. Small ulcer usually presents without GI symptoms. Esophageal ulcer might be a rare but unique lesion.
Terminology
BD is a rare, recurrent multisystem inflammatory disease that often presents with mucosal ulcerations and ocular lesions. GI involvement can result in severe morbidity and mortality. The prevalence of intestinal involvement in patients with BD has been reported to be 3%-25%, although it varies in different populations. Several small-sample studies were conducted to investigate the prevalence of GI involvement in BD patients with GI symptoms. However, the real frequency of GI involvement, including “silent” or asymptomatic ulcers, in BD is unknown.
Peer review
This is an interesting and large study on a rather rare disease in Western countries. The gastrointestinal involvement of Behcet’s disease in Chinese patients has been assessed by endoscopy. The results are interesting and suggest that GI lesions commonly occur in Chinese BD patients. The most frequently involved area is the ileocecal region. Esophageal ulcer might be a rare but unique lesion.
Footnotes
P- Reviewer: Sadik R S- Editor: Qi Y L- Editor: Wang TQ E- Editor: Ma S
References
- 1.O’Duffy JD. Behçet’s disease. Curr Opin Rheumatol. 1994;6:39–43. [PubMed] [Google Scholar]
- 2.Sakane T, Takeno M, Suzuki N, Inaba G. Behçet’s disease. N Engl J Med. 1999;341:1284–1291. doi: 10.1056/NEJM199910213411707. [DOI] [PubMed] [Google Scholar]
- 3.Kaklamani VG, Vaiopoulos G, Kaklamanis PG. Behçet’s Disease. Semin Arthritis Rheum. 1998;27:197–217. doi: 10.1016/s0049-0172(98)80001-2. [DOI] [PubMed] [Google Scholar]
- 4.Nakae K, Masaki F, Hashimoto T, Inaba G, Mochizuki M, Sakane T. C 10 Recent epidemiological features of Behçet’s disease in Japan. La Rev de Méd Int. 1993;14 Supplement 1:28s. [Google Scholar]
- 5.Zouboulis CC, Kötter I, Djawari D, Kirch W, Kohl PK, Ochsendorf FR, Keitel W, Stadler R, Wollina U, Proksch E, et al. Epidemiological features of Adamantiades-Behçet’s disease in Germany and in Europe. Yonsei Med J. 1997;38:411–422. doi: 10.3349/ymj.1997.38.6.411. [DOI] [PubMed] [Google Scholar]
- 6.Kasahara Y, Tanaka S, Nishino M, Umemura H, Shiraha S, Kuyama T. Intestinal involvement in Behçet’s disease: review of 136 surgical cases in the Japanese literature. Dis Colon Rectum. 1981;24:103–106. doi: 10.1007/BF02604297. [DOI] [PubMed] [Google Scholar]
- 7.Kobayashi K, Ueno F, Bito S, Iwao Y, Fukushima T, Hiwatashi N, Igarashi M, Iizuka BE, Matsuda T, Matsui T, et al. Development of consensus statements for the diagnosis and management of intestinal Behçet’s disease using a modified Delphi approach. J Gastroenterol. 2007;42:737–745. doi: 10.1007/s00535-007-2090-4. [DOI] [PubMed] [Google Scholar]
- 8.Shimizu T, Ehrlich GE, Inaba G, Hayashi K. Behçet disease (Behçet syndrome) Semin Arthritis Rheum. 1979;8:223–260. doi: 10.1016/0049-0172(79)90004-0. [DOI] [PubMed] [Google Scholar]
- 9.Bayraktar Y, Ozaslan E, Van Thiel DH. Gastrointestinal manifestations of Behcet’s disease. J Clin Gastroenterol. 2000;30:144–154. doi: 10.1097/00004836-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Lehner T. Oral ulceration and Behçet’s syndrome. Gut. 1977;18:491–511. doi: 10.1136/gut.18.6.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ha HK, Lee HJ, Yang SK, Ki WW, Yoon KH, Shin YM, Jung HY, Yu E, Lee SI, Kim KW, et al. Intestinal Behçet syndrome: CT features of patients with and patients without complications. Radiology. 1998;209:449–454. doi: 10.1148/radiology.209.2.9807572. [DOI] [PubMed] [Google Scholar]
- 12.Oshima Y, Shimizu T, Yokohari R, Matsumoto T, Kano K, Kagami T, Nagaya H. Clinical Studies on Behçet’s Syndrome. Ann Rheum Dis. 1963;22:36–45. doi: 10.1136/ard.22.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baba S, Maruta M, Ando K, Teramoto T, Endo I. Intestinal Behçet’s disease: report of five cases. Dis Colon Rectum. 1976;19:428–440. doi: 10.1007/BF02590829. [DOI] [PubMed] [Google Scholar]
- 14.Yurdakul S, Tüzüner N, Yurdakul I, Hamuryudan V, Yazici H. Gastrointestinal involvement in Behçet’s syndrome: a controlled study. Ann Rheum Dis. 1996;55:208–210. doi: 10.1136/ard.55.3.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yi SW, Cheon JH, Kim JH, Lee SK, Kim TI, Lee YC, Kim WH. The prevalence and clinical characteristics of esophageal involvement in patients with Behçet’s disease: a single center experience in Korea. J Korean Med Sci. 2009;24:52–56. doi: 10.3346/jkms.2009.24.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karincaoglu Y, Borlu M, Toker SC, Akman A, Onder M, Gunasti S, Usta A, Kandi B, Durusoy C, Seyhan M, et al. Demographic and clinical properties of juvenile-onset Behçet’s disease: A controlled multicenter study. J Am Acad Dermatol. 2008;58:579–584. doi: 10.1016/j.jaad.2007.10.452. [DOI] [PubMed] [Google Scholar]
- 17.Ning-Sheng L, Ruay-Sheng L, Kuo-Chih T. High frequency of unusual gastric/duodenal ulcers in patients with Behçet’s disease in Taiwan: a possible correlation of MHC molecules with the development of gastric/duodenal ulcers. Clin Rheumatol. 2005;24:516–520. doi: 10.1007/s10067-005-1083-z. [DOI] [PubMed] [Google Scholar]
- 18.Houman MH, Ben Ghorbel I, Lamloum M, Khanfir M, Braham A, Haouet S, Sayem N, Lassoued H, Miled M. Esophageal involvement in Behcet’s disease. Yonsei Med J. 2002;43:457–460. doi: 10.3349/ymj.2002.43.4.457. [DOI] [PubMed] [Google Scholar]
- 19.Criteria for diagnosis of Behçet’s disease. International Study Group for Behçet’s Disease. Lancet. 1990;335:1078–1080. [PubMed] [Google Scholar]
- 20.Mizushima Y. Recent research into Behçet’s disease in Japan. Int J Tissue React. 1988;10:59–65. [PubMed] [Google Scholar]
- 21.Cheon JH, Kim ES, Shin SJ, Kim TI, Lee KM, Kim SW, Kim JS, Kim YS, Choi CH, Ye BD, et al. Development and validation of novel diagnostic criteria for intestinal Behçet’s disease in Korean patients with ileocolonic ulcers. Am J Gastroenterol. 2009;104:2492–2499. doi: 10.1038/ajg.2009.331. [DOI] [PubMed] [Google Scholar]
- 22.Lee CR, Kim WH, Cho YS, Kim MH, Kim JH, Park IS, Bang D. Colonoscopic findings in intestinal Behçet’s disease. Inflamm Bowel Dis. 2001;7:243–249. doi: 10.1097/00054725-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Dilşen N, Koniçe M, Aral O, Ocal L, Inanç M, Gül A. Comparative study of the skin pathergy test with blunt and sharp needles in Behçet’s disease: confirmed specificity but decreased sensitivity with sharp needles. Ann Rheum Dis. 1993;52:823–825. doi: 10.1136/ard.52.11.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ideguchi H, Suda A, Takeno M, Ueda A, Ohno S, Ishigatsubo Y. Behçet disease: evolution of clinical manifestations. Medicine (Baltimore) 2011;90:125–132. doi: 10.1097/MD.0b013e318211bf28. [DOI] [PubMed] [Google Scholar]
- 25.Kobayashi T, Kishimoto M, Swearingen CJ, Filopoulos MT, Ohara Y, Tokuda Y, Oshikawa H, Yoshida K, Utsunomiya M, Kimura M, et al. Differences in clinical manifestations, treatment, and concordance rates with two major sets of criteria for Behçet’s syndrome for patients in the US and Japan: data from a large, three-center cohort study. Mod Rheumatol. 2013;23:547–553. doi: 10.1007/s10165-012-0696-8. [DOI] [PubMed] [Google Scholar]
- 26.Hatemi I, Hatemi G, Celik AF, Melikoglu M, Arzuhal N, Mat C, Ozyazgan Y, Yazici H. Frequency of pathergy phenomenon and other features of Behçet’s syndrome among patients with inflammatory bowel disease. Clin Exp Rheumatol. 2008;26:S91–S95. [PubMed] [Google Scholar]
- 27.Kitauchi S, Ohata H, Kuroda R, Hirose M, Sakaguchi A, Nishi S, Nishioka S. [Follow-up observation of intestinal Behçet disease treated with salazosulfapyridine and mesalazine for 8 years and 9 months] Nihon Shokakibyo Gakkai Zasshi. 1998;95:140–144. [PubMed] [Google Scholar]
- 28.Iida M, Kobayashi H, Matsumoto T, Okada M, Fuchigami T, Yao T, Fujishima M. Postoperative recurrence in patients with intestinal Behçet’s disease. Dis Colon Rectum. 1994;37:16–21. doi: 10.1007/BF02047208. [DOI] [PubMed] [Google Scholar]
- 29.Yamamoto T, Tamura M, Hamauzu T, Nakayama A, Kawasugi K, Kamakura M, Kinoshita T, Kuyama Y, Yamanaka M, Wang LM, et al. Intestinal Behçet’s disease associated with non-Hodgkin’s lymphoma. J Gastroenterol. 1997;32:241–245. doi: 10.1007/BF02936375. [DOI] [PubMed] [Google Scholar]
- 30.Tada M. [Etiology and treatment of inflammatory bowel diseases. 4. Intestinal Behcet’s disease] Nihon Naika Gakkai Zasshi. 1993;82:675–678. [PubMed] [Google Scholar]
- 31.Ketch LL, Buerk CA, Liechty D. Surgical implications of Behçet’s disease. Arch Surg. 1980;115:759–760. doi: 10.1001/archsurg.1980.01380060057016. [DOI] [PubMed] [Google Scholar]
- 32.Bottomley WW, Dakkak M, Walton S, Bennett JR. Esophageal involvement in Behçet’s disease. Is endoscopy necessary? Dig Dis Sci. 1992;37:594–597. doi: 10.1007/BF01307585. [DOI] [PubMed] [Google Scholar]
- 33.Ideguchi H, Suda A, Takeno M, Miyagi R, Ueda A, Ohno S, Ishigatsubo Y. Gastrointestinal manifestations of Behçet’s disease in Japan: a study of 43 patients. Rheumatol Int. 2014;34:851–856. doi: 10.1007/s00296-013-2838-5. [DOI] [PubMed] [Google Scholar]
- 34.Bektas M, Altan M, Alkan M, Ormeci N, Soykan I. Manometric evaluation of the esophagus in patients with Behçet’s disease. Digestion. 2007;76:192–195. doi: 10.1159/000112645. [DOI] [PubMed] [Google Scholar]
- 35.Orikasa H, Ejiri Y, Suzuki S, Ishikawa H, Miyata M, Obara K, Nishimaki T, Kasukawa R. A case of Behçet’s disease with occlusion of both caval veins and “downhill” esophageal varices. J Gastroenterol. 1994;29:506–510. doi: 10.1007/BF02361251. [DOI] [PubMed] [Google Scholar]
- 36.Bayraktar Y, Balkanci F, Kansu E, Dundar S, Uzunalimoglu B, Kayhan B, Telatar H, Gurakar A, Van Thiel DH. Cavernous transformation of the portal vein: a common manifestation of Behçet’s disease. Am J Gastroenterol. 1995;90:1476–1479. [PubMed] [Google Scholar]
- 37.Arendt T, Kloehn S, Bastian A, Bewig B, Lins M, Mönig H, Fölsch UR. A case of Behçet’s syndrome presenting with Dieulafoy’s ulcer. Z Gastroenterol. 1997;35:935–938. [PubMed] [Google Scholar]
- 38.Abe T, Yachi A, Yabana T, Ishii Y, Tosaka M, Yoshida Y, Yonezawa K, Ono A, Ikeda N, Matsuya M. Gastric non-Hodgkin’s lymphoma associated with Behçet’s disease. Intern Med. 1993;32:663–667. doi: 10.2169/internalmedicine.32.663. [DOI] [PubMed] [Google Scholar]
- 39.Tada Y, Koarada S, Haruta Y, Mitamura M, Ohta A, Nagasawa K. The association of Behçet’s disease with myelodysplastic syndrome in Japan: a review of the literature. Clin Exp Rheumatol. 2006;24:S115–S119. [PubMed] [Google Scholar]
- 40.Kawabata H, Sawaki T, Kawanami T, Shimoyama K, Karasawa H, Fukushima T, Masaki Y, Ogawa N, Hirose Y, Ozaki K, et al. Myelodysplastic syndrome complicated with inflammatory intestinal ulcers: significance of trisomy 8. Intern Med. 2006;45:1309–1314. doi: 10.2169/internalmedicine.45.1718. [DOI] [PubMed] [Google Scholar]
- 41.Ahn JK, Cha HS, Koh EM, Kim SH, Kim YG, Lee CK, Yoo B. Behcet’s disease associated with bone marrow failure in Korean patients: clinical characteristics and the association of intestinal ulceration and trisomy 8. Rheumatology (Oxford) 2008;47:1228–1230. doi: 10.1093/rheumatology/ken162. [DOI] [PubMed] [Google Scholar]
- 42.Vanis N, Mehmedovič A, Mesihovič R, Saray A. Anaemia and inflammatory bowel disease. Prilozi. 2013;34:35–42. [PubMed] [Google Scholar]
- 43.Gasche C, Lomer MC, Cavill I, Weiss G. Iron, anaemia, and inflammatory bowel diseases. Gut. 2004;53:1190–1197. doi: 10.1136/gut.2003.035758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vermeire S, Van Assche G, Rutgeerts P. C-reactive protein as a marker for inflammatory bowel disease. Inflamm Bowel Dis. 2004;10:661–665. doi: 10.1097/00054725-200409000-00026. [DOI] [PubMed] [Google Scholar]
- 45.Lakhanpal S, Tani K, Lie JT, Katoh K, Ishigatsubo Y, Ohokubo T. Pathologic features of Behçet’s syndrome: a review of Japanese autopsy registry data. Hum Pathol. 1985;16:790–795. doi: 10.1016/s0046-8177(85)80250-1. [DOI] [PubMed] [Google Scholar]
- 46.Price AB, Morson BC. Inflammatory bowel disease: the surgical pathology of Crohn’s disease and ulcerative colitis. Hum Pathol. 1975;6:7–29. doi: 10.1016/s0046-8177(75)80107-9. [DOI] [PubMed] [Google Scholar]
- 47.Kim ES, Chung WC, Lee KM, Lee BI, Choi H, Han SW, Choi KY, Chung IS. A case of intestinal Behcet’s disease similar to Crohn’s colitis. J Korean Med Sci. 2007;22:918–922. doi: 10.3346/jkms.2007.22.5.918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Naganuma M, Iwao Y, Kashiwagi K, Funakoshi S, Ishii H, Hibi T. A case of Behçet’s disease accompanied by colitis with longitudinal ulcers and granuloma. J Gastroenterol Hepatol. 2002;17:105–108. doi: 10.1046/j.1440-1746.2002.02573.x. [DOI] [PubMed] [Google Scholar]


