Abstract
AIM: To compare the outcome of hand sewing and stapling for anastomotic leakage after esophagectomy.
METHODS: A rigorous study protocol was established according to the recommendations of the Cochrane Collaboration. An electronic database search, hand search, and reference search were used to retrieve all randomized controlled trials that compared hand-sewn and mechanical esophagogastric anastomoses.
RESULTS: This study included 15 randomized controlled trials with a total of 2337 patients. The results revealed that there was no significant difference in the incidence of anastomotic leakage between the methods [relative risk (RR) = 0.77, 95% confidence interval (CI): 0.57-1.04; P = 0.09], but a subgroup analysis yielded a significant difference for the sutured layer and year of publication (Ps < 0.05). There was also no significant difference in the incidence of postoperative mortality (RR = 1.52, 95%CI: 0.97-2.40; P = 0.07). However, the anastomotic strictures rate was increased in the stapler group compared with the hand-sewn group (RR = 1.45, 95%CI: 1.11-1.91; P < 0.01) in the end-to-side subgroup, while the incidence of anastomotic strictures was decreased (RR = 0.34, 95%CI: 0.16-0.76; P < 0.01) in the side-to-side subgroup.
CONCLUSION: The stapler reduces the anastomotic leakage rate compared with hand sewing. End-to-side stapling increases the risk of anastomotic strictures, but side-to-side stapling decreases the risk.
Keywords: Anastomotic leakage, Esophagectomy, Hand-sewn sutures, Mechanical sutures, Meta-analysis
Core tip: This was an important meta-analysis comparing the results of hand-sewn and stapling techniques for esophagogastric anastomosis after esophageal cancer resection. We performed some subgroup analyses that suggested some associations with anastomotic leakage: (1) the number of layers sutured (single or double); (2) year of publication (before 2003 vs 2003-2013); and (3) anastomotic sites (intrathoracic or cervical). A better understanding of this may yield a consensus for comparison of anastomotic leakage rate following the two methods of esophagogastric anastomosis after esophagogastrectomy for esophageal cancer.
INTRODUCTION
Esophageal carcinoma is a multifaceted and complex disease process of rapidly rising incidence that exerts an increasing social and financial burden on global healthcare systems[1-3]. Currently, esophagectomy continues to be the standard treatment for esophageal cancer. After esophageal resection for carcinoma, the stomach is commonly used for restoring alimentary continuity. The success of esophagogastric anastomosis is closely correlated with the patient’s outcome, including anastomotic leakage and stricture. Anastomotic leakage is a feared and frequent complication leading to increased hospital stay, and is a significant cause of early postoperative morbidity. Different anastomotic techniques have been described in order to minimize this risk.
Since the development of the mechanical stapler in the 1990s, there have been many reports showing that the stapler decreases the rate of leakage after esophagogastrostomy[4-7]. However, several meta-analyses recently conducted to compare hand-sewn and stapler anastomosis methods have revealed that there is no significant difference in the risk of developing anastomotic leakage, and the stapler method more frequently contributes to the development of anastomotic strictures[8-10]. These meta-analyses had some limitations: (1) they did not include all published randomized controlled trials (RCTs); and (2) the clinical heterogeneity among the included RCTs indicates that several subgroup meta-analyses are needed.
We conducted a systematic review and meta-analysis of RCTs that compared stapler and hand-sewn methods for esophagogastric anastomosis after esophagectomy, and examined the contribution of each method to the occurrence of anastomotic leakage, 30-d mortality, and anastomotic strictures. Subgroup analyses were also performed to evaluate the anastomotic leakage rate between the two methods related to the sutured layers, the anastomotic sites, and the year of publication. Through this pooled analysis, we hope to gain a consensus about treatment options for clinicians regarding esophagogastric anastomosis after esophagectomy.
MATERIALS AND METHODS
Study selection
The rigorous study protocol was established according to the recommendations of the Cochrane Collaboration. Before the meta-analysis, we pre-specified all the objectives, exclusion and inclusion criteria, major outcomes, and the methods used for synthesis to ensure the high quality of this meta-analysis.
Two investigators independently searched the Cochrane Library database Central, Medline, Embase, Chinese Biomedical Database and Chinese Scientific Journals Database (up to December 2013). All RCTs involving patients with esophageal cancer who underwent esophagogastric anastomosis after esophagectomy were included in the analysis. The search terms were “esophagectomy”, “anastomosis”, “esophagus”, “hand-sewn”, “manual”, “stapled”, “mechanical” and “gastric” and MeSH headings “anastomosis”, “hand-sewn”, “manual”, “stapled”, “mechanical” and “esophagectomy” were used in combination with the Boolean operators AND or OR. The electronic search was supplemented by a hand search of published abstracts from conference proceedings including the International Society for Diseases of the Esophagus, the China Esophageal Society Meeting, United European Gastroenterology Week, and some Surgery Associations. In reference searches, we scanned lists of trials that were selected from electronic searching to identify further associative trials. The two investigators independently obtained and reviewed copies of these full articles according to the inclusion criteria of this study. When disagreement occurred in the trial selection, it was discussed with another author to reach consensus.
Data collection and outcomes
Data were extracted by the two investigators using standardized forms. The quality of all selected articles was ranked in accordance with the Jadad composite scale[11]. According to this scale, low quality studies had a score ≤ 2 and high quality studies had a score ≥ 3.
The primary outcome measure for the meta-analysis was anastomotic leakage. The secondary outcome measures were 30-d mortality and anastomotic strictures (developing within 6 mo of operation and requiring endoscopy).
Statistical analysis
Statistical analysis was performed by RevMan version 5.2.9 (provided by the Cochrane Collaboration, Oxford, United Kingdom). The data extracted from the included trials were combined and the relative risk (RR) was calculated with 95% confidence intervals (CIs). The Cochran’s Q statistic (χ2 test) and the Higgins I2 statistic were used to determine the percentage of total variations across studies due to heterogeneity. If the I2 statistic was ≤ 50%, the fixed effect model was used to pool studies, otherwise, the random effects model was used. To examine clinical heterogeneity, the following subgroup analyses were conducted to evaluate the anastomotic leakage: (1) the site of anastomosis (intrathoracic vs cervical); (2) year of publication (2003-2013 vs before 2003); and (3) double or single suture layer for the hand-sewn method. For obvious clinical heterogeneity, we performed two subgroup analyses (side-to-side stapler vs hand-sewn, and end-to-side stapler vs hand-sewn) to evaluate the anastomotic stricture.
RESULTS
Characteristics of included trials
Fifteen RCTs (2337 patients) that met the inclusion criteria were identified; all were performed between 1990 and 2013[5,12-26] (Figure 1). Table 1 shows the details for each trial, including baseline characteristics, year of publication, anastomotic method, and Jadad score.
Figure 1.
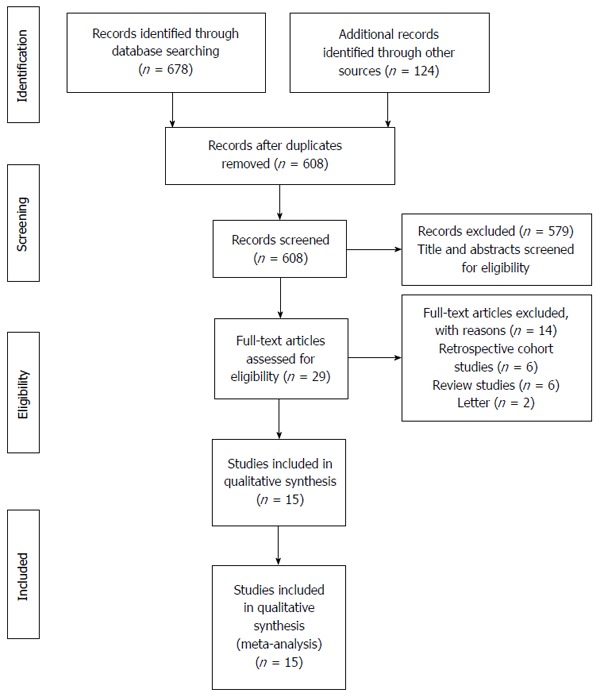
Flow chart of the literature search according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.
Table 1.
Study characteristics
| Ref. | Year | Anastomostic methods | No. of patients | Male/female | Mean age (yr) | Jadad score |
| Fok et al[4] | 1991 | Hand-sewn | 25 | Details unknown | 63.7 | 2 |
| Stapler | 27 | 65.3 | ||||
| Valverde et al[26] | 1996 | Hand-sewn | 74 | 67/7 | 59 | 3 |
| Stapler | 78 | 71/7 | 59 | |||
| Craig et al[25] | 1996 | Hand-sewn | 50 | 27/23 | 65 | 2 |
| Stapler | 50 | 34/16 | 65 | |||
| Law et al[24] | 1997 | Hand-sewn | 61 | 54/7 | 64 | 2 |
| Stapler | 61 | 53/8 | 64 | |||
| Laterza et al[23] | 1999 | Hand-sewn | 21 | 4/17 | 50.9 | 3 |
| Stapler | 20 | 3/17 | 51.9 | |||
| Walther et al[22] | 2003 | Hand-sewn | 41 | 28/13 | 68 | 3 |
| Stapler | 42 | 23/13 | 66 | |||
| Hsu et al[21] | 2004 | Hand-sewn | 32 | 27/5 | 63 | 2 |
| Stapler | 31 | 30/1 | 61 | |||
| Okuyama et al[19] | 2007 | Hand-sewn | 18 | 16/2 | 64.3 | 2 |
| Stapler | 14 | 13/1 | 63.6 | |||
| Luechakiettisak et al[18] | 2008 | Hand-sewn | 59 | 50/9 | 63.6 | 2 |
| Stapler | 58 | 48/10 | 62 | |||
| Aquino et al[17] | 2009 | Hand-sewn | 15 | Details unknown | 45.6 | 3 |
| Stapler | 15 | 45.6 | ||||
| Zhang et al[15] | 2010 | Hand-sewn | 244 | 142/102 | 60 | 2 |
| Stapler | 272 | 158/114 | 59 | |||
| Wu et al[20] | 2005 | Hand-sewn | 154 | 122/32 | 54 | 3 |
| Stapler | 162 | 116/46 | 55 | |||
| Saluja et al[13] | 2012 | Hand-sewn | 87 | 54/33 | 50.9 | 3 |
| Stapler | 87 | 61/26 | 51.4 | |||
| Cayi et al[14] | 2012 | Hand-sewn | 125 | 92/33 | 56 | 2 |
| Stapler | 102 | 79/31 | 59 | |||
| Wang et al[12] | 2013 | Hand-sewn | 52 | 27/5 | 60.8 | 3 |
| Stapler | 92 | 30/1 | 58.9 |
Anastomotic leakage
All 15 trials reported the incidence of anastomotic leakage following surgery. There was no significant difference in anastomotic leakage between the two groups (RR = 0.77, 95%CI: 0.57-1.04; P = 0.09) (Figure 2). Statistical heterogeneity was not detected (I2 = 17%, χ2 = 16.8, df = 14; P = 0.27). The subgroup analyses yielded significant differences for the number of suture layers for the hand-sewn method and the year of publication (Figure 3). One subgroup analysis found that the stapler method had an obvious benefit over the single-layer hand-sewn method in reducing the incidence of postoperative anastomotic leakage (RR = 0.37, 95%CI: 0.18-0.76; P < 0.01); however, there was no benefit when compared with the double-layer hand-sewn method (RR = 1.01, 95%CI: 0.66-1.53; P = 0.98). Another subgroup analysis showed that during the latest decade, the stapler method was superior to the hand-sewn method in preventing anastomotic leakage (RR = 0.66, 95%CI: 0.45-0.96; P = 0.03). The subgroup analysis of anastomotic site yielded no significant difference in anastomotic leakage between the two groups (RR = 1.23, 95%CI: 0.70-2.18; P = 0.47).
Figure 2.
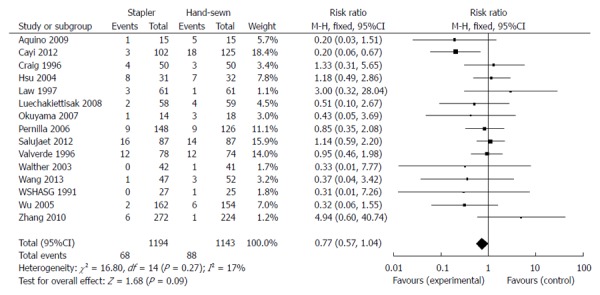
Forest plot for anastomotic leakage. Fifteen studies were included.
Figure 3.
Subgroup analyses for anastomotic site, number of suture layers in the hand-sewn method, and year of publication.
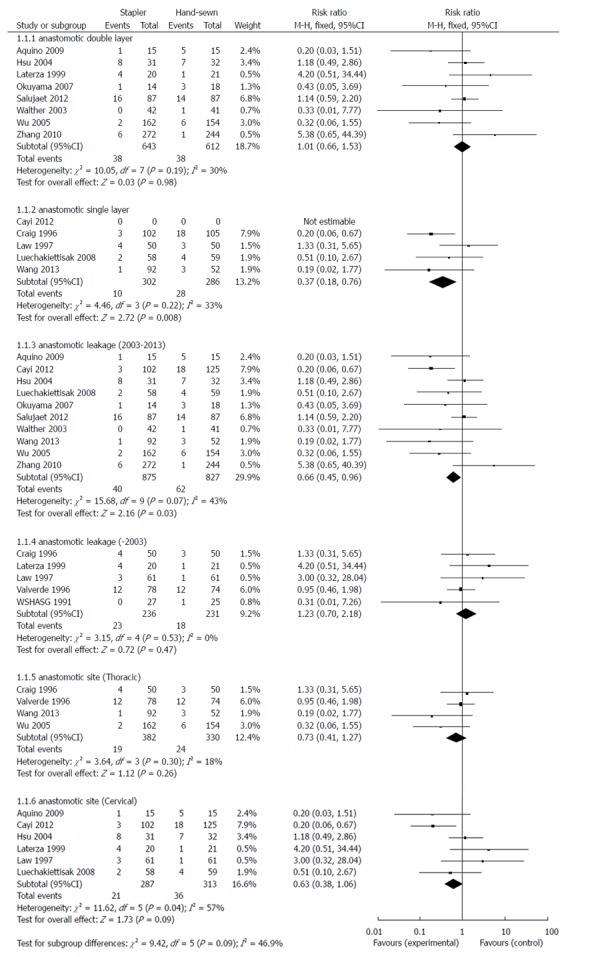
Thirty-day mortality
Fourteen trials reported the incidence of 30-d mortality, with no significant difference observed following stapled vs hand-sewn anastomosis (RR = 1.52, 95%CI: 0.97-2.40; P = 0.07) (Figure 4). There was no evidence of statistical heterogeneity (I2 = 0%, χ2 = 8.17, df = 9; P = 0.52).
Figure 4.
Forest plot for 30-d mortality. Fifteen studies were included.
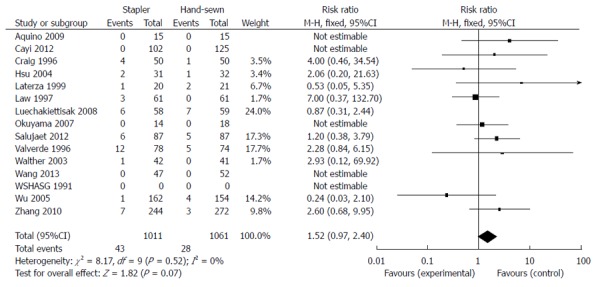
Anastomotic strictures
Fourteen studies reported the incidence of anastomotic stricture following surgery. Because there was obvious clinical heterogeneity present in these studies, we performed two subgroup-analyses. In one analysis, there was a significant increase in the incidence of anastomotic stricture following end-to-side stapled anastomosis compared with hand-sewn anastomosis (RR = 1.45, 95%CI: 1.11-1.91; P < 0.01) (Figure 5). However, in the other analysis, side-to-side stapled anastomosis contributed to reducing the incidence of anastomotic stricture compared with hand-sewn anastomosis (RR = 0.34, 95%CI: 0.16-0.76: P < 0.01).
Figure 5.
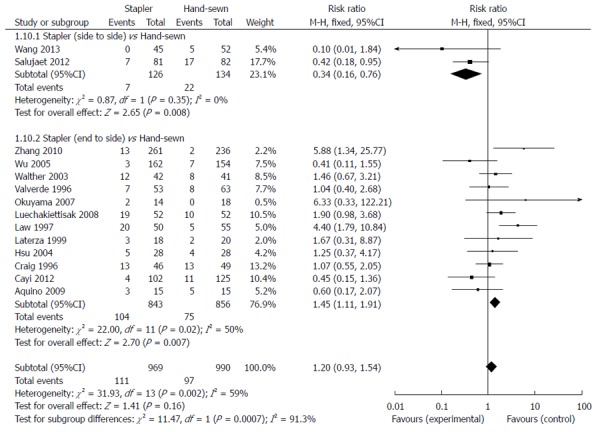
Forest plot for anastomotic strictures including two subgroup analyses.
DISCUSSION
Since the 1990s, the use of the stapler for esophagogastric anastomosis has become increasingly popular. However, compared with the routine hand-sewn method, the superiority of the stapler method is still controversial. Anastomotic leakage is one of the main postoperative complications that is associated with a high mortality rate. Since the development of the mechanical stapler, there have been many reports to show that the stapler can decrease the rate of leakage after esophagogastrostomy[6,7,27,28]. Also, several RCTs have shown that mechanical suturing is as adequate as manual suturing, leading to a lower incidence of anastomosis leakage.
The results of this study revealed that there is no significant difference between the hand-sewn and stapler groups in the incidence of developing anastomotic leakage. However, the subgroup analyses revealed two important findings. First, the use of a stapler method contributed to a reduced anastomotic leakage rate over the last decade. Second, the stapler was superior to the single-layer hand-sewn method in preventing postoperative anastomotic leakage.
For this study, we made attempts wherever possible to follow the recommendations of the Cochrane Collaboration. A rigorous study protocol was pre-specified and several electronic databases, references, and international conference abstracts for relevant trials, were searched without restrictions on language. Several pooled analyses on this topic have demonstrated a similar incidence of anastomotic leakage between the two groups[8,9,29,30]. These pooled analyses either did not attempt to produce subgroup analyses or they did not include an adequate number of publications. The largest number of RCTs to date was included in the present study, and through subgroup analyses, we also examined the contribution of the site of anastomosis, the number of suture layers for the hand-sewn method, and the year of publication as effect modifiers. A major merit of this study was that we performed the analyses by the pre-specified protocol that closely adhered to the Cochrane Collaboration. Therefore, repeating the meta-analysis might achieve a consensus with statistically greater power and better quality of analysis for surgeons with regard to the method of esophagogastric anastomosis after esophagectomy.
Although all the studies met our inclusion criteria, to some extent, this meta-analysis showed heterogeneity; the suture materials and the surgical techniques varied among the studies. We specifically selected three main factors that were suspected as effective modifiers. First, despite the methods of esophagogastric anastomosis, there was no consensus on whether the site of anastomosis (intrathoracic or cervical) affected the outcome of esophagectomy. Second, it is still controversial whether the stapler method is more effective in preventing anastomotic leakage than either single-layer or double-layer suturing methods. Third, although stapler technology has improved over the past 20 years, and has matured during the current decade, and whether year of publication affects the outcome is unclear[14,24]. To make these potential problems clear, we performed subgroup analyses that were stratified by such techniques.
The primary outcome measures from our meta-analysis demonstrated that there was no significant difference between the two groups for anastomotic leakage. However, in one subgroup analysis, there was a significantly decreased incidence of anastomotic leakage compared with hand-sewn anastomosis in 2003-2013. In another subgroup analysis, stapling was significantly superior to the single-layer hand-sewn method in reducing anastomotic leakage. For secondary outcome measures, the difference identified between the hand-sewn and stapler groups was increased anastomotic stricture in the end-to-side stapling group, while there was decreased anastomotic stricture in the side-to-side stapling group.
CONCLUSION
The results of our meta-analysis suggest that stapler anastomosis should remain the first option, because it can significantly reduce the anastomotic leakage. Furthermore, application of the stapler is usually easy and standardized, such that it should not increase the incidence of technical errors. In contrast, hand-sewn methods require surgical expertise and may not be practicable everywhere. Although in this meta-analysis the end-to-side stapler method was associated with the risk of postoperative anastomotic stricture, several new mechanical anastomosis methods (including side-to-side stapling) have been used to resolve this problem[30,31].
COMMENTS
Background
Currently, the standard treatment for esophageal cancer continues to be esophagectomy. Hand-sewn and stapler anastomosis are two major methods for esophagogastric anastomosis after esophagectomy. The purpose of this meta-analysis was to compare the outcomes from hand-sewn and stapler methods for esophagogastric anastomosis after esophagectomy by pooling all data from relevant randomized controlled trials (RCTs), to reach a consensus for comparison of anastomotic leakage.
Research frontiers
Several meta-analyses undertaken to compare hand-sewn and stapler anastomosis methods revealed that there was no significant difference in the risk of developing anastomotic leakage, and that stapler anastomosis contributed more frequently to the development of anastomotic strictures.
Innovations and breakthroughs
Previous meta-analyses did not include all published RCTs, and there is clinical heterogeneity among the ones that were included, indicating that several subgroup meta-analyses are needed. The study presented here is believed to be the first meta-analysis to include subgroup analyses, which indicate an association between anastomotic leakage and: (1) the number of layers sutured; (2) year of publication; and (3) the anastomotic site.
Applications
The results suggest that the stapler method reduces the anastomotic leakage rate compared with the single-layer hand-sewn method. In addition, although the end-to-side stapler method increased the risk of anastomotic strictures, the side-to-side stapler was associated with a decreased rate.
Terminology
Hand-sewn anastomosis is the esophagogastric anastomosis performed by hand with interrupted absorbable monofilament sutures. Stapler anastomosis means that the esophagogastric anastomosis is performed using circular or linear staplers.
Peer review
This is a nicely written manuscript and the analyses seem to be well performed. The topic of the esophagogastric anastomosis is not really new, but it is still one of the mainly important problems in esophageal surgery.
Footnotes
P- Reviewer: dos Santos JS, Furka A, Nozaki INA, Reeh M, Smith RC S- Editor: Ma YJ L- Editor: AmEditor E- Editor: Wang CH
References
- 1.Biere SS, van Berge Henegouwen MI, Maas KW, Bonavina L, Rosman C, Garcia JR, Gisbertz SS, Klinkenbijl JH, Hollmann MW, de Lange ES, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet. 2012;379:1887–1892. doi: 10.1016/S0140-6736(12)60516-9. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 3.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64:9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 4.Fok M, Ah-Chong AK, Cheng SW, Wong J. Comparison of a single layer continuous hand-sewn method and circular stapling in 580 oesophageal anastomoses. Br J Surg. 1991;78:342–345. doi: 10.1002/bjs.1800780323. [DOI] [PubMed] [Google Scholar]
- 5.Suturing or stapling in gastrointestinal surgery: a prospective randomized study. West of Scotland and Highland Anastomosis Study Group. Br J Surg. 1991;78:337–341. doi: 10.1002/bjs.1800780322. [DOI] [PubMed] [Google Scholar]
- 6.Kondra J, Ong SR, Clifton J, Evans K, Finley RJ, Yee J. A change in clinical practice: a partially stapled cervical esophagogastric anastomosis reduces morbidity and improves functional outcome after esophagectomy for cancer. Dis Esophagus. 2008;21:422–429. doi: 10.1111/j.1442-2050.2007.00792.x. [DOI] [PubMed] [Google Scholar]
- 7.McManus KG, Ritchie AJ, McGuigan J, Stevenson HM, Gibbons JR. Sutures, staplers, leaks and strictures. A review of anastomoses in oesophageal resection at Royal Victoria Hospital, Belfast 1977-1986. Eur J Cardiothorac Surg. 1990;4:97–100. doi: 10.1016/1010-7940(90)90222-l. [DOI] [PubMed] [Google Scholar]
- 8.Honda M, Kuriyama A, Noma H, Nunobe S, Furukawa TA. Hand-sewn versus mechanical esophagogastric anastomosis after esophagectomy: a systematic review and meta-analysis. Ann Surg. 2013;257:238–248. doi: 10.1097/SLA.0b013e31826d4723. [DOI] [PubMed] [Google Scholar]
- 9.Markar SR, Karthikesalingam A, Vyas S, Hashemi M, Winslet M. Hand-sewn versus stapled oesophago-gastric anastomosis: systematic review and meta-analysis. J Gastrointest Surg. 2011;15:876–884. doi: 10.1007/s11605-011-1426-9. [DOI] [PubMed] [Google Scholar]
- 10.Markar SR, Arya S, Karthikesalingam A, Hanna GB. Technical factors that affect anastomotic integrity following esophagectomy: systematic review and meta-analysis. Ann Surg Oncol. 2013;20:4274–4281. doi: 10.1245/s10434-013-3189-x. [DOI] [PubMed] [Google Scholar]
- 11.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 12.Wang WP, Gao Q, Wang KN, Shi H, Chen LQ. A prospective randomized controlled trial of semi-mechanical versus hand-sewn or circular stapled esophagogastrostomy for prevention of anastomotic stricture. World J Surg. 2013;37:1043–1050. doi: 10.1007/s00268-013-1932-x. [DOI] [PubMed] [Google Scholar]
- 13.Saluja SS, Ray S, Pal S, Sanyal S, Agrawal N, Dash NR, Sahni P, Chattopadhyay TK. Randomized trial comparing side-to-side stapled and hand-sewn esophagogastric anastomosis in neck. J Gastrointest Surg. 2012;16:1287–1295. doi: 10.1007/s11605-012-1885-7. [DOI] [PubMed] [Google Scholar]
- 14.Cayi R, Li M, Xiong G, Cai K, Wang W. [Comparative analysis of mechanical and manual cervical esophagogastric anastomosis following esophagectomy for esophageal cancer] Nanfang Yike Daxue Xuebao. 2012;32:908–909. [PubMed] [Google Scholar]
- 15.Zhang YS, Gao BR, Wang HJ, Su YF, Yang YZ, Zhang JH, Wang C. Comparison of anastomotic leakage and stricture formation following layered and stapler oesophagogastric anastomosis for cancer: a prospective randomized controlled trial. J Int Med Res. 2010;38:227–233. doi: 10.1177/147323001003800127. [DOI] [PubMed] [Google Scholar]
- 16.Ma RD, Zhang WT, Xu QR, Chen LQ. [Esophagogastrostomy by side-to-side anastomosis in prevention of anastomotic stricture: a randomized clinical trial] Zhonghua Waike Zazhi. 2010;48:577–581. [PubMed] [Google Scholar]
- 17.Aquino JL, Camargo JG, Said MM, Merhi VA, Maclellan KC, Palu BF. [Cervical esophagogastric anastomosis evaluation with a mechanical device versus manual suture in patients with advanced megaesophagus] Rev Col Bras Cir. 2009;36:19–23. doi: 10.1590/s0100-69912009000100006. [DOI] [PubMed] [Google Scholar]
- 18.Luechakiettisak P, Kasetsunthorn S. Comparison of hand-sewn and stapled in esophagogastric anastomosis after esophageal cancer resection: a prospective randomized study. J Med Assoc Thai. 2008;91:681–685. [PubMed] [Google Scholar]
- 19.Okuyama M, Motoyama S, Suzuki H, Saito R, Maruyama K, Ogawa J. Hand-sewn cervical anastomosis versus stapled intrathoracic anastomosis after esophagectomy for middle or lower thoracic esophageal cancer: a prospective randomized controlled study. Surg Today. 2007;37:947–952. doi: 10.1007/s00595-007-3541-5. [DOI] [PubMed] [Google Scholar]
- 20.Wu YS, Ye M, Ma LY. Mechanical compared with hand-sewn Esophagogastric Anastomosis after esophagectomy for esophageal cancer. Zhonghua Weichang Waike Zazhi. 2005;8:367–368. [Google Scholar]
- 21.Hsu HH, Chen JS, Huang PM, Lee JM, Lee YC. Comparison of manual and mechanical cervical esophagogastric anastomosis after esophageal resection for squamous cell carcinoma: a prospective randomized controlled trial. Eur J Cardiothorac Surg. 2004;25:1097–1101. doi: 10.1016/j.ejcts.2004.02.026. [DOI] [PubMed] [Google Scholar]
- 22.Walther B, Johansson J, Johnsson F, Von Holstein CS, Zilling T. Cervical or thoracic anastomosis after esophageal resection and gastric tube reconstruction: a prospective randomized trial comparing sutured neck anastomosis with stapled intrathoracic anastomosis. Ann Surg. 2003;238:803–812; discussion 812-814. doi: 10.1097/01.sla.0000098624.04100.b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Laterza E, de’ Manzoni G, Veraldi GF, Guglielmi A, Tedesco P, Cordiano C. Manual compared with mechanical cervical oesophagogastric anastomosis: a randomised trial. Eur J Surg. 1999;165:1051–1054. doi: 10.1080/110241599750007883. [DOI] [PubMed] [Google Scholar]
- 24.Law S, Fok M, Chu KM, Wong J. Comparison of hand-sewn and stapled esophagogastric anastomosis after esophageal resection for cancer: a prospective randomized controlled trial. Ann Surg. 1997;226:169–173. doi: 10.1097/00000658-199708000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Craig SR, Walker WS, Cameron EW, Wightman AJ. A prospective randomized study comparing stapled with handsewn oesophagogastric anastomoses. J R Coll Surg Edinb. 1996;41:17–19. [PubMed] [Google Scholar]
- 26.Valverde A, Hay JM, Fingerhut A, Elhadad A. Manual versus mechanical esophagogastric anastomosis after resection for carcinoma: a controlled trial. French Associations for Surgical Research. Surgery. 1996;120:476–483. doi: 10.1016/s0039-6060(96)80066-3. [DOI] [PubMed] [Google Scholar]
- 27.Ercan S, Rice TW, Murthy SC, Rybicki LA, Blackstone EH. Does esophagogastric anastomotic technique influence the outcome of patients with esophageal cancer? J Thorac Cardiovasc Surg. 2005;129:623–631. doi: 10.1016/j.jtcvs.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 28.Urschel JD, Blewett CJ, Bennett WF, Miller JD, Young JE. Handsewn or stapled esophagogastric anastomoses after esophagectomy for cancer: meta-analysis of randomized controlled trials. Dis Esophagus. 2001;14:212–217. doi: 10.1046/j.1442-2050.2001.00187.x. [DOI] [PubMed] [Google Scholar]
- 29.Kayani B, Garas G, Arshad M, Athanasiou T, Darzi A, Zacharakis E. Is hand-sewn anastomosis superior to stapled anastomosis following oesophagectomy? Int J Surg. 2014;12:7–15. doi: 10.1016/j.ijsu.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 30.Takemura M, Yoshida K, Fujiwara Y. Modified triangulating stapling technique for esophagogastrostomy after esophagectomy for esophageal cancer. Surg Endosc. 2013;27:1249–1253. doi: 10.1007/s00464-012-2586-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Okushiba S, Kawarada Y, Shichinohe T, Manase H, Kitashiro S, Katoh H. Esophageal delta-shaped anastomosis: a new method of stapled anastomosis for the cervical esophagus and digestive tract. Surg Today. 2005;35:341–344. doi: 10.1007/s00595-004-2943-x. [DOI] [PubMed] [Google Scholar]


