Abstract
Background:
Protecting households from risk of impoverishment due to out-of-pocket costs in health care is a major challenge for health systems. Therefore, this study aimed at evaluating some health expenditure of inpatient and outpatient care as well as assessing the predictors of catastrophic costs for inpatient care in one of central provinces of Iran.
Methods:
In this cross-sectional study, 760 household were selected by multistage sampling method in Markazi province of Iran and interviewed in order to complete a standard questionnaire. Catastrophic costs were evaluated in a scale that varied from 0 (no money for care) to 100 (spending all income and wealth). Patients who were paid over 20% of household financial sources or 40% of month income were regarded as being exposed to catastrophic costs. Negative binomial model with robust estimator logit function was used for prediction of catastrophic costs.
Results:
Based on data analysis, 42.6% of hospitalized subjects encountered catastrophic costs. Moreover, 11.2% households faced catastrophic cost among all participated households and 39.3% were reported to need inpatient need care. Multivariate regression model showed that age range 40-59 years and being in the lower levels of wealth index were significant predictors of facing catastrophic costs (P < 0.05).
Conclusions:
Lack of money is the most important cause of un-seeking care. Hospitalizations due to inpatient care needs, household members aged 40-59 years old, especially with chronic diseases and nonrich status of the household were the highest predictors of facing catastrophic costs. Reducing out-of-pocket costs can increase health care utilization.
Keywords: Catastrophic costs, health expenditures, inpatient care, negative binomial model, outpatient care
INTRODUCTION
In each country, the government and health system are responsible for providing sufficient and cost-effective health and curative care.[1] Moreover, increasing the accessibility and utilization of health services are critical for improving health systems.[2] Primary health care is largely financed and delivered by public sector while the secondary and tertiary level care are provided by both public and private in Iran.[3,4] Despite increasing the insurance coverage in Iran, 10-20% of population is not covered by any insurance[3] and according to the WHO report, over 58% of health expenditure is out-of-pocket in 2001.[5]
Protecting households from the risk of impoverishment due to out-of-pocket expenses for health care is a major challenge for health systems. It is because out-of-pocket payments can make some of families face with catastrophic costs and pay an important proportion of income for health care.[2] Sometimes, low cost payment for common illnesses can financially affect the poor households with no insurance to cover catastrophic costs.[6]
Household health expenditure is defined catastrophic when the ratio of the household's out-of-pocket health expenditure and its disposable income goes from 30% or 40% of capacity to pay, or if it reaches 10% of total expenditures.[7,8] Therefore, in developed countries protecting household and people from catastrophic spending by social institutions such as social insurance is established as an ideal goal in health policy.[6]
The out-of-pocket health expenditure varies among countries according to their health policies and insurance coverage from 1.6% of total health expenditure in Niue to 80% in Vietnam, 82.9% in Guinea, and 90% to Cambodia according to the reports.[7,8,9] Based on WHO report, the out-of-pocket cost for health expenditure was 58% in 2001. These costs forced some households below the poverty line due to catastrophic costs.[8] Furthermore, the out-of-pocket costs can even have a preventive effect for seeking and obtaining health care due to financial burden.[2] As such, the aim of this study is to evaluate some specified time and cost expenditure for inpatient and outpatient care as well as assess the predictors of catastrophic costs for inpatient care in Markazi province of Iran.
METHODS
This study was a cross-sectional one in which 760 households was selected by multistage sampling method in Markazi province of Iran. In the first stage, each household was selected based on proportional stratified sampling regarding urban and village population. Then, in each stratum random cluster sampling was used to select the eligible cluster. In the final phase, systematic random sampling was applied to include eligible household according to predefined sample size. The study included those households of which all members were volunteers and if one member was not so, that household was excluded.
Data were collected by a standard questionnaire that had been used previously in health utilization care survey in 2002.[10,11] The interview was conducted with all family members, excluding those subjects who were under 15 years old or unable to respond to the questions. Their mothers or nurses were interviewed. If one of the family members did not fulfill the interview, that household was excluded from sampling. Beside some demographic factors such as age, gender, having insurance and socio-economic variables, the usage of inpatients and outpatient care was asked in the interview sessions. Moreover, data of time spending and cost for receiving care were included in the interview. More details of this method have been described in some of my recent works.[1,4,12] Catastrophic cost was evaluated in a scale that varied from 0 to 100. In this scale, the financial sources for paying inpatient care were assessed as 0 = no cost, 25 = over 50% of household month income, 50 = all household month income, 75 = using saved money or borrowing inside of all income, 100 = selling out all wealth. Catastrophic costs were defined as payment over 40% of total household financial sources for taking inpatient care. However, catastrophic cost has been defined in recent studies as households with over 40% of capacity to pay out-of-pocket for health.[6] In the current study, patients who paid over 20% of household financial sources or 40% of month income were regarded as being exposed to catastrophic costs since data of income and food expenditures were not collected due to poor validity in our study population as is the case in other developing countries.[3] The results of the current study were calculated for 802 and 284 subjects who were reported to need outpatient and inpatient care, respectively.
Statistical analysis
Wealth index was created by principle component analysis (PCA) on 12 asset variables including vehicle, refrigerator, liquid-crystal-display television, indoor and healthy toilet and bathroom, washing and dishwasher machine, microwave oven, mobile, private computer, access to internet, and house ownership. The first component of PCA described 25.4% of total variances. Robust estimator in negative binomial method was used for removing the clustering effect of household and modeling of most important predictors of catastrophic costs, respectively. All data analysis conducted in SPSS Chicago Inc (version 16) software and P value considered at 0.05.
RESULTS
Out of all 760 target household, 758 household were interviewed correctly and 2711 subjects answered the questions (response rate 99.74%). Of all participated households 28.5% (216 households) were reported to have inpatient need for health care at least for one of the family members in the previous year. Overall, 10.5% (284 subjects) of all studied participants had reported in patient need care in the year prior to the interview. 50.7% (144 subjects) of the households with inpatient need were residing in urban areas and 87.3% (248 subjects) were insured. In addition, 35.1% of participants (952 subjects) were reported to have outpatient need for care in the last 2 weeks before the interview. Seeking care for inpatient and outpatient care was 91.5% and 67.4%, respectively. Using care after seeking it for inpatient and outpatient care was 97.6% and 97.7%, respectively for all subjects. The most important causes of not attempting to seek care were lack of money 31.4%, self-treatment 20.9% and lack of time 18.6% for outpatient care and lack of money and family problems for inpatient care.
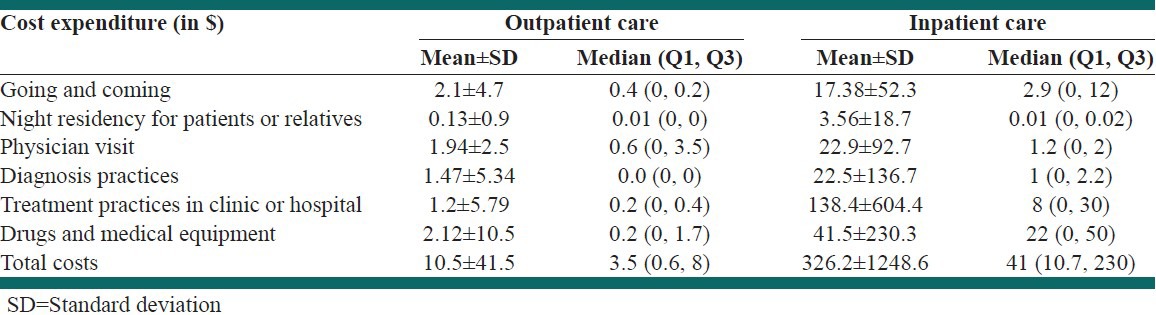
The mean of time expenditure for receiving outpatient care is presented in Table 1 on subjects who were seeking it. According to the results of Table 1, patients who needed outpatient care reached care in 13 min, but the time spent for outpatients care was equal to 105 h approximately. As shown in Table 2, the mean cost expenditure for each outpatient and inpatient care was 10.5$ and 326$, respectively. The highest out-of-pocket cost was related to drugs and medical equipment in the first rank and commuting to/from the clinic for outpatient care while the one related to the hospital treatment costs was the most important cause for out-of-pocket cost in inpatient care.
Table 1.
Time expenditure for receiving outpatient care in subjects whom seeking them
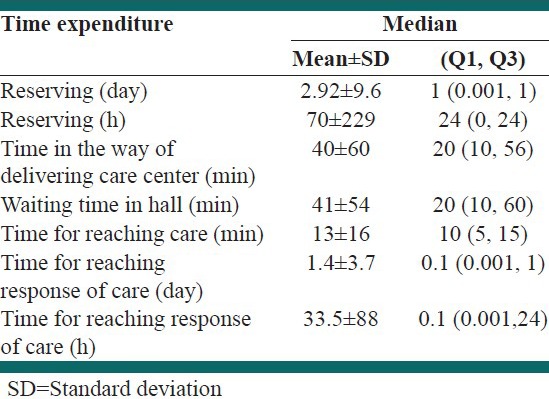
Table 2.
Cost expenditure for receiving outpatient and inpatient care in Dollar
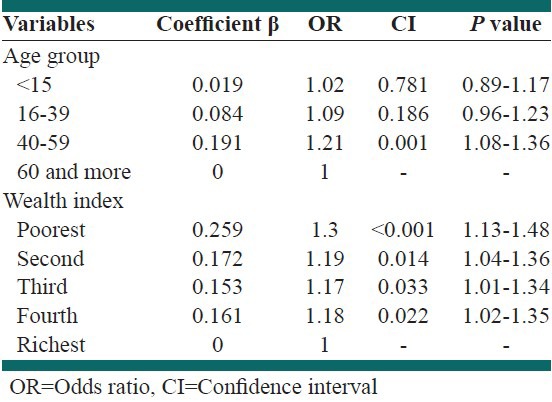
According to the results, 42.6% (121/284) of hospitalized subjects encountered with catastrophic costs. In addition, 11.2% (85/758) households faced catastrophic costs among all participated households and 39.3% (85/216) were reported to need inpatient need care. Negative binomial model results [Table 3] showed that the age range 40-59 years is one of the predictors of facing catastrophic costs (P < 0.05). Furthermore, based on the results only being in the richest level of wealth index did not show a significant relationship with facing catastrophic costs while the other levels of wealth index showed significant association. On the other hand, being in the first to fourth quintile of wealth index was the highest predictor of facing catastrophic costs (P < 0.05). Moreover, being insured, complementary insurance, sex, job type, and educational level did not show any significant association with catastrophic costs (P > 0.05).
Table 3.
Predictors of exposing to catastrophic costs in subjects with inpatient need according to negative binomial model
DISCUSSION
The prevalence of un-using care after seeking it in our study was low and less than 5% for in- and out-patient care. Our results showed that nearly 10% of subjects with inpatient need and 35% of subjects with outpatient need did not seek them due to the lack of money and time. This finding is in accordance with results of another study that has been conducted in Iran.[13] In Hosseinpoor et al., 30.5% of people with outpatient need did not seek it.[13] However, another study showed that around 40% of the population did not seek care from medical providers after the need.[2] These results are the same as our results.
According to our definition, 11.2% of all participated households and 39.3% of households with hospitalized patients encountered with catastrophic costs. In another study by Kavosi et al. the proportion of household with catastrophic cost was calculated based on Xu method and it was shown to be 11.8% and 12.6% for 2003 and 2007, in Tehran, respectively.[14] Another study in Ghazvin showed that 24% of households experienced catastrophic cost, but only 3% of it was due to hospitalization costs.[15] Furthermore, Gotsadze et al. showed that in Georgia the proportion of catastrophic cost was 11.7% in 2007.[16] These result showed that paying out over 20% of household financial sources or 40% of month income can be defined for catastrophic costs, if data of food expenditure do not exist. Another advantage of using total expenditure is in removing the recall bias during the study for data collection of disposable incomes,[8] since the validity and reliability of these data were not assessed in developing countries.[8] However, another study in Iran estimated that in 2007 only 2.5% of households were exposed to catastrophic cost that was lower than that in other studies.[17] It is a considerable estimate, but the method for calculating this result is different with the above-mentioned studies.
According to binomial negative model, the age range of 40-59 years old was as an important factor for facing catastrophic costs. Other studies also showed the same results.[14,16] However, some studies also showed household members with low age range (younger than 12 years old) can be related to financial health expenditure.[17] Moreover, based on regression results, being in the richest level of wealth index can prevent household from encountering catastrophic costs. The rate of facing catastrophic costs in Uganda was higher in poor people than the nonpoor.[14] Another interesting finding in our data was the increasing trend of odds ratio by decreasing the level of wealth index. However, being in the poorest level of wealth index increases the chance of facing catastrophic health expenditure up to 48% while being in the second, third, or fourth level increases this chance up to 36%. According to the results, it is concluded that poor people are more susceptible to poverty from catastrophic health expenditure. This truth is shown in other national and international studies.[3,6,9,16,17]
Furthermore, the most important factors determining the financial catastrophe health expenditures in our study are hospitalization due to inpatient care need; household members aged 40-59 years old especially with chronic diseases and nonrich status of the household. This is as the same as the other results of Gotsadze et al. study in Georgia.[16]
However, our results showed that only 8.5% of subjects with inpatient need did not seek it; however, it is considerable that the most important factor for un-seeking care was reported to be lack of money. Therefore, in our study and other studies evaluating hospitalized patients, the ratio of households with catastrophic health expenditure was underestimated.
Household capacity to pay is not considered as its total effective income, but as defined as effective income after providing subsistence needs.[18] Since the data of income in developing countries is not reliable and valid, expenditure cost is suggested as a surrogate variable. However, in the current study, we have not subsistence expenditure to calculate the average food expenditure for the 45th and 55th percentile households that were suggested by Cavagnero et al.[2,6] Moreover, the monitoring and tracing the change in out-of-pocket health expenditure and catastrophic cost is very difficult and limited due to cultural and methodological issues.[8] However, this study could reflect some health expenditure for inpatient and outpatient care in Iran based on a national survey data. In addition, the amount of expenditure costs for in- and out-patient care is determined regarding each service, separately. Furthermore, based on these results, the lack of money was the most important factor for un-seeking care and the most of out-of-pocket cost was related to drugs and medical equipment. Hence, the government and ministry of health should enforce the insurance companies to increase the financial coverage of drugs and medical equipment. This policy helps people increase health care utilization and decrease the out-of-pocket cost. However, we could not determine the costs for outpatient care due to lack of data. And because gathering data from all provinces was inaccessible, the generalizability of these finding is restricted.
CONCLUSIONS
The utilization of in- and out-patient care after seeking it is high. The most important causes of un-seeking care are lack of money and time, self-treatment and family problems. The rate of patients with catastrophic health expenditure is higher than that in the developed countries. Hospitalization due to inpatient care needs, household members aged 40-59 years old especially with chronic diseases and nonrich status of the household are the strong predictors of facing catastrophic costs.
ACKNOWLEDGMENTS
The authors would like to thank all the interviewers and the participants who cooperated in data collection as well as all the engaged staff of Department of Health in Markazi province. Mr. A. Omidi-Oskouei is, also, appreciated for his ongoing assistance in the English editing of the paper.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hassanzadeh J, Mohammadbeigi A, Eshrati B, Rezaianzadeh A, Rajaeefard A. Determinants of inequity in health care services utilization in Markazi province of Iran. Iran Red Crescent Med J. 2013;15:363–70. doi: 10.5812/ircmj.3525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cavagnero E, Carrin G, Xu K, Aguilar-Rivera AM. Health financing in Argentina: An empirical study of health care expenditure and utilization. Innovations in Health Financing, Working Paper Series. 2006;(8) [Google Scholar]
- 3.Kavosi Z, Rashidian A, Pourreza A, Majdzadeh R, Pourmalek F, Hosseinpour AR, et al. Inequality in household catastrophic health care expenditure in a low-income society of Iran. Health Policy Plan. 2012;27:613–23. doi: 10.1093/heapol/czs001. [DOI] [PubMed] [Google Scholar]
- 4.Mohammadbeigi A, Hassanzadeh J, Eshrati B, Rezaianzadeh A. Decomposition of inequity determinants of healthcare utilization, Iran. Public Health. 2013;127:661–7. doi: 10.1016/j.puhe.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 5.WHO. Health System Profile: Islamic Republic of Iran Cairo: Regional Health Systems Observatory, WHO Eastern Mediterranean Regional Office. 2006 [Google Scholar]
- 6.Zahraei SM, Gouya MM, Azad TM, Soltanshahi R, Sabouri A, Naouri B, et al. Successful control and impending elimination of measles in the Islamic Republic of Iran. J Infect Dis. 2011;(204 Suppl 1):S305–11. doi: 10.1093/infdis/jir076. [DOI] [PubMed] [Google Scholar]
- 7.Wagstaff A, van Doorslaer E. Catastrophe and impoverishment in paying for health care: With applications to Vietnam 1993-1998. Health Econ. 2003;12:921–34. doi: 10.1002/hec.776. [DOI] [PubMed] [Google Scholar]
- 8.Lu C, Chin B, Li G, Murray CJ. Limitations of methods for measuring out-of-pocket and catastrophic private health expenditures. Bull World Health Organ. 2009;87:238–44. doi: 10.2471/BLT.08.054379. 244A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Damme W, Van Leemput L, Por I, Hardeman W, Meessen B. Out-of-pocket health expenditure and debt in poor households: Evidence from Cambodia. Trop Med Int Health. 2004;9:273–80. doi: 10.1046/j.1365-3156.2003.01194.x. [DOI] [PubMed] [Google Scholar]
- 10.Naghavi M, Jamshidi HR, Jafari N, Farzadfar F, Khosravi Am R, Ahbar M, et al. Tehran: Tandis Publication; 2011. Health Care Utilization Iran 2002. [Google Scholar]
- 11.Ministry of Health and Medical Education. 1st ed. Tehran: Ministry Health and Medical Education Publication; 2008. Guideline for Conducting Health Care Utilization Survey. [Google Scholar]
- 12.Mohammadbeigi A, Hassanzadeh J, Eshrati B, Rezaianzadeh A. Socioeconomic inequity in health care utilization, Iran. J Epidemiol Glob Health. 2013;3:139–46. doi: 10.1016/j.jegh.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hosseinpoor AR, Naghavi M, Alavian SM, Speybroeck N, Jamshidi H, Vega J. Determinants of seeking needed outpatient care in Iran: Results from a national health services utilization survey. Arch Iran Med. 2007;10:439–45. [PubMed] [Google Scholar]
- 14.Xu K, Evans DB, Kadama P, Nabyonga J, Ogwal PO, Nabukhonzo P, et al. Understanding the impact of eliminating user fees: Utilization and catastrophic health expenditures in Uganda. Soc Sci Med. 2006;62:866–76. doi: 10.1016/j.socscimed.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 15.Asefzadeh S, Alijanzadeh M, Gholamalipoor S, Farzaneh A. Households Encountering with Catastrophic Health Expenditures in Qazvin, Iran. Health Inf Manage. 2013;10:146–53. [Google Scholar]
- 16.Gotsadze G, Zoidze A, Rukhadze N. Household catastrophic health expenditure: Evidence from Georgia and its policy implications. BMC health services research. 2009;9:69. doi: 10.1186/1472-6963-9-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehrara M, Fazaeli A. Health finance equity in Iran: An analysis of household survey data (1382-1386) J Health Adm. 2010;13:51–62. [Google Scholar]
- 18.Xu K, Klavus J, Evans DB, Hanvoravongchai P, Zeramdini R, Murray CJ. Geneva: World Health Organization; 2003. The impact of vertical and horizontal inequality on the fairness in financial contribution index. Health Systems Performance Assessment: Debates, Methods and Empiricism. [Google Scholar]


