Abstract
Background:
Hypertension and diabetes are major risk factors for cardiovascular and cerebrovascular disease. Adherence is a primary determinant of the effectiveness of treatment because poor adherence attenuates optimum clinical benefit and paves the way for complications.
Methods:
The cross-sectional community-based survey was carried out among men and women aged 30 years and above in the field practice area of a medical college to assess treatment compliance with respect to hypertension and type 2 diabetes mellitus. The study comprised of 426 subjects, already diagnosed with hypertension (287) and type 2 diabetes mellitus (139). During house visits, data were collected by personal face-to-face interview using a pre-tested structured questionnaire. Compliance was determined by indirect methods, which included self-reporting and interviews with the patients.
Results:
Compliance to hypertension treatment was found to be 82.2%, while 83.6% of individuals with type 2 diabetes mellitus were on regular medication. Among the individuals on regular medication, 88 (37.3%) of them had controlled blood pressure. Although the compliance was good, blood pressure control was not optimal. Adherence was better among females as compared with males. Literacy status and socio-economic background were not found to be associated with treatment compliance. High cost of treatment for hypertension (39.3%) and diabetes (30.4%) and asymptomatic nature of the disease were the most common reasons cited for not taking regular medications.
Conclusions:
Adherence to hypertension and diabetes treatment was good. High cost of medications and asymptomatic nature of the disease were the reasons identified among the non-adherent patients.
Keywords: Adherence, hypertension, treatment compliance, type 2 diabetes mellitus
INTRODUCTION
Hypertension, dyslipidemia and diabetes are well-known risk factors for cardiovascular disease (CVD). According to the World Diabetes Atlas, India is projected to have around 51 million people with diabetes.[1] In 2004, the prevalence of diabetes averaged 16% in urban India and only 3% in rural India.[2,3] The prevalence of hypertension in India is reported as ranging from 10% to 30.9%, respectively.[4] At an underestimate, there are 31.5 million hypertensives in rural and 34 million in urban populations.[5]
Large-scale clinical trials have shown that pharmacological treatment can reduce the morbidity and mortality associated with CVD and that long-term or lifelong treatment is often indicated.[6] Given the lack of symptoms for the presence of disease, medication adverse effects become an important factor in non-compliance and non-persistence.[7] Patient compliance or adherence is defined as the extent to which a person's behavior coincides with health-related advice.[8] According to the World Health Organization, non-compliance with long-term medication for chronic conditions is a common problem that leads to compromised health benefits and serious economic consequences.[6] In addition, it has also been identified as the predominant reason for the failure of medical therapy and disease progression.[9]
Patient dissatisfaction with the doctor, poor doctor-patient relationship, or long waiting times to obtain appointments increase the risk of non-compliance. Multiple drug therapy and multiple frequency of dosing also increase the risk of non-compliance.[8] The lack of a patient-friendly, flexible health care system has also been identified as the primary reason for non-compliance.[10] With this background in mind, the study was designed to determine treatment compliance among patients with hypertension and type 2 diabetes mellitus and to determine the factors responsible for non-compliance in a South Indian population. In addition, assessment of the applicability of the rule of halves pertaining to hypertension was the secondary objective for the current study.
METHODS
Study design and participants
The cross-sectional community-based survey was carried out in the field practice area of Department of Community Medicine, of a Medical College, which is situated along the coastal area in the southern part of Karnataka, India. The field practice area covers a population of 45,587 living in 7164 families spread out in 11 villages, along the coastline. Modern medicine facilities are easily accessible to the people in the area, both Government and private. In addition, the Department of Community Medicine provides primary health care to the population, through Rural Maternity and Child Welfare (RMCW) homes, which is provided at no cost to the patients. The study population included all men and women aged 30 years and above. Data were collected over a period of 18 months between 2006 and 2008. The subjects of the study were already diagnosed cases, identified from a prevalence study on type 2 diabetes mellitus and hypertension in the community.[11,12] The diagnosis of hypertension and diabetes was based on patient records, i.e., when the subjects had already been diagnosed with the disease and were taking medications for the same from a physician, they were considered to be cases for the study and no other diagnostic criteria was applied. This comprised of 426 subjects, 287 and 139 hypertensive and diabetic patients respectively.
Study variables and instrument
Institutional ethical committee clearance was obtained prior to the initiation of the study. Written informed consent was obtained from all the subjects. During house visits, data were collected by personal face-to-face interview using a pre-tested structured questionnaire. Main domains of the questionnaire were: Socio-demographic details, nature of treatment, source of health care, regularity of taking prescribed medicines. No scoring system was used. The tool was pilot tested and validity was appraised by experts (consensual validity). Socio-economic status was assessed using modified Pareek and Trivedi scale.[13] Compliance to treatment was determined by indirect methods, which included interviews and self-reporting by the patients. Non-adherence was assessed using patients self-reports of how they had been taking their medication in the week preceding the interview. Patients who reported taking less than 80% of their prescribed medicines were considered to be non-compliant to treatment.
Statistical analysis
Prevalence of diabetes and hypertension are presented as percentages. A Chi-square test was used to compare the compliance considering the different demographic and socio-economic categories. Unadjusted odds ratio (OR) with the 95% confidence interval (95% CI) were calculated for the various socio-demographic characteristics against treatment compliance. The same variables were included for multiple logistic regression analysis using the forward conditional method, with treatment compliance as the dependent variable and the socio-demographic characteristics as the independent variables. All statistical analysis was performed using Statistical Package for Social Sciences (SPSS) version 15.0 from SPSS South Asia Bangalore, India. P <0.05 was considered as significant.
RESULTS
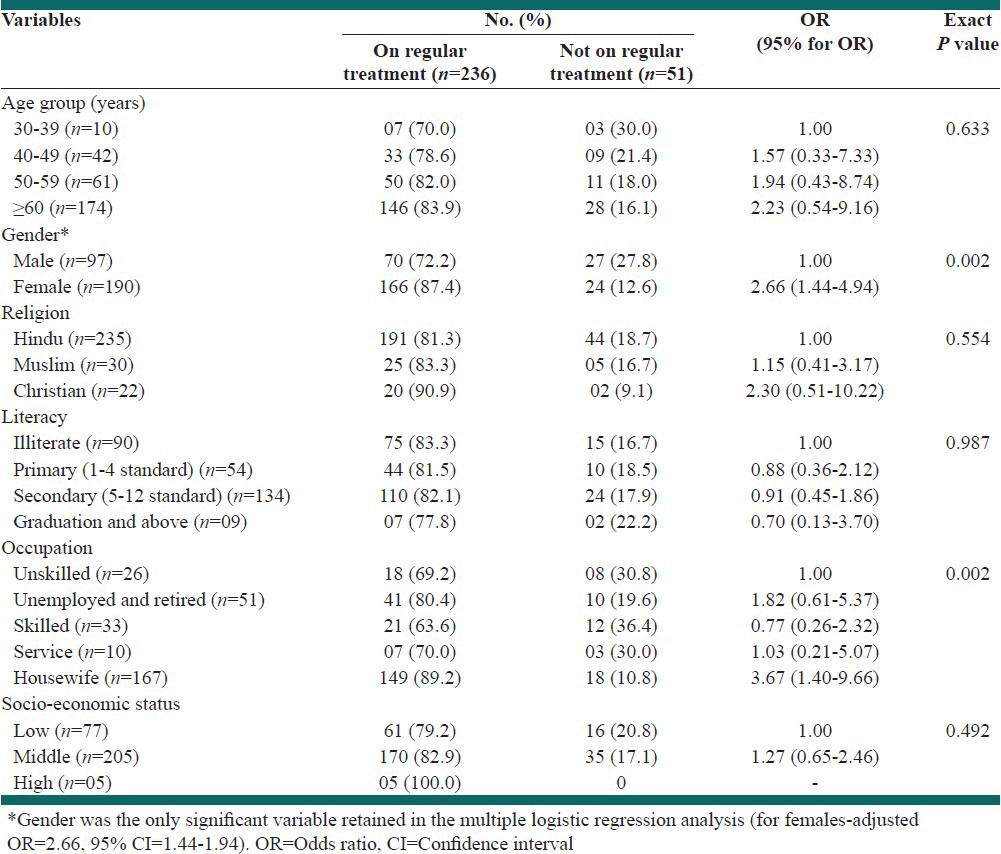
The subjects of the study were already diagnosed cases, identified from a prevalence study on type 2 diabetes mellitus and hypertension in the community.[11,12] This comprised of 426 subjects, 287 and 139 hypertensive and diabetic patients respectively. Among the hypertensive patients 236 (82.2%) were taking regular treatment. Among the individuals on regular medication, 88 (37.3%) of them had controlled blood pressure i.e., <140/90 mmHg. This conveys that although the compliance was good, blood pressure control was still far beyond the optimal target. Among the known cases of diabetes, compliance to treatment was 83.6% (116) and of these 73.5% (86) had random blood sugar (RBS <200 mg/dL) levels at the time of examination. Target for glycemic control have been set for fasting and post prandial blood glucose levels, but there are no set targets for random blood glucose (RBS) level. Hence, the cut-off level of RBS <200 mg/dL, was chosen for the present study. The other reason for selecting this particular cut-off was based on the investigator's convenience as RBS was estimated at the time of the interview for all subjects including diabetics, but irrespective of their RBS values, were not tested further. As fasting and post prandial blood glucose levels were not estimated, standard guidelines were not used to assess treatment compliance. Individuals aged ≥60 years comprised the major proportion 174 (60.6%) of known hypertensives, among whom, 28 (16%) were not taking their medications regularly, as shown in Table 1.
Table 1.
Influence of socio-demographic characteristics on treatment compliance among hypertensive patients (n=287)
Eighty patients (27.5%) were both diabetic and hypertensive. Among the hypertensives, not on regular treatment, 18 (35.3%) had controlled blood pressure, while among the non-compliant diabetics, 16 (69.6%) had RBS <200 mg/dL.
Compliance to hypertension treatment was better among females as compared to males (87.4% vs. 72.2%) and this difference was noted to be statistically significant (χ2= 10.15, P < 0.05, adjusted OR = 2.66, 95% CI = 1.44-1.94). Similar significant difference was also noted with respect to diabetes treatment, as depicted in Table 2.
Table 2.
Influence of socio-demographic characteristics on treatment compliance among diabetic patients (n=139)
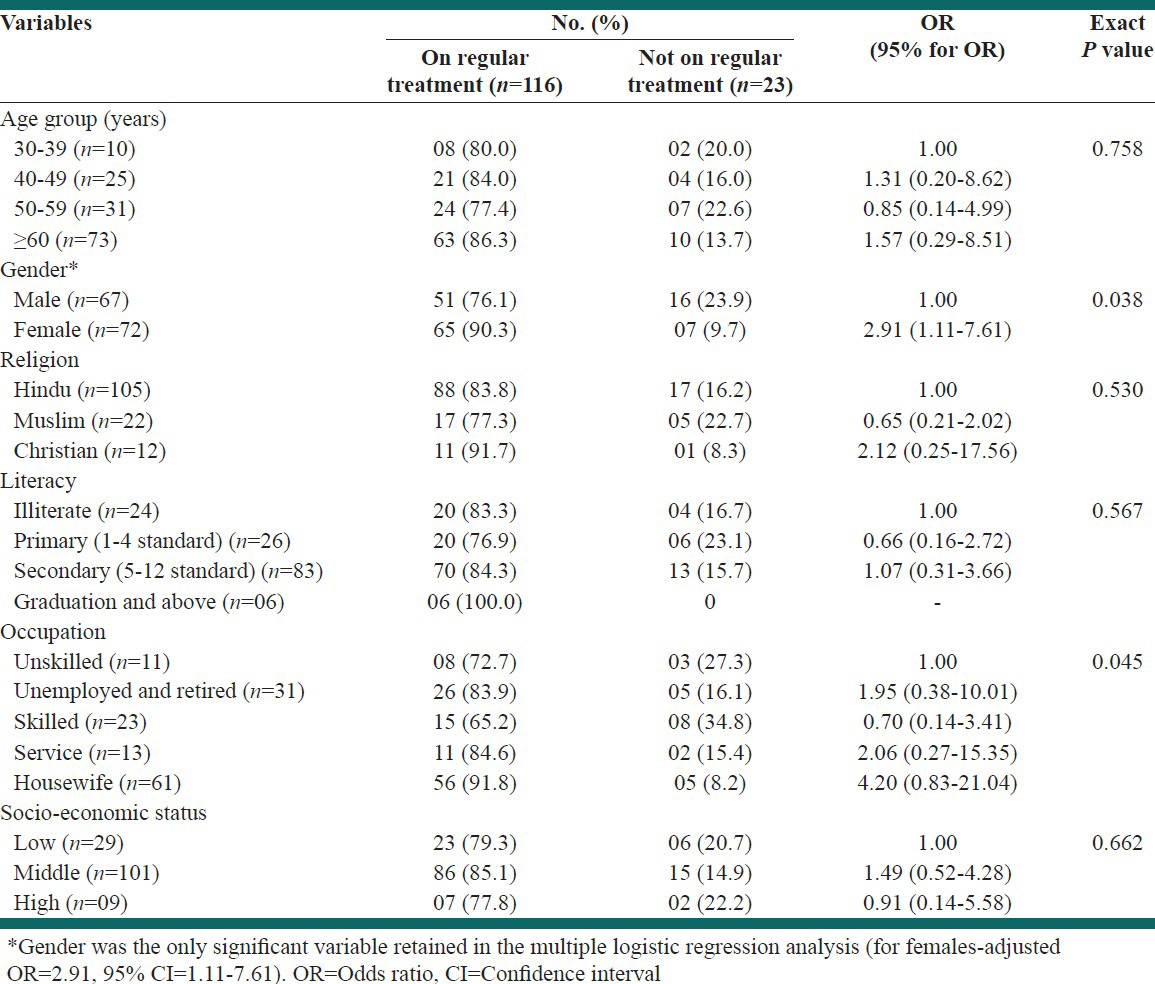
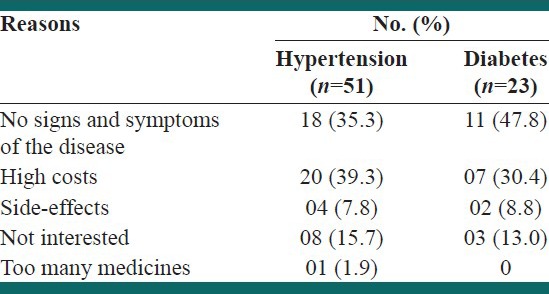
Literacy status and socio-economic background did not have any bearing on adherence to treatment, in our study. Compliance to therapy was more among housewives as compared to other occupation groups, with respect to both hypertension and type 2 diabetes mellitus [Tables 1 and 2]. Univariate analysis of different variables affecting compliance showed that the odds of treatment compliance was higher for hypertensive treatment among housewives, and the odds of compliance was poor among males for both hypertension and diabetes. High cost of treatment for hypertension 20 (39.3%) and diabetes 07 (30.4%) and asymptomatic nature of the disease were the most common reasons cited for not taking regular medications [Table 3]. Nearly, half 11 (47.8%) of the diabetics and 18 (35.3%) of the hypertensives, presumed that the disease was under control, as they had no signs and symptoms and therefore were not taking medicines.
Table 3.
Reasons for non-compliance
DISCUSSION
In the present study, compliance to hypertension treatment was found to be 82.2%, while 83.6% of individuals with type 2 diabetes mellitus were on regular medication. Adherence to treatment was better among females when compared with males. High cost of treatment for hypertension (39.3%) and diabetes (30.4%) and asymptomatic nature of the disease were the most common reasons cited for not taking regular medications.
Treatment adherence for hypertension in the present study was 82%, which is similar to the compliance rate of 88.6% reported among hypertensives attending a hypertension clinic in Kuwait.[14] Others have reported varying compliance rates ranging from 40% to 70%, respectively.[8,15,16] The methods employed in assessing the compliance and the health care delivery system could partly explain the differing rates of compliance.
Contrary to report that diabetic patients are non-adherent to their treatment,[17,18] the present study demonstrated 83.6% of the subjects to be compliant to treatment. Sweileh et al. also noted that diabetic patients had better overall rate of compliance than hypertensive patients.[8] Compliance was 91.5% to anti-diabetic treatment among 59 diabetics, as against 47% to anti-hypertensive treatment among 207 hypertensives, in a cross-sectional study conducted on 560 participants in Delhi.[19] These study findings are in congruence with the present study findings.
The present study has shown that compliance is affected by age. With increasing age, the degree of compliance decreases for several reasons. For example, most of the elderly have memory problems related to age. Furthermore, most elderly patients have vision and hearing problems that might increase the potential of mistakes in taking medications. Another problem with elderly is that most of them have several diseases and take several drugs at the same time which might be confusing.[8] Women were found to be more compliant to treatment than men in our study, but gender was not identified as a significant variable in other studies.[8,14,15] Illiterate patients cannot read or distinguish their medications which increases the risk of errors and non-compliance.[8] However, it was noted that people with education up to secondary level and those with skilled jobs to be non-adherent as compared to other education and occupation groups, while other studies have reported formal education to be influential on patient's rate of compliance.[8,16] This could be partly explained by the overall good literacy rate among this coastal population.
The “rule of halves” for hypertension states that: ‘half the people with high blood pressure are not known, half of those known are not treated and half of those treated are not controlled’. If this rule is valid, then only one in eight of the hypertensive population would be receiving the optimal treatment.[20] An attempt was made to assess the applicability of the rule of halves in the current study. Among the hypertensive subjects, 23% were aware of the condition, of whom 82% of them were on treatment and of these, only 37.3% had their blood pressure under control, which represents 31% of the total hypertensive group. Thus, the “rule of halves” seems to be valid for hypertension in the community, which is concurrent with the findings of another urban South Indian population.[20,21] It has taken 30-40 years of sustained effort to substantially improve hypertension detection and control in western countries, and the rates are still far from optimal.[20] That is to say, in a country like India we have a long way to go, to attain optimum levels of treatment compliance.
Patients receiving treatment for chronic conditions often hold reservations about their drugs and make active decisions about continuing to use them.[22] Among the various reasons for non-compliance, affordability for the drugs, asymptomatic nature of the disease,[14,15,23,24] and side-effects of drugs[14,16] have been commonly documented. The present study findings too were in agreement with the existing literature, with respect to reasons for non-compliance.
The current study was designed to provide an insight into treatment adherence among patients with hypertension and diabetes. Though the study was able to identify factors contributing to lack of compliance, in terms of patient-related (disinterest), condition-related (asymptomatic nature of the disease), therapy-related (cost of drugs), and socio-economic factors (affordability), in-depth review of non-compliance was not done. The other limitation of the study was that only patient's response with respect to treatment adherence was taken and not the ideal pill count method for assessment. Feasibility constraints forced the researchers to adopt this method for assessment. The investigators believe the results reported by the subjects are not falsified, as modern medicine facilities are easily accessible to the people in the area. In addition, the Department of Community Medicine provides primary health care at no cost to the patients, through RMCW homes. In these centers, medications are given to the patients on a weekly basis. Hence, they have to come the following week, if they need medicines. In this regard, the clinic attendance is consistently good, week after week. This could be the contributing factor for the high level of compliance in the present study.
High cost of treatment was cited by the subjects as a deterring factor, indicating that in spite of medicines being provided to the patients, the complex nature of the disease requires multiple drug combinations, some of which patients will have to buy on their own. To summarize, although treatment compliance is good, from the perspective of achieving desirable clinical outcomes, the negative effect of therapeutic non-compliance needs to be minimized and more detailed studies on factors influencing compliance need to be done to fill in the knowledge gap and contribute to formulating strategies for countering non-compliance.
CONCLUSIONS
Compliance to hypertension and type 2 diabetes mellitus treatment was found to be good in the current study. High cost of treatment and asymptomatic nature of the disease were the most common reasons cited for not taking regular medications. To address these issues, it may be recommended that health care professionals involved in the management of hypertension and diabetes need to create greater awareness among their patients in order to foster better control of the disease and improve health outcomes, while the pricing of medications is beyond the control of the treating physician.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Anjana RM, Ali MK, Pradeepa R, Deepa M, Datta M, Unnikrishnan R, et al. The need for obtaining accurate nationwide estimates of diabetes prevalence in India-rationale for a national study on diabetes. Indian J Med Res. 2011;133:369–80. [PMC free article] [PubMed] [Google Scholar]
- 2.Mohan V, Deepa M, Deepa R, Shanthirani CS, Farooq S, Ganesan A, et al. Secular trends in the prevalence of diabetes and impaired glucose tolerance in urban South India – The Chennai Urban Rural Epidemiology Study (CURES-17) Diabetologia. 2006;49:1175–8. doi: 10.1007/s00125-006-0219-2. [DOI] [PubMed] [Google Scholar]
- 3.Diamond J. Medicine: Diabetes in India. Nature. 2011;469:478–9. doi: 10.1038/469478a. [DOI] [PubMed] [Google Scholar]
- 4.Padmavati S. A meta-analysis-National heart institute, New Delhi. Indian Heart J. 2002;54:99–102. [PubMed] [Google Scholar]
- 5.Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens. 2004;18:73–8. doi: 10.1038/sj.jhh.1001633. [DOI] [PubMed] [Google Scholar]
- 6.Cramer JA, Benedict A, Muszbek N, Keskinaslan A, Khan ZM. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: A review. Int J Clin Pract. 2008;62:76–87. doi: 10.1111/j.1742-1241.2007.01630.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halpern MT, Khan ZM, Schmier JK, Burnier M, Caro JJ, Cramer J, et al. Recommendations for evaluating compliance and persistence with hypertension therapy using retrospective data. Hypertension. 2006;47:1039–48. doi: 10.1161/01.HYP.0000222373.59104.3d. [DOI] [PubMed] [Google Scholar]
- 8.Sweileh WM, Aker O, Hamooz S. Rate of compliance among patients with diabetes mellitus and hypertension. An-Najah Univ J Research-A-(Natural Sciences) 2005;19:1–12. [Google Scholar]
- 9.Thrall G, Lip GY, Lane D. Compliance with pharmacological therapy in hypertension: Can we do better, and how? J Hum Hypertens. 2004;18:595–7. doi: 10.1038/sj.jhh.1001722. [DOI] [PubMed] [Google Scholar]
- 10.Srinivas G, Suresh E, Jagadeesan M, Amalraj E, Datta M. Treatment-seeking behavior and compliance of diabetic patients in a rural area of south India. Ann N Y Acad Sci. 2002;958:420–4. doi: 10.1111/j.1749-6632.2002.tb03017.x. [DOI] [PubMed] [Google Scholar]
- 11.Rao CR, Kamath VG, Shetty A, Kamath A. A study on the prevalence of type 2 diabetes in coastal Karnataka. Int J Diabetes Dev Ctries. 2010;30:80–5. doi: 10.4103/0973-3930.62597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rao CR, Kamath VG, Shetty A, Kamath A. High blood pressure prevalence and significant correlates: A quantitative analysis from coastal Karnataka, India. ISRN Preventive Med. 2013. [Last accessed on 2014 Mar 10]. Available from: http://dx.doi.org/10.5402/2013/574973 . [DOI] [PMC free article] [PubMed]
- 13.Pareek U, Trivedi G. New Delhi: Manasayan Publishers; 1995. Manual of Socio-Economic Status Scale (rural) [Google Scholar]
- 14.Al-Mehza AM, Al-Muhailije FA, Khalfan MM, Al-Yahya AA. Drug compliance among hypertensive patients; an area based study. Eur J Genet Med. 2009;6:6–10. [Google Scholar]
- 15.Kumar PN, Halesh LH. Antihypertensive treatment: A study on correlates of non adherence in a tertiary care facility. Int J Biol Med Res. 2010;1:248–52. [Google Scholar]
- 16.Kabir M, Iliyasu Z, Abubakar IS, Jibril M. Compliance to medication among hypertensive patients in Murtala Mohammed Specialist Hospital, Kano, Nigeria. J Community Med Prim Health Care. 2004;16:16–20. [Google Scholar]
- 17.Shah JH, Murata GH, Duckworth WC, Hoffman RM, Wendel CS. Factors affecting compliance in type 2 diabetic patients: Experience from the diabetes outcomes in veterans study (DOVES) Int J Diab Dev Ctries. 2003;23:75–82. [Google Scholar]
- 18.Upadhyay DK, Palaian S, Shankar PR, Mishra P. Knowledge, attitude and practice about diabetes among diabetes patients in Western Nepal. Rawal Med J. 2008;33:8–11. [Google Scholar]
- 19.Laskar A, Sharma N, Bhagat N. Lifestyle disease risk factors in a north Indian community in Delhi. Indian J Community Med. 2010;35:426–8. doi: 10.4103/0970-0218.69279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mohan V, Deepa M, Farooq S, Datta M, Deepa R. Prevalence, awareness and control of hypertension in Chennai – The Chennai Urban Rural Epidemiology Study (CURES-52) J Assoc Physicians India. 2007;55:326–32. [PubMed] [Google Scholar]
- 21.Deepa R, Shanthirani CS, Pradeepa R, Mohan V. Is the ‘rule of halves’ in hypertension still valid? – Evidence from the Chennai Urban Population Study. J Assoc Physicians India. 2003;51:153–7. [PubMed] [Google Scholar]
- 22.Benson J, Britten N. Patients’ decisions about whether or not to take antihypertensive drugs: Qualitative study. BMJ. 2002;325:873. doi: 10.1136/bmj.325.7369.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kale S, Patil A, Mandlecha RH. Compliance and adverse drug effects of antihypertensives in rural India. J Clin Diagn Res. 2011;5:775–9. [Google Scholar]
- 24.Thakur K, Malhotra P, Walia I, Kumar R. Health awareness and treatment compliance of high blood pressure among women in a peri-urban colony of Chandigarh, India. J Indian Med Assoc. 1999;97:217–9. [PubMed] [Google Scholar]


