Abstract
The Japan Diabetes Complications Study, a randomised lifestyle intervention study of type 2 diabetes conducted at 59 institutes throughout Japan that enrolled 2033 eligible patients from January 1995 to March 1996, was directed at: (i) determining the incidence and progression rates of complications of diabetes; (ii) exploring clinical risk factors for complications of diabetes; and (iii) determining the association between lifestyle factors, including diet and physical activity, and complications of diabetes, in addition to comparing, in a randomised manner, the effects on type 2 diabetes of an extensive lifestyle intervention and conventional treatment. The protocol for the study originally specified four study populations according to primary outcomes, consisting of: (1) a macroangiopathy group (N = 1771); (ii) a nephropathy group (N = 1607); (iii) a retinopathy-incident group (N = 1221); and (iv) a retinopathy-progression group (N = 410). The primary outcomes were: (i) development of retinopathy; (ii) progression of retinopathy; (iii) development of overt nephropathy; and (iv) occurrence of macroangiopathic events including proven coronary heart disease and stroke. The study was originally planned to follow patients for 8 years, and an extended follow-up is ongoing. Information about primary outcomes, laboratory tests, and other clinical variables for each patient was collected at a central data centre through an annual report from each investigator. Additionally, extensive lifestyle surveys were conducted at baseline and 5 years after the beginning of the study intervention in both the intervention and conventional treatment groups. A description of the occurrence of complications of diabetes and of all-cause mortality, provided in this paper, demonstrated a clear gender-based difference in cardiovascular disease and all-cause mortality. The data set of the study is not freely available, but collaborative ideas are welcome. Potential collaborators should discuss ideas informally with the principal investigator by e-mail.
Keywords: Cardiovascular disease, dietary survey, nephropathy, physical activity, retinopathy
Why was the cohort set up?
Lifestyle interventions, including those of diet, exercise, or both, play a crucial role in the prevention and care of diabetes, and can prevent type 2 diabetes1 as well as ameliorate glycaemia and other risk factors for complications2–7 in patients with established diabetes. However, the effects of these interventions on complications of diabetes remain unknown, although a few studies have been done8,9 of lifestyle modification in combination with pharmacotherapy for hyperglycaemia, hypertension, and dyslipidaemia in patients with type 2 diabetes. In this context, the Japan Diabetes Complications Study (JDCS) (RCT registration number C000000222 at www.umin.ac.jp), an open-label, randomised clinical trial of Japanese patients with type 2 diabetes, was set up to clarify whether a long-term therapeutic intervention focused mainly on lifestyle education would have an effect on the incidence of events involving macro- and microvascular complications of type 2 diabetes in patients with established type 2 diabetes.10 A primary analysis of the randomised comparison, done at the 8-year follow-up,10 showed that the incidence rate of stroke in the intervention group was significantly lower than in the conventional treatment group [hazard ratio (HR): 0.62, 95% confidence interval (CI): 0.39–0.98, P = 0.04], and that the incidence rates of coronary heart disease, retinopathy, and nephropathy did not differ significantly in the two groups. The JDCS accordingly concluded that lifestyle modification had a significant effect on stroke incidence in patients with established type 2 diabetes.
In addition to the randomised comparison of a long-term therapeutic intervention vs. conventional treatment for type 2 diabetes, the JDCS sought to: (i) determine the incidence and rates of progression of complications of diabetes; (ii) explore clinical risk factors for complications of diabetes; and (iii) determine the association of lifestyle factors, including diet and physical activity, with complications of diabetes. The study therefore included extensive lifestyle surveys at baseline and at 5 years, and an extended follow-up period. This paper reports the findings of the JDCS as an ongoing cohort study.
Who is in the cohort?
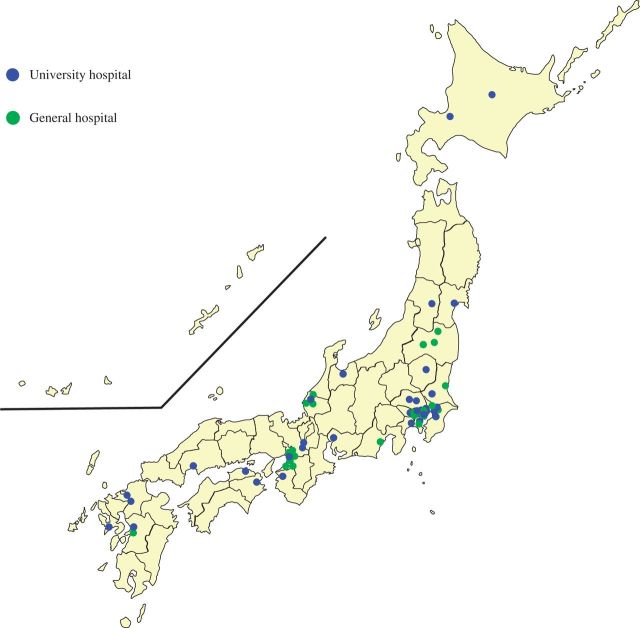
The eligibility criteria for the JDCS were: (i) a previous diagnosis of type 2 diabetes; (ii) an age of 40–70 years; and (iii) a blood concentration of hemoglobin A1C (HbA1C) of ≥ 6.5%. Diabetes mellitus and impaired glucose tolerance (IGT) were diagnosed according to the Report of the Committee of the Japan Diabetes Society on the Classification and Diagnostic Criteria of Diabetes Mellitus, in which the cut-off values for glucose levels are almost identical to those of the World Health Organization (WHO). From January 1995 to March 1996, the study enrolled, as its initial population, 2205 patients (mean age 58.6 years; 47% women) from outpatient clinics in 59 university and general hospitals throughout Japan that specialise in diabetes care (Figure 1). Before April 1996, when the interventional phase of the study began, patients who did not meet the eligibility criteria were excluded, leaving 2033 patients (92%) who were randomised to the intervention group (N = 1017) or to the conventional treatment group (N = 1016). This was the overall study population used in future analyses.
Figure 1.
Outpatient clinics at 59 university and general hospitals nationwide in Japan that specialise in diabetes care
Throughout the study period, patients in both the conventional therapy and intervention groups received the same treatment that they had before the start of the study, with therapeutic management during the study being provided by specialists in diabetes. This included dietary advice by an administrative dietician on the basis of the Food Exchange Lists Dietary Guidance for Persons with Diabetes.11 In addition to this routine conventional treatment, patients in the intervention group were provided with education through individual counselling on dietary habits, physical activities, and adherence to treatment, including the proper use of medicines. Counselling was provided by physicians, nurses, dieticians, and other health-care staff members during each outpatient clinic visit. Patients in the intervention group also received 15-minute telephone counselling sessions at least once every 2 weeks from nurses, dieticians, and psychotherapists trained in diabetes education. These telephone sessions were based on a structured and uniform format. A diary to record laboratory and other data during the study was distributed to the patients in the intervention group to provide better feedback on therapeutic results. A pedometer was also given to patients in the intervention group for objective assessment of their exercise. Goals were set for patients in the intervention group and their physicians, including an HbA1c level < 6.5%, body mass index (BMI) < 22 kg/m2, blood pressure (BP) < 140/85 mmHg, serum cholesterol level < 220 mg/dL, serum triglyceride level < 150 mg/dL, serum high-density lipoprotein (HDL) cholesterol > 40 mg/dL, waist-to-hip ratio < 0.9 for men and < 0.8 for women, smoking cessation, and abstinence from alcohol. The goals for BP and serum cholesterol levels were updated in accordance with the revision of guidelines made by the Japan Diabetes Society (JDS), which were < 130/80 mmHg and < 220 mg/dL, respectively.
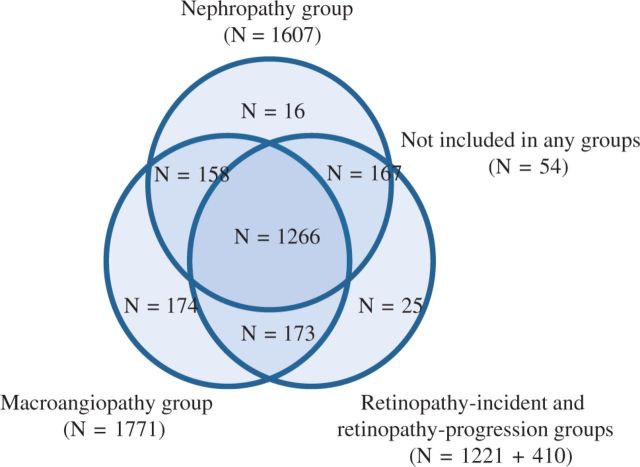
The protocol for the JDCS originally specified four analysis populations according to primary outcomes (Figure 2). The macroangiopathy group consisted of 1771 patients after the exclusion of patients with a history of angina pectoris, myocardial infarction, stroke, peripheral arterial disease, familial hypercholesterolaemia, or type III hyperlipidaemia. The nephropathy group was originally defined as the analysis population for incident overt nephropathy among patients with normo or low microalbuminuria. This analysis population consisted of 1558 patients after the exclusion of those with non-diabetic nephropathy, nephrotic syndrome, serum creatinine levels >120 μmol/L, or a mean value of two spot urine examinations that showed an albumin excretion rate of <150 mg/g creatinine.12 In future analyses, in which incident overt nephropathy from high microalbuminuria can be of secondary interest, we plan to extend the nephropathy group by including 49 patients with an albumin excretion rate of 150 to 300 mg/g creatinine. The retinopathy-incident group consisted of 1221 patients after the exclusion of candidates who had retinopathy or a major ocular disease (e.g., glaucoma, dense cataract, or a history of cataract surgery). The retinopathy-progression group consisted of 410 patients after the exclusion of those in the retinopathy-incident group who had a pre-proliferative or proliferative retinopathy or a major ocular disease (e.g., glaucoma, dense cataract, or a history of cataract surgery).
Figure 2.
The four analysis populations in the JDCS according to primary outcomes
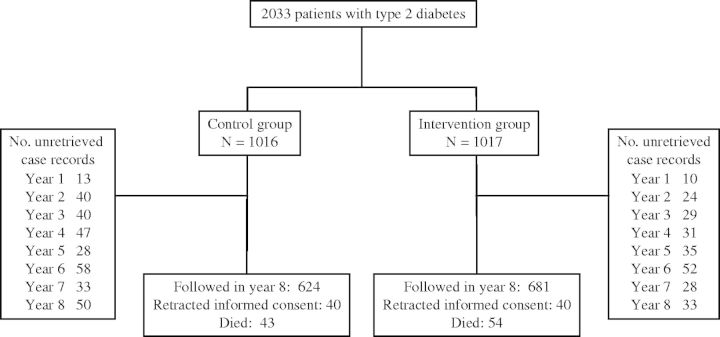
Figure 3 is a flow diagram of the data collection and follow-up populations in the JDCS. The overall 8-year follow-up rate was 73%; 1305 patients were followed in the eighth year of the study, 80 patients retracted informed consent, and 97 patients died before the eighth year of follow-up. Of the patients eligible for enrollment in the JDCS, 1588 patients (78%) responded to the baseline dietary survey and 1207 (76%) of these responding patients completed the 8-year follow-up, leaving 381 patients for whom dietary data had been available but who did not complete the 8-year follow-up. Table 1 compares baseline characteristics of the entire study cohort (1087 men and 946 women) with those for whom no baseline dietary data were available (N = 445), and those who were not followed for 8 years (N = 551). The mean age and HbA1c concentration of the patients without baseline dietary data and those not followed for 8 years were similar to those of the entire study cohort. The prevalence of diabetic retinopathy was relatively low in the patients without baseline dietary data.
Figure 3.
Flow diagram of data collection and follow-up in the JDCS
Table 1.
Comparison of baseline characteristic of patients in the entire cohort, those with no baseline dietary data, and those not followed for 8 years
| Men in the entire cohort |
Women in the entire cohort |
No baseline dietary data |
Not followed for 8 years |
|||||
|---|---|---|---|---|---|---|---|---|
| (N = 1087) |
(N = 946) |
(N = 445) |
(N = 551) |
|||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Age (year) | 58.1 | 7.0 | 59.0 | 6.8 | 57.9 | 7.1 | 58.4 | 7.1 |
| HbA1c (%) | 7.7 | 1.2 | 8.1 | 1.4 | 7.8 | 1.2 | 8.0 | 1.4 |
| Fasting blood sugar (mg/dL) | 158.9 | 41.4 | 161.3 | 45.4 | 158.6 | 42.8 | 164.1 | 45.4 |
| Years after diagnosis (year) | 11.5 | 7.7 | 10.2 | 6.6 | 10.7 | 7.7 | 10.8 | 7.6 |
| Diabetic retinopathy (%) | 19.0% | 21.5% | 13.0% | 17.2% | ||||
| Weight (kg) | 62.5 | 8.8 | 54.4 | 8.3 | 59.9 | 10.0 | 59.0 | 9.5 |
| BMI (kg/m2) | 22.8 | 2.7 | 23.3 | 3.4 | 23.4 | 3.2 | 23.1 | 3.0 |
| Waist circumference (cm) | 82.3 | 7.8 | 76.6 | 9.6 | 80.5 | 9.6 | 80.1 | 9.1 |
| Waist-to-hip ratio | 0.89 | 0.06 | 0.84 | 0.07 | 0.88 | 0.08 | 0.87 | 0.08 |
| SBP (mmHg) | 131.1 | 15.7 | 132.4 | 16.9 | 131.7 | 16.8 | 131.2 | 15.9 |
| DBP (mmHg) | 77.3 | 9.9 | 76.3 | 10.1 | 77.4 | 10.2 | 76.9 | 9.5 |
| Total cholesterol (mg/dL) | 194.5 | 34.5 | 209.4 | 33.7 | 203.9 | 35.1 | 202.8 | 36.2 |
| LDL-C (mg/dL) | 116.7 | 32.5 | 129.2 | 30.9 | 123.2 | 32.7 | 124.1 | 33.4 |
| HDL-C (mg/dL) | 52.3 | 16.5 | 57.2 | 16.7 | 54.5 | 16.2 | 54.4 | 16.8 |
| Triglyceridesa (mg/dL) | 130.2 | 85.4 | 99.0 | 71.0 | 109.0 | 87.0 | 104.0 | 69.0 |
| LP(a)a (mg/dL) | 22.8 | 27.2 | 17.0 | 19.6 | 17.0 | 19.8 | 16.0 | 21.0 |
| Spot urine ACRa (mg/gCr) | 60.6 | 271.3 | 18.5 | 31.6 | 20.2 | 44.0 | 20.4 | 41.5 |
| eGFR (mL/min/1.73m2) | 85.3 | 28.5 | 88.6 | 29.2 | 85.0 | 24.8 | 87.6 | 27.5 |
| Treated with insulin (%) | 19.5% | 22.5% | 21.9% | 17.7% | ||||
| Treated with OHA without insulin (%) | 64.2% | 66.7% | 64.5% | 65.7% | ||||
| Treated with antihypertensive agents (%) | 22.4% | 32.8% | 28.2% | 27.1% | ||||
| Treated with agents for dislipidaemia (%) | 16.7% | 35.1% | 27.8% | 24.4% | ||||
| Current smoker (%) | 44.7% | 8.8% | 26.7% | 31.6% | ||||
Abbreviations: ACR: albumin-to-creatinine ratio; BMI: body mass index; DBP: diastolic blood pressure; eGFR: estimated glomerular filtration rate; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; Lp(a): lipoprotein(a); OHA: oral hypoglycemic agents; SBP: systolic blood pressure.
aMedian and interquartile range.
How often have they been followed?
We originally planned to follow patients for 8 years, and an extended follow-up is ongoing. Information about primary outcomes, laboratory test results, and other clinical variables for each patient was collected at a central data centre through an annual report from each examining physician. Extensive lifestyle surveys were also conducted at baseline and 5 years after the beginning of the study intervention in both study groups. Table 3 summarises all of the measurements made and data collection used in the JDCS.
Table 3.
Summary of data collection in the Japan Diabetes Complications Study
| Baseline (1995) | 1996 to 1999 | 5 year follow-up (2000) | 2001 and after | |
|---|---|---|---|---|
| Background characteristics | ADC | |||
| Clinical and laboratory measurementsa | ADC | ADC | ADC | ADC |
| Chest radiographs | ADC | ADC | ADC | ADC |
| Neurological examination | ADC | ADC | ADC | ADC |
| Urine testsb | ADC | ADC | ADC | ADC |
| Ophthalmological examination | ADC | ADC | ADC | ADC |
| Therapeutic measures | ADC | ADC | ADC | ADC |
| Electrocardiograms | ADC | ADC | ADC | ADC |
| Cardiovascular events | ADC | ADC | ADC | ADC |
| Lifestyle surveys | ADC | ADC |
Abbreviation: ADC: annual data collection.
aBody weight, waist circumference, hip circumference, blood pressure, fasting plasma glucose, HbA1C, insulin, C-peptide, and lipids, measured at least semi-annually.
bSerum creatinine, blood urea nitrogen, urine protein, and urine albumin, measured at least semi-annually.
What has been measured?
Primary outcomes
Primary outcomes of the JDCS consisted of micro- and macro-vascular complications. Retinopathy was evaluated by qualified ophthalmologists at each participating institution, using the classification designed for this research, as follows: (i) stage 0, no retinopathy; (ii) stage 1, haemorrhage and hard exudates; (iii) stage 2, soft exudates; (iv) stage 3, intraretinal microvascular abnormalities and venous changes including beading, loops, and duplication; and (v) stage 4, new vessels, vitreous haemorrhage, fibrous proliferation, and retinal detachment. The retinopathy endpoints were; (i) development of retinopathy (from stage 0 to any other stage confirmed in two continuous years); and (ii) progression from stage 1 to stage 3 or 4. The nephropathy endpoint was defined as the development of overt nephropathy (spot urinary albumin excretion >300 mg/g creatinine in two consecutive samples). Macroangiopathy endpoints included the incidence of definite coronary heart disease (angina pectoris or myocardial infarction) or stroke. Diagnosis of angina pectoris and myocardial infarction was made according to criteria defined by the WHO/ Multinational Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA) project, and diagnosis of stroke was made according to guidelines defined by the Ministry of Health, Labour and Welfare of Japan.13 Adjudication of endpoints was done by central committees consisting of experts in each complication, on the basis of additional data such as findings on computed tomography (CT) or magnetic resonance imaging (MRI) of the brain or sequential changes in electrocardiograms.
Dietary survey
Food Frequency Questionnaires based on food groups (FFQg)14 and 24-hour dietary records were collected at baseline and 5 years after the beginning of the study intervention from both the intervention and conventional treatment groups. In brief, the FFQg consists of items about 29 food groups and 10 kinds of cookery and elicits information about the average intake per week of each food or food groups in commonly used units or portion sizes. The FFQg was externally validated through a comparison with weighed dietary records for 7 continuous days of 66 subjects aged 19–60 years.14 The coefficients of correlation of the FFQg with dietary records for energy, protein, fat, carbohydrate, and calcium intakes were 0.47, 0.42, 0.39, 0.49, and 0.41, respectively. The intakes of 26 of 31 nutrients usually estimated in dietary surveys were not significantly different with the two methods according to 5 paired Student’s t-tests.14 The ratio of the value obtained by dividing the FFQg by the dietary records ranged from 72% (vitamin B12) to 121% (vitamin C). The average value of this ratio was 104%. After patients completed the questionnaire, the dietician checked the sheets in an interview. To calculate nutrient and food intakes, we use standardised software for population-based surveys and nutrition counselling in Japan (Excel EIYO-KUN version 4.5; University Nutrition Database), which is based on the Standard Tables of Food Composition in Japan15 edited by the Japanese Ministry of Education, Culture, Sports, Science, and Technology.
Physical activity survey
Leisure-time physical activity was assessed at baseline through a self-administered questionnaire, which was almost identical to that used and validated in the Health Professionals’ Follow-up Study.16 Patients were asked the average frequency (times per week) and duration (minutes per one time) of their normal walking, brisk walking, jogging, golfing, tennis, swimming, aerobics dancing, cycling, and other miscellaneous exercises (specified by each patient). The duration of each activity in minutes was multiplied by the typical energy expenditure for the activity expressed in metabolic equivalents (METs) on the basis of the newest compendium of Ainsworth,17 and this was then summed for all activities to yield a MET-hour score per week. One MET, the energy expended in sitting quietly, is equivalent to 3.5 mL of oxygen uptake per kilogram of body weight per minute, or 1 kcal per kilogram of body weight per hour.
Occupation was surveyed with a self-administered questionnaire based on the Japan Standard Classification of Occupations,18 which was also used in the National Health and Nutritional Examination Survey19 in Japan. The occupational classifications in the survey were: (i) professional or skilled workers and technicians; (ii) administrative or managerial workers; (iii) office or clerical workers; (iv) sales workers; (v) service workers; (vi) armed force and police occupation; (vii) agricultural, forestry and fishery workers; (viii) workers in transport, trades and storage; (ix) labourers in manufacturing, mining, and construction; (x) no work or housewives.
Physical activity was determined with Baecke’s Total Physical Activity Index20 at 5 years. The extent of physical activity at baseline and that according to Baecke’s index were significantly correlated (Spearman’s rank correlation coefficient, r = 0.28; p > 0.01).
Laboratory tests and clinical variables
Other measurements included treatments, physical examinations, blood pressure, neurological/ophthalmological examinations, and laboratory tests such as for HbA1c, fasting plasma glucose/insulin/C-peptide, serum lipids/creatinine/urea nitorogen, and urine analysis. Assays for HbA1c assays are standardised by the Laboratory Test Committee of the JDS in values established by the JDS; the US National Glycohemoglobin Standardization Program (NSGP) value of HbA1c would be calculated as follows: 0.25 + 1.02 × JDS value.21 Diabetes-related distress and information about cigarette smoking were collected through a self-administered questionnaire.
Follow-up and response to lifestyle survey
The overall 8-year follow-up rate in the JDCS was 73% (Figure 3), and the follow-up rates in the macroangiopathy group, nephropathy group, retinopathy-incident group, and retinopathy-progression group were 75%, 78%, 77%, and 77%, respectively. At baseline, and of the 2033 patients in the JDCS cohort, 1486 completed both the FFQg and the 24-hour dietary record, 30 completed the FFQg only, and 72 completed the 24-hour dietary record only (overall response: 78%). Of the 1516 respondents to the baseline measurement of FFQg, 998 (66%) completed the FFQg at 5 years. Of the total of 2033 patients in the study cohort, 1917 (94%) completed the questionnaire on physical activity. Of the 1917 respondents to the baseline measurement of physical activity, 1217 (63%) completed the Baecke’s Total Physical Activity Index at 5 years.
What has it found? Key findings and publications
Primary results of randomised comparison
The registration of patients in the JDCS was completed in March 1996, and the interventions for the intervention group were continued until March 2003. In the primary analysis of the randomised comparison at the 8-year follow-up,1 the status of control of most classic cardiovascular risk factors, including body weight, glycaemia, serum lipids, and blood pressure, did not differ in the two study groups, but the incidence rate of stroke in the intervention group (5.48/1000 person-years) was significantly lower than that in the conventional treatment group (9.52/1000 person-years) according to both Kaplan–Meier analysis (p = 0.02) and multivariate Cox analysis (HR: 0.62, 95% CI: 0.39–0.98, P = 0.04). The incidence rates of coronary heart disease, retinopathy, and nephropathy did not differ significantly in the two study groups.
Diabetes complications and all-cause mortality over 8 years
Table 2 shows the occurrence of complications of diabetes and all-cause mortality in the patients in the JDCS who had type 2 diabetes. The crude incidence rates per 1000 person-years of diabetic retinopathy in men and women in the retinopathy-incident group were 34.77 and 42.70, respectively. The crude progression rates of diabetic retinopathy in men and women in the retinopathy-progression group were 17.65 and 24.75, respectively. The crude incidence rates of overt nephropathy in men and women in the extended nephropathy group were 9.47 and 7.40, respectively. The crude incidence rates of cardiovascular disease (coronary heart disease and stroke) in men and women in the macroangiopathy group were 17.03 and 10.47, respectively. The all-cause mortality rates in men and women in the overall JDCS cohort were 8.39 and 5.68, respectively.
Table 2.
Crude incidence rates of diabetes complications and all-cause mortality over 8 years
| Total |
Men |
Women |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Event | CIR | N | Event | CIR | N | Event | CIR | |
| Incident retinopathy | 1221 | 325 | 38.27 | 671 | 165 | 34.77 | 550 | 160 | 42.70 |
| Progression of retinopathy | 410 | 65 | 13.88 | 207 | 28 | 17.03 | 203 | 37 | 10.47 |
| Overt nephropathy | 1607 | 96 | 8.48 | 842 | 56 | 9.47 | 765 | 40 | 7.40 |
| Cardiovascular disease | 1771 | 163 | 21.09 | 940 | 104 | 17.65 | 831 | 59 | 24.75 |
| All-cause mortality | 2033 | 98 | 7.11 | 1087 | 61 | 8.39 | 946 | 37 | 5.68 |
Abbreviation: CIR: crude incidence rate per 1000 person-years.
Other publications
In addition to reporting its primary results,10 the JDCS reported the pathophysiological characteristics of East Asian patients with type 2 diabetes.22–25 In a 3-year interim report, we found small but significant differences in HbA1c levels in the intervention group (7.62 ± 1.20%) and conventional therapy group (7.78 ± 1.27%) that had appeared as early as 2 years after the beginning of the intervention in the JDCS and were maintained in the third year of the study.13 The transition rate from normo- and low microalbuminuria to overt nephropathy was 6.7/1000 person-years, and was significantly higher for the low microalbuminuric group than for the normoalbuminuric group (18.5 and 2.3/1000 person-years, respectively).12 The rates of incidence and progression of diabetic retinopathy were 38.3/1000 person-years and 21.1/1000 person-years, respectively.26 The JDCS also identified risk factors for cardiovascular disease in Japanese patients.27 With regard to coronary heart disease, the serum triglyceride concentration was a leading predictor of disease, and was comparable to the LDL cholesterol concentration in this regard (HR per 1 SD increase in triglycerides: 1.54, 95% CI: 1.22–1.94; HR per 1 SD increase in LDL cholesterol: 1.49, 95% CI: 1.25–1.78).28 These findings showed that the observed incidence rates of microvascular complications in the Japanese study population were lower than those in the Caucasian population and that the risk factors for complications of diabetes can also differ, suggesting ethnic disparities in the aetiology of complications of diabetes in the two populations. Further investigation is therefore needed of the epidemiological associations of clinical risk factors, lifestyle factors, and complications of diabetes in Asian population.
What are the main strengths and weaknesses?
The main strengths of the JDCS are: (i) a nationally representative patient population, in that the study subjects were recruited from 59 university and general hospitals throughout Japan; (ii) a follow-up done by diabetes specialists annually, ensuring the accuracy and quality of data, and especially of the primary outcome data; and (iii) relatively high response rates to lifestyle surveys. There are points for improvement as well. Calibration techniques for the dietary survey, such as the use of a doubly-labelled water method and multi-day 24-hour dietary records, were unavailable. The sample size of the study was small relative to population-based cohort studies, because it was based on the JDCS being a randomised trial. Additionally, the laboratory tests in the study were conducted at its participating institutions and not standardised prospectively, although laboratory tests are well standardised on a nationwide level in Japan.
Can I get hold of the data? Where can I find out more?
All data management for the JDCS is conducted at a central data centre in Tokyo. Our data set is not freely available, but collaborative ideas are welcome. Potential collaborators should discuss ideas informally with the principal investigator, who takes responsibility for collaboration by e-mail (jdcstudy@md.tsukuba.ac.jp).
Funding
The JDCS is financially supported by the Ministry of Health, Labour and Welfare, Japan.
Conflict of interest: None declared.
KEY MESSAGES.
This study of 2033 Japanese patients with type 2 diabetes was originally established in 1995 as a randomised lifestyle intervention trial. Its analysis of primary data at 8 years revealed a significant effect of the intervention used in the study on the incidence of stroke but not of other macro- or microvascular complications of diabetes.
The study also aimed to explore epidemiological associations of clinical risk factors for diabetes, of lifestyle factors with the complications of diabetes, and of complications of diabetes themselves. Extensive lifestyle surveys, including surveys of diet and physical activity, were done at baseline and at 5 years, and an extended follow-up is ongoing.
Little is known about the effects of lifestyle factors on the prognosis of Asian patients with type 2 diabetes characterised by low body weight. Comparing our cohort, which is representative of Japanese patients type 2 diabetes, with studies of Caucasian patients should provide further insights into ethnic disparities in this disease.
References
- 1.Gillies CL, Abrams KR, Lambert PC, et al. Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ. 2007;334:299. doi: 10.1136/bmj.39063.689375.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conn VS, Hafdahl AR, Mehr DR, et al. Metabolic effects of interventions to increase exercise in adults with type 2 diabetes. Diabetologia. 2007;50:913–21. doi: 10.1007/s00125-007-0625-0. [DOI] [PubMed] [Google Scholar]
- 3.Davies MJ, Heller S, Skinner TC, et al. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. BMJ. 2008;336:491–95. doi: 10.1136/bmj.39474.922025.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Christian JG, Bessesen DH, Byers TE, et al. Clinic-based support to help overweight patients with type 2 diabetes increase physical activity and lose weight. Arch Intern Med. 2008;16:141–46. doi: 10.1001/archinternmed.2007.13. [DOI] [PubMed] [Google Scholar]
- 5.Herder C, Peltonen M, Koenig W, et al. Anti-inflammatory effect of lifestyle changes in the Finnish Diabetes Prevention Study. Diabetologia. 2009;52:433–42. doi: 10.1007/s00125-008-1243-1. [DOI] [PubMed] [Google Scholar]
- 6.Norris SL, Lau J, Smith SJ, et al. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159–71. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 7.Loveman E, Cave C, Green C, et al. The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation. Health Technol Assess. 2003;7:iii, 1–190. doi: 10.3310/hta7220. [DOI] [PubMed] [Google Scholar]
- 8.Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348:383–93. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 9.Gaede P, Lund-Andersen H, Parving HH, et al. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358:580–91. doi: 10.1056/NEJMoa0706245. [DOI] [PubMed] [Google Scholar]
- 10.Sone H, Tanaka S, Iimuro S, et al. for the Japan Diabetes Complications Study Group. Long-term lifestyle intervention lowers the incidence of stroke in Japanese patients with type 2 diabetes: a nationwide multicentre randomised controlled trial (the Japan Diabetes Complications Study) Diabetologia. 2010;53:419–28. doi: 10.1007/s00125-009-1622-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The Japan Diabetes Society. Food Exchange Lists Dietary Guidance for Persons with Diabetes. Tokyo: Bunkodo; 2002. [Google Scholar]
- 12.Katayama S, Moriya T, Tanaka S, et al. for the Japan Diabetes Complications Study Group. Low transition rate from normo- and low microalbuminuria to proteinuria in Japanese type 2 diabetic individuals: the Japan Diabetes Complications Study (JDCS) Diabetologia. 2011;54:1025–31. doi: 10.1007/s00125-010-2025-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sone H, Katagiri A, Ishibashi S, et al. JDC Study Group. Effects of lifestyle modifications on patients with type 2 diabetes: the Japan Diabetes Complications Study (JDCS) study design, baseline analysis and three-year interim report. Horm Metab Res. 2002;34:509–15. doi: 10.1055/s-2002-34791. [DOI] [PubMed] [Google Scholar]
- 14.Takahashi K, Yoshimura Y, Kaimoto T, et al. Validation of a food frequency questionnaire based on food groups for estimating individual nutrient intake. Jpn J Nutr. 2001;59: 221–32. [Google Scholar]
- 15.Ministry of Education C, Sports, Science and Technology, Japan. Standard Tables of Food Composition in Japan 2004. http://www.mextgojp/b_menu/shingi/gijyutu/gijyutu3/toushin/05031802htm (in Japanese), accessed 7 Oct 2011.
- 16.Tanasescu M, Leitzmann MF, Rimm EB, Hu FB. Physical activity in relation to cardiovascular disease and total mortality among men with type 2 diabetes. Circulation. 2003;107:2435–39. doi: 10.1161/01.CIR.0000066906.11109.1F. [DOI] [PubMed] [Google Scholar]
- 17.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–81. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 18.The Statistics Bureau and the Director-General for Policy Planning of Japan MoIAaC. Japan Standard Classification of Occupations. http://www.statgojp/index/seido/shokgyou/indexhtm. 1997 (in Japanese)
- 19.Ministry of Health Law. Japan National Health and Nutrition Survey. http://www.mhlwgojp/bunya/kenkou/kenkou_eiyou_chousahtml. 2010 (in Japanese)
- 20.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36:936–42. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 21.The Committee on the Standardization of Diabetes Mellitus-Related Laboratory Testing of Japan Diabetes Society. International clinical harmonization of hemoglobin A1c in Japan: From JDS to NGSP values. Available from http://www.jds.or.jp/jds_or_jp0/uploads/photos/813.pdf (20 June 2012, date last accssed)
- 22.Sone H, Yoshimura Y, Ito H, Ohashi Y, Yamada N Japan Diabetes Complications Study Group. Energy intake and obesity in Japanese patients with type 2 diabetes. Lancet. 2004;363:248–49. doi: 10.1016/S0140-6736(03)15348-2. [DOI] [PubMed] [Google Scholar]
- 23.Sone H, Mizuno S, Fujii H, et al. Japan Diabetes Complications Study. Is the diagnosis of metabolic syndrome useful for predicting cardiovascular disease in Asian diabetic patients? Analysis from the Japan Diabetes Complications Study. Diabetes Care. 2005;28:1463–71. doi: 10.2337/diacare.28.6.1463. [DOI] [PubMed] [Google Scholar]
- 24.Sone H, Tanaka S, Ishibashi S, et al. Japan Diabetes Complications Study (JDCS) Group. The new worldwide definition of metabolic syndrome is not a better diagnostic predictor of cardiovascular disease in Japanese diabetic patients than the existing definitions: additional analysis from the Japan Diabetes Complications Study. Diabetes Care. 2006;29:145–47. doi: 10.2337/diacare.29.1.145. [DOI] [PubMed] [Google Scholar]
- 25.Sone H, Tanaka S, Iimuro S, et al. Waist circumference as a cardiovascular and metabolic risk in Japanese patients with type 2 diabetes. Obesity. 2009;17:585–92. doi: 10.1038/oby.2008.481. [DOI] [PubMed] [Google Scholar]
- 26.Kawasaki R, Tanaka S, Tanaka S, et al. on behalf of the Japan Diabetes Complications Study Group. Incidence and progression of diabetic retinopathy in Japanese adults with type 2 diabetes: 8 year follow-up study of the Japan Diabetes Complications Study (JDCS) Diabetologia. 2011;54:2288–94. doi: 10.1007/s00125-011-2199-0. [DOI] [PubMed] [Google Scholar]
- 27.Sone H, Tanaka S, Tanaka S, et al. for the Japan Diabetes Complications Study Group. Serum level of triglycerides is a potent risk factor comparable to LDL cholesterol for coronary heart disease in Japanese patients with type 2 diabetes: Subanalysis of the Japan Diabetes Complications Study (JDCS) J Clin Endocrinol Metab. 2011;96:3448–56. doi: 10.1210/jc.2011-0622. [DOI] [PubMed] [Google Scholar]
- 28.Sone H, Tanaka S, Tanaka S, et al. on behalf of the Japan Diabetes Complications Study Group. Comparison of various lipid variables as predictors of coronary heart disease in Japanese men and women with type 2 diabetes. Subanalysis of the Japan Diabetes Complications Study (JDCS) Diabetes Care. 2012;35:1150–57. doi: 10.2337/dc11-1412. [DOI] [PMC free article] [PubMed] [Google Scholar]