Abstract
Background: Factors underlying socioeconomic inequalities in mortality are not well understood. This study contributes to our understanding of potential pathways to result in socioeconomic inequalities, by examining alcohol consumption as one potential explanation via comparing socioeconomic inequalities in alcohol-attributable mortality and all-cause mortality.
Methods: Web of Science, MEDLINE, PsycINFO and ETOH were searched systematically from their inception to second week of February 2013 for articles reporting alcohol-attributable mortality by socioeconomic status, operationalized by using information on education, occupation, employment status or income. The sex-specific ratios of relative risks (RRRs) of alcohol-attributable mortality to all-cause mortality were pooled for different operationalizations of socioeconomic status using inverse-variance weighted random effects models. These RRRs were then combined to a single estimate.
Results: We identified 15 unique papers suitable for a meta-analysis; capturing about 133 million people, 3 741 334 deaths from all causes and 167 652 alcohol-attributable deaths. The overall RRRs amounted to RRR = 1.78 (95% confidence interval (CI) 1.43 to 2.22) and RRR = 1.66 (95% CI 1.20 to 2.31), for women and men, respectively. In other words: lower socioeconomic status leads to 1.5–2-fold higher mortality for alcohol-attributable causes compared with all causes.
Conclusions: Alcohol was identified as a factor underlying higher mortality risks in more disadvantaged populations. All alcohol-attributable mortality is in principle avoidable, and future alcohol policies must take into consideration any differential effect on socioeconomic groups.
Keywords: Alcohol-attributable mortality, socioeconomic status, meta-analysis, socioeconomic inequality, socioeconomic differences, alcohol, all-cause mortality, SES, education, income, occupation
Key Messages.
Socioeconomic differences in mortality are more pronounced in alcohol-attributable causes of death compared with all-cause mortality.
All alcohol-attributable mortality is in principle avoidable and future alcohol policies should take into consideration any differential effect on socioeconomic groups.
Primary healthcare practitioners and family doctors could play an important role in reducing socioeconomic inequality in mortality by using evidence-based screening, brief intervention and treatment referral practices.
Background
Low socioeconomic status (SES) has been repeatedly shown to be associated with an elevated mortality risk.1–5 Life expectancy in Europe is increasing, and socioeconomic differences in mortality are increasing.6 In most studies, SES has been identified via education, income or occupation.7 For all three indicators of SES, substantial differences in mortality have been shown.8–11 However, the underlying factors and mechanisms are not fully understood. For instance, attempts to explain such socioeconomic differences via influences of material wealth (e.g. financial resources, car ownership),12–14 behavioural activities (e.g. physical activity, smoking behaviour)9,10,15 or psychological factors (e.g. stress, coping strategies)16,17 could explain only part of the underlying differences, with inconsistent results.
This study tries to explain socioeconomic differences in mortality by focusing on causes of death related to alcohol consumption. Alcohol is known to be causally associated with more than 200 International Classification of Disease (ICD) three-digit disease and injury categories, including more than 30 such categories being 100% attributable to alcohol;18,19 i.e. these latter diseases and injuries would disappear completely without prior exposure to alcohol. Recently, the Global Burden of Disease and Injury Study revealed alcohol use as the fifth largest risk factor for global burden of disease:20 3.9% of the global burden of disease was attributable to alcohol use, 5.4% and 2.0% for men and women, respectively.
Individual studies seem to indicate that socioeconomic differences in mortality may be particularly large when alcohol-attributable causes of death are examined.21–23 Furthermore, although the effects of economic downturns and rising unemployment on health and inequality in health have been discussed controversially,24 strongly rising unemployment rates have been specifically linked to increased alcohol-attributable mortality.25 But to date no systematic review across countries and measures of SES has been undertaken to statistically compare socioeconomic differences in all-cause and alcohol-attributable mortality. This study is the first to give a quantitative overview of the profile of socioeconomic mortality differences by comparing relative risk in alcohol-attributable and all-cause mortality. Specifically we wanted to test the following hypothesis: independently of measurement (by education, occupation, employment status or income), the relative risk comparing low with high SES is larger for alcohol-attributable mortality than for all-cause mortality.
Methods
This systematic review and meta-analysis followed the Meta-analysis of Observational Studies in Epidemiology—a Proposal for Reporting (MOOSE,26 see Supplementary Table S1 for research checklist, available as Supplementary data at IJE online). It was based on a wider search for all studies examining the impact of SES on alcohol-attributable mortality and selected only studies that reported both alcohol-attributable mortality and all-cause mortality (see study protocol in Supplementary Text S1, available as Supplementary data at IJE online).
The meta-analysis was carried out in Germany at Technische Universität Dresden where no ethics approval is required for meta-analyses.
Literature research and study selection
Web of Science, MEDLINE, PsycINFO and ETOH were searched from their inception to the second week of February 2013, using the following terms: (alcohol related mortality OR alcohol attributable death OR alcohol attributable mortality) AND (ratio* OR risk*) AND (ses OR social class OR socioeconomic variable* OR socioeconomic status OR socioeconomic factor*). In order to meet the specific requirements of the databases, the search-algorithm was slightly adapted, using MeSH terms in MEDLINE and PsycINFO (see study protocol in Supplementary Text S1, available as Supplementary data at IJE online). All titles and abstracts were screened for eligibility criteria as listed in Table 1. A rating of accordance was carried out by S.B., J.R. and C.P. on a sample of 10 abstracts: mean accordance was 73%, with the less experienced raters showing inclusion of more studies. To be conservative, we decided to retrieve all potentially relevant articles in full text. Final decisions about inclusion were discussed between J.R., M.R. and C.P. Since a number of studies reported on overlapping populations (leading to duplicate data) we chose the article for in clusion based on the quality criteria mentioned below.
Table 1.
Inclusion and exclusion criteria for study selection
| Criterion | Inclusion | Exclusion |
|---|---|---|
| Mortality | Mortality is measured at individual level; Mortality is attributed to alcohol | Indirectly affected people are investigated (e.g. non-alcoholized victims of alcoholized car drivers) |
| SES | SES is measured via occupation, employment status, income, or education; SES is measured on at least two values; SES is measured at individual level | SES is measured by the parent’s SES or childhood SES |
| Design | The study is empirical and quantitative | The study is an intervention study |
| Sample | The sample is population-based; participants are at least 15 years of age | A clinical sample is investigated |
| Results | Alcohol-attributable mortality is reported by SES of the deceased; one measure of risk (relative risk, odds ratio, hazard ratio) and its CI, or raw data for calculation are reported | |
| Language | Language is restricted to English or German |
Data abstraction
We abstracted several variables concerning characteristics of the study population: design; measurement of SES, categorized into education, occupation, income and employment status (e.g. employed vs unemployed); measurement of mortality; results; and adjustments for confounding (for details see study protocol in Supplementary Text S1, available as Supplementary data at IJE online). All differences in abstraction were discussed and consensually decided between J.R., M.R. and C.P. Alcohol-attributable diagnoses investigated in each study were documented using their ICD-10 code. Rate ratios, hazard ratios, relative risks and odds ratios were treated as equivalent measures of relative risk. Concerning adjustments, we gave preference to risk estimates that were only age-adjusted in order to avoid over-adjustment, e.g. adjusting one measure of SES for another measure of SES. Missing value imputation was applied as per study protocol (Supplementary Text S1, available as Supplementary data at IJE online). In two cases with missing data on key variables, it was possible to obtain original data directly from the authors.23,27
Study quality
The following aspects of study quality were derived from main quality features in observational studies:28 representativeness of the sample; loss of data due to problems in measurement of SES; operationalization of alcohol-attributable mortality concerning alcohol-attributable fractions; linkage of survey data; and age-adjustment. These quality features were monitored using a custom-made quality checklist (see Supplementary Table S2, available as Supplementary data at IJE online), because common checklists are usually tailored for randomized clinical trials. Since the quality aspects differ in their importance, an aggregate score was not applied. Details of the definition of quality criteria can be found in the study protocol (Supplementary Text S1, available as Supplementary data at IJE online).
Statistical analysis
For each study, the ratio of relative risks (RRR) between alcohol-attributable mortality (numerator) and all-cause mortality (denominator) was calculated. The underlying relative risks were based on the mortality rate of the lowest SES category divided by the mortality rate of the highest SES category. For instance, if SES was measured by education with four categories (university, college, high school, less than high school), the relative risk would be derived from dividing the mortality rate for the lowest SES (less than high school) by the rate of the highest SES level (university). These comparisons of lowest with highest SES are standard in the scientific analyses of inequality and our methodology was also chosen to include the maximum of underlying research.
The RRRs described above were pooled for each SES measure separately using random effects meta-analyses. In a second step, the resulting RRRs were pooled to obtain a global estimation across all four measures of SES. The resulting RRR describes the factor by which subjects with lower SES die more from alcohol-attributable causes of death compared with all causes of death. All meta-analyses were conducted stratified by sex using inverse-variance weighted DerSimonian-Laird random effects models to allow for between-study heterogeneity.29 We quantified between-study heterogeneity using Cochran’s Q30 and the I2 statistic.31 I2 can be interpreted as the proportion of the total variation in the estimated RRRs for each study that is due to heterogeneity between studies. I2 values above 50% were considered substantial. Potential publication bias was examined using Egger’s regression-based test.32 In order to control for disproportionate influence of any single study, leave-one-out analyses were performed. For investigation of possible sex differences random effects meta-regression33 was performed. Following the recommendation of the Cochrane Handbook, meta-regression was conducted only when at least 10 cohorts from primary studies were available.34 All calculations were conducted on the natural log-scale using STATA software (Version 11).
Results
Literature search results
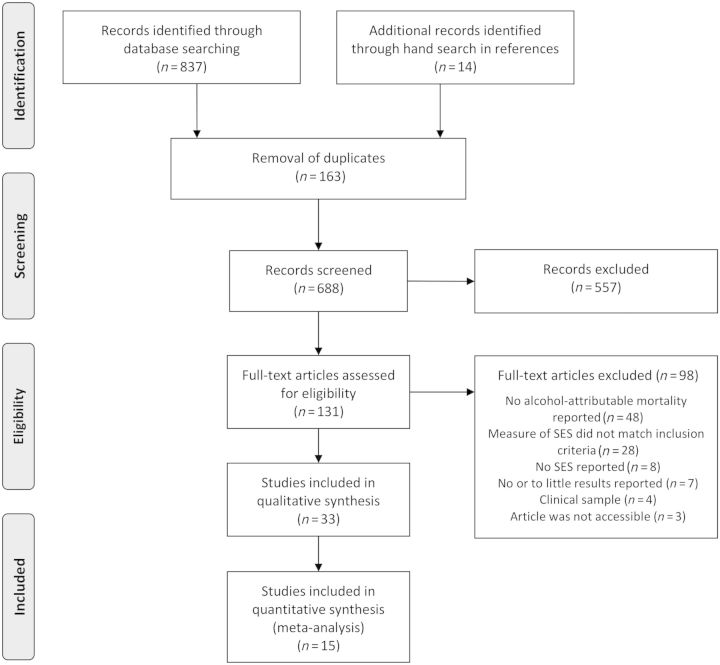
In total 33 articles were eligible for inclusion as per inclusion criteria (Table 1). After exclusion of population overlap and studies that did not report on all-cause mortality, 15 studies remained for statistical analyses (Figure 1 ), reporting on data assessed between 1970 and 2006. Of the 15 studies most were from Finland (n = 6), the others from Sweden (n = 2), Russia (n = 2), Estonia (n = 1), Poland (n = 1), Switzerland (n = 1) and Canada (n = 1). One study reported data from seven countries and nine different cohorts27 and one reported two cohorts from the same country.35 Overall, these meta-analyses included about 133 million people (69 million women and 64 million men), 3 741 334 deaths from all causes (1 500 381 women and 2 240 953 men) and 167 652 alcohol-attributable deaths (29 302 women and 138 350 men). For detailed information about the included studies see Table 2. All diagnoses, their ICD-10 code and the number of studies that included the respective diagnosis are listed in Supplementary Table S3 and details on the measures extracted in the meta-analysis (measure of SES, alcohol-attributable mortality and outcome measures) are displayed in Supplementary Table S4 (both available as Supplementary data at IJE online).
Figure 1.
Flow diagram for study selection and exclusion. SES, socioeconomic status.
Table 2.
Study characteristics of all studies included in the meta-analysis
| Study | Country | Sex (age in years) | SES Assessmenta | SES indicator (Number of levels) | Mortality assessmentb | Version of ICD | N | N all-cause (alc.-attrib.)c | Qualityd |
|---|---|---|---|---|---|---|---|---|---|
| Valkonen (1993)36 | Finland | F, M (35-64) | 1970, 1975, 1980 | Occupation (4) | 1971–75, 1976–80, 1981–85 | Not specified | 1 567 000e | 147 808 (11 000e) | (+) |
| Koskinen (1994)37 | Finland | F, M (35-64) | 1980 | Education (3) | 1981–85 | Not specified | 1 622 000e | 52 533 (2488) | (+) |
| Mäkelä (1997)38 | Finland | F, M (20+) | 1985, 1990 | Occupation (3) | 1987–90, 1991–93 | ICD-9 | 3 249 000e | 276 730 (20 835) | (+) |
| Shkolnikov (1998)23 | Russia | F, M (20-69) | 1989 | Education (2) | 1989 | ICD-8, ICD-9 | 89 436 000e | 503 824 (9210) | (−) |
| Martikainen (2001)21 | Finland | F, M (30-90) | 1990 | Income (10) | 1991–96 | ICD-9 | 2 709 000e | 260 941 (6556) | (+) |
| Hemström (2002)39 | Sweden | F, M (20-64) | 1980, 1990 | Occupation (3) | 1990–95 | ICD-9 | 1 480 000e | 192 117 (9547) | (+) |
| Kivimäki (2003)40 | Finland | F, M (18-36) | 1990–00 | Employment status (4) | 1990–2001 | ICD-9, ICD-10 | 92 351 | 1332 (414) | (−) |
| Leinsalu (2003)35 | Estonia | F, M (20-70) | 1989, 2000 | Education (3) | 1987–90; 1999–2000 | ICD-9, ICD-10 | 2 097 607 | 107 480 (3500e) | (−) |
| Voss (2004)41 | Sweden | F, M (15-47) | 1973 | Employment status (2) | 1973–83 | ICD-8, ICD-9 | 20 632 | 1191 (50) | (−) |
| Kivimäki (2007)42 | Finland | F, M (19-64) | 1994–2000 | Education (2), Occupation (3) | 1994–2000 | ICD-9, ICD-10 | 65 405 | 626 (179) | (−) |
| Mackenbach (2008)27 | Finland | F, M (30-74) | 1990 | Education (3) | 1990–2000 | ICD-9, ICD-10 | 2 587 000e | 269 781 (14 100e) | (+) |
| Norway | F, M (30-74) | 1990 | Education (3) | 1990–2000 | ICD-9, ICD-10 | 1 995 500e | 213 022 (10 800e) | (+) | |
| Belgium | F, M (30-74) | 1991 | Education (3) | 1991–95 | ICD-9, ICD-10 | 5 524 500e | 283 349 (13 500e) | (+) | |
| Italy (Turin) | F, M (30-74) | 1991 | Education (3) | 1991–2001 | ICD-9, ICD-10 | 487 000e | 50 621 (2600e) | (+) | |
| Sweden | F, M (30-74) | 1991 | Education (3) | 1991–2000 | ICD-9, ICD-10 | 4 583 000e | 404 151 (23 700e) | (+) | |
| Spain (Barcelona) | F, M (30-74) | 1992 | Education (3) | 1992–2001 | ICD-9, ICD-10 | 858 000e | 77 101 (4400e) | (+) | |
| Denmark | F, M (30-74) | 1996 | Education (3) | 1996–2000 | ICD-9, ICD-10 | 3 094 500e | 136 065 (7600e) | (+) | |
| Spain (Basque country) | F, M (30-74) | 1996 | Education (3) | 1996–97 | ICD-9, ICD-10 | 3 663 300e | 22 585e (2000e) | (+) | |
| Spain (Madrid) | F, M (30-74) | 1996 | Education (3) | 1996–2001 | ICD-9, ICD-10 | 1 108 800e | 41 704 (3300e) | (+) | |
| Zagozdzon (2009)43 | Poland (Gdansk) | F, M (20-64) | 1999 | Employment status (2) | 1999–2004 | ICD-10 | 367 848 | 8521 (1500e) | (−) |
| Faeh (2010)44 | Switzerland | F, M (30-69) | 1992/1993 | Education (3) | 1990–2000 | ICD-8, ICD-10 | 3 450 120 | 261 314 (16 156) | (−) |
| Pridemore (2010)45 | Russia (Izhevst) | M (25-54) | 2002 | Education (6) | 2003–05 | ICD-10 | 3149 | 1559 (100) | (−) |
| Tjepkema (2012)22 | Canada | F, M (25-80) | 1991 | Education (4) | 1991–2006 | ICD-9, ICD10 | 2 734 800 | 426 979 (4117) | (+) |
F=Female; M=Male.
aAll data are based on census or register data except of Pridemore et al.45 who performed proxy interviews and Kivimäki et al.42 who also included survey data.
bAll data are based on some sort of death register except Pridemore et al.45 who performed proxy interviews.
cNumber of deaths from all causes (number of alcohol-attributable deaths).
d(+), all quality criteria are met; (−), at least one quality criterion is not met.
eEstimated value as described in study protocol (Supplementary Text S1, available as Supplementary data at IJE online).
Meta-analyses
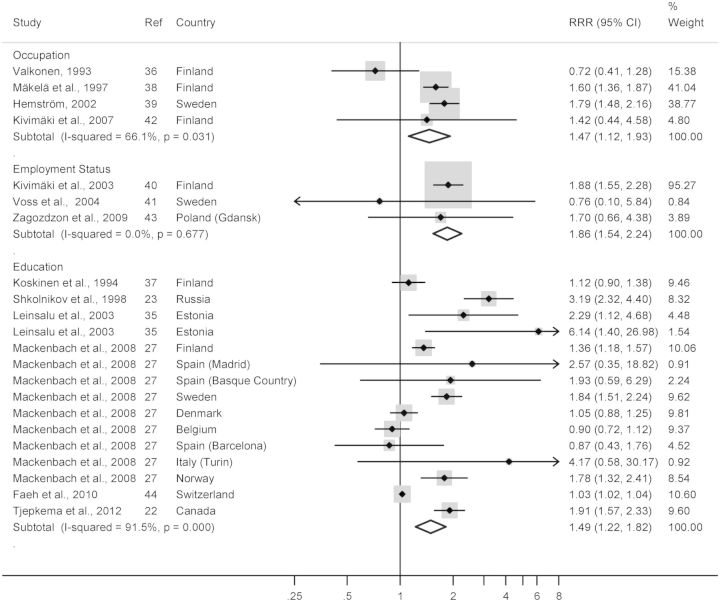
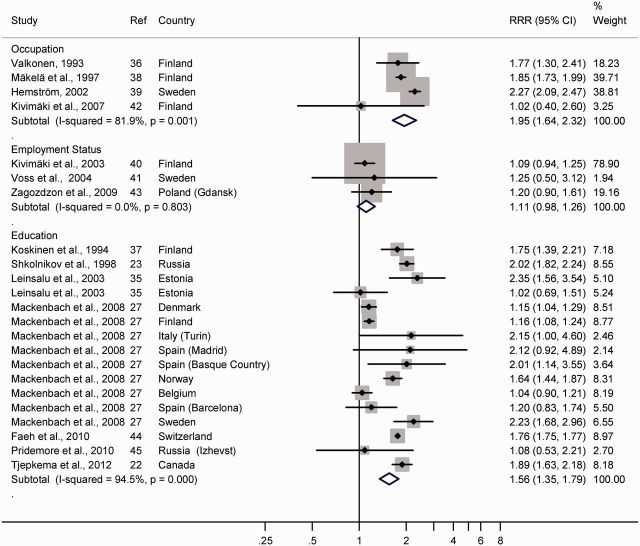
All analyses were stratified by sex (Figure 2 and 3). For education, six and seven studies were pooled for women and men, respectively: the resulting RRRs were 1.49 (95% CI 1.22 to 1.82) for women and RRR = 1.56 (95% CI 1.35 to 1.79) for men. Meta-analyses pooling the four eligible studies for occupation led to the following effects: RRR = 1.47 (95% CI 1.12 to 1.93) and RRR = 1.95 (95% CI 1.64 to 2.32), for women and men, respectively. Three studies reported on employment status; the pooled RRR for employment status for women was: RRR = 1.86 (95% CI 1.54 to 2.24); the confidence interval of the RRR of socioeconomic inequality in alcohol-attributable compared with all-cause mortality in men did include one RRR = 1.11 (95% CI 0.98 to 1.26). One study reported on income; the RRRs were 2.49 (95% CI 1.92 to 3.23) and 2.28 (95% CI 2.00 to 2.60), for women and men, respectively.
Figure 2.
Random effects meta-analyses for women. Forest plot of pooled RRR for women, stratified by measure of SES. Size of squares corresponds to the weight of each study in the meta-analysis. Ref, reference number in references; RRR, ratio of relative risk; SES, socioeconomic status; CI, confidence interval.
Figure 3.
Random effects meta-analyses for men. Forest plot of pooled RRR for men, stratified by measure of SES. Size of squares corresponds to the weight of each study in the meta-analysis. Ref, reference number in references; RRR, ratio of relative risk; SES, socioeconomic status; CI, confidence interval.
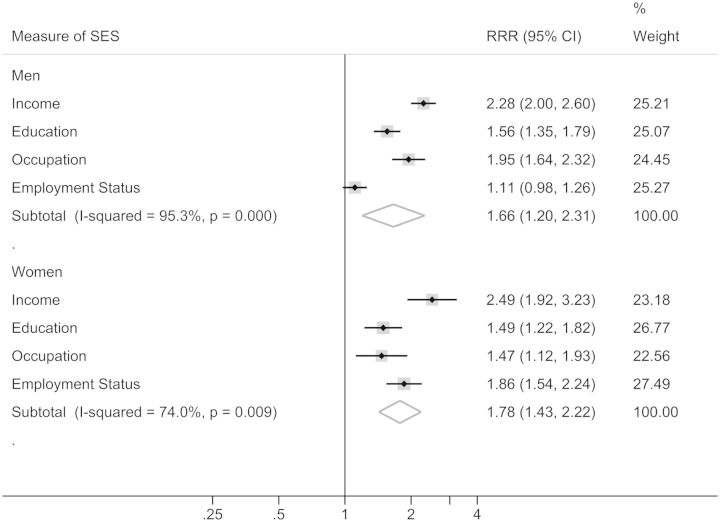
Pooling the RRRs from education, occupation, employment status and income resulted in RRR = 1.78 (95% CI 1.43 to 2.22) and RRR = 1.66 (95% CI 1.20 to 2.31), for women and men, respectively (Figure 4). The results indicate a 1.5–2-fold higher mortality for alcohol-attributable causes compared with all causes in subjects with low SES.
Figure 4.
Overall random effects meta-analyses. Forest plot of pooled RRR across measures of SES, stratified by sex. Size of squares corresponds to the weight of each study in the meta-analysis. RRR, ratio of relative risk; SES, socioeconomic status; CI, confidence interval.
Quality assessment, heterogeneity, and bias control
With regard to study quality, representativeness of the sample for the whole population was not given in three studies; one study excluded a considerable share of the study population due to problems in classification of SES. Five studies included at least one disease category that is not wholly alcohol-attributable (see Supplementary Table S2; available as Supplementary data at IJE online). Four studies did not link individual (census) information about SES to individual death certificates; one study did not report age-adjusted results. Seven studies fulfilled all quality criteria.
Substantial heterogeneity was detected in the meta-analyses for education as well as for occupation in both sexes, with an I2 > 50% and a Q-value with P < 0.01. In the analyses of employment status, no heterogeneity was detected for either of the sexes with I2 = 0% and a Q-value with P > 0.1. Because of the number of primary studies, random effects meta-regression and Egger’s test for publication bias were only possible for education. No substantial difference in RRRs for sex was found. Finnish studies did not differ substantially from the other studies. Egger’s regression test showed bias for women (P < 0.01) but not for men (P = 0.15). Leave-one-out analysis revealed substantial influence only in the meta-analysis of employment status for men. The results for employment status were mainly based on one study40 (see Figures 2 and 3).
Discussion
Principal findings
The reasons underlying socioeconomic differences in mortality are not fully understood. The present study compared socioeconomic inequality in alcohol-attributable and all-cause mortality. The overall analysis pooling results from education, occupation, employment status and income showed that the relative risk of dying from alcohol-attributable causes is roughly 1.7-fold the relative risk of all-cause mortality for both sexes. This indicates that whereas low SES is associated with an elevated risk of dying, this risk is especially elevated for alcohol-attributable causes of death. Meta-analyses stratified by measure of SES revealed consistent results. Employment status in men was the only exception, but because of the small number of studies for employment status, the results for this SES indicator have to be interpreted with caution.
Methodological limitations
All but one (Canada22) studies underlying our results were from European countries. Most of them were high-income countries at the time of data collection, with Estonia and Russia being the only exceptions. Finnish studies are disproportionately represented. Thus the results are generalizable for European high-income countries or other high-income countries with comparable distributions in socioeconomic indicators. Working with aggregated data (as is the case in meta-analyses) always entails the risk of ecological fallacy.46 This should be kept in mind when discussing mechanisms underlying the socioeconomic differences because factors such as individual alcohol consumption or occupations were beyond our control.
As indicated in Table 2, data on cause of death were derived from public registers and might vary in preciseness within and across studies. It is possible that alcohol-attributable causes are underrepresented because of the stigma attached to them. We cannot rule out the possibility of such a bias or a bias related to the SES of the deceased.
We found substantial statistical between-study heterogeneity in almost all analyses, mostly because of the large sample size and resulting small errors of the mean in almost all studies included. We therefore used inverse-variance weighted DerSimonian-Laird random effects models to allow for this between-study heterogeneity when calculating the CIs.29 The lower number of alcohol-attributable deaths in women partially led to broad CIs, limiting the reliability of the estimation. Further large-scale investigations are needed for women.
We examined study quality for all studies included in the meta-analysis (Supplementary Table S2, available as Supplementary data at IJE online). Meta-regressions for each quality criterion were not feasible due to the small number of studies included.34 Investigation of study quality showed that each of the three studies investigating employment status as indicator of SES did not fulfill several criteria.40,41,43 These limitations should be considered when the respective results are interpreted.
Interpretation of results
The most obvious explanation for those socioeconomic differences in alcohol-attributable mortality would be systematic differences in alcohol consumption habits and patterns. Across different measures of SES, studies from a number of European countries as well as the USA, New Zealand and Australia showed differences in drinking patterns over social classes.47–53 Men of high SES tended to drink frequently, smaller amounts of alcohol per drinking occasion, whereas men with low SES tended to drink larger amounts on fewer occasions, e.g. drink in order to get drunk. For women, SES-related differences in drinking patterns were less consistent. Particularly in Western/European countries (Germany, The Netherlands, Switzerland, France, Austria, and the UK) women of a high SES were more likely to consume heavily compared with women of middle or lower SES. In men as well as women, the share of abstinence increased with descending SES. Mäkelä and Paljärvi found in a Finnish sample that socioeconomic differences in alcohol-attributable morbidity and mortality could not be fully explained by differences in alcohol consumption patterns.54 Overall the findings indicate a multiplicative interaction of alcohol and SES, leading to greater harm in subjects with low SES even when the average level of alcohol consumption and some consumption patterns are controlled for. In the following, we consider healthcare supply, dietary habits, and smoking behaviours as putative main factors underlying this phenomenon.
Alcohol-related primary care interventions are cost-effective measures to reduce alcohol consumption and mortality.55,56 Studies showed that people of low SES are more often confronted with barriers to accessing health services than people of high SES.57,58 These barriers refer to accessibility (e.g. costs, transport) and availability (e.g. proximity to residence, waiting lists) of healthcare supply. Furthermore, at-risk drinking59 and alcohol-related disorders are highly stigmatized.60,61 People with alcohol dependence are often seen as being unpredictable, dangerous and responsible for their disorder and related problems.61,62 This stigma has been shown to be particularly high for subjects of low SES.63 A high perceived stigmatization was in turn related to decreased perception of treatment need and a reduced usage of health services.63,64 These findings show that, due to a lack of accessibility and availability of healthcare services as well as stigmatization, especially subjects of a low SES are unlikely to receive professional help in alcohol-related diseases and disorders.
Investigation of dietary patterns in Western countries found repeatedly that people with a low SES were more likely to purchase foods that are high in fat, salt and sugar65 and to consume processed and fast food.66,67 Moreover, low SES was linked to dietary patterns inconsistent with dietary recommendations,68–70 such as low fruit and vegetable consumption.71–73 This kind of malnutrition probably interacts with alcohol consumption: Especially the intake of proteins and vitamins is affected by alcohol consumption, leading to increased risk of liver diseases as well as harmful effects on multiple health outcomes.74,75 Furthermore, malnutrition and heavy alcohol consumption interact to produce immunosuppressive effects,76 which are in turn linked to a number of disease endpoints such as liver disease or infectious diseases.77–79 These results suggest that dietary patterns of people with low SES interact with alcohol consumption in a harmful way and might thereby contribute to socioeconomic differences in alcohol-attributable mortality. Not surprisingly, obesity as well is distributed unequally in society.80,81 Again, adverse interactions of obesity and alcohol intake have been shown, e.g. for an increased risk of colorectal cancer.82 Evidence on the interaction of alcohol and nutrition/obesity and their implications for socioeconomic inequality in mortality is still sparse and epidemiological research is needed.
In several Western/European countries, smoking behaviour is much more prevalent among people with low SES.83–86 Reviews revealed a multiplicative interaction of alcohol and smoking leading to an increased risk of aero-digestive cancers.87,88 Given the SES-related differences in smoking behaviour, people of low SES are at higher risk of being affected by the described interactive effects of alcohol and smoking. Aero-digestive cancers (concerning e.g. oral cavity, larynx, pharynx, or oesophagus) constitute only a small proportion of alcohol-attributable deaths, limiting the potential impact of the interaction hypothesized.
In summary, our results indicate that alcohol plays an important role in the development of socioeconomic differences in mortality. This might partially be due to the fact that it interacts with other risk factors such as nutrition, smoking behaviour or health care utilization, all of which were unequally distributed across SES as well.
Implications for policy and practice
All alcohol-attributable harm is in principle avoidable.89 In Europe an estimated 13.9% of all deaths in adult (aged 15–64 years) men and 7.7% of all deaths in adult (aged 15–64 years) women are attributable to alcohol.90 Based on our estimations, the relative risk (occupation) of all-cause mortality in men could be reduced by 6% if 30% of alcohol-attributable deaths in subjects with low SES were prevented. A prevention of 50% of those deaths would reduce socioeconomic differences in all-cause mortality by 10%. For women, the same reductions in alcohol-attributable mortality would lead to a 2.5% and a 4.5% reduction of the relative risk for all-cause mortality, respectively.
Most preventive measures concerning alcohol-related harm reduction target society as a whole and rather little is known about effective measures targeting subjects with low SES. Herttua and colleagues investigated the development of alcohol-attributable deaths after a reduction of alcohol taxes.91 They found a stronger increase of alcohol-attributable deaths among people of low SES compared with people of high SES. If this effect would work the reverse way as well, i.e. that an increase of taxes leads to relative decrease of alcohol-attributable death in low SES, remains undecided. Next to measures of taxation, limitation of selling times, liquor licenses and density of alcohol selling stores have turned out to be effective.92 It is imaginable to reduce the socioeconomic slope by targeted reduction of alcohol availability in underprivileged areas. The moral justifiability and political practicability of some of these measures may be debatable, however. In any case such measures should be combined with community-based preventive measures and educational opportunities.93,94 Next to restrictive measures, policy makers should revise social welfare spending which, for instance, can buffer detrimental effects of unemployment and financial crises, such as alcohol-attributable mortality.25,95 Stuckler, Basu, and McKee showed that a rise in social welfare spending was associated with a decrease in alcohol-attributable mortality whereas rising healthcare spending was not.96
Nevertheless, primary healthcare practitioners could constitute a direct way of reducing societal differences in alcohol-attributable health and mortality. Alcohol-related primary care interventions, such as screening and brief counselling, have been shown to be cost-effective measures to reduce alcohol consumption, related harm and mortality.55,56,97–100 Especially patients of low SES should be informed about risks and consequences of alcohol use as well as basic rules for risk-reduced alcohol consumption, such as lower risk drinking guidelines.101 Additionally, primary healthcare practitioners could play an important role in reducing socioeconomic inequality in mortality by linking patients to specialized alcohol treatment services.
Future research
Specific pathways from low SES through alcohol consumption to mortality need to be investigated in future research. This requires longitudinal observational studies that allow for an accurate investigation of SES, societal-, territorial- and healthcare-related circumstances, alcohol consumption patterns, dietary habits, smoking behaviour, and health service use. Another important, yet unresolved question is how to specifically target people of low SES with alcohol-related preventive measures. Intervention studies aiming at a reduction of the socioeconomic gap in alcohol-attributable mortality are needed.
Supplementary Data
Supplementary data are available at IJE online.
Funding
This work was supported by the province of Ontario financially and concerning infrastructure (to J.R.). The funders had no role in study design, data collection, analysis, interpretation, decision to publish, or preparation of the manuscript.
Details of contributors
C.P. is named as the guarantor and has overall responsibility of all steps. J.R. and S.B. supervised the whole working process. C.P., J.R. and S.B. conceived and designed the meta-analysis. C.P., J.R. and M.R. performed the literature research and study selection. C.P., S.B. and J.R. performed rating of inclusion/exclusion. M.R., J.R. and C.P. decided on statistical procedures and analyzed the data. They had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. C.P. wrote the first draft of the manuscript. All authors contributed to the writing and revision of the manuscript and final approval of the version to be published. C.P. confirms that the material has not been published previously.
Supplementary Material
Acknowledgements
We kindly thank Drs Mackenbach and Leon for providing us with original data. Furthermore we would like to thank Drs Stenius and Connor for providing us with literature that was not accessible online. The first author was offered an internship by the Centre for Addiction and Mental Health, during which a lot of the basic work for the meta-analysis was carried out.
Conflict of interest: The authors had no involvements that might raise the question of bias in the work reported or in the conclusions, implications or opinions stated.
References
- 1.Sorlie PD, Backlund E, Keller JB. US mortality by economic, demographic, and social characteristics: The National Longitudinal Mortality Study. Am J Public Health 1995;85:949–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mackenbach JP, Kunst AE, Cavelaars A, et al. Socioeconomic inequalities in morbidity and mortality in western Europe. Lancet 1997;349:1655–59. [DOI] [PubMed] [Google Scholar]
- 3.Blakely T, Tobias M, Atkinson J. Inequalities in mortality during and after restructuring of the New Zealand economy: repeated cohort studies. BMJ 2008;336:371–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strand BH, Grøholt EK, Steingrímsdóttir OA, Blakely T, Graff-Iversen S, Næss Ø. Educational inequalities in mortality over four decades in Norway: prospective study of middle aged men and women followed for cause specific mortality, 1960–2000. BMJ 2010;340:c654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huisman M, Kunst AE, Bopp M, et al. Educational inequalities in cause-specific mortality in middle-aged and older men and women in eight western European populations. Lancet 2005;365:493–500. [DOI] [PubMed] [Google Scholar]
- 6.Mackenbach JP, Karanikolos M, McKee M. The unequal health of Europeans: successes and failures of policies. Lancet 2013;381:1125–34. [DOI] [PubMed] [Google Scholar]
- 7.Duncan OD. Occupational components of educational differences in income. J Am Stat Assoc 1961;56:61–66. [Google Scholar]
- 8.Kunst AE, Groenhof F, Mackenbach JP; EU Working Group on Socioeconomic Inequalities Health. Occupational class and cause specific mortality in middle aged men in 11 European countries: comparison of population based studies. BMJ 1998;316:1636–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balia S, Jones AM. Mortality, lifestyle and socio-economic status. J Health Econ 2008;27:1–26. [DOI] [PubMed] [Google Scholar]
- 10.Feinglass J, Lin S, Thompson J, et al. Baseline health, socioeconomic status, and 10-year mortality among older middle-aged Americans: findings from the Health and Retirement Study, 1992–2002. J Gerontol B Psychol Sci Soc Sci 2007;62:S209–17. [DOI] [PubMed] [Google Scholar]
- 11.Elo IT, Preston SH. Educational differentials in mortality: United States, 1979-85. Soc Sci Med 1996;42:47–57. [DOI] [PubMed] [Google Scholar]
- 12.Schrijvers CT, Stronks K, van de Mheen HD, Mackenbach JP. Explaining educational differences in mortality: the role of behavioral and material factors. Am J Public Health 1999;89:535–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fujishiro K, Xu J, Gong F. What does “occupation” represent as an indicator of socioeconomic status?: exploring occupational prestige and health. Soc Sci Med 2010;71:2100–07. [DOI] [PubMed] [Google Scholar]
- 14.Davey Smith G, Shipley MJ, Rose G. Magnitude and causes of socioeconomic differentials in mortality: further evidence from the Whitehall Study. J Epidemiol Community Health 1990;44:265–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lantz PM, Golberstein E, House JS, Morenoff J. Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of US adults. Soc Sci Med 2010;70:1558–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krueger PM, Chang VW. Being poor and coping with stress: health behaviors and the risk of death. Am J Public Health 2008;98:889–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Talala KM, Huurre TM, Laatikainen TK, Martelin TP, Ostamo AI, Prattala RS. The contribution of psychological distress to socio-economic differences in cause-specific mortality: a population-based follow-up of 28 years. BMC Public Health 2011;11:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rehm J. The risks associated with alcohol use and alcoholism. Alcohol Res Health 2011;34:135–43. [PMC free article] [PubMed] [Google Scholar]
- 19.Rehm J, Baliunas D, Borges GL, et al. The relation between different dimensions of alcohol consumption and burden of disease: an overview. Addiction 2010;105:817–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martikainen P, Mäkelä P, Koskinen S, Valkonen T. Income differences in mortality: a register-based follow-up study of three million men and women. Int J Epidemiol 2001;30:1397–405. [DOI] [PubMed] [Google Scholar]
- 22.Tjepkema M, Wilkins R, Long A. Cause-specific mortality by education in Canada: A 16-year follow-up study. Health Rep 2012;23:3–11. [PubMed] [Google Scholar]
- 23.Shkolnikov VM, Leon AC, Adamets S, Andreev E, Deev AD. Educational level and adult mortality in Russia: an analysis of routine data 1979 to 1994. Soc Sci Med 1998;47:357–69. [DOI] [PubMed] [Google Scholar]
- 24.Suhrcke M, Stuckler D. Will the recession be bad for our health? It depends. Soc Sci Med 2012;74:647–53. [DOI] [PubMed] [Google Scholar]
- 25.Stuckler D, Basu S, Suhrcke M, Coutts A, McKee M. The public health effect of economic crises and alternative policy responses in Europe: an empirical analysis. Lancet 2009;374:315–23. [DOI] [PubMed] [Google Scholar]
- 26.Stroup DF, Berlin JA, Morton S, et al. Meta-analysis of observational studies in epidemiology – A proposal for reporting. JAMA 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- 27.Mackenbach JP, Stirbu I, Roskam AJR, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med 2008;358:2468–81. [DOI] [PubMed] [Google Scholar]
- 28.Sanderson S, Tatt LD, Higgins JPT. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol 2007;36:666–76. [DOI] [PubMed] [Google Scholar]
- 29.DerSimoniain R, Laird N. Meta-analysis in clinical trials. Clin Trials 1986;7:177–88. [DOI] [PubMed] [Google Scholar]
- 30.Cochran WG. The combination of estimates from different experiments. Biometrics 1954;10:101–29. [Google Scholar]
- 31.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- 32.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 2002;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thompson SG, Higgins JPT. How should meta-regression analyses be undertaken and interpreted? Stat Med 2002;21:1559–73. [DOI] [PubMed] [Google Scholar]
- 34.Deeks JJ, Higgins JPT, Altman DG. Cochrane Handbook for Systematic Reviews of Interventions, Analysing Data and Undertaking Meta-Analyses . The Cochrane Collaboration; 2011, version 5.1.0. www.cochrane-handbook.org. [Google Scholar]
- 35.Leinsalu M, Vågerö D, Kunst AE. Estonia 1989-2000: Enormous increase in mortality differences by education. Int J Epidemiol 2003;32:1081–87. [DOI] [PubMed] [Google Scholar]
- 36.Valkonen T. Problems in the measurement and international comparison of socioeconomic differences in mortality. Soc Sci Med 1993;36:409–18. [DOI] [PubMed] [Google Scholar]
- 37.Koskinen S, Martelin T. Why are socioeconomic mortality differences smaller among women than among men. Soc Sci Med 1994;38:138–96. [DOI] [PubMed] [Google Scholar]
- 38.Mäkelä P, Valkonen T, Martelin T. Contribution of deaths related to alcohol use to socioeconomic variation in mortality: register based follow up study. BMJ 1997;315:211–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hemström Ö. Alcohol-related deaths contribute to socioeconomic differentials in mortality in Sweden. Eur J Public Health 2002;12:254–62. [DOI] [PubMed] [Google Scholar]
- 40.Kivimäki M, Vahtera J, Virtanen M, Elovainio M, Pentti J, Ferrie JE. Temporary employment and risk of overall and cause-specific mortality. Am J Epidemiol 2003;158:663–68. [DOI] [PubMed] [Google Scholar]
- 41.Voss M, Nylen L, Floderus B, Diderichsen F, Terry PD. Unemployment and early cause-specific mortality: A study based on the Swedish twin registry. Am J Public Health 2004;94:2155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kivimäki M, Gunnell D, Lawlor DA, et al. Social inequalities in antidepressant treatment and mortality: A longitudinal register study. Psychol Med 2007;37:373–82. [DOI] [PubMed] [Google Scholar]
- 43.Zagozdzon P, Zaborski L, Ejsmont J. Survival and cause-specific mortality among unemployed individuals in Poland during economic transition. J Public Health (Oxf) 2009;31:138–46. [DOI] [PubMed] [Google Scholar]
- 44.Faeh D, Bopp M; Swiss Natl Cohort Study G. Educational inequalities in mortality and associated risk factors: German- versus French-speaking Switzerland. BMC Public Health 2010;10:567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pridemore WA, Tomkins S, Eckhardt K, Kiryanov N, Saburova L. A case-control analysis of socio-economic and marital status differentials in alcohol- and non-alcohol-related mortality among working-age Russian males. Eur J Public Health 2010;20:569–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lau J, Ioannidis JPA, Schmid CH. Summing up evidence: one answer is not always enough. Lancet 1998;351:123–27. [DOI] [PubMed] [Google Scholar]
- 47.Knupfer G. The prevalence in various social-groups of 8 different drinking patterns, from abstaining to frequent drunkenness – Analysis of 10 United-States surveys combined. Br J Addiction 1989;84:1305– 18. [DOI] [PubMed] [Google Scholar]
- 48.Giskes K, Turrell G, Bentley R, Kavanagh A. Individual and household-level socioeconomic position is associated with harmful alcohol consumption behaviours among adults. Aust N Z J Public Health 2011;35:270–77. [DOI] [PubMed] [Google Scholar]
- 49.Van Oers JAM, Bongers IMB, Van de Goor LAM, Garretsen HFL. Alcohol consumption, alcohol-related problems, problem drinking, and socioeconomic status. Alcohol Alcohol 1999;34:78–88. [DOI] [PubMed] [Google Scholar]
- 50.Bloomfield K, Grittner U, Kramer S, Gmel G. Social inequalities in alcohol consumption and alcohol-related problems in the study countries of the EU concerted action ‘Gender, Culture and Alcohol Problems: A multi-national study’. Alcohol Alcohol 2006;41:I26–I36. [DOI] [PubMed] [Google Scholar]
- 51.Huckle T, You RQ, Casswell S. Socio-economic status predicts drinking patterns but not alcohol-related consequences independently. Addiction 2010;105:1192–202. [DOI] [PubMed] [Google Scholar]
- 52.Kuntsche S, Gmel G, Knibbe RA, et al. Gender and cultural differences in the association between family roles, social stratification, and alcohol use: a European cross-cultural analysis. Alcohol Alcohol Suppl 2006;41:i37–46. [DOI] [PubMed] [Google Scholar]
- 53.Marmot M. Inequality, deprivation and alcohol use. Addiction 1997;92:S13–S20. [PubMed] [Google Scholar]
- 54.Mäkelä P, Paljärvi T. Do consequences of a given pattern of drinking vary by socioeconomic status? A mortality and hospitalisation follow-up for alcohol-related causes of the Finnish drinking habits surveys. J Epidemiol Community Health 2008;62:728–33. [DOI] [PubMed] [Google Scholar]
- 55.Kaner EFS, Beyer F, Dickinson HO, et al. Effectiveness of brief alcohol interventions in primary care populations (review). Cochrane Database Syst Rev 2007;2:CD004148. [DOI] [PubMed] [Google Scholar]
- 56.Cuijpers P, Riper H, Lemmers L. The effects on mortality of brief interventions for problem drinking: a meta-analysis. Addiction 2004;99:839–45. [DOI] [PubMed] [Google Scholar]
- 57.Newacheck PW, Hung YY, Park MJ, Brindis CD, Irwin CE. Disparities in adolescent health and health care: Does socioeconomic status matter? Health Serv Res 2003;38:1235–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Steele L, Dewa C, Lee K. Socioeconomic status and self-reported barriers to mental health service use. Can J Psychiatry 2007;52:201–06. [DOI] [PubMed] [Google Scholar]
- 59.Fortney J, Mukherjee S, Curran G, Fortney S, Han XT, Booth BM. Factors associated with perceived stigma for alcohol use and treatment among at-risk drinkers. J Behav Health Serv Res 2004;31:418–29. [DOI] [PubMed] [Google Scholar]
- 60.Corrigan PW, Lurie BD, Goldman HH, Slopen N, Medasani K, Phelan S. How adolescents perceive the stigma of mental illness and alcohol abuse. Psychiatr Serv 2005;56:544–50. [DOI] [PubMed] [Google Scholar]
- 61.Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: a review of population studies. Alcohol Alcohol 2011;46:105–12. [DOI] [PubMed] [Google Scholar]
- 62.Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illnesses. Br J Psychiatry 2000;177:4–7. [DOI] [PubMed] [Google Scholar]
- 63.Keyes KM, Hatzenbuehler ML, McLaughlin KA, et al. Stigma and treatment for alcohol disorders in the United States. Am J Epidemiol 2010;172:1364–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Glass JE, Kristjansson SD, Bucholz KK. The influence of perceived alcoholism stigma on pathways into treatment for alcohol problems. Alcohol Clin Exp Res 2011;35:203A-A.21058961 [Google Scholar]
- 65.Turrell G, Kavanagh AM. Socio-economic pathways to diet: modelling the association between socio-economic position and food purchasing behaviour. Public Health Nutr 2006;9:375–83. [DOI] [PubMed] [Google Scholar]
- 66.Kjollesdal MKR, Holmboe-Ottesen G, Wandel M. Associations between food patterns, socioeconomic position and working situation among adult, working women and men in Oslo. Eur J Clin Nutr 2010;64:1150–57. [DOI] [PubMed] [Google Scholar]
- 67.Thornton LE, Bentley RJ, Kavanagh AM. Individual and area-level socioeconomic associations with fast food purchasing. J Epidemiol Community Health 2011;65:873–80. [DOI] [PubMed] [Google Scholar]
- 68.Giskes K, Turrell G, van Lenthe FJ, Brug J, Mackenbach JP. A multilevel study of socio-economic inequalities in food choice behaviour and dietary intake among the Dutch population: the GLOBE study. Public Health Nutr 2006;9:75–83. [DOI] [PubMed] [Google Scholar]
- 69.Tarasuk V, Fitzpatrick S, Ward H. Nutrition inequities in Canada. Appl Physiol Nutr Metab 2010;35:172–79. [DOI] [PubMed] [Google Scholar]
- 70.Lallukka T, Laaksonen M, Rahkonen O, Roos E, Lahelma E. Multiple socio-economic circumstances and healthy food habits. Eur J Clin Nutr 2007;61:701–10. [DOI] [PubMed] [Google Scholar]
- 71.Irala-Estevez JD, Groth M, Johansson L, Oltersdorf U, Prattala R, Martinez-Gonzalez MA. A systematic review of socio-economic differences in food habits in Europe: consumption of fruit and vegetables. Eur J Clin Nutr 2000;54:706–14. [DOI] [PubMed] [Google Scholar]
- 72.Shohaimi S, Welch A, Bingham S, et al. Residential area deprivation predicts fruit and vegetable consumption independently of individual educational level and occupational social class: a cross sectional population study in the Norfolk cohort of the European Prospective Investigation into Cancer (EPIC-Norfolk). J Epidemiol Community Health 2004;58:686–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Boylan S, Lallukka T, Lahelma E, et al. Socio-economic circumstances and food habits in Eastern, Central and Western European populations. Public Health Nutr 2011;14:678–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mezey E. Interaction between alcohol and nutrition in pathogenesis of alcoholic liver-disease. Semin Liver Dis 1991;11:340–48. [DOI] [PubMed] [Google Scholar]
- 75.Lieber CS. Relationships between nutrition, alcohol use, and liver disease. Alcohol Res Health 2003;27:220–31. [PMC free article] [PubMed] [Google Scholar]
- 76.Watzl B, Watson RR. Role of alcohol-abuse in nutritional immunosuppression. J Nutr 1992;122:733–37. [DOI] [PubMed] [Google Scholar]
- 77.Gramenzi A, Caputo F, Biselli M, et al. Review article: alcoholic liver disease – pathophysiological aspects and risk factors. Aliment Pharmacol Ther 2006;24:1151–61. [DOI] [PubMed] [Google Scholar]
- 78.Leevy CM, Moroianu SA. Nutritional aspects of alcoholic liver disease. Clin Liver Dis 2005;9:67–81. [DOI] [PubMed] [Google Scholar]
- 79.Samokhvalov A, Shuper PA, Rehm J. Infectious Disease. In: Boyle P, Boffetta P, Lowenfels AB, et al. (eds). Alcohol Science, Policy and Public Health. Oxford, UK: Oxford University Press, 2013. [Google Scholar]
- 80.Robertson A, Lobstein T, Knai C. Obesity and Socio-Economic Groups in Europe:Evidence Review and Implications for Action. Report SANCO/2005/C4-NUTRITION-03 . Brussels: European Commission, 2007. [Google Scholar]
- 81.Sassi F. Obesity and the Economics of Prevention: Fit not Fat. Paris: OECD Publishing, 2010. [Google Scholar]
- 82.Zhao J, Zhu Y, Wang PP, et al. Interaction between alcohol drinking and obesity in relation to colorectal cancer risk: a case-control study in Newfoundland and Labrador, Canada. BMC Public Health 2012;12:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Reid JL, Hammond D, Driezen P. Socio-economic status and smoking in Canada, 1999-2006: Has there been any progress on disparities in tobacco use? Can J Public Health 2010;101:73–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Barbeau EM, Krieger N, Soobader MJ. Working class matters: Socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. Am J Public Health 2004;94:269–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Schaap MM, van Agt HME, Kunst AE. Identification of socioeconomic groups at increased risk for smoking in European countries: Looking beyond educational level. Nicotine Tob Res 2008;10:359–69. [DOI] [PubMed] [Google Scholar]
- 86.Hiscock R, Bauld L, Amos A, Fidler JA, Munafo M. Socioeconomic status and smoking: a review. Ann N Y Acad Sci 2012;1248:107–23. [DOI] [PubMed] [Google Scholar]
- 87.Taylor B, Rehm J. When risk factors combine: The interaction between alcohol and smoking for aerodigestive cancer, coronary heart disease, and traffic and fire injury. Addict Behav 2006;31:1522–35. [DOI] [PubMed] [Google Scholar]
- 88.Zygogianni A, Kyrgias G, Mystakidou K, et al. Potential role of the alcohol and smoking in the squamous cell carcinoma of the head and neck: review of the current literature and new perspectives. Asian Pac J Cancer Prev 2011;12:339–44. [PubMed] [Google Scholar]
- 89.Rehm J, Taylor B, Patra J, Gmel G. Avoidable burden of disease: conceptual and methodological issues in substance abuse epidemiology. Int J Methods Psychiatr Res 2006;15:181–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shield K, Kehoe T, Gmel G, Rehm MX, Rehm J. Societal burden of alcohol. In: Anderson P, Moller L, Galea G (eds). Alcohol in the European Union Consumption, Harm and Policy Approaches. Copenhagen: WHO Regional Office for Europe, 2012. [Google Scholar]
- 91.Herttua K, Mäkelä P, Martikainen P. Changes in alcohol-related mortality and its socioeconomic differences after a large reduction in alcohol prices: a natural experiment based on register data. Am J Epidemiol 2008;168:1110–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Babor T, Caetano R, Casswell S, et al. Alcohol: No Ordinary Commodity: Research and Public Policy. Oxford, UK: Oxford University Press, 2010. [Google Scholar]
- 93.Graham K, Chandler-Coutts M. Community action research: Who does what to whom and why? Lessons learned from local prevention efforts (international experiences). Subst Use Misuse 2000;35:87–110. [DOI] [PubMed] [Google Scholar]
- 94.Holder HD, Moore RS. Institutionalization of community action projects to reduce alcohol-use related problems: Systematic facilitators. Subst Use Misuse 2000;35:75–86. [DOI] [PubMed] [Google Scholar]
- 95.Karanikolos M, Mladovsky P, Cylus J, et al. Financial crisis, austerity, and health in Europe. Lancet 2013;381:1323–31. [DOI] [PubMed] [Google Scholar]
- 96.Stuckler D, Basu S, McKee M. Budget crises, health, and social welfare programmes. BMJ 2010;340:c3311. [DOI] [PubMed] [Google Scholar]
- 97.Solberg LI, Maciosek MV, Edwards NM. Primary care intervention to reduce alcohol misuse. Ranking its health impact and cost effectiveness. Am J Prev Med 2008;34:143–52. [DOI] [PubMed] [Google Scholar]
- 98.Kristenson H, Osterling A, Nilsson JA, Lindgarde F. Prevention of alcohol-related deaths in middle-aged heavy drinkers. Alcohol Clin Exp Res 2002;26:478–84. [DOI] [PubMed] [Google Scholar]
- 99.Ballesteros J, Duffy JC, Querejeta I, Arino J, Gonzalez-Pinto A. Efficacy of brief interventions for hazardous drinkers in primary care: Systematic review and meta-analyses. Alcohol Clin Exp Res 2004;28:608–18. [DOI] [PubMed] [Google Scholar]
- 100.Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Brief physician advice for problem drinkers: Long-term efficacy and benefit-cost analysis. Alcohol Clin Exp Res 2002;26:36–43. [PubMed] [Google Scholar]
- 101.Stockwell T, Butt P, Beirness D, Gliksman L, Paradis C. The basis for Canada's new low-risk drinking guidelines: a relative risk approach to estimating hazardous levels and patterns of alcohol use. Drug Alcohol Rev 2012;31:126–34. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.