Abstract
BACKGROUND AND OBJECTIVES:
A 2007 meta-analysis showed probiotics, specifically Lactobacillus rhamnosus GG (LGG), shorten diarrhea from acute gastroenteritis (AGE) by 24 hours and decrease risk of progression beyond 7 days. In 2005, our institution published a guideline recommending consideration of probiotics for patients with AGE, but only 1% of inpatients with AGE were prescribed LGG. The objective of this study was to increase inpatient prescribing of LGG at admission to >90%, for children hospitalized with AGE, within 120 days.
METHODS:
This quality improvement study included patients aged 2 months to 18 years admitted to general pediatrics with AGE with diarrhea. Diarrhea was defined as looser or ≥3 stools in the preceding 24 hours. Patients with complex medical conditions or with presumed bacterial gastroenteritis were excluded. Admitting and supervising clinicians were educated on the evidence. We ensured LGG was adequately stocked in our pharmacies and updated an AGE-specific computerized order set to include a default LGG order. Failure identification and mitigation were conducted via daily electronic chart review and e-mail communication. Primary outcome was the percentage of included patients prescribed LGG within 18 hours of admission. Intervention impact was assessed with run charts tracking our primary outcome over time.
RESULTS:
The prescribing rate increased to 100% within 6 weeks and has been sustained for 7 months.
CONCLUSIONS:
Keys to success were pharmacy collaboration, use of an electronic medical record for a standardized order set, and rapid identification and mitigation of failures. Rapid implementation of evidence-based practices is possible using improvement science methods.
KEY WORDS: evidence-based practice, gastroenteritis, probiotics, quality improvement, diarrhea, Lactobacillus rhamnosus
Since the introduction of the rotavirus vaccine, disease burden attributable to acute gastroenteritis (AGE), as measured by health care utilization and costs, has decreased substantially.1,2 However, AGE remains a health care burden because of the approximately one-third of children younger than 3 who are unvaccinated2 or infected with other viruses.3
The mainstay treatment of AGE historically has been rehydration, which does not reduce the severity or duration of intestinal symptoms.4 A meta-analysis of the use of probiotics for pediatric AGE demonstrated that the probiotic strain Lactobacillus rhamnosus GG (LGG) showed significant reductions in the duration of diarrhea and risk of diarrhea lasting >7 days.5 Evidence-based guidelines produced in developed countries identify LGG as a valid and effective adjunct to oral rehydration for the treatment of AGE, as does a recent American Academy of Pediatrics clinical report.6–9 Adherence to one such guideline demonstrated shortened diarrhea and improved weight gain among children with AGE.10 Cincinnati Children’s Hospital Medical Center (CCHMC) has developed evidence-based guidelines for over 15 years. In 2005, our institution updated an evidence-based clinical practice guideline that recommended consideration of probiotic use for patients with AGE.11 Despite the evidence and local recommendation, only 1% of patients with AGE admitted to general pediatrics were prescribed probiotics.
The aim of this study was to increase the percentage of children with AGE admitted to general pediatrics who received LGG from 1% to >90% within 120 days.
Methods
Setting
CCHMC is a large, urban pediatric academic medical center that uses an electronic medical record (EMR). In fiscal year 2011, CCHMC had 200 patients admitted to general pediatrics with the diagnosis of AGE. Patients admitted to the general pediatric service are admitted at the main campus and a satellite community campus. At the main hospital, care is provided by teams of residents and medical students who are supervised by CCHMC pediatric hospitalists for 85% of the patients and community-based pediatricians for the remaining 15%. Approximately 160 medical students and 180 pediatrics residents receive clinical training annually on the main hospital general pediatric service. Care at the satellite community campus is almost exclusively given by attending physicians. This quality improvement (QI) initiative took place on 3 general pediatric inpatient units: 2 at the main campus and 1 at the satellite location.
Planning the Intervention
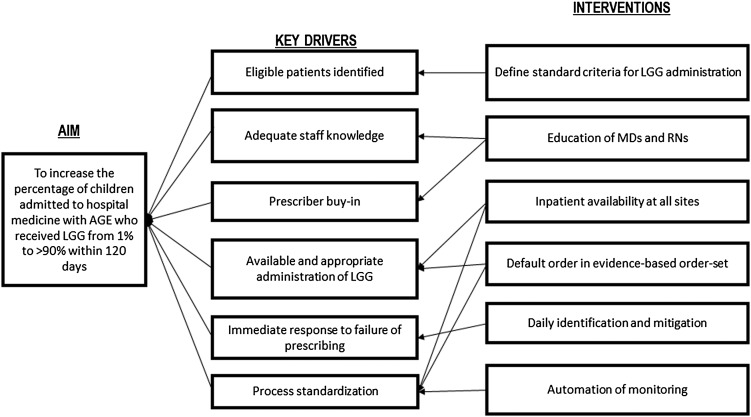
One CCHMC pediatric hospitalist attending physician and a visiting pediatrician co-led a multidisciplinary team that included other hospital medicine attending physicians, a research assistant, physician and nurse representatives of the evidence-based guideline development group, and a QI coach. The team used a Rapid Cycle Improvement Collaborative12 at CCHMC, which involved 7 group learning sessions over 4 months to learn the Model for Improvement13 and apply QI methods to achieve an improvement goal. The team met approximately weekly in the initial phase of the project to gauge progress and plan interventions. The team mapped the existing AGE admission process, conducted a failure mode effects analysis,14 identified key drivers of LGG use, and developed interventions to promote LGG use. Figure 1 depicts the final key driver diagram. Patients considered for inclusion were between 2 months and 18 years old and admitted to the general pediatric service with the diagnosis of AGE with diarrhea. Compliant with the World Health Organization definition, diarrhea was defined as decreased stool consistency or 3 or more stools in the preceding 24-hour period. Patients with complex comorbid conditions or with presumed bacterial gastroenteritis, such as patients presenting with bloody diarrhea, were excluded.
FIGURE 1.
Key driver diagram.
Improvement Activities
Interventions focused on 4 main areas to address the key drivers identified a priori. The interventions were tested through Plan-Do-Study-Act cycles.13
Education
In April 2011, the improvement team presented the evidence for LGG to residents and medical students at a morning conference and to the hospitalist attending physicians at a regularly scheduled meeting. At the session, participants completed pre- and post-assessment surveys on their knowledge and practice of the evidence that LGG, when administered to children with AGE, shortens the course of acute and protracted diarrhea. Nursing staff on the general units were informed of this same information by nursing leadership. A second educational session was given in July 2011 to teach the incoming residents and remind the existing residents about probiotics and AGE.
To spread knowledge of the evidence and the improvement efforts, several means of communication were used to reach out to community physicians and other members of the CCHMC community. A 1-page flyer summarizing the evidence and implementation project was disseminated by CCHMC representatives who serve as liaisons between the hospital and community-based practices. A paragraph on the evidence and the QI project was also posted on the CCHMC internal Web site and included in an institution-wide bulletin distributed to medical staff. Contact information for the team leaders and a Web link to our institutional Best Evidence Statement,15 which summarizes the evidence for use of LGG in children with diarrhea, were included on all materials.
To further remind residents and orient visiting residents and medical students to the project, a member of the improvement team attended the monthly general pediatric teams’ orientation meeting to provide a 1- to 2-minute reminder. Relevant information regarding eligibility criteria and dosage information was posted in the resident team rooms and on the resident Web site. Several months into the project, the residency program implemented a shift-based schedule to address new Accreditation Council for Graduate Medical Education work-hour restrictions. Consequently, residents working the night shift were not able to attend the team orientation meeting. To educate this subset, 2 slides summarizing the LGG project were delivered during their existing weekly evening educational sessions.
Updated run charts were posted in both resident team rooms and attending workrooms to provide feedback on performance.
Pharmacy
In April 2011, our improvement group partnered with pharmacy to ensure LGG was available in an adequate dose of 1010 colony-forming units per capsule, and was stocked at both the main and satellite locations, as it had previously only been stocked at the main location.
Order Set
To incorporate a higher reliability intervention,16,17 the team worked with an EMR system specialist to update the existing gastroenteritis order set to include a hyperlink to the Best Evidence Statement and an order that defaulted to the prescription of LGG specifying the appropriate dose and schedule of administration. Practitioners choosing the AGE order set needed to delete the order for LGG to not prescribe LGG.
Identify and Mitigate
A research assistant reviewed the EMR each weekday to identify eligible patients with AGE. To prevent failures, the research assistant notified the attending physician and residents responsible for the patient’s care by e-mail when an eligible patient was identified who did not have LGG ordered. The e-mail notification included a reminder of the LGG project aim, evidence for LGG use in patients with AGE, and information on the appropriate dosage and timing of administration. This mitigation strategy was designed to remind the team so they could prescribe LGG if deemed medically appropriate and also to reinforce the practice change. These e-mail notifications were recently discontinued in an effort to scale down improvement efforts.
Methods of Evaluation
Preintervention data were collected through manual chart review of all patients discharged from the general pediatrics service between January 1 and April 3, 2011. Postintervention data were obtained through a daily manual electronic chart review of eligible patients admitted between April 4, 2011, and February 26, 2012. To identify eligible patients, a research assistant trained in data collection and interpretation reviewed the list of general pediatrics patients each weekday, searching the problem list created by the admitting team for the following keywords: acute gastroenteritis, diarrhea, dehydration, or vomiting. Each Monday morning, the research assistant also reviewed patients admitted during the weekend. Once a patient was identified, the research assistant reviewed the medical record and applied inclusion and exclusion criteria and case definitions to determine eligibility. When eligibility was uncertain, the case was reviewed with at least 2 physicians on the improvement team to reach consensus. Prescription of LGG at admission was defined as LGG being ordered for an eligible patient within 18 hours of admission, regardless of whether the team received a reminder.
Analysis
Pre and post data from educational sessions were analyzed by using a χ2 test to calculate values for statistical significance. The research assistant recorded performance data and created run charts using Microsoft Excel (Microsoft, Redmond, WA). Run charts were updated weekly to reflect the percentage of eligible patients receiving LGG, and displayed data in a timed sequence to help detect special causes of variation.18
Human Subject Protection
The CCHMC institutional review board reviewed the project and considered it to be a local QI initiative and not research involving human subjects. Informed consent beyond the standard consent for treatment of all inpatients was not required.
Results
Pre- and postassessment surveys for the attending physicians, residents, and medical students on their LGG knowledge demonstrated that the educational sessions significantly improved knowledge of LGG efficacy and improved their likelihood to prescribe probiotics (Table 1).
TABLE 1.
Survey of Practitioners’ Knowledge About Probiotics and Current or Planned Prescribing Habits
| Before Probiotic Education | After Probiotic Education | P Value | |
|---|---|---|---|
| I typically treat children with AGE with probiotics. | % agreement | % agreement | |
| Residents or medical students (n = 30) | 0 | 80 | .001 |
| Hospital medicine attending physicians (n = 11) | 18 | 63 | .001 |
| The evidence supports probiotics’ reduction of diarrhea. | % correct | % correct | |
| Residents or medical students (n = 30) | 55 | 96 | .001 |
| Hospital medicine attending physicians (n = 11) | 70 | 100 | <.001 |
| Probiotics have a dose-dependent efficacy. | % correct | % correct | |
| Residents or medical students (n = 30) | 59 | 100 | .001 |
| Hospital medicine attending physicians (n = 11) | 70 | 100 | <.001 |
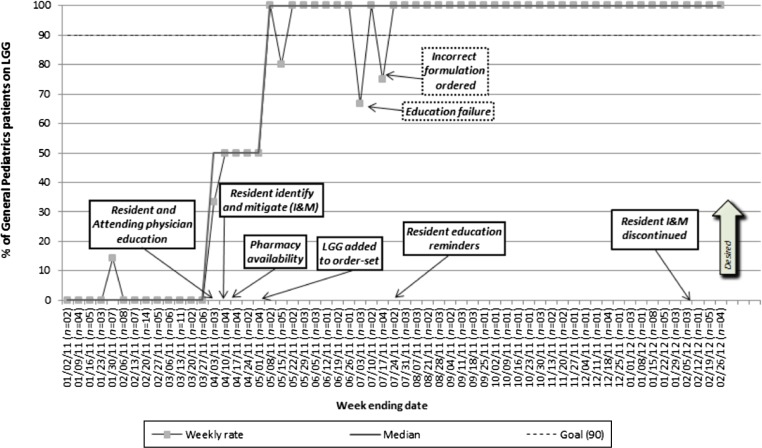
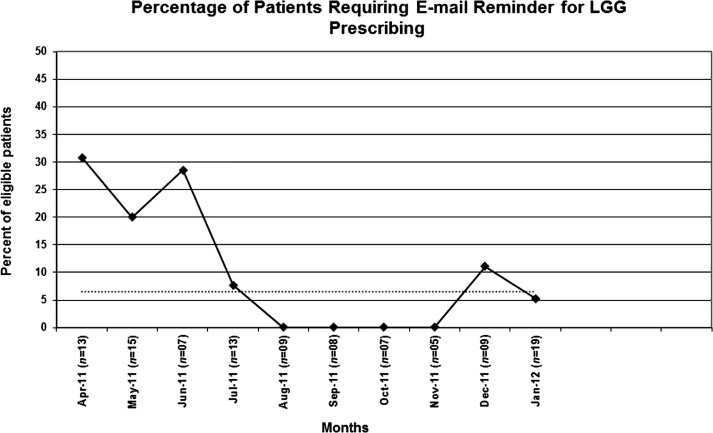
Prescription of LGG at admission for children with AGE increased from 1% to 100% within 6 weeks of beginning the project (Fig 2). Three failures occurred soon after the new interns started in July 2011. Subsequently, prescribing of LGG at admission has been sustained for the past 7 months at 100%. The percentage of eligible patients requiring real-time e-mail mitigation had declined since the early phases of the project (Fig 3).
FIGURE 2.
Run chart depicting prescription rate of LGG over time. Annotations denoting timing of designed interventions.
FIGURE 3.
Run chart of percentage of patients requiring e-mail reminder for prescribing.
Discussion
We used improvement science and reliability methods17 to successfully implement an evidence-based practice change within 6 weeks that has been sustained for >7 months. Improvement science is the application of the scientific method to improve health care delivery systems.13,19 Historically, practice change that adopts evidence-based recommendations is a slow process, taking on average 17 years for research to be translated into practice.20 Our Hospital Medicine division has had similar success with changing practice related to hand hygiene21,22 and rapid adoption of evidence to change practice regarding the treatment of osteomyelitis.23 We propose that rapid and sustainable evidence-based practice change can be achieved by applying improvement science methods.
Education is often the first step in any change process; however, education and training are low reliability interventions when used alone.17 Thus, a successful change initiative must include additional strategies to achieve sustainability. In our project, we used education to develop consensus for the practice change, to ensure that physicians and nurses understood the potential risks and benefits of LGG, and to establish the foundation for subsequent interventions. We learned from our failures in July that given the frequent change of care providers within an academic setting, repetition of education was essential; however, as the message spread among our care teams, less formalized, more concise education proved effective.
Key partnerships within our institution led to interventions incorporating higher reliability interventions that helped us to achieve our goal. The inpatient pharmacy took steps to ensure that LGG was available in the correct formulation at both inpatient sites. EMR analysts modified an existing order set to include LGG as the default order at the correct dose. In addition to facilitating LGG ordering, the EMR afforded us the ability to identify eligible patients quickly. Once identified, near real-time mitigation of failures in LGG ordering helped to increase our success, especially during the initial weeks of the project. This project leveraged the existing relationships, the value of evidence-based practice, and the culture of QI that exists within our institution. However, we do not believe that such efforts are limited to facilities with an existing QI framework, as optimized care delivery based on evidence is a universal concept.
There are some limitations to our rapid implementation project. Because the volume of patients admitted from week to week was small, we cannot say if the methods are generalizable to higher-volume conditions. Reliable delivery of evidence-based care may require different interventions when addressing low- versus high-volume conditions. Because the purpose of the project was to create a framework for evidence-based practice implementation based on a target with a solid foundation of evidence for efficacy with minimal harm, LGG for use in children with AGE was an excellent place to start.5–9 Although no staff were added as a result of our project, the effort was relatively great, involving research assistant, physician, and pharmacist time. In our experience, chart review and identification and mitigation need not be conducted by a research assistant. With the proper training, a resident, medical student, or administrative assistant would be able to complete the task with relatively minimal physician or pharmacist oversight. Our next steps include further decreasing the labor required to sustain our system. This will include automation of eligible patient identification using the EMR and switching to a retrospective review process, as recent performance has been sustained with sufficiently minimal need to identify and mitigate (Fig 3), which allowed this effort to be discontinued with maintained success.
A second limitation of our study is our reliance on documentation in the EMR (eg, diagnosis in problem list) to identify eligible patients. Chart review has been shown to improve the positive predictive value of case identification using International Classification of Diseases, Ninth Revision codes, but still achieved only an 85% positive predictive value in 1 study.24 Thus, we may not have identified all eligible patients. To limit this as a potential for bias, we used a single trained reviewer who used a standardized approach to identify eligible patients and collect patient data. Additionally, when the reviewer was unsure whether to include or exclude a patient, we used a consensus process to guard against misclassification.
The finding of a low baseline prescription rate in the face of extensive evidence and local recommendation was somewhat surprising, but this same practice pattern has been noted among the international pediatric gastroenterology community.25 As we disseminated our education, we discovered a number of barriers that may have contributed to this phenomenon. First, we were not able to cite strong evidence that use of LGG in an inpatient setting decreases length of stay. The average length of stay for AGE in our institution is 39 hours. Based on this short time frame and our small sample size, we were unable to demonstrate any benefit of LGG therapy on this outcome (data not shown). However, starting LGG on admission could have an effect after discharge by hastening the child’s return to school and parents’ return to work. Neither was measured in our study because health outcomes after discharge were beyond the scope of our rapid implementation QI project. Second, LGG is considered a dietary supplement by the Food and Drug Administration. Therefore, the dosage contained in each capsule may not be as precise as with a drug regulated by the Food and Drug Administration, and it is not covered by most prescription insurance. To overcome these potential issues, we selected a commercially available LGG formulation that best evidence suggests would yield the greatest therapeutic benefit (1010 colony-forming units).9 We also worked with our outpatient pharmacy to reduce the out-of-pocket expense to the family by offering prescriptions of remaining doses of LGG, rather than requiring purchase of a 30-pill package.
This second barrier has generated interest in family preferences for LGG. Because most patients’ insurance will not cover the cost of LGG, parents are faced with a decision at discharge of whether they are willing to pay out-of-pocket to complete the 7-day course to potentially shorten the duration of diarrhea by 1 day. Viewed from this perspective, LGG is a preference-sensitive decision.26 We are currently studying parental preferences through the development and testing of a decision aid that engages families in the decision to give LGG to their child.
Finally, we have begun to spread the framework of rapid adoption of evidence-based practice using QI science. Current efforts within our institution include rapid implementation of published evidence-based guidelines for the management of first urinary tract infection,27 ongoing implementation of evidence and shared decision making for osteomyelitis,23 and planned implementation of evidence-based guidelines for the management of community-acquired pneumonia.28,29
Conclusions
The rapid implementation of evidence-based practice is possible when using improvement science methods. Keys to the success of our specific project were interdisciplinary collaboration, use of an EMR, and identification and mitigation of failures.
Acknowledgments
We thank the CCHMC Hospital Medicine faculty and pediatrics residents for their enthusiasm and commitment, as well as Evaline A. Alessandrini, Melissa Healey, Trina Hemmelgarn, Diane Herzog, Betsy List, Gayle Lykowski, Kate Rich, and Karen Tucker, whose collaborative efforts made this possible.
Glossary
- AGE
acute gastroenteritis
- CCHMC
Cincinnati Children’s Hospital Medical Center
- EMR
electronic medical record
- LGG
Lactobacillus rhamnosus GG
- QI
quality improvement
Footnotes
Drs Parker, Schaffzin, Lo Vecchio, Simmons and Ms Yau, Vonderhaar, Gerhardt contributed to the acquisition of data. Drs Parker, Schaffzin, Lo Vecchio, Guiot, Brinkman, White, Simmons and Ms Yau, Vonderhaar, Gerhardt drafted the manuscript. All authors are responsible for the reported research, participated in the concept and design, analysis and interpretation of data, drafting and revising of the manuscript, contributed to the critical revision of the manuscript for important intellectual content, and approved the manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
References
- 1.Cortes JE, Curns AT, Tate JE, et al. Rotavirus vaccine and health care utilization for diarrhea in US children. N Engl J Med. 2011;365(12):1108–1117 [DOI] [PubMed] [Google Scholar]
- 2.Payne DC, Staat MA, Edwards KM, et al. Direct and indirect effects of rotavirus vaccination upon childhood hospitalizations in 3 US counties, 2006–2009. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 2011;53:245–53 [DOI] [PubMed]
- 3.Elliott EJ. Acute gastroenteritis in children. BMJ. 2007;334(7583):35–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murphy C, Hahn S, Volmink J. Reduced osmolarity oral rehydration solution for treating cholera. Cochrane Database Syst Rev. 2004;(4):CD003754. [DOI] [PubMed] [Google Scholar]
- 5.Szajewska H, Skórka A, Ruszczyński M, Gieruszczak-Białek D. Meta-analysis: Lactobacillus GG for treating acute diarrhoea in children. Aliment Pharmacol Ther. 2007;25(8):871–881 [DOI] [PubMed] [Google Scholar]
- 6.Guarino A, Albano F, Ashkenazi S, et al. European Society for Paediatric Gastroenterology, Hepatology, and Nutrition. European Society for Paediatric Infectious Diseases . European Society for Paediatric Gastroenterology, Hepatology, and Nutrition/European Society for Paediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe. J Pediatr Gastroenterol Nutr. 2008;46(suppl 2):S81–S122 [DOI] [PubMed] [Google Scholar]
- 7.Harris C, Wilkinson F, Mazza D, Turner T, Health for Kids Guideline Development Group . Evidence based guideline for the management of diarrhoea with or without vomiting in children. Aust Fam Physician. 2008;37(spec no. 6):22–29 [PubMed] [Google Scholar]
- 8.National Institute for Health and Clinical Excellence (UK). Clinical guideline on Diarrhoea and Vomiting Caused by Gastroenteritis: Diagnosis, Assessment and Management in Children Younger than 5 Years. London; 2009. Available at: http://publications.nice.org.uk/diarrhoea-and-vomiting-in-children-cg84. Accessed January 22, 2013. [PubMed]
- 9.Thomas DW, Greer FR, American Academy of Pediatrics Committee on Nutrition. American Academy of Pediatrics Section on Gastroenterology, Hepatology, and Nutrition . Probiotics and prebiotics in pediatrics. Pediatrics. 2010;126(6):1217–1231 [DOI] [PubMed] [Google Scholar]
- 10.Albano F, Lo Vecchio A, Guarino A. The applicability and efficacy of guidelines for the management of acute gastroenteritis in outpatient children: a field-randomized trial on primary care pediatricians. J Pediatr. 2010;156(2):226–230 [DOI] [PubMed] [Google Scholar]
- 11.Cincinnati Children’s. Evidence-based clinical care guideline for medical management of acute gastroenteritis in children aged 2 months through 5 years. 2005. Available at: www.cincinnatichildrens.org/service/j/anderson-center/evidence-based-care/gastroenteritis/. Accessed February 1, 2012
- 12.Cincinnati Children’s. Improvement science education. 2011. Available at: www.cincinnatichildrens.org/service/j/anderson-center/education/additional-programs/. Accessed February 1, 2012
- 13.Langley GJ, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco, CA: Jossey Bass; 2009 [Google Scholar]
- 14.DeRosier J, Stalhandske E, Bagian JP, Nudell T. Using health care failure mode and effect analysis: the VA National Center for Patient Safety's prospective risk analysis system. Jt Comm J Qual Improve 2002;28:248–67, 09 [DOI] [PubMed]
- 15.Cincinnati Children's Hospital Medical Center. Use of Lactobacillus rhamnosus GG in children with acute gastroenteritis. Available at: http://www.cincinnatichildrens.org/workarea/linkit.aspx?linkidentifier=id&itemid=88039&libid=87727. Accessed March 3, 2012 [Google Scholar]
- 16.Nolan T, Resar R, Haraden C, Griffin FA. Improving the Reliability of Health Care. In: IHI Innovation Series white paper. Boston, MA: Institute for Healthcare Improvement; 2004:1–16. Available at: www.ihi.org/knowledge/Pages/IHIWhitePapers/ImprovingtheReliabilityofHealthCare.aspx. Accessed March 3, 2012
- 17.Luria JW, Muething SE, Schoettker PJ, Kotagal UR. Reliability science and patient safety. Pediatr Clin North Am. 2006;53(6):1121–1133 [DOI] [PubMed] [Google Scholar]
- 18.Provost LP, Murray SK. The Health Care Data Guide: Learning From Data for Improvement. 1st ed. San Francisco, CA: Jossey-Bass; 2011 [Google Scholar]
- 19.Deming W. The New Economics for Industry, Government, Education. Cambridge, MA: Massachusetts Institute of Technology, Center for Advanced Engineering Study; 1993 [Google Scholar]
- 20.Balas EA, Boren SA. Managing clinical knowledge for health care improvement. In: van Bemmel JH, McCray AT, eds. Yearbook of Medical Informatics 2000: Patient-centered Systems. Bethesda, MD: Schattauer; 2000:65–70 [PubMed] [Google Scholar]
- 21.Linam WM, Margolis PA, Atherton H, Connelly BL. Quality-improvement initiative sustains improvement in pediatric health care worker hand hygiene. Pediatrics. 2011;128(3). Available at: www.pediatrics.org/cgi/content/full/128/3/e689. [DOI] [PubMed] [Google Scholar]
- 22.White CM, Statile AM, Conway PH, et al. Utilizing improvement science methods to improve physician compliance with proper hand hygiene. Pediatrics. 2012;129(4). Available at: www.pediatrics.org/cgi/content/full/129/4/e1042. [DOI] [PubMed] [Google Scholar]
- 23.Conway PH, Kirkendall E, Vossmeyer M, et al. Rapid Adoption of Evidence for Treatment of Routine Osteomyelitis. (Oral Presentation) 2011 Pediatric Academic Societies/Asian Society for Pediatric Research Joint Meeting. Denver, CO; 2011. [Google Scholar]
- 24.Tieder JS, Hall M, Auger KA, et al. Accuracy of administrative billing codes to detect urinary tract infection hospitalizations. Pediatrics. 2011;128(2):323–330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weizman Z. Probiotics use in childhood acute diarrhea: a web-based survey. J Clin Gastroenterol. 2011;45(5):426–428 [DOI] [PubMed] [Google Scholar]
- 26.Wennberg JE, Fisher ES, Skinner JS. Geography and the debate over Medicare reform. Health Aff (Millwood). 2002;(suppl Web exclusives):W96–114. [DOI] [PubMed] [Google Scholar]
- 27.Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management, Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128(3):595–610 [DOI] [PubMed] [Google Scholar]
- 28.Bradley JS, Byington CL, Shah SS, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis 2011;53:e25–76 [DOI] [PMC free article] [PubMed]
- 29.Harris M, Clark J, Coote N, et al. British Thoracic Society guidelines for the management of community acquired pneumonia in children: update 2011. Thorax. 2011;66(suppl 2):ii1–23 [DOI] [PubMed]